Abstract
Introduction:
Following inception in 2005 as a multiregional practice-based research network (PBRN), the “National Dental PBRN” expanded nationwide in 2012, and in 2019 implemented additional organizational changes. The objectives are to: (1) describe the new structure and function of the network; and (2) quantify its scientific productivity since 2005.
Methods:
A national Administrative and Resource Center is based in Alabama; regional and specialty nodes are based in Alabama, Florida, Illinois, Minnesota, Oregon, New York, and Texas. A Network Coordinating Center is based in Oregon. Studies are funded via investigator-initiated grants. Scientific productivity is assessed using specific metrics, including the Relative Citation Ratio.
Results:
To date, 58 studies have been completed or are in data collection or development. These studies have investigated a broad range of topics using a wide variety of study designs. Of the studies that have completed enrollment, 70,665 patients were enrolled, as were 19,827 practitioners (some participated in multiple studies), plus electronic records for 790,493 patients in two data-only studies. To date, these studies have led to 193 peer-reviewed scientific publications in 62 different journals. The mean (1.40) Relative Citation Ratio of Network publications connotes a greater-than-average influence in their fields.
Conclusions:
These metrics demonstrate that the PBRN research context can successfully engage practitioners and patients from diverse settings nationally with a high and sustained level of scientific productivity. This infrastructure has enabled clinical scientists in oral health and nonoral health topics and provided additional recruitment venues outside of the typical academic health center research context.
Keywords: Research infrastructure, multicenter studies, metrics, practice-based research networks, practice patterns
Introduction
Practice-based research networks (PBRNs) offer unique advantages to clinical research and quality improvement [1-6], primarily because they bring practice-relevant topics onto the research agenda and are conducted in “real-world,” nonacademic clinical settings where almost all of the population receives its health care. Historically most PBRNs have focused on medical care [7], but a recent review documented the growth in number of dental PBRNs [8]. This review concluded that the largest dental PBRN globally is the “National Dental PBRN” (“Network”), and relied on the Network’s most-recent publication about these topics (from 2013) [9]. From 2005 to 2012, the Network operated as a multiregional PBRN in four USA regions and one region that comprised three Scandinavian countries. From 2012 to 2019, the Network became nationwide throughout the USA as six regions and no longer operated a Scandinavian region. Beginning in 2019, new organizational changes were made, the description of which comprises one purpose of this current article.
Journal impact factor and the h-index [10] are commonly used measures of scientific impact. However, these metrics have important limitations, such as obscuring large differences in the influence of individual articles or undervaluing some fields of research by failing to normalize raw citation counts. In an effort to address the limitations of these and other measures, the Relative Citation Ratio (RCR) was developed to quantify the influence of a research article that is article level and independent of the scientific field [11]. To facilitate its public use, a National Institutes of Health (NIH) PubMed site was established [12]. All peer-reviewed articles from NIH-funded studies are required to be publicly available in this database [13].
The aforementioned review [8] compared scientific productivity between PBRNs and independent investigative teams. These comparisons included number of publications, range of clinical topics studied, and number of practitioners and patients enrolled. Only limited information was available to the authors about network-specific productivity. Indeed, reports of PBRN performance metrics are rare for both medical and dental PBRNs, and have primarily focused on the number of studies completed and the number of participants involved [6,14,15]. There is no broad consensus about which metrics to quantify productivity across PBRNs and other research networks. The National Dental PBRN has reported productivity based on the metrics of practitioner engagement (e.g., practitioner participation in studies, webinars, network activities that provide continuing education credit, presentations and publications, and practitioner meetings) [16,17], but has not reported other measures of overall network scientific productivity, such as the number of peer-reviewed publications and impact as measured by RCR. Therefore, this article aims to: (1) describe the new organizational structure and function of the Network and (2) quantify the Network’s scientific productivity.
Methods
The Network’s mission is “To improve oral health by conducting dental practice-based research and by serving dental professionals through education and collegiality.” It seeks to maximize the practicality of conducting research in everyday clinical practice across geographically dispersed regions and diverse practice types. Its structure is designed to focus some activities at the regional level (e.g., interactions with practitioners), while managing other activities centrally (e.g., study development).
Overall Network Structure and Oversight
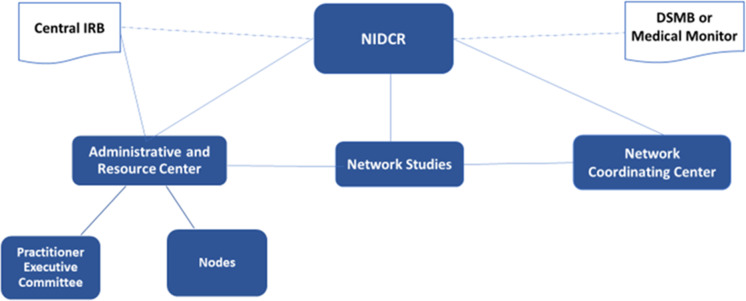
The overall structure of the Network was revised in 2019 [18,19], as depicted in Fig. 1. The Network’s main funder is NIH. An Administrative and Resource Center (ARC) and Network Coordinating Center (NCC) support the infrastructure for study development and implementation. The NCC is located in Oregon and provides both scientific and administrative functions. NCC biostatisticians support study development and analysis plans and NCC management staff provide support for study operations and data management. The NCC also designs and implements technology for the network “Hub” which supports the practitioner and participation databases; houses key network-wide documents; implements and tracks study data collection, data quality management, study monitoring procedures, and data analysis. The ARC is the national administrative base (located in Alabama) for six regional nodes and one specialty node that span all 50 US states and territories. Nodes are administratively based in Alabama, Florida, Minnesota, New York, Oregon, Illinois, and Texas. All enrolled practitioners are associated with one of these regional centers. The ARC also directs “Components” focused on specific administrative tasks: a Communications and Dissemination Component; a Practitioner Recruitment and Engagement Component; a Practitioner Training Component; and a Practitioner and Patient Compensation System, which are based either in Alabama or Florida. Each Component Director and Node Director reports to the National Network Director, who is responsible for overall scientific, technical, and administrative leadership and who has primary responsibility for planning and directing Network infrastructure and managing Network operations and fiscal resources. Also shown in Fig. 1, the ARC manages the Practitioner Executive Committee (PEC) and Network interactions with the Central Institutional Review Board (CIRB; ethics committee). The PEC comprises practitioner representatives from each Network region, who provides input about the design, feasibility, and clinical interest of studies and research topics. The Network’s CIRB has been in operation since 2014 and enables the Network to comply with the NIH policy that requires a single IRB review for multi-site studies involving nonexempt human subject research in which each site conducts the same protocol.
Fig. 1.
Overall network structure and oversight. DSMB: Data Safety and Monitoring Board; IRB: Institutional Review Board; NIDCR: National Institute of Dental and Craniofacial Research
Fig. 1 also depicts a Data and Safety Monitoring Board (DSMB). The DSMB is an independent group of experts that advises the NIH and study investigators on clinical studies, especially studies that involve an intervention. Its responsibilities include monitoring human subject safety; evaluating study data; reviewing study conduct and progress; and making recommendations to NIH concerning a study’s continuation, modification, or termination. NIH may appoint a “medical monitor” instead of a DSMB for minimal-risk studies.
Overall Committee Operations
Committees manage the bulk of Network operations. The main committee operational structure is depicted in Fig. 2. All committees have both ARC and NCC representation, and one of these two entities takes main responsibility for each committee. Study Principal Investigators lead “Study Teams,” which also include assigned ARC and NCC staff. Committees and Study Teams meet either weekly, biweekly, monthly, or quarterly, depending on the committee.
Fig. 2.
Network committee structure. ARC: Administrative and Resource Center; NCC: Network Coordinating Center; DSMB: Data Safety and Monitoring Board; IRB: Institutional Review Board; NIDCR: National Institute of Dental and Craniofacial Research.
The Directors Committee provides primary operational oversight. This committee is responsible for optimizing and monitoring overall Network performance, prioritizing tasks, and approving study administration policies and procedures. It also reviews study coordination across nodes and makes decisions about practitioner recruitment, training, and engagement.
The ARC/NCC Leadership Team acts on behalf of the Directors Committee to facilitate its work. This group manages on a weekly to biweekly basis the operational and business components of the Network.
The Coordination Committee discusses node coordination and study implementation issues, shares best practices, and provides a forum for node coordinators and NCC Study Managers to collaborate throughout study development/implementation.
The IRB Committee implements the policies and operations of the CIRB. Because the CIRB has been in operation for several years, it currently meets on a rare, ad hoc basis only.
The Publications and Presentations Committee implements and ensures compliance with the Network’s publications policies document [20].
The Data Committee develops and implements strategies to standardize, collect, manage, analyze and share Network data; provides guidance on data collection tools and prioritizes data quality measures.
The Technology and Infrastructure Committee identifies, prioritizes, and evaluates Network “Hub” needs and functionality.
Study Teams are responsible for developing study-specific documents and procedures to ensure efficient implementation in the Network, providing input regarding data management systems for data collection and quality management activities, preparing documents for CIRB submission, and adhering to NIH policies. During the implementation phase, study teams are responsible for meeting enrollment and retention targets, implementing quality management processes, reporting, and responding to requests regarding study oversight.
Other Operations
Other key operations of the Network have remained very similar to that which was reported in our earlier publication [9]. These operations include recruitment and retention activities, enrollment processes, practitioner engagement activities, and the benefits of participating as communicated by network practitioners. Previous publications have reported the number and characteristics of Network practitioners, and these numbers also are almost always reported during study-specific publications. Appendix A provides descriptive information about currently enrolled numbers.
Measures of Study Characteristics
A broad range of study types is conducted in the Network. These include national clinical observational studies, national experimental (randomized clinical trial) studies, national questionnaire studies, pilot clinical studies, clinical simulation studies, and qualitative studies. Most studies are conducted nation-wide, but some involve only one to three regions. Many different funding mechanisms have been used since the Network’s inception in 2005, but since 2019 the Network has conducted only investigator-initiated studies; these are usually funded through specific NIH mechanisms [21,22]. Study length has ranged from less than a year to 3 years.
Clinical topics were categorized into one or more treatment classifications based on the American Dental Association Current Dental Terminology codes [23], with these classifications: Diagnostic; Preventive; Restorative; Endodontics; Periodontics; Prosthodontics (combined categories of Removable Prosthodontics, Maxillofacial Prosthetics, Implant Services, and Fixed Prosthodontics); Oral and Maxillofacial Surgery; Orthodontics; Adjunctive General Services. Clinical topics based on treatment classification were chosen instead of a diagnostic classification system because a single treatment may be the result of different diagnoses, and because in our experience Network clinicians often conceptualize clinical topics in treatment terms. We acknowledge that diagnostic codes, if they were widely recorded in everyday clinical dental practice, would enable a better linkage to health outcomes [24]. The Network also has had an impact internationally by either advising about the formation of new networks in other countries, such as in Japan and Brazil, or collaborating in research studies with investigators in the United Kingdom.
Measures of Scientific Productivity
Given that a key aspect of the Network’s mission is to conduct research studies and impact the field of clinical research and clinical care, we quantified metrics that have to do with study characteristics and publications: (1) number of studies conducted; (2) breadth of clinical topics investigated; (3) number of practitioners and patients enrolled; (4) number of peer-reviewed scientific publications produced; (5) scientific influence as measured by number of citations, RCRs, and weighted RCRs for Network peer-reviewed publications with a publication date of 2020 or earlier (n = 167); and (6) number of different journal titles.
All Network publications are included in the NIH PubMed database in compliance with NIH policy, making access to their PubMed identification number (“PMID”) publicly available and easily entered into the NIH iCite website for quick calculation. We used the iCite tool [12] for citation, RCR, and weighted RCR calculations.
RCR represents the field-normalized and time-normalized citation rate. Article citation rates are divided by an expected citation rate derived from the performance of articles in the same field and benchmarked to a peer comparison group. Fields are defined for each article by using its co-citation network. The RCR is benchmarked to 1.0 for a typical (median) NIH paper in the corresponding year of publication, ensuring that a paper with a median RCR of 1.0 has received the same number of citations per year as the median NIH-funded paper in its field, while a paper with a RCR of 2.0 has received twice as many citations per year as the median NIH-funded paper in its field. RCR data are available for articles that are at least one calendar year old. The database contains many papers that were not NIH funded and the same RCR value translates to a lower percentile ranking for papers that are not NIH funded. The RCR methodology was validated using citation data from about 90,000 published papers emanating from NIH-funded research and comparing calculated RCRs to the opinions on manuscript reach of recognized experts in selected fields. The weighted RCR is the sum of RCRs for Network articles, which weights the article count by their influence relative to NIH-funded papers. A highly influential set of articles will have a higher weighted RCR than the number of total publications, while a set of articles with below-average influence will have a lower weighted RCR than the number of total publications.
Results
Study Characteristics
Table 1 lists the characteristics of Network studies completed in data collection or in development. Fifty-six studies have been completed or are in development.
Table 1.
Characteristics of 58 Network studies completed or in development as of June 2022
| Study # | Study title | Study design | # practitioners |
# patients | Study type(s) | Clinical topic category(ies) |
|---|---|---|---|---|---|---|
| Conducted from 2005 to 2012 | ||||||
| 1 | Dental tobacco control RCT | Randomized clinical trial | 190 | 11,898 | Qx and Clinical | Preventive |
| 2 | Practice-based root canal treatment effectiveness 1 | Retrospective cohort study | 13 | 84 | Clinical | Endodontics |
| 3 | Assessment of caries diagnosis and treatment | Cross-sectional (paper Qx to dentists) | 494 | -- | Qx | Diagnostic; Restorative |
| 4 | Reasons for placing the first restoration on permanent tooth surfaces | Cross-sectional; consecutive patients | 192 | 4844 | Clinical | Restorative |
| 5 | Reasons for replacement or repair of dental restorations | Cross-sectional; consecutive patients | 157 | 6092 | Clinical | Restorative |
| 6 | CONDOR case-control study of ONJ 2 | Case-control study | 81 | 764 | Clinical | Oral/Max Surgery |
| 7 | Retrospective cohort study of ONJ | Retrospective cohort study using electronic data | -- | 572,606 | Clinical | Oral/Max Surgery |
| 8 | Longitudinal study of dental restorations placed on previously un-restored surfaces | Prospective cohort study | 192 | 4844 | Clinical | Restorative |
| 9 | Longitudinal study of repaired or replaced dental restorations | Prospective cohort study | 157 | 6092 | Clinical | Restorative |
| 10 | Development of a patient-based provider intervention for early caries management 1 | Cross-sectional; clinical data collection and Qx | 10 | 336 | Qx and Clinical | Diagnostic; Restorative |
| 11 | Patient satisfaction with dental restorations | Cross-sectional | 159 | 4680 | Clinical | Restorative |
| 12 | Prevalence of questionable occlusal caries lesions | Cross-sectional | 58 | 4478 | Clinical | Diagnostic; Restorative |
| 13 | Longitudinal study of questionable occlusal caries lesions | Prospective cohort study | 58 | 4478 | Clinical | Diagnostic; Restorative |
| 14 | Hygienists’ internet tobacco cessation RCT | Randomized clinical trial | 100 | 1814 | Clinical | Preventive |
| 15 | Blood glucose testing in dental practice | Cross-sectional | 23 | 387 | Clinical | Diagnostic |
| 16 | Assessing the impact of participation in PBRNs on patient care | Cross-sectional (paper Qx with dentists and dental hygienists) | 613 | -- | Qx | Adjunctive |
| 17 | Assessing the impact of participation in PBRNs on patient care - repeated 2 years | Cross-sectional (paper Qx with dentists and dental hygienists) | 556 | -- | Qx | Adjunctive |
| 18 | Peri-operative pain and root canal therapy | Prospective cohort study | 55 | 655 | Clinical | Endodontics |
| 19 | Persistent pain and root canal therapy | Prospective cohort study | 55 | 655 | Clinical | Endodontics |
| 20 | Diagnoses for persistent dentoalveolar pain following root canal therapy 1 | Nested case series study | 63 | 354 | Clinical | Endodontics |
| 21 | Primary care management of TMD | Cross-sectional (electronic Qx with dentists) | 434 | -- | Qx | Diagnostic; Oral/Max Surgery; Prosthodontics |
| 22 | Infrastructure update survey | Cross-sectional (electronic Qx with dentists) | 649 | -- | Qx | Adjunctive |
| 23 | Isolation techniques used when performing root canal treatment | Cross-sectional (electronic and paper Qx with dentists) | 1491 | -- | Qx | Endodontics |
| 24 | Management of suspicious occlusal caries lesions | Randomized clinical trial | 125 | 3093 | Qx and Clinical | Diagnostic; Restorative |
| 25 | Management of dentin hypersensitivity (two parts) | #1: Cross-sectional (electronic Qx with dentists) | #1, #2: 200 | #2: 1876 | Qx and Clinical | Restorative |
| #2: Prospective cohort study | ||||||
| 26 | Reducing prescription opioid misuse | Cross-sectional (electronic Qx with dentists) | 822 | -- | Qx | Adjunctive |
| 27 | Understanding dental information networks | Cross-sectional (electronic Qx with dentists) | 1860 | -- | Qx | Adjunctive |
| 28 | Quit Advisor DDS smoking cessation study 1 | Feasibility non-randomized controlled clinical trial | 30 | 248 | Clinical | Preventive |
| 29 | Factors for Successful Crowns Questionnaire | Cross-sectional (electronic Qx with dentists) | 1852 | -- | Qx | Prosthodontics |
| 30 | Factors for Successful Crowns Clinical Study | Prospective cohort study | 207 | 3847 | Clinical | Prosthodontics |
| 31 | Leveraging EDR data for clinical research | Retrospective cohort study (EDR extraction of patients who received root canal treatment and select restorations) | 99 | 217,887 | Clinical | Endodontics; Restorative |
| 32 | Common practices of head & neck examinations in U.S. dental offices | Cross-sectional (electronic and paper Qx with dentists) | 1126 | -- | Qx | Diagnostic |
| 33 | Cracked tooth registry study | Prospective cohort study | 236 | 3017 | Clinical | Diagnostic; Restorative |
| 34 | Risk for oral cancer/HPV study | Prospective cohort study | 37 | 1025 | Clinical | Diagnostic |
| 35 | Anterior open-bite treatment | Prospective cohort study | 96 | 358 | Clinical | Orthodontics |
| 36 | Predicting root canal treatment outcomes | Prospective cohort study | 172 | 1883 | Clinical | Endodontics |
| 37 | TMD treatment methods | Prospective cohort study | 185 | 1901 | Clinical | Diagnostic; Oral/Max Surgery; Prosthodontics |
| 38 | Multi-risk assessment in the dental office (two parts) 1 | #1: Cross-sectional (paper Qx with dentists); #2: Cross-sectional clinical study |
#1: 475 #2: 30 |
#2: 857 | #1: Qx; #2: Clinical |
Diagnostic |
| 39 | Prophylactic use of antibiotics in dental office | Cross-sectional (electronic and paper Qx with dentists) | 2169 | -- | Qx | Adjunctive |
| Conducted from 2020 to present | ||||||
| 40 | Assessment of PPE for dental healthcare professionals 1 | Prospective cohort study | 70 | -- | Clinical | Adjunctive |
| 41 | COVID-19 Research Registry | Cross-sectional (electronic Qx with dentists) | 1819 | -- | Qx | Adjunctive |
| 42 | Evaluation of aerosol-generating procedures in dental settings 1 | Clinical simulation | -- | -- | Clinical simulation | Adjunctive |
| 43 | Evaluation of aerosol composition in dental settings 1 | Clinical simulation | -- | -- | Clinical simulation | Adjunctive |
| 44 | Particle topography and aerosol size distribution in dental settings in the COVID-10 era 1 | Clinical simulation | -- | -- | Clinical simulation | Adjunctive |
| 45 | Selective versus nonselective caries removal in permanent teeth | Cross-sectional (electronic Qx with dentists) | 478 | -- | Qx | Restorative |
| 46 | Treatment of patients on conventional and direct oral anticoagulants | Cross-sectional (electronic Qx with dentists) | 866 | -- | Qx | Adjunctive |
| 47 | Coronavirus vaccine acceptability and readiness among dentists | Cross-sectional (electronic Qx with dentists) | 550 | -- | Qx | Adjunctive |
| 48 | Pragmatic return to effective dental infection control through triage and testing 1 | Prospective cohort study | 30 | 43 | Clinical | Adjunctive |
| 49 | Dental management of patient with special health care needs | Cross-sectional (electronic Qx with dentists) | 505 | -- | Qx | Adjunctive |
| 50 | An innovative mDentistry eHygiene study amid the COVID-19 pandemic 1 | Prospective cohort feasibility study | 18 | 62 | Clinical | Adjunctive |
| 51 | Acute pain pathways 4 | Prospective cohort study | In progress; 25 planned |
In progress; 150 planned |
Clinical | Adjunctive |
| 52 | Understanding pain after dental procedures | Prospective cohort study | In progress; 150 planned |
In progress; 3000 planned |
Clinical | Endodontics; Periodontics; Oral/Max Surgery |
| 53 | Dental implant registry | Prospective cohort study | 200 (planned) |
1000 (planned) | Clinical | Periodontics; Prosthodontics; Oral/Max Surgery |
| 54 | Diagnosis of dental hard tissue conditions 3 | Cross-sectional (electronic Qx with dentists and patients) | 660 (planned) |
1350 (planned) | Qx | Diagnostic |
| 55 | Effectiveness of nicotine replacement sampling in dental practices 2 | Randomized clinical trial | 50 (planned) |
1200 (planned) |
Clinical | Preventive |
| 56 | Mental health screening and referral in dental practices 1 | Cross-sectional | 60 (planned) |
150 (planned) |
Clinical | Diagnostic |
| 57 | Risk factors associated with the prevalence of peri-implantitis disease | Cross-sectional | 100 (planned) |
1000 (planned) |
Clinical | Periodontics; Prosthodontics; Oral/Max Surgery |
| 58 | Indications for periodontal adjunctive antibiotics in dental practice | Randomized clinical trial | 35 (planned) |
1050 (planned) |
Clinical | Periodontics; |
One network region only
Two network regions only
Three network regions only
One network region only; the study is a collaboration with five other sites at academic health center (i.e., non-PBRN) clinics in the USA, funded by U01-FD-005938. The planned enrollment of 1500 patients across the entire collaboration is at 1235 as of June 9, 2022.
Abbreviations: EDR: electronic dental record; HPV: human papillomavirus; ONJ: osteonecrosis of the jaw; Qx: questionnaire; PPE: personal protective equipment; RCT: randomized clinical trial; TMD: temporomandibular disorders
Detailed study information can be accessed at http://nationaldentalpbrn.org/studies.php
An early version of this table was published in 2018 [17].
Of the studies that have completed enrollment (studies 1–50), 19,827 practitioners have been enrolled (some participated in multiple studies), along with 70,665 patient participants (excluding data-only studies). Two data-only studies (studies 7 and 31) examined electronic health records for 790,493 patients.
The 58 studies listed in Table 1 comprise 22 questionnaire studies, 38 clinical studies, and 3 clinical simulation studies. Study designs have included 28 cross-sectional designs, 1 case-control design, 1 nested case series design, 18 prospective cohort studies, 3 retrospective cohort studies, 1 non-randomized feasibility controlled clinical trial, 5 randomized controlled clinical trials, and 3 clinical simulations.
Clinical topics were categorized as investigating 14 Diagnostic topics, 4 Preventive topics, 14 Restorative topics, 8 Endodontics topics, 4 Periodontics topics, 6 Prosthodontics topics, 7 Oral and Maxillofacial Surgery topics, 1 Orthodontics topic, and 17 Adjunctive General Services topics.
Publication Productivity
The Network has produced 193 peer-reviewed publications to date [20]. A total of 167 had publication dates of 2020 or earlier. Peer-reviewed publications have appeared in a total of 62 different journal titles so far, which comprise a broad range of scientific disciplines.
Fig. 3 shows results from the iCite analysis of the 167 publications that had publication dates of 2020 or earlier, displaying number per year, weighted RCR by year, and total citations by year cited. Not shown in the figure are these metrics: 11.13 publications per year; 2927 total citations; a mean (SE) of 17.53 (1.79) and a median of 11.0 citations per publication; mean (SE) of 2.09 (0.17) citations per publication per year. The mean (SE) RCR was 1.40 (0.11), the median was 1.07, and the weighted RCR was 233.84.
Fig. 3.
Graphic presentation of iCite results from Network publications that were published 2006–2020 (n = 167), as of March 29, 2022. The graphs were produced by the iCite system [12]. RCR: Relative Citation Ratio.
We compared the percentile ranking of the 167 publications to the corpus of PubMed publications based on RCRs; nine of the 167 publications were ranked above the 90th percentile and 15 articles were ranked between the 80th and 90th percentiles. An article-specific report is publicly available [25].
The weighted RCR (234 in the case of this analysis) was considerably higher than the number of total publications (167 in the case of this analysis), which indicated that this set of publications was highly influential relative to the average paper in the PubMed database.
Discussion
Having described the Network’s organizational changes in 2019 in the context of a Network history that began in 2005, we have documented that a PBRN can productively engage community practitioners, patients, and clinical research investigators over a sustained multi-year period. This adds to the evidence and conclusions made in a recent review of PBRNs [8]. Our report focuses on one particular network to document its productivity as measured by recruiting and engaging practitioners in research, completing many studies, and disseminating research findings through peer-reviewed publications. These results suggest that everyday practitioners can be crucial partners in developing, implementing, and disseminating scientific research, and that community practices can be an effective venue for clinical research. Network studies have generated numerous, timely, and influential publications, in a broad range of clinical topic areas.
That the median RCR of Network publications exceeded 1.0 and the weighted RCR substantially exceeded the total number of publications upon which the analysis was based, demonstrate that the network’s publications have had a greater-than-average influence in their fields [11]. Because of its mission, the Network attempts to balance its interest in communicating with and disseminating to a clinical audience, with its desire to maintain a strong scientific credibility. Consequently, the Network decides on many occasions to target a particular peer-reviewed scientific journal because it has a heavily clinical readership, even though the journal’s impact factor is not as high as other target journals that we believe would accept the manuscript. Consequently, our a priori goal before conducting the iCite analysis was much lower (25th percentile) than the actual percentile obtained (higher than the 50th percentile). As one of several methods to quantify publication quality or its impact on the field, the RCR has performed better than journal impact factor, citations per year, or the Thompson–Reuters ratio [11,26,27]. Establishing consensus about methods to quantify success and productivity of large research groups may be important to justify continued funding or establishing new networks [28,29]. Self-citation and publication frequency among network coauthors has the potential to inflate RCRs, but the effect is minimized by the wide range of study topics that limit the extent of self-citation (numerator), while articles overly benefitting from self-citation would increase the field citation rate (denominator). A limitation to PBRN research is that a high RCR demonstrates prominence among scientific peers, yet does not capture the Network’s influence on everyday clinical practice and patient health, which is the ultimate goal of the Network. Impact on everyday practice can be the key research question for some studies [30-32], although the typical goal is to contribute to the evidence base in a manner similar to individual “R01” studies or clinical trials. PBRNs offer recruitment sites (community practices) that complement or supplement academic health center sites with geographic and patient demographic diversity, while also providing an infrastructure to engage simultaneously both academic clinical scientists and the “end-users” (community practitioners) of results from the studies, at each step of the study development and implementation process [9,32].
The National Dental PBRN has operated at a high level of scientific productivity and has demonstrated the feasibility and effectiveness of PBRNs as a research context. The network seeks to foster a future in which research and quality improvement are done routinely in everyday clinical practice – just because that is what health care providers do as a profession. The ultimate goal is to advance the delivery of evidence-based care into daily clinical practice for the benefit of patients.
Acknowledgments
Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. An Internet site devoted to details about the network is located at http://NationalDentalPBRN.org.
This work was supported by NIH grants U19-DE-28717 (GHG), U01-DE-28727 (MAM), U19-DE-22516 (GHG), U01-DE-16747 (GHG), and UL1-TR-003096 (Robert Kimberly).
We gratefully acknowledge the current practitioner members of the network’s Practitioner Executive Committee members, all of whom are in private practice: Julie Ann Barna, DDS, Lewisburg, PA; Theresa E. Madden, DDS, MS, PhD, Olympia, WA; Tara R. Rios, DDS, Brownsville, TX; Peggy Richardson, DDS, MS, Tinley Park, IL; Diedra J. Snell, DDS, Port Gibson, MS; Joseph C. Spoto, III, DMD, Apollo Beach, FL. We also acknowledge excellent suggestions for an earlier version of this manuscript by Robert Kimberly, MD, Director of the University of Alabama at Birmingham Center for Clinical and Translational Research.
We also acknowledge the network’s Administrative and Resource Center, National Coordinating Center, and Regional Coordination staff: in Birmingham, AL: Muna Anabtawi, DDS, MS, CCRP, Ellen Funkhouser, DrPH, Yolanda “Terri” Jones, Shermetria Massengale, MPH, CHES, and Ellen Sowell, BA; in Portland, OR: Kim Funkhouser, BS, Suzanne Gillespie, MA, MS, Chalinya Ingphakorn, BS, Reesa Laws, BS, Michael Leo, PhD, Celeste Machen, BS, Sweta Mathur, BSD, MPH, PhD, Sacha Reich, BS, PMP, Kim Stewart, MPH, Natalia Tommasi, MA, LPC, Lisa Waiwaiole, MS; in Gainesville, FL: James “Danny” Johnson, Brenda E. Thacker, RDH, CCRP; in Minneapolis, MN: Sarah Basile, RDH, MPH, Chris Enstad, BS, Kimberly Johnson, RDH, MPH, Heather Weidner, RDH; in Rochester, NY: Kathy Bohn, AAS, Rita Cacciato, RDH, MS, Pat Regusa, BFA, Kathy Scott-Anne, BS, BA; in San Antonio, TX: Marissa Mexquitic, MS.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/cts.2022.421.
click here to view supplementary material
Disclosures
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article. Authors’ institutions receive funding from NIH to support network activities.
Statement of Institutional Review Board Approval
The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully. All Network studies and operations receive approval from the National Dental PBRN Central IRB or regional IRBs, depending on the activity.
References
- 1. Davis MM, Gunn R, Kenzie E, et al. Integration of improvement and implementation science in practice-based research networks: a longitudinal, comparative case study. Journal of General Internal Medicine 2021; 36(6): 1503–1513. DOI 10.1007/s11606-021-06610-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Westfall JM, Roper R, Gaglioti A, Nease DE Jr . Practice-based research networks: strategic opportunities to advance implementation research for health equity. Ethnicity and Disease 2019; 29: 113–118. DOI 10.18865/ed.29.S1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hall-Lipsy E, Barraza L, Robertson C. Practice-based research networks and the mandate for real-world evidence. American Journal of Law and Medicine 2018; 44(2-3): 219–236. DOI 10.1177/0098858818789428. [DOI] [PubMed] [Google Scholar]
- 4. Riley-Behringer M, Davis MM, Werner JJ, Fagnan LJ, Stange KC. The evolving collaborative relationship between practice-based research networks (PBRNs) and clinical and translational science awardees (CTSAs). Journal of Clinical and Translational Science 2017; 1(5): 301–309. DOI 10.1017/cts.2017.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hickner J, Green LA. Practice-based research networks (PBRNs) in the United States: growing and still going after all these years. Journal of the American Board of Family Medicine 2015; 28(5): 541–545. DOI 10.3122/jabfm.2015.05.150227. [DOI] [PubMed] [Google Scholar]
- 6. Peterson KA, Lipman PD, Lange CJ, Cohen RA, Durako S. Supporting better science in primary care: a description of practice-based research networks (PBRNs) in 2011. Journal of the American Board of Family Medicine 2012; 25(5): 565–571. DOI 10.3122/jabfm.2012.05.120100. [DOI] [PubMed] [Google Scholar]
- 7. PBRN Registry. Agency for healthcare research and quality [Internet] [cited June 10, 2022]. (https://pbrn.ahrq.gov/pbrn-registry)
- 8. Canceill T, Monsarrat P, Faure-Clement E, Tohme M, Vergnes JN, Grosgogeat B. Dental practice-based research networks (D-PBRN) worldwide: a scoping review. Journal of Dentistry 2021; 104(184): 103523. DOI 10.1016/j.jdent.2020.103523. [DOI] [PubMed] [Google Scholar]
- 9. Gilbert GH, Williams OD, Korelitz JJ, et al. Purpose, structure, and function of the United States national dental practice-based research network. Journal of Dentistry 2013; 41(11): 1051–1059. DOI 10.1016/j.jdent.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hirsch JE. An index to quantify an individual’s scientific research output. Proceedings of the National Academy of Science USA 2005; 102(46): 16569–16572. DOI 10.1073/pnas.0507655102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hutchins BI, Yuan X, Anderson JM, Santangelo GM. Relative citation ratio (RCR): a new metric that uses citation rates to measure influence at the article level. PLoS Biology 2016; 14(9): e1002541. DOI 10.1371/journal.pbio.1002541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. iCite New Analysis Page. National Institutes of Health Office of Policy Analysis [Internet] [cited June 10, 2022]. (https://icite.od.nih.gov/analysis)
- 13. NIH Public Access Policy, National Institutes of Health, [Internet] [cited June 10, 2022]. (https://publicaccess.nih.gov/) [Google Scholar]
- 14. Werner JJ. Measuring the impact of practice-based research networks (PBRNs). Journal of the American Board of Family Medicine 2012; 25(5): 557–559. DOI 10.3122/jabfm.2012.05.120176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Green LA, Hickner J. A short history of primary care practice-based research networks: from concept to essential research laboratories. Journal of the American Board of Family Medicine 2006; 19(1): 1–10. DOI 10.3122/jabfm.19.1.1. [DOI] [PubMed] [Google Scholar]
- 16. Mungia R, Funkhouser E, Makhija SK, et al. Practitioner engagement in activities of the national dental practice-based research network (PBRN): 7-year results. Journal of the American Board of Family Medicine 2020; 33(5): 687–697. DOI 10.3122/jabfm.2020.05.190339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mungia R, Funkhouser E, Buchberg Trejo MK, et al. Practitioner participation in national dental practice-based research network (PBRN) studies: 12-year results. Journal of the American Board of Family Medicine 2018; 31(6): 844–856. DOI 10.3122/jabfm.2018.06.180019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. National Dental Practice-Based Research Network: Administrative and Resource Center. RFA-DE-19-001 [Internet], National Institutes of Health, National Institute of Dental and Craniofacial Research [cited June 10, 2022]. (https://grants.nih.gov/grants/guide/rfa-files/RFA-DE-19-001.html)
- 19. National Dental Practice-Based Research Network: Coordinating Center. RFA-DE-19-002 [Internet], National Institutes of Health, National Institute of Dental and Craniofacial Research [cited June 10, 2022]. (https://grants.nih.gov/grants/guide/rfa-files/RFA-DE-19-002.html)
- 20. National Dental Practice-Based Research Network Publications Page. [Internet] [cited June 10, 2022]. (https://www.nationaldentalpbrn.org/publications/). The current policy document is directly available at https://www.nationaldentalpbrn.org/wp-content/uploads/2020/06/National.Dental.PBRN_.PP_.policy.2020-05-16.pdf
- 21. National Dental Practice-Based Research Network Infrastructure Access. PAR-20-073 [Internet], National Institutes of Health, National Institute of Dental and Craniofacial Research [cited June 10, 2022]. (https://grants.nih.gov/grants/guide/pa-files/PAR-20-073.html)
- 22. National Dental Practice-Based Research Network Clinical Trial or Observational Study Planning and Implementation Cooperative Agreement. PAR-20-306 [Internet], National Institutes of Health, National Institute of Dental and Craniofacial Research [cited June 10, 2022]. (https://grants.nih.gov/grants/guide/pa-files/PAR-20-306.html)
- 23. The CDT 2022 Current Dental Terminology code [Internet], American Dental Association [cited June 10, 2022]. (https://www.ada.org/publications/cdt)
- 24. Yansane A, Tokede O, White J, et al. Utilization and validity of the dental diagnostic system over time in academic and private practice. JDR Clinical and Translational Research 2019; 4(2): 143–150. DOI 10.1177/2380084418815150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Dental Practice-Based Research Network Peer-Reviewed Publications page. [Internet] [cited June 10, 2022]. (https://www.nationaldentalpbrn.org/Peer-Reviewed-Publications/#1589322198976-c295e5c0-8c1c). The article-specific report is directly available at https://www.nationaldentalpbrn.org/wp-content/uploads/2022/01/iCite.Influence.report2022-01-21.pdf
- 26. Hutchins BI, Hoppe TA, Meseroll RA, Anderson JM, Santangelo GM. Additional support for RCR: a validated article-level measure of scientific influence. PLoS Biology 2017; 15(10): e2003552. DOI 10.1371/journal.pbio.2003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Janssens ACJW, Goodman M, Powell KR, Gwinn M. A critical evaluation of the algorithm behind the Relative Citation Ratio (RCR). PLoS Biology 2017;15(10): e2002536. DOI 10.1371/journal.pbio.2002536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yu F, Van AA, Patel T, et al. Bibliometrics approach to evaluating the research impact of CTSAs: a pilot study. Journal of Clinical and Translation Science 2020; 4(4): 336–344. DOI 10.1017/cts.2020.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bragg KM, Marchand GC, Hiplert JC, Cumming JL. Using bibliometrics to evaluate outcomes and influence of translational biomedical research centers. Journal of Clinical and Translational Science 2022; 6(1): E72. DOI 10.1017/cts.2021.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kakudate N, Yokoyama Y, Sumida F, et al. Web-based intervention to improve the evidence-practice gap in minimal intervention dentistry: findings from a dental practice-based research network. Journal of Dentistry 2021; 115: 103854. DOI 10.1016/j.jdent.2021.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rindal DB, Flottemesch TJ, Durand EU, et al. Practice change toward better adherence to evidence-based treatment of early dental decay in the National Dental PBRN. Implementation Science 2014; 9(1): 177. DOI 10.1186/s13012-014-0177-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gilbert GH, Gordan VV, Funkhouser EM, et al. Caries treatment in a dental practice-based research network: movement toward stated evidence-based treatment. Community Dentistry and Oral Epidemiology 2013; 41(2): 143–153. DOI 10.1111/cdoe.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gilbert GH, Richman JS, Gordan VV, et al. Lessons learned during the conduct of clinical studies in the dental PBRN. Journal of Dental Education 2011; 75(4): 453–465. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/cts.2022.421.
click here to view supplementary material