Abstract
Introduction
Herbal medicines (HM) and growth hormones (GH) are widely used to treat short stature (SS) in children. This systematic review aimed to evaluate the effectiveness and safety of combination therapy with HM and GH (CHG) compared to those of GH monotherapy (GHM) in children with SS.
Methods
We searched 17 electronic databases from inception to 1 April 2021. Only randomized controlled trials (RCTs) were included. Two authors independently performed the selection and quality assessment of the included studies using Cochrane Handbook criteria. Relative risk (RR) was used to measure dichotomous outcomes with a 95% confidence interval (CI). Mean difference (MD) or standard MD (SMD) was used to measure continuous outcomes with a 95% CI.
Results
Seven RCTs involving 455 participants with SS were included. Standard deviations in height (MD = 0.31, 95% CI: 0.24–0.38, p < 0.00001), and insulin-like growth factor binding protein-3 (MD = 1.39, 95% CI: 0.93–1.85, p < 0.00001) were significantly higher in the CHG group than in the GHM group. Growth velocity (MD = 1.82, 95% CI: 1.34–2.31, p < 0.00001) and insulin-like growth factor-1 (MD = 61.85, 95% CI: 55.80–67.90, p < 0.00001) were significantly higher in the CHG group. Adverse events were significantly lower in the CHG group (risk ratio: 0.10, 95% CI: 0.02–0.54, p = 0.007). However, the level of evidence was low.
Conclusions
CHG demonstrated significantly better efficacy than GHM for treating SS, with a low incidence of adverse events. However, since the level of evidence is low, methodologically standardized RCTs are required to verify these results.
1. Introduction
Individuals with short stature (SS) are two or more standard deviations (SDs) shorter than those with an average height of the same age and sex [1]. Approximately, 80% of individuals with SS have idiopathic SS (ISS), without identifiable deficiencies or disorders of growth hormone (GH) and endocrine, organ system, or genetic disorders [2]. Interest in height growth is expanding globally, and studies have reported that shorter height significantly impacts children's quality of life and depression scores [3, 4]. In particular, studies have reported that ISS can cause emotional issues in children and adolescents and result in socio-psychological and socio-economic effects [5, 6].
In Korea, recombinant human GH injection is a conventional treatment for ISS since the United States (US) Food and Drug Administration (FDA) approved the use of GH in 2003 [7]. Several studies have reported that administering GH in patients with ISS is effective in increasing the predicted adult height (PAH) and improving the growth velocity (GV) [8–10]. However, its long-term effects remain controversial [11].
There have been reports of certain side effects of GH, including elevated intracranial pressure, scoliosis, slipped capital femoral epiphysis, and type 2 diabetes [12]. It is recommended that side effects should be monitored, and fasting blood sugar and HbA1c levels should be measured every 3–6 months. In contrast, insulin-like growth factor-1 (IGF-1) and insulin-like growth factor binding protein-3 (IGFBP-3) should be tested every 6–12 months. Daily injections of GH and frequent follow-up blood tests are additional psychological burdens for children who undergo GH therapy, which often lasts for more than 2 years [12]. Furthermore, it is of concern that the efficacy decreases with prolonged treatment compared with that obtained during the first year of treatment. In Korea, survey results indicate low satisfaction with GH therapy (29.1%), and studies reveal that GH therapy does not positively impact children's quality of life and self-esteem [13, 14]. Due to various concerns, such as potential side effects and the fear of frequent injections among children and adolescents, complementary and alternative medical treatments are often sought to increase height growth [15]. Herbal medicine (HM) has been used to treat various diseases and is currently one of the most popular complementary and alternative medicines [16]. HM has been used for thousands of years in East Asia to treat growth disorders and SS. Previous studies used animal models to demonstrate that HM acted on different pathways from those targeted by GH by inducing the expression of IGF-1 and bone morphogenetic protein 2 and promoting longitudinal bone growth through cell proliferation in the epiphyseal plate [17, 18].
Systematic reviews on the treatment of SS primarily focused on the effects of GH [10, 19–21], and currently, investigations on the effects of HM are also being conducted [16, 22]. Several studies have been performed to determine the effects of combination therapy with HM and GH (CHG) for treating SS. However, currently, there is no review comparing the efficacy and safety of GH monotherapy (GHM) and CHG in patients with SS. Therefore, this study aimed to evaluate the effectiveness and safety of CHG compared to those of GHM in children with SS.
2. Methods
2.1. Study Protocol and Registration
The protocol of this systematic review and meta-analysis was registered on the Open Science Framework (OSF) platform, with the option to prospectively register a systematic review [23] (registration number: DOI 10.17605/OSF.IO/NMY5G). The protocol has been previously published [24].
2.2. Inclusion Criteria for Studies
2.2.1. Types of Studies
Randomized controlled trials (RCTs) evaluating the effectiveness of GHM and CHG in treating SS were included.
2.2.2. Participants
This study included children aged 0–18 years who exhibited decreased GV or were diagnosed with ISS according to the following diagnostic criteria: two or more SDs lower than the average height of an individual of the same age and sex, without identifiable deficiencies or disorders of GH.
2.2.3. Types of Interventions
In this review, we only included studies that compared CHG and GHM. The presentations of HM, such as decoction, capsules, tablets, pills, powders, and extracts, were not restricted. In addition, only HM prescribed by traditional East Asian medicine doctors was included in the study.
2.2.4. Outcomes
The primary outcome was an improvement in growth-related anthropometric indicators, such as PAH, GV, and SDs in height, and changes in growth-related hormones, such as IGF-1 and IGFBP-3. The secondary outcome was an improvement in height and weight. The incidence of adverse events (AE) during treatment was recorded.
2.3. Search Methods for the Identification of Studies
2.3.1. Electronic Searches
We searched Medline, EMBASE, Central, CINAHL, AMED, and the East Asian databases, such as OASIS, KTKP, KISS, KoreaMed, KMbase, RISS, DBPIA, CNKI, Wanfangdata, CQVIP, CiNii, and J-stage. All studies available in the respective databases, from inception to 1 April 2021, were included in the search strategy.
2.3.2. Search Strategy
The search terms and text words were: (“Short stature” [TIAB] OR “idiopathic short stature”[TIAB] OR “Growth disorder”[Mesh] OR “Dwarfism”[Mesh] OR “Failure to Thrive”[Mesh]) AND (“Herbal medicine”[Mesh] OR “Medicine, Korean Traditional”[Mesh] OR “Medicine, Chinese Traditional”[Mesh] OR “Medicine, Kampo”[Mesh] OR “Drug, Chinese Herbal”[Mesh] OR “Plant extract”[Mesh] OR “Plants, Medicinal”[Mesh] OR “traditional oriental medicine”[TIAB] OR “traditional Korean medicine”[TIAB] OR “traditional Chinese medicine”[TIAB] OR “kampo medicine”[TIAB] OR “herb∗”[TIAB]) AND (“Randomized Controlled Trial”[Publication Type] OR “Controlled clinical trial”[Publication Type] OR “randomized”[TIAB]). No language limitations were imposed. All details of the search strategy are described in the protocol article [24] and Supplementary Table 1.
2.4. Data Collection and Analysis
2.4.1. Study Selection
Two authors (SBS and JAL) independently performed the study selection. We excluded studies that did not fulfill the inclusion criteria (see Supplementary Table 2). Any disagreement was resolved through discussion and consensus with a third researcher (HLL). The selection process was recorded in the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow diagram (Figure 1).
Figure 1.

Flowchart showing the results of the literature search. AMED, Allied and Complementary Medicine Database; CENTRAL, Cochrane Central Register of Controlled Trials; CINAHL, Cumulative Index to Nursing and Allied Health Literature; CNKI, China National Knowledge Infrastructure; OASIS, Oriental Medicine Advanced Searching Integrated System; RISS, Research Information Service System; KISS, Korean Studies Information Service System; KTKP, Korean Traditional Knowledge Portal.
2.4.2. Data Extraction and Management
Two authors (SBS and HLA) independently performed data extraction using a data extraction form in Microsoft Excel (Microsoft, Redmond, WA, USA). In case of discrepancies, we rechecked the extracted data and attempted to resolve them through discussion. The unresolved issues after the discussion were referred to a third reviewer (HHL) for arbitration.
We extracted the following items: data for study identification (last name of the first author, publication year, and country); details of the participants (age, sex, height, and height percentile), sample size, the details of the interventions (treatment group, control group, duration of the intervention, and composition of HM, if possible), outcome measures, results, and AE. When data were missing in the reports, we contacted the corresponding author of the RCT for missing information.
2.4.3. Assessment of Risk of Bias in the Included Studies
Two researchers (SBS and HHL) assessed the risk of bias in the included studies according to the Cochrane Handbook criteria, version 5.2.0. We evaluated the following seven items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias as “Low risk,” “High risk”, and “Unclear risk” [25].
2.4.4. Measures of Treatment Effect
We used relative risk (RR) to measure dichotomous outcomes and mean difference (MD) for continuous outcomes with a 95% confidence interval (CI). If the studies presented results on different scales, we used the standard MD (SMD) with a 95% CI.
2.4.5. Assessment of Heterogeneity
Chi-squared and I2 tests were used to test for heterogeneity, and I2 > 50% indicated high heterogeneity. We performed meta-analyses using random- or fixed-effects models based on our analyses of the collected data. A fixed-effect model was used when no statistical heterogeneity was detected among the trials (I2 < 50%). In contrast, a random-effects model was used if methodological heterogeneity was detected.
2.4.6. Data Synthesis
We conducted the review in accordance with the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions. We performed analyses using Review Manager (RevMan) version 5.4 for Windows (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). We used GRADEpro software (McMaster University/Evidence Prime, Inc., Hamilton, Canada) to create a table summarising the findings. We assessed the primary and secondary outcomes, and p-values ≤0.025 were considered statistically significant.
2.4.7. Assessment of Reporting Biases
Due to the small number of included studies, we did not generate funnel plots to detect reporting biases.
2.4.8. Subgroup Analysis and Sensitivity Analyses
Due to the small number of included studies, subgroup analyses and sensitivity analyses to explore the sources of potential heterogeneity were not performed.
3. Results
3.1. Description of the Included Studies
3.1.1. Results of the Search
We identified 356 studies by searching electronic databases (Figure 1). In the Korea and Japan databases, no studies met the inclusion criteria. After excluding 108 duplicates, 202 studies were screened by reading their titles and abstracts. A total of 46 studies were potentially relevant, and full texts were screened for further assessment. Finally, seven studies [26–32] were included in this review.
3.1.2. General Characteristics of Included Studies
All seven RCTs [26–32] were conducted in China and published between 2015 and 2020; all were published in Chinese. The included studies involved 455 participants with ISS, and the sample sizes ranged from 20 to 45 participants. All details of the general characteristics of the included studies are presented in Supplementary Table 3.
3.1.3. Risk of Bias in the Included Studies
We observed that many RCTs had an unclear risk of bias in certain domains because we could not obtain information from the articles. Detailed information is shown in the “Risk of bias” graph and the “Risk of bias” summary (Figures 2 and 3). All details on the risk of bias in the included studies are summarised in Supplementary Table 3.
Figure 2.

Risk of bias graph.
Figure 3.

Risk of bias summary.
3.1.4. Excluded Studies
We excluded 39 articles after careful examination of full-text copies. Common reasons for excluding studies were: no random allocation and HM monotherapy as the experimental intervention (see Supplementary Table 2).
3.2. Meta-Analysis Results
3.2.1. Predicted Adult Height
None of the seven RCTs provided data on the PAH.
3.2.2. Growth Velocity
Six of the seven included RCTs [27–32] comparing the GV exhibited significant heterogeneity in the data (p < 0.00001, I2 = 92%, Figure 4). Owing to this significant heterogeneity in comparison, a random-effects model was applied. The results of the random-effects model analysis confirmed that the experimental group showed significant improvements in GV compared with the control groups (MD = 1.82, 95% CI: 1.34–2.31, p < 0.00001).
Figure 4.
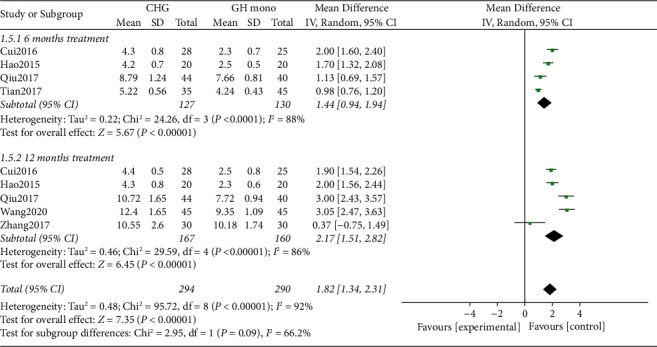
Forest plot comparing growth velocity between the CHG and GHM groups. CHG, combination therapy with herbal medicine and growth hormone; GHM, growth hormone monotherapy.
3.2.3. SDs in Height
Two of the seven included RCTs [26,29] involving 128 participants were evaluated for the changes in SDs in height, with no significant heterogeneity in the data (p = 1.00, I2 = 0%; Figure 5). The results of the fixed-effects model analysis combined with effect sizes confirmed a significant difference between the experimental and control groups (MD = 0.31, 95% CI: 0.24–0.38, p < 0.00001), with the experimental group outperforming the control group.
Figure 5.

Forest plot comparing standard deviations in height between the CHG and GHM groups. CHG, combination therapy with herbal medicine and growth hormone; GHM, growth hormone monotherapy.
3.2.4. Insulin-Like Growth Factor 1
Three of the seven included RCTs comparing IGF-1 showed no significant heterogeneity in the data [30–32] (p = 0.89, I2 = 0%; Figure 6). The results of the fixed-effects model analysis combined with effect sizes indicated a significant difference between the experimental and control groups (MD = 61.85, 95% CI: 55.80–67.90, p < 0.00001), with the experimental group outperforming the control group.
Figure 6.

Forest plot comparing insulin-like growth factor 1 between the CHG and GHM groups. CHG, combination therapy with herbal medicine and growth hormone; GHM, growth hormone monotherapy.
3.2.5. Insulin-Like Growth Factor Binding Protein-3
Two of the seven included RCTs [30, 31] comparing IGFBP-3 showed no significant heterogeneity in the data (p = 0.28, I2 = 13%, Figure 7). The results of fixed-effects model analysis combined with effect sizes confirmed a significant difference between the experimental and control groups (SMD = 1.39, 95% CI: 0.93–1.85, p < 0.00001), with the experimental group outperforming the control group.
Figure 7.
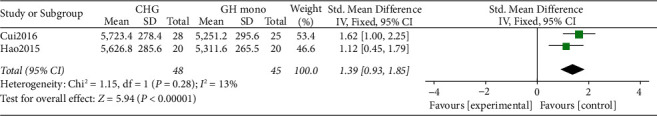
Forest plot comparing insulin-like growth factor binding protein-3 between the CHG and GHM groups. CHG, combination therapy with herbal medicine and growth hormone; GHM, growth hormone monotherapy.
3.2.6. Adverse Events
Three of the seven included studies [29–31] comparing AEs showed no significant heterogeneity in the data (p = 0.77, I2 = 0%; Figure 8). The results of fixed-effects model analysis combined with effect sizes indicated a significant difference between the experimental and control groups (RR = 0.10, 95% CI: 0.02–0.54, p = 0.007). The experimental group had a significantly lower rate of AE than the control group.
Figure 8.

Forest plot comparing adverse events between the CHG and GHM groups. CHG, combination therapy with herbal medicine and growth hormone; GHM, growth hormone monotherapy.
3.3. Level of Evidence
The level of evidence is presented in Table 1. When comparing the CHG group with the GHM group, there was a “moderate” level of evidence for SDs in height [26, 29], weight (kg) [30,31], and IGFBP-3 (ng/mL) [30, 31] and “low” level of evidence for height (cm) [26, 27, 29–31], IGF-1 (ng/mL) [30–32], and AE [29–31]. The evidence level for GV (cm/year) [27–32] was “very low”. The low level of evidence was largely due to a high risk of bias, high heterogeneity, and overlap in the 95% CIs.
Table 1.
Summary of findings.
| Patients or population: idiopathic short stature | |||||
|---|---|---|---|---|---|
| Intervention: CHG | |||||
| Comparison: GH monotherapy | |||||
| Outcomes | Anticipated absolute effects∗ (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with GH monotherapy | Risk with CHG | ||||
| Height (cm) | The mean height (cm) was 0 | MD 3.32 (2.7–3.93) higher | — | 420 (5 RCTs) | ⊕⊕○○ LOWa,b |
| Change in height SDs | The mean change in height SDS was 0 | MD 0.31 (0.24–0.38) higher | — | 128 (2 RCTs) | ⊕⊕⊕○ MODERATEa |
| Weight (kg) | The mean weight (kg) was 0 | MD 2.47 (1.83–3.11) higher | — | 186 (2 RCTs) | ⊕⊕⊕○ MODERATEa |
| Growth velocity (cm/year) | The mean growth velocity (cm/year) was 0 | MD 1.82 (1.34–2.31) higher | — | 584 (6 RCTs) | ⊕○○○ VERY LOWa,b,c |
| IGF-1 (ng/mL) | The mean IGF-1 was 0 | MD 61.85 (55.8–67.9) higher | — | 153 (3 RCTs) | ⊕⊕○○ LOWa,b |
| IGFBP-3 (ng/ml) | — | SMD 1.39 (0.93–1.85) higher | — | 93 (2 RCTs) | ⊕⊕⊕○ MODERATEa |
| Adverse events | 144 per 1 000 | 14 per 1 000 (3–78) | RR 0.10 (0.02–0.54) | 173 (3 RCTs) | ⊕⊕○○ LOWa,b |
GRADE Working Group grades of evidence; High certainty: We are very confident that the true effect lies close to that of the estimate of the effect; Moderate certainty: We are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; Low certainty: Our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect; Very low certainty: We have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of the effect. ∗The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). aIn all RCTs, the blinding of participants and personnel was incomplete. bConfidence intervals cross null effect. cHeterogeneity is very high (I2 = 92%). CI, confidence interval; MD, mean difference; SDs, standard deviation; SMD, standardized mean difference; RR, risk ratio.
4. Discussion
This review provides a quantitative evaluation of the clinical efficacy and safety of CHG for treating SS by integrating outcomes from seven clinical RCTs involving 455 participants with ISS. The results of our analyses demonstrated that the efficacy of CHG was significantly better than that of GHM for treating SS. These results included significant improvements in GV, IGF-1, IGFBP-3, SDs in height, height, and weight, and a lower incidence rate of AEs in the CHG group than in the GHM group.
We could not perform meta-analyses for all our predefined outcomes because the data on PAH were not reported in any of the included RCTs. In Korea, PAH is often used as a primary indicator in height growth-related studies [22, 33]. Clinical RCTs using PAH as a major focus should be conducted in the future. If a meta-analysis on the change in PAH is conducted, the effect of CHG and GHM on height growth can be confirmed in more diverse ways.
The GV and SDs in height are critical evaluation indicators in height growth research and are used in many studies. However, due to the methodological limitations of clinical research, most studies did not reflect variations according to participants' age or sexual maturity. Therefore, heterogeneity may have occurred in the interpretation of the results. In future clinical RCTs, it is necessary to address heterogeneity by varying recruitment according to children's age or sexual maturity.
The results of these analyses indicated that CHG was effective in maintaining a low incidence of AE. Four cases of headache were reported in the GHM group and one in the CHG group. Two cases of obesity, three cases of redness and swelling at the injection site, and two cases of a decrease in serum T4 concentration were reported in the GHM group. The side effects of recombinant human GH therapy, currently used as a conventional treatment for ISS, may include injection site hematoma, pain, headache, scoliosis, glucose intolerance, and compromised cardiorespiratory functions [34, 35]. In two [30, 31] of the three studies [29–31] that reported AE, obesity, decrease in serum T4 concentration, and redness and swelling at the injection site were reported in the GHM group. In contrast, no AE was reported in the CHG group. Therefore, CHG is believed to mitigate the side effects; however, the clinical significance is limited.
4.1. Limitations
Overall, the evidence from the present review supports using CHG to treat children with SS. However, the RCTs included in this systematic review have several significant limitations.
First, all the research was conducted in China, which could be attributed to the widespread use of HM in Asian countries; however, it can be a potential bias factor. Explicit strategies, including databases from China, South Korea, and Japan, were designed to implement all available searches, but no search results were found. Furthermore, since our search was conducted until March 2021, further research related to our review may have been published, which could be included in future research.
Second, no negative results were reported and there may have been a reporting bias. Although publication bias could not be verified due to the small number of included studies, the fact that no negative results were reported may be considered a bias.
Third, the methodological quality of the included studies was low. None of the seven included studies reported blinding of participants and personnel, and only one study reported allocation concealment. In addition, no studies used the consolidated standards of reporting trials (CONSORT) checklist.
Fourth, there was a limitation in increasing the research heterogeneity and reducing reliability. The intervention dosage was not specified, the long-term follow-ups were not performed, and variables that significantly impacted results, such as participants' age or sexual maturity, were not controlled.
Finally, none of the included studies suggested the mechanisms underlying the synergistic effect exhibited by GH and HM. This makes it difficult to judge the clinical significance of the combination therapy.
4.2. Implications for Practice
The results of this study suggest that CHG has a positive effect in treating SS compared to GHM. As a viable and integrated approach to treating SS, CHG can be used as an effective complementary and alternative medical treatment option in combination with conventional GH therapy. Therefore, in clinical practice, more integrated treatment approaches are required to improve the effectiveness of treatment.
4.3. Implications for Research
The literature included in this systematic review had poor methodological quality, resulting in a reduced recommendation grade and level of evidence for systematic evaluation. Therefore, future clinical research should be conducted while considering the following factors:
In compliance with the CONSORT checklist, randomization, allocation concealment, and blinding should be described in detail.
Methodological standardization of RCT evaluation related to composition, dosage, and usage of HM therapy is required.
In research on childhood growth, the heterogeneity of results should be addressed by considering the participants' age and sexual maturity when recruiting.
In many countries, well-designed, large-scale, high-quality, multicentre RCTs are necessary for a more reliable research evaluation.
5. Conclusion
CHG provided significant improvements in GV and changes in SDs in height compared to GHM, maintaining a low incidence of AE. Therefore, we can assume that HM can help improve the effectiveness of GH and reduce the side effects. Despite these benefits, there are some limitations, such as the poor methodological quality of the analyzed studies and the high heterogeneity of the results. Furthermore, a definite mechanism through which GH and HM synergistically improve height growth has not yet been described. Before CHG is accepted as an evidence-based treatment option in clinical practice, more methodologically improved research data are required.
Acknowledgments
The authors would like to thank Editage (https://www.editage.co.kr/) for English language editing. This work was supported by the Traditional Korean Medicine R&D Program, funded by the Ministry of Health and Welfare through the Korea Health Industry Development Institute (KHIDI) (Grant number HF20C0183), and the INNOPOLIS foundation funded by the Ministry of Science and ICT (MSIT) (Grant number 2020-DD-RD-0413).
Data Availability
The data used to support the findings of this study are included in the article as supplementary tables.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
All authors made a substantial contribution to this work. HLL, SBS, HLA, and JAL developed the review protocol. HLL and JAL contributed to the conception and design of the review. SBS and JAL read and screened abstracts and titles of potentially relevant studies. SBS and HLA were responsible for extracting data. SBS and HHL were responsible for rating the quality of the papers. SBS drafted the manuscript. JAL and HLL critically reviewed the draft and suggested amendments before submission.
Supplementary Materials
Supplementary Table 1. Details of search strategy; Supplementary Table 2. List of excluded studies; Supplementary Table 3. Characteristics of included studies.
References
- 1.Ranke M. B. Towards a consensus on the definition of idiopathic short stature. Hormone Research . 1996;45 doi: 10.1159/000184851. [DOI] [PubMed] [Google Scholar]
- 2.Pedicelli S., Peschiaroli E., Violi E., Cianfarani S. Controversies in the definition and treatment of idiopathic short stature (ISS) Journal of Clinical Research in Pediatric Endocrinology . 2009;1:105–115. doi: 10.4008/jcrpe.v1i3.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sandberg D. E., Gardner M. Short stature. Pediatric Clinics of North America . 2015;62(4):963–982. doi: 10.1016/j.pcl.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Backeljauw P., Cappa M., Kiess W., et al. Impact of short stature on quality of life: a systematic literature review. Growth Hormone & IGF Research . 2021;57-58 doi: 10.1016/j.ghir.2021.101392.101392 [DOI] [PubMed] [Google Scholar]
- 5.Wheeler P. G., Bresnahan K., Shephard B. A., Lau J., Balk E. M. Short stature and functional impairment: a systematic review. Archives of Pediatrics and Adolescent Medicine . 2004;158(3):236–243. doi: 10.1001/archpedi.158.3.236. [DOI] [PubMed] [Google Scholar]
- 6.Zlotkin D., Varma S. K. Psychosocial effects of short stature. Indian Journal of Pediatrics . 2006;73(1):79–80. doi: 10.1007/bf02758266. [DOI] [PubMed] [Google Scholar]
- 7.Cuttler L., Silvers J. B. Growth hormone and health policy. Journal of Clinical Endocrinology and Metabolism . 2010;95(7):3149–3153. doi: 10.1210/jc.2009-2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang J., Choi Y., Choi I., Kim H. S., Kim D. H. The effect of growth hormone on patients with growth hormone deficiency and idiopathic short stature. Korean Journal of Pediatrics . 2004;47:310–318. [Google Scholar]
- 9.Lee K., Han H. Effects of growth hormone therapy in children with idiopathic short stature. Korean Journal of Pediatrics . 2005;48:865–870. [Google Scholar]
- 10.Paltoglou G., Dimitropoulos I., Kourlaba G., Charmandari E. The effect of treatment with recombinant human growth hormone (rhGH) on linear growth and adult height in children with idiopathic short stature (ISS): a systematic review and meta–analysis. Journal of Pediatric Endocrinology & Metabolism . 2020;33(12):1577–1588. doi: 10.1515/jpem-2020-0287. [DOI] [PubMed] [Google Scholar]
- 11.Kim J. H., Chung H. R., Lee Y. A., et al. Growth responses to growth hormone therapy in children with attenuated growth who showed normal growth hormone response to stimulation tests. Korean Journal of Pediatrics . 2009;52(8):922–929. doi: 10.3345/kjp.2009.52.8.922. [DOI] [Google Scholar]
- 12.Lee K. H. Growth hormone therapy in short stature children. Journal of the Korean Medical Association . 2008;51(9):849–855. doi: 10.5124/jkma.2008.51.9.849. [DOI] [Google Scholar]
- 13.Theunissen N. C., Kamp G. A., Koopman H. M., Zwinderman K. A., Vogels T., Wit J. M. Quality of life and self–esteem in children treated for idiopathic short stature. The Journal of Pediatrics . 2002;140(5):507–515. doi: 10.1067/mpd.2002.123766. [DOI] [PubMed] [Google Scholar]
- 14.Huh K., Park M. J. Questionnaire–based analysis of growth–promoting attempts among children visiting a university growth clinic. Korean Journal of Pediatrics . 2009;52(5):576–580. doi: 10.3345/kjp.2009.52.5.576. [DOI] [Google Scholar]
- 15.Choi S., Park E. A clinical study of the pediatric patients who visited oriental medical Hospital for Growth Treatment. Journal of Pediatrics of Korean Medicine . 2018;32:51–62. [Google Scholar]
- 16.Lee B., Kwon C. Y., Jang S. Comparative effectiveness of east Asian traditional medicine for treatment of idiopathic short stature in children: a protocol for systematic review and network meta-analysis. Medicine (Baltimore) . 2020;99(43) doi: 10.1097/md.0000000000022856.e22856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim J. Y., Song M., Lee D., et al. Effect of HT042, herbal formula, on longitudinal bone growth in spontaneous dwarf rats. Molecules . 2013;18(11):13271–13282. doi: 10.3390/molecules181113271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cho S. M., Lee S. H., Lee D., et al. The Korean herbal formulation Yukmijihwangtang stimulates longitudinal bone growth in animal models. BMC Complementary and Alternative Medicine . 2017;17(1):p. 239. doi: 10.1186/s12906-017-1651-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loftus J., Heatley R., Walsh C., Dimitri P. Systematic review of the clinical effectiveness of Genotropin (somatropin) in children with short stature. Journal of Pediatric Endocrinology & Metabolism: Journal of Pediatric Endocrinology & Metabolism . 2010;23(6):535–551. doi: 10.1515/jpem.2010.092. [DOI] [PubMed] [Google Scholar]
- 20.Yang Y., Bai X., Yuan X., et al. Efficacy and safety of long–acting growth hormone in children with short stature: a systematic review and meta–analysis. Endocrine . 2019;65(1):25–34. doi: 10.1007/s12020-019-01950-9. [DOI] [PubMed] [Google Scholar]
- 21.Bryant J., Baxter L., Cave C. B., Milne R. Recombinant growth hormone for idiopathic short stature in children and adolescents. Cochrane Database of Systematic Reviews . 2007;18(3) doi: 10.1002/14651858.CD004440.pub2.CD004440 [DOI] [PubMed] [Google Scholar]
- 22.Kweon J., Cho S., Yu S. Review of clinical researches for herbal medicine treatment in pediatric growth – focusing on recent national studies. Journal of Pediatrics of Korean Medicine . 2018;32:103–112. [Google Scholar]
- 23.Pieper D., Rombey T. Where to prospectively register a systematic review. Systematic Reviews . 2022;11:p. 8. doi: 10.1186/s13643-021-01877-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shim S. B., Ahn H. R., Lee J. A., Lee H. L. Comparative effectiveness and safety of growth hormone monotherapy and combination therapy with herbal medicine and growth hormone in short stature children; A protocol for systematic review and meta–analysis. Medicine (Baltimore): Case Reports and Study Protocols . 2021;2(5):e0104–4. doi: 10.1097/md9.0000000000000104. [DOI] [Google Scholar]
- 25.Higgins J. P., Churchill R., Chandler J. Chapter 8. Assessing risk of bias in included studies. In: Higgins J. P., Altman D. G., Sterne J. A., editors. Cochrane Handbook for Systematic Reviews of Interventions Version 520 (Updated June 2017) Newyork, NY, USA: John Wiley & Sons; 2017. [Google Scholar]
- 26.Kong R. Clinical effect of integrated traditional Chinese and western medicine on children with idiopathic short stature. Cap Food Med . 2019;26:35–36. [Google Scholar]
- 27.Qiu Y. Guangzhou, China: Guangzhou University of Chinese Medicine; 2017. The clinical observation of the jianpi yishen party joint growth hormone for the treatment of dwarfism children. Master’s thesis. [Google Scholar]
- 28.Wang S. K., Feng B. Liu–jun–zi decoction and recombinant human growth hormones for the treatment of idiopathic short stature. Henan Med Res . 2020;29:4936–4938. [Google Scholar]
- 29.Tian H., Zeng Yh. Analysis of short–term curative effect of 35 cases of idiopathic short stature treat with the combination of Chinese and Western medicine. Journal of Pediatrics of Traditional Chinese Medicine . 2017;13:39–43. [Google Scholar]
- 30.Cui Y., Yu W., Liang W. Clinical study of spleen deficiency–decoction and growth hormone for the treatment of idiopathic dwarfism. Psychological Documents . 2016;22:61–62. [Google Scholar]
- 31.Hao Y. Effect of Jianpi Yishen therapy combined with recombinant human growth hormone on the treatment of idiopathic short stature and its effect on serum IGF–1 and IGFBP–3 expression. Modern Journal of Integrated Traditional Chinese and Western Medicine . 2015;24:2900–2902. [Google Scholar]
- 32.Zhang X. Tianjin, China: Tianjin University of Traditional Chinese Medicine; 2017. To explore the treatment of idiopathic short stature with TCM–WM and gene of ISS. Master’s thesis. [Google Scholar]
- 33.Kim E. J., Lim Y. J., Lee H. S., Hwang J. S. The effect of gonadotropin releasing hormone agonist and growth hormone on predicted adult height in girls with precocious puberty. Annals of Pediatric Endocrinology & Metabolism . 2007;12:111–118. [Google Scholar]
- 34.Wolfgram P. M., Carrel A. L., Allen D. B. Long–term effects of recombinant human growth hormone therapy in children with Prader–Willi syndrome. Current Opinion in Pediatrics . 2013;25(4):509–514. doi: 10.1097/mop.0b013e328362c7a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coutant R., Bosch Muñoz J., Dumitrescu C. P., et al. Effectiveness and overall safety of NutropinAq® for growth hormone deficiency and other paediatric growth hormone disorders: completion of the International Cooperative Growth Study, NutropinAq® European Registry (iNCGS) Frontiers in Endocrinology . 2021;12 doi: 10.3389/fendo.2021.676083.676083 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Details of search strategy; Supplementary Table 2. List of excluded studies; Supplementary Table 3. Characteristics of included studies.
Data Availability Statement
The data used to support the findings of this study are included in the article as supplementary tables.


