Abstract
Background:
Esophagogastric junction contractile integral (EGJ-CI) and EGJ morphology are high-resolution manometry (HRM) metrics that assess EGJ barrier function. Normative data standardized across world regions and HRM manufacturers are limited.
Methods:
Our aim was to determine normative EGJ metrics in a large international cohort of healthy volunteers undergoing HRM (Medtronic, Laborie, and Diversatek software) acquired from 16 countries in four world regions. EGJ-CI was calculated by the same two investigators using a distal contractile integral-like measurement across the EGJ for three respiratory cycles and corrected for respiration (mm Hg cm), using manufacturer-specific software tools. EGJ morphology was designated according to Chicago Classification v3.0. Median EGJ-CI values were calculated across age, genders, HRM systems, and regions.
Results:
Of 484 studies (28.0 years, 56.2% F, 60.7% Medtronic studies, 26.0% Laborie, and 13.2% Diversatek), EGJ morphology was type 1 in 97.1%. Median EGJ-CI was similar between Medtronic (37.0 mm Hg cm, IQR 23.6–53.7 mm Hg cm) and Diversatek (34.9 mm Hg cm, IQR 22.1–56.1 mm Hg cm, P = 0.87), but was significantly higher using Laborie equipment (56.5 mm Hg cm, IQR 35.0–75.3 mm Hg cm, P < 0.001). 5th percentile EGJ-CI values ranged from 6.9 to 12.1 mm Hg cm. EGJ-CI values were consistent across world regions, but different between manufacturers even within the same world region (P ≤ 0.001). Within Medtronic studies, EGJ-CI and basal LESP were similar in younger and older individuals (P ≥ 0.3) but higher in women (P < 0.001).
Conclusions:
EGJ morphology is predominantly type 1 in healthy adults. EGJ-CI varies widely in health, with significant gender influence, but is consistent within each HRM system. Manufacturer-specific normative values should be utilized for clinical HRM interpretation.
Keywords: barrier function, esophagogastric junction, lower esophageal sphincter pressure
1 |. INTRODUCTION
Evaluation of the esophagogastric junction (EGJ) is an important component of esophageal physiologic testing using high-resolution manometry (HRM). The EGJ is an anatomically complex structure composed of the lower esophageal sphincter (LES) and crural diaphragm (CD), which together represent the barrier between the esophageal and gastric lumens.1 The integrity of the barrier is influenced by CD contraction and relaxation during respiration, and LES resting tone.2,3 Barrier function has traditionally been assessed using LES resting pressures at mid-respiration and end-expiration as well as LES length.4
Two HRM metrics have been proposed as measures of EGJ barrier function by the Lyon Consensus5. First, EGJ barrier morphology can be categorized based on the relationship between the LES and CD into normal (type 1, LES superimposed on CD), and abnormal (hiatus hernias: type 2, <3 cm separation; type 3, ≥3 cm separation).6–8 The second metric, EGJ contractile integral (EGJ-CI), is a novel HRM metric designed to assess EGJ barrier function, taking inspiratory and expiratory pressures, and EGJ length into account. While abnormal morphology and low EGJ-CI have been demonstrated to associate with abnormal esophageal reflux burden, normative data are limited to small single-center studies and have not been systematically evaluated across multiple centers and world regions.5
In this study, we analyzed HRM studies from asymptomatic, healthy volunteers obtained from collaborators worldwide. We aimed to define normative EGJ anatomy and physiology across different HRM systems and world regions.
2 |. METHODS
Studies from healthy, asymptomatic volunteers were solicited from motility laboratories and research centers worldwide. Respondents were asked to provide de-identified HRM studies, performed using commercially available HRM systems (Medtronic; Laborie; Sandhill Scientific, now Diversatek). Studies were uploaded into secure online repositories along with patient demographics. Each individual institution or motility center performed studies in healthy asymptomatic volunteers, mostly enrolled through local advertisement, with local institutional review board approval of the protocol utilized. Since this investigation involved interpretation of de-identified data collected from these individual institutions and motility centers without any link to human subjects, formal approval was not deemed necessary, and a waiver of consent was provided through the Human Research Protection Office (institutional review board) at Washington University in St. Louis School of Medicine.
Each study was re-analyzed by two investigators (BDR, CPG) using dedicated analysis software specific to each HRM manufacturer. For the purpose of this study, only the resting or landmark phase was analyzed. This consists of a 20–30 second period of quiet rest typically in the recumbent or semi-recumbent position after acclimatization to the catheter, devoid of swallows or artifacts.9 Studies without an adequate resting phase were excluded.
Traditional metrics consisted of EGJ pressures and anatomic measurements and were extracted using embedded software. LES pressures were measured across three respirations at the mid-respiratory point (basal LES pressure, reflecting combined LES and CD pressures) and at the end of expiration (end-expiratory LES pressure, reflecting intrinsic LES resting tone). Length of the LES/EGJ high pressure zone was also retrieved. In type 2 morphology, LES length was measured independent of CD contribution; however, in type 1 morphology the two structures are superimposed, producing a single LES/EGJ length measurement.
Morphology of the EGJ was characterized by assessing the relationship between the intrinsic LES and CD. Normal EGJ morphology (type 1) consisted of superimposed LES and CD. Axial separation indicated presence of a hiatus hernia, where <3 cm defined type 2 morphology, and ≥3 cm defined type 3 morphology.6,10
Methodology similar to that used to calculate esophageal body distal contractile integral (DCI) is utilized for EGJ-CI calculation. Vigor of the EGJ barrier function is evaluated by generating a measure of length and vigor of the EGJ relative to the gastric baseline, using embedded software tools within each HRM platform (Figure 1). This is analyzed over three respirations and made independent of respiratory cycle by dividing by duration of the three cycles (reported as mm Hg cm).11 The EGJ-CI is measured across the LES alone in type 3 EGJ morphology, although this was not applicable to this study, as there were no individuals with type 3 morphology.
FIGURE 1.
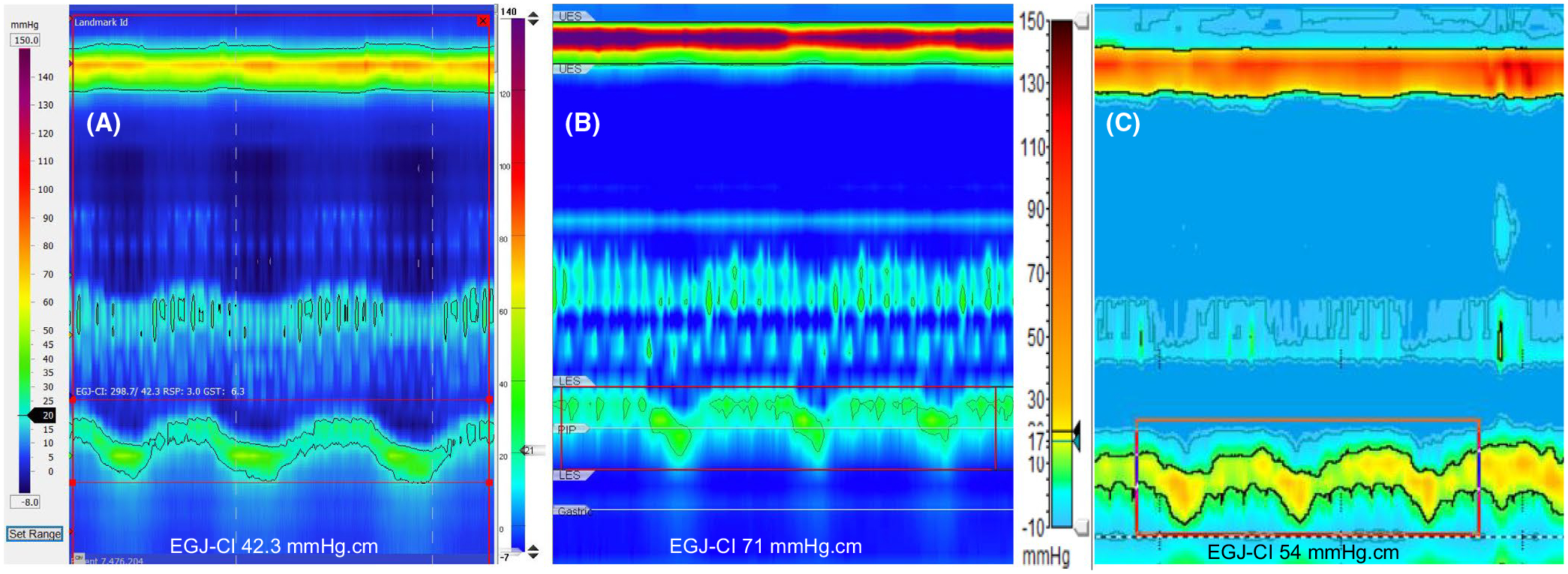
Measurement of esophagogastric junction contractile integral (EGJ-CI). Vigor of the EGJ barrier is measured above the gastric baseline pressure, taking EGJ length, contraction pressure and respiratory variation over three respiratory cycles, and corrected for duration of respiration by dividing the recorded value by the duration of three respirations. A, Medtronic system, where a beta version of an automated software tool was used. B, Laborie, where an automated software tool was used. C, Diversatek, where manual calculation was required after creating a distal contractile integral-like box and separate estimation of the gastric pressure.
2.1 |. Data analysis
Data are reported as mean ± standard error of the mean (SEM) or mean, interquartile range (IQR), and 5th-95th percentiles unless otherwise indicated. Categorical data were compared using the χ-squared and Fisher’s exact test, and continuous data were analyzed using the two-tailed Student’s t test, ANOVA, or Kruskal–Wallis test, with Bonferroni correction for multiple comparisons when appropriate. A P value of <0.05 was considered significant. SPSS Statistics v26.0 was utilized for all statistical analyses.
3 |. RESULTS
Of 484 unique studies (28.0 years, IQR: 24.0–35.0; 56.2% female) acquired from 16 countries in 4 continents, 60.7% were performed using Medtronic equipment, 26.0% using Laborie, and 13.2% using Diversatek. Medtronic studies were evenly split between males and females, while females were represented in greater proportions in studies using Laborie (69.8%) and Diversatek (57.8%, P = 0.001 across groups). Individuals studied using Laborie were significantly younger (median age 26.0 years, range 20–71 years) compared to those evaluated using Medtronic (27.7 years, range 18–79 years) and Diversatek (30.0 years, range 20–59 years, P < 0.001, Table 1), despite overlaps in range of ages. Notably, statistically significant differences were observed between HRM manufacturers in all categories of EGJ metrics evaluated (Table 1). EGJ morphology was type 1 in 97.1% of all volunteers (Table 1), with the remainder exclusively type 2 morphology. The median LES lengths were 3.0 cm with Laborie and Sandhill, but median length was significantly longer using Medtronic (3.7 cm, P < 0.001 compared to both).
TABLE 1.
Clinical characteristics by HRM system.
| Medtronic n = 294 | Laborie n = 126 | Diversatek n = 64 | P value | |
|---|---|---|---|---|
| World regions | ||||
| Asia | 68 (23.1%) | 69 (54.8%) | 39 (60.9%) | <0.001 |
| Europe | 43 (14.6%) | 57 (45.2%) | ||
| Latin America | 64 (21.8%) | 25 (39.1%) | ||
| North America | 119 (40.5%) | |||
| Age (y) | 27.7 (24.0–34.9) | 26.0 (22.8–37.0) | 30.0 (28.0–35.8) | <0.001 |
| Gender (% female) | 147 (50.0%) | 88 (69.8%) | 37 (57.8%) | 0.001 |
| EGJ morphology | ||||
| Type 1 | 288 (98.0%) | 122 (96.8%) | 60 (93.8%) | 0.19 |
| Type 2 | 6 (2.0%) | 4 (3.2%) | 4 (6.3%) | |
| EGJ-CI (mmHg.cm) | 37.0 (23.6–53.7) | 56.5 (35.0–75.3) | 34.9 (22.1–56.1) | <0.001 |
| Basal LESP (mmHg) | 22.5 (16.3–30.3) | 29.0 (21.8–44.0) | 27.1 (20.2–35.7) | 0.002 |
| End-expiratory LESP (mmHg) | 13.7 (8.1–20.5) | 14.0 (8.0–21.0) | 9.8 (5.5–14.9) | <0.001 |
| LES length (cm) | 3.7 (3.2–4.2) | 3.0 (2.6–3.5) | 3.0 (2.2–3.5) | <0.001 |
Values expressed as median (interquartile range) or number (%).
Abbreviations: EGJ, esophagogastric junction; EGJ-CI, EGJ contractile integral; HRM, high-resolution manometry; LES, lower esophageal sphincter; LESP, LES pressure.
The median EGJ-CI was similar between Medtronic (37.0 mmHg. cm, IQR 23.6–53.7 mmHg.cm) and Diversatek (34.9 mm Hg cm, IQR 22.1–56.1 mmHg.cm, P = 0.87), but was significantly higher using Laborie equipment (56.5 mm Hg cm, IQR 35.0–75.3 mmHg. cm, P < 0.001 compared to both groups, Figure 2). Fifth percentile EGJ-CI values were 8.4, 12.1, and 6.9 mmHg.cm in Medtronic, Laborie, and Diversatek studies, respectively (Figure 2). Basal LES pressures were significantly different between the three manufacturers (P = 0.002 for each comparison, Table 1). Fifth percentile basal LES pressure values were 7.4, 10.7, and 11.9 mmHg, and end-expiratory LES pressures were 1.5, 2.0, and 1.5 mmHg for Medtronic, Laborie, and Diversatek, respectively (Figure 2). Although basal and end-expiratory LES pressures correlated significantly with EGJ-CI in all manufacturers (P < 0.001), correlation coefficients were stronger in the Medtronic and Laborie subgroups (r2 = 0.70 and 0.81, respectively) compared to Diversatek (r2 = 0.28, Figure 3A) in basal LES pressures. Correlations between EGJ-CI and end-expiratory LES pressure followed similar trends in Medtronic and Laborie subgroups (r2 = 0.72 and 0.66, respectively), although Diversatek studies demonstrated poorer correlation (r2 = 0.09, Figure 3B).
FIGURE 2.
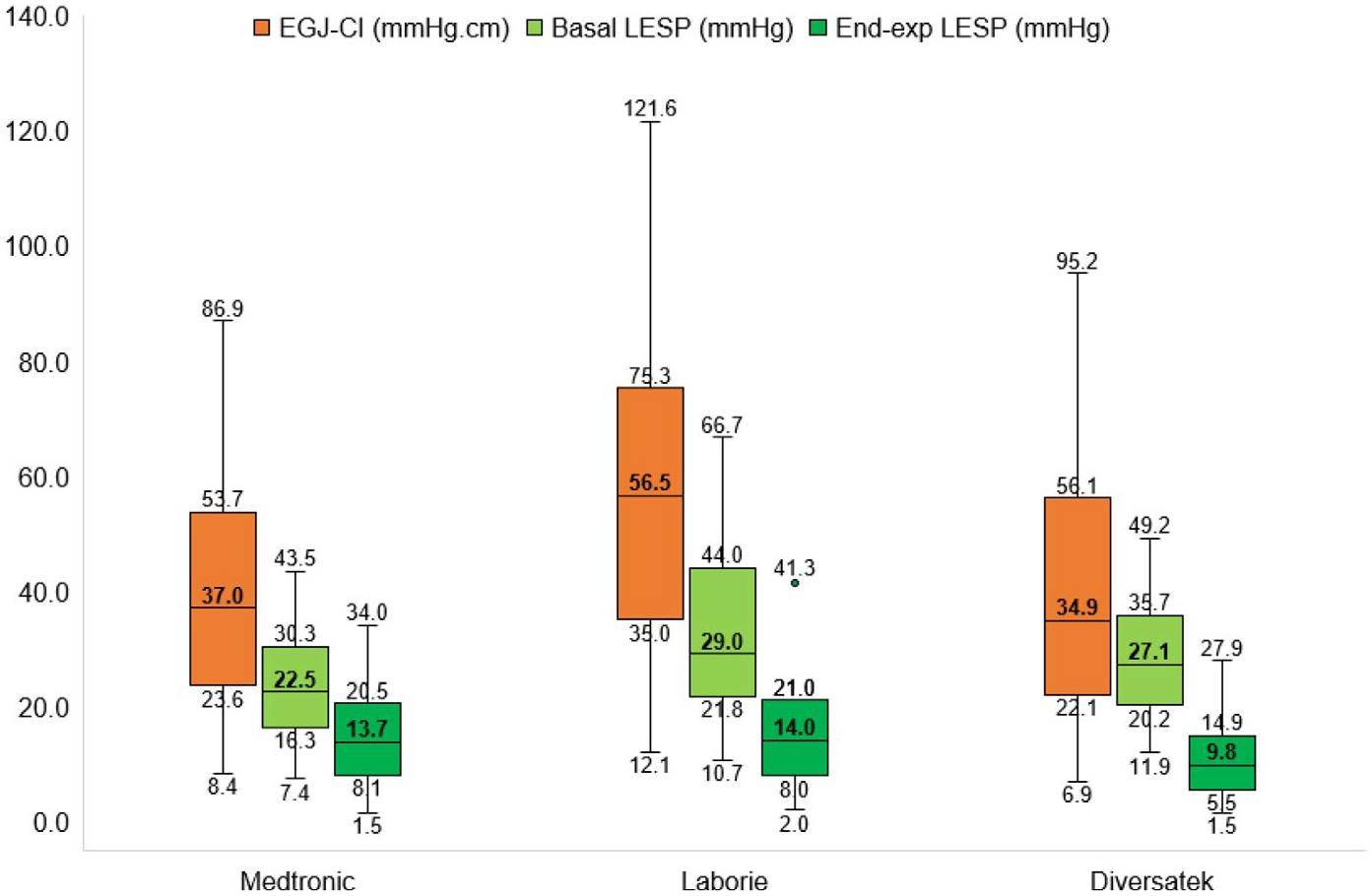
Assessment of esophagogastric junction (EGJ) function using the three HRM software systems, displayed using box and whisker plots. The extents of the box plots represent 25th-75th percentile values, and the whiskers depict 5th and 95th percentile values. The horizontal line within the boxes depicts the median value in bold font. While EGJ contractile integral (EGJ-CI) values measured using Medtronic and Diversatek were similar, measurements using Laborie systems were significantly higher. Lower esophageal sphincter pressures, both basal and end-expiratory, were significantly different between HRM systems.
FIGURE 3.
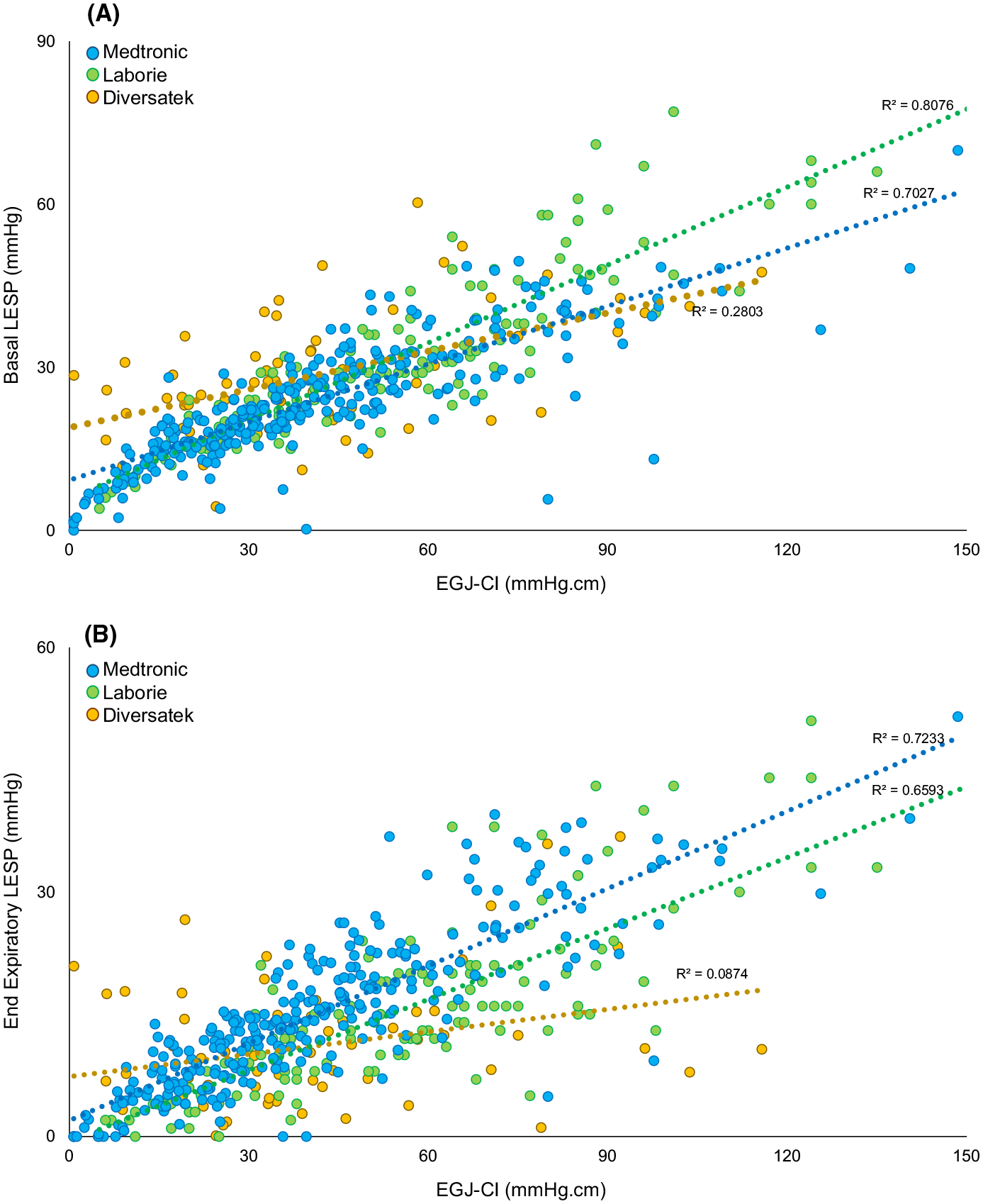
Correlation between A. esophagogastric junction contractile integral (EGJ-CI) and basal lower esophageal sphincter pressure (LESP), and B. EGJ-CI and end-expiratory LESP. Correlation was stronger with Medtronic and Laborie systems.
All four regions (Asia, Europe, Latin America, North America) contributed studies analyzed using Medtronic equipment. However, Laborie studies were provided from Asian and European countries only, while Diversatek studies were provided by Asian and Latin American countries. When analyzing by world regions, EGJ-CI calculated using each manufacturer was found to be consistent across world regions, but different between manufacturers even within the same world region (Figure 4A). Basal LESP followed the same trend for Asia and Latin America but not Europe (Figure 4B). Although end-expiratory pressures were similar in both Medtronic and Laborie studies, there was a statistically significant difference when comparing across world regions using Diversatek (P = 0.001, Figure 4C).
FIGURE 4.
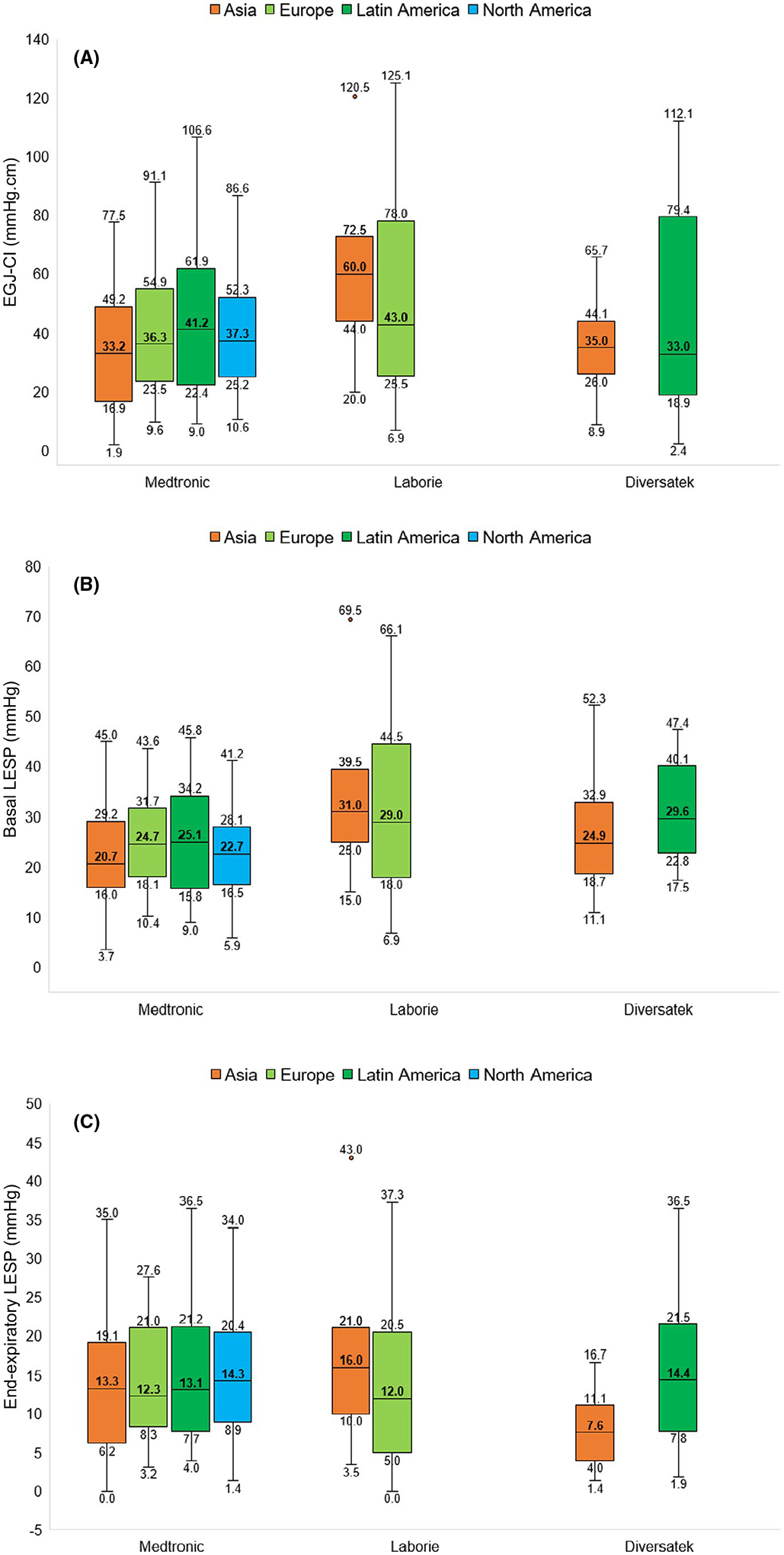
Variation in esophagogastric junction (EGJ) function assessment (A: EGJ contractile integral (EGJ-CI), B: basal lower esophageal sphincter pressure (LESP), C: end-expiratory LESP) across world regions displayed using box and whisker plots. The extents of the box plots represent 25th-75th percentile values, and the whiskers depict 5th and 95th percentile values. The horizontal line within the boxes depicts the median value in bold font. Values were generally consistent within each measurement system across world regions, while values were significantly different between systems, even when assessed within the same world region.
Small and non-significant differences were found in proportions of volunteers >50 years of age (7.8%−8.5%, P > 0.05) between manufacturers, but absolute numbers were smaller in the Laborie (10 studies) and Diversatek (five studies) groups compared to Medtronic (25 studies). Given this, representation from each world region, and equal representation between males and females, only Medtronic studies were analyzed for age and gender differences. In those >50 years of age, EGJ-CI, basal LESP, end-expiratory LESP, and LES length were all numerically lower than in their younger counterparts. However, only in end-expiratory LESP and LES length were the differences significant (P ≤ 0.048, Table 2). When assessing metrics by gender, females were noted to have a significantly greater EGJ-CI, basal LESP, and end-expiratory LESP; only LES length was similar between men and women (Table 2).
TABLE 2.
Comparison of EGJ metrics by age and gender in Medtronic subgroup.
| Age | Gender | |||||
|---|---|---|---|---|---|---|
| <50 y | ≥50 y | Female | Male | |||
| n = 269 | n = 25 | P value | n = 147 | n = 147 | P value | |
| EGJ-CI (mmHg.cm) | 37.4 (24.1–53.8) | 34.5 (21.2–54.2) | 0.26 | 42.0 (27.5–57.7) | 30.4 (19.3–48.4) | <0.001 |
| Basal LESP (mmHg) | 22.8 (16.4–30.4) | 20.1 (14.6–30.0) | 0.31 | 26.2 (18.6–32.4) | 20.3 (15.6–26.4) | <0.001 |
| End-expiratory LESP (mmHg) | 14.1 (8.4–20.8) | 10.7 (6.6–14.9) | 0.048 | 15.4 (9.6–22.5) | 11.7 (6.7–18.5) | <0.001 |
| LES length (cm) | 3.7 (3.3–4.2) | 3.3 (2.6–4.0) | 0.02 | 3.7 (3.3–4.3) | 3.7 (3.1–4.1) | 0.33 |
Values expressed as median (interquartile range) or number (%).
Abbreviations: EGJ, esophagogastric junction; EGJ-CI, EGJ contractile integral; LES, lower esophageal sphincter; LESP, LES pressure.
4 |. DISCUSSION
This international study utilized data from 16 countries in four continents and three manufacturers to establish normative HRM values for EGJ morphology and barrier function metrics. We report that EGJ morphology is almost exclusively type 1 in asymptomatic volunteers (2.9% type 2 and no type 3 morphology). Our findings suggest that normality, as reflected by 5th to 95th percentile values, covers a broad range and varies by manufacturer, thus precluding use of EGJ-CI as a stand-alone metric in defining competence of the EGJ barrier.
The predominance of existing literature evaluated EGJ barrier function using static pressure measurements at either the end or midpoint of expiration.4,12 With HRM, software tools have allowed pressure pattern interrogation using innovative and reproducible methods. Concepts first applied to assess esophageal smooth muscle contraction (namely, DCI) were initially utilized used to interrogate the EGJ,13 although employing a fixed time window. Given recognition of CD contribution and respiratory variation between individuals, EGJ-CI evolved from earlier metrics to include three respiratory cycles.14 In its current form, the EGJ-CI is measured above the gastric baseline and divided by the duration of 3 respiratory cycles to ensure consistency and independence from respiratory cycle duration5,11. Early investigations showed promise in identifying patients with pathologic reflux defined by erosive disease or abnormal reflux burden11,14,15. The importance of CD contribution to EGJ barrier function, particularly related to inspiratory augmentation, was further demonstrated by 3-D HRM studies3,16. Capturing the complete respiratory cycle is a proposed benefit of EGJ-CI3. However, existing studies lacked standardized calculation methods precluding definitive assessments regarding normal values.
International consensus literature recommended the use of EGJ-CI as an adjunctive HRM measure and proposed standardization by measuring above the gastric baseline and including of the CD except in those with type 3 morphology.5,7 Using this methodology, we analyzed studies from asymptomatic individuals across 16 countries and using the 3 most commonly employed HRM systems to determine international normative standards. From the outset, we noted that EGJ-CI data are broad in range, providing a possible explanation for prior difficulties in establishing normal thresholds. That each manufacturer’s values were consistent across world region analyses suggests consistency in methodology, and that differences between HRM manufacturers may contribute more to disagreements than variations in extraction and interpretation. However, variation of correlation coefficients between EGJ-CI and basal and end-expiratory pressures between manufacturers suggests that there is still opportunity for improved standardization.
We report the 5th and 95th percentile EGJ-CI values in asymptomatic volunteers. The 95th percentile value (86.9–124.0 mmHg. cm) is likely of low clinical consequence. The 5th percentile EGJ-CI values (6.9–12.1 mmHg.cm) overlapped significantly across all manufacturers with values previously associated with abnormal reflux burden. Of note, EGJ-CI values below the 25th percentile (22.1, 23.6, and 35.0 mmHg.cm in Diversatek, Medtronic, and Laborie, respectively) overlapped much less with values between the 25th percentile (3–20 mmHg.cm) and 75th percentile (21.0–63.0 mmHg. cm) in GERD patients, albeit using different gastric baseline thresholds.11,14,15,17–20 Limited data using a 24-channel, water-perfused HRM system manufactured by a Brazilian company suggested higher thresholds (5th percentile, 21.7 mmHg.cm; 25th percentile, 34.3 mmHg.cm).21 In another small subset of patients studied using 3D Medtronic HRM catheter, median EGJ-CI values were higher (65.4, IQR 52.3–98.9 mmHg.cm) when calculated at 2 mm Hg above the gastric baseline.3 This lack of consistency suggests that EGJ-CI is best utilized as an adjunctive metric rather than providing a definitive zone of normality, consistent with the Lyon consensus recommendation.5
Our data suggest that EGJ-CI is not affected by age, which agrees with a report by Cock et al, who noted similar EGJ-CI in younger and older individuals, even at ages higher than those evaluated in this study22. In contrast, when grouping by sex, female volunteers had higher EGJ-CI and conventional LES pressure metrics using the Medtronic system (Table 2). EGJ-CI was consistent across all 4 world regions when the same HRM system was used, and in spite of differences between systems. Finally, we noted that EGJ morphology is consistently type 1, with limited type 2 morphology and no type 3 morphology, regardless of world region or manufacturer.
The strength of this investigation lies in contribution from experienced motility centers worldwide and the large number of studies collected. The volume of studies (Medtronic subgroup, in particular) allowed insight into age and gender influences and comparison across manufacturers and world regions. Additionally, inter-reviewer variability was mitigated through independent joint analysis of each study by the same two investigators. These measures allowed a more complete perspective of normative values than has been previously possible. However, our study is not without limitations. We noted less worldwide availability of asymptomatic volunteer studies using Laborie and Diversatek, preventing the detailed subgroup analysis performed on asymptomatic volunteers evaluated using Medtronic equipment. Additionally, although these subjects were collected from experienced motility centers, endoscopic records, and ambulatory reflux monitoring data were not available to independently confirm healthy asymptomatic designation. Most centers enrolled asymptomatic subjects via advertisement, but precise enrollment criteria across centers could not be verified. Additional data regarding subject characteristics, including height, weight, nutritional status, and alcohol and tobacco use, would have benefited the analysis. These studies were obtained during the fasting state and according to standard manometry protocols, and therefore do not provide insights into the postprandial or ambulatory settings. The influence of volunteer position during manometry and utilization of solid state versus water-perfused equipment could not separately analyzed due to lack of granular data. We also note that the technical process of obtaining EGJ measurements varies between manufacturer, with varying degrees of interpretation automation. Our data would have been more robust if larger numbers of older volunteers had been studied, although we acknowledge the difficulty in identifying such individuals. Future normative projects will also benefit from inclusion of studies from the African continent, which was not represented here. Nevertheless, our report represents normative data from across the world and the 3 most commonly employed HRM systems and contributes to normative assessments of EGJ barrier function worldwide.
In conclusion, important variations exist in EGJ metrics between HRM manufacturers. However, assessments from the same manufacturer can be reliably interpreted regardless of world region, as long as manufacturer-specific thresholds are utilized. Normal EGJ barrier function, though almost exclusively type 1 morphology, covers a broad spectrum of function on physiologic assessment, precluding use of a singular normative threshold and limiting usefulness of 5th percentile values. This supports the concept that intact barrier function is dependent upon complex influences. Assessment of treatment outcomes based on a range of normality and using the standardized technique we describe may improve our understanding of EGJ barrier function.
Key Points.
Esophagogastric junction (EGJ) morphology and EGJ contractile integral (EGJ-CI) are high-resolution manometry (HRM) metrics evaluating EGJ barrier function at rest.
EGJ morphology is overwhelmingly type 1 (superimposed lower esophageal sphincter and crural diaphragm) in healthy volunteers.
EGJ-CI varies widely in health, with higher values in women, and HRM manufacturer-specific normative thresholds.
ACKNOWLEDGMENTS
No writing assistance was obtained.
DISCLOSURES
BDR: no disclosures; AR: no disclosures; SB: no disclosures; SB: no disclosures; DAC: Medtronic (teaching and consulting); also has a licensing agreement with Medtronic; DC: no disclosures; SG: no disclosures: HA: no disclosures; JH: no disclosures; OK: no disclosures; YYL: no disclosures; AML: no disclosures; AP: no disclosures; JP: no disclosures; RR: no disclosures; JMRT: Consulting: Medtronic, Takeda, Asofarma. Lecture Fee: Medtronic, Takeda, Asofarma, Janssen and Sanfer. SR: consulting Medtronic, research support Diversatek Healthcare, Medtronic; ES: Lecture Fee: Medtronic, Takeda, Janssen, MSD, Abbvie, Malesci; Consulting: Medtronic, Takeda, Janssen, MSD, Reckitt Bencikser, Sofar, Unifarco, SILA, Oftagest; JS: received research grants or acted as consulter/speaker for AB-biotics, Allergan, Bayer, Cassen-Recordati, Norgine, Reckitt Benkiser, Salvat and Zespri; DS: research grants: Reckitt Benckiser UK, Jinshan Technology China, Alfa Sigma Italy; ST: no disclosures; ZW: no disclosures; FZ: Reckitt Benckiser (consulting); JEP: Medtronic, Diversatek, Torax, Ironwood, Takeda, and Astra Zeneca (consulting); Impleo (research funding); Crospon (stock options); CPG: Consulting: Medtronic, Diversatek, Isothrive, Ironwood, Quintiles.
Footnotes
CONFLIC T OF INTEREST
No conflicts of interest exist.
REFERENCES
- 1.Mittal RK, Balaban DH. The esophagogastric junction. N Engl J Med. 1997;336:924–932. [DOI] [PubMed] [Google Scholar]
- 2.Kwiatek MA, Pandolfino JE, Kahrilas PJ. 3D-high resolution manometry of the esophagogastric junction. Neurogastroenterol Motil. 2011;23:e461–e469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xiao Y, Lin Z, Li Y, et al. Correlation between novel 3D high-resolution manometry esophagogastric junction metrics and pH-metry in reflux disease patients. Neurogastroenterol Motil. 2018;30:e13344. [DOI] [PubMed] [Google Scholar]
- 4.Murray JA, Clouse RE, Conklin JL. Components of the standard oesophageal manometry. Neurogastroenterol Motil. 2003;15:591–606. [DOI] [PubMed] [Google Scholar]
- 5.Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pandolfino JE, Kim H, Ghosh SK, et al. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol. 2007;102:1056–1063. [DOI] [PubMed] [Google Scholar]
- 7.Gyawali CP, Roman S, Bredenoord AJ, et al. Classification of esophageal motor findings in gastro-esophageal reflux disease: Conclusions from an International Consensus Group. Neurogastroenterol Motil. 2017;29. [DOI] [PubMed] [Google Scholar]
- 8.Tolone S, de Cassan C, de Bortoli N, et al. Esophagogastric junction morphology is associated with a positive impedance-pH monitoring in patients with GERD. Neurogastroenterol Motil. 2015;27:1175–1182. [DOI] [PubMed] [Google Scholar]
- 9.Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am. 2014;24:527–543. [DOI] [PubMed] [Google Scholar]
- 10.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gor P, Li Y, Munigala S, et al. Interrogation of esophagogastric junction barrier function using the esophagogastric junction contractile integral: an observational cohort study. Dis Esophagus. 2016;29:820–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandolfino JE, Kahrilas PJ, American Gastroenterological A. AGA technical review on the clinical use of esophageal manometry. Gastroenterology. 2005;128:209–224. [DOI] [PubMed] [Google Scholar]
- 13.Hoshino M, Sundaram A, Mittal SK. Role of the lower esophageal sphincter on acid exposure revisited with high-resolution manometry. J Am Coll Surg. 2011;213:743–750. [DOI] [PubMed] [Google Scholar]
- 14.Nicodeme F, Pipa-Muniz M, Khanna K, et al. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil. 2014;26:353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tolone S, De Bortoli N, Marabotto E, et al. Esophagogastric junction contractility for clinical assessment in patients with GERD: a real added value? Neurogastroenterol Motil. 2015;27:1423–1431. [DOI] [PubMed] [Google Scholar]
- 16.Nicodeme F, Soper NJ, Lin Z, et al. Calculation of esophagogastric junction vector volume using three-dimensional high-resolution manometry. Dis Esophagus. 2015;28:684–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xie C, Wang J, Li Y, et al. Esophagogastric junction contractility integral reflect the anti-reflux barrier dysfunction in patients with gastroesophageal reflux disease. J Neurogastroenterol Motil. 2017;23:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang D, Patel A, Mello M, et al. Esophagogastric junction contractile integral (EGJ-CI) quantifies changes in EGJ barrier function with surgical intervention. Neurogastroenterol Motil. 2016;28:639–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ham H, Cho YK, Lee HH, et al. Esophagogastric junction contractile integral and morphology: two high-resolution manometry metrics of the anti-reflux barrier. J Gastroenterol Hepatol. 2017;32:1443–1449. [DOI] [PubMed] [Google Scholar]
- 20.Riva CG, Siboni S, Sozzi M, et al. High-resolution manometry findings after Linx procedure for gastro-esophageal reflux disease. Neurogastroenterol Motil. 2020;32:e13750. [DOI] [PubMed] [Google Scholar]
- 21.Domingues GR, Michelsohn NH, Viebig RG, et al. Normal values of esophageal high-resolution manometry: a Brazilian Multicenter Study. Arq Gastroenterol. 2020;57(2):209–215. [DOI] [PubMed] [Google Scholar]
- 22.Cock C, Besanko LK, Burgstad CM, et al. Age-related impairment of esophagogastric junction relaxation and bolus flow time. World J Gastroenterol. 2017;23:2785–2794. [DOI] [PMC free article] [PubMed] [Google Scholar]


