Introduction
Many individuals develop persistent symptoms after recovering from Coronavirus disease 2019 (COVID-19), termed long COVID. We report the first case of a long COVID patient with new exertional chest pain and dyspnea after recovering from COVID-19. Evaluation culminated in a diagnosis of coronary microvascular dysfunction (CMD) on Positron Emission Tomography (PET), raising the possibility of CMD as an etiologic factor in long COVID syndrome.
Case history
A 53-year-old female with severe obesity (body mass index 50.7 kg⋅m2) and prior ablation for premature ventricular contractions (PVCs) presented with new persistent fatigue, exertional dyspnea, and mid-sternal chest pain, 4 weeks after recovering from a mild COVID-19 infection.
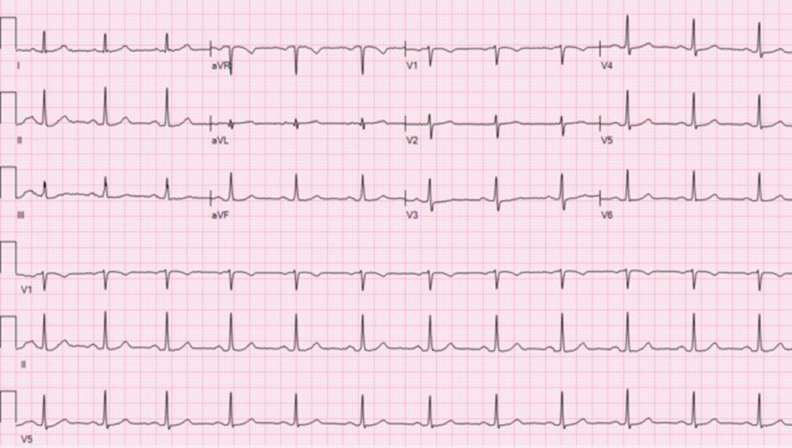
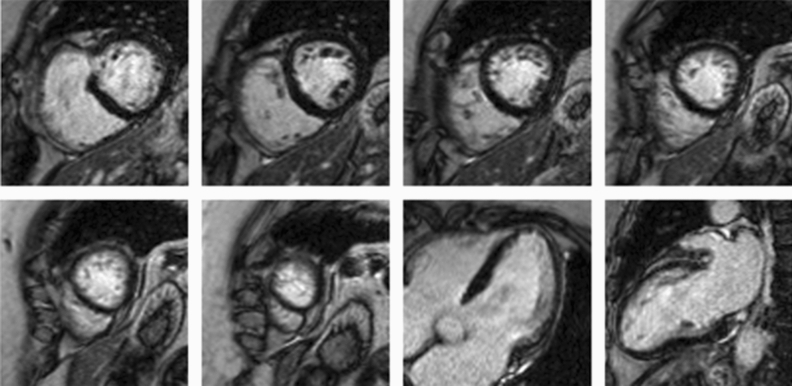
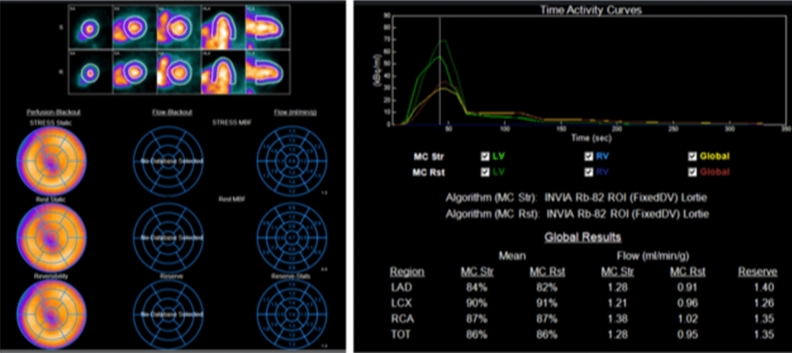
Electrocardiogram is shown in (Figure 1). Left and right ventricular function were normal on echocardiography, but pulmonary and ventricular filling pressures could not be reliably assessed. Vasodilator stress Cardiac Magnetic Resonance showed normal biventricular size and function without delayed enhancement or ischemia (Figure 2). Cardiopulmonary Exercise Testing showed a severely decreased maximal VO2 (38% of predicted), normal pulmonary function, and no EKG abnormalities with exercise. Catheterization showed normal pulmonary artery and filling pressures at rest, with a hypertensive response with exercise with no significant increase in filling pressures. Coronary angiography showed non-obstructive epicardial coronary disease (Figure 3).
Figure 1.
Electrocardiography was normal and she had no PVCs on extended Holter monitoring. Labs showed mild elevation of D-dimers (0.66 ug⋅ml) with normal high sensitivity Troponin T
Figure 2.
Cardiac MRI showed normal ventricular size and function without delayed enhancement; no stress inducible perfusion abnormalities
Figure 3.
Coronary angiography with epicardial coronary atherosclerotic disease without significant stenosis
CMD was suspected and cardiac PET showed a globally decreased myocardial flow reserve (1.34), confirming the diagnosis of CMD. The resting myocardial blood flow was normal (0.95 ml⋅g⋅min), and peak myocardial blood flow was 1.28 ml⋅g⋅min (Figure 4). Patient was treated with high intensity statin, nitrates, ranolazine, lisinopril, and referred for cardiac rehabilitation. Her symptoms improved and she recovered in one year.
Figure 4.
PET showed a globally decreased myocardial flow reserve, with resting myocardial blood flow was normal (0.95 ml⋅g⋅min), and peak myocardial blood flow of 1.28 ml⋅g⋅min
A link between CMD and COVID is conceivable and may explain some of the new or persistent cardiovascular symptoms after COVID1,2. Future research is needed to elucidate the effects of COVID-19 on coronary microvascular function.
Acknowledgments
Disclosures
Dr. Malahfji receives support from the Houston Methodist Research Institute. Dr. Al-Mallah receives research support from Siemens, unrelated to this work. None for the remaining authors.
Footnotes
Funding
Dr. Malahfji receives support from the Houston Methodist Research Institute. Dr. Al-Mallah receives research support from Siemens, unrelated to this work. None for the remaining authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Maan Malahfji, Email: mmalahfji@houstonmethodist.org.
Mouaz H. Al-Mallah, Email: mal-mallah@houstonmethodist.org.
References
- 1.Satterfield BA, Bhatt DL, Gersh BJ. Cardiac involvement in the long-term implications of COVID-19. Nat Rev Cardiol. 2021 doi: 10.1038/s41569-021-00631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crea F, Camici PG, Bairey Merz CN. Coronary microvascular dysfunction: an update. Eur Heart J. 2014;35:1101–1111. doi: 10.1093/eurheartj/eht513. [DOI] [PMC free article] [PubMed] [Google Scholar]