Abstract
Objectives
This study aimed to evaluate the level of knowledge, perception, and experience of teledentistry amongst Brazilian dentists with the ongoing COVID-19 pandemic.
Methods
Between June and July 2020, an online questionnaire was used to collect information on the demographic and professional profiles of dentists and their levels of knowledge, perception, and attitudes towards teledentistry. Descriptive statistics were reported as percentages, and Chi-squared test was used to compare responses amongst general practitioners, specialists, and those with varying levels of professional experience.
Results
This study included 575 dentists, the majority of whom were from the southeast region of Brazil (73.4%) and had a specialist degree (70.4%). Approximately 42.4% of the study sample had graduated more than 10 years ago, 39.3% between 2 and 10 years ago, and 18.3% up to 2 years ago. In general, the majority of dentists exhibited only a superficial awareness of the resolution that regulates teledentistry in Brazil. A greater number of specialists were aware of the resolution (P = .007) and felt confident performing teledentistry (P = .000) compared to general practitioners, whilst those with more experience (graduated more than 10 years ago) exhibited greater knowledge (P = .012) and preparation (P = .000). More than 60% of the dentists, regardless of dental specialty and clinical experience, had no knowledge of providing prescriptions via teledentistry. The majority of general practitioners (89.5%) and specialists (81.4%) had no previous experience using teledentistry.
Conclusions
The findings of this study suggest that Brazilian dentists are inadequately prepared for the implementation of teledentistry.
Key words: COVID-19, Teledentistry, Survey, Dental care
Introduction
The spread of the coronavirus disease (COVID-19) can be attributed to the transmission of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)1 through respiratory droplets or aerosols containing the viable virus, resulting in a high risk of cross-infection between patients and dental practitioners.2,3
In response to the COVID-19 pandemic, several countries established social isolation and quarantine protocols to limit the proliferation of the virus and possible mass contagion.4,5 In line with these measures, the Brazilian Federal Council of Dentistry (FCD) and the National Health Surveillance Agency recommended that dental care be limited to emergencies and urgencies.6
Considering the immense social and economic implications of the restriction of dental care, teledentistry presents key advantages in the dental management of patients without the risk of infection.6, 7, 8 It is possible to screen and obtain important information, such as symptoms, travel history, or contact with persons with known COVID-19. In addition, it can support and supplement health care professionals working in the emergency department of hospitals and primary health centres to provide emergency care to patients who have reported dental concerns without unnecessary exposure to extra personnel.7,9,10
Upon becoming a pandemic epicenter on June 4, 2020, the Brazilian FCD passed a resolution on June 22, 2020, which laid out the principles, guidelines, and legal provisions for the regulation of teledentistry in Brazil.8 Moreover, the documentation of all digital dental assistance provided to patients in their medical records was made mandatory to ensure the registration of all control and guidance measures and assure strict adherence to all ethical and legal protocols.
Additionally, the FCD also developed guidance documentation5 on ways to manage the key issues of teledentistry, including care of patients who were already undergoing treatment and were unable to return to the office, maintenance of medical records, and payment for consultations.
However, the efficacy of this method is largely dependent on the level of awareness amongst health professionals, as shown by previous evidence that those with prior experience with telemedicine were able to adopt it comfortably in the context of the COVID-19 pandemic, whilst those without prior experience required help with the clinical and technical issues associated with video-conferencing.8,11
Teledentistry typically involves remote communication and monitoring via telephone and video calls, and the dentist can help clarify the patient's doubts regarding their dental routine, provide oral health education, carry out prediagnosis, and identify cases requiring immediate treatment.6,10,12,13 Although the Brazilian public health service currently provides dental care to patients suspected of having COVID-19 as well as their close contacts via teleorientation and monitoring,14 there is limited evidence on the level of knowledge and experience about teledentistry amongst private dentists. One limitation of this technology is the poor resolution of the images provided by the patients or the stability and quality of the internet connection, which can adversely effect the proper evaluation by the dentist. Therefore, it has been identified that this diagnostic tool is palliative and cannot be used in all cases.6
The continuing pandemic and associated preventive measures have had severe repercussions on existing dental appointments and have contributed to increased patient anxiety regarding longerappointments and the quality of treatment.15 In this context, teledentistry provides dentists with an opportunity to guide patients, provide reassurance regarding treatment, and clarify their doubts until an effective SARS-CoV-2 vaccine has been developed and administered. Therefore, this study aimed to evaluate the level of knowledge, perceptions, and experience of teledentistry amongst Brazilian dentists.
Materials and methods
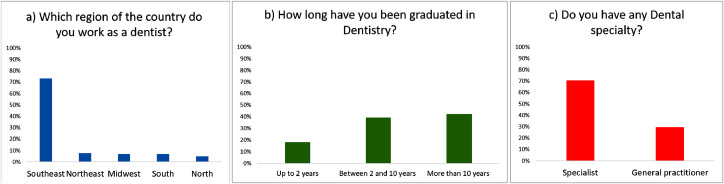
Between June 27 and July 11, 2020, dentists with varying levels of education and areas of specialisation were asked to complete an online questionnaire (written in Portuguese). Google Forms was used to collect the data, and the questionnaire web link was shared via email, WhatsApp Messenger, Facebook, and Instagram. The participants were recruited based on the above-mentioned dentists’ social media groups. A brief introduction consisting of an invitation to participate, a brief summary of the study, and a confirmation that all information collected would remain confidential was shared with the participants prior to starting the questionnaire. For the inclusion criteria, amongst the candidates who agreed to complete the questionnaire, only those who had already graduated from dental school and had an active dental practice were considered eligible for this study. Dental students, candidates with professional profiles other than dentistry, and those with no active dental practice were excluded. Information on the participants’ dental experience, specialties, and academic degrees is presented in Figure 1 and Supplementary files 1 and 2.
Fig. 1.
Professional profile according to (a) country region; (b) dental practice experience; and (c) dental specialty.
A total of 575 participants from different regions of the country (namely, south, southeast, midwest, north, and northeast) completed the questionnaire, which contained 14 required items collecting information on their demographic and professional profile, knowledge and perception of teledentistry, and their experience of using it. For the knowledge parameter, the dentists’ information and understanding of the FCD resolution in teledentistry was evaluated. As for the perception parameter, information was obtained about the dentists’ feelings and apprehension about teledentistry practice. The experience parameter evaluated the dentists’ background with teledentistry practice, and they were asked about their previous experience and how they performed teledentistry assistance. In addition, the participants were questioned about the charge for teledentistry assistance. The minimum sample size to obtain 84% of statistical power level was 564. The study had 575 participants, therefore the power level was higher than 84%.
Statistical analysis
Descriptive statistics were reported as proportions, whilst the Chi-squared test was used to compare responses amongst general practitioners, specialists, and those with varying levels of clinical experience. All statistical analyses were carried out using the Statistical Package for the Social Sciences (SPSS) version 17.0 (SPSS Inc.), and α = 5% was considered statistically significant.
Results
Professional profile
This study included 575 responses from dentists in all regions of the country. Figure 1 presents the data of professional profiles according to country region, dental practice experience, and dental specialty. Supplementary files 1 and 2 present the dentists’ specialties according to the dental practice
Knowledge and perception regarding teledentistry
Supplementary files 3 and 4 show the results for generalizability the entire sample not considering the dentists’ specialties or dental practice experience. In general, it was observed that most of the dentists had superficial knowledge of the teledentistry resolution (38.9%); consider that there will be some difficulties to using teledentistry (37.7%); believe that teledentistry would not be completely effective (48.9%); and believe that the patients probably would experience some difficulties when using teledentistry (71.5%). Also, most of the participants did not participate in teledentistry provision (83.8%); don't know how to prescribe medication via teledentistry (63%); and would charge for the teledentistry provision (70.4%).
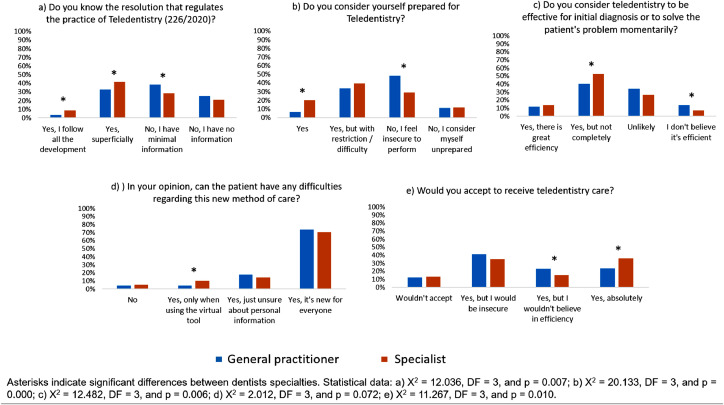
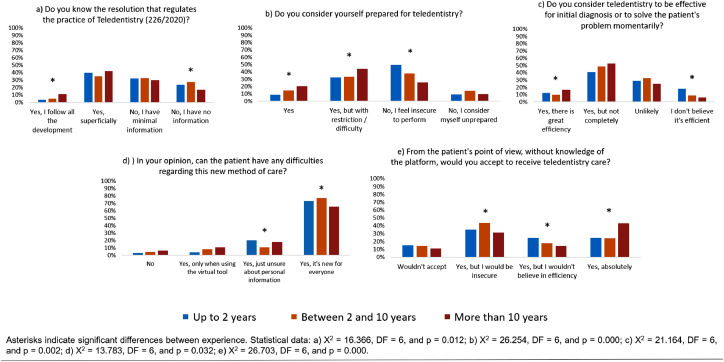
Considering the participants’ knowledge about the resolution of June 22, 2020, it was observed that most of the general practitioners had minimal information (Figure 2a, P = .007) and less experienced dentists had no information (Figure 3a, P = .012). There was a greater number of specialists (Figure 2b) and more experienced dentists (Figure 3b) who felt completely prepared to perform teledentistry (P = .000) than the number of general practitioners (Figure 2b) and less experienced dentists (Figure 3b). Most of the general practitioners (Figure 2c) and less experienced dentists (Figure 3c) did not believe that teledentistry could be effective for initial diagnosis or to solve patients’ problems (P = .006 and P = .002, respectively).
Fig. 2.
Comparison of the participants’ responses about the knowledge and perception of teledentistry, considering dental specialty.
Fig. 3.
Comparison of the participants’ responses about the knowledge and perceptions of teledentistry, considering dental practice experience.
Overall, despite dental specialties or practice experience, most of the participants believed that the patients could have difficulties with teledentistry due to the novelty of this mode of health care. Figure 2d shows the statistical similarity for the responses between general practitioners and specialists (P = .072), and Figure 3d shows statistical similarity according to the dentists’ experience (P = .032).
It was observed that most of the specialists (Figure 2e; P = .010) and more experienced dentists (Figure 3e; P = .000) were willing to provide teledentistry care.
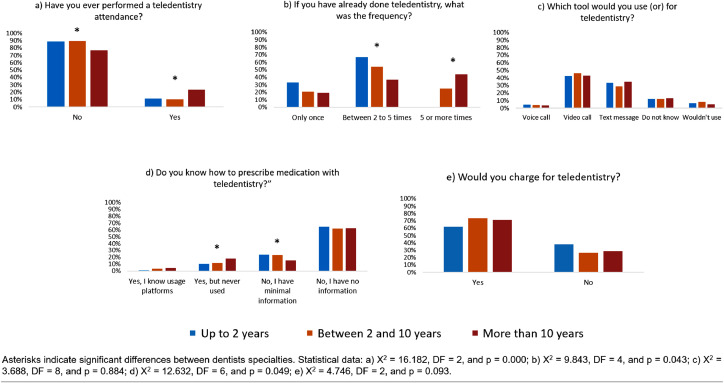
Experience
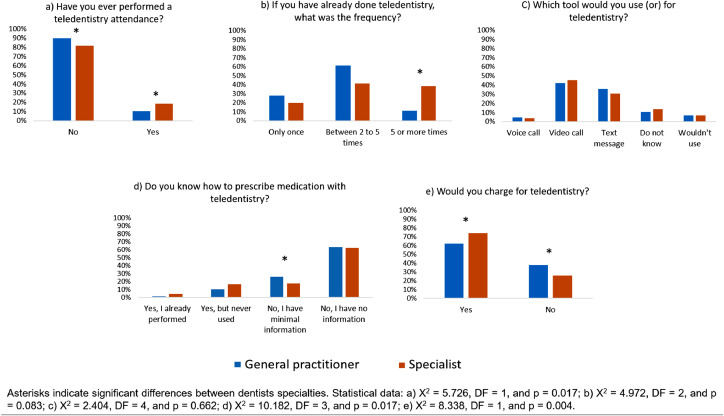
Most of the participants, irrespective of their dental specialties (Figure 4a) or practice experiences (Figure 5a), affirmed that they had never undergone teledentistry consultation before. For the participants with previous teledentistry experience, a greater number of specialists (Figure 4b, P = .083) and more experienced dentists (Figure 5b, P = .043) had performed at least 5 teledentistry consultations.
Fig. 4.
Comparison of the participants’ responses about the teledentistry practice, considering dental specialty.
Fig. 5.
Comparison of the participants’ responses about the teledentistry practice, considering dental practice experience.
Video calls and text messages were the most commonly used tools for teledentistry, irrespective of dental specialties (Figure 4c) or practice experience (Figure 5c). Overall, despite dental specialties or practice experience, most of the participants had no information about providing drug prescriptions with teledentistry. Figure 4d shows the statistical similarity for the responses between general practitioners and specialists (P = .017), and Figure 5d shows statistical similarity according to the dentists’ experience (P = .049).
It was observed that most of the participants would charge for teledentistry consultation (Figures 4e and 5e); however, there was a significant difference between the responses of general practitioners and specialists (P = .004). The amounts suggested by the participants to charge for a teledentistry consultation are presented in Supplementary File 5.
Discussion
An upsurge in the risk of infections in the context of the ongoing COVID-19 pandemic has resulted in a reduction of face-to-face appointments between dentists and patients.2,10,13 Until an effective vaccine has been adequately distributed worldwide and the disease spread has been controlled, teledentistry provides an effective alternative for the provision of dental care to patients already undergoing treatment as well as to those requiring initial diagnoses.5,12 However, awareness and experience with regard to teledentistry is essential in order for it to be effective.11,16 This study provides insight into the level of knowledge, perceptions, and experience of teledentistry amongst Brazilian dentists, particularly in the context of the COVID-19 pandemic. This questionnaire study included 575 dentists from different regions of the country (majority from the southeast region: 73.4%) who had graduated from dental school at least 10 years ago (42.4%) and had some type of specialist degree (70.4%).
The study questionnaire was distributed in June and July 2020, when the rates of COVID-19 infection were rising in Brazil17 and elaborate control measures such as social isolation and quarantine were being implemented by the Brazilian Federal Ministry of Health. At the time of the questionnaire distribution, quarantine was recommended for at least 1 month in the majority of the cities represented by the study participants.17
The findings of this study showed that a majority of the dental specialists (41.6%) were only superficially aware of the resolution of June 22, 2020, which regulates teledentistry in Brazil, whilst general practitioners (38.6%) were found to have minimal information about the resolution. Moreover, this did not change with the dentist's level of experience. These results were expected to a certain extent, because the resolution was fairly recent at the time when the questionnaire was distributed, although there was a significant effort from the FCD to reach Brazilian dentists via social networking campaigns in order to provide current information on dental treatment during the COVID-19 pandemic.
The majority of study participants reported feeling unprepared or insecure about performing teledentistry, and this could partly be explained by obstacles such as the need to develop additional knowledge and skills in digital systems for the execution of teledentistry, for example, patient record acquisition, management, sharing, and storage of personal information.13,18,19 Interestingly, specialists and professionals with more than 10 years of experience felt significantly more prepared to perform teledentistry compared to general practitioners and those with less experience, which could be due to a greater level of knowledge on oral and dental diseases and, subsequently, greater confidence in carrying out diagnosis and treatment amongst this group, as observed in previous studies.20,21 In addition, corroborating the results of the present study, it was previously observed that practicing general dentists had a higher awareness of teledentistry than postgraduate and undergraduate dental students.22
A significantly greater number of general practitioners and professionals with up to 2 years of experience considered teledentistry to be inefficient for initial diagnosis and treatment than specialists and professionals with more than 10 years of experience. These results could be explained by the greater level of knowledge and confidence amongst more experienced dentists20,21 as well as a lack of knowledge on the validity of this model of care. However, a recent systematic review23 demonstrated that teledentistry was a valid tool for reducing inappropriate orthodontic referrals, and it did not appear to significantly affect the professional's clinical judgment when compared to a visual examination. In addition, studies within the COVID-19 scenario have provided evidence of the relevance and applicability of teledentistry regarding the dental area of expertise.6, 7, 8, 9,13
Nevertheless, in the present study, despite the professional profile, a large number of dentists considered teledentistry to be inefficient. It has been previously reported that the reasons for the slow adoption of teledentistry are driven by professional readiness, lack of appropriate intraoral imaging, concerns about financial compensation, and impossibility of using radiographic examinations.6,9,24 Moreover, as previously reported,9 the lack of trust in teledentistry could be related to the restricted telehealth experience in medical and dental curricula.
Regardless of the clinical expertise or level of experience, more than 80% of the study participants had never performed teledentistry, and a minor proportion had conducted only 2 to 5 digital dental consultations. The results of this study suggest that Brazilian dentists are inadequately prepared for implementation of teledentistry, which, in turn, can impair the quality of care provided to patients. Previous studies18,23,25 have suggested that efficiency, improved quality of care, and reduced burden of oral disease were associated with key factors, such as maintenance of electronic health records and referral systems, digitisation of images, and appropriate teleconsultation, diagnosis, and monitoring.
A majority of the dentists included in this study preferred using video calls or text messages to carry out digital appointments, and these findings agree with those of previous studies that demonstrated that video conferencing was the preferred method for early diagnosis and assessment of dental caries prevalence.7,8,13,18,19,24,26,27
Considering the area of expertise, in the present study it was observed that most of the participants were endodontists (23.47%) and orthodontists (14.26%). This result could indicate that the dental specialty can influence professional adherence to teledentistry, as these professionals were more interested in the study evaluation. During the COVID-19 pandemic, it has been observed that most dental emergencies are of endodontic origin, such as symptomatic irreversible pulpitis, symptomatic apical periodontitis, acute apical abscess, and traumatic dental injuries.28 Therefore, future studies should be performed to provide a specific interpretation of each dental specialty regarding the efficiency of teledentistry.
A key finding of the current study was that, regardless of the clinical experience, more than 60% of the dentists who completed the questionnaire had no knowledge of providing prescriptions via teledentistry, which, in turn, could lead to self-medication or difficulty in accessing important drugs, such as antibiotics, amongst patients.24,29,30
Financial compensation for teledentistry assistance can be a significant disincentive for dental professionals.9,13 In this study, it was observed that most of the dentists would charge for the consultation; however, there was significant uncertainty regarding the amount to be charged. Therefore, dental authorities could regulate factors such as the time and technology required to deliver teledentistry in order to consider the appropriate remuneration for teledentistry consultations.13
Since there was a high percentage of participants from the southeast region, the results of this study could not be generalised to the entire Brazilian population. However, the Brazilian southeast region contains the majority of dental professionals and dental schools in the country, which could support the generalisability of the results. In addition, the lack of previous evidence in this area combined with an unprecedented situation, such as the COVID-19 pandemic, highlights the need to update the dental education of undergraduate students in order to prepare them for the implementation of teledentistry. Furthermore, these findings provide a quick overview of the concerns reported by dentists regarding teledentistry during the quarantine period in Brazil. Further, these data also emphasise the need for greater investment in the dissemination of adequate information and training regarding this mode of care by Brazilian dental regulation boards.
Conclusions
The COVID-19 pandemic has necessitated remote dental care via teledentistry and, in turn, highlighted a significant lack of knowledge and experience in the same amongst Brazilian dentists, regardless of the clinical expertise and experience. The findings of this study demonstrated a level of insecurity regarding the provision of remote dental care assistance amongst Brazilian dentists.
Conflict of Interest
None disclosed.
Acknowledgements
The authors would like to thank all the Brazilian professionals who answered the questionnaire and the coworkers for the assistance during the questionnaire dissemination to Brazilian dentists.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.identj.2021.07.007.
Appendix. Supplementary materials
REFERENCES
- 1.Harapan H, Itoh N, Yufika A, et al. Coronavirus disease 2019 (COVID-19): a literature review. J Infect Public Health. 2020;13:667–673. doi: 10.1016/j.jiph.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ge ZY, Yang LM, Xia JJ, Fu XH, Zhang YZ. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang. 2020;21:61–68. doi: 10.1631/jzus.B2010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Recommendation: postpone non-urgent dental procedures, surgeries, and visits. Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/oralhealth/infectioncontrol/statement-COVID.html. Accessed August 17,2020.
- 4.American Dental Association. ADA recommending dentists postpone elective procedures. American Dental Association. Available from: https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-recommending-dentists-postpone-elective-procedures. Accessed August 17, 2020.
- 5.Resolução 226/2020 do Conselho Federal de Odontologia. Available from: http://sistemas.cfo.org.br/visualizar/atos/RESOLUÇÃO/SEC/2020/226. Accessed July 9, 2020.
- 6.Telles-Araujo GT, Caminha RDG, Kallás MS, Santos PSDS. Teledentistry support in COVID-19 oral care. Clinics (Sao Paulo) 2020;75:e2030. doi: 10.6061/clinics/2020/e2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wakhloo T, Reddy GS, Chug A, Dhar M. Relevance of teledentistry during the COVID-19 pandemic. J Family Med Prim Care. 2020;25:4494–4495. doi: 10.4103/jfmpc.jfmpc_874_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Santana LADM, Santos MALD, Albuquerque HIM, et al. Teledentistry in Brazil: a viable alternative during COVID-19 pandemic. Rev Bras Epidemiol. 2020;23 doi: 10.1590/1980-549720200082. [DOI] [PubMed] [Google Scholar]
- 9.Haider MM, Allana A, Allana RR. Barriers to optimizing teledentistry during COVID-19 pandemic. Asia Pac J Public Health. 2020;32:523–524. doi: 10.1177/1010539520967603. [DOI] [PubMed] [Google Scholar]
- 10.Plaza-Ruíz SP, Barbosa-Liz DM, Agudelo-Suárez AA. Impact of COVID-19 on the knowledge and attitudes of dentists toward teledentistry. JDR Clin Trans Res. 2021;25 doi: 10.1177/2380084421998632. [DOI] [PubMed] [Google Scholar]
- 11.Wright JH, Caudill R. Remote treatment delivery in response to the COVID pandemic. Psychother Psychosom. 2020;89:130–132. doi: 10.1159/000507376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skelton-Macedo MC, Jacob CH, Ramos DL, Cardoso RJ, Antoniazzi JH. Teleodontologia: valores agregados para o clínico/especialista. Rev Assoc Paul Cir Dent. 2012;66:95–99. [Google Scholar]
- 13.Talla PK, Levin L, Glogauer M, Cable C, Allison PJ. Delivering dental care as we emerge from the initial phase of the COVID-19 pandemic: teledentistry and face-to-face consultations in a new clinical world. Quintessence Int. 2020;51(8):672–677. doi: 10.3290/j.qi.a44920. [DOI] [PubMed] [Google Scholar]
- 14.de almeida Carrer FC, Matuck B, Gomes de Lucena EH, et al. Teleodontologia e SUS: uma importante ferramenta para a retomada da Atenção Primária à Saúde no contexto da pandemia de COVID-19. Available from:https://preprints.scielo.org/index.php/scielo/preprint/view/837/version/886. Accessed June 24, 2020.
- 15.Peloso RM, Pini NI, Neto DS, et al. How does the quarantine resulting from COVID-19 impact dental appointments and patient anxiety levels? Brazilian Oral Research. 2020;34:1–11. doi: 10.1590/1807-3107bor-2020.vol34.0084. [DOI] [PubMed] [Google Scholar]
- 16.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 17.Secretarias Estaduais de Saúde. Available from: https://covid.saude.gov.br. Accessed September 28, 2020.
- 18.Daniel SJ, Kumar S. Teledentistry: a key component in access to care. J Evid Based Dent Pract. 2014;14:201–208. doi: 10.1016/j.jebdp.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Ghai S. Teledentistry during COVID-19 pandemic. Diabetes Metab Syndr. 2020;14:933–935. doi: 10.1016/j.dsx.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akbari N, Raeesi V, Khazaei T, Ramezanzadeh K, Ebrahimipour S. Evaluation of general dentists' and dental specialists' knowledge about oral cancer in South Khorasan-Iran 2014. Asian Pac J Cancer Prev. 2015;16:6987–6990. doi: 10.7314/APJCP.2015.16.16.6987. [DOI] [PubMed] [Google Scholar]
- 21.Ziegeler C, Wasiljeff K, May A. Nondental orofacial pain in dental practices–diagnosis, therapy and self-assessment of German dentists and dental students. Eur J Pain. 2019;23:66–71. doi: 10.1002/ejp.1283. [DOI] [PubMed] [Google Scholar]
- 22.Abbas B, Wajahat M, Saleem Z, Imran E, Sajjad M, Khurshid Z. Role of teledentistry in COVID-19 pandemic: a nationwide comparative analysis among dental professionals. Eur J Dent. 2020;14:S116–S122. doi: 10.1055/s-0040-1722107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alabdullah JH, Daniel SJ. A systematic review on the validity of teledentistry. Telemed J E Health. 2018;24:639–648. doi: 10.1089/tmj.2017.0132. [DOI] [PubMed] [Google Scholar]
- 24.Irving M, Stewart R, Spallek H, Blinkhorn A. Using teledentistry in clinical practice as an enabler to improve access to clinical care: a qualitative systematic review. J Telemed Telecare. 2018;24:129–146. doi: 10.1177/1357633X16686776. [DOI] [PubMed] [Google Scholar]
- 25.Khan SA, Omar H. Teledentistry in practice: literature review. Telemed J E Health. 2013;19:565–567. doi: 10.1089/tmj.2012.0200. [DOI] [PubMed] [Google Scholar]
- 26.Birur P. Smartphone and mHealth innovations for early diagnosis. In: Giannobile W, editor. IADR 10th World Congress on Preventive Dentistry, Budapest, Hungary. J Dent Res 2013. Available from: https://iadr.abstractarchives.com/home. Accessed December 15, 2021.
- 27.Giudice A, Barone S, Muraca D, et al. Can teledentistry improve the monitoring of patients during the Covid-19 dissemination? A descriptive pilot study. Int J Environ Res Public Health. 2020;13(17):3399. doi: 10.3390/ijerph17103399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silva WO, Vianna Silva Macedo RP, Nevares G, et al. Recommendations for managing endodontic emergencies during coronavirus disease 2019 outbreak. J Endod. 2021;47:3–10. doi: 10.1016/j.joen.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dana R, Azarpazhooh A, Laghapour N, Suda KJ, Okunseri C. Role of dentists in prescribing opioid analgesics and antibiotics: an overview. Dent Clin North Am. 2018;62:279–294. doi: 10.1016/j.cden.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 30.Ruiz ME. Risks of self-medication practices. Curr Drug Saf. 2010;5:315–323. doi: 10.2174/157488610792245966. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.