Asian Americans were the fastest-growing population segment in the United States in the last two decades. The population growth of all Asians was 34% from 2010 to 2019, compared with 6% for all Americans (Budiman, 2020). In the older population, aged 65 years and above, Asian Americans are also the fastest-growing minority group (Budiman & Ruiz, 2021). The older Asian American population was 2.5 million in 2019 and is projected to grow to 7.9 million by 2060. In 2019, Asian Americans made up 4.6% of the older population. By 2060, the percentage is projected to be 8% (Administration for Community Living, 2021). Asian Americans are very diverse in their nations of origins and languages, with more than 50 ethnicities and 100 different languages and dialects (Budiman, 2020). Most Asian Americans trace their roots to countries in East Asia, Southeast Asia, and the Indian subcontinent. The following six origin groups account for the majority of the U.S. Asian population (85%): Chinese, Filipino, Indian, Vietnamese, Korean, and Japanese. Aside from Native Hawaiians and Other Pacific Islanders, Asian Americans accounted for 31% of the U.S. older immigrant’s population and by the year 2055 will surpass Hispanics as the largest immigrant group (Mizoguchi et al., 2019), and they represent distinct cultural beliefs and customs, incomes, levels of education, geographic locations, religions, languages, immigration patterns, and levels of acculturation (Budiman & Ruiz, 2021). Thus, in this paper, the term Asian Americans did not include Native Hawaiian and Other Pacific Islanders.
Myths on the Stereotype of the “Model Minority”
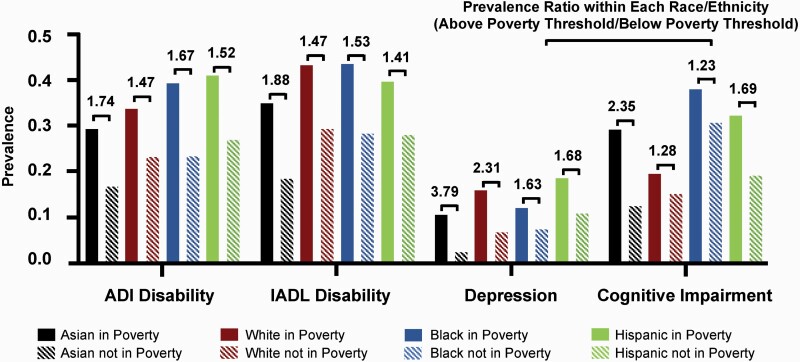
The “model minority” stereotype presents Asian Americans as monolithic. Some of the major characteristics of this stereotype are high educational attainment, high mediate family income, and good health status. In fact, Asian Americans have the largest income divide (Kochhar & Cilluffo, 2018). Many older Asian Americans lack the financial resources of their younger counterparts. The sentiment of a financially strong Asian American population discounts the growing number of older Asian Americans with a rising poverty rate. For example, according to the American Community Survey of 2015 (Bishaw & Glassman, 2016), the poverty rate for older Asians aged 65 and above was 13%, while the rate of all older Americans was 9%. Further, between 2009 and 2014, the poverty rate increased by 40% for older Asian Americans (Gloria, 2020). The income inequality in the older Asian population is associated with the highest health disparities compared with other races or ethnicities. Using data from the National Health and Nutrition Examination Survey 2011–2018, we conducted an analysis and compared the prevalence ratios of four major health outcomes among older adults within each of the race or ethnicity groups. The sample includes 2,869 adults aged 60 and older (421 Asians, 768 non-Hispanic Blacks, 651 Hispanics, and 1,029 non-Hispanic Whites). Income was measured by the Poverty-Income Ratio (PIR), which represents the ratio of the household income relative to the poverty threshold after adjustments for geographic location and family size. A PIR of less than 1.00 represents those below the official poverty threshold, and PIR values of 1.00 or greater indicate people above the poverty threshold. In our analysis, having a PIR <1.0 is defined as living in poverty and having a PIR ≥1.0 is defined as not living in poverty (Keppel et al., 2004).
The health outcomes in this study included physical disabilities, cognitive impairments, and depressive symptoms. Physical disabilities were measured by the inability to perform activities of daily living (defined as answering “some difficulty” or “much difficulty” in performing one or more of the following tasks: getting in and out of bed, eating, dressing yourself) and instrumental activities of daily living (defined as answering “some difficulty” or “much difficulty” in performing one or more of the following tasks: managing money, performing house chores, preparing meals). Cognitive impairment was measured as having a score <14 using the Consortium to Establish a Registry for Alzheimer’s Disease–Immediate Recall (Welsh et al., 1994). Having depressive symptoms was defined as having a score <10 in the Patient Health Questionnaire (Moriarty et al., 2015). Our analyses found that for those in poverty, Blacks had the highest prevalences of instrumental activities of daily living disabilities and cognitive impairments (36.7% and 34.2%, respectively) and Hispanics had the highest prevalences of activities of daily living disabilities and depressive symptoms (34.1% and 14.8%, respectively; see Figure 1). However, the health disparities were most prominent within Asians with regard to income. Compared with older adults not in poverty within the same racial or ethnic group, Asians in poverty had the highest prevalence ratios of physical, cognitive, and functional disabilities (all P values < 0.05). Among the four health outcomes in Asians, depressive symptoms had the highest disparity. Older Asian Americans in poverty had a 3.79 times higher rate of depressive symptoms than those not in poverty.
Figure 1.
Comparison of the prevalence ratio of health outcomes among older adults within each race or ethnicity group: below poverty and above poverty. ADL, activities of daily living; IADL, instrumental activities of daily living.
Older Asian Americans are reported to have a lower prevalence and a lower incidence of mental health problems and dementia compared with non-Hispanic Whites (Gilsanz et al., 2019; Kim et al., 2012; Kim & Choi, 2010; Mayeda et al., 2016). For example, previous research using a nationally representative sample of community-dwelling older adults in the United States has reported that older Asian Americans exhibit the lowest prevalence rates of mood disorders (2.3%), psychological distress (2.6%), and anxiety disorders (5.1%) compared with older non-Hispanic Whites, non-Hispanic Blacks, and Hispanics (Kim et al., 2012). A 14-year cohort study found that the age-standardized incidence of dementia for all older Asian Americans is lower than for Whites (15.2/1000 vs. 19.3/1000 person-years, respectively; Mayeda et al., 2016). As mentioned earlier, the older Asian population is highly diverse culturally, demographically, linguistically, and socioeconomically, and the aggregated data for these groups masked critical health disparities and their drivers. For example, previous literature consistently reported older Asian women had the highest suicide rate in women of all racial or ethnic groups (Kim et al., 2012; Zhang et al., 2022). In addition, a systematic review of 1,215 studies found that when disaggregated by Asian subgroups, the annual incidence of dementia in older Japanese Americans is significantly higher than in non-Hispanic Whites (2.0% vs. 1.6%, respectively; Mehta & Yeo, 2017).
Researchers and health-care professionals believe that the relatively lower estimation of mental illness and dementia among older Asian Americans is partly due to the fact that this group is less likely to report mental and cognitive health problems due to cultural shame, misperceptions, and stigma surrounding mental and cognitive disorders (Cheng et al., 2010; Lee et al., 2009; Yeo et al., 2018). Consequently, they are less likely to receive timely screening, service, and treatment. Using the data we collected in the Boston Chinese community, 9% of the older Chinese immigrants had depressive symptoms; however, none of them reported visiting a psychiatrist in the previous 12 months (Wu, Chi, et al., 2010). In 2017–2018, older Asian Americans were 60% less likely to use mental health services as compared to Whites (Zhang et al., 2022). White older adults might be more likely to seek mental health care at lower levels of need, while Asian and Hispanic older adults might only seek services when they perceive a greater need (Zhang et al., 2022). Furthermore, older Asian Americans are less knowledgeable about dementia compared with their non-Hispanic White counterparts (Lee et al., 2009; Sun et al., 2014). Early symptoms of dementia are often misunderstood as a normal part of aging among different Asian American subgroups (i.e., Chinese, Vietnamese, Korean, Filipino, and Asian Indians; Jang et al., 2010; Lee & Casado, 2019), and dementia is generally perceived as mental illness and a certain form of insanity among the East Asian American subgroup, leading to profound levels of stigma surrounding dementia (Jang et al., 2010; Wu, Lombardo, et al., 2010). All of these hinder the timely screening, diagnosis, and treatment of mental and cognitive disorders, which obscures important disparities in health and results in the knowledge gaps about health conditions among specific older Asian American groups.
Asian American Health Status: Pictures Incomplete
Much of our knowledge of Asian American health has been determined by studies in which investigators have either grouped Asian American subjects together or examined one subgroup alone (e.g., Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese; Holland & Palaniappan, 2012). National health surveys that collect information on Asian American race and ethnicity frequently omit this population in research reports. When national health data are reported for Asian American subjects, they are often reported for the aggregated group. This aggregation may mask differences between Asian American subgroups. When health data are reported by Asian American subgroups, they are generally reported for one subgroup alone. Findings from national survey data often show that Asian Americans have a better health status than other racial or ethnic groups. The findings from these data highlight the notion of the model minority for Asian Americans.
Here are some of the findings from our previous studies that examined oral health outcomes among Asian American older adults. We first examined edentulism (i.e., complete tooth loss) trends among adults aged 50 and above in five ethnic groups in the United States: Asians, African Americans, Hispanics, Native Americans, and non-Hispanic Caucasians (Wu et al., 2012). Data came from the National Health Interview Surveys (NHIS) between 1999 and 2008. This study generated the predicted rates of edentulism, adjusting for time, sociodemographic characteristics, and levels of education. The findings show that in 2008, Native Americans had the highest rate of edentulism (23.98%), followed by African Americans (19.39%), Caucasians (16.90%), Asians (14.22%), and Hispanics (14.18%).
Using the same data set, we further examined differences in edentulism within middle-aged and older Asian subgroups in comparison to the other three racial and ethnic groups (Blacks, Hispanics, and Whites; Wu et al., 2013). The findings show that the rates of edentulism differed substantially across Asian subgroups. Filipinos had the highest rate of edentulism in the Asian group. In addition, Filipinos also had a higher rate than those from three other racial or ethnic groups. Compared with Whites, Chinese had a lower risk of being edentulous, whereas being Filipino increased the risk. The rate for Asian Indians was similar to that for Whites. Nonetheless, rates of decline were similar across the Asian population groups. One caveat of these studies is that the NHIS was conducted only in English; individuals who did not speak English were more likely to have a lower socioeconomic status and, thus, have a higher risk of poor oral health. Most of the older Asian Americans are immigrants, and 34% of them have low English proficiency according to the 2013 American Community Surveys (Batalova et al., 2015). Therefore, studies using these national surveys, such as the NHIS, are likely to yield biased findings on Asian Americans.
While older Chinese Americans showed better oral health status than other racial or ethnic groups using national survey data, we conducted a systematic review on oral health and dental care utilization among older Chinese immigrant populations (Mao et al., 2015). Of the 15 eligible studies, three were conducted in the United States. The findings were different from the ones presented above using national survey data. These review results showed that older Chinese immigrants had poorer oral health and less dental care use than the general population in their host country. All these included studies featured small, nonrepresentative samples recruited from Chinese communities, service agencies, and other sources. Most of the data collection was conducted in Chinese. The generalizability of significant results was a major concern.
Oral health disparities reflect some of the most challenging issues faced in the United States, such as a lack of access to dental care, a lack of publicly funded dental insurance for older adults, and racial prejudice. Findings from these oral health–related studies show many health disparities within Asian American populations. Seemingly contradictory findings from these studies are mainly due to the differences in sampling, data collection, and representation of the survey data.
Issues Related to Asian American Health Research
Asian Americans are one of the most understudied racial or ethnic minority groups in the United States. The lack of data on Asian Americans results in deficits in health-care systems, which fail to understand the complexity and diversity of the population’s health risks (Ma et al., 2021; Yi et al., 2021).
Asian Americans are one of the most understudied racial or ethnic minority groups in the United States. The lack of data on Asian Americans results in deficits in health-care systems, which fail to understand the complexity and diversity of the population’s health risks.
Methodological Considerations
Several major methodological concerns need to be addressed while conducting research on older Asian Americans. Currently, there is a lack of national representation of Asian Americans in large data sets. Another major data issue is the potential exclusion of those Asian older adults with limited English capacity and those who are undocumented. In addition, there is a lack of disaggregated data for Asian subpopulations. Among the limited data that include Asian Americans, only a few subpopulation groups were included, such as Chinese, Indians, and Filipinos, which limited the ability to describe and/or intervene on specific health concerns for Asian subgroups. Moreover, for Asian Americans, there is a lack of longitudinal data to study this population’s health trajectory and the multilevel factors that affect their health status over the life course. In addition to the lack of data on Asian Americans, measurement is another concern. There is a great need to have culturally appropriate instruments to measure psychosocial factors and mental health–related outcomes.
Research Underfunded
Limited research funding was invested in studying Asian Americans. Based on an analysis on federally sponsored research from 1986 to 2000, less than 0.1% of grants were funded to Asian Americans (Ghosh, 2003). Approximately 0.17% of National Institutes of Health grants were to Asian Americans (2000–2018; Ðoàn et al., 2019). Given the increased number and proportion of older Asian population in the United States, as well as the paucity of our current understanding of this population’s health, federal action is required to close the funding disparity. Representation and equitable research funding for older Asian Americans is essential, because adequate funding provides the needed resources for research in this population, which determines funding priorities, interventions, and translating research into policy and practices that are equitable (Ðoàn et al., 2019; Dong, 2019).
Conceptual Framework to Understand Asian American Health
The majority (86%) of older Asian Americans are foreign-born immigrants (Budiman & Ruiz, 2021). Many young and adult immigrants came to the United States mainly for educational and job opportunities, while the reasons for immigration for older immigrants are very different. Many came here for family unification and to help raise grandchildren, and a small percentage may come into this country as refugees (Wu, 2022). It is critical to developing a conceptual framework to help understand the mechanisms and pathways of factors that impact late-life health outcomes among older Asian immigrant populations. Recently, we developed an integrative framework for immigration, aging, and health status (Wu et al., 2021). In this framework, the immigration process is situated within the life course and within larger structures and contexts. Immigration is a crucial part of the larger context in studying immigrant health outcomes. Immigration is a dynamic process that may interact with various aspects of the lives of older immigrants. This framework captures multilevel factors, including structural- and contextual-level factors, community-level factors, and individual-level factors, as well as interactions and pathways across these factors and processes. This framework highlights the impact of pre-immigration antecedents, often neglected in immigrant research, on health outcomes. These factors include early life conditions before immigration and characteristics in the country of origin (e.g., socioeconomic development, health-care system, and quality of education).
Immigration factors characterize the immigration process and capture the critical factors and changes during exposure to different cultures and environments. These environmental, psychosocial, and behavioral factors reflect cultural values, social norms, and health beliefs that are particularly relevant to immigration. Structural racism is a major upstream contributor to health-care disparities. Structural racism manifests as the historical and continued invisibility of Asian Americans, whose experiences of disparities and diverse needs are omitted in research, data, and policy. During the pandemic, this invisibility intersected with rising anti-Asian violence and other persistent structural inequities that contributed to higher mortality from coronavirus disease 2019 in older Asian Americans compared to non-Hispanic Whites (Ma et al., 2021).
Research and Policy Implications
Multiple approaches are needed to challenge persistent stereotypes of older Asian Americans and address health disparities in the population. What emerged from our experience is that there is a demand for building research infrastructure and community partnerships.
Building Research Infrastructure
There is a need to allocate federal and foundation funding for more national and local data collection (Chen, 2019), including oversampling of Asian Americans in data collection and reporting of race and ethnicity data by Asian American subgroup; investing in infrastructure support for cohort studies; enhancing existing data sources to enable data disaggregation; and incorporating novel technology for objective measurements (Kanaya et al., 2022). The needs for small Asian subgroups are likely to be overlooked. In this case, funding can be allocated to conduct small-scale studies using qualitative and mixed-methods approaches and clinical trials that could generate more comprehensive data to capture people’s lived experiences.
With the establishment of the Asian Recourse Center for Minority Aging Research (P30AG059304), funded by the National Institute on Aging in 2018, and the Rutgers–New York University Center for Asian Health Promotion and Equity (P50MD017356), funded by the National Institute on Minority Health and Health Disparities in 2021, we have witnessed increased research support toward these efforts. Localized programs for research, like the Study of Older Korean Americans (R01AG047106) and the Population Study of Chinese Elderly (R01AG042318), supported by the National Institute on Aging, have been successful in supporting data collection and reporting for large, epidemiological studies of older Chinese and Korean adults in the United States. However, evidence on the determinants of these disparities is still limited. Increased efforts should be made on national and international levels to understand the experiences and health of older Asians and to fill the knowledge gaps. In addition, we need to increase mentored research and training for the next generation of diverse scientists in health-disparity research, to advance health equity for Asian Americans.
Community Partnership
Building community partnership is essential for all aspects of research, including developing study protocol designs, recruitment, data collection, and interpretation and dissemination of study findings (Kanaya et al., 2022; Yi et al., 2021). Forging partnerships could strengthen collaboration and infrastructure particularly around data collection and reporting on older Asian subgroups. Working with community partners can also help identify care needs and help develop culturally and linguistically appropriate health-care services and interventions that meet the needs of diverse older Asian populations.
Building community partnership is essential for all aspects of research, including developing study protocol designs, recruitment, data collection, and interpretation and dissemination of study findings.
Contributor Information
Bei Wu, Rory Meyers College of Nursing, New York University, New York, New York, USA; Aging Incubator, New York University, New York, New York, USA.
Xiang Qi, Rory Meyers College of Nursing, New York University, New York, New York, USA.
Funding
This work was supported by the National Institutes of Health (P50MD017356 and P30AG059304).
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Administration for Community Living. (2021, November 24). 2020 profile of Asian Americans age 65 and older.Department of Health and Human Service. https://acl.gov/sites/default/files/Profile%20of%20OA/AsianProfileReport2021.pdf [Google Scholar]
- Batalova, J. Z., Batalova, J., & Zong, J. (2015, July 7). The limited English proficient population in the United States in 2013. Migrationpolicy.Org. https://www.migrationpolicy.org/article/limited-english-proficient-population-united-states-2013
- Bishaw, A., & Glassman, B. (2016, September 16). Poverty: 2014 and 2015. US Department of Commerce, Economics and Statistics Administration, US Census Bureau.
- Budiman, A. (2020, May 7). Asian Americans are the fastest-growing racial or ethnic group in the U.S. electorate. Pew Research Center.https://www.pewresearch.org/fact-tank/2020/05/07/asian-americans-are-the-fastest-growing-racial-or-ethnic-group-in-the-u-s-electorate/
- Budiman, A., & Ruiz, N. G. (2021, April 29). Key facts about Asian Americans, a diverse and growing population. Pew Research Center. https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-americans/
- Chen, M. S. (2019). Rectifying disparities in funding of Asian American, Native Hawaiian, and Pacific Islander research by the US National Institutes of Health. JAMA Network Open, 2(7), e197561. doi: 10.1001/jamanetworkopen.2019.7561 [DOI] [PubMed] [Google Scholar]
- Cheng, J. K. Y., Fancher, T. L., Ratanasen, M., Conner, K. R., Duberstein, P. R., Sue, S., & Takeuchi, D. (2010). Lifetime suicidal ideation and suicide attempts in Asian Americans. Asian American Journal of Psychology, 1(1), 18–30. doi: 10.1037/a0018799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ðoàn, L. N., Takata, Y., Sakuma, K.-L. K., & Irvin, V. L. (2019). Trends in clinical research including Asian American, Native Hawaiian, and Pacific Islander participants funded by the US National Institutes of Health, 1992 to 2018. JAMA Network Open, 2(7), e197432. doi: 10.1001/jamanetworkopen.2019.7432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, X. (2019). Advancing Asian health equity: Multimodal approach to translate research into practice and policy. Journal of the American Geriatrics Society, 67(S3). doi: 10.1111/jgs.16110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh, C. (2003). Healthy People 2010 and Asian Americans/Pacific Islanders: Defining a baseline of information. American Journal of Public Health, 93(12), 2093–2098. 10.2105/ajph.93.12.2093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilsanz, P., Corrada, M. M., Kawas, C. H., Mayeda, E. R., Glymour, M. M., Quesenberry, C. P., Lee, C., & Whitmer, R. A. (2019). Incidence of dementia after age 90 in a multiracial cohort. Alzheimer’s & Dementia, 15(4), 497–505. doi: 10.1016/j.jalz.2018.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloria, G. (2020). Household income by race and Hispanic origin: 2005–2009 and 2015–2019. US Census Bureau. https://www.census.gov/content/dam/Census/library/publications/2020/acs/acsbr19-07.pdf [Google Scholar]
- Holland, A. T., & Palaniappan, L. P. (2012). Problems with the collection and interpretation of Asian-American health data: Omission, aggregation, and extrapolation. Annals of Epidemiology, 22(6), 397–405. doi: 10.1016/j.annepidem.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang, Y., Kim, G., & Chiriboga, D. (2010). Knowledge of Alzheimer’s disease, feelings of shame, and awareness of services among Korean American elders. Journal of Aging and Health, 22(4), 419–433. doi: 10.1177/0898264309360672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanaya, A. M., Hsing, A. W., Panapasa, S. V., Kandula, N. R., Araneta, M. R. G., Shimbo, D., Wang, P., Gomez, S. L., Lee, J., Narayan, K. M. V., Mau, M. K. L. M., Bose, S., Daviglus, M. L., Hu, F. B., Islam, N., Jackson, C. L., Kataoka-Yahiro, M., Kauwe, J. S. K., Liu, S., … Hong, Y. (2022). Knowledge gaps, challenges, and opportunities in health and prevention research for Asian Americans, Native Hawaiians, and Pacific Islanders: A report from the 2021 National Institutes of Health Workshop. Annals of Internal Medicine, 175(4), 574–589. doi: 10.7326/M21-3729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keppel, K. G., Pearcy, J. N., & Klein, R. J. (2004). Measuring progress in Healthy People 2010. Healthy People 2010 Statistical Notes: From the Centers for Disease Control and Prevention/National Center for Health Statistics, 25, 1–16. doi: 10.1037/e583732012-001 [DOI] [PubMed] [Google Scholar]
- Kim, G., Bryant, A. N., & Parmelee, P. (2012). Racial/ethnic differences in serious psychological distress among older adults in California: SPD and race/ethnicity. International Journal of Geriatric Psychiatry, 27(10), 1070–1077. doi: 10.1002/gps.2825 [DOI] [PubMed] [Google Scholar]
- Kim, J., & Choi, N. G. (2010). Twelve-month prevalence of DSM-IV mental disorders among older Asian Americans: Comparison with younger groups. Aging & Mental Health, 14(1), 90–99. doi: 10.1080/13607860903046461 [DOI] [PubMed] [Google Scholar]
- Kochhar, R., & Cilluffo, A. (2018, July 12). Income inequality in the U.S. is rising most rapidly among Asians. Pew Research Center’s Social & Demographic Trends Project. https://www.pewresearch.org/social-trends/2018/07/12/income-inequality-in-the-u-s-is-rising-most-rapidly-among-asians/ [Google Scholar]
- Lee, S. E., & Casado, B. L. (2019). Knowledge of Alzheimer’s disease among Vietnamese Americans and correlates of their knowledge about Alzheimer’s disease. Dementia, 18(2), 713–724. doi: 10.1177/1471301217691616 [DOI] [PubMed] [Google Scholar]
- Lee, S. E., Lee, H. Y., & Diwan, S. (2009). What do Korean American immigrants know about Alzheimer’s disease (AD)? The impact of acculturation and exposure to the disease on AD knowledge. International Journal of Geriatric Psychiatry, 25(1), 66–73. doi: 10.1002/gps.2299 [DOI] [PubMed] [Google Scholar]
- Ma, K. P. K., Bacong, A. M., Kwon, S. C., Yi, S. S., & Ðoàn, L. N. (2021). The impact of structural inequities on older Asian Americans during COVID-19. Frontiers in Public Health, 9, 690014. doi: 10.3389/fpubh.2021.690014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao, W., Wu, B., & Chi, I. (2015). Oral health among older Chinese immigrants and implications for social work practice. Health & Social Work, 40(3), e75–e82. doi: 10.1093/hsw/hlv035 [DOI] [Google Scholar]
- Mayeda, E. R., Glymour, M. M., Quesenberry, C. P., & Whitmer, R. A. (2016). Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimer’s & Dementia, 12(3), 216–224. doi: 10.1016/j.jalz.2015.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta, K. M., & Yeo, G. W. (2017). Systematic review of dementia prevalence and incidence in United States race/ethnic populations. Alzheimer’s & Dementia, 13(1), 72–83. doi: 10.1016/j.jalz.2016.06.2360 [DOI] [PubMed] [Google Scholar]
- Mizoguchi, N., Walker, L., Trevelyan, E., & Ahmed, B. (2019). The older foreign-born population in the United States: 2012–2016 (American Community Survey reports). American Community Survey. https://www.census.gov/content/dam/Census/library/publications/2019/acs/acs-42.pdf [Google Scholar]
- Moriarty, A. S., Gilbody, S., McMillan, D., & Manea, L. (2015). Screening and case finding for major depressive disorder using the Patient Health Questionnaire (PHQ-9): A meta-analysis. General Hospital Psychiatry, 37(6), 567–576. doi: 10.1016/j.genhosppsych.2015.06.012 [DOI] [PubMed] [Google Scholar]
- Sun, F., Gao, X., Shen, H., & Burnette, D. (2014). Levels and correlates of knowledge about Alzheimer’s disease among older Chinese Americans. Journal of Cross-Cultural Gerontology, 29(2), 173–183. doi: 10.1007/s10823-014-9229-6 [DOI] [PubMed] [Google Scholar]
- Welsh, K. A., Butters, N., Mohs, R. C., Beekly, D., Edland, S., Fillenbaum, G., & Heyman, A. (1994). The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part V. A normative study of the neuropsychological battery. Neurology, 44(4), 609–614. doi: 10.1212/wnl.44.4.609 [DOI] [PubMed] [Google Scholar]
- Wu, B. (2022, March 23). New older immigrants in the U.S. http://generations.asaging.org/new-older-immigrants-us
- Wu, B., Chi, I., Plassman, B. L., & Guo, M. (2010). Depressive symptoms and health problems among Chinese immigrant elders in the US and Chinese elders in China. Aging & Mental Health, 14(6), 695–704. doi: 10.1080/13607860802427994 [DOI] [PubMed] [Google Scholar]
- Wu, B., Liang, J., Landerman, L., & Plassman, B. (2013). Trends of edentulism among middle-aged and older Asian Americans. American Journal of Public Health, 103(9), e76–82. doi: 10.2105/AJPH.2012.301190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, B., Liang, J., Plassman, B. L., Remle, C., & Luo, X. (2012). Edentulism trends among middle-aged and older adults in the United States: Comparison of five racial/ethnic groups: Edentulism trends in the US. Community Dentistry and Oral Epidemiology, 40(2), 145–153. doi: 10.1111/j.1600-0528.2011.00640.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, B., Lombardo, N. B. E., & Chang, K. (2010). Dementia care programs and services for Chinese Americans in the U.S. Ageing International, 35(2), 128–141. doi: 10.1007/s12126-010-9055-2 [DOI] [Google Scholar]
- Wu, B., Mao, W., Qi, X., & Pei, Y. (2021). Immigration and oral health in older adults: An integrative approach. Journal of Dental Research, 100(7), 686–692. doi: 10.1177/0022034521990649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo, G., Gerdner, L., & Gallagher-Thompson, D. (2018). Ethnicity and the dementias. doi: 10.4324/9781315161358 [DOI]
- Yi, S. S., Ðoàn, L. N., Choi, J. K., Wong, J. A., Russo, R., Chin, M., Islam, N. S., Taher, M., Wyatt, L., Chong, S. K., Trinh-Shevrin, C., & Kwon, S. C. (2021). With no data, there’s no equity: Addressing the lack of data on COVID-19 for Asian American communities. EClinicalMedicine, 41, 101165. doi: 10.1016/j.eclinm.2021.101165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, L., O’Malley, I., Cruz-Gonzalez, M., Sánchez González, M. L., & Alegría, M. (2022). Factors associated with mental health service use among Black, Latinx, and Asian older adults in community-based organizations. Journal of Applied Gerontology, 41(3), 680–689. doi: 10.1177/07334648211012802 [DOI] [PMC free article] [PubMed] [Google Scholar]