Abstract
Purpose
The paper intends to do a scoping review of people with intellectual disabilities in emergency care where this group seems to face access barriers and discrimination. It analyses the conceptual and methodological framework for studies examining the former.
Methods
A scoping review is conducted. The studies’ quality is assessed via a checklist developed by the authors drawing on a compilation of common assessment tools for study quality.
Results
Fourteen quantitative studies fulfil the inclusion criteria for further analysis. Summary measures are extracted. Results are synthesized with Andersen’s Behavioral Model of Health Service Use. Studies employ a combination of variables attributable to different aspects of population characteristics and health behavior.
Conclusion
Most studies seek to quantify or predict emergency care overuse by people with intellectual disabilities. Future studies should also take patients’ poor health or treatment outcomes and their perspectives into account.
Keywords: emergency care, hospital, barriers to health care, health care system, health inequality
Introduction
People with Intellectual Disabilities
Following the biopsychosocial model (see Figure 1) of the International Classification of Functioning, Disability and Health (ICF), we understand disability as the outcome of an interaction between health conditions and the personal and environmental context.1 In this sense, disability as a social category is to be distinguished from impairment understood as “differences in what bodies can do”.2 The ICF frames disability as a participation restriction that does not have to result from impairment.3
Figure 1.
Biopsychosocial Model of ICF.
Notes: Reprinted from World Health Organization. Towards a Common Language for Functioning, Disability and Health: ICF: the International Classification of Functioning, Disability and Health. Available from: https://www.who.int/classifications/icf/icfbeginnersguide.pdf?ua=1.1
Thus, capacity can be distinguished from performance regarding the interaction with barriers and facilitators. Difficulties in learning are best described as an activity limitation or participation restriction in the domain of Learning and Applying Knowledge. These difficulties depend on individual mental functions and interact with environmental factors like technology, attitudes, support in relationships, or the design of services. Moreover, different individual characteristics such as body functions and structures and personal factors can result in activity limitations or participation restrictions in the domain of Learning and Applying Knowledge when interacting with environmental factors.1
Health Situation of People with Intellectual Disabilities
The “World Report on Disability” shows that people with disabilities on the one hand suffer from illnesses that affect the entire population in equal measure, but on the other hand, are usually more affected by (chronic) comorbidities than people without disabilities.4 Compared to people without disabilities, people with disabilities seek inpatient and outpatient care more frequently.1 International findings show premature mortality of people with intellectual disabilities5,6 and discrimination in health care.6–8 Discrimination in the health care system for example manifests in “diagnostic overshadowing”.6–8 As a result, intellectual disabilities as a “master category” overshadow health problems that are, in fact, independent of them, and acute diseases are not diagnosed or are insufficiently treated.
Medical Care for People with Intellectual Disabilities
Explorative, non-representative studies indicate numerous problems for people with intellectual disabilities in hospital care: Bilateral communication barriers make the diagnosis and even the recognition of symptoms more difficult. This for example is the case, if unusual behavior is interpreted as non-compliance or a consequence of the impairment rather than as an indication of pain.5,7–9 Moreover, the quality of patient-provider communication varies depending on disability status. People with disabilities – and among them people with intellectual disabilities – are less likely to receive crucial elements of effective patient-provider communication such as explanations on subsequent treatment steps.10 Relatives, personal assistants, or caregivers can act as mediators but report that they are not taken seriously.7,8 For example, written information about patients with intellectual disabilities is not read or passed on. In other cases, it is reported that hospital staff only talk to caretakers and not to patients.11
Patients with and without disabilities both share the experience of meeting barriers obtaining high-quality health care, for instance, regarding a lack of coordination between different health care providers, time constraints during visitation, or the provision of inadequate information.12 However, patients with disabilities further experience disability-specific barriers to obtaining good health care.12 For various reasons, the treatment of patients with intellectual disabilities is often associated with additional time and resource expenditure currently not refinanced in a system of standardized procedures.13,14 There are reports of incorrect accommodation on pediatric, geriatric, and psychiatric wards, avoidable sedation and coercive measures, early discharge,13 insufficient basic care or support with food and fluid intake, personal hygiene, toilet visits, or comfortable positioning of the patient.5,9 It even seems to occur that individual treatments is not granted in case of additional effort,13 and continuous accompaniment is defined as a prerequisite for admission.14 However, such a prerequisite ignores the life and work realities of potential companions (relatives, personal assistants, employees of services for people with disabilities).13,15
And lastly, hospital staff report difficulties when dealing with patients with intellectual disabilities15 due to reservations, a lack of experience with or ignorance of this group of patients.8 Reservations manifest in reasons given for the omission of examinations or treatment for patients with multiple disabilities, in which judgments about their quality of life become apparent, independent of the patients’ individual will to live.6,7 Many of these care problems are commonly interpreted as general problems of routine inpatient care8 or general developments in the health care system,13 which have a more pronounced impact on patients with intellectual disabilities.8
Research Gap
Against this background, it can reasonably be assumed that people with intellectual disabilities face access barriers and discrimination in the specific setting of emergency care. The situation of people with intellectual disabilities in emergency care has not yet been adequately described, however. and solutions to the known problems have rarely been found or implemented. The scoping review should therefore contribute to a better understanding of people with intellectual disabilities in emergency care. The challenges faced in emergency care, of course, vary with the specific form of intellectual disability. Given the limited number of available studies, it was impossible to further differentiate.
Methods
A scoping review is carried out to understand the situation of people with learning disabilities in emergency care.16,17 Reporting is done according to the “Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist”18,19 (Supplementary 1: PRISMA-ScR Checklist).
Protocol and Registration
The detailed review protocol is invested (Supplementary 2: Protocol), but it is not registered at the international prospective register of systematic reviews (PROSPERO).
Eligibility Criteria
To provide a snapshot of current practices all peer-reviewed papers published in English or German from 1st January 2009 to 1st February 2020 are included, thus collecting the results of the last ten years. The study design has to be quantitative. Only studies with a focus on adults with learning disabilities in emergency care are included. Secondary literature, such as commentaries, editorials, opinions or perspectives and dissertations, posters, literature research, reviews, and qualitative research, are excluded to increase the studies’ homogeneity.
Information Sources
A sensitive search strategy was developed to identify all relevant studies. In order to get a quick insight into the state of research, the search was carried out (only) in the PubMed/MEDLINE database. Dates of coverage are 1st January 2009 to 1st February 2020, whereby the latter is the date last searched.
Search
According to the PICO scheme, the search strategy consists of two components (P: participants, I: intervention). The first component represents the term “adults with intellectual disabilities” and its synonyms; which are combined with the Boolean operator “OR.” The second component embodies all names and synonyms for “emergency care”, which are also combined via “OR.” Finally, these two components are combined with “AND” to include only studies meeting both criteria. The search strategy was applied to the PubMed/MEDLINE database using MeSH (Medical Subject Headings) terms for PubMed/MEDLINE (Supplementary 3: Search strategy).
Study Selection
Title screening, abstract screening, and full-text screening were conducted and supervised by the authors (JY, UK, YW) independently to assess whether the studies fulfil the inclusion criteria. Disagreements were resolved through discussion. Studies investigating emergency care for adults with intellectual disabilities were included. Studies focusing on children, older people with Alzheimer’s disease or dementia without intellectual disabilities, or patients only with psychiatric diseases were excluded. Likewise, studies focusing on the diagnosis of learning disabilities were excluded. These exclusions guarantee the homogeneity of the sample. Studies analyzing the emergency care of people with intellectual disabilities in a particular life phase (eg, pregnancy, last year of life) are allowed. Citavi 6.5 is used to manage the references and to collect all included studies in one database.
Data Collection Process
Data was extracted from the articles by the reviewer JY. The reviewers UK and YW subsequently checked the extracted data. Disagreements were solved via discussion. All objectively reported outcomes are included.
Data Items
Data items, title, authors, year of publication, country, sample (size), control group (size), study design, and reported variables were extracted when given (see Table 1).
Table 1.
Summary Measures
| Number | Title | Authors | Year | Country | Sample (Size) | Control Group (Size) | Independent Variables | Dependent Variables | Study Design | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Predictors of Emergency Room and Hospital Utilization Among Adults with Intellectual and Developmental Disabilities23 | Blaskowitz, M. G.; Hernandez, B.; Scott, P. W. | 2019 | USA | Adults with intellectual and developmental disability n: 597 |
None | Age, gender, level of intellectual disability, chronic health problems, mental health diagnoses, polypharmacy, supported living arrangement, region |
ER use for a medical/physical reason, hospitalization for a medical/physical reason, ER use for a behavioral/psychiatric reason, hospitalization for a behavioral/psychiatric reason | Prevalence study, secondary data: survey of medical charts |
Predictors (environmental and individual risk factors) for ED use: institutionalized people are less likely to be admitted; people from deprived neighborhoods with a lack of care are less likely to visit the ED |
| 2. | Rate and characteristics of urgent hospitalization in persons with profound intellectual disabilities compared with general population24 | Amor-Salamanca, A.; Menchon, J. M. | 2018 | Spain | Adults with severe/ profound intellectual disability n: 28 |
Other hospitalized ED patients n: 83 |
Gender, age, living arrangement | Emergency visits, admission to hospital after emergency visit | Retrospective cohort study, secondary data: discharge reports |
No differences in the proportion of people with profound intellectual disability and controls admitted to hospital after their emergency visit; the median hospital stay was higher for people with profound intellectual disability s: 7.5 vs 4 days for controls |
| 3. | Factors associated with ambulatory care sensitive emergency department visits for South Carolina Medicaid members with intellectual disability25 | McDermott, S.; Royer, J. A.; Mann, J. R.; Armour, B. S. | 2018 | USA | Individuals with intellectual disability identified from ICD-9 CM codes n: 14.650 |
Subgrouping: moderate-to-profound intellectual disability (37. 8%), mild intellectual disability (33.8%), unspecified intellectual disability (16.4%), Down syndrome/other genetic causes (11.9%) |
age, race, sex, rurality of county, residential service setting, years of enrollment, supplemental nutrition assistance | Primary care visits, ED visits, and subsequent inpatient hospital admission, timing of services | Retrospective cohort study, secondary data: discharge dataset |
ED overuse of intellectual disability subgroups due to conditions that are manageable in primary care; living in the community, comorbidity, and previous primary care were associated with more frequent ED visits |
| 4. | Postpartum Hospital Utilization among Massachusetts Women with Intellectual and Developmental Disabilities: A Retrospective Cohort Study26 | Mitra, M.; Parish, S. L.; Akobirshoev, I.; Rosenthal, E.; Moore Simas, T. A. | 2018 | USA | Women with intellectual and developmental disability identified from ICD-9 CM codes n: 1104 |
Women without intellectual and developmental disability n: 778,409 |
Woman who gave birth, maternal age, race/ethnicity, education, marital status, type of health insurance, adequacy of prenatal care, diseases | Postpartum hospital admissions, ED visits during three critical postpartum periods (1–42, 43–90, and 1–365 days), nondelivered hospitalizations, observational stays | Retrospective cohort study, secondary data: Massachusetts Pregnancy to Early Life Longitudinal Data System (PELL) |
Women with intellectual and developmental disability had markedly higher rates of postpartum hospital admissions and ED visits after a childbirth |
| 5. | Antenatal Hospitalization Among US Women with Intellectual and Developmental Disabilities: A Retrospective Cohort Study27 | Mitra, M.; Parish, S. L.; Clements, K. M.; Zhang, J.; Moore Simas, T. A. | 2018 | USA | Women with intellectual and developmental disability identified from ICD-9 CM n: 498 |
Women without intellectual and developmental disability n: 1,531 |
Women who gave birth, maternal age, education, race/ethnicity, marital status, health insurance; father named on the birth certificate; adequacy of prenatal care utilization, smoking during pregnancy, diseases | Hospital utilization during pregnancy: ED visit, observational stays, and non-delivery hospital stays | Retrospective cohort study, secondary data: Massachusetts Pregnancy to Early Life Longitudinal Data System (PELL) | Higher likelihood of women with intellectual and developmental disability to visit ED or get hospitalized during pregnancy |
| 6. | Postpartum Acute Care Utilization Among Women with Intellectual and Developmental Disabilities28 | Brown, H. K.; Cobigo, V.; Lunsky, Y.; Vigod, S. | 2017 | Canada | Women with intellectual and developmental disability n: 3803 |
Women without intellectual and developmental disability n: 378,313 |
Women who gave birth, maternal age, parity, neighborhood income quintile, region of residence, preexisting diseases, diseases during pregnancy | Postpartum hospital admissions, ED visits | Retrospective cohort study, secondary data: Ontario (Canada) health and social services administrative data | Women with intellectual and developmental disability, compared to those without, had an increased risk for postpartum hospital admissions overall, for psychiatric reasons but not for medical reasons |
| 7. | Emergency department and inpatient hospitalizations for young people with fragile X syndrome29 | McDermott, S.; Hardin, J. W.; Royer, J. A.; Mann, J. R.; Tong, X.; Ozturk, O. D.; Ouyang, L. | 2015 | USA | Adolescents and young adults with fragile x syndrome, identified from ICD-9 CM n: 125 (fragile x syndrome) |
Adolescents and young adults with intellectual disability, people with autism spectrum disorder identified from ICD-9 CM. people without disability n: 2,592 (autism spectrum disorder) 10,685 (intellectual disability) |
Gender, age, and insurance coverage | Hospital encounters | Prevalence study, secondary data: state’s health and human services data, hospital discharge dataset | People with fragile x syndrome, autism spectrum disorder, or intellectual disability are more likely to have had hospital encounters |
| 8. | Predictors of emergency department visits by persons with intellectual disability experiencing a psychiatric crisis30 | Lunsky, Y.; Balogh, R.; Cairney, J. | 2012 | Canada | Adults with intellectual disability who visited ED in response to a crisis n: 96 |
Adults with intellectual disability who did not visit ED in response to a crisis n:480 |
Persons who visited the ED in response to the first crisis, people who did not visit the ED in response to the first crises | Predictors of ED use: level of disability, type of residence, crisis plan, family physician, history of involvement with the criminal justice system, and history of ED visits | Cohort study, primary data: staff assessment | Significant predictors of ED visits: level of disability, type of residence, crisis plan, family physician, history of involvement with the criminal justice system, and history of ED visits |
| 9. | Quantifying emergency department admission rates for people with a learning disability31 | Williamson, T.; Flowers, J.; Cooke, M. | 2012 | UK | Persons with learning disability identified from the ICD-10 n: 246 |
None | Age, sex | Hospital admission via ED | Prevalence study, secondary data: Admission data from Birmingham Heartlands Hospital | Admission rates of patients with learning disability |
| 10. | Life events and emergency department visits in response to crisis in individuals with intellectual disabilities32 | Lunsky, Y.; Elserafi, J. | 2011 | Canada | Adults with intellectual disability who visited ED in response to a crisis n: 96 |
Adults with intellectual disability who did not visit ED in response to a crisis n:480 |
Stressful life events | Hospital use | Cohort study, primary data: Informants provided data (Psychiatric Assessment for Adults with Developmental Disabilities Checklist) |
Individuals experiencing life events in the past year were more likely to visit the ED in response to crisis than those who did not experience any life events |
| 11. | The Impact of Medicaid Managed Care on Health Service Utilization Among Adults with Intellectual and Developmental Disabilities33 | Yamaki, K.; Wing, C.; Mitchell, D.; Owen, R.; Heller, T. | 2019 | USA | People with intellectual and developmental disability from a region that reformed Medicaid n: 1,121 |
People with intellectual and developmental disability from a different region n:1,102 |
Transition from fee-for-service to Medicaid managed care | Utilization of ED and/or primary care physicians, inpatient hospitalization | Quasi-experiment, secondary data: state Medicaid agency, integrated care program | Medicaid managed care reduced avoidable ED visits (manageable conditions, mental conditions) |
| 12. | Emergency Department Use: Common Presenting Issues and Continuity of Care for Individuals with and without Intellectual and Developmental Disabilities34 | Durbin, A.; Balogh, R.; Lin, E.; Wilton, A. S.; Lunsky, Y.24 | 2018 | Canada | Adults with intellectual and developmental disability n: 66,484 |
Adults without intellectual and developmental disability n: 2,760,670 |
Level of continuity of primary care | ED visits | Retrospective cohort study, secondary data: administrative health and social services data | Individuals with intellectual and developmental disability were more likely than individuals with no intellectual and developmental disability to visit the ED; for both groups, greater primary care continuity was associated with less ED use, but this relationship was more marked for adults with intellectual and developmental disability |
| 13. | Use of health services in the last year of life and cause of death in people with intellectual disability: a retrospective matched cohort study35 | Brameld, K.; Spilsbury, K.; Rosenwax, L.; Leonard, H.; Semmens, J.25 | 2018 | Australia | Decedents with intellectual disability identified from ICD n: 591 |
Decedents without intellectual disability n: 29,713 |
Cause of death | ED visit, hospital admissions | Retrospective cohort study, secondary data: Data Linkage Branch, Western Australian Department of Health, Intellectual Disability Exploring Answers (IDEA) Database |
People with intellectual disability had increased odds of presentation, admission, or death from conditions that have been defined as ambulatory care sensitive and are potentially preventable |
| 14. | Pain underreporting associated with profound intellectual disability in emergency departments36 | Amor-Salamanca, A.; Menchon, J. M. | 2017 | Spain | Persons with profound intellectual disability n: 100 |
Patients without profound intellectual disability n: 300 |
Age, gender | Reasons and diagnoses in ED, patients behaviour while travelling to the hospital, time spent waiting and being examined in the ED |
Retrospective cohort study, secondary data: clinical report from the ED, primary data: interview conducted by the person who had accompanied the patient to the hospital | Somatic complaints were the main reason for ED attendance among persons with profound intellectual disability; a diagnosis implying physical pain was given less often to people with profound intellectual disability than to controls |
Abbreviations: ED-Emergency Department, ER-Emergency Room, CD-International Classification of Disease.
Quality Assessment
After study selection, a quality assessment was conducted (see Table 2). In expectation of different study types, the studies’ quality was assessed via a checklist developed by the authors drawing on a compilation of common assessment tools for study quality.20 The checklist considers the study design, the selection of cases, and, if necessary, the selection of the control group. These results do not influence the data synthesis.
Table 2.
Quality Assessment
| Number | Study Design | Cases | Controls | |||||
|---|---|---|---|---|---|---|---|---|
| Study Type | Time(s) of Measurement | Direction | Understandable Description | Selection of Cases | Basis for Case Definition | Selection of Controls | Basis for Distinction of Cases from Controls | |
| a) Intervention b) Prevalence c) Cohort d) Case Control |
a) Longitudinal b) Cross-Sectional |
a) prospective b) Retrospective |
a) yes b) No |
a) Population-Based b) Health Insurance-Based c) Hospital-Based d) Natural Group |
a) Secondary Data b) Proxy Assessment c) Self-Declaration d) Not Defined |
a) Community Controls b) Health Insurance Controls c) Hospital Controls d) Subgrouping e) No Controls |
a) Secondary Data b) Proxy Assessment c) Self-Declaration d) Not Defined e) Not Applicable |
|
| 1. | Prevalence | Cross-sectional | Retrospective | Yes | Provider based | Proxy assessment | No controls | Not applicable |
| 2. | Cohort | Longitudinal | Retrospective | No | Provider-based | Secondary data | Hospital controls | Not defined |
| 3. | Cohort | Longitudinal | Retrospective | Yes | Health insurance-based | Secondary data | Subgrouping | Secondary data |
| 4. | Cohort | Longitudinal | Retrospective | Yes | Population-based | Secondary data | Community controls | Secondary data |
| 5. | Cohort | Longitudinal | Retrospective | Yes | Population-based | Secondary data | Community controls | Secondary data |
| 6. | Cohort | Longitudinal | Retrospective | Yes | Population-based | Secondary data | Community controls | Secondary data |
| 7. | Prevalence | Cross-sectional | Retrospective | Yes | Population-based | Secondary data | Subgrouping | Secondary data |
| 8. | Cohort | Cross-sectional | Retrospective | No | Provider based | Proxy assessment | Subgrouping | Proxy assessment |
| 9. | Prevalence | Cross-sectional | Retrospective | Yes | Hospital-based | Secondary data | No controls | Not applicable |
| 10. | Cohort | Cross-sectional | Retrospective | No | Provider based | Proxy assessment | Subgrouping | Proxy assessment |
| 11. | Quasi-experiment | Longitudinal | Retrospective | Yes | Health insurance-based | Secondary data | Health insurance-based | Not defined |
| 12. | Cohort | Cross-sectional | Retrospective | Yes | Population-based | Secondary data | Community controls | Secondary data |
| 13. | Cohort | Cross-sectional | Retrospective | Yes | Population-based | Secondary data | Community controls | Secondary data |
| 14. | Cohort | Longitudinal | Retrospective | No | Provider based | Secondary data | Hospital controls | Not defined |
Summary Measures
Due to an expected heterogeneity in methodological approaches and outcomes, no meta-analysis was conducted. Additionally, it was decided not to develop a forest plot of the studies’ results because of too much variation (eg, data types, study design) (see Table 2). Therefore, the results’ synthesis and analysis have a descriptive character (see Table 1).
Synthesis of Results
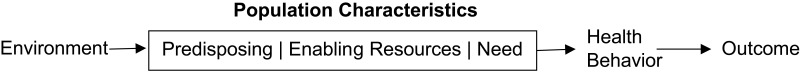
All variables surveyed are mapped to the Behavioral Model of Health Services Use developed by Ronald M. Andersen to synthesize the results (see Figure 2).21,22 This model was developed to assess and subsequently promote equal access to healthcare via understanding users’ health-seeking behavior.21,22
Figure 2.
Behavioral Model of Health Services Use (own Illustration after Ronald M. Andersen).
The model differs between environment characteristics (health care system, external environment), population characteristics, health behavior (personal health practices, use of health services) and outcome (health status, quality of life). Population characteristics are further broken down into predisposing characteristics (demographics, social structure, health beliefs), enabling resources (personal, family, community) and need (perceived need, evaluated need). The authors classify all variables surveyed (see Table 3).
Table 3.
Synthesis of Results
| Number | Predisposing Characteristics | Enabling Resources | Need | Health Behavior | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Demographic | Social Structure | Health Beliefs | Personal | Family | Community | Perceived | Evaluated | Personal Health Practices | Use of Health Services | |
| 1. |
Independent variable: age, gender, level of intellectual disability, chronic health problems, mental health diagnoses, polypharmacy |
Independent variable: region |
None | None | None |
Independent variable: supported living arrangement |
None | Dependent variable: hospitalization for a medical/physical reason, hospitalization for a behavioral/psychiatric reason | None |
Dependent variable: ER use for a medical/physical reason, ER use for a behavioral/psychiatric reason |
| 2. |
Independent variable: gender, age |
None | None | None | None |
Independent variable: living arrangement |
None |
Dependent variable: admission to hospital after emergency visit |
None |
Dependent variable: emergency visits |
| 3. |
Independent variable: age, race, sex |
Independent variable: rurality of county |
None | None | None | Independent variable: residential service setting | None |
Dependent variable: subsequent inpatient hospital admission |
None |
Independent variable: years of enrollment, supplemental nutrition assistance dependent variable: primary care visits, ED visits, timing of services |
| 4. |
Independent variable: woman who gave birth, maternal age, race/ethnicity, education, marital status, diseases |
None | None | None | None |
Independent variable: type of health insurance |
None |
Dependent variable: postpartum hospital admissions, nondelivered hospitalizations, observational stays |
None |
Independent variable: adequacy of prenatal care utilization dependent variable: ED visits during three critical postpartum periods (1–42, 43–90, and 1–365 days) |
| 5. |
Independent variable: women who gave birth, maternal age, education, race/ethnicity, marital status, father named on the birth certificate; diseases |
None | None | None | None |
Independent variable: health insurance |
None |
Dependent variable: hospital utilization during pregnancy: observational stays, and non-delivery hospital stays |
Independent variable: smoking during pregnancy |
Independent variable: adequacy of prenatal care utilization dependent variable: hospital utilization during pregnancy: ED visit |
| 6. |
Independent variable: women who gave birth, maternal age, parity, preexisting diseases, diseases during pregnancy |
Independent variable: neighborhood income quintile, region of residence |
None | None | None | None | None |
Dependent variable: postpartum hospital admissions |
None |
Dependent variable: postpartum ED visits |
| 7. |
Independent variable: gender, age |
None | None | None | None |
Independent variable: insurance coverage |
None | None | None |
Dependent variable: hospital encounters |
| 8. |
Dependent variable: predictors of ED use: level of disability, history of involvement with the criminal justice system |
None | None | None | None | Dependent variable: type of residence, crisis plan, family physician, | None | None | None |
Independent variable: persons who visited the ED in response to the first crisis, people who did not visit the ED in response to the first crises dependent variable: history of ED visits |
| 9. |
Independent variable: age, sex |
None | None | None | None | None | None | Dependent variable: hospital admission via ED | None |
Dependent variable: ED visits |
| 10. | Independent variable: stressful life events | None | None | None | None | None | None | None | None | Dependent variable: hospital use |
| 11. | None | None | None | None | None | Independent variable: transitioned from fee-for-service to Medicaid managed care | None | Dependent variable: inpatient hospitalization | None |
Dependent variable: utilization of ED and/or primary care physicians |
| 12. | None | None | None | None | None | None | None | None | None |
Independent variable: level of continuity of primary care dependent variable: ED visits |
| 13. | Independent variable: cause of death | None | None | None | None | None | None | Dependent variable: hospital admissions | None |
Dependent variable: ED visit |
| 14. |
Independent variable: age, gender |
None | None | None | None | None |
Dependent variable: reasons in ED |
Dependent variable: diagnoses in ED, patient’s behaviour while travelling to the hospital |
None | None |
Results
Figure 3 shows the process of study selection. The search strategy identifies 2.321 peer-reviewed articles (after the removal of duplicates). After title screening, 359 articles qualified for abstract screening, reducing the number to 30 relevant for full-text screening. In the end 14 quantitative studies fulfil the inclusion criteria for further analysis.
Figure 3.
Study Selection Flow Chart.
The studies’ title, authors, year of publication, country, sample size, control group size, independent and dependent variables, and study designs were extracted. Further, a summary of the studies’ results was given. The included studies were published between 2011 and 2019, with ten of the fourteen studies published between 2017 and 2019. Ten of the fourteen selected studies were conducted in North America, six in the USA, and four in Canada. Two studies were conducted in Spain and one study in Australia and the UK, respectively. Only ten different first authors published the fourteen studies. Sample sizes vary between 28 and 66,484 cases (see Table 1).
Drawing on a compilation of common checklists to assess the quality of studies based on their respective study type, the authors developed a checklist to assess the selected studies’ quality (see Table 2).20 Assessing study quality makes it possible to evaluate state of the art as relevant to this journal’s audience. All studies were retrospective in character, seven of them longitudinal. Our sample’s most common study type is cohort studies (10), followed by prevalence studies (3) and one quasi-experiment. Four studies did not deliver an understandable description of the study design. Most studies defined their cases (10) and controls (6) based on secondary data. Cases selection was population-based (6), provider-based (5), health-insurance-based (2), and hospital-based (1). If applicable and defined controls were selected from the community (5), hospital (2), or health-insurance (1). In some studies, subgroups were compared (4).
The synthesis of results against the background of Andersen’s Behavioral Model of Health Services Use (see Table 3) was found to be feasible. Studies employ a combination of variables attributable to different aspects of population characteristics and health behavior. The selected studies assess neither environment characteristics (health care system, external environment) nor outcomes (health status, quality of life); the respective columns were therefore deleted (see Table 3). Among the variables attributable to population characteristics, the studies in our sample employ variables on predisposing characteristics, enabling resources, and need. Data collected on predisposing characteristics mainly concern demographics (12) and also social structure (3), but not health beliefs (0).
Regarding enabling resources, the studies in our sample only identify community resources (8) but not personal resources (0) or family resources (0). Ten studies contain variables on evaluated need; only one study contains variables on perceived need. Among the variables attributable to health behavior, 13 of 14 studies incorporate variables attributable to the use of health services, whereas only one study incorporates a variable on personal health practices.
Discussion
The studies in our sample use a person-centered terminology, even if they employ a person-first language, namely Persons with Intellectual Disabilities, Persons with Intellectual and Developmental Disabilities, Persons with severe/profound intellectual disability or Persons with a specific diagnosis (eg Fragile X Syndrome). A person-centered approach to disability (in contrast to a focus on person-environment fit) is probably applied due to the studies’ medical context.
The scoping review based on a PubMed/MEDLINE search includes 14 studies. It cannot be ruled out that a systematic review extended to other databases might have identified further studies. Since PubMed/MEDLINE is a meta-database focusing on medical research, the authors assume that the results published here are directive concerning the care situation of people with disabilities in emergency care.
Summary measures (see Table 1) indicate that most studies aim to quantify emergency care overuse by people with intellectual disabilities or seeking to establish predictors for such overuse. This focus might be explained by the massive financial implications of ED over-utilization.37 Two studies concentrate on preventing emergency care overuse via primary care and access to primary care via health insurance respectively. One can suppose that such interventions might also benefit patients in general.
An assessment of the studies’ quality (see Table 2) indicates that most selected studies draw upon secondary data and are therefore of retrospective character. Cohort studies are the most common study design, whereas none of the studies in our sample is an intervention study. Given the still very modest number of studies as a whole, this dearth of intervention studies is hardly surprising. Four out of fourteen studies do not describe their study design in an understandable way.
Analyzing our findings against the background of Andersen’s Behavioral Model of Health Services Use was found to be feasible (see Table 3). Most studies employ a combination of variables attributable to different aspects of population characteristics and health behavior. The selected studies assess neither environment characteristics (health care system, external environment) nor outcomes (health status, quality of life). As health outcomes for patients with intellectual disabilities can be assumed to be poor on reasonable grounds (see background), the lack of focus on health outcomes for this patient group is concerning, nonetheless. We found only one study (14) that tackled the underreporting of pain, which marks a poor treatment outcome for patients. Another study (13) found that patients with intellectual disabilities have increased odds of needing emergency care for and dying from ambulatory care sensitive conditions. Such potentially preventable deaths hint at poor outcomes for this patient population’s health status (leave aside their quality of life). However, the dearth of intervention studies (see above) can partly explain the lack of focus on outcomes in our sample. Still, even retrospective cohort studies based on secondary data could focus on this patient group’s health outcomes.
The synthesis of results against the background of Andersen’s Behavioral Model of Health Services Use further indicates that patients’ perspectives are ignored in included studies. Neither their health beliefs, personal or family resources, nor perceived needs are made the subject of discussion. The similarities in study design (retrospective cohort studies based on secondary data) can to some extent explain why patient perspectives as self-declarations are missing. Of course, it has to be noted here that qualitative studies were excluded from the sample to ensure the selected studies’ comparability. Still, there are no mixed methods studies either, which would have been allowed.
Conclusion
Most studies in our sample seek to quantify or predict emergency care overuse by people with intellectual disabilities. Like other care problems stated in the introduction, the overuse of emergency care is not specific to this patient population.22 Healthcare systems tackle this rather general problem by different measures, such as strengthening primary care or extending insurance coverage, impacting patients with intellectual disabilities more significantly than other patient groups.
Future studies should include poor health (or treatment) outcomes for this patient group, partly explained by a missing person-environment fit. However, the study designs in our sample cannot tackle missing accommodations, access barriers, or discrimination.
Lastly, future studies should include the perspectives of people with intellectual disabilities in their roles as patients. Different study types are needed, such as intervention studies, mixed-method studies, and participatory research. The inclusion of people with intellectual disabilities’ perspectives is paramount. After all, this group has often been excluded from research assuming they are not viable research partners.23
Acknowledgments
We would like to thank our student assistants, Saskia Golasch and Franz Falk, for their support in researching the articles.
Disclosure
The study at hand did not receive any funding. None of the authors has any conflict of interest or financial interests relevant to this article to declare.
References
- 1.World Health Organization. Towards a Common Language for Functioning, Disability and Health: ICF: the International Classification of Functioning, Disability and Health. Available from: https://www.who.int/classifications/icf/icfbeginnersguide.pdf?ua=1. Accessed July 21, 2020.
- 2.Coleman-Fountain E, McLaughlin J. The interactions of disability and impairment. Social Theory Health. 2013;11(2):133–150. doi: 10.1057/sth.2012.21 [DOI] [Google Scholar]
- 3.Hirschberg M. Conceptualisations of Disability in ICF and CPRD: their contribution to the realization of the Right to Work. In: Wansing G, Welti F, Schäfers M, editors. The Right to Work for Persons with Disabilities: International Perspectives. Baden-Baden: Nomos; 2018. [Google Scholar]
- 4.World Health Organization, The World Bank. World report on disability. Available from: http://whqlibdoc.who.int/publications/2011/9789240685215_eng.pdf. Accessed July 11, 2022.
- 5.Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK population-based study. Lancet. 2014;383(9920):889–895. doi: 10.1016/S0140-6736(13)62026-7 [DOI] [PubMed] [Google Scholar]
- 6.The Learning Disabilities Mortality Review (LeDeR) Programme. Annual Report December 2017. Bristol; 2017; 2. Available from: http://www.bristol.ac.uk/media-library/sites/sps/leder/leder_annual_report_2016-2017.pdf. Accessed August 7, 2019.
- 7.Mencap. Death by Indifference. Available from: https://www.mencap.org.uk/sites/default/files/2016-06/DBIreport.pdf. Accessed July 11, 2022.
- 8.Michael J. Health Care for All: independent Inquiry Into access to healthcare for people with learning disabilities. Available from: https://www.emerald.com/insight/content/doi/10.1108/13595474200800036/full/pdf?title=healthcare-for-all-the-independent-inquiry-into-access-to-healthcare-for-people-with-learning-disabilities. Accessed 19 February, 2020.
- 9.Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L Confidential Inquiry into premature deaths of people with learning disabilities (CIPOLD): final Report. Available from: https://www.bristol.ac.uk/media-library/sites/cipold/migrated/documents/fullfinalreport.pdf. Accessed February 19, 2020. [DOI] [PubMed]
- 10.Marlow NM, Samuels SK, Jo A, Mainous AG. Patient-provider communication quality for persons with disabilities: a cross-sectional analysis of the Health Information National Trends Survey. Disabil Health J. 2019;12(4):732–737. doi: 10.1016/j.dhjo.2019.03.010 [DOI] [PubMed] [Google Scholar]
- 11.Bundesärztekammer. Stellungnahme der zentralen Kommission zur Wahrung ethischer Grundsätze in der Medizin und ihren Grenzgebieten (Zentrale Ethikkommission) bei der Bundesärztekammer: „Advance Care Planning (ACP)“. Deutsches Ärzteblatt. 2010;107(7):297–300. [Google Scholar]
- 12.McClintock HF, Barg FK, Katz SP, et al. Health care experiences and perceptions among people with and without disabilities. Disabil Health J. 2016;9(1):74–82. doi: 10.1016/j.dhjo.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasseler M. Menschen mit geistigen und mehrfachen Behinderungen in der akut-stationären Versorgung. Dtsch Med Wochenschr. 2015;140(21):e217–23. doi: 10.1055/s-0041-106610 [DOI] [PubMed] [Google Scholar]
- 14.Roser J-M, Budroni H, Schnepp W. Abschlussbericht zum Projekt Entwicklung einer Zielvereinbarung zur barrierefreien Krankenhausversorgung von Menschen mit Mehrfachbehinderungen. Available from: https://www.diefachverbaende.de/files/fachthemen/2011-10-24-AbschlussberichtZielvereinbarungbarrierefreiesKrankenhaus2011.pdf. Accessed February 19, 2020.
- 15.Steffen P, Blum K. Menschen mit geistiger Behinderung: defizite in der Versorgung: ergebnisse einer explorativen Untersuchung in zwei Hamburger Bezirken. Deutsches Ärzteblatt. 2012;109(17):860–862. [Google Scholar]
- 16.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 17.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and Explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 20.Zeng X, Zhang Y, Kwong JSW, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8(1):2–10. doi: 10.1111/jebm.12141 [DOI] [PubMed] [Google Scholar]
- 21.Andersen RM. Revisiting the Behavioral Model and Access to Medical Care: does it Matter. J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 22.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 23.Blaskowitz MG, Hernandez B, Scott PW. Predictors of Emergency Room and Hospital Utilization Among Adults With Intellectual and Developmental Disabilities (IDD). Intellect Dev Disabil. 2019;57(2):127–145. doi: 10.1352/1934-9556-57.2.127 [DOI] [PubMed] [Google Scholar]
- 24.Amor-Salamanca A, Menchon JM. Rate and characteristics of urgent hospitalisation in persons with profound intellectual disabilities compared with general population. J Intellect Disabil Res. 2018;62(3):179–186. doi: 10.1111/jir.12436 [DOI] [PubMed] [Google Scholar]
- 25.McDermott S, Royer J, Mann JR, Armour BS. Factors associated with ambulatory care sensitive emergency department visits for South Carolina Medicaid members with intellectual disability. J Intellect Disabil Res. 2018;62(3):165–178. doi: 10.1111/jir.12429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitra M, Parish SL, Akobirshoev I, Rosenthal E, Moore Simas TA. Postpartum Hospital Utilization among Massachusetts Women with Intellectual and Developmental Disabilities: a Retrospective Cohort Study. Matern Child Health J. 2018;22(10):1492–1501. doi: 10.1007/s10995-018-2546-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitra M, Parish SL, Clements KM, Zhang J, Simas TAM. Antenatal Hospitalization Among U.S. Women With Intellectual and Developmental Disabilities: a Retrospective Cohort Study. Am J Intellect Dev Disabil. 2018;123(5):399–411. doi: 10.1352/1944-7558-123.5.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown HK, Cobigo V, Lunsky Y, Vigod S. Postpartum Acute Care Utilization Among Women with Intellectual and Developmental Disabilities. J Womens Health. 2017;26(4):329–337. doi: 10.1089/jwh.2016.5979 [DOI] [PubMed] [Google Scholar]
- 29.McDermott S, Hardin JW, Royer JA, et al. Emergency department and inpatient hospitalizations for young people with fragile X syndrome. Am J Intellect Dev Disabil. 2015;120(3):230–243. doi: 10.1352/1944-7558-120.3.230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lunsky Y, Balogh R, Cairney J. Predictors of emergency department visits by persons with intellectual disability experiencing a psychiatric crisis. Psychiatr Serv. 2012;63(3):287–290. doi: 10.1176/appi.ps.201100124 [DOI] [PubMed] [Google Scholar]
- 31.Williamson T, Flowers J, Cooke M. Quantifying emergency department admission rates for people with a learning disability. Emerg Med J. 2012;29(9):771–772. doi: 10.1136/emj.2010.107318 [DOI] [PubMed] [Google Scholar]
- 32.Lunsky Y, Elserafi J. Life events and emergency department visits in response to crisis in individuals with intellectual disabilities. J Intellect Disabil Res. 2011;55(7):714–718. doi: 10.1111/j.1365-2788.2011.01417.x [DOI] [PubMed] [Google Scholar]
- 33.Yamaki K, Wing C, Mitchell D, Owen R, Heller T. The Impact of Medicaid Managed Care on Health Service Utilization Among Adults With Intellectual and Developmental Disabilities. Intellect Dev Disabil. 2019;57(4):289–306. doi: 10.1352/1934-9556-57.4.289 [DOI] [PubMed] [Google Scholar]
- 34.Durbin A, Balogh R, Lin E, Wilton AS, Lunsky Y. Emergency Department Use: common Presenting Issues and Continuity of Care for Individuals With and Without Intellectual and Developmental Disabilities. J Autism Dev Disord. 2018;48(10):3542–3550. doi: 10.1007/s10803-018-3615-9 [DOI] [PubMed] [Google Scholar]
- 35.Brameld K, Spilsbury K, Rosenwax L, Leonard H, Semmens J. Use of health services in the last year of life and cause of death in people with intellectual disability: a retrospective matched cohort study. BMJ Open. 2018;8(2):e020268. doi: 10.1136/bmjopen-2017-020268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amor-Salamanca A, Menchon JM. Pain underreporting associated with profound intellectual disability in emergency departments. J Intellect Disabil Res. 2017;61(4):341–347. doi: 10.1111/jir.12355 [DOI] [PubMed] [Google Scholar]
- 37.Coster JE, Turner JK, Bradbury D, Cantrell A. Why Do People Choose Emergency and Urgent Care Services? A Rapid Review Utilizing a Systematic Literature Search and Narrative Synthesis. Acad Emerg Med. 2017;24(9):1137–1149. doi: 10.1111/acem.13220 [DOI] [PMC free article] [PubMed] [Google Scholar]