Abstract
Background
Intercostal chest drain (ICD) insertion is a skill that medical trainees lack confidence in performing. This study explores the impact of a national programme of Simulation-Based Mastery Learning (SBML) on procedural confidence, including the impact of time intervals between booster sessions and interim clinical experience.
Methods
Internal Medicine Trainees in Scotland were surveyed about confidence and clinical experience with ICD insertion before and immediately after SBML and booster session. Data were matched and analysed using paired sample t-tests. Short interval and long interval groups were compared using Student’s unpaired t-test. The impact of interim clinical experience was assessed using Analysis of Variance.
Results
Mean confidence in ICD insertion rose following SBML, fell between initial and booster session, and increased again following booster session (P = < 0.001). 33 of 74 trainees had successfully inserted an ICD between sessions. Fall in confidence was unaffected by the time interval between training sessions, but was mitigated by interim clinical experience.
Conclusions
SBML boosts trainee confidence in ICD insertion. However, there is evidence of confidence decay, possibly due to a lack of clinical experience between sessions. More research is needed to explore barriers to transfer of skills from simulated to real-world environments.
Keywords: Simulation-based mastery learning, Chest drain, Transition from simulation to practice
Background
Intercostal chest drain (ICD) insertion is a potentially life-saving, complex procedural intervention, usually performed in an acute hospital environment. ICD insertion can have significant adverse outcomes including iatrogenic pneumo/haemothorax, infection, organ puncture and, rarely, death [1]. Previous studies have suggested that doctors in training are becoming less competent and less confident at inserting ICDs [2–6]. If these skills are taught but unused, they will decay over time [7]. ‘Skill decay’ is defined as the degradation or loss of trained or acquired skills, after a period of non-use [7]; with greater time intervals between use associated with greater loss of skill [8]. Given ICD insertion comes with significant risk of complications, understanding how best to train doctors in becoming competent and confident in this skill is key for medical educators.
The relationship between confidence and competence is complex, but both are important in the acquisition of new skills [9]. Stewart et al. suggest that competence is defined by what one is able to do (incorporating an element of external validation of ability), while confidence can be defined as a belief in one’s ability to complete a task (incorporating one’s level of anxiety) [10]. There is also the related motivational construct of self-efficacy, the judgements that trainees make about their capabilities, [11] which is sometimes referred to as task-specific self-confidence [12]. Ideally, confidence and competence should align such that the more competent one is, the more confidence one has. Although many have argued that confidence or self-efficacy can be used as a proxy for performance, [11, 13–15] previous studies have shown that confidence and competence correlate poorly [16–19]. Despite this, confidence remains important. Confidence impacts willingness to undertake procedures [2] with a lack of confidence leading to avoidance of practising technical skills in the workplace [20]. There is also evidence that self-efficacy positively influences the successful transfer of training of skills to the workplace [21]. It is therefore crucial that doctors in training develop sufficient confidence in essential procedures in order to seek opportunities to practice their skills, which should ultimately lead to improved competence and better patient outcomes.
Simulation-based mastery learning (SBML) is a robust, evidence-based teaching methodology designed to improve the acquisition of procedural skills, with the aim of supporting all learners to achieve an agreed standard [22, 23]. The premise of SBML is that all learners can achieve the same level of competence, but that different time periods or repeated application of deliberate practice may be required [22]. It is well evidenced that SBML has significant advantages for acquiring competence in new skills, as it can ensure a standardisation of experience, provide a learning environment with no risk to patients, provide safety for the novice learner, and bridge the gap between clinically available opportunities and participants’ learning needs [22]. One-off simulation sessions have been shown to improve competence, confidence, and reduce ICD insertion complication rates [24–26].
However, after such simulation sessions, skill decay inevitably occurs. A previous meta-analysis of skill decay literature showed substantial loss of skill after 365 days of non-use [7]. More recent studies have suggested that skill decay can begin much earlier than previously thought [27–30]. SBML booster sessions can be utilised to mitigate skill decay, [31–33] but debate remains as to the best timing of such sessions. In addition, there is a lack of research exploring the decay of confidence in procedural skills following SBML, which could influence trainees’ willingness to undertake procedures in the workplace [2]. Confidence decay is expected after non-use, but some trainees will have the opportunity to transfer procedural skills to the workplace. The impact of such clinical exposure between SBML sessions on confidence is underexplored and could influence training needs. A better understanding of confidence decay following SBML sessions could inform the need for and timing of booster sessions. Given the evidence of substantial skill decay after 12 months, we aimed to explore whether confidence decays after a similar interval, and to determine the impact of clinical exposure in the intervening period.
Purpose of the study
We aimed to explore the relationship between SBML and confidence in ICD insertion, specifically:
What impact (if any) does SBML have on ICD insertion confidence?
What impact (if any) does a booster session have on ICD insertion confidence?
Is there a difference in level of confidence decay in ICD insertion between short interval to booster (< 12 months) versus long interval to booster (12 months or more) groups?
What is the impact (if any) of practising in the workplace on ICD insertion confidence decay? Specifically:
a. Does decay of confidence differ when participants have clinical experience in the workplace have a long or short interval to booster, versus if they have no clinical experience?
b. Is there a relationship between number of successful attempts in the workplace and decay in confidence?
Methods
Context
In the UK, Internal Medicine Training (IMT) is a three-year national programme for doctors who have at least two years of post-graduation clinical experience. Those wishing to apply for higher level training in a medical speciality must complete IMT or prove equivalent competences via an alternative route. IMT in Scotland incorporates a national simulation strategy, which includes a three-day boot camp during the first year of IMT (IMT1), with mixed groups from all four Scottish regions (West, North, East and South-East) hosted at the Scottish Centre for Simulation and Clinical Human Factors. In the second year of the training programme (IMT2) trainees attend a skills day at either the Royal College of Physicians and Surgeons of Glasgow (West and South-East trainees), or Aberdeen Royal Infirmary (North and East trainees), to revisit some of the skills covered at boot camp in IMT1.
The SBML pathway in this context involves study of pre-learning materials and peer assisted deliberate practice, followed by a checklist-based summative assessment to ensure the passing standard is reached [23]. Practical procedures covered using SBML include ICD insertion, lumbar puncture, ascitic drain insertion and central venous access [23]. ICD insertion (guidewire technique) is formally assessed at both IMT1 boot camp and IMT2 skills day, using an identical checklist-based process encompassed within a two hour session. The learning materials used during these training events were created by NHS Lothian and are available on the Medical Education Directorate website [34].
Data collection
Participants completed evaluation questionnaires before and immediately after each of the two training events (IMT1 boot camp and IMT2 skills day), and data was tracked for each participant across both courses. At the time of completing each survey, participants consented to their anonymised data being used for course improvements and research. Pre and post event, participants were asked to consider their clinical practice and answer the following question:
‘How confident are you that you could safely and successfully perform the following procedures under direct supervision (with a consultant at the end of the bed)?’
They were asked to self-rate confidence on a Likert scale from 1 to 7 where 1 = not at all confident and 7 = completely confident. Participants were also asked how many times they had attempted each procedure (successfully and unsuccessfully) in clinical practice (including all supervised or independent attempts), between training events. The time interval between courses for each participant was calculated.
Data analysis
The Scottish national IMT simulation strategy provides one simulation training course per trainee for each training year. However, IMTs can attend any course within that training year, and are currently randomly assigned, leading to variability in time interval between participants attending these courses. As mentioned, previous meta-analysis of skill decay literature has shown substantial loss of skill after 365 days of non-use [7]. We aimed to determine if those who had a less than 12 month interval between training events, had a significant advantage over those with a greater than 12 month interval. This would either support maintaining one intervention per training year, or provide evidence for a need to reform our training programme to incorporate more frequent intervention. Electronic evaluation survey data was collected from participants pre and post both events between August 2019 and May 2021. The relevant data was anonymised by use of participant codes, matched to track self-reported confidence changes across the two events.
Confidence change was calculated by subtracting the post- IMT1 boot camp Likert score for confidence from the pre- IMT2 skills day (booster session) Likert score for confidence. A negative value for confidence change indicated confidence decay. The data was analysed using SPSS (version 14) and Excel (version 2205). The following statistical tests were performed:
Aim 1: Differences in confidence before and after the initial SBML session were compared using a paired samples t-test
Aim 2: Differences in confidence before and after the booster session were compared using a paired samples t-test
Aim 3: We examined change in confidence between the post-initial session score and the pre-booster session score. The confidence decay between short interval (< 12 months) and long interval (> = 12 month) groups were compared using Student’s unpaired t-test
Aim 4a: Confidence decay between short and long interval groups, split by clinical experience of performing ICD insertion in the workplace versus no experience were compared using Analysis of Variance.
Aim 4b: Confidence decay between groups who were successful in ICD insertion in the workplace between the initial course and the booster were compared using Analysis of Variance.
Differences were considered statistically significant if p < 0.01 (5% significance level with a Bonferroni correction for five comparisons).
Results
One hundred and five trainees attended the IMT1 boot camp between August 2019 and January 2020, and 100 trainees subsequently attended the IMT2 skills day between September 2020 and May 2021. Seventy-four participants had complete data sets for the data extracted with regard to ICD insertion, allowing tracking of matched data from IMT1 boot camp to IMT2 skills day. Twenty-six participants were excluded due to incomplete survey responses. This was the only exclusion criterion. Demographic data for the 74 included participants is included below in Table 1.
Table 1.
Demographic data for participants
| Gender | Male | Female | ||
| Trainees | 34 | 40 | ||
| Age range | 24–29 | 30–35 | 36 and over | |
| Trainees | 66 | 7 | 1 | |
| Region | East | North | South East | West |
| Trainees | 8 | 10 | 18 | 38 |
Aims 1 and 2: Impact of SBML and the booster session on confidence
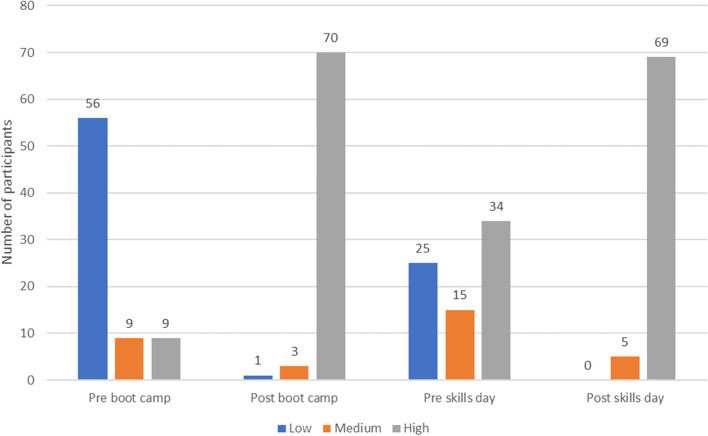
Prior to SBML, the mean score for self-reported confidence in ICD insertion was low (mean of 2.6 out of 7). There was a statistically significant increase (p < 0.001) in mean confidence following the boot camp initial SBML session (from mean confidence 2.6 to 5.9 out of 7). The mean confidence level then decreased following the interval between boot camp (initial) and skills day (booster). The mean self-reported confidence from subsequent skills day data was 4.2 out of 7, rising to 5.9 out of 7 following the session, and this rise was again statistically significant (p < 0.001). This is further exemplified in Fig. 1 which shows a breakdown of self-reported confidence at each stage with responses grouped into low confidence (Likert response 1–3), medium confidence [4] and high confidence [5–7].
Fig. 1.
Number of participants who reported low, medium or high confidence at different stages of their training
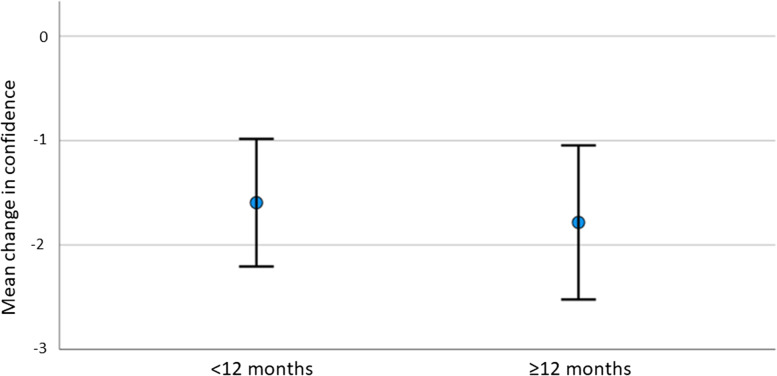
Aim 3: Impact of booster session timing on confidence decay
There was no statistically significant difference (p = 0.69) in confidence decay between groups with a short time interval between the initial SMBL and booster session (confidence decay -1.59) versus groups with a long time interval of > = 12 months (confidence decay -1.78), as depicted in Fig. 2.
Fig. 2.
Confidence decay in groups with a short interval (< 12 months) versus long interval (> = 12 months) between initial session and booster session
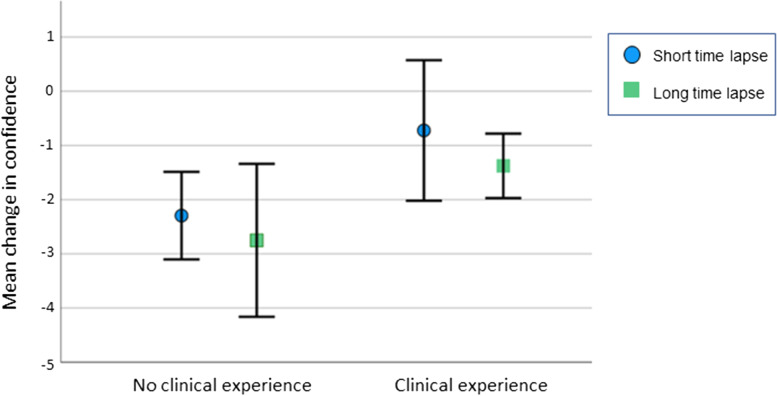
Aim 4a: Confidence decay in short and long interval groups grouped according to level of clinical experience
Figure 3 shows the differences between the four groups. The trend is towards greater confidence decay in the groups with no clinical experience, however within this small study the results are not statistically significant (p = 0.023).
Fig. 3.
Confidence decay according to clinical experience and time interval between initial session and booster session
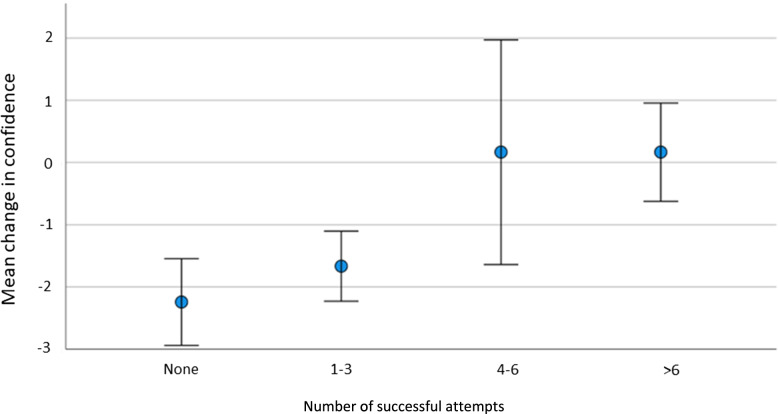
Aim 4b: Relationship between successful clinical attempts between the initial and booster sessions and confidence decay
Fewer than half (44%) of the participants successfully inserted an ICD in clinical practice between the IMT1 boot camp and the IMT2 skills day. The breakdown of number of successful attempts of participants is displayed in Table 2.
Table 2.
Number of successful ICD attempts between initial and booster session
| Number of successful ICD insertion attempts | Number of participants |
|---|---|
| None | 41 |
| 1 -3 | 21 |
| 4—6 | 6 |
| 7—10 | 5 |
| > 10 | 1 |
Confidence decay appeared to be ameliorated by successful ICD insertion attempts in clinical practice between the initial and booster sessions (as shown in Fig. 4), and there was a statistically significant difference within the data (p = 0.003). The dataset was not sufficiently large to assess the number of successful insertions needed to reduce confidence decay, but does show that there is a definite association between higher numbers of successful attempts and reduction in confidence decay.
Fig. 4.
Difference in confidence levels of groups with differing numbers of successful attempts at ICD insertion between the initial and booster training sessions
Only eight participants recorded unsuccessful attempts. Of these, six recorded 1–3 unsuccessful attempts and two recorded 4–6 unsuccessful attempts. Six of those with unsuccessful attempts also recorded successful attempts.Interestingly, the two participants with unsuccessful attempts but no successful attempts did not report a confidence decay.This dataset is too small to draw any conclusions about the effect of unsuccessful attempts on confidence, but it would be an interesting question for a future study.
Discussion
This study explores the impact of a national structured SBML programme on trainee confidence in ICD insertion, and how this is impacted by the time interval between training sessions and intervening clinical practice. This study shows that SBML for ICD insertion improves trainee reported confidence. Mean confidence fell between sessions but was improved with a booster session, with no significant difference in confidence decay if the booster session was less than or more than 12 months after the initial session. Although confidence fell even when trainees had clinical experience in the interim, there was some mitigation of the confidence decay with clinical experience.
These findings are congruent with the extensive evidence basis for the use of SBML, which has been shown to improve participant confidence [15, 22, 24, 35–38]. This longitudinal study adds to the SBML literature by exploring change in confidence over time and shows evidence of confidence decay. The ultimate aim of training interventions is to transfer skills to the workplace and trainees’ confidence in their own abilities to do so is a key factor in the transfer of skills being successful [21]. Although trainees may be deemed competent to perform procedures on a manikin in a skills lab, there are numerous factors in the work environment that can influence skill transfer [39]. If trainees have persistent low self-efficacy for skills they feel they should be confident and competent to perform in their role, then this could lead to discomfort or anxiety [40]. Previous studies have found that internal medicine residents were uncomfortable with bedside medical procedures [40, 41] and, in particular, uncomfortable with the skill of ICD insertion [40]. Training programmes should aim to improve and maintain confidence in essential skills in order to ensure opportunities are sought and a potential cycle of avoidance and further reduced confidence prevented. SBML in this context can boost confidence but how best to maintain this for trainees requires further consideration.
Trainees must have access to clinical opportunities to perform in order to transfer skills to the workplace which, as exemplified in this study, is challenging, particularly for the skill of ICD insertion [39]. This study found significant mitigation of confidence decay for trainees with higher numbers of successful attempts in clinical practice during the intervening period, in keeping with other studies finding that clinical practice increases confidence in ICD insertion [2, 6, 42, 43]. However, less than half of the trainees had successfully inserted an ICD during the interim time interval. It is possible that the COVID-19 pandemic, during which ICD insertion for pneumothorax was classified as an ‘aerosol generating procedure’, requiring enhanced personal protective equipment, may have contributed to the lack of opportunities over the study period. It is possible that the majority of our participants had not reached a “threshold” number of drain insertions which would maintain their confidence [44]. Studies exploring competence have suggested that the number of ICD insertions needed to gain and subsequently maintain competence may be between five and ten per year [3, 44]. The trend within this dataset would suggest that approximately 4–6 may be the threshold to ameliorate confidence decay between sessions. Given the low number of ICD attempts between sessions for our participants, the clinical implications of achieving this number, and therefore maintaining the confidence of each trainee, presents major challenges.
Implications for practice
Unlike the findings in other published literature, [45] time interval between training sessions within the parameters of this study had no significant impact on the degree of confidence loss. Based on these findings, there appears to be no benefit in shortening the time interval between training days to less than one year. This study suggests that, for those considering implementation of a similar SBML training programme, one training session per training year will boost confidence. However, there may be an argument to consider reducing the interval between sessions for trainees who have not had the opportunity to perform ICD insertion in clinical practice. The results of this study add to the evidence for SBML, and support the ongoing use of the IMT2 skills day as a booster session to support confidence in ICD insertion. It raises the question of whether booster session trainee allocations should be based on clinical experience.
Strengths and limitations
This national study tracked participants across two training sessions, using longitudinal data over two years, providing a strong evidence base for reviewing the training programme and altering practice. There are limitations in measuring self-reported confidence as we know this may not correlate well with competence, for example trainees may be over-confident but not competent or a lack of confidence may not reflect lack of competence. However, given all trainees achieved competence during the assessed session, individual self-reported confidence was deemed an important indicator of their self-efficacy in transferring skills to the workplace. It must also be recognised that there are other factors which could influence confidence in performing ICD insertion, such as the precise timing of clinical experience between sessions and supervisor support during such experience, that have not been addressed in this study [39].
Future work
Future work could explore the barriers to transfer of procedural skills to the workplace, including opportunities to perform from trainee, supervisor and organisational perspectives. Recent work has identified factors such as opportunities to perform the procedure clinically and support from supervisors as crucial to facilitating successful transfer [39, 46]. While our results indicate that intervals of 7–20 months between sessions have little impact on trainee confidence, further work is needed to evaluate if shorter intervals of a few months between SBML training interventions maintain confidence or indeed promote transfer to clinical practice. With a larger powered study, the time intervals between sessions could be further subdivided to explore shorter booster session timing impact on confidence. It would also be helpful to assess if findings are similar in relation to other important but infrequently used procedural skills, other than ICD insertion.
Conclusions
This study reinforces the need for SBML and booster sessions for ICD insertion, particularly given the challenges of obtaining clinical exposure for internal medicine trainees. The finding of confidence decay being mitigated by successful attempts in clinical practice between training sessions should be of interest to medical educators involved in the training of important but infrequently used skills. Further research into opportunities to perform in the workplace is needed to establish how best to support trainees transferring this skill into clinical practice in order to maintain confidence.
Acknowledgements
The authors thank all of the trainee participants and all of the faculty involved in the IMT1 boot camp and IMT2 skills days, including staff at the Royal College of Physicians Glasgow, Aberdeen Royal Infirmary and the Scottish Centre for Simulation and Clinical Human Factors.
Abbreviations
- ICD
Intercostal Drain
- IMT
Internal Medicine Training
- SBML
Simulation-Based Mastery Learning
- UK
United Kingdom
Authors’ contributions
JK contributed to the conception and the design of the study, data collection, analysis and interpretation of the data, the initial drafting and revision of the manuscript and led the redrafting of the manuscript for resubmission. EMc led the conception and the design of the study, data collection, analysis and interpretation of the data, and the initial drafting and revision of the manuscript. SAS contributed to the conception and design of the study, data collection, data analysis and the drafting and revision of the paper. SES contributed to the analysis and interpretation of the data, the initial drafting and revision of the paper. JT and VT contributed to the conception and the design of the study, data collection and revision of the paper. All authors (JK, EMc, SAS, SES, JT and VT) approved the final manuscript for publication and have agreed to be accountable for all aspects of the work.
Funding
No funding to declare.
Availability of data and materials
The datasets analysed during the current study are not publicly available as they are part of a larger data set which may be subject to future publication, and contains information that could compromise individual privacy. Data are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval to collect anonymised participant information was granted by the NHS Education for Scotland ethics review board, reference number NES/Res/14/20/Med. Participants were informed that their data may be used in research, and gave their active consent, or had the option to opt out of the survey with no penalty. All data was collected in accordance with UK data processing regulations and guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hooper CE, Welham SA, Maskell NA. Pleural procedures and patient safety: A national BTS audit of practice. Thorax. 2015;70(2):189–191. doi: 10.1136/thoraxjnl-2013-204812. [DOI] [PubMed] [Google Scholar]
- 2.Connick RM, Connick P, Klotsas AE, Tsagkaraki PA, Gkrania-Klotsas E. Procedural confidence in hospital based practitioners: Implications for the training and practice of doctors at all grades. BMC Med Educ. 2009;9(1):1–8. doi: 10.1186/1472-6920-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corcoran JP, Hallifax RJ, Talwar A, Psallidas I, Sykes A, Rahman NM. Intercostal chest drain insertion by general physicians: Attitudes, experience and implications for training, service and patient safety. Postgrad Med J. 2015;91(1075):244–250. doi: 10.1136/postgradmedj-2014-133155. [DOI] [PubMed] [Google Scholar]
- 4.Villanueva C, Doyle M, Parikh R, Manganas C. Patient Safety During Chest Drain Insertion-A Survey of Current Practice. J Patient Saf. 2021;17(3):e115–e120. doi: 10.1097/PTS.0000000000000304. [DOI] [PubMed] [Google Scholar]
- 5.Tasker F, Newbery N, Burr B, Goddard AF. Survey of core medical trainees in the United Kingdom 2013 - Inconsistencies in training experience and competing with service demands. Clin Med J R Coll Physicians London. 2014;14(2):149–156. doi: 10.7861/clinmedicine.14-2-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong CA, Lee O, Kennedy Y, Kenealy H, Hood C, Sivakumaran P, et al. The training, experience, and confidence of junior doctors in performing pleural procedures. N Z Med J. 2009;122(1304):23–32. [PubMed] [Google Scholar]
- 7.Arthur W, Bennett W, Stanush PL, McNelly TL. Factors that influence skill decay and retention: A quantitative review and analysis. Hum Perform. 1998;11(1):57–101. doi: 10.1207/s15327043hup1101_3. [DOI] [Google Scholar]
- 8.Offiah G, Ekpotu LP, Murphy S, Kane D, Gordon A, O’Sullivan M, et al. Evaluation of medical student retention of clinical skills following simulation training. BMC Med Educ. 2019;19(1):1–7. doi: 10.1186/s12909-019-1663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlisle C. Reflecting on levels of confidence and competence in skills acquisition. Med Educ. 2000;34(11):886–887. doi: 10.1046/j.1365-2923.2000.00826.x. [DOI] [PubMed] [Google Scholar]
- 10.Stewart J, O’Halloran C, Barton JR, Singleton SJ, Harrigan P, Spencer J. Clarifying the concepts of confidence and competence to produce appropriate self-evaluation measurement scales. Med Educ. 2000;34(11):903–909. doi: 10.1046/j.1365-2923.2000.00728.x. [DOI] [PubMed] [Google Scholar]
- 11.Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37(2):122–147. doi: 10.1037/0003-066X.37.2.122. [DOI] [Google Scholar]
- 12.Artino AR, Dong T, DeZee KJ, Gilliland WR, Waechter DM, Cruess DF, et al. Development and initial validation of a survey to assess students’ self-efficacy in medical school. Mil Med. 2012;177(SUPPL 1):31–7. doi: 10.7205/MILMED-D-12-00240. [DOI] [PubMed] [Google Scholar]
- 13.Watters C, Reedy G, Ross A, Morgan NJ, Handslip R, Jaye P. Does interprofessional simulation increase self-efficacy: A comparative study. BMJ Open. 2015;5(1):1–7. doi: 10.1136/bmjopen-2014-005472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stajkovic A, Luthans F. Self-efficacy and work-related performance: a meta-analysis. Psychol Bull. 1998;124(2):240–61. doi: 10.1037/0033-2909.124.2.240. [DOI] [Google Scholar]
- 15.Jiang G, Chen H, Wang S, Zhou Q, Li X, Chen K, et al. Learning curves and long-term outcome of simulation-based thoracentesis training for medical students. BMC Med Educ. 2011;11(1):39. doi: 10.1186/1472-6920-11-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnsley L, Lyon PM, Ralston SJ, Hibbert EJ, Cunningham I, Gordon FC, et al. Clinical skills in junior medical officers: A comparison of self-reported confidence and observed competence. Med Educ. 2004;38(4):358–367. doi: 10.1046/j.1365-2923.2004.01773.x. [DOI] [PubMed] [Google Scholar]
- 17.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. J Am Med Assoc. 2006;296(9):1094–1102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]
- 18.O’Donoghue D, Davison G, Hanna LJ, McNaughten B, Stevenson M, Thompson A. Calibration of confidence and assessed clinical skills competence in undergraduate paediatric OSCE scenarios: A mixed methods study 13 Education 1303 Specialist Studies in Education. BMC Med Educ. 2018;18(1):1–8. doi: 10.1186/s12909-018-1318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Massoth C, Röder H, Ohlenburg H, Hessler M, Zarbock A, Pöpping DM, et al. High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ. 2019;19(1):1–8. doi: 10.1186/s12909-019-1464-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brydges R, Tran J, Goffi A, Lee C, Miller D, Mylopoulos M. Resident learning trajectories in the workplace: A self-regulated learning analysis. Med Educ. 2020;54(12):1120–1128. doi: 10.1111/medu.14288. [DOI] [PubMed] [Google Scholar]
- 21.Burke L, Hutchins H. Training Transfer: An Integrative Literature Review. Hum Resour Dev Rev. 2007;6(3):263–296. doi: 10.1177/1534484307303035. [DOI] [Google Scholar]
- 22.Mcgaghie WC, Issenberg SB, Barsuk JH, Wayne DB. A critical review of simulation-based mastery learning with translational outcomes. Med Educ. 2014;48(4):375–385. doi: 10.1111/medu.12391. [DOI] [PubMed] [Google Scholar]
- 23.Scahill EL, Oliver NG, Tallentire VR, Edgar S, Tiernan JF, Scahill EL, et al. An Enhanced Approach to Simulation-Based Mastery Learning: Optimising the Educational Impact of a Novel, National Postgraduate Medical Boot Camp. Adv Simul. 2021;6(1):1–10. doi: 10.1186/s41077-021-00157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barsuk JH, Cohen ER, Williams MV, Scher J, Jones SF, Feinglass J, et al. Simulation-Based Mastery Learning for Thoracentesis Skills Improves Patient Outcomes: A Randomized Trial. Acad Med. 2018;93(5):729–735. doi: 10.1097/ACM.0000000000001965. [DOI] [PubMed] [Google Scholar]
- 25.Vijayakumar B, Hynes G, Kitt J, Millette S, FitzPatrick M. An effective procedure skills training programme for GIM registrars. Futur Healthc J. 2021;8(1):e117–e122. doi: 10.7861/fhj.2020-0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wayne DB, Barsuk JH, O’Leary KJ, Fudala MJ, McGaghie WC. Mastery learning of thoracentesis skills by internal medicine residents using simulation technology and deliberate practice. J Hosp Med. 2008;3(1):48–54. doi: 10.1002/jhm.268. [DOI] [PubMed] [Google Scholar]
- 27.Latif RK, Bautista A, Duan X, Neamtu A, Wu D, Wadhwa A, et al. Teaching basic fiberoptic intubation skills in a simulator: initial learning and skills decay. J Anesth. 2016;30(1):12–9. doi: 10.1007/s00540-015-2091-z. [DOI] [PubMed] [Google Scholar]
- 28.Smith KK, Gilcreast D, Pierce K. Evaluation of staff’s retention of ACLS and BLS skills. Resuscitation. 2008;78(1):59–65. doi: 10.1016/j.resuscitation.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 29.de Ruijter PA, Biersteker HA, Biert J, van Goor H, Tan EC. Retention of first aid and basic life support skills in undergraduate medical students. Med Educ Online. 2014;19(1):1–10. doi: 10.3402/meo.v19.24841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Preisner R, Jasti H, Elnicki M, Jeong K. Impact of Web-Based Review on Long-Term Retention of Simulation-Acquired Knee and Shoulder Aspiration and Injection Skills. J Grad Med Educ. 2012;4(4):460–466. doi: 10.4300/JGME-D-11-00239.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moazed F, Cohen ER, Furiasse N, Singer B, Corbridge TC, McGaghie WC, et al. Retention of Critical Care Skills After Simulation-Based Mastery Learning. J Grad Med Educ. 2013;5(3):458–463. doi: 10.4300/JGME-D-13-00033.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matterson HH, Szyld D, Green BR, Howell HB, Pusic MV, Mally PV, et al. Neonatal resuscitation experience curves: simulation based mastery learning booster sessions and skill decay patterns among pediatric residents. J Perinat Med. 2018;46(8):934–941. doi: 10.1515/jpm-2017-0330. [DOI] [PubMed] [Google Scholar]
- 33.Sullivan A, Elshenawy S, Ades A, Sawyer T. Acquiring and Maintaining Technical Skills Using Simulation: Initial, Maintenance, Booster, and Refresher Training. Cureus. 2019;11(9):1–8. doi: 10.7759/cureus.5729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.NHS Lothian. The Medical Education Directorate. Mastery Skills Pathway. 2020 [cited 2022 May 22]. Available from: https://www.med.scot.nhs.uk/simulation/the-mastery-programme.
- 35.Barsuk JH, McGaghie WC, Cohen ER, Balachandran JS, Wayne DB. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med. 2009;4(7):397–403. doi: 10.1002/jhm.468. [DOI] [PubMed] [Google Scholar]
- 36.Barsuk JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009;37(10):2697–2701. [PubMed] [Google Scholar]
- 37.Cook DA, Brydges R, Zendejas B, Hamstra SJ, Hatala R. Mastery learning for health professionals using technology-enhanced simulation: A systematic review and meta-analysis. Acad Med. 2013;88(8):1178–1186. doi: 10.1097/ACM.0b013e31829a365d. [DOI] [PubMed] [Google Scholar]
- 38.McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does Simulation-based Medical Education with Deliberate Practice Yield Better Results than Traditional Clinical Education? A Meta-Analytic Comparative Review of the Evidence. Acad Med. 2011;86(6):706–711. doi: 10.1097/ACM.0b013e318217e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kerins J, Smith SE, Stirling SA, Wakeling J, Tallentire VR. Transfer of training from an internal medicine boot camp to the workplace: enhancing and hindering factors. BMC Med Educ. 2021;21(1):1–12. doi: 10.1186/s12909-021-02911-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang GC, Smith CC, Gordon CE, Feller-Kopman DJ, Davis RB, Phillips RS, et al. Beyond the comfort zone: Residents assess their comfort performing inpatient medical procedures. Am J Med. 2006;119(1):71.e17–71.e24. doi: 10.1016/j.amjmed.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 41.Hicks CM, Gonzales R, Morton MT, Gibbons RV, Wigton RS, Anderson RJ. Procedural experience and comfort level in internal medicine trainees. J Gen Intern Med. 2000;15(10):716–722. doi: 10.1046/j.1525-1497.2000.91104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel M, Oosthuizen G, Child S, District A, Board H, Windsor JA. Training effect of skills courses on confidence of junior doctors performing clinical procedures. N Z Med J. 2008;121(1275):37–45. [PubMed] [Google Scholar]
- 43.Barlow T, Sanders B, Barlow D. Low Volume of Exposure Affects Trainees’ Confidence in Chest Drain Placement. Bull R Coll Surg Engl. 2013;95(4):1–3. doi: 10.1308/147363513X13500508918494. [DOI] [Google Scholar]
- 44.Naicker TR, McLeod DT. Chest Drain insertion training; is Simulation training the answer? Thorax. 2010;65(Suppl 4):A114–A114. doi: 10.1136/thx.2010.150979.37. [DOI] [Google Scholar]
- 45.D’Angelo AL, Ray RD, Jenewein CG, Jones GF, Pugh CM. Residents’ perception of skill decay during dedicated research time. J Surg Res. 2015;199(1):23–31. [DOI] [PMC free article] [PubMed]
- 46.Bannister SL, Dolson MS, Lingard L, Keegan DA. Not just trust: factors influencing learners’ attempts to perform technical skills on real patients. Med Educ. 2018;52(6):605–619. doi: 10.1111/medu.13522. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analysed during the current study are not publicly available as they are part of a larger data set which may be subject to future publication, and contains information that could compromise individual privacy. Data are available from the corresponding author on reasonable request.