Abstract
Objective:
Innovative strategies are needed to reduce young adult drinking. Real-time feedback via mobile health (mHealth) technology (e.g., smartphone devices/apps) may facilitate moderate drinking, yet requires evidence of feasibility, acceptability and usability.
Method:
Young adults reporting frequent heavy drinking (N=99, Mage=23, 51% male) participated in a manualized, brief, motivational interview on recent typical and peak blood alcohol concentration (BAC), then were randomized to use 1 of 3 forms of technology: 1) smartphone breathalyzer device/app; 2) app that estimates BAC based on factors including sex, weight, number/types of drinks over time; or 3) self-text messaging after each drink. Technologies were tested initially in small-group laboratory alcohol self-administration sessions. Participants then completed a 2-week field test wherein they had free access to all 3 technologies. Participants reported on usability and acceptability.
Results:
Laboratory alcohol self-administration did not differ significantly by technology condition. The smartphone breathalyzer and BAC estimator app had favorable acceptability and usability. Participants used at least 1 form of technology on 67% of drinking days in the field period. In exploratory analyses, alcohol use during the field period was significantly lower than baseline including a decrease of nearly 1 drink per drinking day.
Conclusions:
These findings support the feasibility of research combining lab and field methods to test moderate drinking technologies in young adults. Findings further support the acceptability and usability of these technologies, along with young adults’ openness to using them. Exploratory results suggest potential efficacy of combined mobile technology intervention to be tested in subsequent controlled studies.
Keywords: technology, mHealth, harm reduction, negative consequences, motivational interviewing
Introduction
Alcohol use disorder is common among young adults, with a prevalence of 23% compared to 14% or less among older adults (Grant et al., 2017). About 35% of young adults report past-month heavy drinking (SAMHSA, 2018), which relates to consequences like traffic accidents and sexual assault (Hingson et al., 2017; Wilhite et al., 2018). Further, heavy drinking in this vulnerable period can have negative effects on the still developing brain (Bava & Tapert, 2010). Aspects of young adults’ lives (e.g., fewer responsibilities; Arnett, 2019) support alcohol misuse and relatedly, young adults typically have limited motivation to reduce drinking (Marino & Fromme, 2018) making intervention challenging. As a result, young adult alcohol misuse is a public health crisis and this population needs targeted interventions.
Although there is evidence to support the efficacy of motivational interviewing (M.I.)-based interventions for young adults (Tanner-Smith & Lipsey, 2015), effect sizes are modest (Huh et al., 2015). Personalized feedback is an efficacious component of M.I.-based interventions (Carey et al., 2012). Typically, these interventions give feedback based on aggregate self-reports over a period of time (e.g., past month) to motivate behavior change, but do not give feedback on drinking and related impairment in the moment (during, immediately before, or after drinking).
While feedback based on behavior in the aggregate has value, theory and evidence support a need for in-the-moment intervention. Behavioral economic theory highlights alcohol as immediately available and rewarding (Bickel et al., 2014; Vuchinich & Tucker, 1988). Young adults tend to be more impulsive and sensitive to reward than older adults as their frontal cortical development is outpaced by reward regions of their brain (Rutherford et al., 2010). Self-regulation theory posits that motivation can offset difficulty in resisting rewards (Muraven & Baumeister, 2000). However, young adults not seeking treatment may not have sufficient motivation to control drinking on their own (Epler et al., 2009; Weaver et al., 2013). Accordingly, evidence shows slowing pace of drinking is difficult. For instance, young adults report using moderate drinking strategies (e.g., counting drinks) less often than ancillary strategies (e.g., designated drivers) (DeMartini et al., 2013). Relatedly, a very brief, web-based intervention was efficacious when it included ancillary strategies, but not when it focused on direct strategies to slow drinking (Leeman et al., 2016). These collective findings suggest young adults need more help, preferably while drinking, to slow their pace of drinking and improve their decisions about whether to continue drinking. Efficacious, in-the-moment interventions could complement traditional interventions that occur outside the drinking context.
Technology, particularly smartphone applications (apps), are promising and could target drinking in the moment. Fortunately, young adults are open to technology to moderate drinking (Kazemi et al., 2013; Weaver et al., 2013) and over 90% of young adults in the United States own a smartphone (Pew, 2019). Although there are hundreds of apps for changing drinking (e.g., education, social support), little research has evaluated their efficacy (Kazemi et al., 2017). The only app with substantial efficacy data is designed to support recovery/abstinence (Gustafson et al., 2014; McTavish et al., 2012): a very different indication than facilitating moderate drinking in young adults who drink heavily. To our knowledge, the only published evidence of an app offering an advantage over a control condition in reducing young adult alcohol use was a small pilot trial (n=40) of an app providing self-monitoring, personalized feedback and behavioral strategies, as an adjunct to motivational interviewing in homeless young adults. The app did not provide in-the-moment feedback on impairment (Thompson Jr et al., 2020).
In considering in-the-moment interventions, reducing blood alcohol content (BAC) is a critical target, especially for young adults, who have the highest incidence of driving under the influence (Hingson et al., 2017; Lipari et al., 2016). Some individual interventions for young adults have reduced peak estimated BAC (eBAC), but effect sizes tend to be small (Carey et al., 2007). Most people have difficulty estimating BAC, particularly at higher drinking levels (Carey & Hustad, 2002; Grant et al., 2012). These findings highlight a need for concrete tools to provide accurate, in-the-moment BAC feedback targeted at young adult drinkers.
Fortunately, available smartphone technologies provide objective BAC feedback in the moment, including an app that produces estimates based on sex, weight, number of drinks, time elapsed, reported stomach fullness and recent drinking history (see Luczak et al., 2018). Estimates are potentially useful, but do not account for individual differences in alcohol metabolism (Turner et al., 2004). Intervention studies to date using BAC estimator apps have had mixed results including findings of increased drinking (Berman et al., 2019; Gajecki et al., 2014). However, these studies did not include an M.I.-based intervention to increase motivation to use the technology to reduce drinking. Apps that measure rather than estimate BAC will address limitations with BAC estimator apps and may have even greater harm reduction potential, particularly when coupled with an M.I.-based intervention.
Accordingly, breathalyzer apps have recently been developed to produce accurate readings in concert with a small, linked device (Brains, 2019). A small group of studies have used breath alcohol devices/apps to document abstinence in contingency management (Alessi & Petry, 2013; Koffarnus et al., 2018; Oluwoye et al., 2000). In addition, a recent small study reported formative research on a smartphone device/app-based-intervention, but without efficacy data (Min et al., 2020). Thus, while BAC-related smartphone technologies have promise, research has not sufficiently evaluated young adult use of these technologies to reduce drinking.
Research on BAC-related smartphone technologies will also need to address whether there are sex differences in efficacy, acceptability and usability. Women tend to reach higher BACs than men at a given number of drinks because they weigh less on average, have less total body water at a given weight (Ely et al., 1999) and less alcohol dehydrogenase to break alcohol down (Baraona et al., 2001). However, women also tend to have greater success with brief interventions (Carey et al., 2007) and use moderate drinking strategies more frequently (Prince et al., 2013). Thus, the value of these BAC-based smartphone interventions for women and men is an open question.
To address these gaps, after brief, M.I.-based counseling on BAC, this study evaluated feasibility, usability, acceptability, and efficacy of BAC-related, moderate drinking technologies during a laboratory alcohol self-administration session (Table 1; Leeman et al., 2013; 2018), followed by a 2-week field test in real world situations. To our knowledge, this is the first study to test multiple types of BAC apps as moderate drinking tools. We hypothesized the breathalyzer and BAC estimator would be associated with less laboratory alcohol self-administration than self-texting (i.e., lower eBAC, fewer drinks). For usability/ease, we predicted self-text would score higher than either of the other technologies. For acceptability, we predicted the BAC estimator and self-text would be equivalent in self-consciousness when using while the breathalyzer would score higher than self-text. However, we predicted the breathalyzer would score higher than self-text on perceived value. We also predicted participants would use the breathalyzer and BAC estimator more frequently in the lab than self-text. We planned to test for sex differences and based on the field period, compare frequency of use, alcohol drinking, acceptability and usability across the three technologies.
Table 1.
Summary of Procedures Involved in Alcohol Drinking Sessions
| Time | Procedures |
|---|---|
| Appointment earlier in day | BrAC reading, urine test, pregnancy test for women. Technology randomization, instruction and practice technology use with staff. |
| 1pm | Participants asked to eat lunch but stop eating at this time |
| 3:30–3:45p | Participants transported to simulated bar laboratory for the session. |
| 4pm | Participants arrive at simulated bar lab, then BrAC. Instructions/rules for the session reviewed, self-reports and cognitive/psychomotor tasks. Instructions and practice technology use again. Participants relinquished their personal phones |
| 5pm | Alcoholic and non-alcoholic self-administration begins, ad libitum. Participants’ eBAC tracked, not permitted to reach eBAC ≥ .10. Participants encouraged to use assigned technology but not to share results with others |
| 8pm | Alcohol self-administration ends. Small glass of water to remove mouth alcohol, self-reports, BrAC for all participants, then cognitive/psychomotor tasks. Participants’ personal phones returned. |
| 9pm/hourly | Self-reports, then BrAC for all participants |
| 11pm | Self-reports and BrAC. Technology acceptability and usability ratings. Instruction in and practice use of other two technologies not assigned for the session. Technology provided and apps put on participants’ own phones |
| 12am | Self-reports, BrAC. Released when BrAC <0.02%, ride home paid for by study |
Notes. BrAC = breath alcohol concentration, eBAC = estimated blood alcohol concentration
Methods
Participants
We recruited young adults ages 21–25 to an alcohol technology study using social media, other web ads and flyer postings. Inclusion criteria were self-report of 4 or more heavy drinking days (4 or more drinks for women, 5 or more for men), 1 or more days with an eBAC of 0.10% or higher, and 10 or more days with 1 or more alcoholic drinks in the past 30 days. Exclusion criteria were treatment-seeking or past-12-month substance misuse treatment; urine positive for illegal drugs except THC; current DSM-IV substance dependence except alcohol; history of medically-assisted detoxification or current withdrawal; 2 breath alcohol (BrAC) readings >0.00% at the outset of appointments; a medical issue contraindicating alcohol use; body mass index <18.5 or >35; pregnancy, lactation or birth control refusal in women; a recent prescription for or current psychotropic drug use; psychosis/severe psychiatric conditions; disliking beer; or past-12-month moderate drinking app use. The study was approved by the institutional review board. Data collection occurred between February 2017-April 2020.
The sample was divided about evenly between men and women. Regarding race and ethnicity, the sample was 63.6% white, non-Hispanic/Latino/a, 20.2% Hispanic/Latino/a, 8.1% Asian, 3% Black/African-American, 2% other or mixed race and 3% did not report. A slight majority (51.5%) were not currently students. On average, participants drank on more than half of the days in the month, reported heavy drinking about 1 out of every 3 days, nearly 6 drinks per drinking day, a mean eBAC almost twice the legal limit and peak eBAC almost 4 times the legal limit. There were no differences in demographics or baseline drinking across study technology conditions (Table 2).
Table 2.
Sample Characteristics by Study Technology Condition and Overall
| Variable | Smartphone Breathalyzer Cond. (n= 33) | BAC Estimator Condition (n= 33) |
Self-Texting Condition (n= 33) |
Overall (N= 99) |
|---|---|---|---|---|
| Percent male | 45.5% | 60.6% | 48.5% | 50.5% |
| Age | 22.67(1.29) | 23.03(1.02) | 22.79(1.39) | 22.83(1.24) |
| Race/ethnicity | ||||
| White non-Hispanic/Latino/a | 63.6% | 66.7% | 60.6% | 63.6% |
| Black/A-A, non-Hispanic/Latino/a | 6.1% | 0% | 3% | 3% |
| Hispanic/Latino/a | 18.2% | 21.2% | 21.2% | 20.2% |
| Asian | 6.1% | 9.1% | 9.1% | 8.1% |
| Other | 3% | 3% | 0% | 2% |
| Did not report | 3% | 0% | 6.1% | 3% |
| Non-student status | 51.5% | 54.5% | 48.5% | 51.5% |
| Current at least weekly smoker | 15.2% | 15.2% | 15.2% | 15.2% |
| Family history of alcohol problems | 21.2% | 48.5% | 33.3% | 34.3% |
| Alcohol abuse (lifetime/current) | 51.5/30.3% | 36.4/21.2% | 45.5/24.2% | 44.4/25.3% |
| Alc. dependence (LT/current) | 42.4/21.2% | 39.4/21.2% | 42.4/24.2% | 41.4/22.2% |
| Past 30-day alcohol frequency/quantity reported at screening: mean (SD), range of responses | ||||
| Frequency of any use | 16.55(4.32) 10 – 26 |
16.97(6.41) 10 – 30 |
15.42(5.15) 10 – 29 |
16.31(5.35) 10 – 30 |
| Drinks per week | 21.76(11.02) 9.57 – 56.93 |
22.51(13.36) 8.40 – 61.83 |
20.72(12.54) 7 – 66.27 |
21.66(12.24) 7 – 66.27 |
| Drinks per drinking day | 5.71(2.78) 2.62 – 15.6 |
5.60(2.01) 2.32 – 12.05 |
5.57(2.05) 2.73 – 12.91 |
5.63(2.29) 2.32 – 15.6 |
| Frequency of heavy drinking days | 9.45(4.84) | 10.30(5.63) | 8.55(3.71) | 9.43(4.80) |
| 4–23 | 4–23 | 4–18 | 4–23 | |
| Mean eBAC | .15% (.05%) .07%−.31% |
.14% (.04%) .06%−.26% |
.14% (.05%) .08%−.27% |
.14% (.05%) .06%−.31% |
| Peak eBAC | .35% (.12%) 0.20%−.83% |
.30% (.12%) 0.17%−0.70% |
.34% (.11%) .17%−.58% |
.33% (.12%) .17%−.83% |
| Peak drinking (number of drinks) | 13.55 (5.62) 6–30 |
11.97 (5.15) 6–25 |
13.36 (5.66) 6–26 |
12.96 (5.47) 6–30 |
Notes. A-A= African-American, eBAC = estimated blood alcohol concentration, heavy drinking day = 5 or more for men, 4 or more for women. There were no statistically significant differences across study technology condition for any of these variables.
Procedures (Figure 1)
Figure 1.
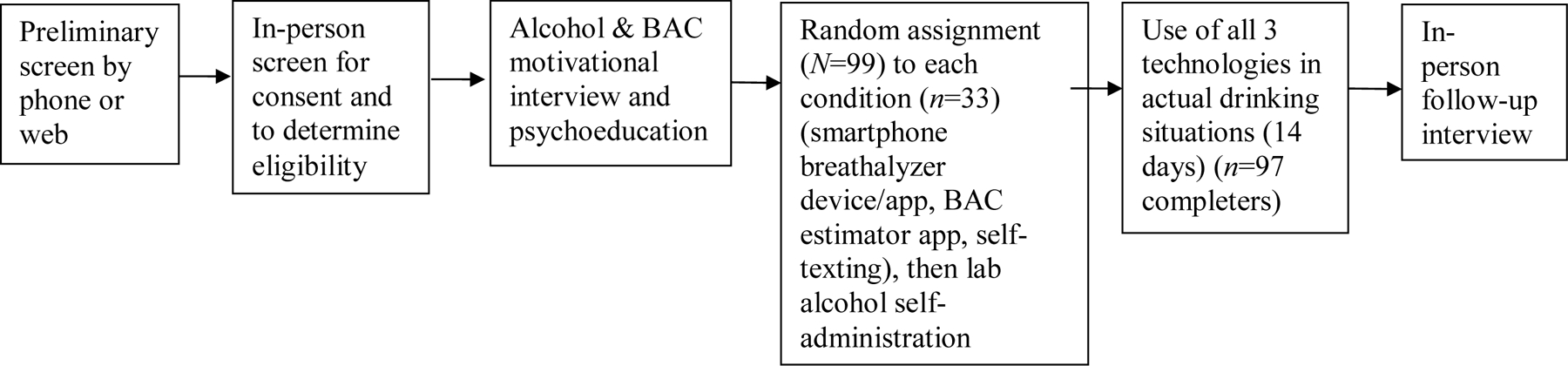
Steps Involved in Study Participation
Screening.
After pre-screening by web or phone, participants were scheduled for an in-person screen including informed consent; BrAC (must=0.00%); urine drug and pregnancy tests; Timeline Followback (TLFB; Sobell & Sobell, 2003) for past 30-day alcohol and cigarette use; medical history; diagnostic interview for substance use disorder; Clinical Institute Withdrawal Assessment (Sullivan et al., 1999); cognitive/psychomotor tests; and self-reports. Eligible participants unlikely to know each other were scheduled in groups of 3 for a drinking session.
BAC-focused counseling.
Before learning their technology condition, participants took part in 20–30 minutes of manualized, individual counseling on BAC, developed for this study (Leeman, Fucito, & Martens, 2017). The counseling was based on M.I. principles (Miller et al., 1992). Master’s or doctoral-level interventionists with M.I. experience read the manual and completed a 20-hour training based on a M.I.-based brief intervention trial (Martens et al., 2013). They completed at least three audio-recorded practice sessions and got written and verbal feedback on each from the supervising clinical psychologist, who determined when each interventionist delivered the intervention at a sufficient proficiency level based on these practice sessions. At that point, the interventionist was able to deliver the intervention to actual study participants. Participants received personalized feedback on typical quantity/frequency of alcohol use, and recent typical and peak eBAC. Interventionists provided BAC-related psychoeducation covering the ascending and descending limbs of the BAC curve and ways to drink to a safer BAC while seeking positive effects of drinking (e.g., during social events). Interventionists were blind to study technology condition.
M.I. competence and fidelity to the manual were assessed with a protocol similar to Martens and colleagues’ (2013) trial. Three external master’s or doctoral-level psychologists were trained to rate recordings for competence and adherence to 17 components including whether the interventionist introduced the goals of the session and offered opportunity for questions, if key aspects of the personalized feedback and information about BAC were presented, if the interventionist asked for participants’ reactions and how they might use the information at the conclusion, and M,I.-specific competencies (e.g., developing discrepancy, reflective listening, eliciting change talk). Raters gave each component a competence/adherence score of 1 (not done or done below expectations), 2 (met expectations) or 3 (above expectations). Recordings were selected randomly. Raters first reviewed the same 4 recordings for training. After evaluation of initial ratings and discussion, the raters evaluated 9 more recordings, 4 of which overlapped among raters. After evaluation of consistency in ratings across the overlapping recordings to ensure continued adherence, raters evaluated 5 more non-overlapping recordings. The second set of 4 overlapping ratings, occurring after training was completed, was used to evaluate agreement among raters. The 30 non-overlapping sessions, evaluated by a single rater, were used to evaluate fidelity to the M.I.-based counseling and psychoeducation intervention.
Percent agreement among the 3 raters was calculated for each of the 17 categories rated for the second set of 4 overlapping counseling recordings. There was agreement on 75.2% of ratings. Across the 30 non-overlapping recordings, the mean fidelity score was 1.91 on the 1–3 range (SD=0.15).
Moderate drinking technologies.
Participants were then randomized to 1 of 3 forms of technology for use during a laboratory alcohol drinking session. The 3 technologies were 1) the BACTrack Mobile Pro breath alcohol device/app (2.5.6 was the latest version of the app used in the study), 2) the Intellidrink BAC estimator app (see Luczak et al., 2018), and 3) a self-texting control procedure where participants sent themselves a text with their beverage (e.g., “beer”) after each alcoholic drink and counted the number of texts before subsequent drinking decisions. Each participant in a drinking session was randomized to a different technology. Moderate drinking technology use by young adults is rare, thus we attempted to capture in the lab the most likely “real world” scenario of one young adult in a social/drinking group using a particular moderate drinking technology.
The breath alcohol device works with an app, connected by Bluetooth. BrAC is registered on the app and tracked over time with a graph. The device uses fuel cell technology similar to police breathalyzers. Via written and oral instructions, participants were advised to wait 15 min. after the end of each drink before taking a reading to enhance accuracy. Although the app did not have a built-in timer, staff suggested use of smartphone alarms. To provide a reading, they were instructed to press a button in the app, take a deep breath, then blow into a disposable tube attached to the device for 5–7 sec. After the device analyzed BrAC, the reading appeared in the app on the center of the screen. Participants were advised to use the device before ordering a second drink and each thereafter during the laboratory session and field-use period.
The BAC estimator app gives eBAC readings using proprietary formulas and algorithms based on the Widmark equation (Matthews & Miller, 1979) that take into account sex, weight, number of drinks, time elapsed, reported stomach fullness (low, medium, high) and recent drinking history (rare, occasional, and frequent). We created all participants’ profiles with the “occasional” drinker option and asked them to maintain that setting out of a concern that some might object to being labeled a “frequent” drinker. We set the app to the low stomach fullness setting initially due to the request that they fast before the lab session, but also asked participants to maintain that setting during the field period for continuity and due to uncertainty regarding whether they would report stomach fullness accurately and remember to adjust across drinking situations. We also expected that erring on the side of higher eBAC would be preferable for encouraging drinking reduction. This condition was included to compare acceptability and usability with the breathalyzer and to assess whether BAC estimator use is associated with moderate drinking. We considered 10 options and chose IntelliDrink for ease of use; positive user ratings; ability to enter drinks 1-by-1; tracking with a graph like the breathalyzer app; and its basis in the Widmark equation. Users enter the time they began, then make entries when they finish each drink or afterward, along with the time they completed the drink. Participants were instructed to make an entry and note eBAC before ordering each drink after their first.
For the self-texting, drink counting procedure, participants were instructed to send a text message to themselves after each drink and take note of the number of texts before opting to have subsequent drinks. This procedure was intended as a control condition in that it involves use of technology but does not provide BAC-related information.
Session procedures.
To help ensure participants did not know each other prior to the drinking session, staff scheduled participants who were not in the same academic department (if students), did not live at the same location (e.g., apartment complex), and did not have the same employer. Including friends/acquaintances within sessions would have forced accounting for closeness of these relationships within and across sessions, which would have added complexity that could not be addressed adequately in a study of this size. Sayette and colleagues (2012) similarly conducted small group drinking sessions involving young adults who did not know each other in their research on relationships between alcohol use and social/emotional bonding.
On the day of the drinking session, participants were instructed to not consume alcohol and to eat lunch but not after 1pm. Participants met with study staff on the day of the session for BrAC, urine tests to receive instructions and practice their assigned technology. They were provided written instructions including how to use their technology, and that technology use may help them to achieve and maintain optimal BAC and avoid disincentives associated with excessive drinking built into the drinking paradigm for the session (see below). Possible barriers to technology use and solutions were discussed. Participants were reminded of the study goal to get their opinions on the technology and thus they were encouraged but not required to use their assigned technology. Staff then walked through use of the technology with participants and they practiced its use. In some cases, for participant convenience, this appointment was scheduled immediately before the start of the session (Table 1).
Participants were provided transportation by the study. At arrival, BrAC was again tested. Participants forfeited their phone and used the assigned technology on a study phone instead. Study staff reviewed general instructions and session rules, followed by baseline measures. Staff and participants then reviewed instructions for the assigned technology and practiced again.
Alcohol self-administration was conducted per NIAAA guidelines (National Advisory Council on Alcohol Abuse and Alcoholism, 2005) by 3 staff (supervisor, server, assistant) in a simulated bar lab. At 5pm, participants could consume beer and non-alcoholic drinks ad libitum for 3 hours. Participants were again encouraged to use their assigned technology and asked not to share their technology or resulting readings with others. Staff asked participants if they wanted an initial drink but all subsequent ordering was initiated by participants only. Participants could switch between drink options but had to complete each drink (alcoholic or non-alcoholic) before ordering their next. Beer options were of uniform caloric (128–140 calories) and alcohol content (4.4–4.6%). Drink ordering and consumption was monitored and recorded for data and safety by the server and assistant. Data were transmitted to the supervisor in the next room for tracking using individualized charts for each participant. These charts contained eBACs for all possible beer quantities in 5-minute increments calculated with a standard formula based on the Widmark equation: (((number of beers/2) * (constant of 9 for females and 7.5 for males/weight)) – (number of hours x .016)). Participants were not permitted to order a beer that would lead to eBAC ≥0.10%.
All participants took part in a laboratory alcohol drinking session conducted according to the impaired control laboratory paradigm (Leeman et al., 2013; 2018). This paradigm involves probabilistic disincentives for excessive alcohol use that disregards a moderate drinking guideline (3 drinks or less for men, 2 or less for women). The guideline models the type of pre-determined limit on alcohol use to which people with impaired control have difficulty adhering (Heather et al., 1993). The probabilistic disincentives are partial losses of pay after the session that are tied to performance on 4 cognitive and psychomotor tasks sensitive to alcohol (Brandt, 1991; Brumback et al., 2007; Chait & Perry, 1994; Wechsler, 1981). Inclusion of the drinking guideline and probabilistic disincentives increase variability in alcohol self-administration compared to a control condition without these aspects (Leeman et al., 2013). Participant task performance results are outside the scope of this paper and not reported here.
For each task failed (i.e., performed worse than screening beyond a small grace range), participants drew from a hat at the follow-up appointment for a reduction of $0, $5, or $10 (i.e., 1 hour of subject pay) from a bonus payment beyond their base payment. The goal is to model negative consequences of alcohol use. The probabilistic nature of the monetary loss models the uncertainty of consequences, while having pay losses occur in the future models the often distal nature of consequences. While experience of consequences is not part of impaired control per se, in young adults, impaired control has been linked to negative consequences (Leeman et al., 2009). These elements (controlled drinking guideline; probabilistic, distal consequences; group sessions to model social drinking; naturalistic setting) enhance ecological validity.
Alcohol self-administration ended at 8pm at which time participants provided a breath alcohol sample, and repeated the cognitive/psychomotor tasks and self-reports (Table 1). Staff then took the study phones from participants to download their data. Participants’ own phones were returned. After these activities, participants were given food. Cigarette smoking and vaping were allowed off-site. BrAC and self-reports were repeated hourly. At 11pm, participants rated the acceptability and usability of their assigned technology. Participants then put the breath alcohol and BAC estimator apps on their own phones. Participants with a non-compatible phone or who preferred not to use their own phone for these purposes were given a study smartphone to use for the two-week field-testing period. They were then instructed on how to use the other technologies that were not assigned to them for the session and practiced their use with study staff. Participants practiced until they used each technology correctly, which was verified by study staff. Beginning at 12am, participants were dismissed and provided transportation home once their BrAC reached .02% or less.
Post-session field testing period.
Post-session, participants had 2 weeks to use all 3 forms of moderate drinking technology outside the lab. Participants earned $10 per day and $20 for using each of the 3 technologies at least once during the field period. No other compensation was tied to technology use. At the end of the field-testing period, participants completed another TLFB, ratings of acceptability and usability for all 3 technologies, rank ordered their preference, and a semi-structured interview to convey their experiences in the study and input on the technologies.
Measures
Alcohol and cigarette use.
The TLFB (Sobell & Sobell, 2003) uses a calendar with memory prompts to facilitate recall of substance use each day in a specified period (30 days in this study). Reliability and validity of estimates over 30 days have been verified (Carey, 1997).
Alcohol abuse/dependence.
The Structured Clinical Interview for DSM-IV (SCID; First et al., 2002) was used to diagnose lifetime and current alcohol and drug abuse and dependence.
Acceptability and usability.
Participants rated technology with a version of the System Usability Scale (Brooke, 2016) modified to fit mobile, alcohol-related technology. The version in this study included 16 items rated on 7-point scales, anchored with 1 = “strongly disagree” and 7 = “strongly agree.” We opted a priori to consider individually 3 acceptability items (“I think I would like to use this mobile technology frequently”; “I felt self-conscious while using this mobile technology” and “This mobile technology has value in helping people to moderate their drinking”) and 1 usability item (“I thought the mobile technology was easy to use”).
Data analysis
Probability plots were reviewed to assess normality and need for transformations. Analyses were conducted using SPSS, version 27. Determining feasibility was one of the goals of this study, including whether participants would use the moderate drinking technologies in the lab session and field period, and if so, how often. For simplicity, we counted use of one of the technologies 1 or more times in a drinking day as an instance of smartphone technology use (e.g., self-texting 7 times in a night would be counted as 1 instance of self-texting) during the field period. The number of overall drinking days consisted of drinking days reported on the TLFB plus dates when technology use occurred without an accompanying report on the TLFB.
The primary analytic method was multiple regression (linear for continuous, Poisson or negative binomial—whichever best fit the data—for count outcomes) with study technology condition and sex as the main predictor variables. Study condition was dummy coded as smartphone breathalyzer versus other and BAC estimator versus other with self-texting as the reference condition. Primary Outcome 1 was peak eBAC during laboratory alcohol self-administration. Peak eBAC was sensitive to differences between the control condition and experimental impaired control paradigm in the original proof of concept study (Leeman et al., 2013). Results were confirmed using linear or generalized linear mixed models with group (participants completing a drinking session together) as a random effect and the same predictors as the regressions as fixed effects. Mixed models can account for nested structure of data in groups. A similar strategy was used for Primary Outcome 2 (number of beers self-administered in the lab), Secondary Outcomes (acceptability and usability ratings at session end) and frequency of use during drinking sessions. For Exploratory Aim 1, sex by condition interactions were tested in addition to the variables in the primary analyses. For Exploratory Aim 2, rank orders of preference for the 3 technologies based on the 2-week field period were compared non-parametrically. Mixed models with random effects of subject and fixed effect of study technology condition were planned to assess differences across moderate drinking technologies on ratings of acceptability, frequency of technology use and alcohol drinking reported when using each form of technology during the 2-week field period.
Estimating effect size was challenging due to lack of relevant prior studies. Our goal was to power the study for comparisons between each BAC app and the control condition, not for comparisons between BAC apps. Mean peak eBAC in the impaired control paradigm in the initial study was 0.063% (Leeman et al., 2013). We expected the self-text control condition in this study to drink to a similar level. In a recent study (Leeman et al., 2018), most participants were already able to track their number of beers even without technology, thus we did not anticipate that self-texting would affect alcohol self-administration. For a 160lb male, 1 less drink over the same period in a BAC app condition equates to a mean peak eBAC of about 0.040%. Allowing 20% larger SD than the control group to account for individual differences in BAC app efficacy yielded Cohen’s d=0.78. An n of 33 per condition would enable detection of an effect of this size at α=.025 (to account for 2 comparisons) with 80% power and 2-sided test.
Results
Differences in laboratory ad libitum drinking by technology condition
There were no statistically significant differences by study technology condition in peak eBAC (Figure 2) during the alcohol drinking session (smartphone breathalyzer: β= −.02, p = .852; BAC estimator: β= −.06, p=.625). The sample reached a mean peak eBAC of .062% (SD=.026%, range: .002%−.10%). There was no statistically significant sex difference (men coded 1, women coded 2; β= .17, p=.105), nor was there a significant study technology condition-by-sex interaction.
Figure 2.
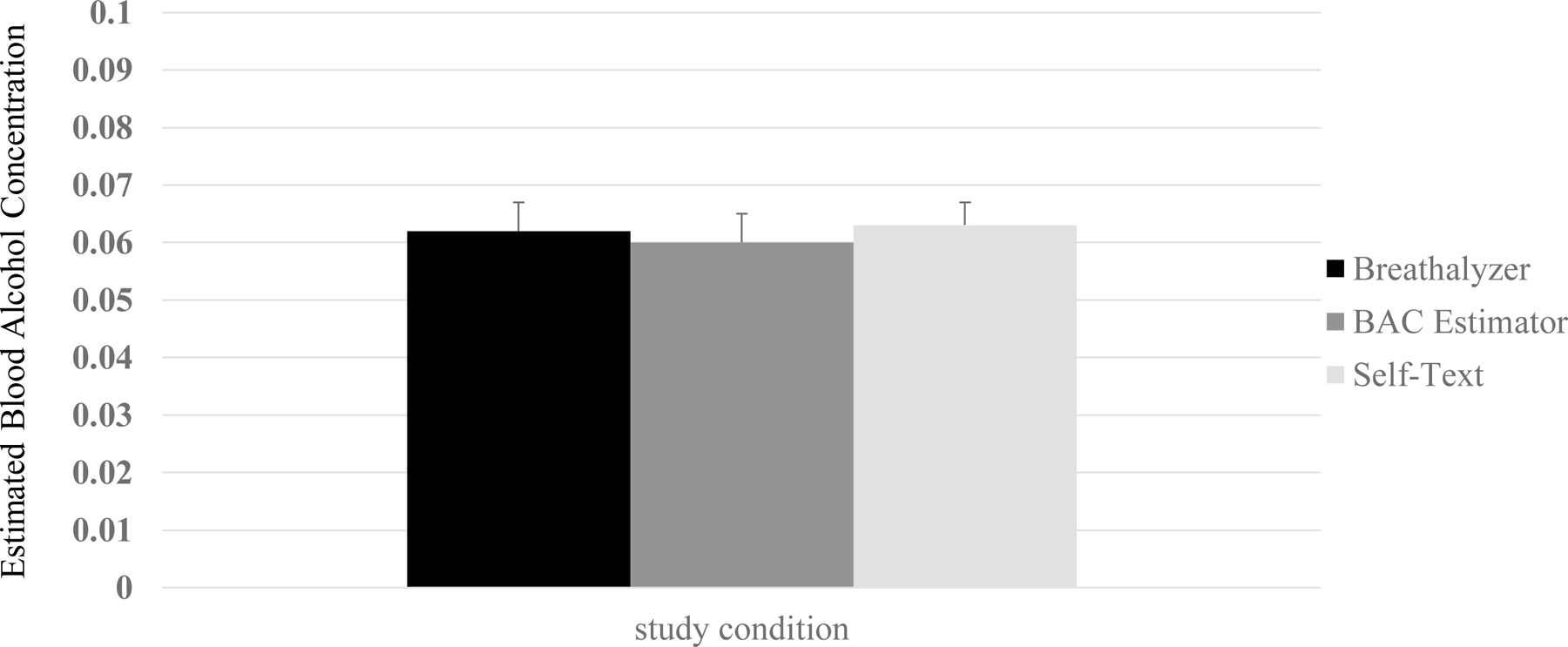
Peak Estimated Blood Alcohol Concentration During Alcohol Drinking Sessions by Study Condition
There was also no significant difference in number of beers self-administered ad libitum (smartphone breathalyzer: β= −.05, p = .683; BAC estimator: β= −.04, p=.700) (Supplemental figure 1). The sample self-administered a mean of 4.01 beers (SD=1.55, range: 1–7.74 beers). There was a significant sex difference (men: M=4.60, SD=1.67, women: M=3.41, SD=1.14) (β= −.39, p < .001). There was not a significant study technology condition-by-sex interaction. Mixed effects models including session group yielded similar results for eBAC and number of beers.
Overall, 25 of the 99 participants were cut off from further alcohol self-administration at some point during their session. There was not a statistically significant difference in being cut off across study technology condition, X2(2, N=99)= 0.75, p=.688).
Technology use in laboratory and in the field
During the lab session, participants used their assigned technology 3.37 times (SD=2.12, range: 0–11) on average. Based on negative binomial regression, there were no significant differences in technology use by condition (breathalyzer: β= −.08, p=.616; BAC estimator: β= .11 p=.458). There was also no significant sex difference (β= −.17, p=.175) or condition-by-sex interaction. A generalized linear mixed model with negative binomial distribution and log link function including session group as a random effect yielded similar results. Thirteen participants did not use technology (8 breathalyzer, 1 BAC estimator, 4 self-text). Based on a post-hoc logistic regression, there were no significant differences by condition or sex in odds of non-use.
Regarding feasibility, 97 of 99 (97.8%) participants completing a lab session finished the entire field period. Participants had 8.66 instances of technology use on average (SD=5.33) in the field period. Participants used at least one technology on 66.5% of drinking days (542/815).
A generalized linear mixed model with Poisson distribution and log link function (ICC=.45) was a good fit to the technology field use data, F(2, 266)=2.24, p=.05. There was a significant difference in technology use across technology type (Figure 3) but no significant differences by study technology condition from the lab session, sex or sex-by-condition interaction. The BAC estimator was used significantly more frequently than self-texting (β= .26, p=.002). The breathalyzer did not differ significantly from the BAC estimator or self-texting in number of field period uses.
Figure 3.
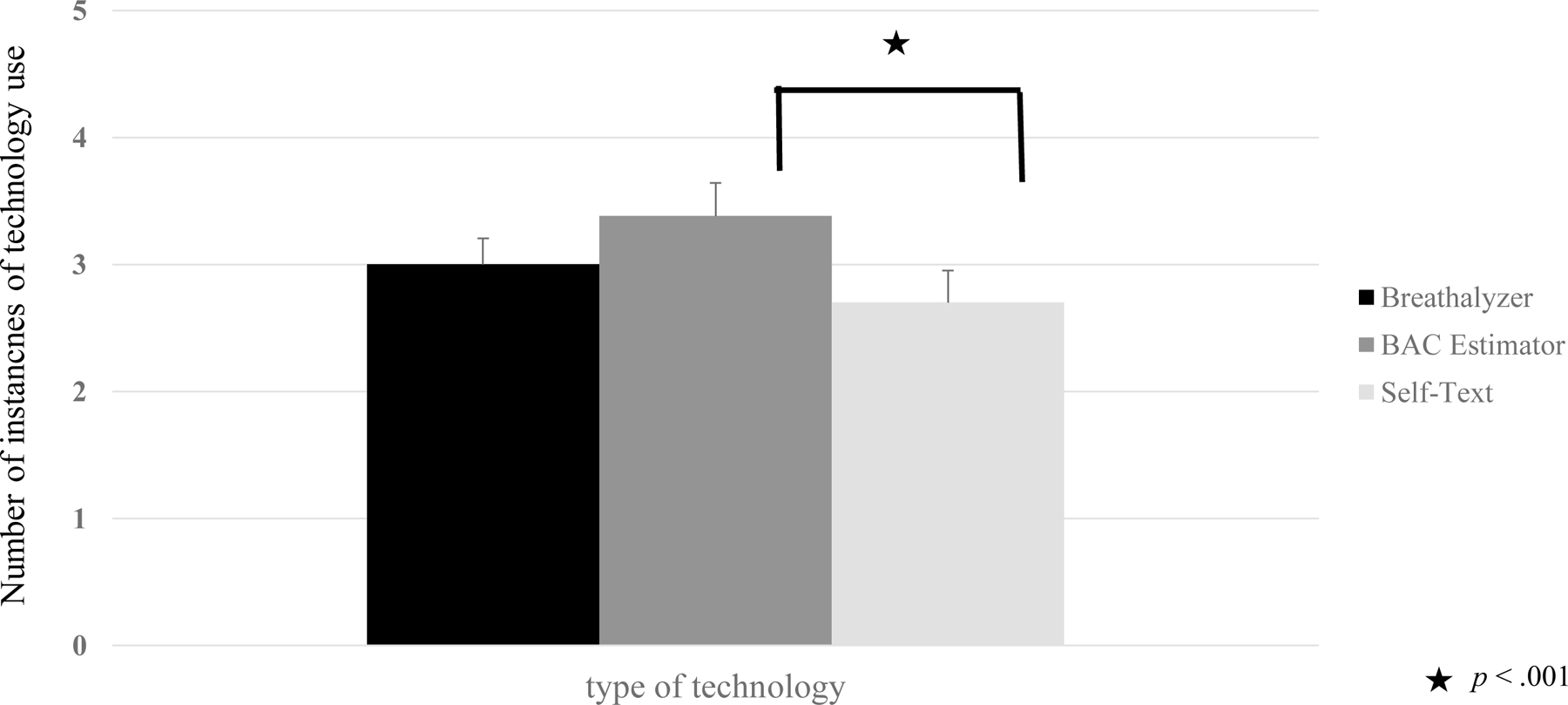
Number of Instances of Moderate Drinking Technology Use During the Field Period
Acceptability and usability of technology
Based on the lab session, participants randomized to the breathalyzer (β= .43, p<.001) and BAC estimator (β= .29, p=.012) gave higher scores than those randomized to self-text on like to use frequently. For perceived value, the BAC estimator rated significantly higher than self-text (β= .29, p=.013). There was a non-significant trend where the smartphone breathalyzer had higher perceived value than self-text (β= .22, p=.059). For self-consciousness, the breathalyzer rated significantly higher than self-text (β= .28, p=.017). These ratings did not differ significantly between the BAC estimator and self-text (β= −.13, p=.228). Regarding usability/ease, the BAC estimator did not rate as highly as self-text (β= −.29, p=.013). The breathalyzer did not differ significantly from self-text (Figure 4). There were no significant sex differences or sex-by-study technology condition interactions and mixed effects models including session group yielded similar results.
Figure 4.
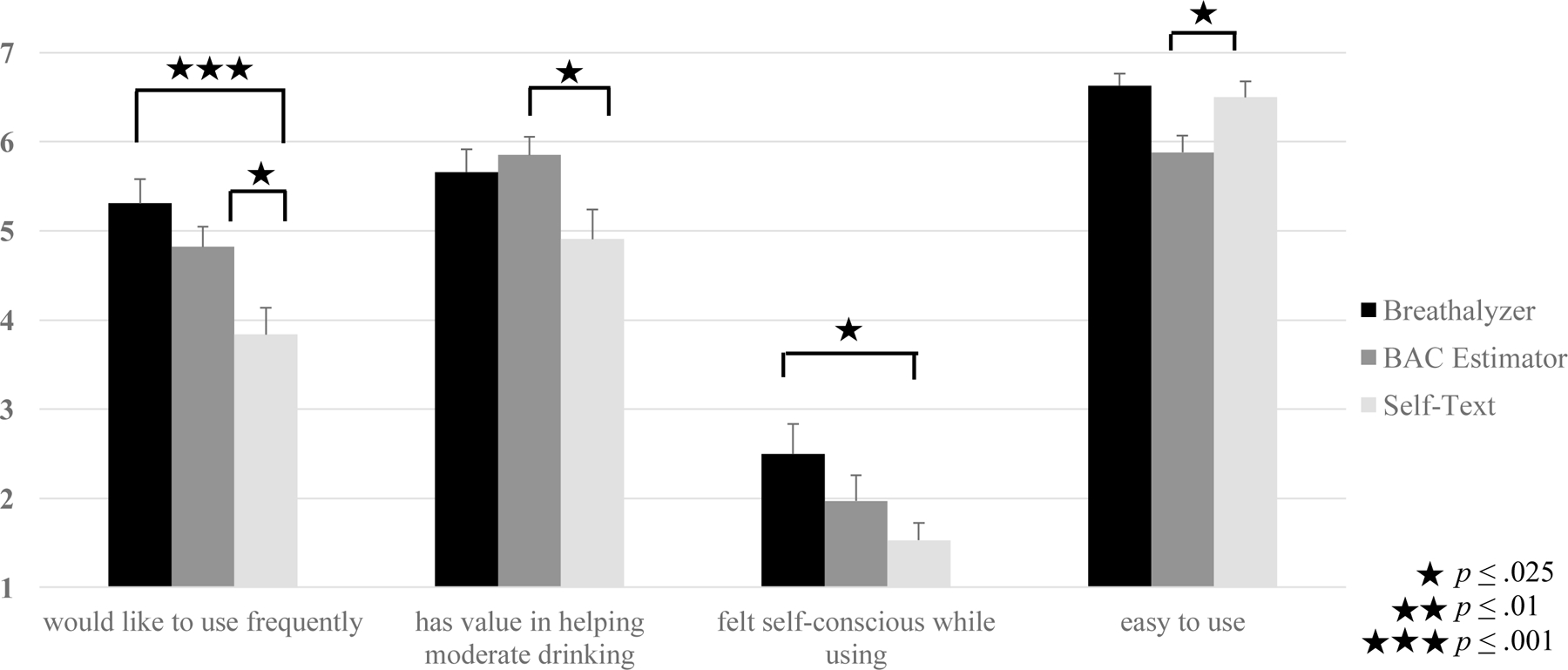
Acceptability and Usability across Technology Conditions Post-Alcohol Drinking Session
For acceptability and usability based on the field period, we compared ratings within-subjects only among those who used all 3 forms of technology (n=76). This led us to eliminate from these analyses, those who did not complete the field period (n=2), who chose not to use all 3 (n=8), and who could not use the BAC estimator during a period of technical difficulty when access to the app was limited (n=13). Planned mixed effects models did not converge for like to use frequently and ease of use. The intraclass correlation was low for perceived value (ICC=.08). Though a mixed effects model appeared to be appropriate for self-consciousness (ICC=.24), repeated measures ANOVAs were substituted for all acceptability and usability variables for consistency. For like to use frequently, the breathalyzer and BAC estimator rated significantly higher than self-text, F(2, 144) = 21.58, p< .001, η2p= .23. There were also sex differences, F(2, 144) = 8.78, p< .001, η2p= .11. Women had higher scores than men for the breathalyzer and self-text but men had higher scores for the BAC estimator (Supplemental Table 1). For perceived value, the breathalyzer and BAC estimator both rated significantly higher than self-text, F(2, 142) = 27.05, p< .001, η2p=.28. There were also sex differences, F(2, 142) = 5.23, p= .006, η2p= .07, due to women having higher scores than men for self-text whereas there were non-significant differences for the breathalyzer and BAC estimator. For self-consciousness, the BAC estimator did not differ significantly from self-text whereas the breathalyzer rated significantly higher than self-text, F(2, 129) = 27.14, p< .001, η2p=.27. There were no significant sex differences. Regarding ease, the smartphone breathalyzer did not differ significantly from self-text, but the BAC estimator rated significantly lower than self-text, F(2, 117) = 35.65, p< .001, η2p=.33, though the mean score was about a 5 out of 7 indicating participants still found the BAC estimator relatively easy to use (Figure 5). There were also sex differences, F(2, 117) = 9.98, p< .001, η2p= .12. Women had higher ease of use scores than men for self-text whereas men had higher scores for the BAC estimator with no significant difference for the breathalyzer (Supplemental Table 1). There were no statistically significant differences by study technology condition from the lab session, or significant sex-by-study technology condition interactions.
Figure 5.
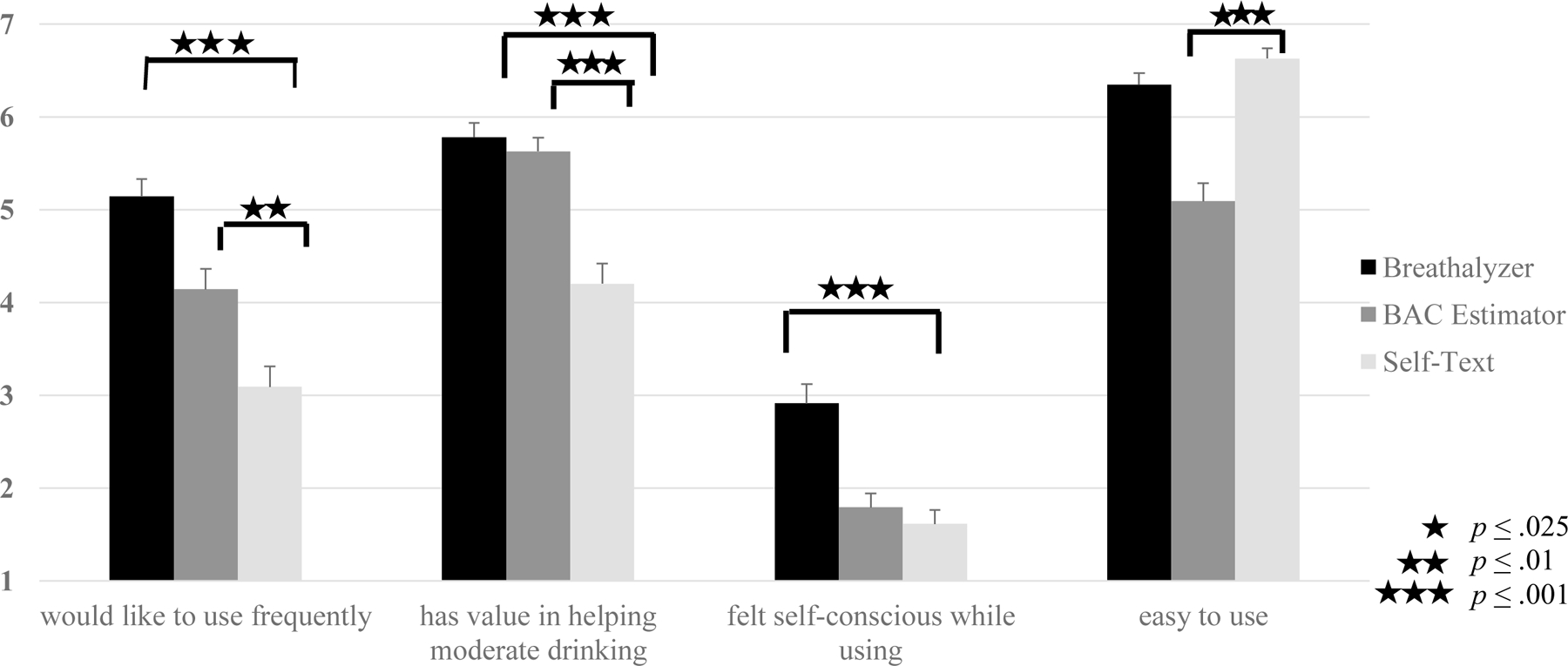
Acceptability and Usability across Types of Technology Post-Field Period Within Subject
When asked to rank order their preference, the breathalyzer was the first choice of 60.5% who used all 3: a significant departure from chance, based on the binomial distribution (p < .001). The BAC estimator was next, favored by 28.9%, which did not differ from chance. Only 10.5% preferred the self-text procedure, also a significant departure from chance (p < .001).
Exploratory comparisons of alcohol use in the field versus baseline
During the field period, participants used more than 1 form of technology on 40.2% of the drinking days when they used technology and on 26.7% of drinking days overall, making it difficult to compare alcohol use associated with individual technology use per our planned exploratory aim. Instead, we compared alcohol use reported on the TLFB between the baseline and field period within-subject collectively using repeated measures ANOVA including technology condition during the lab session and sex. Participants reported significantly less alcohol use in the field period compared to baseline on all variables examined: drinks per week (baseline: M=21.73[SD=12.36], field period: M=17.22[SD=12.68], F[1, 93] = 25.92, p< .001, η2p= .22), drinks per drinking day (F[1, 93] = 18.75, p< .001, η2p= .17) (Figure 6), mean eBAC on drinking days (baseline: M=0.14%[SD=0.05%], field period: M=0.12% [SD=0.05%], F[1, 93] = 20.12, p< .001, η2p= .18) and peak eBAC (baseline: M=0.33% [SD=0.12%], field period: M=0.24%[SD=0.11%], F[1, 93] = 40.94, p< .001, η2p= .31). Reductions in drinking applied to both sexes, but there were significant main effects due to men reporting more drinks per week (F[1, 93] = 6.46, p= .013, η2p= .07) and per drinking day (F[1, 93] = 13.92, p< .001, η2p= .13) but no significant differences in mean or peak eBAC. There were no differences by study technology condition from the lab session.
Figure 6.
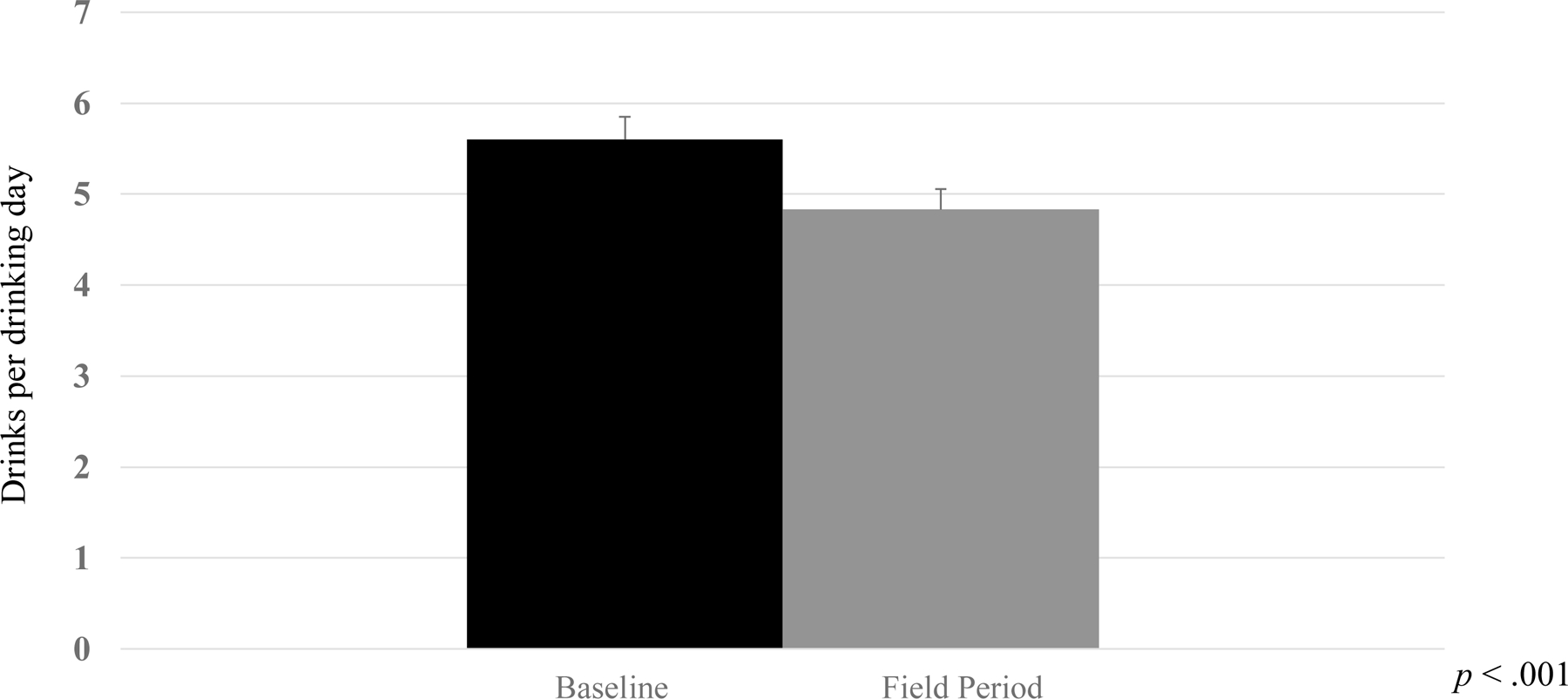
Mean Drinks per Drinking Day at Baseline Before the Alcohol Drinking Session and During the Field Period
Discussion
There were no significant effects of technology assignment on ad libitum drinking in the laboratory drinking sessions. During the 2-week field period, the BAC estimator app was used the most frequently. Although the smartphone breath alcohol device and app had favorable acceptability and usability ratings, participants did not use it more frequently than self-text. Participants used the 3 technologies frequently in the field and reported significantly less drinking during the field period than at baseline according to exploratory analyses.
These findings advance the literature on mobile and in-the-moment interventions for young adult drinkers, which lacks established, empirically supported options. Specifically, these findings advance understanding of smartphone breathalyzer devices/apps and BAC estimator apps as moderate drinking technologies. Although smartphone breathalyzers have been used as assessment tools in contingency management studies (Alessi & Petry, 2013; Koffarnus et al., 2018; Oluwoye et al., 2000) and have been the subject of formative research (Min et al., 2020), data on smartphone breathalyzers as intervention components are lacking. The present findings indicate that smartphone breathalyzers are acceptable and usable in an at-risk population. Though published findings support the validity of eBAC produced by Intellidrink (see Luczak et al., 2018), intervention findings with other BAC estimator apps have been mixed including some iatrogenic findings (Berman et al., 2019; Gajecki et al., 2014). Intellidrink also received favorable acceptability and usability ratings and was the most frequently used app during the field period. Acceptability and usability are crucial to technology-based interventions (Kazemi et al., 2017). If people do not like using technology, do not value it and/or do not find it easy to use, there will be no widespread dissemination and implementation, regardless of efficacy.
Despite favorable acceptability and usability, the breathalyzer did not stand out regarding frequency of use. Self-consciousness may be part of the reason. The breathalyzer rated higher than self-text, though the rating was not high overall (just under 3 on a 1–7 scale). Participant interview comments offered clarification. Given the breathalyzer’s monetary value, some participants expressed concern about losing it or having it stolen, particularly when they drank in unfamiliar or “sketchier” contexts (e.g., “dive” bars). Several participants who expressed concern about self-consciousness or loss/theft stated that they preferred the more discreet BAC estimator or self-texting in these contexts.
Though acceptability and usability ratings were strong overall, there were small-to-medium effect sex differences. Based on concerns raised in the post-field period interview about having to carry the smartphone breathalyzer (despite its small size), women’s more favorable attitudes may have been due to convenience since more women carry purses and other bags. These differences were not large enough to raise concerns, but sex differences in acceptability and usability of moderate drinking technology should continue to be examined.
In addition to participants’ favorable attitudes toward the technologies, there was no evidence of iatrogenic effects in this study. Further, the field period results indicate that after a brief M.I. session, a smartphone breathalyzer and BAC estimator app may be parts of a multi-component, mobile intervention with capability to reduce young adult drinking.
These promising findings further support the strong potential of technology-based interventions for young adults (Epler et al., 2009; Weaver et al., 2013). Although cost is a consideration, young adults regularly pay for technology. The average young adult in the United States spends $161 per month on cellphone charges (Fottrell, 2017) and about 60% of students reported monthly electronics spending (Nielsen, 2012). Though the breathalyzer in this study retails for about $100, other models cost $40 or less and the price of technology tends to decrease over time. While the Intellidrink BAC estimator app was widely available in the Apple app store for a nominal fee at the start of this study, it is no longer readily available to consumers though can be obtained from the developer for research purposes.
If anything, the potential importance of these technology-based interventions has increased due to the COVID-19 pandemic. Technology-based interventions have added benefit because they can be delivered without in-person contact. Since COVID-19 has forced many mental health services to be conducted remotely, technology-based interventions like these are likely to become normative. Emerging evidence shows an overall increase in alcohol use (Rodriguez, Litt, & Stewart, 2020; McPhee, Keough, Rundle, Wardell, & Hendershot, 2020) and among young adults, an increase in drinking days since COVID-19 (Graupensperger, Fleming, Jaffe, Rhew, Patrick, & Lee, 2021). These findings emphasize the importance of efficacious mobile interventions to provide in-the-moment assistance to young adult drinkers.
The present findings suggest several future research directions. Participant comfort in using moderate drinking technologies, particularly smartphone breathalyzers, could be enhanced. As part of instructions, study staff suggested ways to use the breathalyzer discreetly (e.g., in the bathroom). In future studies, these tips could be reinforced further by providing them in the moment, perhaps via text message, but this advice does not address other concerns such as losing the device. As such, it may be inevitable that young adults will use smartphone breathalyzer devices during fewer drinking events than other technologies. Thus, a future research goal may be to focus on the best ways to help young adults to learn as much as possible from these limited experiences through enhanced adjunctive brief counseling interventions and psychoeducation. Future research could develop a combined intervention made up of enhanced, brief BAC-focused M.I. coupled with these and perhaps other moderate drinking technologies. With a combined intervention, such as a new smartphone app that facilitates multiple technology use, the app could suggest an alternative in a situation where breathalyzer use may be awkward. Participants also cited forgetting as a barrier to use. Other than advising participants that they could set alarms on their smartphone, we did not assist participants in remembering to use the technology. Future research could make use of push notifications on the phone and other techniques as memory prompts.
Scenarios raised by participants in the post-field period interviews highlight the importance of context, which must be accounted for if interventions are to be successful. Ecological momentary assessment would enable us to learn more about the importance of context (e.g., bar, party, private residence, number of people with the participant) in relation to moderate drinking technology use and alcohol use. Adding a daily morning questionnaire to alcohol reduction technology use in the field would enable comparisons of technology plus daily monitoring to monitoring alone. However, monitoring is an inherent part of breathalyzer or BAC estimator use. Future studies may also provide brief M.I. to only a portion of the sample to isolate effects of this component from the technology components. In future field use studies, technology access could be provided for only half of this period, enabling proximal, within-subject comparisons with versus without technology access.
While other findings in this study were suggestive, the lack of significant differences in ad libitum drinking across technology conditions ran counter to hypotheses. As in prior studies using the impaired control laboratory paradigm (Leeman et al., 2013; 2018), mean self-administration during the laboratory session was at about the mid-point of the possible range of response and there was substantial variability among participants (McKee, 2009). These findings indicate that the lab paradigm was implemented successfully. Two potential explanations for the null lab session findings are that the technologies tested do not have efficacy in moderating drinking, or that the technologies have efficacy but were not ideally suited for testing in a lab paradigm. Regarding the first possibility, significant reductions in alcohol use during the field period compared to baseline offer suggestive evidence of efficacy though the possibility of assessment reactivity effects must be considered. Regarding the latter possibility, to be suited to lab testing, an intervention has to offer potential for immediate behavior change. The field period provided participants with multiple opportunities to use the technologies. Accordingly, participants used each technology an average of about 3 times each for a total of just under 9 times overall in the field. The more favorable exploratory results in the field period than in the lab suggest these technologies may take some time to result in drinking reduction and thus may not be ideally suited to efficacy testing in a lab paradigm.
The study had other limitations. Moderate drinking technologies, especially those that relate to BAC, may be more of a necessity with mixed drinks, beverages with unknown alcohol content, and/or during drinking events involving a variety of beverages, rather than consumption of only beer as in our lab sessions. Drinkers may be better able to approximate their amount of consumption and impairment for standard drinks of beer than for other beverages. Regarding our BAC-focused motivational interview and psychoeducation, coder agreement on fidelity ratings was slightly over 75%, which was lower than anticipated. This calculation was based on a small batch of shared ratings, which we viewed as appropriate given the size of the study. In future studies, additional concrete coding examples will be provided to further ground the meaning of each level in the 3-level rating system. The mean rating of just under 2 indicated that interventionists tended to deliver aspects of the counseling intervention with acceptable fidelity. While our field period had advantages of ecological validity, lack of assessment/researcher control brought limitations. For instance, it was impossible to determine the extent to which participants used the technology correctly (e.g., waiting 15 minutes after completing drinking before breath alcohol readings). In addition, our inclusion of an active control condition (i.e., self-texting) in the lab alcohol drinking sessions precluded comparisons between technology use and non-use. However, we have found in prior research using the same lab paradigm (Leeman et al., 2018) that participants are typically able to recollect number of drinks consumed on their own, thus self-texting likely provided minimal assistance in moderating drinking. Nonetheless, future studies may opt to include a no technology condition for comparison purposes.
In summary, our findings, including a very high rate of completion; enrollment of a frequent heavy-drinking sample over 1/3 of whom were members of ethnic/racial minority groups, with a slight majority of non-students all speak to the feasibility of moderate drinking technology research in young adults. Our finding of almost 9 instances of technology use when participants were compensated for only 3 is promising and speaks to, at minimum, openness and curiosity about these technologies and potentially, a degree of motivation to reduce drinking. The next step is a controlled study to test a multi-component intervention made up of enhanced M.I.-based counseling followed by use of these technologies in a manner that emphasizes concurrent use; that takes social context into account; and gives tailored, in-the-moment memory prompts. As more mental health services are offered remotely, post-COVID, mobile interventions like these have the potential to be especially helpful to young adults given their willingness to use apps and the possibility that in-the-moment interventions can motivate behavior change.
Supplementary Material
Public Health Significance.
Young adult alcohol misuse is a public health crisis requiring novel interventions. In-the-moment interventions utilizing mobile technology are promising approaches for young adults. This study supports the feasibility of research on these technologies and provides evidence for their perceived value and ease of use.
Acknowledgments
Clinical trials.gov # NCT02963818. Preliminary versions of these results were presented at the 2018 and 2019 annual meetings of the Research Society on Alcoholism (RSA), the 2018 and 2019 Collaborative Perspectives on Addiction meetings, the 2019 annual meeting of the Association for Behavioral and Cognitive Therapies (ABCT), the 2019 State of the Science Meeting hosted by the Southeastern Coastal Center for Agricultural Health & Safety, the 2020 annual meeting of the National Hispanic Science Network and at research colloquia at the University of North Texas Health Science Center (2018), Yale School of Medicine (2019), the University of Massachusetts (2020) and St. Jude Children’s Research Hospital (2021). Unrelated to the present work, Dr. O’Malley reports the following: consultant/advisory board member for Alkermes, Amygdala, Indivior, Mitsubishi Tanabe, Opiant; a member of the American Society of Clinical Psychopharmacology Alcohol Clinical Trials Initiative supported by Alkermes, Amygdala Neurosciences, Arbor Pharmaceuticals, Dicerna, Ethypharm, Indivior, Lundbeck, Mitsubishi, and Otsuka; donated medications from Astra Zeneca, Novartis, and Pfizer; and DSMB member for NIDA (Emmes Corporation). This research was supported by National Institutes of Health Grants R21 AA023368, T32 AA025877, UH2/UH3 AA02614, T32 AA007459, The State of Florida and The Mary F. Lane Endowed Professorship. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the State of Florida. The funding sources had no other role other than financial support. The authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest relevant to this article to disclose. The authors acknowledge the assistance of Maria Costanza Benvenuti, Patricia Chauca, Neo Gebru, Ralitza Gueorguieva, Jamie Guinn, Jacqueline Hobbs, Taylor Kerstetter, Cassidy LoParco, Frederick Muench, Amanda Palmer, Robert Prather, Adelya Urmanche, and Ali Yurasek
Footnotes
The authors report no other conflicts.
References
- Alessi SM, & Petry NM (2003). A randomized study of cellphone technology to reinforce alcohol abstinence in the natural environment: Portable CM for alcohol abstinence. Addiction, 108(5), 900–909. doi: 10.1111/add.12093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ (2019). Conceptual foundations of emerging adulthood. In Murray JL & Arnett JJ (Eds.), Emerging adulthood and higher education: A new student development paradigm (pp. 11–24). Routledge. [Google Scholar]
- Baraona E, Abittan CS, Dohmen K, Moretti M, Pozzato G, Chayes ZW, Schaefer C, & Lieber CS (2001). Gender differences in pharmacokinetics of alcohol. Alcoholism-Clinical and Experimental Research, 25(4), 502–507. [PubMed] [Google Scholar]
- Bava S, & Tapert SF (2010). Adolescent brain development and the risk for alcohol and other drug problems. Neuropsychoogyl Review, 20(4), 398–413. doi: 10.1007/s11065-010-9146-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman AH, Andersson C, Gajecki M, Rosendahl I, Sinadinovic K, & Blankers M (2019). Smartphone apps targeting hazardous drinking patterns among university students show differential subgroup effects over 20 weeks: Results from a randomized, controlled trial. Journal of Clinical Medicine, 8(11), 1807. doi: 10.3390/jcm8111807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10(1), 641–677. doi: 10.1146/annurev-clinpsy-032813-153724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brains J (2019). The best breathalyzers for personal use. Business Insider https://www.businessinsider.com/best-breathalyzer. Accessed December 26, 2020 [Google Scholar]
- Brandt J (1991). Development of a new memory test with six equivalent forms. The Clinical Neuropsychologist, 5(2), 125–142. 10.1080/13854049108403297 [DOI] [Google Scholar]
- Brooke JB (1996). SUS - a quick and dirty usability scale. In Usability evaluation in industry (pp. 189–194). In Jordan P, Thomas B, Weerdmeester B, & McLelland I (Eds). Taylor and Francis: London. [Google Scholar]
- Brumback T, Cao D, & King A (2007). Effects of alcohol on psychomotor performance and perceived impairment in heavy binge social drinkers. Drug and Alcohol Dependence, 91(1), 10–17. doi: 10.1016/j.drugalcdep.2007.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, & Carey MP (2012). Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clinical Psychology Review, 32(8), 690–703. doi: 10.1016/j.cpr.2012.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, & Hustad JT (2002). Are retrospectively reconstructed blood alcohol concentrations accurate? Preliminary results from a field study. Journal of Studies on Alcohol, 63(6), 762–766. doi: 10.15288/jsa.2002.63.762. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Carey MP, & DeMartini KS (2007). Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors, 32(11), 2469–2494. doi: 10.1016/j.addbeh.2007.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chait LD, & Perry JL (1994). Acute and residual effects of alcohol and marijuana, alone and in combination, on mood and performance. Psychopharmacol, 115(3), 340–349. doi: 10.1007/BF02245075. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Palmer RS, Leeman RF, Corbin WR, Toll BA, Fucito LM, & O’Malley SS (2013). Drinking less and drinking smarter: Direct and indirect protective strategies in young adults. Psychology of Addictive Behaviors, 27(3), 615–626. doi: 10.1037/a0030475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epler AJ, Sher KJ, Loomis TB, & O’Malley SS (2009). College student receptiveness to various alcohol treatment options. Journal of American College Health, 58(1), 26–32. doi: 10.3200/JACH.58.1.26-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely M, Hardy R, Longford NT, & Wadsworth MEJ (1999). Gender differences in the relationship between alcohol consumption and drink problems are largely accounted for by body water. Alcohol and Alcoholism, 34(6), 894–902. doi: 10.1093/alcalc/34.6.894 [DOI] [PubMed] [Google Scholar]
- First B, Spitzer RL, Gibbon M, & Williams JBW (2002) Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Fottrell Q (2017). This is why millennials can’t have nice things or save any money. Market Watch.com. https://www.marketwatch.com/story/this-is-why-millennials-cant-have-nice-things-or-save-any-money-2017-06-26. Accessed December 8, 2020. [Google Scholar]
- Gajecki M, Berman AH, Sinadinovic K, Rosendahl I, & Andersson C (2014). Mobile phone brief intervention applications for risky alcohol use among university students: A randomized controlled study. Addiction Science & Clinical Practice, 9(1), 11–11. doi: 10.1186/1940-0640-9-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, Jung J, Zhang H, Fan A, & Hasin DS (2017). Prevalence of 12-Month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: Results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry, 74(9), 911–923. doi: 10.1001/jamapsychiatry.2017.2161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant S, LaBrie JW, Hummer JF, & Lac A (2012). How drunk am I? Misperceiving one’s level of intoxication in the college drinking environment. Psychology of Addictive Behaviors, 26(1), 51–58. doi: 10.1037/a0023942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graupensperger S, Fleming CB, Jaffe AE, Rhew IC, Patrick ME, & Lee CM (2021). Changes in young adults’ alcohol and marijuana use, norms, and motives from before to during the COVID-19 pandemic. Journal of Adolescent Health, 68(4), 658–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih M-Y, Atwood AK, Johnson RA, Boyle MG, Levy MS, Driscoll H, Chisholm SM, & Dillenburg L (2014). A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry, 71(5), 566–572. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heather N, Tebbutt JS, Mattick RP, Zamir R (1993). Development of a scale for measuring impaired control over alcohol consumption: A preliminary report. Journal of Studies on Alcohol, 54(6), 700–9. doi: 10.15288/jsa.1993.54.700. [DOI] [PubMed] [Google Scholar]
- Hingson R, Zha W, & Smyth D (2017). Magnitude and trends in heavy episodic drinking, alcohol-impaired driving, and alcohol-related mortality and overdose hospitalizations among Eemerging adults of college ages 18–24 in the United States, 1998–2014. Journal of Studies on Alcohol and Drugs, 78(4), 540–548. doi: 10.15288/jsad.2017.78.540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh D, Mun EY, Larimer ME, White HR, Ray AE, Rhew IC, Kim SY, Jiao Y, & Atkins DC (2015). Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcoholism Clinical and Experimental Research, 39(5), 919–931. doi: 10.1111/acer.12714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemi DM, Cochran AR, Kelly JF, Cornelius JB, Belk C (2013). Integrating mHealth mobile applications to reduce high risk drinking among underage students. Health Education Journal, 73(3), 262–273. 10.1177/0017896912471044 [DOI] [Google Scholar]
- Kazemi DM, Borsari B, Levine MJ, Li S, Lamberson KA, & Matta LA (2017). A systematic review of the mHealth interventions to prevent alcohol and substance abuse. Journal of Health Communication, 22(5), 413–432. doi: 10.1080/10810730.2017.1303556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Bickel WK, & Kablinger AS (2018). Remote alcohol monitoring to facilitate incentive-based treatment for alcohol use disorder: A Randomized Trial. Alcoholism Clinical and Experimental Research, 42(12), 2423–2431. doi: 10.1111/acer.13891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, DeMartini KS, Gueorguieva R, Nogueira C, Corbin WR, Neighbors C, & O’Malley SS (2016). Randomized controlled trial of a very brief, multicomponent web-based alcohol intervention for undergraduates with a focus on protective behavioral strategies. Journal of Consulting and Clinical Psychology, 84(11), 1008–1015. doi: 10.1037/ccp0000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, Corbin WR, Nogueira C, Krishnan-Sarin S, Potenza MN, & O’Malley SS (2013). A human alcohol self-administration paradigm to model individual differences in impaired control over alcohol use. Experimental and Clinical Psychopharmacology, 21(4), 303–314. doi: 10.1037/a0033438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, Fucito LM, & Martens MP (2017). Manual for Blood Alcohol Content (BAC)-focused motivational counseling for young adults Unpublished treatment manual. [Google Scholar]
- Leeman RF, Nogueira C, Wiers RW, Cousijn J, Serafini K, DeMartini KS, Bargh JA, & O’Malley SS (2018). A test of multisession automatic action tendency retraining to reduce alcohol consumption among young adults in the context of a human laboratory paradigm. Alcoholism: Clinical and Experimental Research, 42(4), 803–814. doi: 10.1111/acer.13613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, Toll BA, Taylor LA, & Volpicelli JR (2009). Alcohol-induced disinhibition expectancies and impaired control as prospective predictors of problem drinking in undergraduates. Psychology of Addictive Behaviors, 23(4), 553–563. doi: 10.1037/a0017129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipari RN, Hughes A, & Bose J (2016). Driving under the influence of alcohol and illicit drugs. In The CBHSQ Report Substance Abuse and Mental Health Services Administration (US). [PubMed] [Google Scholar]
- Luczak SE, Hawkins AL, Dai Z, Wichmann R, Wang C, & Rosen IG (2018). Obtaining continuous BrAC/BAC estimates in the field: A hybrid system integrating transdermal alcohol biosensor, Intellidrink smartphone app, and BrAC Estimator software tools. Addictive Behaviors, 83, 48–55. doi: 10.1016/j.addbeh.2017.11.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino EN & Fromme K (2018). Alcohol-induced blackouts, subjective intoxication, and motivation to decrease drinking: Prospective examination of the transition out of college. Addictive Behaviors, 80, 89–94. doi: 10.1016/j.addbeh.2018.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Smith AE, & Murphy JG (2013). The efficacy of single-component brief motivational interventions among at-risk college drinkers. Journal of Consulting and Clinical Psychology, 81(4), 691–701. doi: 10.1037/a0032235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews DB, & Miller WR (1979). Estimating blood alcohol concentration: Two computer programs and their applications in therapy and research. Addictive Behaviors, 4(1), 55–60. doi: 10.1016/0306-4603(79)90021-2 [DOI] [PubMed] [Google Scholar]
- McKee SA (2009). Developing human laboratory models of smoking lapse behavior for medication screening. Addiction Biology, 14(1), 99–107. doi: 10.1111/j.1369-1600.2008.00135.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhee MD, Keough MT, Rundle S, Heath LM, Wardell JD, & Hendershot CS (2020). Depression, environmental reward, coping motives and alcohol consumption during the COVID-19 pandemic. Frontiers in Psychiatry, 11, 1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTavish FM, Chih MY, Shah D, & Gustafson DH (2012). How patients recovering from alcoholism use a smartphone intervention. Journal of Dual Diagnosis 8(4), 294–304. doi: 10.1080/15504263.2012.723312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W, Zweben A, DiClemente C, & Rychtarik R (1992). Motivational enhancement therapy manual National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Min A, Lee D, Gao G, Jeong S, & Shih PC (2020). Design and assessment of a personal breathalyzer intervention to support responsible drinking. International Journal of Human-Computer Studies, 137, 102382. 10.1016/j.ijhcs.2019.102382 [DOI] [Google Scholar]
- Muraven M, & Baumeister RF (2000). Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychological Bulletin, 126(2), 247–259. doi: 10.1037/0033-2909.126.2.247 [DOI] [PubMed] [Google Scholar]
- National Advisory Council on Alcohol Abuse and Alcoholism. (2005). Recommended council guidelines on ethyl alcohol administration in human experimentation http://www.niaaa.nih.gov/Resources/ResearchResources/job22.htm
- Nielsen. (2012). Survey new U.S. smartphone growth by age and income http://www.nielsen.com/us/en/newswire/2012/survey-new-u-s-smartphone-growth-by-age-and-income.html
- Oluwoye O, Reneau H, Herron J, Alcover KC, McPherson S, Roll J, McDonell MG (2020). Pilot study of an integrated smartphone and breathalyzer contingency management intervention for alcohol use. Journal of Addiction Medicine, 14(3):193–198. doi: 10.1097/ADM.0000000000000553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center (2019). Mobile fact sheet https://www.pewresearch.org/internet/fact-sheet/mobile. Accessed November 29, 2020
- Prince MA, Carey KB, & Maisto SA (2013). Protective behavioral strategies for reducing alcohol involvement: A review of the methodological issues. Addictive Behaviors, 38(7), 2343–2351. doi: 10.1016/j.addbeh.2013.03.010 [DOI] [PubMed] [Google Scholar]
- Rodriguez LM, Litt DM, & Stewart SH (2020). Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors, 110, 106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutherford HJ, Mayes LC, & Potenza MN (2010). Neurobiology of adolescent substance use disorders: Implications for prevention and treatment. Child and Adolescent Psychiatric Clinics of North America, 19(3), 479–492. doi: 10.1016/j.chc.2010.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayette MA, Creswell KG, Dimoff JD, Fairbairn CE, Cohn JF, Heckman BW, Kirschner TR, Levine JM, & Moreland RL (2012). Alcohol and group formation: A multimodal investigation of the effects of alcohol on emotion and social bonding. Psychological Science, 23(8), 869–878. doi: 10.1177/0956797611435134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L, & Sobell M (2003). Alcohol consumption measures. In Allen JP & Wilson VB (Eds.), Assessing alcohol problems: A guide for clinicians & researchers, 2nd edition (pp. 75–99). National Institute on Alcohol Abuse and Alcohol. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2018) National Survey of Drug Use and Health (NSDUH) releases https://www.samhsa.gov/data/report/2018-nsduh-detailed2018)-tables. Accessed September 3, 2020
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, & Sellers EM (1989). Assessment of alcohol withdrawal: The revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). British Journal of Addiction, 84(11), 1353–7. doi: 10.1111/j.1360-0443.1989.tb00737.x [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 51, 1–18. doi: 10.1016/j.jsat.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson Jr, Aivadyan C, Stohl M, Aharonovich E, & Hasin DS (2020). Smartphone application plus brief motivational intervention reduces substance use and sexual risk behaviors among homeless young adults: Results from a randomized controlled trial. Psychology of Addictive Behaviors, 34(6), 641–649. doi: 10.1037/adb0000570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner JC, Bauerle J, & Shu J (2004). Estimated blood alcohol concentration correlation with self-reported negative consequences among college students using alcohol. Journal of Studies on Alcohol, 65(6), 741– 749. doi: 10.15288/jsa.2004.65.741 [DOI] [PubMed] [Google Scholar]
- Vuchinich RE, & Tucker JA (1988). Contributions from behavioral theories of choice to an analysis of alcohol abuse. Journal of Abnormal Psychology, 97(2), 181. doi: 10.1037//0021-843x.97.2.181 [DOI] [PubMed] [Google Scholar]
- Weaver E, Horyniak D, Jenkinson R, Dietze P, & Lim M (2013). “Let’s get Wasted!” and other apps: Characteristics, acceptability, and use of alcohol-related smartphone applications. Journal of Medical Internet Research - mHealth uHealth 1(1), e9. doi: 10.2196/mhealth.2709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (1981). WAIS-R manual: Wechsler Adult Intelligence Scale-Revised Harcourt, Brace, & Jovanovich. [Google Scholar]
- Wilhite ER, Mallard T, & Fromme K (2018). A longitudinal event-level investigation of alcohol intoxication, alcohol-related blackouts, childhood sexual abuse, and sexual victimization among college students. Psychology of Addictive Behavior, 32(3), 289–300. doi: 10.1037/adb0000353 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


