Abstract
Background
Development of skills in diagnostic reasoning is paramount to the transition from novice to expert clinicians. Efforts to standardize approaches to diagnosis and treatment using clinical pathways are increasingly common. The effects of implementing pathways into systems of care during diagnostic education and practice among pediatric residents are not well described.
Objective
To characterize pediatric residents' perceptions of the tradeoffs between clinical pathway use and diagnostic reasoning.
Methods
We conducted a qualitative study from May to December 2019. Senior pediatric residents from a high-volume general pediatric inpatient service at an academic hospital participated in semi-structured interviews. We utilized a basic interpretive qualitative approach informed by a dual process diagnostic reasoning framework.
Results
Nine residents recruited via email were interviewed. Residents reported using pathways when admitting patients and during teaching rounds. All residents described using pathways primarily as management tools for patients with a predetermined diagnosis, rather than as aids in formulating a diagnosis. As such, pathways primed residents to circumvent crucial steps of deliberate diagnostic reasoning. However, residents relied on bedside assessment to identify when patients are “not quite fitting the mold” of the current pathway diagnosis, facilitating recalibration of the diagnostic process.
Conclusions
This study identifies important educational implications at the intersection of residents' cognitive diagnostic processes and use of clinical pathways. We highlight potential challenges clinical pathways pose for skill development in diagnostic reasoning by pediatric residents. We suggest opportunities for educators to leverage clinical pathways as a framework for development of these skills.
Objectives
To characterize pediatric residents' perceptions of the tradeoffs between clinical pathway use and diagnostic reasoning.
Findings
The use of clinical pathways supports management decisions by resident physicians but may allow residents to bypass critical points in the diagnostic reasoning process.
Limitations
We interviewed residents from a single pediatric training program with ubiquitous use of clinical pathways, and focused on an inpatient care setting.
Bottom Line
We highlight potential educational implications of clinical pathway use and suggest ways in which educators can leverage clinical pathways as frameworks to support the maturation of trainee diagnostic decision-making.
Introduction
Diagnostic reasoning is a foundational clinical skill1 with established, dedicated milestones for internal medicine and pediatric residency training.2 Medical residency traditionally assumes that skills in diagnostic reasoning develop as a matter of course, given rich patient case exposure, meaningful participation in the diagnostic process, and feedback from supervising faculty, diagnostic test results, and patient outcomes.3 Clinical educators enhance development of these skills by probing the underlying diagnostic decision-making4 and encouraging structured reflection.
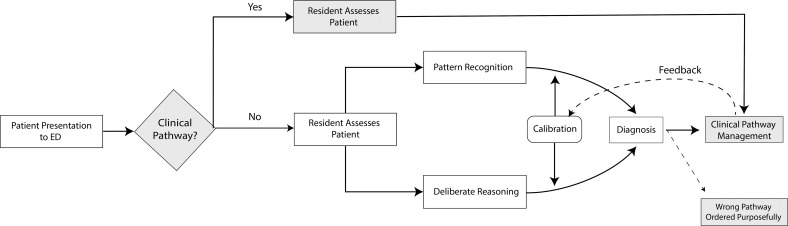
Diagnostic reasoning has been understood using a variety of frameworks, one of which is dual process theory (Figure).5 This theory posits that clinicians employ 2 modes of thinking—a fast, pattern recognition mode for familiar patient presentations and a slow, deliberate mode when facing new, unusual, or complex patient presentations.5,6 Clinicians may iteratively transition to fast thinking through repeated exposures that allow them to refine “illness scripts” and distinguish between conditions with similar presentations.7-12
Figure.
Diagnostic Process Model With Incorporation of Clinical Pathways
Note: Dual Process Theory adapted from Ely et al.5 Overview of the diagnostic process for residents when approaching patients with and without applicable clinical pathways. When clinical pathways are not applicable, residents utilize either a fast thinking (pattern recognition) for familiar patient presentations or slow thinking (deliberate reasoning) for the unfamiliar in an iterative manner (calibration). When clinical pathways are applicable, residents rely on diagnostic decision-making from preceding clinicians and utilize the selected clinical pathway for management decisions without going through either mode of diagnostic thinking.
Recent trends in health care delivery, aimed to promote evidence-based patient care with diagnostic and treatment recommendations, have introduced challenges to a more traditional process of diagnostic reasoning development. In particular, concerns have been raised about the impact of “clinical pathways” on the ways in which residents elicit, synthesize, and communicate key information during patient encounters.13-19 Clinical pathways guide clinicians in the standardized evaluation and management of patients with certain diagnoses or presentations.20 Clinical pathways can include diagnostic and management guidance. Prior literature has explored the positive impact of clinical pathways on resident learners, demonstrating improved task completion21-24 and educational benefits through prompting physicians to educate themselves on the latest evidence or guiding novice physicians to prioritize certain history points.20,25,26 However, as pathways have gained traction, educators at our institution expressed concern that clinical pathways may impact the development of skills in diagnostic reasoning among pediatric trainees by oversimplifying the selection of a pathway for a predetermined diagnosis and over-scripting the associated management decisions of common conditions such that residents and fellows do not engage with the diagnostic aspects of pathways.
Motivated by local concerns raised about the tension between diagnostic reasoning development and changes toward high efficiency clinical practice models, we asked, “How do residents perceive the tradeoffs between clinical pathways and diagnostic reasoning?”
Methods
Setting and Participants
We recruited participants from a large pediatric residency program at a freestanding children's hospital with more than 180 open access clinical pathways.27 Institutionally, our pathways are conceptualized as “structured plans of care that translate guidelines and/or evidence into localized infrastructure and processes [by detailing] a protocol, algorithm, or other inventory of actions…to provide guidance on the evaluation and management of given chief complaints, diagnoses, or clinical processes.”27 Local pathways exist for most common pediatric conditions across the care continuum and are associated with note templates and interprofessional care tools (for physicians, triage nurses, respiratory therapists, bedside registered nurses, etc).
Residents are introduced to pathways as a part of routine clinical care as they admit, care for, document about, and round on patients. For instance, for children admitted with suspected cellulitis/abscess, the clinical pathway28 specifies pertinent history and physical examination findings, strategies for distinguishing cellulitis from inflammation associated with subcutaneous abscess, definitions of various forms of skin infection, antibiotic recommendations, considerations for subspeciality consultation, suggestions about how to gauge clinical improvement, and next steps for evaluation in the case of insufficient improvement. The pathway can be associated with an order set, nursing protocols, patient education, and discharge instructions. Evidence behind the recommendations is cited within the pathway.
We recruited senior pediatric residents via email invitations to participate in 45- to 60-minute, semi-structured interviews. All senior residents who were assigned to one inpatient general pediatric service over the course of the study period were included in the study. Interns or residents who were not assigned to the selected service were excluded. Although residents may receive exposure to clinical pathways from a variety of settings, including ambulatory, emergency department, or critical care units, we purposefully sampled senior residents from a high-volume general pediatric service to target residents who likely had recent exposure to inpatient clinical pathways and to gain perspectives of residents who are farther along in the transition from novice to expert.1 Residents participated voluntarily and without an incentive in the interviews; they gave written consent prior to the interviews.
Study Design
We used a basic interpretive qualitative approach29 to help close a gap in our understanding of diagnostic reasoning in the context of clinical pathways and to address local concerns in our graduate medical education (GME) programs. This approach is similar to other qualitative approaches in that researchers seek to understand how participants make sense of a phenomenon or process, meaning is mediated through the researchers-as-instrument, data are analyzed inductively, and findings are largely descriptive.29 But a basic interpretive qualitative approach differs from other approaches in that it is not firmly rooted in a single disciplinary tradition.
Interview Structure
We developed interview guides informed by 2 of our study team members' experiences as former residents from the training program with exposure to clinical pathways (M.C., I.R.R.) and an existing dual process framework for diagnostic reasoning.5,7,9,30 We designed interview questions to probe for knowledge requirements for expertise in cognitive tasks.31 Pilot interviews were conducted by M.C. and I.R.R. with 3 pediatric residents, resulting in changes to the sequence and clarity of the interview questions (online supplementary data). M.C. and I.R.R. jointly conducted the first 2 interviews to promote consistency in interview style. Thereafter, they conducted in-person, one-on-one interviews outside the main hospital premises to increase privacy during the interview and to promote equanimity between the interviewers (attendings) and the participants (residents). Interviews were audio-recorded, professionally transcribed, and de-identified after transcription.
Data Analysis
We managed data using NVivo 12 software (QSR International, Burlington, MA).32 M.C. and I.R.R. reviewed the first 3 transcripts. They created codes deductively based on dual process theory,5 and added inductively created codes that conceptually extend theories of diagnostic reasoning development.33 Data were analyzed by M.C., I.R.R., and C.B.C. using principles of directed content analysis,34 meaning that coded data were organized into themes derived from the dual process theory framework.7,35 We iteratively reviewed codes and resolved any discrepancies through consensus during group discussion. Data collection and data analysis were iterative processes, so that initial themes could be interrogated in subsequent interviews. M.C. and I.R.R. continued interviews until they were no longer creating new codes from incoming data. Sufficiency36 (ie, when no new ideas or insights related to pathways and diagnosis were introduced) occurred after completion of the first 7 interviews; 2 additional interviews were conducted as a check on the themes we had identified. Member checking with 2 chief residents was performed during the final stage of data analysis to crosscheck our approach; our findings resonated with their experiences.
Managing Reflexivity
Our team included individuals with advanced training and experience in medical education (M.C., H.A., D.F.B.), clinical informatics (I.R.R., N.M., C.P.B.), and diagnostic excellence (C.B.C., I.R.R.). M.C. and I.R.R. conducted interviews and led the coding. They are graduates of the pediatric residency program at the study institution, and as such, approached the study reflexively given some preconceived notions of clinical pathway use. M.C., I.R.R., and N.M. have participated in clinical pathway development and are sensitized to the element of diagnostic fit related to pathways. Finally, M.C., I.R.R., N.M., and C.P.B. are first and foremost pediatricians who applied firsthand knowledge of clinical pathway use. To hold ourselves accountable and check the trustworthiness of the data, we were careful to build on existing theory, to reach data sufficiency,36 and to member check by reviewing study findings with current chief residents.
This study was reviewed by the Institutional Review Board at the Children's Hospital of Philadelphia and met criteria for exemption.
Results
During the study period, email invitations were sent to 19 residents, and 9 interviews were completed. Two residents agreed to participate but were ultimately not interviewed due to reaching sufficiency of the data set and the interruption of clinical rotations and social distancing measures in the setting of the COVID-19 pandemic; the remaining 8 did not respond to the email invitation. Two (22%) participants were second-year residents who were interviewed toward the end of the academic year, and 7 (78%) were third-year residents.
Overall, residents demonstrated a shared understanding of the definition of clinical pathways and similar descriptions of pathway use. Residents used clinical pathways when evaluating patients in the emergency department, as part of the admission process for patients admitted to inpatient units from the emergency department, and in discussion of patients on clinical rounds.
Our analysis identified several key themes. When describing ways that pathways are incorporated into clinical practice, residents cited pathways as important sources of management information and as tools to access certain assessments or treatment protocols. When discussing the influence of pathway use on diagnostic reasoning, residents identified clinical pathways as both a hindrance to and a facilitator of skill development in diagnostic reasoning.
Pathways Were Used as Information References to Guide Management and Treatment, Not Diagnostic Decision-Making Aids
Residents unanimously described clinical pathways as reliable, available, up-to-date sources of medical knowledge or information, rather than tools to guide diagnostic reasoning. They noted that because pathways serve as readily available online repositories of information, they do not memorize specific details regarding dosing intervals or durations of treatment:
Pathways and order sets are great…because there's less time spent thinking about where I should find this information…I'm like, ‘Yeah. Okay. Yep. Vancomycin. Wait. What's the dose? And, what's the frequency?'…I feel like the things that I would have otherwise been just good at looking up and doing repetitively and then sort of learning and knowing concretely. (R1)
Some residents explicitly noted that they reference only the management details in the pathway, as opposed to the embedded diagnostic algorithm (Table). Despite a distinction between practical clinical pathway use and opportunities to practice pattern recognition or deliberate reasoning, many residents described utilizing pathways as a structured guide for teaching medical students or interns. In particular, they felt pathways were especially useful to teach more novice residents and medical students about disease processes and management frameworks.
Table.
Additional Illustrative Quotes From Residents Regarding the Role of Pathways in Formulating Diagnoses
| Theme | Quote |
| Pathways Were Used as Information References to Guide Management and Treatment, Not Diagnostic Decision-Making Aids | |
| Pathways as resources | “The pathways were very new for the oncoming interns, and it was a helpful way to start to frame particular cases for them and also help teach about available resources. [For instance] if you have a [patient] who's coming in with febrile UTI, where do you go to find out which antibiotics? For how long [would you treat]? When would you do IV, when would you do PO?... it was nice to give them a resource to then turn back to again and again as these cases come. I don't think it's quite as helpful in the stage before that when you're really trying to develop your differential or in an undifferentiated patient.” (R4) |
| Pathways, as Tools for Efficient Treatment, Are Applied Even When the Patient Is Not Believed to Fit the Diagnostic Criteria | |
| Management reasoning | “Nobody was particularly comfortable with a definitive diagnosis of asthma when she arrived on the floor because her story was atypical, but I think you could still put someone on a pathway even in the setting of that uncertainty because that's the therapy that you're pursuing at that point in time.” (R4) |
| Clinical Pathways Can Negatively Impact Development of Diagnostic Reasoning Skills by Distancing Residents From the Diagnostic Process and May Introduce Cognitive Bias | |
| Premature closure | “I had one patient who came in and was triaged in the emergency department as a kid who had a focal weakness, a focal deficit, and everybody got really nervous that this was stroke. And so, we had this discussion outside of the room before ever seeing the patient like, “Who do we need to call” and “Where do they fall in the pathway,” and we hadn't even seen the patient yet…it just wasn't a natural thing for someone to just step in the room and do the neurologic examination and verify that there was a focal weakness and then move from there. And so, I think we are—I think we just are really quick to jump to pathways.” (R3) |
| “The downsides are that I do worry that people become dependent on it, um, and not every case sort of fits into a pathway, but when you're used to using a pathway for 60%+ of what we see in pediatrics, you worry a little bit that you will be accustomed to that and try to fit things into a pathway that they're not, and I think I've seen cases of that taking care of patients.” (R7) | |
| Diagnostic momentum | “You just kind of—you get kind of lodged in one way of thinking about things, like ‘This is asthma, this is only asthma so we're gonna treat it like asthma.'” (R8) |
| “These kids are put on autopilot on these pathways, and it really—I find it to be very frustrating because we forget to think about what we're doing.” (R1) | |
| Clinical Pathways Can Positively Impact Diagnostic Reasoning Skills by Providing Opportunity and Scaffolding for Diagnostic Calibration | |
| Forward planning (knowing what to expect) | “We only really start talking about pathway fit when it's not going according to plan, and you start to have setbacks or start to you know, need more escalation, more support than you're used to, or you know, you're not getting to a point of success that you otherwise would have thought you'd be getting to. And so, I think that that's one of the most common spots where we start to say, ‘Is this the right approach for this kid?'” (R3) |
| Monitoring | “But I would say that, more often than not, I've continued the pathway for the first 24 or 36 hours, and it's only as you're kind of pushing into their course and realizing they actually need something a little bit different at this stage, that I've taken kids off [pathway].” (R4) |
Residents used pathways as an efficient means of deciding on treatments and next steps in management. This was invoked particularly for medications such as antibiotics, laboratory tests, and next steps in management that would serve as a reference for the plan of action on clinical rounds. Senior residents were cognizant of reliance on pathway recommendations without an underlying mastery of the content by more novice trainees. A resident described this phenomenon as:
One thing I think is really important for developing physicians, is to create their own plan and rationale, and I see a lot of trainees…like medical students, and like first-month interns, using [pathways] to create their plan and you're like great, so why? But they're like, ‘Oh, I don't know, it's on the pathway.' (R9)
Pathways, as Tools for Efficient Treatment, Are Applied Even When the Patient Is Not Believed to Fit the Diagnostic Criteria
Multiple residents expressed that, in fact, the specific diagnosis associated with the pathway was not as important in selecting a pathway as obtaining the order sets and protocols associated with the pathway. One shared candidly:
I think less about what their, like, actual underlying pathology is and more about how I can get the, like, respiratory exams and medications delivered. (R2)
In other words, because patients on a designated pathway received particular treatments in a protocolized manner, the resident selected a pathway based on the treatment recommendations associated with the pathway rather than the diagnosis. This was particularly true for respiratory conditions; most residents described initiation of a pathway order set for a patient to obtain a specific treatment protocol even though they did not believe the patient fit the diagnostic criteria for the protocol (Table).
One recurrent way in which pathways were used was for distributing patient assessments across the interdisciplinary team. As one resident explained:
There's a ventilator wean pathway now that…takes a lot of the grunt work and the hourly assessments and those things away from the resident and puts them on other providers. (R3)
Such collaborations with interprofessional team members allowed for timely, standardized, and team-based care; however, residents expressed some ambivalence about not engaging personally in the routine, frequent, bedside patient evaluation for common conditions.
Clinical Pathways Can Negatively Impact Development of Diagnostic Reasoning Skills by Distancing Residents From the Diagnostic Process and May Introduce Cognitive Bias
Residents felt that the frequent use of clinical pathways meant that they were entering the patient encounter with a diagnosis established by a preceding clinician and following a standard protocol for management and treatment, and therefore not participating in the deliberate reasoning process (Figure). As one resident stated:
There are some patients who come into the hospital without diagnoses, and we work on teasing those things out. But the emergency department is where the majority of our diagnoses are made and then come up on a pathway. And we don't really rethink those diagnoses. We don't really rethink those clinical assessments. We trust what a provider has done before us, and sometimes we get that wrong. (R3)
Residents stated that their role was generally to facilitate treatment and reassessment, rather than form an initial diagnosis. Residents described bypassing portions of the diagnostic process (Figure), and primarily interacting with a pathway diagnosis after a preceding physician had completed the illness script selection. Multiple residents described examples of potential biases such as premature closure or diagnostic momentum that they felt were imparted by the use of clinical pathways (Table).
Clinical Pathways Can Positively Impact Diagnostic Reasoning Skills by Providing Opportunity and Scaffolding for Diagnostic Calibration
The framework provided by a clinical pathway allowed for clear delineation of the expected clinical trajectory, and was, therefore, described by residents as being helpful in identifying patients with an element of uncertainty:
I've definitely taken kids off of the…pathway because I feel like they're not quite fitting the mold. Whether because their course is a little bit more prolonged or their picture is a little bit less clear…. (R4)
The pathway here is likened to the feedback portion of the diagnostic process (Figure), as the resident describes using deviations from the anticipated patient course supplied by the clinical pathway to reconsider the diagnostic fit. Pathways were described as a structure to evaluate a patient's clinical status and scaffolding for understanding of illnesses that allowed more senior residents to identify patients who were not evolving typically:
By the end of 3 years, you're like, ‘Not only do I know the algorithm of the pathway, but I know the data and I know maybe, like, how to think about it a little bit differently when the kid doesn't fit this perfectly.' (R1)
All interviewed residents described scenarios where they started or continued a patient on a clinical pathway and delayed reconsideration of the diagnosis until prompted to do so by an attending physician, another member of the care team such as a respiratory therapist, or in the setting of a patient's clinical decompensation. This external trigger was required to restart the diagnostic process (Table). Many residents described feeling removed from the calibration step of the diagnostic process (Figure), noting that calibration and reassessment of diagnosis occurs “at the bedside,” or through real-time patient evaluation.
Discussion
Our study illustrates the ways in which clinical pathway use influences diagnostic reasoning processes of pediatric residents at a single academic, quaternary care institution. Residents described ways in which clinical pathways impact the practice and development of skills in diagnostic reasoning. We identified certain areas of vulnerability related to skill development stemming from the use of clinical pathways that can be addressed by educators.
Most notably, we found that the use of clinical pathways distanced residents from deliberate diagnostic reasoning, which may affect the development of diagnostic reasoning skills, in particular the refinement of illness scripts and script selection.10,37,38 However, residents also described using clinical pathways as benchmarks for the expected clinical course, allowing them to identify deviations that prompted reconsideration and calibration of the initial diagnosis.39 Interacting with clinical pathways in this way illustrates the cognitive toggling between more automatic (Type I) for established diagnoses and deliberate (Type II) thinking in unfamiliar cases.40 The introduction of uncertainty allows residents to engage in the diagnostic process, and creates the opportunity to recognize and acknowledge discomfort, practice pattern recognition, as well as consider available resources and expound upon medical knowledge that underpins clinical decision-making.26,41,42
Residents described that they typically encountered patients who were already established with a diagnosis on a clinical pathway from the emergency department or intensive care unit, and that they did not routinely or systematically assess the accuracy of the pathway diagnosis. This may be consistent with prior work showing that the use of clinical pathways can lead to tunnel vision and cognitive bias related to premature closure and diagnostic momentum.20 However, we saw that residents use pathways primarily as efficiency tools, to access order sets and maximize workflow without necessarily being bound to a particular diagnosis, which may be more akin to management reasoning, that is directly affected by the context of high volume, high turnover clinical services.43
There may be an opportunity to change resident perceptions of a single “correct” diagnosis (whether it be a label defined by initiation of a clinical pathway or a diagnosis carried forward by physician communication between settings of the hospital care system). Educators can alternatively support the concept of making a diagnosis an iterative, evolving process.26,41,44 Clinical pathways can be leveraged to prompt structured reflection and recognition of diagnostic uncertainty.41,42,45 There are opportunities to develop self-monitoring cues via pathway “on-ramps” and “off-ramps” to more clearly designate pathway appropriateness at various points throughout the clinical course. Faculty can also guide residents to verbalize their diagnostic reasoning out loud on rounds, especially for undifferentiated patients, to determine a resident's ability to identify an illness script and select the most likely diagnostic hypothesis.7
Another common interaction with clinical pathways by residents in our study was as a point of reference for management. This is consistent with literature suggesting that pathways have educational benefit as a source for knowledge25 and that knowledge-based interventions can support diagnostic reasoning.46 The content and embedded references in clinical pathways can be used as evidence-based teaching frameworks, as described by the residents in our study, or as resources to build illness script libraries and script selection tools. Clinical pathways can also facilitate teaching by faculty, offering unique opportunities to develop the knowledge base for multiple learner levels simultaneously. For example, an intern may be referred to clinical pathway criteria to develop illness scripts for a diagnosis or to pathway order sets to learn about medication selection and dosing, whereas a senior resident can be tasked with exploring the primary literature and expert guidelines supporting the pathway management recommendations.
Our findings must be considered in light of the limitations of our approach. First, we interviewed residents from a single pediatric training program with ubiquitous use of clinical pathways, and we focused on inpatient care. Findings may look different in other clinical settings, although several study findings may be relevant across other institutions or disciplines. Second, participation for this study was opt-in, which may present an element of selection bias to our interview responses and overall low sample size. Third, by virtue of a basic interpretive qualitative approach, our findings are not necessarily high-level interpretation, but rather, descriptive in nature. This is not necessarily a limitation but does bound the assumptions we are able to draw from our data. We have incorporated several strategies to support trustworthiness of our analysis including reflection on our reflexivity, member checking, peer review, and a robust description of the richness of our data.
Next steps for our institution include adapting strategies to promote development of skills in diagnostic reasoning that incorporate clinical pathways and considering opportunities to explicitly consider resident decision-making in pathway development. We also intend to promote faculty development in utilization of scripts in the setting of diagnostic uncertainty (eg, for use during emergency department rotations and inpatient clinical rounds).
Conclusions
Clinical pathways are important tools for provision of efficient, evidence-based care. The use of pathways supports management decisions but may allow residents to bypass critical points in the diagnostic reasoning process. We highlight opportunities for medical educators to leverage clinical pathways as frameworks to support the maturation of trainee diagnostic decision-making.
Supplementary Material
Acknowledgments
The authors would like to thank the residents who participated in the interviews for this project.
Funding Statement
Funding: The authors report no external funding source for this study.
Footnotes
Conflict of interest: The authors declare they have no competing interests.
The abstract was previously presented at the Pediatric Academic Society National Meeting, Baltimore, MD, April 24-May 1, 2019, and the American Academy of Pediatrics National Clinical Exhibition, New Orleans, LA, October 25-29, 2019.
References
- 1.Humphrey-Murto S, Wood TJ, Ross S, et al. Assessment pearls for competency-based medical education. J Grad Med Educ . 2017;9(6):688–691. doi: 10.4300/JGME-D-17-00365.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. Milestones by Specialty Accessed October 5. 2021. https://acgme.org/what-we-do/accreditation/milestones/milestones-by-specialty/
- 3.de Jong J, Visser M, Van Dijk N, van der Vleuten C, Wieringa-de Waard M. A systematic review of the relationship between patient mix and learning in work-based clinical settings. A BEME systematic review: BEME Guide No. 24. Med Teach . 2013;35(6):e1181–e1196. doi: 10.3109/0142159X.2013.797570. [DOI] [PubMed] [Google Scholar]
- 4.Rencic J. Twelve tips for teaching expertise in clinical reasoning. Med Teach . 2011;33(11):887–892. doi: 10.3109/0142159X.2011.558142. [DOI] [PubMed] [Google Scholar]
- 5.Ely JW, Graber ML, Croskerry P. Checklists to reduce diagnostic errors. Acad Med . 2011;86(3):307–313. doi: 10.1097/ACM.0b013e31820824cd. [DOI] [PubMed] [Google Scholar]
- 6.Musgrove JL, Morris J, Estrada CA, Kraemer RR. Clinical reasoning terms included in clinical problem solving exercises? J Grad Med Educ . 2016;8(2):180–184. doi: 10.4300/JGME-D-15-00411.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowen JL. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med . 2006;355(21):2217–2225. doi: 10.1056/NEJMra054782. [DOI] [PubMed] [Google Scholar]
- 8.Pelaccia T, Tardif J, Triby E, Charlin B. An analysis of clinical reasoning through a recent and comprehensive approach the dualprocess theory Med Educ Online. 16103402/meov16i05890. 2011. [DOI] [PMC free article] [PubMed]
- 9.Boshuizen HPA, Schmidt HG. On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novices. Cogn Sci . 1992;16(2):153–184. doi: 10.1016/0364-0213(92)90022-M. [DOI] [Google Scholar]
- 10.Yazdani S, Hoseini Abardeh M. Five decades of research and theorization on clinical reasoning: a critical review. Adv Med Educ Pract . 2019;10:703–716. doi: 10.2147/AMEP.S213492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Branson CF, Williams M, Chan TM, et al. Improving diagnostic performance through feedback: the diagnosis learning cycle. BMJ Qual Saf . 2021;30(12):1002–1009. doi: 10.1136/bmjqs-2020-012456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eva KW. What every teacher needs to know about clinical reasoning. Med Educ . 2005;39(1):98–106. doi: 10.1111/j.1365-2929.2004.01972.x. [DOI] [PubMed] [Google Scholar]
- 13.Chi J, Artandi M, Kugler J, et al. The five-minute moment. Am J Med . 2016;129(8):792–795. doi: 10.1016/j.amjmed.2016.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Patel VL, Kushniruk AW, Yang S, Yale JF. Impact of a computer-based patient record system on data collection, knowledge organization, and reasoning. J Am Med Inform Assoc . 2000;7(6):569–585. doi: 10.1136/jamia.2000.0070569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varpio L, Day K, Elliot-Miller P, et al. The impact of adopting EHRs: how losing connectivity affects clinical reasoning. Med Educ . 2015;49(5):476–486. doi: 10.1111/medu.12665. [DOI] [PubMed] [Google Scholar]
- 16.Varpio L, Rashotte J, Day K, King J, Kuziemsky C, Parush A. The EHR and building the patient's story: a qualitative investigation of how EHR use obstructs a vital clinical activity. Int J Med Inf . 2015;84(12):1019–1028. doi: 10.1016/j.ijmedinf.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Tierney MJ, Pageler NM, Kahana M, Pantaleoni JL, Longhurst CA. Medical education in the electronic medical record (EMR) era: benefits, challenges, and future directions. Acad Med . 2013;88(6):748–752. doi: 10.1097/ACM.0b013e3182905ceb. [DOI] [PubMed] [Google Scholar]
- 18.Peled JU, Sagher O, Morrow JB, Dobbie AE. Do electronic health records help or hinder medical education? PLoS Med . 2009;6(5):e1000069. doi: 10.1371/journal.pmed.1000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quinn M, Forman J, Harrod M, et al. Electronic health records, communication, and data sharing: challenges and opportunities for improving the diagnostic process. Diagn Berl Ger . 2019;6(3):241–248. doi: 10.1515/dx-2018-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O'Hara K, Tanverdi M, Reich J, Scudamore DD, Tyler A, Bakel LA. Qualitative study to understand pediatric hospitalists and emergency medicine physicians' perspectives of clinical pathways. Pediatr Qual Saf . 2020;5(2):e270. doi: 10.1097/pq9.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hassan ISA. Cognitive schemes and strategies in diagnostic and therapeutic decision making: a primer for trainees. Perspect Med Educ . 2013;2(5-6):321–331. doi: 10.1007/s40037-013-0070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kellogg KM, Fairbanks RJ. Approaching fatigue and error in emergency medicine: narrowing the gap between work as imagined and work as really done. Ann Emerg Med . 2018;72(2):181–183. doi: 10.1016/j.annemergmed.2018.02.030. [DOI] [PubMed] [Google Scholar]
- 23.Farias M, Friedman KG, Lock JE, Rathod RH. Gathering and learning from relevant clinical data: a new framework. Acad Med . 2015;90(2):143–148. doi: 10.1097/ACM.0000000000000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA . 1998;280(15):1339–1346. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 25.Talib HJ, Lax Y, Reznik M. The impact of a clinical asthma pathway on resident education. BioMed Res Int . 2018;2018:5472876. doi: 10.1155/2018/5472876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chan TM, Mercuri M, Turcotte M, Gardiner E, Sherbino J, de Wit K. Making decisions in the era of the clinical decision rule: how emergency physicians use clinical decision rules. Acad Med . 2020;95(8):1230–1237. doi: 10.1097/ACM.0000000000003098. [DOI] [PubMed] [Google Scholar]
- 27.The Children's Hospital of Philadelphia About the Clinical Pathways Accessed February 24. 2022. https://www.chop.edu/pathways/about .
- 28.The Children's Hospital of Philadelphia Cellulitis/Abscess Clinical Pathway—Inpatient Accessed October 26. 2021. https://www.chop.edu/clinical-pathway/cellulitis-abscess-suspected-inpatient-care-clinical-pathway .
- 29.Merriam SB. Qualitative Research and Case Study Applications in Education . Hoboken, NJ: Wiley & Sons Inc; 1998. [Google Scholar]
- 30.Dhaliwal G, Ilgen J. Clinical reasoning: talk the talk or just walk the walk? J Grad Med Educ . 2016;8(2):274–276. doi: 10.4300/JGME-D-16-00073.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klein G, Militello L. How Professionals Make Decisions 1st ed. Boca Raton, FL: CRC Press; 2004. The Knowledge Audit as a Method for Cognitive Task Analysis; pp. 335–342. [Google Scholar]
- 32.Sbaraini A, Carter SM, Evans RW, Blinkhorn A. How to do a grounded theory study: a worked example of a study of dental practices. BMC Med Res Methodol . 2011;11(1):128. doi: 10.1186/1471-2288-11-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hsieh H, Shannon S. Three approaches to qualitative content analysis. Qual Health Res . 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 34.Potter WJ, Levine-Donnerstein D. Rethinking validity and reliability in content analysis. J Appl Commun Res . 1999;27(3):258–284. doi: 10.1080/00909889909365539. [DOI] [Google Scholar]
- 35.Sandhu H, Carpenter C, Freeman K, Nabors SG, Olson A. Clinical decisionmaking: opening the black box of cognitive reasoning. Ann Emerg Med . 2006;48(6):713–719. doi: 10.1016/j.annemergmed.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 36.LaDonna KA, Artino AR, Balmer DF. Beyond the guise of saturation: rigor and qualitative interview data. J Grad Med Educ . 2021;13(5):607–611. doi: 10.4300/JGME-D-21-00752.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yazdani S, Hoseini Abardeh M. A novel model of clinical reasoning: cognitive zipper model. J Adv Med Educ Prof . 2020;8(2):61–71. doi: 10.30476/jamp.2020.82230.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schiff GD. Minimizing diagnostic error: the importance of follow-up and feedback. Am J Med . 2008;121(suppl 5):38–42. doi: 10.1016/j.amjmed.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Cristancho S, Lingard L, Regehr G. From problem solving to problem definition: scrutinizing the complex nature of clinical practice. Perspect Med Educ . 2017;6(1):54–57. doi: 10.1007/s40037-016-0314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jacoby LL. A process dissociation framework: separating automatic from intentional uses of memory. J Mem Lang . 1991;30(5):513–541. doi: 10.1016/0749-596X(91)90025-F. [DOI] [Google Scholar]
- 41.Ilgen JS, Eva KW, de Bruin A, Cook DA, Regehr G. Comfort with uncertainty: reframing our conceptions of how clinicians navigate complex clinical situations. Adv Health Sci Educ Theory Pract . 2019;24(4):797–809. doi: 10.1007/s10459-018-9859-5. [DOI] [PubMed] [Google Scholar]
- 42.Ilgen JS, Teunissen PW, de Bruin ABH, Bowen JL, Regehr G. Warning bells: how clinicians leverage their discomfort to manage moments of uncertainty. Med Educ . 2021;55(2):233–241. doi: 10.1111/medu.14304. [DOI] [PubMed] [Google Scholar]
- 43.Cook DA, Durning SJ, Sherbino J, Gruppen LD. Management reasoning: implications for health professions educators and a research agenda. Acad Med . 2019;94(9):1310–1316. doi: 10.1097/ACM.0000000000002768. [DOI] [PubMed] [Google Scholar]
- 44.Ilgen JS, Eva KW, Regehr G. What's in a label? Is diagnosis the start or the end of clinical reasoning? J Gen Intern Med. 2016;31(4):435–437. doi: 10.1007/s11606-016-3592-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cooke S, Lemay JF. Transforming medical assessment: integrating uncertainty into the evaluation of clinical reasoning in medical education. Acad Med . 2017;92(6):746–751. doi: 10.1097/ACM.0000000000001559. [DOI] [PubMed] [Google Scholar]
- 46.Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med . 2017;92(1):23–30. doi: 10.1097/ACM.0000000000001421. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.