Abstract
Introduction
Intervertebral disk degeneration is a universal and natural process. However, no reports have summarized anatomical age-related intervertebral disk height and disk degenerative changes in the thoracolumbar spine or examined sex-specific differences. This study aimed to establish age-related changes and gender-specific differences of intervertebral disk height and disk degeneration of the thoracolumbar spine in a large cohort of relatively healthy subjects and also to evaluate the relationship between the degree of thoracolumbar disk height and disk degeneration.
Methods
Six hundred and twenty-seven relatively healthy subjects (307 males and 320 females; average age, 49.6±16.5 years) were enrolled. We included at least 50 males and 50 females in each decade of life between the 20s and the 70s. We measured intervertebral disk height from T10/T11 to L5/S1, vertebral body height from T10 to S1 on lateral neutral radiographs. Lumbar disk degeneration was defined according to the Pfirrmann classification in sagittal plane magnetic resonance imaging.
Results
Age-related decreases in intervertebral disk height were most prominent at L4/L5 in middle-aged and elderly individuals of both sexes. The grade of disk degeneration significantly increased with age in both genders at every level. Mild disk degeneration was observed even in the 20s. The disk degeneration occurred around the L4/L5 level. Although grade V disk degeneration was not identified for males in the 20s and the 30s, it appeared after the 40s and then increased further with age. The intervertebral disk height at the lower lumbar disks decreased with a progression in the disk degeneration grade in both genders.
Conclusions
This large-scale cross-sectional analysis of the thoracolumbar spine in relatively healthy subjects demonstrated that lumbar disk height narrowing progresses with age and is correlated with the progression of disk degeneration.
Keywords: thoracolumbar spine, intervertebral disk height, disk degeneration, healthy subjects, age-related and gender differences
Introduction
As a part of aging one of the universal and natural processes in the human body is intervertebral disk degeneration, which leads to loosing of elasticity of the disk due to diminished proteoglycans and water retaining molecules in the disk. As the water in the disk reduces, the capacity of the disk to resist compression and torque also reduces impairing the disk height and structural integrity1).
Magnetic resonance imaging (MRI) is routinely used by physicians to assist in the clinical diagnosis of disk degeneration2,3). To facilitate communication between clinicians regarding the degree of disk degeneration in patients, several MRI-based metrics have been developed; among them is the gold-standard Pfirrmann et al3) 5-grade system, which mentions that the disks could be rated by independent raters with reasonably high confidence and reproducibility developed by Urrutia et al4).
Visual assessment of disk height and other features seen in T2 weighted images is included in this classification. A lower score is given if a nominal height is maintained, provided that other aspects of the visual inspection complemented that finding. The association between disk height loss and degeneration is also documented by several other studies3,5-7).
Although the intervertebral disk height is estimated to decrease with age-related degeneration, few studies have evaluated the relationship between intervertebral disk height and degeneration of disk in a large age- and sex-balanced cohort6). Such extensive data would enable individualized treatment on the basis of the patient's age and sex. Nevertheless, to the best of our knowledge, there are no reports that have summarized anatomical age-related intervertebral disk height and degenerative disk changes in the thoracolumbar spine or examined sex-specific differences.
Thus, to investigate the relationship between intervertebral disk height and thoracolumbar spine disk degeneration, we conducted a large sex- and age-balanced cohort study of 627 relatively healthy volunteers. This study primarily aimed to establish age-related changes and gender-specific differences of intervertebral disk height and thoracolumbar spine disk degeneration of relatively healthy subjects in a large cohort. Additionally, we evaluated the relationship between the degree of the thoracolumbar disk height and disk degeneration.
Materials and Methods
Study population
After obtaining the approval from the institutional review board of Chubu Rosai Hospital (IRB approval no., 2009-2) and officially announcing the study purpose, we recruited relatively healthy Japanese volunteers who provided written informed consent. Sensory or motor symptoms such as clumsiness, numbness, weakness, and gait disturbance; severe low back pain; spinal trauma or congenital spinal deformity history; brain or spinal surgery history; and neurological diseases like neuropathy and cerebral ischemic disease and neuropathy along with females with pregnancy, worker's compensation received by individuals or presenting with symptoms post motor vehicle accident, and those in whom there was difficulty in examining the sagittal radiograph parameters of lumbosacral transitional anomalies or spinal malformations were excluded from the study. Visual analog scale measurements of the lower back, buttock, and leg pain were taken before deciding on the inclusion of patients in this study and excluded cases with severe pain anywhere above 80 mm as cases with severe pain8). Finally, a total of 627 relatively healthy subjects (307 males and 320 females; mean age, 49.6±16.5 years) with appropriate imaging results were enrolled; at least 50 subjects from each sex were included in the following age groups: 20-29, 30-39, 40-49, 50-59, 60-69, and 70-79 years (Table 1).
Table 1.
Demographics of Healthy Subjects at Present Study.
| Decade | Males | Females | |
|---|---|---|---|
| 20s | Number | 50 | 52 |
| Age (years) | 26.0±2.3 | 25.0±2.7 | |
| Body height (cm) | 171.3±6.3 | 158.8±5.5 | |
| Body weight (kg) | 65.1±9.9 | 51.3±5.6 | |
| BMI (kg/m2) | 22.2±2.9 | 20.4±1.8 | |
| 30s | Number | 51 | 50 |
| Age (years) | 35.0±3.0 | 35.0±3.0 | |
| Body height (cm) | 170.4±6.0 | 159.1±6.5 | |
| Body weight (kg) | 67.2±10.9 | 52.5±7.3 | |
| BMI (kg/m2) | 23.1±3.2 | 20.7±2.6 | |
| 40s | Number | 50 | 57 |
| Age (years) | 44.5±3.1 | 44.8±3.0 | |
| Body height (cm) | 172.9±5.1 | 156.4±5.7 | |
| Body weight (kg) | 71.7±13.5 | 54.2±8.8 | |
| BMI (kg/m2) | 23.9±4.4 | 22.2±3.7 | |
| 50s | Number | 56 | 51 |
| Age (years) | 54.2±2.7 | 53.7±2.5 | |
| Body height (cm) | 168.3±5.8 | 156.4±4.9 | |
| Body weight (kg) | 68.5±9.6 | 54.8±9.5 | |
| BMI (kg/m2) | 24.1±3.1 | 22.4±3.9 | |
| 60s | Number | 50 | 60 |
| Age (years) | 64.5±2.9 | 64.7±3.1 | |
| Body height (cm) | 166.1±6.1 | 154.5±5.5 | |
| Body weight (kg) | 63.8±7.5 | 52.3±7.7 | |
| BMI (kg/m2) | 23.1±2.3 | 21.9±3.2 | |
| 70s | Number | 50 | 50 |
| Age (years) | 73.3±2.6 | 73.2±2.6 | |
| Body height (cm) | 165.4±5.8 | 151.9±4.7 | |
| Body weight (kg) | 64.0±6.8 | 51.5±7.2 | |
| BMI (kg/m2) | 23.5±2.5 | 22.3±2.8 | |
| Total | Number | 307 | 320 |
| Age (years) | 49.7±16.4 | 49.6±16.7 | |
| Body height (cm) | 169.1±6.4 | 156.1±6.0 | |
| Body weight (kg) | 66.7±10.2 | 52.8±7.9 | |
| BMI (kg/m2) | 23.3±3.2 | 21.7±3.2 |
Values given are means±standard deviation unless otherwise specified.
BMI indicates body mass index.
To measure the body height of vertebrae and intervertebral disk height, we obtained lateral neutral thoracolumbar radiographs with the subject in the recumbent position. We measured the vertebral body height at the anterior wall, center, and posterior wall at each vertebral level (from T10 to L5) and intervertebral disk height at the anterior edge, center, and posterior edge at each disk level (from T10/T11 to L5/S1)9). 1.5-Tesla superconducting magnet (Signa Horizon Excite HD version 12; GE Healthcare, UK) was used to perform MRI scans. We obtained MRI to evaluate the degree of disk degeneration. Slice thicknesses of 3 and 4 mm in the sagittal and axial planes, respectively, were done to perform the scans. In the sagittal scans, T1-weighted images [fast spin-echo repetition time (TR), 450 ms; echo time (TE), 13 ms], and T2-weighted images (fast spin-echo TR, 4,000 ms; TE, 85 ms) were obtained. Axial scans were performed by using T2-weighted images (fast spin-echo TR, 4,000 ms; TE, 102 ms). All the images were transferred to a computer in Digital Imaging and Communications in Medicine format, and under the supervision of a certified spine surgeon, an experienced radiation technologist measured each parameter using Osiris 4 imaging software (Icestar Media Ltd, Essex, UK) as described previously10-14).
We evaluated disk degeneration at thoracolumbar spinal levels, including T10/T11, T11/T12, T12/L1, L1/L2, L2/L3, L3/L4, L4/L5, and L5/S1. According to the grading system proposed by Pfirrmann et al (Supplemental Table 1)3,15). Two spine surgeons (F.K. and K.S.) graded the degree of disk degeneration into five grades using T2-weighted neutral sagittal images. We defined lumbar disk degeneration according to the Pfirrmann classification system (Fig. 1). We assessed the disk degeneration grade between decades or gender at the eight levels (from T10/T11 to L5/S1).
Figure 1.
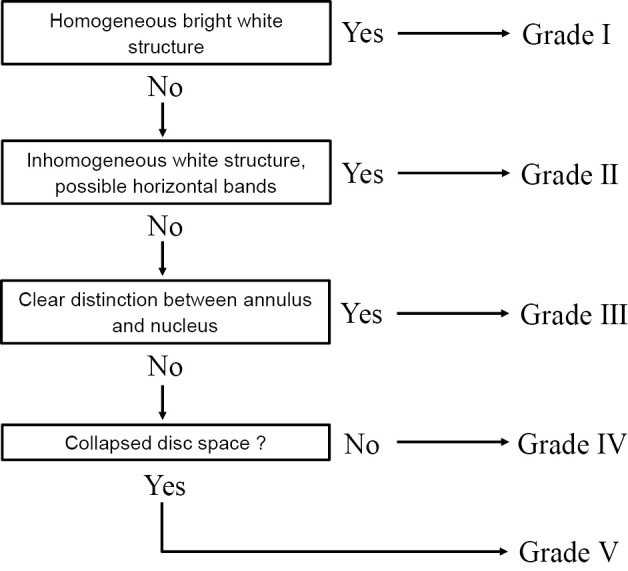
Algorithm for the grading system and assessment of lumbar disk degeneration grade using the Pfirrmann classification system.
To reduce the potential influence of physique such as body height, the absolute value of the actual measurement was adjusted by the parameters of the same individual. We proposed a measurement termed the disk index. The ratio of disk height to vertebral body height is defined as disk index and was calculated to evaluate the narrowing of the disk space using the formula: [(intervertebral disk height at the center)/(vertebral body height at the center) × 100%]. We calculated the disk index from T10/T11 to L5/S1 levels using the cranial vertebral body height and assessed the L5/S1 level using the L5 vertebral body height.
Statistical analysis
SPSS software version 27.0 (IBM Corp., Armonk, NY, USA) was used for analyses of data, and mean ± standard deviation was used to express all values. For nonparametric analysis of differences between males and females, the Mann-Whitney U-test was used, and p<0.05 was considered statistically significant.
Results
Table 1 mentions the descriptive characteristics including height, weight, and body mass index; this figure shows that body height tends to decrease with increasing age.
Vertebral body height at the anterior wall, center, and posterior wall gradually increased from T10 to L3; the shortest height was at T10, and the longest was at L3 or L4 or L5 in all age groups and both sexes. In all the age groups, the vertebral body heights were shorter in females than in males. The height at the anterior wall, center, and posterior wall slightly decreased with increasing age in both sexes, at most vertebral levels. The height at the center was shorter compared with that at the anterior and posterior walls. The vertebral body height at the posterior wall was longer than that at the anterior wall in the thoracolumbar region from T10 to L2 (Table 2, 3).
Table 2.
Vertebral Body Height at Each Vertebral Level in Males on Lateral Plain Radiography (mm).
| Decade | 20s | 30s | 40s | 50s | 60s | 70s | Total | |
|---|---|---|---|---|---|---|---|---|
| Anterior wall | T10 | 27.4±2.2 | 27.6±2.0 | 27.4±1.9 | 27.1±2.3 | 26.3±1.8 | 26.3±2.1 | 27.0±2.1 |
| T11 | 28.2±2.2 | 28.4±2.1 | 28.3±2.4 | 27.5±2.1 | 26.7±2.1 | 27.1±2.2 | 27.7±2.3 | |
| T12 | 29.2±2.5 | 29.8±1.9 | 29.5±2.5 | 28.8±1.9 | 28.3±2.3 | 28.6±2.4 | 29.0±2.3 | |
| L1 | 30.7±2.2 | 31.1±2.1 | 31.2±2.3 | 30.6±2.0 | 29.6±2.1 | 29.9±2.8 | 30.5±2.3 | |
| L2 | 33.0±2.1 | 33.3±2.1 | 33.5±2.2 | 32.4±2.1 | 31.3±2.3 | 31.6±3.2 | 32.5±2.5 | |
| L3 | 34.0±2.3 | 34.7±1.9 | 34.5±2.4 | 33.8±2.5 | 32.7±2.8 | 32.6±2.4 | 33.7±2.5 | |
| L4 | 33.9±1.9 | 34.4±2.2 | 34.5±2.4 | 33.9±2.2 | 32.9±2.6 | 32.0±3.2 | 33.6±2.6 | |
| L5 | 34.9±2.4 | 35.7±2.4 | 35.2±2.6 | 34.5±3.1 | 33.7±2.8 | 33.1±2.9 | 34.5±2.8 | |
| Center | T10 | 26.4±1.9 | 26.3±2.0 | 26.6±1.8 | 26.2±2.0 | 25.6±1.7 | 25.9±1.7 | 26.2±1.9 |
| T11 | 28.1±2.0 | 28.2±1.8 | 28.0±2.0 | 27.6±1.9 | 27.3±1.6 | 27.3±1.8 | 27.7±1.9 | |
| T12 | 30.0±2.1 | 30.6±1.8 | 30.1±2.2 | 29.5±1.8 | 29.1±1.7 | 29.3±1.8 | 29.8±2.0 | |
| L1 | 31.8±2.0 | 32.1±1.7 | 32.1±1.9 | 31.5±1.9 | 30.7±1.6 | 30.8±2.2 | 31.5±2.0 | |
| L2 | 32.4±1.8 | 32.7±1.6 | 33.0±2.1 | 31.9±2.1 | 31.1±1.8 | 32.1±2.5 | 32.2±2.1 | |
| L3 | 32.8±1.8 | 33.2±1.8 | 33.3±2.3 | 32.6±2.4 | 31.9±2.1 | 32.2±2.3 | 32.7±2.2 | |
| L4 | 33.2±1.7 | 33.6±1.6 | 33.5±2.5 | 32.7±2.5 | 31.9±2.6 | 32.3±2.7 | 32.9±2.4 | |
| L5 | 32.5±2.3 | 33.3±2.1 | 32.3±3.0 | 31.9±3.1 | 31.0±2.6 | 31.6±2.6 | 32.1±2.7 | |
| Posterior wall | T10 | 28.4±2.1 | 29.1±2.1 | 28.6±2.3 | 28.4±2.1 | 28.1±2.1 | 27.9±2.2 | 28.4±2.2 |
| T11 | 30.9±2.3 | 31.3±2.3 | 30.9±2.4 | 30.6±2.4 | 30.3±2.3 | 30.4±2.6 | 30.7±2.4 | |
| T12 | 33.3±2.3 | 33.7±2.4 | 33.7±2.4 | 33.2±1.9 | 32.8±2.5 | 32.9±2.4 | 33.3±2.3 | |
| L1 | 35.2±2.0 | 35.7±2.1 | 35.8±2.4 | 35.1±2.1 | 34.6±2.0 | 35.4±2.1 | 35.3±2.2 | |
| L2 | 35.5±2.0 | 35.7±2.1 | 36.1±2.4 | 34.9±2.2 | 34.6±2.0 | 35.6±2.5 | 35.4±2.2 | |
| L3 | 35.2±2.0 | 35.2±2.0 | 35.4±2.5 | 34.7±2.3 | 34.0±2.4 | 34.1±3.1 | 34.8±2.5 | |
| L4 | 33.4±2.0 | 33.7±2.0 | 33.9±2.5 | 33.2±2.2 | 32.5±2.2 | 32.3±3.3 | 33.2±2.5 | |
| L5 | 31.2±2.5 | 31.7±1.8 | 30.8±2.9 | 30.3±3.2 | 30.4±2.7 | 30.0±2.8 | 30.7±2.8 | |
Values given are means±standard deviation unless otherwise specified.
Table 3.
Vertebral Body Height at Each Vertebral Level in Females on Lateral Plain Radiography (mm).
| Decade | 20s | 30s | 40s | 50s | 60s | 70s | Total | |
|---|---|---|---|---|---|---|---|---|
| Anterior wall | T10 | 24.8±1.9 | 24.6±1.8 | 25.2±1.7 | 24.5±1.6 | 23.5±3.4 | 23.9±1.9 | 24.5±1.9 |
| T11 | 25.8±1.8 | 25.7±1.5 | 26.1±2.0 | 25.5±1.6 | 24.5±1.7 | 24.6±2.3 | 25.3±1.9 | |
| T12 | 27.8±2.2 | 27.6±2.0 | 28.2±2.0 | 27.8±1.7 | 26.3±3.2 | 26.5±3.2 | 27.4±2.5 | |
| L1 | 29.9±2.1 | 29.6±2.0 | 30.1±1.7 | 29.5±1.8 | 28.8±2.4 | 27.7±3.0 | 29.3±2.3 | |
| L2 | 32.0±2.2 | 31.6±1.9 | 32.3±1.9 | 31.8±2.4 | 30.6±2.9 | 29.8±3.6 | 31.4±2.7 | |
| L3 | 33.4±2.1 | 33.1±2.1 | 33.1±2.0 | 33.0±2.3 | 31.9±2.5 | 31.0±2.7 | 32.6±2.4 | |
| L4 | 33.4±2.4 | 32.8±1.7 | 33.3±1.8 | 32.7±2.4 | 31.4±2.9 | 31.0±3.1 | 32.4±2.6 | |
| L5 | 33.8±2.4 | 33.2±2.0 | 33.8±2.5 | 33.6±2.3 | 31.5±2.9 | 31.2±2.4 | 32.9±2.7 | |
| Center | T10 | 23.7±2.1 | 23.2±1.5 | 24.2±1.9 | 23.9±2.3 | 23.6±2.3 | 22.7±1.9 | 23.6±2.1 |
| T11 | 25.4±2.2 | 24.9±1.6 | 25.5±2.1 | 25.1±1.5 | 25.0±1.9 | 24.5±2.1 | 25.1±1.9 | |
| T12 | 27.8±2.2 | 27.2±1.8 | 27.6±2.0 | 27.4±1.5 | 26.9±2.5 | 26.3±2.9 | 27.2±2.2 | |
| L1 | 29.8±2.1 | 29.5±1.6 | 29.8±1.8 | 29.1±1.8 | 28.6±2.1 | 27.7±3.0 | 29.1±2.2 | |
| L2 | 30.7±2.2 | 30.8±2.1 | 30.8±2.1 | 30.3±2.0 | 29.6±2.3 | 28.3±3.3 | 30.1±2.5 | |
| L3 | 31.6±2.2 | 31.5±2.2 | 31.1±1.8 | 31.1±2.0 | 30.7±2.4 | 29.4±2.8 | 30.9±2.3 | |
| L4 | 31.7±2.3 | 31.6±2.1 | 31.9±1.9 | 31.1±2.1 | 30.5±2.6 | 29.3±2.8 | 31.0±2.5 | |
| L5 | 30.8±2.5 | 30.7±2.2 | 30.3±4.6 | 30.6±2.3 | 29.4±3.0 | 28.7±2.7 | 30.1±3.1 | |
| Posterior wall | T10 | 25.2±2.0 | 25.1±2.0 | 25.7±2.0 | 25.5±1.8 | 25.1±1.9 | 24.7±2.0 | 25.2±2.0 |
| T11 | 27.5±2.4 | 27.2±2.1 | 27.7±2.0 | 27.7±1.8 | 27.0±1.9 | 27.0±1.9 | 27.3±2.0 | |
| T12 | 30.0±2.4 | 29.9±2.0 | 30.0±2.3 | 30.4±1.9 | 29.5±2.6 | 29.3±2.8 | 29.8±2.4 | |
| L1 | 32.2±2.4 | 32.0±2.0 | 32.3±2.3 | 32.1±2.0 | 31.6±2.6 | 30.6±2.8 | 31.8±2.4 | |
| L2 | 33.1±2.2 | 33.1±2.2 | 33.0±2.0 | 32.9±2.4 | 32.3±2.5 | 31.2±2.6 | 32.6±2.4 | |
| L3 | 33.3±2.1 | 32.8±2.1 | 32.6±1.8 | 32.8±2.0 | 32.0±2.4 | 31.3±2.7 | 32.4±2.3 | |
| L4 | 31.5±2.4 | 31.7±2.1 | 31.4±1.8 | 31.5±2.3 | 30.4±2.5 | 29.1±2.5 | 30.9±2.4 | |
| L5 | 29.5±2.5 | 29.0±2.0 | 29.4±2.3 | 28.9±2.2 | 28.0±2.8 | 27.6±2.5 | 28.7±2.5 | |
Values given are means±standard deviation unless otherwise specified.
The intervertebral disk height at the anterior edge, center, and posterior edge gradually increased from T10/T11 to L4/L5 or L5/S1; the shortest height was at T10/T11, and the longest was at L3/L4 or L4/L5 or L5/S1 in all age groups and both sexes. In females, the disk heights at most disk levels were shorter than in males. In middle-aged and elderly individuals of both sexes, age-related decreases in disk height were most prominent at L4/L5 at the center and posterior edge. The height at the posterior edge was shorter than that at the anterior edge and center. The intervertebral disk height at the anterior edge increased gradually with increasing age in both sexes, except in the 70s. The intervertebral disk height at the center decreased gradually with increasing age in both sexes, at the lower lumbar disks. The intervertebral disk height at the posterior edge did not remarkably change with age in either sex, except the lower lumbar disks (Table 4, 5).
Table 4.
Intervertebral Disk Height at Each Disk Level in Males on Lateral Plain Radiography (mm).
| Decade | 20s | 30s | 40s | 50s | 60s | 70s | Total | |
|---|---|---|---|---|---|---|---|---|
| Anterior edge | T10/T11 | 6.3±1.7 | 6.6±1.8 | 6.3±1.2 | 6.4±1.7 | 7.0±1.8 | 7.0±2.0 | 6.6±1.7 |
| T11/T12 | 7.1±1.6 | 7.3±2.0 | 7.2±1.5 | 7.6±2.0 | 8.0±1.8 | 7.9±2.2 | 7.5±1.9 | |
| T12/L1 | 8.4±1.5 | 8.6±1.9 | 8.6±2.1 | 8.8±1.9 | 9.2±1.9 | 9.0±2.2 | 8.8±1.9 | |
| L1/L2 | 9.7±2.0 | 10.2±2.2 | 10.4±2.1 | 10.7±2.2 | 10.2±1.8 | 11.3±2.4 | 10.7±2.3 | |
| L2/L3 | 11.1±2.2 | 11.9±2.6 | 12.3±2.3 | 12.5±2.7 | 13.0±3.2 | 12.4±3.1 | 12.2±2.7 | |
| L3/L4 | 12.6±2.4 | 13.7±3.0 | 13.9±2.5 | 13.7±3.2 | 14.3±2.9 | 13.9±3.6 | 13.7±3.0 | |
| L4/L5 | 14.5±2.8 | 15.3±3.0 | 14.9±3.4 | 15.0±3.7 | 15.0±3.9 | 14.4±4.5 | 14.9±3.5 | |
| L5/S1 | 15.5±6.9 | 14.5±3.2 | 15.4±4.1 | 15.1±4.6 | 16.0±3.9 | 15.5±4.6 | 15.3±4.7 | |
| Center | T10/T11 | 6.6±1.0 | 7.0±1.3 | 6.7±1.3 | 6.7±1.5 | 7.3±1.3 | 6.9±1.4 | 6.9±1.3 |
| T11/T12 | 7.2±1.1 | 7.2±1.2 | 7.5±1.3 | 7.6±1.3 | 8.0±1.8 | 7.7±1.2 | 7.5±1.3 | |
| T12/L1 | 7.6±1.0 | 8.1±1.1 | 8.2±1.5 | 8.4±1.2 | 8.8±1.3 | 8.8±1.4 | 8.3±1.3 | |
| L1/L2 | 9.0±1.4 | 9.2±1.2 | 9.5±1.8 | 9.4±1.6 | 10.2±1.8 | 9.9±2.1 | 9.6±1.7 | |
| L2/L3 | 10.5±1.6 | 11.0±1.5 | 11.2±1.8 | 11.2±1.7 | 10.9±2.1 | 10.2±2.6 | 10.8±1.9 | |
| L3/L4 | 11.1±1.7 | 11.6±1.7 | 11.8±1.9 | 11.3±1.6 | 11.3±2.2 | 10.7±2.4 | 11.3±1.9 | |
| L4/L5 | 11.4±2.0 | 11.8±1.5 | 11.5±2.5 | 10.7±2.3 | 10.0±3.1 | 9.8±3.3 | 11.0±2.6 | |
| L5/S1 | 9.8±2.5 | 9.6±2.2 | 10.2±2.6 | 9.8±3.0 | 9.5±3.2 | 9.2±3.1 | 9.8±2.8 | |
| Posterior edge | T10/T11 | 4.4±1.2 | 4.3±1.1 | 4.6±1.2 | 4.4±1.3 | 4.8±1.3 | 4.6±1.4 | 4.5±1.3 |
| T11/T12 | 5.1±1.1 | 4.9±1.1 | 5.0±1.5 | 4.9±1.4 | 5.4±1.8 | 5.0±1.5 | 5.0±1.4 | |
| T12/L1 | 4.6±1.0 | 4.8±1.0 | 5.1±1.3 | 4.9±1.3 | 5.3±1.3 | 4.8±1.5 | 4.9±1.3 | |
| L1/L2 | 5.8±1.3 | 6.0±1.2 | 6.0±1.7 | 6.2±1.4 | 6.1±1.3 | 5.5±1.6 | 5.9±1.4 | |
| L2/L3 | 6.9±1.8 | 7.6±1.4 | 7.6±1.7 | 7.1±1.5 | 6.6±1.5 | 6.1±1.6 | 7.0±1.7 | |
| L3/L4 | 7.9±1.9 | 8.4±1.3 | 8.2±1.4 | 7.3±1.3 | 7.2±1.6 | 6.7±1.8 | 7.6±1.6 | |
| L4/L5 | 8.5±1.5 | 8.6±1.4 | 8.0±2.0 | 7.7±2.4 | 7.3±2.0 | 7.0±2.5 | 7.9±2.0 | |
| L5/S1 | 8.1±5.5 | 7.2±1.7 | 7.2±2.5 | 6.5±2.3 | 7.2±3.5 | 6.2±2.3 | 7.0±3.2 | |
Values given are means±standard deviation unless otherwise specified.
Table 5.
Intervertebral Disk Height at Each Disk Level in Females on Lateral Plain Radiography (mm).
| Decade | 20s | 30s | 40s | 50s | 60s | 70s | Total | |
|---|---|---|---|---|---|---|---|---|
| Anterior edge | T10/T11 | 5.3±1.3 | 5.5±1.5 | 5.7±1.9 | 5.9±1.8 | 6.6±1.7 | 5.7±1.7 | 5.8±1.7 |
| T11/T12 | 5.9±1.1 | 6.4±1.6 | 6.2±1.7 | 6.3±1.6 | 7.2±1.7 | 6.2±1.9 | 6.4±1.6 | |
| T12/L1 | 6.3±1.2 | 7.1±1.7 | 7.0±1.7 | 7.3±1.5 | 8.1±1.6 | 7.2±1.7 | 7.2±1.7 | |
| L1/L2 | 7.7±1.2 | 8.8±2.1 | 8.8±2.2 | 9.3±2.0 | 10.1±2.1 | 9.3±2.2 | 9.0±2.1 | |
| L2/L3 | 9.3±1.6 | 10.6±2.5 | 10.8±2.3 | 10.7±2.9 | 11.7±2.5 | 11.0±2.6 | 10.7±2.5 | |
| L3/L4 | 11.1±2.4 | 12.5±2.7 | 12.1±2.9 | 12.2±3.1 | 12.8±3.3 | 11.9±2.5 | 12.1±2.9 | |
| L4/L5 | 12.9±2.4 | 14.0±3.1 | 13.2±2.8 | 12.9±3.2 | 13.9±3.7 | 12.8±3.3 | 13.3±3.2 | |
| L5/S1 | 12.0±2.8 | 12.9±2.6 | 13.2±3.2 | 13.2±4.2 | 14.0±4.7 | 14.4±4.7 | 13.5±4.8 | |
| Center | T10/T11 | 5.9±1.0 | 6.2±1.2 | 6.1±1.3 | 6.0±1.0 | 6.4±1.3 | 6.1±1.3 | 6.1±1.2 |
| T11/T12 | 6.3±1.0 | 7.0±1.1 | 6.9±1.5 | 6.7±1.1 | 7.0±1.3 | 6.9±1.7 | 6.8±1.3 | |
| T12/L1 | 6.6±1.1 | 7.3±1.0 | 7.1±1.3 | 7.5±1.3 | 7.9±1.2 | 7.9±1.3 | 7.4±1.3 | |
| L1/L2 | 7.8±1.4 | 8.3±1.3 | 8.6±1.6 | 8.9±1.3 | 9.3±1.7 | 8.9±1.7 | 8.6±1.6 | |
| L2/L3 | 9.3±1.4 | 9.7±1.8 | 9.7±1.5 | 9.7±1.7 | 9.8±2.1 | 9.7±2.2 | 9.7±1.8 | |
| L3/L4 | 10.1±1.6 | 10.5±1.9 | 10.0±1.9 | 10.1±2.0 | 10.0±2.2 | 10.1±2.2 | 10.1±2.0 | |
| L4/L5 | 10.3±1.7 | 10.5±1.9 | 10.0±1.9 | 9.4±2.2 | 9.3±2.7 | 9.3±2.3 | 9.9±2.2 | |
| L5/S1 | 9.0±1.8 | 8.9±2.0 | 9.3±2.7 | 8.4±2.3 | 9.0±3.3 | 9.0±2.4 | 9.0±2.6 | |
| Posterior edge | T10/T11 | 4.6±1.2 | 4.6±1.2 | 4.6±1.1 | 4.5±1.1 | 4.6±1.2 | 4.2±0.9 | 4.5±1.1 |
| T11/T12 | 4.7±1.1 | 4.7±1.2 | 4.8±1.3 | 4.8±1.3 | 5.2±1.4 | 4.9±1.2 | 4.9±1.3 | |
| T12/L1 | 4.7±1.1 | 4.6±1.1 | 5.0±1.2 | 4.7±1.1 | 5.5±1.6 | 5.0±1.5 | 4.9±1.3 | |
| L1/L2 | 5.6±0.9 | 5.7±1.1 | 6.0±1.3 | 5.7±1.1 | 5.6±1.4 | 5.8±1.7 | 5.8±2.2 | |
| L2/L3 | 6.7±1.2 | 6.8±1.6 | 6.7±1.5 | 6.2±1.1 | 6.1±1.6 | 6.0±1.8 | 6.4±1.5 | |
| L3/L4 | 7.4±1.3 | 7.7±1.5 | 7.3±1.6 | 6.5±1.5 | 6.2±1.7 | 6.3±1.8 | 6.9±1.6 | |
| L4/L5 | 8.0±1.8 | 8.1±1.6 | 7.6±1.8 | 6.6±1.7 | 7.3±1.9 | 6.6±2.0 | 7.4±1.9 | |
| L5/S1 | 7.3±1.7 | 7.3±1.9 | 7.2±2.1 | 6.2±1.6 | 7.4±4.5 | 6.9±2.5 | 7.2±3.4 | |
Values given are means±standard deviation unless otherwise specified.
Disk index gradually decreased with increasing age in middle-aged and elderly individuals in males, with the L4/L5 level being the most prominent. Males in their 70s had multiple levels of intervertebral disk narrowing when compared with females. Unexpectedly, the disk index in females did not change with age (Table 6).
Table 6.
Disk Index in Each Disk Level (%).
| Decade | 20s | 30s | 40s | 50s | 60s | 70s | Total | |
| Males | T10/T11 | 25.1±4.3 | 26.6±5.7 | 25.0±4.4 | 25.7±5.9 | 28.5±5.4 | 26.9±5.8 | 26.3±5.4 |
| T11/T12 | 25.9±4.4 | 25.7±4.5 | 26.8±4.9 | 27.6±4.7 | 29.7±5.8 | 28.2±4.8 | 27.3±5.0 | |
| T12/L1 | 25.5±3.8 | 26.4±3.6 | 27.1±4.9 | 28.4±4.7 | 30.4±5.1 | 30.2±5.0 | 28.0±4.9 | |
| L1/L2 | 28.5±4.7 | 28.7±3.9 | 29.8±5.2 | 29.9±5.3 | 33.5±6.2 | 32.1±6.9 | 30.4±5.7 | |
| L2/L3 | 32.5±5.3 | 33.5±4.6 | 34.0±5.4 | 35.1±5.4 | 35.2±7.4 | 31.8±8.8 | 33.7±6.4 | |
| L3/L4 | 34.0±5.8 | 35.0±5.2 | 35.4±5.9 | 34.9±5.5 | 35.5±7.4 | 33.3±7.5 | 34.7±6.3 | |
| L4/L5 | 34.6±6.4 | 35.1±4.7 | 34.5±8.5 | 32.8±7.5 | 35.1±9.8 | 30.4±10.5 | 33.7±8.2 | |
| L5/S1 | 30.3±8.1 | 29.0±6.9 | 31.8±9.2 | 31.5±10.1 | 34.8±10.8 | 29.1±9.5 | 31.1±9.3 | |
| Decade | 20s | 30s | 40s | 50s | 60s | 70s | Total | |
| Females | T10/T11 | 24.9±4.7 | 26.6±5.3 | 25.4±5.7 | 25.2±4.1 | 27.2±5.1 | 26.8±6.2 | 26.0±5.3 |
| T11/T12 | 25.0±4.2 | 28.4±4.8 | 26.9±5.7 | 26.7±4.6 | 28.2±5.5 | 28.4±7.2 | 27.3±5.5 | |
| T12/L1 | 23.9±3.9 | 26.8±4.3 | 25.6±4.8 | 27.4±5.1 | 29.8±5.0 | 30.5±7.0 | 27.3±5.5 | |
| L1/L2 | 26.4±4.6 | 28.2±4.5 | 28.7±5.2 | 30.8±4.4 | 32.5±5.9 | 32.6±7.9 | 29.9±6.0 | |
| L2/L3 | 30.0±4.7 | 31.6±5.4 | 31.5±5.4 | 32.3±6.6 | 33.5±8.2 | 35.1±10.4 | 32.4±7.2 | |
| L3/L4 | 32.0±4.9 | 33.3±5.7 | 32.3±6.3 | 32.4±6.5 | 33.0±7.9 | 35.0±8.9 | 33.0±6.9 | |
| L4/L5 | 32.6±5.3 | 33.2±6.1 | 31.5±6.6 | 30.2±6.7 | 33.5±9.8 | 32.4±9.0 | 32.3±7.5 | |
| L5/S1 | 29.6±6.6 | 29.0±6.3 | 30.7±9.2 | 27.6±7.8 | 31.3±11.0 | 32.8±10.2 | 30.2±8.8 | |
Values given are means±standard deviation unless otherwise specified.
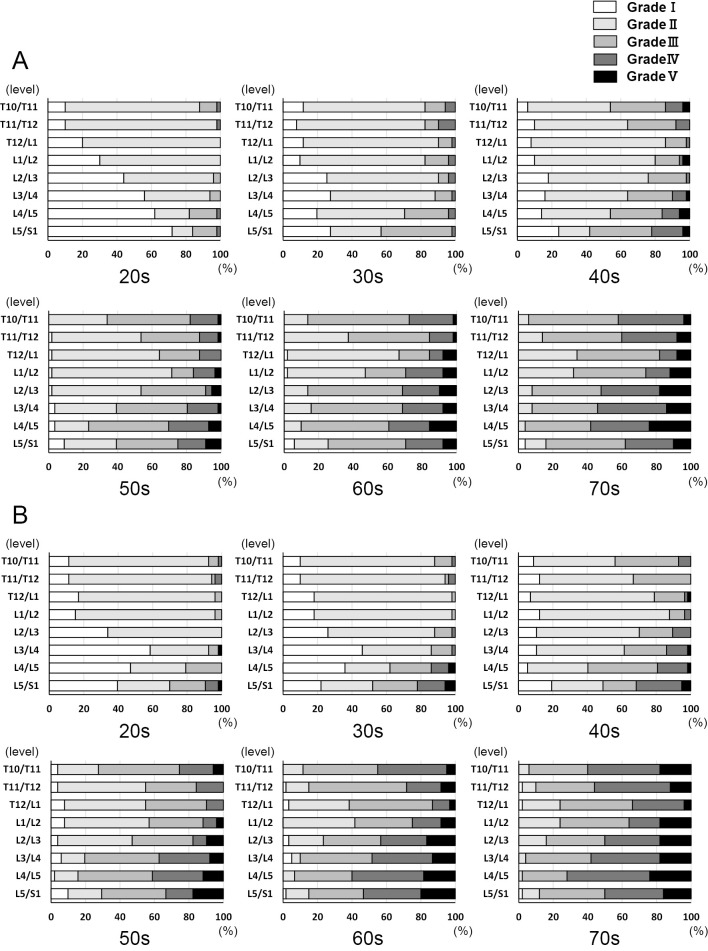
At every age level in both genders, the grade of disk degeneration at the lumbar level increased. We observed that even in the 20s, there was mild disk degeneration. Although Grade V disk degeneration was not identified for males who were in their 20s and 30s, it appeared for males in their 40s and then increased further with age. The first and second most severely degenerated disks in every decade were L4/L5. The disk degeneration occurred around the L4/L5 level (Fig. 2).
Figure 2.
Lumbar disk degeneration using the Pfirrmann classification system in each decade in (A) males and (B) females.
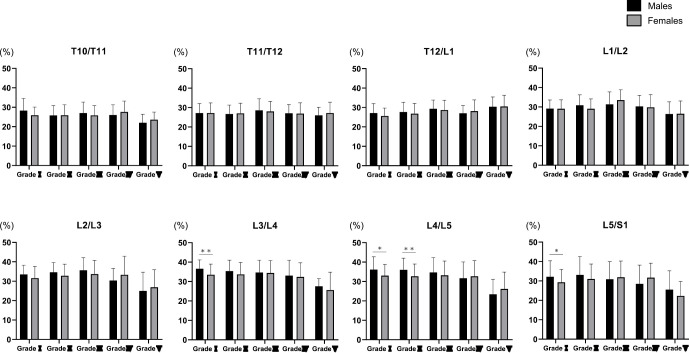
In both the genders along with disk degeneration grade, the disk index from L2/L3 to L5/S1 levels also decreased. The disk index from T10/T11 to L1/L2 levels did not change with a progression in the disk degeneration grade in both genders. There was a significant difference between genders in grade I from the L3/L4 to L5/S1 levels; the disk index in females was lower than in males (p<0.05 to p<0.01). There was also a significant difference between genders grade II at the L4/L5 level; the disk index in females was lower than that in males (p<0.01, Fig. 3).
Figure 3.
Relationship between disk index and thoracolumbar disk degeneration grade at each level.
Values are expressed as mean±SD. *p<0.05; **p<0.01
Discussion
This largest cross-sectional study is the first to report age-related changes and gender-specific differences in thoracolumbar disk height and also to evaluate the relationship between the degree of degeneration of disk and disk height in relatively healthy subjects to the best of our knowledge. Our main findings show that mild thoracolumbar disk degeneration begins in the 20s, thoracolumbar degeneration of disk and height narrowing progresses with age especially after the 40s, mainly at L4/L5 level and the degree of lumbar disk height narrowing was significantly correlated with the grade of degeneration of disk.
With aging, there is a gradual degeneration of the intervertebral disks gradually, which causes disk herniation and degenerative disk disease6). There is a broad burden on society with these conditions. This is well supported by Boos et al. who graded the degenerative changes in 180 cadaveric sagittal lumbar segment slices and reported that there is a significant association between the grade of degenerative change with age6). One of the best radiographic models for detecting degeneration of disk, which also has been widely used in the past few decades to evaluate musculoskeletal disorders is MRI16). Additionally, there have been various cross-sectional studies that have used MRI to elucidate the natural history of human aging and degeneration of disk17,18).
There have been several reported studies on the relationship between disk degeneration and age6,18,19). Boden et al. performed MRI on 67 subjects without low back pain, sciatica, or neurogenic claudication and found that 20% and 36% of subjects who were 60 years old had a herniated nucleus pulposus17). Cheung et al. study on 1043 volunteers investigated lumbar spine MRIs and found that 40% of individuals below the age of 30 years had degeneration of intervertebral disk at lumbar level, with the prevalence of intervertebral degeneration of disk increasing progressively to over 90% by the age of 50-55 years. The most prevalent levels of disk degenerative changes that increase with age are L4/L5 and L5/S119).
In the present study, vertebral body height at the center slightly decreased with increasing age at most vertebral levels. The decrease with age in vertebral body height was more pronounced in females than in males. Although disk index gradually decreased with increasing age in middle-aged and elderly individuals in males, the disk index in females did not change with age. It is speculated that disk index in females was affected by the decrease in vertebral body height compared with males.
This present study found that intervertebral disk height at the center gradually increased from T10/T11 to L4/L5; the shortest height was at T10/T11, and the longest was at L3/L4 or L4/L5 in all decades and both sexes. In middle-aged and elderly individuals of both sexes, age-related degenerative disk height loss was most prominent at L4/L5. As the number of disk surgeries performed increases in the future, these results will serve as useful baseline information for clinicians planning surgical intervention. Owing to their differences from younger subjects, elderly subjects may require special surgical consideration.
The results of the present study indicate that the intervertebral disk height at the center decreased gradually with increasing age in both sexes, at the lower lumbar disks. Lumbar disks are more likely to undergo disk degeneration than thoracic disks, which has been recognized previously, and lower lumbar disks are more prone to undergo severe degeneration than upper lumbar disks20,21). Because greater loading in bending causes disk prolapse leading to bending injuries to the annulus22).
Some of the limitations of this present study that warrant discussion are. First, as the study cohort was limited to Japanese population the generalizability of our findings is limited. Second, only relatively healthy subjects were enrolled in the current study, which could have led to a selection bias in favor of healthy participants only. However, although subjects were all relatively healthy, some had pathological or mild symptomatic backgrounds, which could affect the results. Considering that previous reports show that intraobserver and interobserver reproducibility of MRI measurements was high, measurement was performed only once by one unique observer4). A previous study reported that the overall interobserver agreement of the Pfirrmann classification using the intraclass correlation coefficient was excellent or almost perfect using the weighted kappa. Intraobserver agreement was also excellent, or almost perfect using the weighted kappa4). These measurements of radiographs were carried out by a well-experienced radiological technician with extensive knowledge of anatomy9-11). Our data set was sufficiently large for most evaluations; however, we compared individuals between ages as this was a cross-sectional rather than longitudinal investigation. As another limitation, we obtained radiographs in the recumbent position to make an evaluation that is not in the same standing position as MRI. Although osteoporosis might affect the age-related change of vertebral height, bone mineral density was not investigated in this study22,23). Despite these limitations, this cross-sectional study is the largest of its kind to the best of our knowledge. By comparing degeneration of disk and disk height data from relatively healthy subjects in this study to symptomatic patients in the future, this could lead to determining disk degeneration patterns that result in symptoms.
Age-related changes in disk height of the thoracolumbar spine are gaining more importance than ever because of the increasing number of reconstructive surgeries conducted for lumbar disk disorders. To understand the natural changes in thoracolumbar spine degeneration over time a long-term follow-up study is needed. Although it is practically difficult to observe age-related changes over a subject's entire life span. Thus, to substitute a longitudinal analysis, a large-scale cross-sectional observational study can be conducted. In our study, 627 relatively healthy volunteers were enrolled, and at least 50 subjects belonging to each sex were included in each age group. This study is one of the largest cohort studies conducted on thoracolumbar disk morphology, with a sex ratio of almost 1:1. The reliability of our results is because of the large sample size and balanced sex and age distribution of the study population.
Conclusion
Lumbar disk height narrowing progresses with age and is correlated with the progression of degeneration of the disk is concluded by this large-scale cross-sectional analysis of thoracolumbar spine MRI data in relatively healthy subjects.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: None
Author Contributions: MM and HN drafted and prepared the manuscript. All authors were involved in the data collection. MM performed the statistical analysis. All authors read, critically reviewed, and approved the final version of the submitted article.
Ethical Approval: This study was approved by the institutional review board of Chubu Rosai Hospital (IRB approval no., 2009-2).
Informed Consent: All participants in this study obtained informed consent.
Supplementary Material
Supplemental Table 1
Acknowledgement
We are grateful to Dr. Fumihiko Kato of Chubu Rosai Nursing School, Japan Organization of Occupational Health and Safety, for their great contribution to this study.
References
- 1.Jarman JP, Arpinar VE, Baruah D, et al. Intervertebral disc height loss demonstrates the threshold of major pathological changes during degeneration. Eur Spine J. 2015;24(9):1944-50. [DOI] [PubMed] [Google Scholar]
- 2.Miller TT. Imaging of disk disease and degenerative spondylosis of the lumbar spine. Semin Ultrasound CT MR. 2004;25(6):506-22. [DOI] [PubMed] [Google Scholar]
- 3.Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26(17):1873-8. [DOI] [PubMed] [Google Scholar]
- 4.Urrutia J, Besa P, Campos M, et al. The Pfirrmann classification of lumbar intervertebral disc degeneration: an independent inter- and intra-observer agreement assessment. Eur Spine J. 2016;25(9):2728-33. [DOI] [PubMed] [Google Scholar]
- 5.Benneker LM, Heini PF, Anderson SE, et al. Correlation of radiographic and MRI parameters to morphological and biochemical assessment of intervertebral disc degeneration. Eur Spine J. 2005;14(1):27-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boos N, Weissbach S, Rohrbach H, et al. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo award in basic science. Spine. 2002;27(23):2631-44. [DOI] [PubMed] [Google Scholar]
- 7.Haefeli M, Kalberer F, Saegesser D, et al. The course of macroscopic degeneration in the human lumbar intervertebral disc. Spine. 2006;31(14):1522-31. [DOI] [PubMed] [Google Scholar]
- 8.Nakashima H, Ito K, Katayama Y, et al. The level of conus medullaris in 629 healthy Japanese individuals. J Clin Med. 2021;10(14):3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Machino M, Nakashima H, Ito K, et al. Age-related degenerative changes and sex-specific differences in osseous anatomy and intervertebral disc height of the thoracolumbar spine. J Clin Neurosci. 2021;90:317-24. [DOI] [PubMed] [Google Scholar]
- 10.Yukawa Y, Kato F, Suda K, et al. Normative data for parameters of sagittal spinal alignment in healthy subjects: an analysis of gender specific differences and changes with aging in 626 asymptomatic individuals. Eur Spine J. 2018;27(2):426-32. [DOI] [PubMed] [Google Scholar]
- 11.Yukawa Y, Matsumoto T, Kollor H, et al. Local sagittal alignment of the lumbar spine and range of motion in 627 asymptomatic subjects: age-related changes and sex-based differences. Asian Spine J. 2019;13(4):663-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yukawa Y, Kato F, Suda K, et al. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: radiographic data from over 1,200 asymptomatic subjects. Eur Spine J. 2012;21(8):1492-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kato F, Yukawa Y, Suda K, et al. Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: magnetic resonance imaging of over 1,200 asymptomatic subjects. Eur Spine J. 2012;21(8):1499-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Machino M, Yukawa Y, Imagama S, et al. Age-related and degenerative changes in the osseous anatomy, alignment, and range of motion of the cervical spine: a comparative study of radiographic data from 1016 patients with cervical spondylotic myelopathy and 1230 asymptomatic subjects. Spine. 2016;41(6):476-82. [DOI] [PubMed] [Google Scholar]
- 15.Nakashima H, Yukawa Y, Suda K, et al. Cervical disc protrusion correlates with the severity of cervical disc degeneration: a cross-sectional study of 1211 relatively healthy volunteers. Spine. 2015;40(13):E774-9. [DOI] [PubMed] [Google Scholar]
- 16.Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(3):403-8. [PubMed] [Google Scholar]
- 18.Okada E, Daimon K, Fujiwara H, et al. Ten-year longitudinal follow-up MRI study of age-related changes in thoracic intervertebral discs in asymptomatic subjects. Spine. 2019;44(22):E1317-24. [DOI] [PubMed] [Google Scholar]
- 19.Cheung KM, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine. 2009;34(9):934-40. [DOI] [PubMed] [Google Scholar]
- 20.Wang YX, Griffith JF, Ma HT, et al. Relationship between gender, bone mineral density, and disc degeneration in the lumbar spine: a study in elderly subjects using an eight-level MRI-based disc degeneration grading system. Osteoporos Int. 2011;22(1):91-6. [DOI] [PubMed] [Google Scholar]
- 21.Weiler C, Schietzsch M, Kirchner T, et al. Age-related changes in human cervical, thoracal and lumbar intervertebral disc exhibit a strong intra-individual correlation. Eur Spine J. 2012;21(6):S810-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wáng JQ, Káplár Z, Deng M, et al. Thoracolumbar intervertebral disc area morphometry in elderly Chinese men and women: radiographic quantifications at baseline and changes at year-4 follow-up. Spine. 2018;43(10):E607-14. [DOI] [PubMed] [Google Scholar]
- 23.Wang YX, Griffith JF, Zeng XJ, et al. Prevalence and sex difference of lumbar disc space narrowing in elderly Chinese men and women: osteoporotic fractures in men (Hong Kong) and osteoporotic fractures in women (Hong Kong) studies. Arthritis Rheum. 2013;65(4):1004-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1