Abstract
Objectives:
While evidence highlights the detrimental mental health consequences of chronic stress exposure, the impact of this stress exposure on older Black Americans’ mental health varies by exposure to other types of stressors like discrimination as well as subjective evaluations of stress like chronic stress appraisal.
Methods:
Using data from the 2010/2012 Health and Retirement Study, we use latent profile analysis (LPA) to describe 2,415 Black older adults experience with chronic stress exposure, appraisal, and discrimination and examine which stress contexts are associated with depressive symptomology.
Results:
Analyses revealed five stress clusters—demonstrating the diversity in the stress experience for older Black adults. Black older adults with stress profiles that include lower stress appraisal report fewer depressive symptoms regardless of number of stress exposures.
Discussion:
LPA is as an alternative approach to examining the stress-mental health link that can define stress profiles by both exposure and appraisal-based measures.
Keywords: chronic stress, stress appraisal, mental health, racism
Introduction
“Stress is really a latent construct,” the late Dr. James S. Jackson (1944–2020) said casually in one of his many mentoring sessions for the Michigan Integrative Well-Being and Inequality (MIWI) Training Program in late July of 2020. Simply counting up stress exposures that were designed to capture general stress among white populations, in the way national surveys propose, overlooks both race-based stress as well as the subjective dimensions of the stress process and, thus, may not provide a complete picture of how stress impacts mental health or generates racial health disparities. This is especially true for older Black Americans who have and continue to face chronic strains in the context of overt discrimination and collective race related stressors—having come of age during Jim Crow, desegregation, the Civil Rights Movement, and now the Movement for Black Lives that is responding to the disproportionate killing of Black people by the police (Edwards et al., 2019). More mundane forms of discrimination and chronic strain that older Black people face like perpetual mistreatment in everyday life, being treated with less courtesy and respect by other people at restaurants, stores or while obtaining medical care are happening under the context of collective race-based stressors like the killing of George Floyd by the Minneapolis, Minnesota police department. While the operationalization of stress as a race-neutral, exposure-based measure has established stress as a principal mechanism behind racial differences in mental health (Kraaij et al., 2002; Pearlin et al., 2005; Williams, 2018), it overlooks race-based stressors like discrimination and an important, subjective element of stress—stress appraisal. Efforts to understand the Black aging experience may require a more significant and specific emphasis on the distinct features of the stress experience for Black older adults.
James S. Jackson is known for intellectualizing at least two big ideas in Black health and aging. First, he championed the idea that we could study Black people without using white people as the referent group. While much of his work did interrogate Black-white differences in health, he also insisted that within group differences among Black people were just as—if not more—important than between group differences. Dr. Jackson was among one of the first cohorts of Black scholars to study aging in Black Americans, paving the way for many scholars coming behind him who would have to justify why we only included Black older adults in our study or sample. Second, Jackson outlined a testable hypothesis for the mechanisms behind the Black-white mental health paradox. The paradox, at that time, was an understudied phenomenon suggesting that despite Black Americans having fewer economic resources and greater exposure to stress, discrimination, disease, and disability over the life course relative to whites, Black Americans report lower rates of common stress related forms of psychopathology such as major depression and anxiety disorders (Erving et al., 2018; Mezuk et al., 2013). Dr. Jackson’s Environmental Affordances Model (EAM) is a life course framework that aims to better understand the mental health paradox and the complex processes by which race, stress, and individual coping strategies or behaviors may interact to produce mental and physical health disparities among Black Americans.
This paper examines stress and mental health among older Black Americans from the Health and Retirement Study, amplifying the idea that whites need not always be the referent group nor the gold standard of health. We build on the idea that the stress experience varies for older Black adults by other features in the stress landscape, which may shed light on important pathways that contribute to mental health disparities. Prior stress and mental health research has struggled to explain Black-white differences in depression. Most of this work has over relied on measures of stress exposure to predict mental health outcomes, implying that stress exposure characterizes the stress experience. This paper, inspired by James S. Jackson’s trailblazing career, interrogates the unique and varied stress experience of older Black Americans—using measures of discrimination, chronic stress exposure, and stress appraisal—and their impact on depressive symptomology. The aim of this study was to identify subgroups (i.e., classes) of Black Americans whose stress experience predicts fewer depressive symptoms, identifying potential pathways that lead to Black-white differences in depression.
Ongoing Chronic Stress
Ongoing chronic stressors are persistent and enduring, often having no easy solution, requiring ongoing coping, and often surfacing within major social and role domains. The persistent and unrelenting nature of chronic stressors in older adulthood like ongoing housing insecurity, in comparison to short term acute stressors like getting a divorce or losing a job, often come with grave mental health consequences for older adults who may not have the resources to cope with these strains (Herbert & Cohen, 1993; Lepore, 1995; L. I.; Pearlin, 2010). Prior work has suggested Black older adults are at least two times as likely to report exposure to chronic strains like housing and financial insecurity and are also more likely to report having health problems, problems in a close relationship, and caregiving responsibilities than white older adults (Brown et al., 2018). Financial and housing strain are two major chronic stressors that are particularly pertinent for the mental health of Black older adults, many of whom live on fixed incomes that are often inadequate for providing economic and housing stability (Fenelon & Mawhorter, 2020). Centering chronic stressors in health disparities research exposes lifetime differences in adversity that Black people face. Adversity that extends well into older adulthood. Still chronic stressors are not the sole determinant of subsequent mental health outcomes among Black older adults.
Everyday Discrimination.
Capturing experiences of stress across multiple domains of exposure demonstrates the distinct yet ubiquitous stress experience for older Black adults (Kemeny, 2003; Slavich, 2019). General chronic stressors often co-occur with experiences of everyday discrimination for Black Americans—a pathway by which racism manifests as a fundamental cause of racial disparities in mental and physical health (Kessler et al., 1999; Paradies, 2006; Williams & Collins, 2001; Williams & Mohammed, 2008). Although racial discrimination exists at various levels, including structural, cultural, interpersonal, and/or internalized levels (Cogburn, 2019; Gee & Ford, 2011; Williams & Mohammed, 2008), everyday racial discrimination is generally recurring and interpersonal (Lewis et al., 2015). Well-established measures of everyday discrimination capture the occur-rence of chronic micro and macro aggressions, slights, and unfair treatment (Williams et al., 1997) and have been consistently linked to mental health outcomes—including psychological distress and depression (Assari et al., 2018; Hudson et al., 2016; Kessler et al., 1999; Michaels et al., 2019; Schulz et al., 2006; Williams et al., 1997). The diffusiveness of everyday discrimination on mental health is further demonstrated in studies that have found the association remains after accounting for socioeconomic status, with some studies finding that Black Americans tend to experience more discrimination at higher levels of socioeconomic status (Assari et al., 2018; Gaydosh et al., 2018; Kessler et al., 1999; Williams et al., 1997). The frequency and regularity of chronic stress and everyday discrimination position them as part of the larger social fabric of Black life, likely charting how life course trajectories and the mental health of Black people come to differ in older adulthood (L. I. Pearlin, 2010).
Stress Appraisal.
An additional methodical limitation in much of the empirical work examining stress and mental health is that most stress measures only focus on general lists of verifiable exposures and life situations such as the death of a spouse or living in poverty, and overlook the appraisal processes through which stressors operate to impact more distal outcomes(Lazarus & Folkman, 1984; Park & Folkman, 1997; L. I.; Pearlin, 1989; Thoits, 1995). Psychological stress models emphasize that experiencing the same event can be stressful for some individuals but not for others (Cohen et al., 1995, 2016), positioning the appraisal process as a primary mechanism through which stress exposure operates to impact more distal health outcomes (Kemeny, 2003; McEwen, 1998). Further evidence suggests older Black adults may respond to stressors differently than their white peers, suggesting the stress experience depends not just on an individual’s personal experiences, but also on collective social history, culture, and perhaps the community context in which the exposure occurs (Brown et al., 2018). It is not clear what the mechanisms are behind race/ethnic differences in stress appraisal, but it suggests that simply counting up stress exposures is not the best way to understand how stress impacts the mental health of Black older adults (Brown et al., 2020). Importantly, there is a lack of empirical research examining whether the variability in the subjective components of stress account for the variability in depressive symptoms among Black older adults.
Depressive Symptoms.
Depressive symptomology is an indicator of psychological burden that is frequently assessed in research and clinical settings (Regier, 1988; R. J.; Taylor & Chatters, 2020,R. J. Taylor & Chatters, 2020). Though symptoms alone do not indicate the presence of disorder (as defined by the Diagnostic and Statistical Manual of Mental Disorders) (American Psychiatric Association, 2013), self-reports of depressive symptoms are often used as a marker of psychological distress (Vega & Rumbaut, 1991). Older adults are at increased risk for developing depressive symptoms due to factors such as decreased mobility and independence and increased risk of social isolation (H. O. Taylor et al., 2018). For Black older adults in particular, these concerns may be compounded by disproportionate exposure to chronic stressors and racial discrimination (Neighbors et al., 1983). Both the persistent and cumulative nature of these experiences over the life course suggest increased concern for depressive symptoms among Black people as they age (Marshall & Rue, 2012). Black adults report experiencing more physical health concerns as well as a greater number of depressive symptoms on average than white adults (Barnes & Bates, 2017; George & Lynch, 2003; Vega & Rumbaut, 1991). Increased exposure to everyday discrimination is also associated with elevated levels of depressive symptoms among both African American and Caribbean Black adults over age 55 (Marshall & Rue, 2012; Mouzon et al., 2017).
Interestingly, while depressive symptoms and depressive disorder are highly correlated (Kroenke & Spitzer, 2002), Black people do not experience a greater prevalence of major depression relative to white people, despite having heightened depressive symptoms and exposure to stressors, discrimination, and socioeconomic deprivation (Barnes & Bates, 2017; George & Lynch, 2003; Williams et al., 2007). It may seem counterintuitive, but the chronicity of stress exposures and everyday discrimination for Black adults across the life course may result in a muted stress response, with Black older adults actually perceiving stressors as less distressing relative to their white peers, limiting their potential to manifest as depressive symptomology (Brown et al., 2020, 2018; Neighbors et al., 1983; L.; Pearlin et al., 1981). The discordance between racial patterns in symptomology, distress, and disorder raises questions as to the appropriate measures of both stress and mental health. Are we accurately capturing the stress experience among Black older adults? Is stress exposure the best or only way to represent or quantify the stress experience? Are there other elements of the stress experience besides general exposure-based measures that are predictive of depressive symptomology? The current study aims to characterize the variability in the stress experience for Black older adults by utilizing latent profile analysis (LPA) to derive risk profiles that describe how everyday discrimination, chronic stress exposure and appraisal are associated with depressive symptomology among Black older adults. This may help us understand the stress profiles that confer a lower or higher risk for endorsing depressive symptoms for Black adults in community based, nationally representative samples.
Methods
Data
The data used in this study were from the 2010 and 2012 waves of the Health and Retirement Study (HRS), a population-based longitudinal survey of U.S. adults aged 51 and older. Sponsored by the National Institute on Aging and conducted by the Institute for Social Research at the University of Michigan, the HRS is designed to improve our understanding of the social, economic, environmental, and behavioral factors associated with aging and the health of older adults. In 2010, a random one-half of the HRS sample (subsample A) was selected to participate in an enhanced face-to-face (EFTF) interview, which included the collection of physical measures and biomarkers. The other one-half of respondents received an EFTF interview in 2012 (subsample B). Respondents that were eligible for the EFTF were also eligible for the Psychosocial and Lifestyle self-administered questionnaire (SAQ), which included questions on well-being, lifestyle, social relationships, personality, work, self-related beliefs, stress exposure, and appraisal. The SAQ had a 73.1% response rate in 2010 and a 72.7% response rate in 2012. The low response rates for the SAQ are attributed to the new cohort of respondents that were added in 2010, who were asked to complete the SAQ at the end of a very long baseline interview (over 3 hours, on average) (Smith et al., 2013).
Study Sample
We restricted our sample to self-identified Black respondents that completed the SAQ in either 2010 (n = 1,279) or 2012 (n = 1,188). Information for each respondent was based on when they were eligible to have their first SAQ interview. Missing data were minimal with 2.1% of cases incomplete (n = 52). An analysis of missing data showed that increasing age, male sex, and having less than a high school education increased the likelihood of having missing information. Since respondents missing data constitute a very small proportion of the sample, we only include those with complete data (Bennett, 2001; Schafer & Graham, 2002). The final analytical sample includes 2,415 Black older adults.
Measures
Ongoing Chronic Stress.
Ongoing chronic stress was measured in the HRS by asking respondents to report whether they experienced exposure during the last 12 months or longer to ongoing health problems (in yourself), physical or emotional problems (in spouse or child), problems with alcohol or drug use in family member, difficulties at work, financial strain, housing problems, problems in a close relationship, and helping at least one sick/limited/frail family member or friend on a regular basis. An item assessing ongoing problems in the workplace was excluded from our analysis since more than half of respondents were retired or out of the labor force. For each of the ongoing chronic stressors respondents could choose: 0 = no, it didn’t happen, 1 = yes, it did happen and it was not upsetting, 2 = yes, it did happen and it was somewhat upsetting, or 3 = yes, it did happen and was very upsetting (Troxel et al., 2003).
From this item, we created two measures. First, we created a measure of cumulative chronic stress exposure using the sum of the number of chronic stressors respondents reported experiencing (range = 0–7) during the last 12 months or longer based on respondents’ self-reports (yes/no; Cronbach’s α = .63).
Ongoing Chronic Stress Appraisal.
Next, we created a stress appraisal scale by averaging across responses of how upsetting each of these stressors was among respondents who experienced at least one stressor (range: 0–3; Cronbach’s α = .78). Respondents who reported exposure to a chronic stressor could rate that stressor as 1 = not upsetting, 2 = somewhat upsetting, or 3 = very upsetting. If someone did not experience any stressors, they received a value of zero on the stress appraisal scale.
Perceived Everyday Discrimination.
Respondents were asked about the experience of hassles and chronic stress associated with perceived everyday discrimination that included: being treated with less courtesy and respect by other people, receiving poorer service than others at restaurants or stores, people acting as if they are not smart, people acting as if they are afraid of them, getting threatened or harassed, and receiving poorer service or treatment from doctors or hospitals (Williams et al., 1997). Response categories ranged from 1 = almost every day to 6 = never. We created an index of discrimination by reverse-coding all items and averaging the scores across all six items (Cronbach’s α = .82). Respondents were coded as missing on the scale if there were more than three items with missing values.
CESD symptoms.
The CESD score is the sum of eight negative and positive items based on the Center for Epidemiologic Studies Depression (CESD) scale (Andresen et al., 1994). The negative items were based on whether the respondent experienced the following sentiments (yes/no): depression, everything is an effort, sleep is restless, felt alone, felt sad, and could not get going. The positive indicators were based on whether the respondent felt happy (yes/no) and enjoyed life (yes/no). The items worded in the positive direction were reverse-coded. The Cronbach’s alpha for the CESD in this study was 0.80, indicating good internal consistency.
Sociodemographic Variables.
Our models include sociodemographic variables since this better isolates the relationship between stress exposure, discrimination and appraisal on depressive symptoms. Age is measured as a continuous variable in years (range: 51–101). Sex was dichotomized as male or female. Marital status was categorized as married/partnered, divorced/separated, widowed, and never married. Measures of SES are confounders and thus are included in our models to fully distinguish the impact of chronic stress exposure, appraisal and discrimination on mental health from the impact of SES differences on mental health. Educational attainment was categorized as less than high school, high school or GED, some college, and college and above. Household income was quartiled because it is highly skewed to the right and included the following income cutoffs: $0–$12,000, $12,001–$24,727, $24,728–$52,040, and $52,041–$830,000. Household wealth (assets minus debts) was also quartiled because it is highly skewed to the right and included the following cutoffs: $−444,996 to $0, $1–$24,000, $24, 001–$108,000, and $108,001–$3,345,000.
Analytic Strategy
First, we examined each of the multidimensional stress indicators before conducting the latent profile analysis (LPA) to demonstrate how the mean values for each measure may mask variability in the stress experience for Black older adults. Second, we conducted a LPA for identifying clusters of Black older adults’ experiences with chronic stress exposure, appraisal, and discrimination. We evaluated models with up to six classes and defined the optimal number of classes based on statistical and substantive grounds. For statistical model selection, we used the Akaike information criterion (AIC) and Bayesian information criterion (BIC) for model comparisons, with lower AIC and BIC values indicating better model fit (Magidson et al., 2020). Moreover, we considered the relative improvement in model fit using the Lo–Mendell–Rubin likelihood ratio test (LRT), which compares the k-class model and the (k+1)-class model (Lo, 2001; Vuong, 1989). As a criterion for classification quality, we used entropy to assess class separation, with values greater than or equal to 0.80 indicating good class separation (Celeux & Soromenho, 1996). Then, we evaluated the competing models in terms of interpretability and sample sizes. Third, we examined sociodemographic characteristics of the sample across stress profiles that emerged from the LPA. We compared sociodemographic differences between the stress profiles using Wald-adjusted χ2 comparisons. Lastly, we used negative binomial regression to assess the relationship between the stress profiles that emerged and CESD symptoms. In Model 1, we controlled for age and sex. In Model 2, we additionally controlled for marital status, educational attainment, household income, and household wealth. All models controlled for year of interview to account for differences for when respondents were selected for the SAQ.
All statistical analyses were performed using Stata version 16.1, except for the Lo–Mendell–Rubin LRT, which was performed using R 4.0.4 with the tidyLPA package (Rosenberg et al., 2018). All analyses also account for the complex survey design of the HRS by using Stata’s svy commands and respondent-level weights provided by the HRS, which adjusts for differential sampling probabilities, nonresponse, and population stratification.
Results
Multidimensional Stress Indicators
Table 1 presents univariate statistics for the individual indicators that make up each stress measure (i.e., ongoing chronic stress, discrimination, and stress appraisal). On average, respondents reported experiencing approximately 3 ongoing chronic stressors, with most reporting ongoing health problems (72.3%) and financial strain (63.8%). In addition, at least one-third of respondents reported ongoing physical or emotional problems (41.8%), regularly helping an ailing family member or friend (38.5%), housing problems (33.2%), and problems in a close relationship (30.4%). Discrimination was not a commonly reported experience, with respondents reporting an average of less than one experience of discrimination (= 0.8). However, at least one-third of respondents reported being treated with less courtesy or respect (38.4%) and people acting as if they were not smart (32.3%). Similarly, stress appraisal was low on average (= 0.7), with most respondents reporting their stress as not upsetting (68.4%).
Table 1.
Multidimensional stress indicators reported among HRS Black respondents, 2010–2012 (n = 2,415).
| % or mean | SD | |
|---|---|---|
| Stress exposure (0–7) | 2.9 | 1.9 |
| Ongoing health problems (in yourself) | 72.3 | |
| Ongoing physical or emotional problems (in spouse or child) | 41.8 | |
| Ongoing problems with alcohol or drug use (in family member) | 19.4 | |
| Ongoing financial strain | 63.8 | |
| Ongoing housing problems | 33.2 | |
| Ongoing problems in a close relationship | 30.4 | |
| Regularly help ailing family member or friend | 38.5 | |
| Discrimination (0–6) | 0.8 | 0.9 |
| Treated with less courtesy or respect | 38.4 | |
| Receive poorer service than others at restaurant or stores | 23.0 | |
| People act as if you are not smart | 32.3 | |
| People act as if afraid of you | 17.7 | |
| You are threatened or harassed | 8.9 | |
| Receive poorer service or treatment from doctors or hospitals | 9.9 | |
| Stress appraisal (0–3) | 0.7 | 0.6 |
| Did not experience any stressors | 9.4 | |
| Not upsetting | 68.4 | |
| Somewhat upsetting | 19.8 | |
| Very upsetting | 2.4 |
Note. Percentages and means are weighted.
Stress Clusters
Model fit criteria for the six class solutions tested for the optimal latent model are summarized in Table 2. The 5-class solution had lower AIC and BIC values relative to the other models. Moreover, the Lo–Mendell–Rubin LRT suggests that the 5-class solution is sufficient and that the 6-class solution is not needed. Finally, the entropy measure indicates good classification quality for all models, except the 6-class solution. Thus, we found that the 5-class model is an adequate representation of the data and permits good differentiation of the stress cluster profiles.
Table 2.
Model selection criteria of the six models from the latent profile analysis (n = 2,415).
| Model fit indices | Log likelihood | Degrees of freedom | AIC | BIC | Lo-Mendell-Rubin LRT | Entropy |
|---|---|---|---|---|---|---|
| # Of classes | ||||||
| 1 | −9959.635 | 6 | 19,931.3 | 19,966.3 | 1.00 | |
| 2 | −9537.118 | 10 | 19,094.2 | 19,152.6 | <.001 | 0.96 |
| 3 | −9459.032 | 14 | 18,946.1 | 19,027.8 | <.001 | 0.85 |
| 4 | −9289.421 | 18 | 18,614.8 | 18,719.9 | <.001 | 0.84 |
| 5 | −9259.728 | 22 | 18,563.5 | 18,691.9 | <.001 | 0.80 |
| 6 | −9259.728 | 26 | 18,571.5 | 18,723.2 | NS | 0.74 |
Note. AIC = Akaike information criterion, BIC = Bayesian information criterion, LRT = likelihood ratio test, Indices for optimal model are bolded
Parameter estimates for the 5-class solution are shown in Figure 1. We labeled the first cluster moderate stress, low discrimination, low appraisal (Class 1), representing 35.0% of Black respondents. This stress cluster had respondents who reported some ongoing chronic stressors (= 2.48), reported very low instances of experiencing discrimination (= 0.62), and appraised their stress as not upsetting (= 0.47). The second cluster was labeled high stress, moderate discrimination, moderate appraisal (Class 2), and represented 12.8% of Black respondents. This stress cluster was characterized by respondents who reported a high number of ongoing chronic stressors (= 5.28), reported few instances of experiencing discrimination (= 1.34), and appraised their stress as somewhat upsetting (= 1.35) relative to the other classes. We labeled the third stress cluster high stress, moderate discrimination, high appraisal (Class 3), representing 5.3% of Black respondents. This stress cluster was characterized by respondents who reported a higher number of ongoing chronic stressors (= 5.83), reported several instances of discrimination (= 1.27), and appraised the stressors they experienced as very upsetting (= 2.11) compared to all the other classes. We labeled the fourth stress cluster high stress, low discrimination, low appraisal (Class 4), representing 21.7% of Black respondents. This stress cluster had respondents who reported a high number of ongoing chronic stressors (= 4.01), reported very low instances of discrimination (= 0.69), and appraised their stress as not that upsetting (= 0.88). The final stress cluster represented 25.3% of Black respondents and was labeled low stress, low discrimination, low appraisal (Class 5). This stress cluster was characterized by respondents who hardly reported any ongoing chronic stressors (= 0.74), hardly reported experiencing discrimination (= 0.43), and appraised their stress as not upsetting, if at all, (= 0.13) compared with all the other classes.
Figure 1.
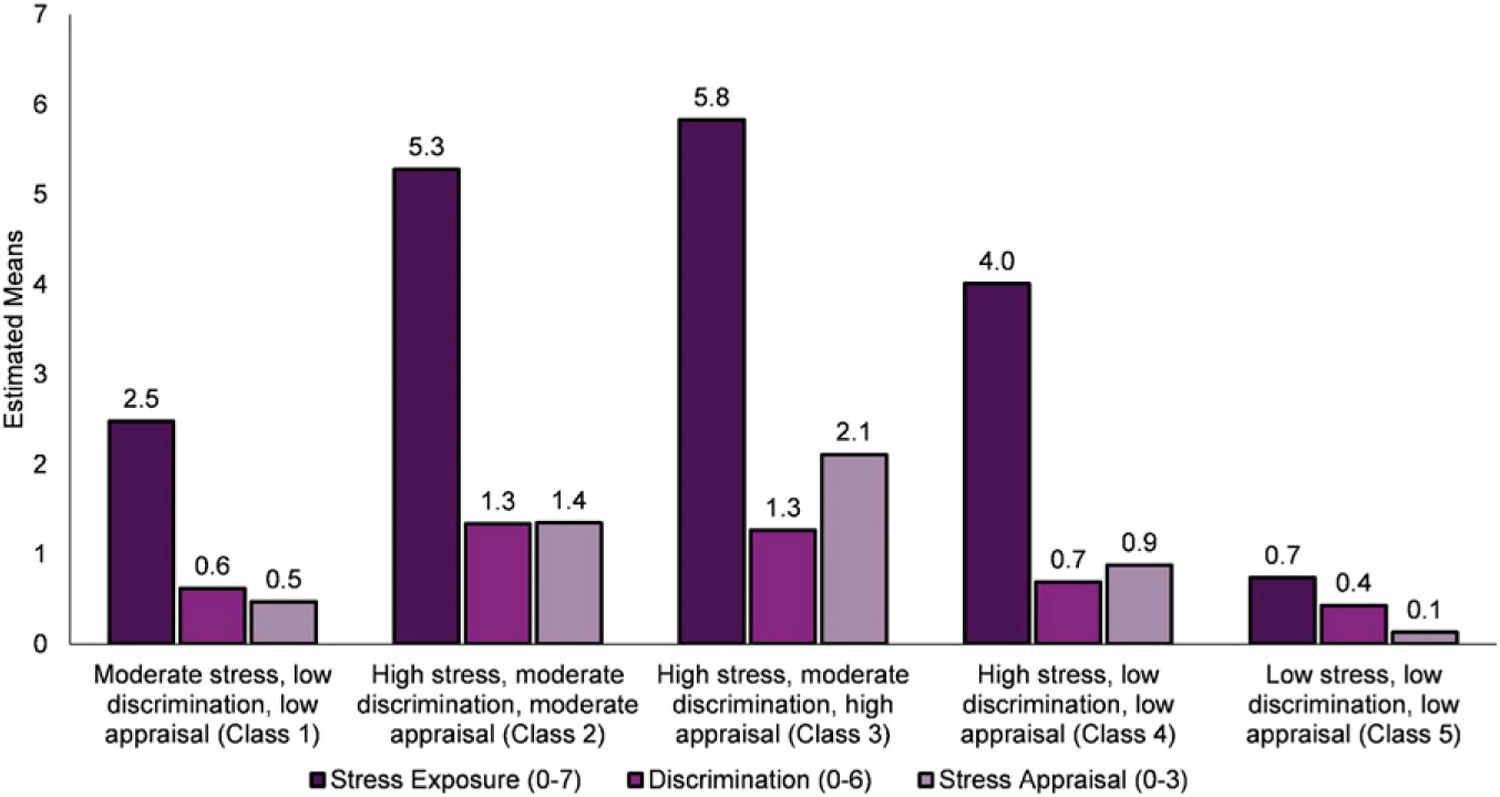
Stress profiles of the optimal five-class model among HRS Black respondents, 2010–2012 (n = 2,415).
Characteristics of Older Blacks by Stress Clusters
Table 3 presents weighted descriptive statistics of the study sample by stress cluster, with Wald-adjusted χ2 tests assessed at p < .05. Respondents across the clusters were, on average, approximately aged 60 and older, with respondents in the low stress, low discrimination, low appraisal cluster being the oldest (= 66.2). Females made up over half the sample across stress clusters. Respondents in the high stress, low discrimination, low appraisal cluster had a higher proportion of respondents who reported being married (38.9%) compared to other clusters. Socioeconomic characteristics show that respondents in the high stress, moderate discrimination, high appraisal and the high stress, moderate discrimination, moderate appraisal cluster were more socioeconomically disadvantaged relative to the other clusters (i.e., less educated, had lower household incomes, and lower household wealth). In contrast, respondents in the low stress, low discrimination, low appraisal cluster were more educated, had higher household income, and higher household wealth. The high stress, moderate discrimination, high appraisal cluster reported the highest number of CESD symptoms (= 4.0) and the low stress, low discrimination, low appraisal cluster reported the least number of CESD symptoms (= 1.1).
Table 3.
Descriptive characteristics of HRS Black respondents by stress cluster, 2010–2012 (n = 2,415).
| Moderate stress, low discrimination, low appraisal | High stress, moderate discrimination, moderate appraisal | High stress, moderate discrimination, high appraisal | High stress, low discrimination, low appraisal | Low stress, low discrimination, low appraisal | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Class 1 | Class 2 | Class 3 | Class 4 | Class 5 | ||||||
| % | N | % | N | % | N | % | N | % | N | |
| Age (mean) | 64.3b,d,e | 844 | 59.9a,d,e | 308 | 62.1e | 128 | 62.6a,b,e | 525 | 66.2a,b,c,d | 610 |
| Female | 56.8 | 525 | 62.8 | 217 | 54.2 | 84 | 60.9 | 349 | 63.3 | 412 |
| Marital status | ||||||||||
| Married | 37.9b | 354 | 27.5a,d,e | 94 | 33.3 | 43 | 38.9b | 219 | 38.2b | 250 |
| Divorced/separated | 27.8 | 205 | 32.2 | 101 | 30.8 | 44 | 30.3 | 144 | 25.4 | 161 |
| Widowed | 18.8 | 184 | 14.6e | 53 | 16.3 | 21 | 15.1e | 90 | 21.3b,d | 135 |
| Never married | 15.5b | 101 | 25.7a,d,e | 60 | 19.6 | 20 | 15.7b | 72 | 15.1b | 64 |
| Soioeconomic status | ||||||||||
| Education | ||||||||||
| Less than high school | 27.6 | 227 | 29.4 | 88 | 26.5 | 34 | 25.4 | 112 | 26.1 | 145 |
| High school/GED | 31.7 | 274 | 29.5 | 105 | 40.2 | 54 | 33.5 | 173 | 31.1 | 197 |
| Some college | 25.4 | 208 | 32.7 | 93 | 24.7 | 26 | 26.9 | 164 | 25.2 | 165 |
| College and above | 15.3b,c | 135 | 8.4a,d,e | 22 | 8.6a,e | 14 | 14.2b | 76 | 17.7b,c | 103 |
| Household income | ||||||||||
| 1st quartile ($0–$12,000) | 24.8b | 199 | 41.8a,d,e | 118 | 33.9 | 36 | 25.2b | 120 | 24.9b | 142 |
| 2nd quartile ($12,001–$24,727) | 23.2c | 195 | 23.4c | 77 | 35.9a,b,e | 50 | 26.4 | 145 | 23.8c | 145 |
| 3rd quartile ($24,728–$52,040) | 22.8 | 235 | 19.6 | 68 | 20.5 | 34 | 23.6 | 138 | 19.00 | 124 |
| 4th quartile ($52,041–$830,000) | 29.2b,c | 215 | 15.1a,d,e | 45 | 9.7a,d,e | 8 | 24.9b,c,e | 122 | 32.3b,c,d | 199 |
| Household wealth | ||||||||||
| 1st quartile ($−444,996 to $0) | 27.7b,c,e | 203 | 35.9a,e | 111 | 43.5a,d,e | 55 | 29.0c,e | 156 | 21.0a,b,c,d | 115 |
| 2nd quartile ($1–$24,000) | 23.2 | 201 | 30.1e | 99 | 27.8 | 35 | 22.2 | 118 | 18.4b | 107 |
| 3rd quartile ($24,001–$108,000) | 25.4 | 221 | 22.1 | 62 | 19.8 | 24 | 26.7 | 133 | 25.7 | 167 |
| 4th quartile ($108,001–$3,345,000) | 23.6b,c,e | 219 | 11.9a,b,e | 36 | 9.0a,d,e | 14 | 22.1b,c,e | 118 | 34.9a.b,d,e | 221 |
| Health | ||||||||||
| CESD symptoms (mean) | 1.5b,c,d,e | 844 | 2.9a,c,d,e | 308 | 4.0a,b,d,e | 128 | 1.9a,b,c,e | 525 | 1.1a,b,c,d | 610 |
| N | 844 | 308 | 128 | 525 | 610 | |||||
Note. Percentages are weighted; sample size (N) unweighted.
Significantly different from high stress, low discrimination, moderate appraisal class.
Significantly different from high stress, high discrimination, high appraisal class.
Significanly different from low stress, low discrimination, high appraisal class.
Significantly different from low stress, low discrimination, high appraisal class.
Significantly different from moderate stress, some discrimination, moderate appraisal class.
Stress Clusters and CESD Symptoms
Table 4 presents estimates from negative binomial regression models for CESD symptoms. Rate ratios (RRs) are presented with 95% confidence intervals (CI). RRs between zero and one indicate a decreased risk of reporting CESD symptoms, and RRs greater than one indicate an increased risk of reporting CESD symptoms. The low stress, low discrimination, low appraisal cluster is the reference group for these analyses. Results show that older Black adults in the moderate stress, low discrimination, low appraisal cluster (RR = 1.28, 95% CI [1.07,1.52]), the high stress, moderate discrimination, moderate appraisal (RR = 2.51, 95% CI [2.08,3.04]), the high stress, moderate discrimination, high appraisal cluster (RR = 3.36, 95% CI [2.69,4.18]), and the high stress, low discrimination, low appraisal cluster (RR = 1.62, 95% CI [1.35,1.94]) report more CESD symptoms relative to older Black adults in the low stress, low discrimination, low appraisal cluster, controlling for age and sex (Model 1). To determine if demographic or socioeconomic measures accounted for the differences observed in stress clusters, Model 2 adds marital status, educational attainment, household income, and household wealth. Results show that the reporting of CESD symptoms is reduced with the additional controls, but do not fully explain the differences found across the stress clusters.
Table 4.
Rate ratios (RR) with 95% confidence intervals (95% CI) for CESD symptoms among HRS Black respondents, 2010–2012 (n = 2, 415).
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| Stress clusters | ||||
| ref = low stress, low discrimination, low appraisal (Class 5) | ||||
| Moderate stress, low discrimination, low appraisal (class 1) | 1.28 | [1.07,1.52] | 1.21 | [1.02,1.43] |
| High stress, moderate discrimination, moderate appraisal (class 2) | 2.51 | [2.08,3.04] | 2.10 | [1.74,2.54] |
| High stress, moderate discrimination, high appraisal (class 3) | 3.36 | [2.69,4.18] | 2.86 | [2.27,3.61] |
| High stress, low discrimination, low appraisal (class 4) | 1.62 | [1.35,1.94] | 1.50 | [1.26,1.79] |
| Demographics | ||||
| Age | 1.00 | [1.00,1.01] | 1.00 | [0.99,1.00] |
| Female | 1.16 | [1.02,1.30] | 1.08 | [0.95,1.22] |
| Marital status (ref = married) | ||||
| Divorced/separated | 1.08 | [0.94,1.24] | ||
| Widowed | 1.05 | [0.87,1.27] | ||
| Never married | 1.05 | [0.87,1.25] | ||
| Socioeconomic status | ||||
| Education (ref = less than high school) | ||||
| High school/GED | 0.87 | [0.76,1.00] | ||
| Some college | 0.74 | [0.63,0.87] | ||
| College and above | 0.63 | [0.50,0.80] | ||
| Household income (ref = 1st quartile) | ||||
| 2nd quartile | 0.91 | [0.79,1.04] | ||
| 3rd quartile | 0.79 | [0.66,0.94] | ||
| 4th quartile | 0.66 | [0.53,0.81] | ||
| Household wealth (ref = 1st quartile) | ||||
| 2nd quartile | 0.93 | [0.79,1.08] | ||
| 3rd quartile | 0.83 | [0.71,0.97] | ||
| 4th quartile | 0.71 | [0.58,0.87] | ||
| Year of interview (ref = 2010) | ||||
| 2012 | 1.00 | [0.89,1.11] | 1.03 | [0.92,1.15] |
Note. All models are weighted.
We plotted the predicted number of CESD symptoms from the final model in Figure 2. Figure 2 shows that older Black adults in the low stress, low discrimination, low appraisal cluster reported the least number of CESD symptoms (= 1.3) compared to any other stress cluster. While older Black adults in the high stress, moderate discrimination, high appraisal cluster reported the greatest number of CESD symptoms (= 3.8), they did not significantly differ from the number of CESD symptoms reported by the high stress, moderate discrimination, moderate appraisal cluster (= 2.8).
Figure 2.
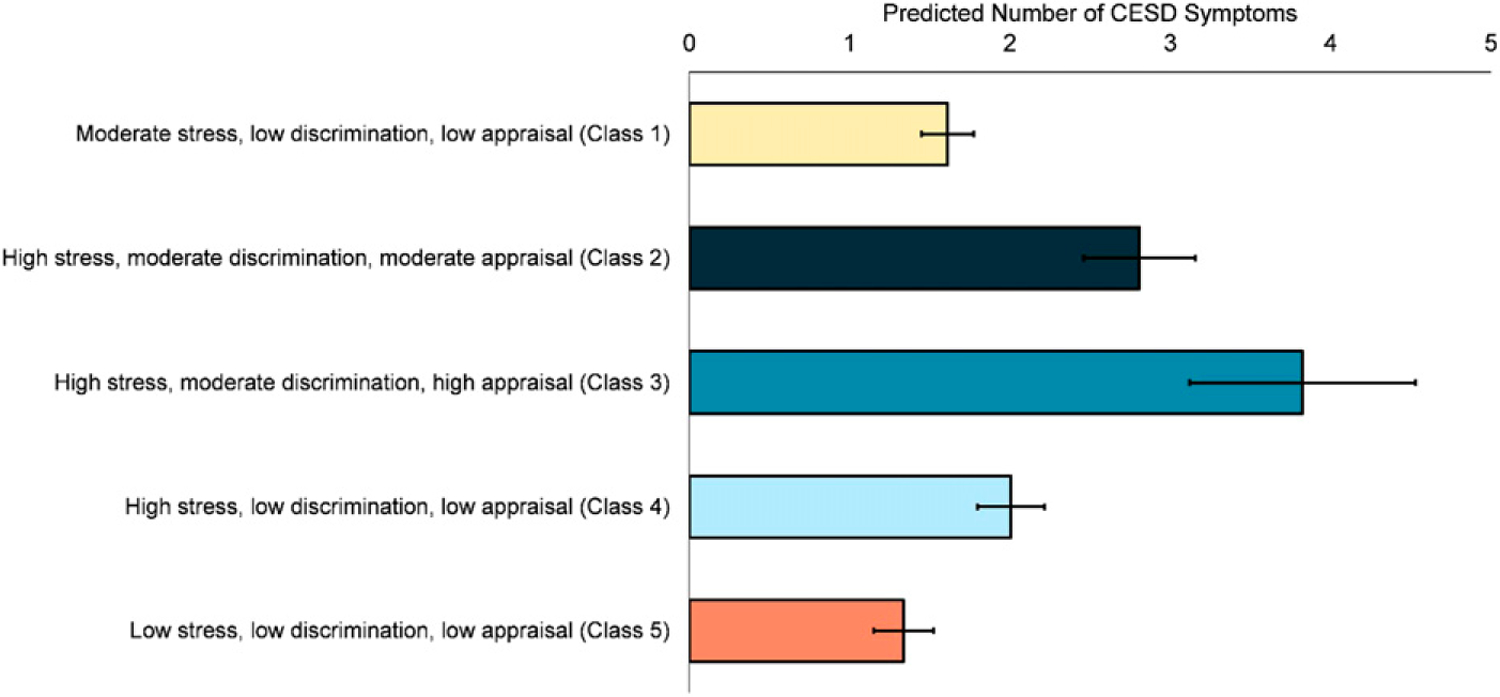
Predicted count of CESD symptoms by stress cluster among HRS Black respondents, 2010–2012 (n = 2,415).
Discussion
The purpose of this study is to build on evidence linking stress and mental health by empirically identifying stress profiles among older Black Americans that are associated with depressive symptomology. The results demonstrate the utility of a latent profile approach to characterize the stress experienced by Black older adults. We found that there is heterogeneity in the stress experience among Black Americans, dispelling notions that the Black experience is only characterized by overwhelming stress burdens. In fact, we found that there were five different profiles of stress exposure, discrimination and appraisal classifications that indicate Black Americans have a range of stress experiences that vary, in part, due to sociodemographic factors. For example, respondents who were classified as experiencing the most extreme stress burdens with high stress, moderate discrimination, and high appraisal (Class 3) were more socioeconomically disadvantaged relative to the other clusters. Respondents in this cluster had lower levels of education, household income, and wealth and also reported more CESD symptoms. The unique correlates within each stress profile suggests that these classes are distinct and suggests that neither the stress experience nor the effect of stress on the mental health of Black older adults can be captured with one dimensional counts of stress exposure. This broadened lens of the stress experience using LPA quantitatively incorporates coping strategies into stress measurement. Our results suggest that, for the high stress, moderate discrimination, and high appraisal cluster (Class 3), low socioeconomic status (SES) may be a source of increased vulnerability for Black older adults who are also exposed to race-related stressors. High SES may serve as a protective factor for Class 1 and Class 4—clusters that are defined by high or moderate stress exposure and discrimination but lower stress appraisal. Class 1 and Class 4 both have relatively higher SES than Class 3 and also report fewer depressive symptoms; thus, they may have the ability to cope with high or moderate stress and discrimination burdens via access to material resources.
The largest two clusters of Black older adults in our sample are the moderate stress, low discrimination, low stress appraisal (Class 1) cluster (n = 844; 35% of the sample) and the low stress, low discrimination, low appraisal (Class 5) cluster (n = 610; 25% of the sample), which are the groups with the highest income, education, and wealth (~55% of the sample), respectively. This suggests that the sampling frame used to recruit Black respondents into the HRS is pulling from relatively lower stress and higher SES clusters of Black older adults. One of the motivations behind Dr. James S. Jackson’s National Survey for American Life (NSAL) was to establish a sample that reflected the full geographic distribution of the Black American population since most community based surveys, like the HRS, were using sampling frames that reflect the older adult population but not necessarily the older Black American population (Lincoln et al., 2007). Focusing on the physical, emotional, mental, structural, and economic conditions of African Americans and Caribbean Blacks, with a major emphasis on mental health and mental illness, Dr. Jackson’s NSAL consists of 64 primary sampling units (PSUs). Fifty-six of these primary areas overlap substantially with existing Survey Research Center’s National Sample primary areas used in the HRS. However, the remaining eight primary areas were chosen from the South in order for the sample to represent African Americans in the proportion in which they are distributed nationally (Jackson et al., 2004; Lincoln et al., 2007). It may be the case that the HRS and other community-based surveys that do not intentionally sample Black people from the American South may only be capturing the stress and depressive symptoms of a relatively advantaged group of Black adults that fall into their sampling frame. One other thing to note, the HRS administered the Psychosocial and Lifestyle self-administered questionnaire that captures the stress and discrimination experience of respondents at the end of a very long baseline interview (over 3 hours, on average). This may lead to lower response rates and impact the type of Black older adults that end up completing the survey (Smith et al., 2013).
Despite there being five unique stress clusters that depict the variability in the stress experience for older Black adults, the clusters that predicted fewer depressive symptoms were those with low appraisal. The group with lowest stress appraisal also has low chronic stress exposure and discrimination profiles (Class 5). Yet, the unique and potentially stress buffering role of appraisal is highlighted when comparing the high stress, moderate discrimination, high appraisal (Class 3) cluster to the high stress, low discrimination, low appraisal (Class 4) cluster, the latter of which reports significantly fewer depressive symptoms. While these groups also differ in exposure to discrimination, appraisal is the consistent correlate of a lower depressive symptom count for all our classes. A central finding of this paper is that mental health outcomes are not just a function of the number of stress exposures and discriminatory events an individual reports. Stress appraisal is a tandem mechanism through which stress exposure and discrimination operate to reduce or exacerbate the detrimental effects of stress on mental health. Differences in whether or not a stressor is actually considered upsetting in the first place may be one mechanism through which Black older adults reduce the detrimental effects of stress on mental health, making a strong case for measuring stress as a latent construct.
One hypothesis that has emerged in the literature to explain the Black-white paradox in mental health is stress appraisal (Brown et al., 2018, 2020). It is highly plausible that given a prolonged history of marginalization, older Black adults have developed other coping mechanisms that may account for their mental fortitude. Older Black adults who appraise chronic stress as less upsetting relative to their white peers (Brown et al., 2018) may have found adaptive means or have habituated to higher stress burdens by reframing stress or developing cognitive shifts to reduce the stressfulness of an exposure (Amirkhan, 1994; Harrell, 2000). Black older adults in our sample came of age during Jim Crow, desegregation, and the Civil Rights Era and thus may perceive the more mundane chronic stressors that are measured here as less stressful since they have lived through very overt periods of racism and discrimination. It may also be that older Black adults who are able to effectively cope with a chronic stressor may report perceiving it as less severe over time even if it was a more intense stressor when the experience initiated. Importantly, these hypotheses engage race and age specific stress and coping mechanisms that highlight the distinct stress experience for older Black adults when trying to better understand Black-white differences in mental health, a point that is relevant for all future Black-white paradox work.
The use of LPA, a unique analysis procedure for questions examining the connection between stress and mental health among older Black adults suggests that we must center stress and stress measurement in the Black experience to capture the unique hardships and coping mechanisms these older adults use to sustain mental and physical well-being as they age. Despite the importance of this work, the findings are limited by restrictions in the study sample. First, one of the problems with studying appraisals is that their location in the stress process is unclear. While we use a measure of appraisal that has been utilized in other studies (Aldwin et al., 1996), the retrospective timing in which the questions are asked require respondents to report the stressfulness of chronic situations, even if it is not impacting them in the moment. Individuals may be reporting stress exposure during the past 12 months but at the point of the interview may be feeling less bothered by the stressor. Rather than older adults in the moment appraising a situation as less stressful, they may report it as less stressful because it did not ultimately affect their mental health, leaving us unable to rule out reverse causality. Similarly, because we are using cross-sectional data, some of our markers of SES may be the consequence of chronic stress exposure and not always the other way around (i.e., lower household income may be a consequence of ongoing physical health issues). Additionally, selective mortality among Black older adults may make the Blacks adults in this sample a select group of individuals who experienced less stress, have more access to socioeconomic resources, and who also cope well or who responded better to stressors. Importantly, we are measuring chronic stress, discrimination, appraisal, and mental health cross-sectionally when the relationship may vary over time. Finally, in measuring the “stress universe,” it would be appropriate to note the importance of including a wider array of race-based or related stressors (e.g., vicarious discrimination, incarceration, and intersectional stressors) in future research on the Black stress experience (Wheaton, 1994; Wheaton et al., 2013).
Defining stress as a latent construct demonstrates the variability in the stress experience for older Black adults, each cluster defining a unique experience with chronic stress exposure, appraisal, and discrimination. Importantly, stress exposure and discrimination are not the only features in the stress landscape that determine depressive symptomology among Black older adults. These stress clusters also suggest that appraisal-based stress measures alter the stress experience and, in some instances, greatly reduce the risk of depressive symptomology. Future work examining the mechanisms behind the Black-white mental health paradox should consider stress as a multidimensional construct. This work may also be furthered by replication in samples like Dr. Jackson’s NSAL since it is representative of the Black population in the United States and can capture the variability of the stress and mental health experience among a wider age range to understand how this relationship might vary over the life course. Dr. Jackson, as evidenced by the existence of the NSAL, seemed to be insightfully motivated to narrate both the joy and sorrow in Black life. His naming of stress as a latent construct acknowledges that the stress that Black people face can also be contextualized by their inner and intricate lives—lives that are weaved despite the stress burdens that America assumes is synonymous to Black life. Stress is not a unidimensional construct or a simple sum of exposures for Black people, but rather a multidimensional experience that has consequences for mental health based on other features of the individual and collective stress experience.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author’s Note
We would like to acknowledge the Program for Research on Black Americans (PRBA) and the Michigan Integrative Well-Being and Inequality Training Program (MIWI) at the University of Michigan for creating spaces for Black scholars to connect, work together, and provide opportunities to obtain mentorship from exceptional leaders like Dr. James S. Jackson.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aldwin CM, Sutton KJ, Chiara G, & Spiro IA (1996). Age differences in stress, coping, and appraisal: Findings from the normative aging study. The Journals of Gerontology: Series B, 51B(4), P188. 10.1093/geronb/51b.4.p179. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Amirkhan JH (1994). Criterion validity of a coping measure. Journal of Personality Assessment, 62(2), 242–261. 10.1207/s15327752jpa6202_6. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, & Patrick DL (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine, 10(2), 77–84. 10.1016/S0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- Assari S, Preiser B, Lankarani M, & Caldwell C (2018). Subjective socioeconomic status moderates the association between discrimination and depression in African American youth. Brain Sciences, 8(4), 71. 10.3390/brainsci8040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes DM, & Bates LM (2017). Do racial patterns in psychological distress shed light on the Black–White depression paradox? A systematic review. Social Psychiatry and Psychiatric Epidemiology, 52(8), 913–928. 10.1007/s00127-017-1394-9. [DOI] [PubMed] [Google Scholar]
- Bennett DA (2001). How can I deal with missing data in my study? Australian and New Zealand Journal of Public Health, 25(5), 464–469. 10.1111/j.1467-842X.2001.tb00294.x. [DOI] [PubMed] [Google Scholar]
- Brown LL, Abrams L, Mitchell UA, & Ailshire JA (2020). Measuring more than exposure: Does stress appraisal matter for Black–White differences in anxiety and depressive symptoms among older adults? Innovation in Aging, 4(5), igaa040. 10.1093/geroni/igaa040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LL, Mitchell UA, & Ailshire J (2018). Disentangling the stress process: Race/Ethnic differences in the exposure and appraisal of chronic stressors among older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 75(3), 650–660. Journal Article 10.1093/geronb/gby072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celeux G, & Soromenho G (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification, 13(2), 195–212. 10.1007/BF01246098. [DOI] [Google Scholar]
- Cogburn CD (2019). Culture, race, and health: Implications for racial inequities and population health. The Milbank Quarterly, 97(3), 736–761. 10.1111/1468-0009.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Gianaros PJ, & Manuck SB (2016). A stage model of stress and disease. Perspect Psychol Sci, 11(4), 456–463. 10.1177/1745691616646305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kessler RC, & Gordon LU (1995). Strategies for measuring stress in studies of psychiatric and physical disorders. APA PsycNet. [Google Scholar]
- Edwards F, Lee H, & Esposito M (2019). Risk of being killed by police use of force in the United States by age, race–ethnicity, and sex. Proceedings of the National Academy of Sciences, 116(34), 16793–16798. 10.1073/pnas.1821204116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erving CL, Thomas CS, & Frazier C (2018). Is the Black-White mental health paradox consistent across gender and psychiatric disorders? American Journal of Epidemiology, 188(2), 314–322. 10.1093/aje/kwy224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A, & Mawhorter S (2020). Housing affordability and security issues facing older adults in the United States. Public policy & aging report, 31(1), 30–32. 10.1093/ppar/praa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaydosh L, Schorpp KM, Chen E, Miller GE, & Harris KM (2018). College completion predicts lower depression but higher metabolic syndrome among disadvantaged minorities in young adulthood. Proceedings of the National Academy of Sciences, 115(1), 109–114. 10.1073/pnas.1714616114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, & Ford CL (2011). Structural racism and health inequities: Old issues, new directions. Du Bois Review: Social Science Research on Race, 8(1), 115–132. 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George LK, & Lynch SM (2003). Race differences in depressive symptoms: A dynamic perspective on stress exposure and vulnerability. Journal of Health and Social Behavior, 44(3), 353–369. 10.2307/1519784. [DOI] [PubMed] [Google Scholar]
- Harrell SP (2000). A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American Journal of Orthopsychiatry, 70(1), 42–57. 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- Herbert TB, & Cohen S (1993). Stress and immunity in humans: A meta-analytic review. Psychosomatic Medicine, 55(4), 364–379. 10.1097/00006842-199307000-00004. [DOI] [PubMed] [Google Scholar]
- Hudson DL, Neighbors HW, Geronimus AT, & Jackson JS (2016). Racial discrimination, John Henryism, and depression among African Americans. Journal of Black Psychology, 42(3), 221–243. 10.1177/0095798414567757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, Trierweiler SJ, & Williams DR (2004). The national survey of American life: A study of racial, ethnic and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research, 13(4), 196–207. 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemeny ME (2003). The psychobiology of stress. Current Directions in Psychological Science, 12(4), 124–129. 10.1111/1467-8721.01246. [DOI] [Google Scholar]
- Kessler RC, DuPont RL, Berglund P, & Wittchen HU (1999). Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. The American Journal of Psychiatry, 156(12), 1915–1923. 10.1176/ajp.156.12.1915. [DOI] [PubMed] [Google Scholar]
- Kraaij V, Arensman E, & Spinhoven P (2002). Negative life events and depression in elderly persons a meta-analysis. The Journals of Gerontology: Series B Psychological Sciences and Social Sciences, 57(1), P87–P94. 10.1093/geronb/57.1.P87. [DOI] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 509–515. 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping (CSZD). Springer Pub. Co. [Google Scholar]
- Lepore SJ (1995). Measurement of chronic stressors (Vol 1–Book, Section, pp. 102–120). Oxford University Press. [Google Scholar]
- Lewis TT, Cogburn CD, & Williams DR (2015). Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology, 11(1), 407–440. 10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln KD, Chatters LM, Taylor RJ, & Jackson JS (2007). Profiles of depressive symptoms among African Americans and Caribbean Blacks. Social Science & Medicine, 65(2), 200–213. 10.1016/j.socscimed.2007.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- Magidson J, Vermunt J, & Madura J (2020). Latent class analysis. In: SAGE research methods foundations. SAGE Publications Ltd. 10.4135/9781526421036883636. [DOI] [Google Scholar]
- Marshall GL, & Rue TC (2012). Perceived discrimination and social networks among older African Americans and caribbean blacks. Family & Community Health, 35(4), 300–311. 10.1097/FCH.0b013e318266660f. [DOI] [PubMed] [Google Scholar]
- McEwen BS (1998). Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840, 33–44. 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- Mezuk B, Abdou CM, Hudson D, Kershaw KN, Rafferty JA, Lee H, & Jackson JS (2013). White Box” Epidemiology and the social neuroscience of health behaviors: The environmental affordances model. Society and Mental Health, 3(2). 10.1177/2156869313480892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaels E, Thomas M, Reeves A, Price M, Hasson R, Chae D, & Allen A (2019). Coding the everyday discrimination scale: Implications for exposure assessment and associations with hypertension and depression among a cross section of mid-life African American women. Journal of Epidemiology and Community Health, 73(6), 577–584. 10.1136/jech-2018-211230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouzon DM Religious involvement and the black -white paradox in mental health. Race Soc Probl. 2017; 9(1):63–78. 10.1007/s12552-017-9198-9 [DOI] [Google Scholar]
- Neighbors HW, Jackson JS, Bowman PJ, & Gurin G (1983). Stress, coping, and black mental health: Preliminary findings from a national study. Prevention in Human Services, 2(3), 5–29. 10.1300/J293v02n03_02. [DOI] [PubMed] [Google Scholar]
- Paradies Y (2006). A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology, 35(4), 888–901. 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Park CL, & Folkman S (1997). Meaning in the context of stress and coping. Review of General Psychology, 1(2), 115–144. 10.1037/1089-2680.1.2.115. [DOI] [Google Scholar]
- Pearlin L, Lieberman M, Menaghan E, & Mullan J (1981). The stress process. Journal of Health and Social Behavior, 22(4), 337–356. 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- Pearlin LI (1989). The sociological study of stress. Journal of Health and Social Behavior, 30(3), 241–256. 10.2307/2136956. [DOI] [PubMed] [Google Scholar]
- Pearlin LI (2010). The life course and the stress process: Some conceptual comparisons. The Journals of Gerontology.Series B, Psychological Sciences and Social Sciences, 65B(2), 207–215. 10.1093/geronb/gbp106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, & Meersman SC (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46(2), 205–219. 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Regier DA (1988). One-Month Prevalence of Mental Disorders in the United States: Based on Five Epidemiologic Catchment Area Sites. Archives of General Psychiatry, 45(11), 977–986. 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- Rosenberg J, Beymer P, Anderson D, van Lissa CJ, & Schmidt J (2018). tidyLPA: An R package to easily carry out latent profile analysis (LPA) using open-source or commercial software. Journal of Open Source Software, 3(30), 978. 10.21105/joss.00978. [DOI] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, & Rowe Z (2006). Discrimination, symptoms of depression, and self-rated health among African American women in detroit: Results from a longitudinal analysis. American Journal of Public Health, 96(7), 1265–1270. 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM (2019). Stressnology: The primitive (and problematic) study of life stress exposure and pressing need for better measurement. Brain, Behavior, and Immunity, 75, 3–5. 10.1016/j.bbi.2018.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J, Fisher GG, Ryan LH, Clarke PJ, House J, & Weir DR (2013). Psychosocial and lifestyle questionnaire 2006—2010: Documentation report. Survey Research Center, Institute for Social Research, University of Michigan. [Google Scholar]
- Taylor HO, Taylor RJ, Nguyen AW, & Chatters L (2018). Social isolation, depression, and psychological distress among older adults. Journal of Aging and Health, 30(2), 229–246. 10.1177/0898264316673511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, & Chatters LM (2020). Psychiatric disorders among older Black Americans: Within- and between-group differences. Innovation in Aging, 4(3), igaa007. 10.1093/geroni/igaa007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits PA (1995). Stress, coping, and social support processes: Where are we? What next? Journal of Health and Social Behavior, 35, 53–79. 10.2307/2626957. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, & Sutton-Tyrrell K (2003). Chronic stress burden, discrimination, and sub-clinical carotid artery disease in African American and Caucasian women. Health Psychology, 22(3), 300–309. 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- Vega WA, & Rumbaut RG (1991). Ethnic minorities and mental health. Annual Review of Sociology, 17(1), 351–383. 10.1146/annurev.so.17.080191.002031. [DOI] [Google Scholar]
- Vuong QH (1989). Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica, 57(2), 307. 10.2307/1912557. [DOI] [Google Scholar]
- Wheaton B (1994). Sampling the stress universe. Avison W & Gotlib I, (Eds.), Vol. 1–Book, Section,, pp. 77–114). Springer; US. 10.1007/978-1-4899-1106-3_4 [DOI] [Google Scholar]
- Wheaton B, Young M, Montazer S, & Stuart-Lahman K (2013). Social stress in the twenty-first century. Aneshensel C, Phelan J, & Bierman A, (Eds.), Vol. 1–Book, Section,, pp. 299–323). Springer; Netherlands. 10.1007/978-94-007-4276-5_15 [DOI] [Google Scholar]
- Williams DR (2018). Stress and the mental health of populations of color: Advancing our understanding of race-related stressors. Journal of Health and Social Behavior, 59(4), 466–485. 10.1177/0022146518814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Collins C (2001). Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports, 116(5), 404–416. 10.1016/S0033-3549(04)50068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, & Jackson JS (2007). Prevalence and distribution of major depressive disorder in African Americans, caribbean blacks, and Non-Hispanic Whites. Archives of General Psychiatry, 64(3), 305–315. 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2008). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32(1), 20–47. 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yan Yu, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]


