Abstract
Background
End-of-life care practices in long-term care facilities (LTCFs) are the focus of growing attention in Europe, due to rapidly increasing number of older persons living in LTCFs. The knowledge about end-of-life discussions or existence of written advance directives in the European LTCFs is scarce. This study’s aim is to investigate the prevalence of written advance directives and their sociodemographic associates, among recently deceased LTCF residents, in six European countries.
Methods
Data from the European Union-funded PACE database were collected from 322 LTCFs in six European countries in 2014. The assessments were performed by using two questionnaires designed for LTCF administrative staff and for staff member.
LTCFs were selected within each country by using proportional stratified random sampling procedure. Facilities with certain types and sizes were included from each country.
Multilevel multivariate analyses were performed to evaluate associations between written advance directives and selected predictors.
Results
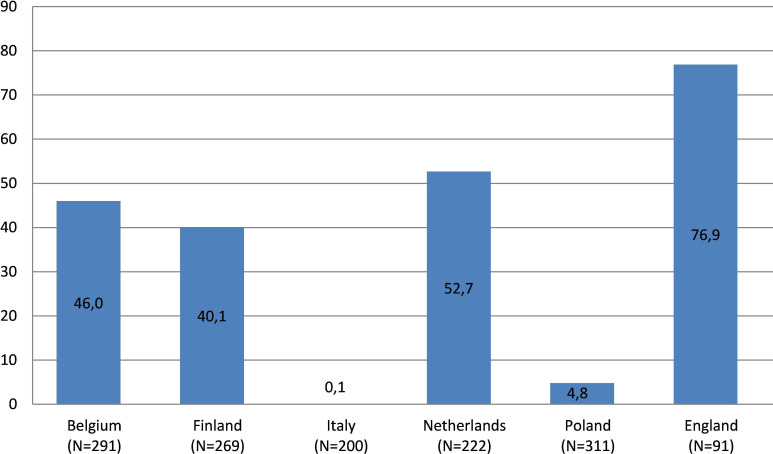
In total, 32.5 % of the 1384 deceased LTCF residents had a written advance directive with a range from 0% to 77 % between countries. The proportion of the most common advance directive, ‘Do not resuscitate in case of cardiac or respiratory arrest (DNR)’, varied correspondingly from 0% to 75%.
LTCF type (OR 2.86 95% CI 1.59 to 5.23) and capability of expressing at the time of admission (OR 3.26 95% CI 2.26 to 4.71) were the independent predictors for advance directive. Residents living in LTCFs where physician was available were less likely to have advance directive compared with residents from LTCFs where physician was not available.
Conclusion
Extensive differences for prevalence of written advance directive exist between countries among older LTCF residents in Europe. Timely and appropriate response to LTCF resident’s health needs and preferences efforts advance care planning.
Keywords: advance directives, living wills, long-term care, palliative care, hospice and palliative care nursing
Introduction
End-of-life care practices in long-term care facilities (LTCFs) are the focus of growing attention in Europe, due to rapidly increasing number of older persons. A written advance directive (AD), such as a living will, is in many countries a legal document to provide guidance for medical and healthcare decisions in the event that a person loses his or her ability to make such decisions.1 Advance care planning (ACP), where ADs are considered, is an important part prior to the decisions.2 Earlier scientific evidence has shown that ADs have a positive impact on the quality of end-of-life care among older persons.3–6
ADs are statements of wishes and preferences which may be oral or written. Often they include declining treatment options such as, ‘do not attempt cardiopulmonary resuscitation (DNR-order)’, ‘do not hospitalise (DNH-order)’ or ‘no blood transfusions’. ADs could also include a wish for the medical team to make all efforts to sustain life. Depending on cultural context, some of the preferences such as euthanasia may or may not be discussed.3 4 7
Efforts to define and standardise ACP have been promoted by a Delphi study which proposed an international definition (2017) supported by European Association for Palliative Care:
Advance care planning enables individuals who have decisional capacity to identify their values, to reflect upon the meanings and consequences of serious illness scenarios, to define goals and preferences for future medical treatment and care, and to discuss these with family and health-care providers. ACP addresses individuals’ concerns across the physical, psychological, social, and spiritual domains. It encourages individuals to identify a personal representative and to record and regularly review any preferences, so that their preferences can be taken into account should they, at some point, be unable to make their own decisions.6
Prevalence of completed ADs in the general population varies within and across countries, due to varying concepts and legislations and according to the population investigated.8–11 In a national sample from Belgium, the oldest age group showed a higher prevalence of AD (12%) than the younger age groups.12 In the Netherlands, those 60 years of age or older AD prevalence was 10%.13
The proportion of LTCF residents with ADs is known to vary by country. However, knowledge about existence of ADs in the European LTCFs is scarce. Contents of ADs have been investigated earlier in European studies, but the definition for ACP in these studies has varied extensively. Until recently, prevalence of ACP among older persons has only been explored in some European countries. According to a recently performed systematic review on palliative care studies, scientific evidence about effective ACP documentation and communication on older person’s end-of-life care wishes and preferences with healthcare professionals has been insufficient.14 There is an explicit need for population-based scientific analysis on ACP and AD among LTCF residents.3 8 15
In this article, we aimed to investigate the prevalence of ADs and their association of sociodemographic variables, among recently deceased LTCF residents, in six European countries. This will draw on data from a larger European Union-funded study, called Palliative care for older persons living in care and nursing homes in Europe (PACE).
Methods
Study design
The PACE study involved a cross-sectional and retrospective design using a large-scale survey to examine end-of-life care among LTCF residents in six European countries (Belgium, Finland, the Netherlands, Italy, Poland and United Kingdom). With its extensive study population of 1384 older LTCF residents, PACE is the largest cross-sectional study of older person’s palliative care in Europe. Detailed information about the study design and procedure has been published previously.16 LTCFs were grouped into three categories according to the level and availability of healthcare professionals. Type 1 LTCFs had physicians and nursing staff with care assistants available in the facility 24 hours a day and 7 days a week. In type 2 LTCF, nursing staff with care assistants were available 24 hours a day and 7 days a week in the facility, and physicians available offsite. In type 3 LTCF, care assistants were available 24/7 in the facility and nurses and physicians available offsite. There was a nurse available 24 hours a day in most of the participating LTCFs.
The researchers in all countries visited each facility and delivered information for the data collection. Data were collected during 2015 from the residents who had died not more than 3 months prior to the researcher’s visit. The questionnaires were translated into each country’s language via forward–backward translation procedures and they were tested in advance and final modifications were added to them. Two reminders to complete the questionnaires were sent after the first-round deadline. More detailed information about the study protocol has been published previously.16
Sampling
LTCFs were selected within each country by using proportional stratified random sampling procedure. For the representative sample, facilities with certain types and sizes were included from each country. Participant LTCFs were selected from different strata based on national or regional register. In the United Kingdom, a national LTCF research support network was used to increase the number of participants. In Italy, a convenience sample of a cluster of LTCFs interested in research from three areas where the largest number of population lives was used as strata.
In the facilities, staff nurses were responding to the questionnaires regarding deceased resident’s end of life. Each facility had one contact person from the administrative staff who responded to the questionnaire regarding the care home.
Data collection
The contact persons in the care homes delivered the questionnaires regarding deceased resident’s end of life to the staff nurses. Moreover, the contact persons received personal guidance in filling in the questionnaire from a researcher. The staff members (preferably nurses), who completed the questionnaire, were chosen among staff by the contact person based on how well the staff nurse had known the deceased resident. The responding staff nurses were allowed to look in the resident’s case notes to help them recall any ADs.
A questionnaire for LTCF administrative staff and a questionnaire for the staff member most closely involved in the care for the resident were used to collect the data for the current study.
The questionnaire for LTCFs administrative staff included questions about the resident’s age, gender and the organisational type of the resident’s LTCF. The questionnaire for staff member contained questions about resident’s health status before death and his or her end-of-life care from the staff member’s perspective. The questionnaire items regarding resident’s health status were presented using structured answering categories or yes–no alternatives. Staff members in all the participating countries were asked about the resident’s ADs.
To investigate the presence of ADs, the questionnaire for staff members asked:
‘Did the resident have a written living will with regard to the following requests?’. The options that were then presented differed per country as these are linked to the different regulations on end-of-life options in the different countries. In all countries, the options included: ‘Do not resuscitate in case of cardiac or respiratory arrest (DNR)’, ‘Do not transfer to a hospital (DNH)’, ‘Discontinue or do not use other treatments (please specify)’, ‘Request to try all life prolonging measures’ and ‘None of the above’. In Belgium and the Netherlands, euthanasia was added as an option, and in Belgium, terminal sedation was also added as an option. In the questionnaire, there was an open space for free answer where the respondents could add text according to their own considerations about other personal statements that were not listed in the questionnaire (see online supplementary annex 1).
bmjspcare-2018-001743supp001.pdf (77.4KB, pdf)
A question about resident’s surrogate decision-maker was formulated as: ‘Did a resident, in prior living will, give a power to a third party to take decisions for him or her in case he or she would be no longer competent to do so?’
Statistical methods
For the current analysis, a variable ‘Written advance directive (yes/no)’ was created from all the individual different variables included under the concept of living will. Postmortem directives were removed. Total number of the deceased residents by country is presented in the baseline characteristics (table 1.) Missing values and the returned questionnaires, in which the particular question about written living will was not answered, are included in the table 1 but they are removed from further statistical analysis. The predictors of written ADs were examined with multilevel univariate and multivariate analyses with facility as the random intercept. All analyses were performed using SAS 9.3 statistical software (2002–2010 by SAS Institute, Cary, North Carolina, USA).
Table 1.
Sociodemographic characteristics of the samples by country
| Belgium | Finland | Italy | The Netherlands | Poland | England | |||||||
| N=291 | N=269 | N=200 | N=222 | N=311 | N=91 | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Type of LTC facility | ||||||||||||
| LTC onsite day and night physicians and nurses | na | na | 0 | 0 | 48 | 25.4 | 117 | 55.5 | 184 | 59.2 | 0 | 0 |
| LTC onsite nurses offsite GPs | 276 | 100 | 267 | 100 | 141 | 74.6 | 94 | 44.6 | 127 | 40.8 | 49 | 53.9 |
| LTC offsite nurses and GPs | na | na | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 42 | 46.2 |
| Not available | 15 | 2 | 11 | 11 | 0 | 0 | ||||||
| Age at death (years) | ||||||||||||
| 35–80 | 41 | 15 | 57 | 21.4 | 46 | 23 | 41 | 20.4 | 117 | 38 | 14 | 17.7 |
| 81–89 | 121 | 44.2 | 127 | 47.6 | 91 | 45.5 | 83 | 41.3 | 126 | 40.9 | 30 | 38 |
| 90–112 | 112 | 40.9 | 83 | 31.1 | 63 | 31.5 | 77 | 38.3 | 65 | 21.1 | 35 | 44.3 |
| Not available | 17 | 2 | 0 | 21 | 3 | 12 | ||||||
| Sex | ||||||||||||
| Male | 98 | 36 | 94 | 35.7 | 63 | 31.7 | 68 | 33 | 112 | 36.5 | 22 | 25 |
| Female | 174 | 64 | 169 | 64.3 | 136 | 68.3 | 138 | 67 | 195 | 63.5 | 66 | 75 |
| Not available | 19 | 6.5 | 6 | 1 | 16 | 4 | 3 | |||||
| Married or civil partnership, or in a long-term relationship | 64 | 22.0 | 62 | 23.0 | 50 | 25.0 | 54 | 24.3 | 44 | 14.1 | 19 | 20.9 |
| Divorced | 4 | 1.4 | 7 | 2.6 | 8 | 4.0 | 3 | 1.4 | 25 | 8.0 | 5 | 5.5 |
| Widowed | 182 | 62.5 | 135 | 50.2 | 106 | 53.0 | 112 | 50.5 | 163 | 52.4 | 50 | 54.9 |
| Never married | 20 | 6.9 | 33 | 12.3 | 31 | 15.5 | 18 | 8.1 | 40 | 12.9 | 9 | 9.9 |
| Unknown or not answered | 21 | 7.2 | 32 | 11.9 | 5 | 2.5 | 35 | 15.8 | 39 | 12.5 | 8 | 8.8 |
| The resident’s capacity of expressing his or her wishes at the time of admission* | ||||||||||||
| Yes or partly | 223 | 78 | 198 | 75 | 91 | 45.7 | 181 | 82.3 | 167 | 54.9 | 73 | 81.1 |
| No | 63 | 22 | 66 | 25 | 108 | 54.3 | 39 | 17.7 | 137 | 45.1 | 17 | 18.9 |
| Not available | 5 | 5 | 1 | 2 | 7 | 1 | ||||||
*Judgement of the staff members.
†
GPs, general practitioners; LTC, long-term care; na, not answered.
Results
Altogether 1707 deceased residents in 322 LTCFs were identified and nursing staff questionnaires were returned for 1384 residents. Response rate was 81.4% for staff member’s questionnaires being highest in Finland with 95.1% and lowest in England with 54.2%.
LTCFs of 302 were included in the current analysis. The sample from Belgium comprised 45 LTCFs with a range of 1–18 deceased residents per facility. The corresponding figures for Finland were 90 and 1–14, for Italy 32 and 1–28, for the Netherlands 46 and 1–32, for Poland 48 and 1–31 and for England 41 and 1–10. Of the nurse’s questionnaires regarding the deceased resident, the question about resident’s written living will and different options included in this concept were not completed for 76 deceased residents.
Characteristics of the study population
Table 1 shows that older age and predominantly female gender of the deceased residents were common in the study population. The age distribution of the residents was otherwise fairly similar across countries except for Poland, where deceased residents were substantially younger than in other countries. Two in three residents (69%) were estimated to have possessed the capacity for decision-making at the time of admission to the LTCF, least often in Italy or Poland and most often in the Netherlands and England.
Incidence of written AD
In total, one in three of the deceased residents (32.5%) had written AD with a range from 0% to 77% from country to country. Figure 1 shows variation of presence of any written AD between countries from staff member’s view.
Figure 1.
Any written advance directive by country, all residents (n=1384 individuals), %, in 2014.
Different types of ADs
The proportion of the most common AD, DNR, varied from 0% to 75%. Table 2 shows a similar cross-national variation in all the other measured AD items.
Table 2.
Preferences of LTCF residents for written advance directives by country in 2014
| Belgium (N=291) | Finland (N=269) | Italy (N=200) | The Netherlands (N=222) | Poland (N=311) | United Kingdom (N=91) | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| One or more advance directive | 134 | 46.0 | 108 | 40.1 | 1 | 0.1 | 117 | 52.7 | 15 | 4.8 | 70 | 76.9 |
| expressed in the living will | ||||||||||||
| Do not attempt cardiopulmonary resuscitation | 121 | 41.6 | 98 | 36.4 | 0 | 0.0 | 103 | 46.4 | 2 | 0.6 | 69 | 75.8 |
| Do not hospitalise | 96 | 33.0 | 21 | 7.8 | 1 | 0.1 | 0 | 0.0 | 6 | 1.9 | 18 | 19.8 |
| Request to try all life prolonging | 6 | 2.1 | 5 | 1.9 | 0 | 0.0 | 2 | 0.9 | 7 | 2.3 | 0 | 0.0 |
| measures | ||||||||||||
| Palliative/terminal sedation | 15 | 5.2 | NA | NA | NA | NA | NA | |||||
| Wish for euthanasia | 10 | 3.4 | NA | NA | 11 | 5.0 | NA | NA | ||||
| Treatments not used or | 0 | 0.0 | 13 | 4.8 | 0 | 0.0 | 12 | 5.4 | 0 | 0.0 | 0 | 0.0 |
| discontinued | ||||||||||||
| Other personal statement | 28 | 9.6 | 10 | 3.7 | 0 | 0.0 | 6 | 2.7 | 2 | 0.6 | 2 | 2.2 |
| Resident's preferences | 16 | 5.5 | 11 | 4.1 | 9 | 4.5 | 10 | 0.5 | 24 | 7.7 | 6 | 6.6 |
| not filled in | ||||||||||||
| Surrogate decision-maker appointed by the resident | 94 | 32.3 | 86 | 32.0 | 30 | 15.0 | NA | 103 | 33.4 | 52 | 57.1 | |
LTCF, long-term care facility; NA, not answered, question not asked.
‘Palliative sedation’ was a country-specific answer option for Belgium, and 5.2% of the Belgian LTCF residents had signed it in their written living will. Euthanasia was another country-specific option included in questionnaires in Belgium and in the Netherlands and 3.4% of the Belgian and 5.0% of the Dutch LTCF residents had chosen it in their written living wills. However, one resident in Finland had also mentioned it in their AD. The item ‘discontinue the use of or do not use of other treatments’ was answered in Finland (4.8%) and in the Netherlands (5.4 %) (table 2).
A number of other directives were reported in the free answers. They included restrictions in initiating chemotherapy (n=11), radiation therapy (n=4), tube feeding or other artificial nutrition (n=11), antibiotics (n=4) or any life-sustaining procedures, including liquids (n=9). Some statements defined the types of care desired such as (n=3), wish for adequate pain relief was stated by three and comfort care by four residents.
Sociodemographic and other factors and their association with ADs
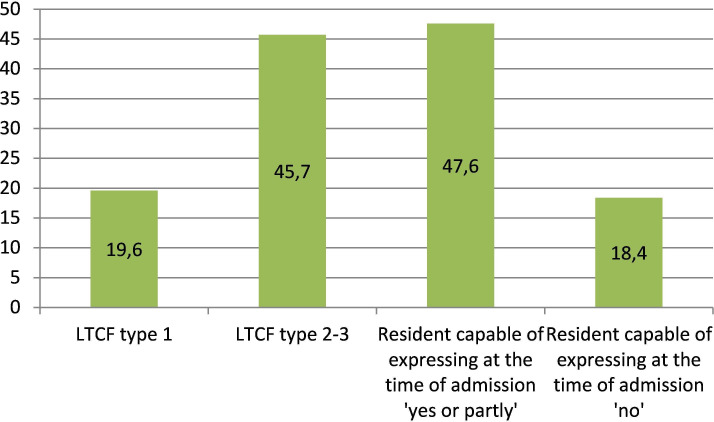
Table 3 shows bivariate associations between one or more written preferences of the resident and sociodemographic factors. The oldest residents and those who were widows were significantly associated with the existence of a written directive. The younger the resident, the less was the likelihood for a written AD. In the multivariate multilevel analyses presented in table 4, LTCF type (OR 2.86, 95% CI 1.59 to 5.23) and capability of expressing at the time of admission (OR 3.26, 95% CI 2.26 to 4.71) were the independent predictors for written AD. These variables and their subcategories are presented as percentages for all the study population in figure 2.
Table 3.
Selected sociodemographic variables and written advance directive in 2014.
| Univariate multilevel analysis: Belgium, Finland, the Netherlands, Poland and the United Kingdom combined. All analyses adjusted by country. Facility as random intercept | ||||||
| Variable | n (%) | Directive exists | P value | OR | 95% Confidence limits | |
| n | % | |||||
| Country | ||||||
| Belgium | 275 (24.6) | 134 | 48.7 | ref | 1 | |
| Finland | 258 (23.1) | 108 | 41.9 | 0.124 | 0.73 | 0.49 to 1.09 |
| The Netherlands | 212 (19.0) | 117 | 55.2 | 0.340 | 1.24 | 0.80 to 1.91 |
| Poland | 287 (25.7) | 14 | 4.9 | <0.001 | 0.05 | 0.03 to 0.10 |
| United Kingdom | 85 (7.6) | 70 | 82.4 | <0.001 | 4.72 | 2.45 to 9.07 |
| Age ≤80 | 291 (23.1) | 70 | 24.1 | ref | 1 | |
| Age 81–89 | 552 (43.8) | 177 | 31.1 | 0.781 | 1.06 | 0.71 to 1.58 |
| Age ≥90 | 416 (33.0) | 170 | 40.8 | 0.136 | 1.37 | 0.91 to 2.07 |
| Sex: male | 428 (33.9) | 132 | 30.8 | ref | 1 | |
| Sex: female | 835 (66.1) | 293 | 35.1 | 0.086 | 1.30 | 0.96 to 1.76 |
| Marital status: married or in a long-term relationship | 270 (21.6) | 89 | 33.0 | ref | 1 | |
| Marital status: never married | 50 (4.0) | 11 | 22.0 | 0.864 | 1.09 | 0.42 to 2.78 |
| Marital status: widowed | 720 (57.5) | 268 | 37.2 | 0.037 | 1.46 | 1.02 |
| Marital status: divorced | 142 (11.3) | 31 | 21.8 | 0.231 | 0.71 | 0.40 |
| Marital status: unknown | 70 (5.6) | 17 | 24.3 | 0.781 | 1.11 | 0.52 |
| Type of LTCF=1 | 276 (25.3) | 54 | 19.6 | ref | 1 | |
| Type of LTCF=2–3 | 814 (74.7) | 372 | 45.7 | <0.001 | 2.86 | 1.59 |
| Resident capable of expressing at admission | ||||||
| Yes or partly | 305 (27.5) | 383 | 47.6 | <0.001 | 3.26 | 2.26 |
| No | 804 (72.5) | 56 | 18.4 | ref | 1 | |
LTCF, long-term care facility.
Table 4.
Any written advance directive and sociodemographic variables in 2014. Results of multivariate multilevel analysis
| Multivariate multilevel analysis: Belgium, Finland, the Netherlands, Poland and the United Kingdom combined. Country adjusted. Facility as random intercept | ||||
| Variable | P value | OR | 95% Confidence limits | Overall p value |
| Country | ||||
| Belgium | ref | 1 | <0.001 | |
| Finland | 0.284 | 0.79 | 0.51 to 1.22 | |
| The Netherlands | 0.018 | 2.04 | 1.13 to 3.70 | |
| Poland | <0.001 | 0.09 | 0.04 to 0.19 | |
| United Kingdom | <0.001 | 4.22 | 2.13 to 8.37 | |
| Age ≤80 | ref | 1 | 0.635 | |
| Age 81–89 | 0.425 | 0.83 | 0.53 to 1.31 | |
| Age ≥90 | 0.832 | 0.95 | 0.59 to 1.53 | |
| Sex: male | ref | 1 | 0.236 | |
| Sex: female | 0.236 | 1.23 | 0.87 to 1.75 | |
| Marital status: married or in a long-term relationship | ref | 1 | 0.099 | |
| Marital status: never married | 0.721 | 0.84 | 0.32 to 2.22 | |
| Marital status: widowed | 0.253 | 1.27 | 0.84 to 1.93 | |
| Marital status: divorced | 0.084 | 0.59 | 0.33 to 1.07 | |
| Marital status: unknown | 0.869 | 1.07 | 0.46 to 2.48 | |
| Type of LTCF=1 | ref | 1 | ||
| Type of LTCF=2–3 | 0.002 | 2.78 | 1.46 to 5.33 | |
| Resident capable of expressing at admission | ||||
| Yes or partly | <0.001 | 3.23 | 2.17 to 4.80 | |
| No | ref | 1 | ||
LTCF, long-term care facility.
Figure 2.
Any written advance directive according to the type of facility 1 and resident’s capability of expression at the time of admission, %, in all countries, in 2014. LTCF type 1 is defined as a long-term care facility (LTCF) with physician and nursing staff with care assistants available 24 hours every day. In type 2 LTCF, nursing staff with care assistants are available 24 hours a day and seven days a week in the facility, and physicians available offsite. In type 3 LTCF, care assistants are available 24/7 in the facility, and nurses and physicians available offsite.
Discussion
Main findings
This study’s findings show from the staff member’s view that written ADs were performed by about a third of older recently deceased residents in LTCFs across Europe. The presence of any written AD, in our study, varied substantially among these LTC residents within and between the six European countries. Being over 90 years also increased the likelihood for having written ADs. Most often, older resident’s ADs were statements to restrict medical treatment such as ‘do not resuscitate in case of cardiac or pulmonary arrest’.
Written ADs were most often prepared by residents, who were capable of expressing himself or herself at the time of admission. According to multivariate analysis, likelihood for having any ADs available before death was more than threefold if the person had been capable of expressing his or her wishes at admission. This study’s results indicate that timing for end-of-life care discussion and ACP with a resident is at its best when a resident has the ability to express himself or herself.
Residents living in nursing or care homes where a physician was available 24 hours a day and 7 days a week were less likely to have written AD compared with facilities where physician was not available in the facility. The presence of nursing or medical professionals in a facility might promote feelings of security in terms of medical treatment at the end-of-life for residents. They were more likely to take the opportunity to make a written AD statement when a physician was not routinely available. This result seems to contradict an earlier study, which showed that resident’s might be willing to have end-of-life discussion with their physician before they make any written statements regarding their end-of-life care.12
Strengths and limitations
This study’s sample of 1384 older LTCF residents is the largest analysis performed about written ADs among LTCF residents in Europe. Response rate for staff questionnaires was high, 81.4% in total.
All countries involved in the study had similar data collection procedure and structured questionnaires. Staff members who were involved in resident’s care knew resident’s individual situation well because data were collected retrospectively within 3 months after the resident’s death.
Regarding the statistical analyses, multilevel analyses accounted for cluster sampling. This made the results less affected by the cultural differences of LTCFs within the country.
The limitations of our study include the nature of data collection and concerns about representativeness. Nurse’s questionnaire’s answers were collected from different sources. Completing the answer categories did not mean that there has been a conversation between a nurse and a resident. For example, in the United Kingdom it is possible that the nurses had drawn on the ACP document which was part of the Gold Standard Framework records to obtain their answer. A specific limitation for the English data is that the nurses and care assistants might have indicated that there were living wills in the nursing home file that in fact were Advance Decisions to Refuse treatment, hence not documents initiated or filled in by the residents themselves.
Another potential bias in the data collection is that the staff who were asked to fill in the questionnaire, was not aware of resident’s written living will documentation. For example, the resident may have told some staff members but not the respondent about their living will. The sampling procedure for LTCFs varied between countries and within countries and it may have had an impact on the comparability of data between countries.
Prevalence of written AD and earlier evidence
The majority of the prevalence studies of AD conducted in Europe vary methodologically and their results are not fully comparable with this study. Similar results of the existence of ACP, among 34% deceased residents, have been found in earlier prevalence study from the Netherlands and Belgium.9 13
When comparing this study’s findings to North American scientific evidence on the topic, it can be seen that the prevalence for any AD among deceased LTCF residents in Europe (32.5%) was less than half from the studies conducted in North American LTCFs (71%–72%).8 The reason for this finding can largely be accounted for by Italy and Poland, where end-of-life planning was generally not found in the LTCFs. However, even if these two countries were excluded, prevalence of ADs in the remaining countries was lower (63.1%) than reported from the US or Canadian LTCFs.17 Prevalence of 76.9% found in the United Kingdom is in line with the North American findings. However, the low percentage of returned staff questionnaires from the United Kingdom suggests caution should be shown in drawing conclusions.
The most often seen AD in European LTCFs was DNR (0%–76%). DNR may be the one most often offered by physicians, and the nursing staff for the older individuals to consider. The appointment of a surrogate decision-maker was seen almost equally often with some variations between countries. Prevalence of DNH showed a variation from 0% to 33%, and all other statements remained under 4% in average. Results of our study suggest that DNR and DNH are used as AD in LTCFs more frequently than previously reported. This is true at least in Finland, where in 2004, DNR order was documented among 13% older persons’ medical records in a study that investigated 67 LTCFs.18 Of those only 0.6% had DNH. This finding is in line with previous trend in general population, shown from the USA by Silveira et al 17: The proportion of deceased people with an AD had increased during 2000 to 2010 from 47% to 72%.17
Medical restrictions and written AD
According to this study’s results, medical treatment restrictions are the ones most often included in resident’s written living will. This is in alignment with evidence from earlier studies, where ADs are shown to be most often conceptualised as limitations for care.3 7 19–22
Apart from items in the structured questionnaire that were used as variables in this study’s analysis, there were also open written statements in the questionnaires which referred mostly to restrictions. Only six residents had stated in their written living will about comfort care and three of them mentioned pain relief.
Question about terminal sedation was available only in Belgium and 5% of the deceased residents had responded positively. This may indicate that either ameliorating pain and other unwanted symptoms is well managed in Belgium LTCFs, and there is no need for particular wishes for comfort care, or discussions with the staff about end-of-life issues mainly offer negative options and restrictions on treatment.
Written ADs and provision of end-of-life care
Care home staff has ACP documentation available for a third of the residents, about the resident’s preferences for end-of-life care. According to the results of this study, we know from nurses’ view that a resident who is capable of expressing himself or herself at the time of admission is more likely to have written ADs. Earlier evidence has also shown that sometimes residents have prepared their written living wills even before being admitted to a nursing or care home.9 11 A staff member, most often a nurse or a physician, initiates ACP with a resident at the time of his or her arrival at the nursing or care home.1 13 23 In an ideal situation, resident’s end-of-life care provided at the facility is based on ACP.
This study’s results show extensive variation between countries in written ADs. The data were collected in a culture-specific context of nursing or care home where the questions were answered by a staff member (preferably, a nurse). The availability of the legally valid documentation of written ADs has varied in the nursing or care home setting according to national regulations and legislations. Same ADs, in particular euthanasia, are not legal in all participating countries. Consequently, it was not possible to ask about their existence in all the countries. Moreover, those LTCF residents, who for some reason preferred to express their living will verbally and not in a written document, were not taken into account.1
The absence of written ADs among the majority of older LTCF residents, as shown in the results of this study, is partly due to their lack of ability to express themselves at the time of admission. Depending on the resident’s knowledge and cognitive capacity, different alternatives to medical treatments are known. Attitude toward ADs might be influenced by the resident’s health condition, closeness of death or the resident’s burden on close relatives or friends.4 23 24 The resident’s earlier acquaintance experiences with death and dying among friends and family might encourage older residents to prepare for their end-of-life care. At the last phase of life, older residents’ health situations may become complex, and dependency on other caregivers increases.8 24 25 Even when there is no doubt about the importance of ACP, an elderly person still wants to have trust in his or her physician, healthcare professional or family member before he or she is willing to make choices regarding future end-of-life care.14 26
ACP is a sign of the recognition of a person’s needs and preferences and it demonstrates a person’s involvement in own end-of-life’s care planning.24 27 Even in a situation where the LTCF resident’s health condition changes, the resident and the surrogate(s) need to have a chance to change their mind and make changes to the living will.13
In the light of this study’s results and earlier scientific evidence, we may suggest that LTCF resident’s health situation, especially impaired cognitive capacity, provides indication of a resident’s involvement in completing ADs. The way resident’s health needs are met at the LTCF facility by the care professionals appears to have an impact on the resident’s willingness for end-of-life care planning and ADs. To answer the questions
Whether meeting resident’s health needs and completing ADs are linked to each other
-
Assess what kind of communication is preferred,
further research about consistency between LTCF resident’s health needs and ADs is suggested.
Conclusions
In European LTCFs, prevalence of written AD varies from country to country. The contents of ADs are mainly restrictive and the most common AD is DNR.
LTCF residents who are capable of expressing himself or herself at the time of admission are more likely to have an AD compared with residents who are not able to express themselves at the arrival to facility. Residents living in a facility without physician available are more likely to have an AD than residents who have physician available.
Footnotes
Collaborators: PACE Consortium.
Contributors: PA made a research plan that was approved by PACE project’s executive committee. Research proposal was critically reviewed by the authors. Data used in this study’s analysis originate from PACE project Study 1 data collection. LD and LVdB were leaders of PACE project Study 1. All authors substantially contributed to the study’s data collection. GG, HF-S, KS and SP were country leads and they conducted PACE Study 1 survey and data collection in PACE Study 1 partner countries. VK and KS coordinated data collection in Poland. BO-P, EL and TS prepared collected data suitable for this study’s statistical analysis. EL, PA and HF-S performed the statistical analyses in collaboration with TS and LVdB and interpreted and discussed the results with all the authors. All the authors took part in interpreting the results. PA made literature search and wrote all sections of the manuscript. HF-S supervised PA throughout the process. All authors have revised and provided comments to the drafted writing. All authors approved the final version of the manuscript which PA submitted.
Funding: PACE project is funded by European Union’s Seventh Framework Programme with grant agreement no 603111. The project was cofunded by Polish Ministry of Science and Higher Education in the years 2014–2019 based on the decision no 3202/7PR/2014/2 dated on November 25, 2014. The funders have no involvement in payment of article processing fee.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
PACE study protocol had been approved by ethical committee according to each participating countries’ national procedure of scientific ethical approval.
References
- 1. Hildén H-M, Louhiala P, Honkasalo M-L, et al. Finnish nurses' views on end-of-life discussions and a comparison with physicians' views. Nurs Ethics 2004;11:165–78. 10.1191/0969733004ne681oa [DOI] [PubMed] [Google Scholar]
- 2. Martin DK, Emanuel LL, Singer PA. Planning for the end of life. The Lancet 2000;356:1672–6. 10.1016/S0140-6736(00)03168-8 [DOI] [PubMed] [Google Scholar]
- 3. Rietjens JAC, van der Heide A, van der Heide A BRINKMAN-STOPPELENBURG A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014;28:1000–25. 10.1177/0269216314526272 [DOI] [PubMed] [Google Scholar]
- 4. Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340:c1345. 10.1136/bmj.c1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reitinger E, Froggatt K, Brazil K, et al. Palliative care in long-term care settings for older people: findings from an EAPC Taskforce. European Journal Of Palliative Care 2013;20:251–3. [Google Scholar]
- 6. Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European association for palliative care. Lancet Oncol 2017;18:e543–51. 10.1016/S1470-2045(17)30582-X [DOI] [PubMed] [Google Scholar]
- 7. Bollig G, Gjengedal E, Rosland JH. They know!-Do they? A qualitative study of residents and relatives views on advance care planning, end-of-life care, and decision-making in nursing homes. Palliat Med 2016;30:456–70. 10.1177/0269216315605753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones AL, Moss AJ, Harris-Kojetin LD. Use of advance directives in long-term care populations. NCHS Data Brief 2011;54:1–18. [PubMed] [Google Scholar]
- 9. Meeussen K, Van den Block L, Echteld M, Echteld M, et al. Advance care planning in Belgium and the Netherlands: a nationwide retrospective study via sentinel networks of general practitioners. J Pain Symptom Manage 2011;42:565–77. 10.1016/j.jpainsymman.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 10. Resnick HE, Schuur JD, Heineman J, et al. Advance directives in nursing home residents aged ≥65 years: United States 2004. Am J Hosp Palliat Care 2009;25:476–82. 10.1177/1049909108322295 [DOI] [PubMed] [Google Scholar]
- 11. van der Heide A, Deliens L, Faisst K, et al. End-of-life decision-making in six European countries: descriptive study. The Lancet 2003;362:345–50. 10.1016/S0140-6736(03)14019-6 [DOI] [PubMed] [Google Scholar]
- 12. De Vleminck A, Pardon K, Houttekier D, et al. The prevalence in the general population of advance directives on euthanasia and discussion of end-of-life wishes: a nationwide survey. BMC Palliat Care 2015;14. 10.1186/s12904-015-0068-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rurup ML, Onwuteaka-Philipsen BD, van der Heide A, et al. Frequency and determinants of advance directives concerning end-of-life care in the Netherlands. Soc Sci Med 2006;62:1552–63. 10.1016/j.socscimed.2005.08.010 [DOI] [PubMed] [Google Scholar]
- 14. Lewis E, Cardona-Morrell M, Ong KY, et al. Evidence still insufficient that advance care documentation leads to engagement of healthcare professionals in end-of-life discussions: a systematic review. Palliat Med 2016;30:807–24. 10.1177/0269216316637239 [DOI] [PubMed] [Google Scholar]
- 15. Sudore RL, Lum HD, You JJ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manage 2017;53:821–32. 10.1016/j.jpainsymman.2016.12.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Van den Block L, Smets T, van Dop N, et al. Comparing palliative care in care homes across Europe (PACE): protocol of a cross-sectional study of deceased residents in 6 EU countries. J Am Med Dir Assoc 2016;17:566.e1–566.e7. 10.1016/j.jamda.2016.03.008 [DOI] [PubMed] [Google Scholar]
- 17. Silveira MJ, Wiitala W, Piette J. Advance Directive completion by elderly Americans: a decade of change. J Am Geriatr Soc 2014;62:706–10. 10.1111/jgs.12736 [DOI] [PubMed] [Google Scholar]
- 18. Laakkonen M-L, Finne-Soveri UH, Noro A, et al. Advance orders to limit therapy in 67 long-term care facilities in Finland. Resuscitation 2004;61:333–9. 10.1016/j.resuscitation.2004.01.010 [DOI] [PubMed] [Google Scholar]
- 19. Karppinen H, Laakkonen M-L, Strandberg TE, et al. Living wills and end-of-life care of older people suffering from cardiovascular diseases: a ten-year follow-up. Eur Geriatr Med 2014;5:31–4. 10.1016/j.eurger.2013.09.009 [DOI] [Google Scholar]
- 20. Laakkonen M-L, Pitkala KH, Strandberg TE, et al. Living will, resuscitation preferences, and attitudes towards life in an aged population. Gerontology 2004;50:247–54. Jul-Aug. 10.1159/000078354 [DOI] [PubMed] [Google Scholar]
- 21. Sudore RL, Fried TR. Redefining the "planning" in advance care planning: preparing for end-of-life decision making. Ann Intern Med 2010;153:256–61. 10.7326/0003-4819-153-4-201008170-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Thompson TDB, Barbour RS, Schwartz L. Health professionals' views on advance directives: a qualitative interdisciplinary study. Palliative Medicine. 2003;17:403–9. 10.1191/0269216303pm784oa [DOI] [PubMed] [Google Scholar]
- 23. Hildén H-M, Honkasalo M-L. Finnish Nurses’ Interpretations of Patient Autonomy in the Context of End-of-Life Decision Making. Nursing Ethics. 2006;13:41–51. 10.1191/0969733006ne856oa [DOI] [PubMed] [Google Scholar]
- 24. Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med 2006;166:890–5. 10.1001/archinte.166.8.890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Amjad H, Towle V, Fried T. Association of experience with illness and end-of-life care with advance care planning in older adults. J Am Geriatr Soc 2014;62:1304–9. 10.1111/jgs.12894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fleming J, Farquhar M, Brayne C, et al. Death and the Oldest Old: Attitudes and Preferences for End-of-Life Care-Qualitative Research within a Population-Based Cohort Study. PLoS One 2016;11:e0150686–25. 10.1371/journal.pone.0150686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Klindtworth K, Oster P, Hager K, et al. Living with and dying from advanced heart failure: understanding the needs of older patients at the end of life. BMC Geriatr 2015;15. 10.1186/s12877-015-0124-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjspcare-2018-001743supp001.pdf (77.4KB, pdf)