Abstract
Surgical attempts to remove large/giant congenital melanocytic naevi (LGCMN) are supported mainly by the theoretical improvement in patients’ self-image; however such surgery can result in unaesthetic scarring. We hypothesize that difference in appearance itself has an impact, and hence surgery cannot negate this impact. The aim of this cross-sectional study was to explore how LGCMN and scarring are perceived by non-affected people. We surveyed the visual impact on 1,015 health and non-health professionals working in a university hospital. Participants were assigned to 1 of 3 surveys, which, based on photographs of children: (i) assessed the visual impact of LGCMN; (ii) the visual impact of scarring; (iii) compared the impact of LGCMN and scarring. Feelings and perceptions evoked by images of children, either with LGCMN or with scarring, were remarkably similar. However, when the images of the same child (with LGCMN or scarring) were shown together, respondents showed significantly increased preference for scarring.
Key words: feelings, congenital melanocytic naevi, scarring, surgery, survey, visual impact
Congenital melanocytic naevi (CMN) are benign cutaneous lesions categorized by the projected adult size (PAS) of the largest lesion, where PAS 20–40 cm in diameter is “large” and PAS > 40 cm in diameter is “giant” (1). Large and giant CMN (LGCMN) are extremely rare malformations with a prevalence estimated at approximately 1 in 20,000 to 500,000 births, respectively (2). The main concerns regarding therapeutic approaches for young children are unresolved. In the past, prophylactic attempts to remove or to reduce LGCMN were based mainly on the idea that they represented a risk factor for developing melanoma as an adult (3). However, it has been observed that the lifetime risk of developing melanoma in children with LGCMN is relatively low (approximately 2–5%) (4). A prospective study suggested that surgery does not reduce the incidence of adverse clinical outcomes, such as neurological complications, and that the development of melanoma can appear even in cases of partially or completely removed LGCMN (5). A malignant transformation may occur, not only in the skin, but also in non-cutaneous sites, affecting the central nervous system (CNS), lymph nodes or subcutaneous soft tissues (4, 6, 7).
SIGNIFICANCE
Large and giant congenital melanocytic naevi are rare pigmented skin disorders involving a great body area, as a result can imply stigmatization and aesthetic impairment. Surgical attempts to remove part or most of the naevus can be proposed to reduce the affected area, but leave visible scars as well. Present study found that feelings experienced by non-affected people looking at children with large and giant congenital melanocytic naevi or scars after surgery were quite similar. However, when the images (large and giant congenital melanocytic naevi or scarring) were shown together, non-affected people reported a general preference for scarring. General population could be more familiar with scars, favoring this preference.
Nevertheless, it is well recognized that patients with visible skin conditions that alter their appearance often experience stigmatization (8, 9). Children with LGCMN are at increased risk of social, behavioural and emotional problems (10), and they often show anxious/depressed and aggressive behaviour. Thus, excision may be recommended as a treatment option during childhood. However, all therapeutic modalities to remove/reduce a LGCMN potentially carry significant morbidity and result in unaesthetic scarring, which may also affect the patient’s quality of life (QoL), appearance and self-image.
Appearance and disfigurement are areas of increasing interest for psychological research, since they have a strong effect on self-concept. Personal views of the self as acceptable/efficacious/comfortable in the world are on the basis of “socio-cultural success”. Lack of self-confidence may impact life choices, such as work, education, and personal relationships, and influence treatment by teachers, peers and caregivers (11).
While stigmatization has been studied extensively in dermatological conditions, such as psoriasis (12), there are only a few studies on the emotional impact and the psychosocial sequelae of LGCMN. One study (13) reported social problems in approximately 30% of children with LGCMN, and behavioural/emotional problems in 26%. Specifically, children with facial birthmarks experienced stigmatization, rejection and social impairment (14). A recent study concluded that children and adolescents with LGCMN experienced a significantly lower QoL and increased emotional and behavioural problems compared with community norms (15). QoL in children is a particularly complex concept (16), since childhood is a specific developmental period that differs from other periods in life.
To the best of our knowledge, no information is available on how the wider general population experiences these alterations in appearance. We hypothesize that the difference in appearance itself may have an impact, and therefore surgery cannot avoid this impact. The main goal of this study was to describe and compare the visual impact of children with LGCMN and children with scars after surgical intervention on a group of university hospital employees. A future study will compare these results with data obtained by the patients themselves and their relatives.
MATERIALS AND METHODS
This is an observational, cross-sectional study conducted between April and October 2018, approved by the research ethics committee of Hospital Clínic Barcelona (HCB2016/0522), which complies with the principles of the Declaration of Helsinki.
Participants
The study population consisted of all employees who had their official corporate email addresses included in the directories of the University of Barcelona and Hospital Clinic of Barcelona. It was composed of administrative staff, faculty members, and health professionals. Inclusion criteria were: (i) age ≥18 years; (ii) able to fully understand the study; (iii) signed electronic informed consent form; (iv) able to read and use a web-based survey interface; (v) having access to the Internet and email. Participants were not offered any financial compensation for their participation. The surveys were conducted in Spanish through a safe website (www.encuesta.com).
Data on participants
General demographic data (age, sex, ethnicity, education, marital status, having children), and personal and family history of skin conditions or cancer were recorded. Participants were also asked to complete standardized questionnaires on personal psychological aspects: the Positive and Negative Affect Schedule (PANAS) (17), which detects positive and negative affect states in clinical and normal populations, and the Socially Desirable Response Set Five-Item Survey (18), which evaluates a respondent’s tendency to give socially desirable responses (Table SI1).
Study procedures
Three different surveys were devised and presented to 3 different, randomly selected populations (Fig. S11): Survey 1 showed images of children with LGCMN on different locations (face, trunk and limbs); Survey 2 showed similar children with scars after surgery to remove LGCMN on the same 3 locations; and Survey 3 showed pairs of images of LGCMN with and without surgical intervention on the same 3 locations. A total of 13,501 email addresses of workers were randomized and assigned to 1 of the 3 surveys; 4,498 for survey 1, 4,502 for survey 2, and 4,501 for survey 3.
Assessment of visual impact of physical appearance
The tools to assess the visual impact of LGCMN consisted of photographs of children aged 3–18 years with LGCMN on 3 different areas of the body (face, trunk, limbs). Each participant in survey 1 was shown 3 pictures of children with LGCMN, 1 with localization on the face, 1 on the trunk, and 1 on the limbs. Each participant in survey 2 was shown 3 pictures of children with scarring on the same 3 localizations as in survey 1. The images of survey 3 consisted of 3 pairs of pictures showing the same children with the LGCMN and after surgery, with the same localization as in the other surveys. Examples of the assessment tool frames are shown in Fig. S21. The pictures were shown in the same order to all participants
Participants completing surveys 1 and 2 were asked about:
Reported feelings: to report what kind of feelings were experienced looking at the images, out of 15 (yes/no answer): interest, excitement, shame, fear, nervousness, amazement, curiosity, disgust, inspiration, anger, unpleasantness, happiness, pity, awe, other.
Perceived character traits: to rate on a scale from 1 to 7 how much they felt that the person in the image was honest, popular, intelligent, trustworthy, attractive, optimistic, effective, capable (these 8 traits were adapted from the Facial Disfigurement Photograph Scale) (19).
Perceived psychosocial problems: their opinion on how much the child’s skin problem had affected him/her over the previous week. The questions concerned the child’s emotions, social relationships, schooling, choice of clothes, social life, sleep, and side-effects due to treatment.
Participants completing survey 3 were asked to compare pairs of images of the same child with CMN and with scarring after surgery. They were asked:
Choice: to choose which one they preferred.
Reported feelings: to choose which of the 2 images triggered a given emotion to a greater degree (possible answers: image 1, image 2, neither). The emotions were the same 15 as those of surveys 1 and 2.
Perceived psychosocial problems: to choose in which case (LGCMN or scar) the child’s skin problem would have caused him/her a given problem.
Statistical analyses
Data were analysed using the statistical package IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp. Categorical variables were described as numbers and percentages, and continuous variables as mean and standard deviation. Differences in mean rating scores were analysed using t-tests, while percentages of positive answers to the different questions were compared using χ2 tests.
The frequency of each of the 15 reported feelings, 8 perceived character traits, and 10 perceived psychosocial problems was compared between populations 1 and 2, also in different subgroups according to socio-demographic variables, personal and family history of skin conditions or cancer, PANAS and Socially Desirable Response Set Five-Item Survey. The same comparisons were done in survey 3 between pairs of images of the same child.
All analyses were performed with 2-sided tests, and p < 0.05 was considered significant. Positive PANAS was categorized into 2 classes (<30 and ≥30), and negative PANAS into <20 and ≥20, based on the median values of the distribution.
RESULTS
Of the 13,498 invitations to participate in the study, 1,065 respondents (7.5%) agreed, 125 for survey 1, 522 for survey 2, and 418 for survey 3 answered all the questionnaires completely. For 50 participants in survey 1 demographic data were not available. The characteristics of the 3 groups of participants are described in Table I. More than half of participants were employed as healthcare providers (medical doctors, nurses and physician assistants). No significant differences were observed between populations 1 and 2 on all the variables. There were only some differences in sex and educational level in population 3 compared with 2.
Table I.
Description of the population participating in each of the 3 surveys: (1) visual impact of large/giant congenital melanocytic naevi (LGCMN); (2) visual impact of scarring; (3) comparison of the impact of LGCMN and scarring
| Total n = 1,015a | Population survey 1 n = 125 | Population survey 2 n = 522 | Population survey 3 n = 418 | |
|---|---|---|---|---|
| Age, years, mean (SD) | 41 (11.0) | 41.0 (12.3) | 41.0 (11.0) | 40.3 (10.8) |
| Range | 18–72 | 21–72 | 18–68 | 18–72 |
| Sex, n (%) | ||||
| Male | 348 (34.3) | 21 (28.0) | 162 (31.0) | 165 (39.5)* |
| Female | 667 (65.7) | 54 (72.0) | 360 (69.0) | 253 (60.5) |
| Marital status, n (%) | ||||
| Single | 271 (26.8) | 21 (22.0) | 142 (27.4) | 108 (25.8) |
| With partner | 641 (63.3) | 50 (66.7) | 327 (63.0) | 264 (63.2) |
| Separated/divorced | 93 (9.2) | 3 (4.0) | 47 (9.0) | 43 (10.3) |
| Widow/er | 7 (0.7) | 1 (1.3) | 3 (0.6) | 3 (0.7) |
| Education, n (%) | ||||
| Primary school | 5 (0.5) | 0 (0.0) | 3 (0.6) | 2 (0.5)** |
| Secondary school | 33 (3.2) | 3 (4.0) | 18 (3.4) | 12 (2.9) |
| High-school | 228 (22.5) | 17 (22.7) | 134 (25.7) | 77 (18.5) |
| Professional education, n (%) | ||||
| University | 566 (55.8) | 38 (50.6) | 289 (55.4) | 239 (57.3) |
| PhD | 182 (18.0) | 17 (22.7) | 78 (14.9) | 87 (20.9) |
| Occupation, n (%) | ||||
| No healthcare | 349 (34.9) | 27 (43.5) | 176 (35.1) | 146 (37.8) |
| Healthcare provider | 600 (65.1) | 35 (56.5) | 325 (64.9) | 240 (62.2) |
| Having children, n (%) | ||||
| Yes | 549 (45.8) | 38 (51.4) | 277 (53.2) | 234 (56.1) |
| No | 463 (54.2) | 36 (48.6) | 244 (46.8) | 183 (43.9) |
| History of personal or familial neoplasiab, n (%) | ||||
| Yes | 637 (63.6) | 53 (70.7) | 336 (64.7) | 248 (62.0) |
| No | 364 (36.4) | 22 (29.3) | 183 (35.3) | 159 (38.0) |
| Disfiguring skin conditionc, n (%) | ||||
| Yes | 133 (13.3) | 12 (16.0) | 60 (11.5) | 61 (15.0) |
| No | 870 (86.7) | 63 (84.0) | 460 (88.5) | 347 (85.0) |
Totals may vary because of missing figures.
Relative or participant her/himself with any kind of tumour/neoplasia.
Relative or participant her/himself with any kind of disfiguring skin condition.
p < 0.05 compared with population 2;
p < 0.05 compared with population 2.
Visual impact evoked by images of the large and giant congenital melanocytic naevi and of surgical scarring; surveys 1 and 2
Feelings reported looking at the images of LGCMN or scars. Both LGCMN and scarring after surgery evoked similar types of feelings (Fig. 1). The most frequent were: interest, amazement, curiosity, pity and awe. Disgust and unpleasantness were reported in particular for localization on the back and the leg. The feelings reported more frequently by participants looking at children with scarring compared with people looking at naevus were, for localization on the face: interest (p = 0.042), excitement (p = 0.042), fear (p = 0.002), amazement (p = 0.027), disgust (p = 0.042), unpleasantness (p = 0.001), pity (p < 0.001), and awe (p < 0.001). For localization on the back: interest (p = 0.003), excitement (p = 0.043), curiosity (p = 0.001), disgust (p = 0.044), pity (p = 0.039), and awe (p =0.002). For localization on the leg: interest (p = 0.002), excitement (0.042), curiosity (p = 0.004), pity (p = 0.040), and awe (p < 0.001).
Fig. 1.
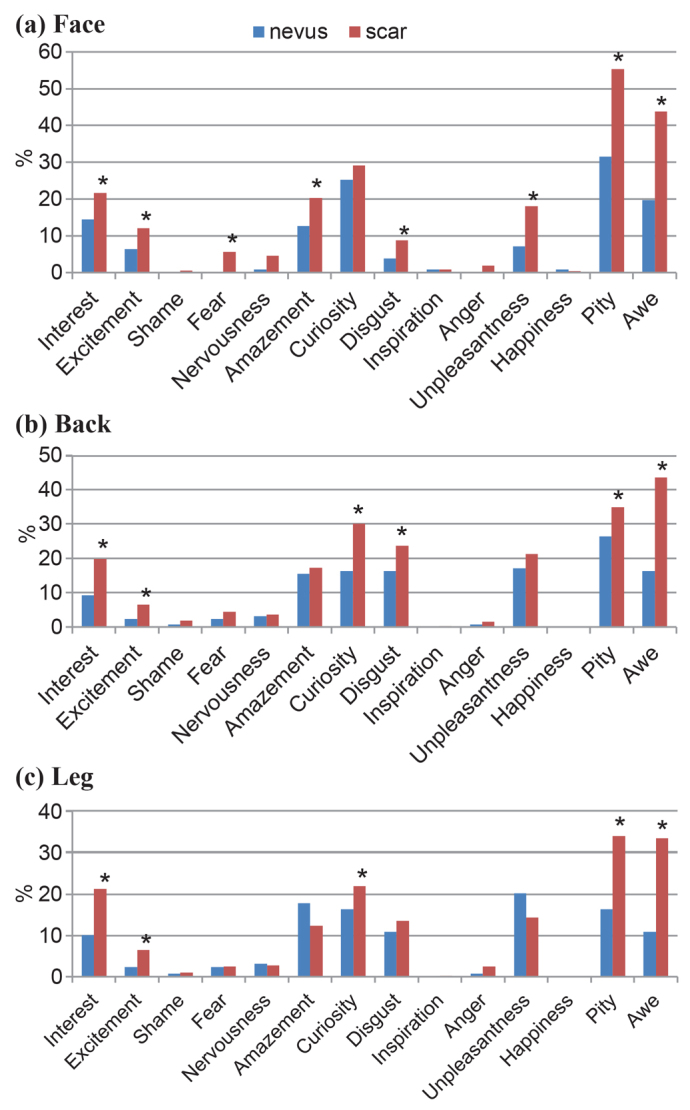
Frequency of feelings experienced by participants looking at the naevus and the scars according to location (results from survey 1 in blue and 2 in red). (a) Lesion on the face. (b) Lesion on the back. (c) Lesion on the leg. *Significant differences between surveys 1 and 2 (p < 0.05 from χ2 test).
There were no relevant differences according to the demographics of participants, socio-familiar status, disfiguring conditions, and level of social desirability.
The negative mood of participants was associated with some negative feelings. In population 2, when looking at scarring on the face 8.4% of people with negative PANAS ≥ 20 reported nervousness vs 3.4% of people with lower negative PANAS score (p = 0.035). When looking at scarring on the back, people with negative mood reported more nervousness (7.0% vs 2.5%, p = 0.034).
Perceived character traits of children with LGCMN and scars. The 2 populations reported very similar perceptions looking at naevus (population 1) or scars after interventions (population 2) (Fig. 2). Significant differences were observed only for perception of attractiveness and optimism for facial lesions, which were reported more often by population 1 (p = 0.020, p = 0.008, respectively), while more attractiveness was reported by population 2 for the back (p = 0.043) and the leg (p = 0.011). In population 1 women gave significantly higher scores than men for the perception of the child as intelligent (p = 0.030) and trustworthy (p = 0.001), for the back intelligent (p = 0.033), effective (p = 0.026), and capable (p = 0.028), and for the leg honest (p = 0.037), trustworthy (p = 0.040), and effective (p = 0.046). People in a positive mood in population 1 found children with naevus more popular (face, p = 0.003), attractive (leg, p = 0.026) and capable (back, p = 0.046) than people not in a positive mood.
Fig. 2.
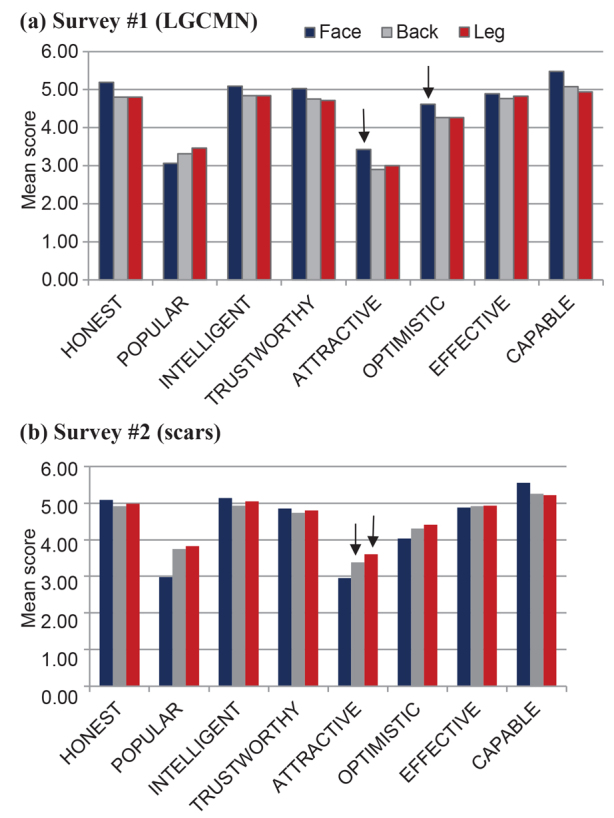
Character traits perceived by participants looking at the child with naevus (survey 1) or with scars (survey 2). Mean values on a scale from 1 “strongly disagree” to 7 “strongly agree”. (a) Survey 1 (LGCMN) (arrows indicate significantly higher values in survey 1 compared with survey 2 (p < 0.005 from t-test)). (b) Survey 2 (scars) (arrows indicate significantly higher values in survey 2 compared with survey 1 (p < 0.005 from t-test)).
Overall, no significant differences in perception of character traits were observed among participants according to age, education, marital status, having children, or having relatives with disfiguring conditions.
In population 2, for scarring on the face people with children gave a higher score to being honest (p=0.048) and popular (p =0.029), and lower scores for attractiveness for lesion on the back (p = 0.007). Significant differences were observed for age: people aged 40 years or older gave higher scores for being honest (p = 0.009), popular (p < 0.001), and intelligent (p = 0.012).
Negative mood and the Socially Desirable Scale status did not influence perception of character traits.
Visually perceived psychosocial problems. Overall, the fields in which participants perceived a high degree of impairment in the depicted children were at school, sleeping, and due to treatments (Fig. 3).
Fig. 3.
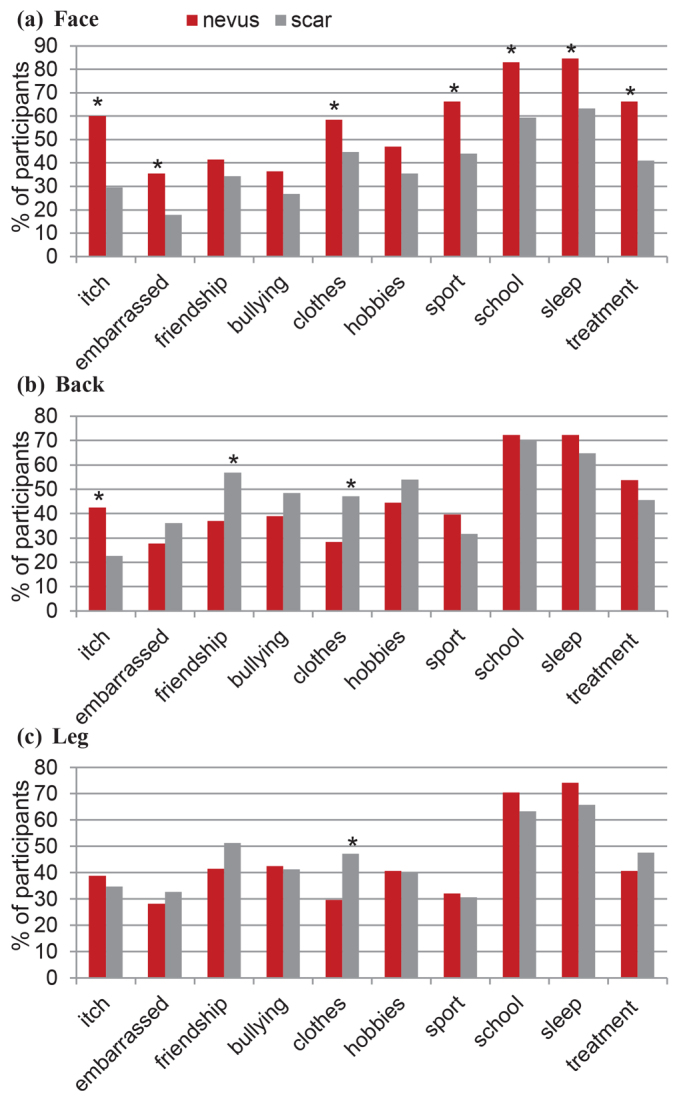
Percentage of people answering “a lot” or “very much” to questions concerning how much some problems may have affected the child with naevus (survey 1) or scars (survey 2). (a) Lesion on the face. (b) Lesion on the back. (c) Lesion on the leg. *Significant difference between survey 1 and 2 (p < 0.05 from χ2 test).
The face was the location where participants felt a higher degree of impairment, for both the presence of naevus and scarring. The proportion of impairment perceived for the face was significantly higher in survey 1 compared with survey 2, except for friendship (p = 0.160), playing/hobbies (p = 0.055), and bullying (p = 0.075).
For back location, participants looking at the scarring thought that children had significantly more problems in terms of friendship (p =0.005) and clothes (p =0.007) than a child with naevus. This was also observed for clothes in children with a lesion on the leg (p = 0.011). Itch was perceived as higher for the back in people looking at naevus (p = 0.002) than scarring.
Perceptions were not significantly influenced by demographics, familial status, disfiguring conditions or social desirable status of participants, except for a few exceptions. In population 2, participants in a less positive mood perceived more impairment in children for face in terms of itch (36.6% vs 26.3%, p = 0.037), problems with sport (51.9% vs 40.7%, p = 0.042), and for the back in friendship (65.2% vs 53.1%, p = 0.037).
Visual impact evoked comparing pairs of images of the large and giant congenital melanocytic naevi and the surgical scars on 3 different locations; survey 3
Overall, participants chose the scars as more acceptable than the naevi; 252 (74.3%) preferred the image of the child with facial scarring, compared with 87 (25.7%) who selected the naevus on the face. Concerning the back, the percentages were 94.6% and 5.4%, respectively, and for the leg 282 (96.6%) individuals preferred the scars and 10 (3.4%) the naevus.
Emotions inspired by the images. Concerning the face, the image with the naevus caused more interest (48.8% vs 31.1%), excitement (55.8% vs 27.4%), amazement (51.9% vs 18.6%), curiosity (40.6% vs 38.2%), disgust (25.3% vs 17.6%), unpleasantness (26.9% vs 17.5%), pity (48.2% vs 27.7%) and awe (64.7% vs 24.6%), always p < 0.05, compared with the image with scarring. Regarding the back and leg locations, all the emotional reactions, except inspiration, were caused more frequently by the image with the naevus than the scarring. Only happiness was reported more frequently looking at the image with scarring.
No relevant differences were observed according to demographics or social-familial status of participants.
Perceptions of the emotions and of psychosocial problems in the child. For all localizations, participants thought that the presence of the naevus would cause significantly more impairment and negative emotions than the scarring (Fig. 4).
Fig. 4.
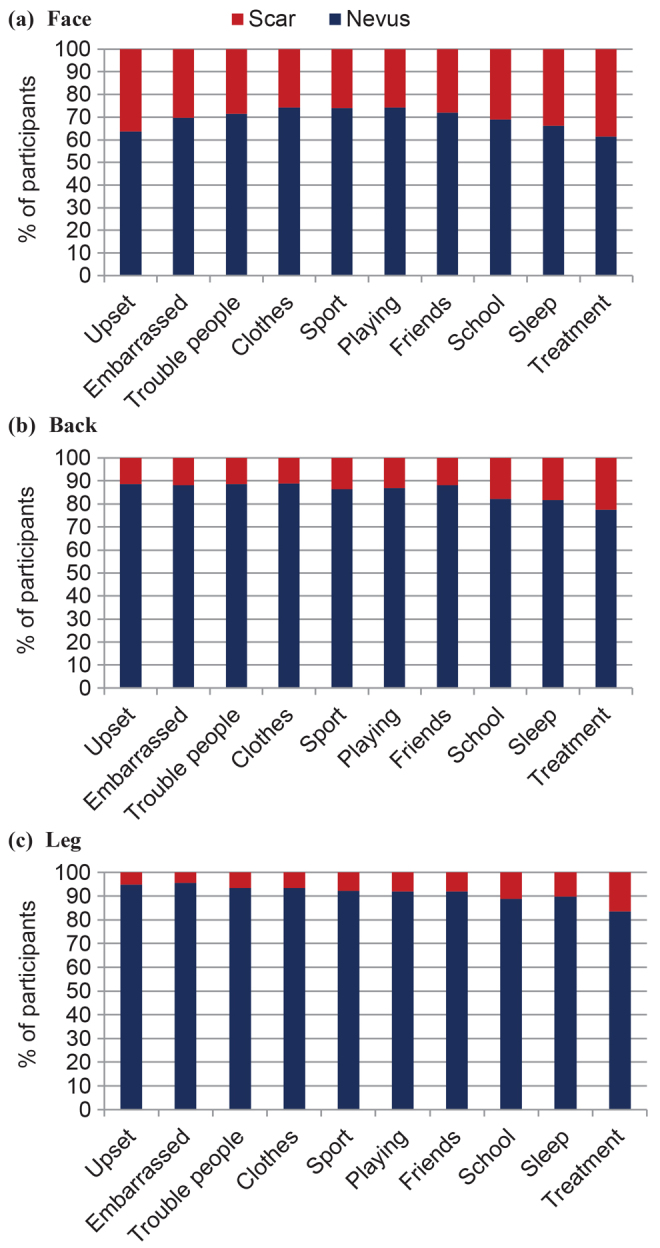
Percentage of participants perceiving that the naevus or the scar would cause a negative given emotion and psychosocial problem of the child (survey 3). (a) Lesion on the face. (b) Lesion on the back. (c) Lesion on the leg.
No relevant differences were detected according to demographics and social-familial status of participants.
DISCUSSION
This study is the first to investigate the visual impact of LGCMN and scarring secondary to surgical excision, on more than 1,000 individuals from a population of health and non-health professionals working in a university hospital.
There is no question that the perception of the individual with a large naevus or scar is of primary importance. Unfortunately, parents faced with the decision of subjecting their child with a large naevus to clinical monitoring vs prophylactic excision will only know the answer to the above in hindsight once their child is old enough to be able to voice an opinion. Clearly, this is not acceptable and parents are left with the burden of deciding between prophylactic excision vs observation. While progress has been made in addressing the risk of melanoma forming in large naevi, the psychological aspects surrounding this issue have not been adequately addressed. With this end there are 2 major questions that parents often ask clinicians: (i) What will my child feel about the naevus vs the scar when they grow up? This has been addressed in a small study by Koot et al. (10). In two-thirds of cases the doctors, patients and family agreed on the degree of satisfaction with the result of treatment. The children themselves were of the opinion that having a burn-like scar was far more socially acceptable than having a naevus. However, it is important to emphasize that, in 25% of cases, the result of the treatment was unsatisfactory. Clearly, more work is required to better understand the factors leading to each individual’s perception about their naevus or scar, but this study at least provides parents with some insights into this issue. (ii) What is the public’s perception of my child’s naevus? The impetus of the current study was to provide data to address this question. The fact that the perceptions and feelings evoked by employees at a university hospital were similar for the scar and the naevus when each scenario was shown separately is very informative, and is likely to provide comfort to parents in whatever decision they make for their child.
In addition, this information helps to focus attention away from aesthetics concerns and redirects the focus towards addressing the risk of developing melanoma and the decision as to whether an absolute risk of between 2% and 3% for developing cutaneous melanoma warrants prophylactic excision.
This study observed that the population’s feelings and perceptions evoked by images of children with LGCMN and scarring were remarkably similar, when only one of the 2 images was shown to the participants.
Nevertheless, when the images of the same child (with LGCMN or scarring) were shown together, the general population reported a general preference for scarring compared with LGCMN. Moreover, children with scarring caused less negative feelings and less perceived impairment of QoL compared with children with LGCMN.
The difference in the results may be explained by the fact that when the 2 images are presented together, the naevus appears more disfiguring than the scarring. When there is no basis for comparison, scarring is seen as particularly disfiguring and causing a great impact on the child’s QoL, similar to the presence of a LGCMN.
The most frequent feelings chosen by the 2 populations looking at the child with LGCMN and with scarring were interest, amazement, curiosity, pity and awe. Therefore, participants seemed to show empathy towards the child, since they rarely reported negative feelings, such as disgust, unpleasantness, shame or fear. Participants experienced the same feelings, regardless of their sex, age, social and familial status, including those having a close relative with a tumour or disfiguring condition. Also, feelings were not influenced by positive or negative mood, with some exceptions, such as an association between negative mood and negative feelings, when looking at scarring.
Concerning the location of LGCMN, a slightly higher visual impact of facial lesions was observed compared with lesions on other parts of the body. This is consistent with other studies concerning the impact on self-esteem of visible scars (20). It has been observed that the emotional burden of disfigurement affecting the head and neck is higher than in any other locations, probably due to the impact on social interaction and self-identity.
Previous studies have shown that many parents preferred scars to a LGCMN and agreed that surgery for those lesions was worthwhile, especially for those located on the head and neck (5, 21). However, it has to be considered that the surgical removal of a LGCMN generally requires multiple interventions, and therefore is not free from risks and sequelae. In most cases, patients must undergo a long reconstruction process that involves different hospital admissions and school absenteeism. Also, invasive treatments may result in undesirable aesthetic outcomes (11). Both the treatments that can be offered and the condition itself may radically affect the QoL of the patient, altering their life trajectory and dignity (22).
The use of photographs with no additional information to investigate the participants’ perception could be a limitation. However, visual methods, such as photographs, are frequently used in research to investigate the perceptions of third parties regarding others’ appearance. Looking at the facial image of a child, the observer can provide an educated guess concerning how much the disfigurement would affect the child’s relationships, self-esteem, and acceptance by their peer-group (14, 22, 23).
The current study has some limitations; firstly, despite having more than 1,000 responders, the results cannot be generalized, since half of the participants were healthcare providers with a high educational level. Indeed, we could assume that health professionals are expected to be more used to post-surgical sequelae than to images of children affected by LGCMN, which is a completely unknown condition for most of them. In addition, it is surprising that the participation rate of survey 1 was lower than that of surveys 2 and 3.The reason for this is unknown, but there could have been a technical issue with the mass emailing, as each survey was sent to more than 4,500 addresses. However, it is important to observe that the 3 populations were highly comparable in terms of demographic and personal features, and, thus, differences in results cannot be attributed to differences in the participants’ characteristics.
In conclusion, the feelings experienced by the non-affected people looking at children with LGCMN or scars were quite similar, independent of surgical attempts to reduce the LGCMN. The opinion of society should not influence the choice of whether a person has surgery. However, the aim of the current study was to explore from a psychosocial point of view the impact of birthmarks and surgery in the general population. The fact that respondents preferred the scar over the naevus when the images were shown side-by-side requires further study, but it probably has more to do with broader societal issues of humans being more comfortable with the familiar (scars) compared with the unfamiliar (large naevi). This latter finding should in no way be taken as an endorsement that scars are “better” than naevi, nor should it distract from the primary message, that there was no difference between the respondents’ answers to the survey regarding the naevus or the scar when each scenario was shown independently. Further studies about the impact of LGCMN and sequelae of surgery on both patients and caregivers will be analysed and compared with the data from the current report.
ACKNOWLEDGEMENTS
The authors are grateful to Paul Hetherington, PhD, for his English editing. We also thank all volunteers who completed and answered the surveys.
This research at the Melanoma Group IDIBAPS – Hospital Clinic of Barcelona was funded mainly by Instituto de Salud Carlos III (ISCIII) through the project PI18/0959 and co-funded by European Regional Development Fund ”A way to make Europe” from the European Union, and by the Centro de Investigación Biomédica en Red de Enfermedades Raras (CIBERER), Spain, and by the Leo Messi Foundation, Barcelona, Spain. Dr Cristina Carrera had a personal grant “Pla estratègic de recerca i innovació en salut 20182020 (ref. BDNS 357800) PERIS” from the Health Department of the Catalan Government (SLT006/17/00296). Neus Calbet-Llopart is the recipient of a PhD Fellowship FPU17/05453 (FPU) from Ministerio de Educación, Cultura y Deportes, Spain. The sponsors had no role in the design and conduct of the study, in the collection, analysis, and interpretation of data, or in the preparation, review, or approval of the manuscript.
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Krengel, S, Scope A, Dusza SW, Vonthein R, Marghoob AA. New recommendations for the categorization of cutaneous features of congenital melanocytic nevi. J Am Acad Dermatol 2013; 68: 441–451. [DOI] [PubMed] [Google Scholar]
- 2.Alikhan A, Ibrahimi OA, Eisen DB. Congenital melanocytic nevi: where are we now? Part I. Clinical presentation, epidemiology, pathogenesis, histology, malignant transformation, and neurocutaneous melanosis. J Am Acad Dermatol 2012; 67: 495.e1-17. [DOI] [PubMed] [Google Scholar]
- 3.Slutsky JB, Barr JM, Femia AN, Marghoob AA. Large congenital melanocytic nevi: associated risks and management considerations. Semin Cutan Med Surg 2010; 29: 79–84. [DOI] [PubMed] [Google Scholar]
- 4.Kinsler VA, O’Hare P, Bulstrode N, Calonje JE, Chong WK, Hargrave D, et al. Melanoma in congenital melanocytic naevi. Br J Dermatol 2017; 176: 1131–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kinsler VA, Birley J, Atherton DJ. Great Ormond Street Hospital for Children Registry for congenital melanocytic naevi: prospective study 1988–2007. Part 1-epidemiology, phenotype and outcomes. Br J Dermatol 2009; 160: 143–150. [DOI] [PubMed] [Google Scholar]
- 6.Bittencourt FV, Marghoob AA, Kopf AW, Koenig KL, Bart RS. Large congenital melanocytic nevi and the risk for development of malignant melanoma and neurocutaneous melanocytosis. Pediatrics 2000; 106: 736–741. [DOI] [PubMed] [Google Scholar]
- 7.Lacoste C, Avril MF, Frassati-Biaggi A, Dupin N, Chrétien-Marquet B, Mahé E, et al. Malignant melanoma arising in patients with a large congenital melanocytic naevus: retrospective study of 10 cases with cytogenetic analysis. Acta Derm Venereol 2015; 95: 686–690. [DOI] [PubMed] [Google Scholar]
- 8.Dimitrov D, Szepietowski JC. Stigmatization in dermatology with a special focus on psoriatic patients. Postepy Hig Med Dosw 2017; 71: 1115–1122. [DOI] [PubMed] [Google Scholar]
- 9.Wu JH, Cohen BA. The stigma of skin disease. Curr Opin Pediatr 2019; 31: 509–514. [DOI] [PubMed] [Google Scholar]
- 10.Koot HM, de Waard-van der Spek F, Peer CD, Mulder PG, Oranje AP. Psychosocial sequelae in 29 children with giant congenital melanocytic naevi. Clin Exp Dermatol 2000; 25: 589–593. [DOI] [PubMed] [Google Scholar]
- 11.Vivar KL, Kruse L. The impact of pediatric skin disease on self-esteem. Int J Womens Dermatol 2017; 4: 27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ginsburg IH, Link BG. Psychosocial consequences of rejection and stigma feelings in psoriasis patients. Int J Dermatol 1993; 32: 587–591. [DOI] [PubMed] [Google Scholar]
- 13.Koot HM, de Waard-van der Spek F, Peer CD, Mulder PG, Oranje AP. Psychosocial sequelae in 29 children with giant congenital melanocytic naevi. Clin Exp Dermatol 2000; 25: 589–593. [DOI] [PubMed] [Google Scholar]
- 14.Masnari O, Schiestl C, Rössler J, Gütlein SK, Neuhaus K, Weibel L, et al. Stigmatization predicts psychological adjustment and quality of life in children and adolescents with a facial difference. J Pediatr Psychol 2013; 38: 162–172. [DOI] [PubMed] [Google Scholar]
- 15.Masnari O, Neuhaus K, Aegerter T, Reynolds S, Schiestl CM, Landolt MA. Predictors of health-related quality of life and psychological adjustment in children and adolescents with congenital melanocytic nevi: analysis of parent reports. J Pediatr Psychol 2019; 44: 714–725. [DOI] [PubMed] [Google Scholar]
- 16.Wallander JL, Koot HM. Quality of life in children: a critical examination of concepts, approaches, issues, and future directions. Clin Psychol Rev 2016; 45: 131–143. [DOI] [PubMed] [Google Scholar]
- 17.Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol 2004; 43: 245–265. [DOI] [PubMed] [Google Scholar]
- 18.Holtgraves T. Social desirability and self-reports: testing models of socially desirable responding. Pers Soc Psychol Bull 2004; 30: 161–172. [DOI] [PubMed] [Google Scholar]
- 19.Gardiner MD, Topps A, Richardson G, Sacker A, Clarke A, Butler PE. Differential judgements about disfigurement: the role of location, age and gender in decisions made by observers. J Plast Reconstr Aesthet Surg 2010; 63: 73–77. [DOI] [PubMed] [Google Scholar]
- 20.Sobanko JF, Sarwer DB, Zvargulis Z, Miller CJ. Importance of physical appearance in patients with skin cancer. Dermatol Surg 2015; 41: 183–188. [DOI] [PubMed] [Google Scholar]
- 21.Bellier-Waast F, Perrot P, Duteille F, Stalder JF, Barbarot S, Pannier M. Prise en charge chirurgicale des naevi géants congénitaux: quel retentissement psychosocial sur l’enfant et son entourage? Ann Chir Plast Esthet 2008; 53: 408–414. [DOI] [PubMed] [Google Scholar]
- 22.Masnari O, Landolt MA, Roessler J, Weingaertner SK, Neuhaus K, Meuli M, et al. Self- and parent-perceived stigmatisation in children and adolescents with congenital or acquired facial differences. J Plast Reconstr Aesthet Surg 2012; 65: 1664–1670. [DOI] [PubMed] [Google Scholar]
- 23.Harcourt D, Hamlet C, Feragen KB, et al. The provision of specialist psychosocial support for people with visible differences: a European survey. Body Image 2018; 25: 35–39. [DOI] [PubMed] [Google Scholar]


