Abstract
Background:
Longer bariatric, colorectal, plastic, spine, and urologic operations increase complications and lengths of stay. We aimed to determine whether this is a risk factor for lung lobectomy morbidity.
Methods:
The STS GTS Database was queried for early-stage non-small cell lung cancer lobectomy with surgical duration treated as a continuous variable. Univariate and multivariate analyses compared patient and clinical characteristics with perioperative outcomes and procedure durations. Robotic were combined with thoracoscopic cases for duration analyses into minimally invasive group. All analyses were conducted in SAS v9.4 (Cary, NC) at a significance level of 0.05.
Results:
In 17,852 patients mean duration of thoracotomy, thoracoscopy and robotic lobectomies were 178± 84, 185 ± 73, and 214 ± 82 minutes respectively (p<0.001). The most common complications were prolonged air leak (12.3%), atrial fibrillation (12%), pneumonia (4.4%), and atelectasis requiring bronchoscopy (4.1%). Procedure duration was associated with increased odds of intraoperative PRBC (p <0.001) and length of stay (LOS) > 5 days (p<0.001) for both thoracotomy and minimally invasive lobectomy. Increased odds of pneumonia (p<0.001), atelectasis (p<0.001), and unexpected intensive care (ICU) admission (p=0.006) for thoracotomy lobectomy were associated with longer procedure duration. Increased lobectomy duration was not associated with readmission (p=0.549) or 30-day mortality (p=0.208).
Conclusions:
Longer early-stage lung cancer lobectomy durations are associated with postoperative morbidity and increased LOS. Although protracted operation effects on long-term survival are unknown, short-term mortality differences were not detected. Measures that decrease operative durations without sacrificing safety and oncologic outcome should be undertaken by surgeons and hospital systems.
Keywords: Lobectomy Lung cancer surgery, Surgery, complications
Longer surgical duration is one element that has been associated with increased perioperative morbidity, length of stay, and hospital readmission for multiple surgical specialties including bariatric, neurosurgical, spine pediatric, colon, and urologic surgery.1–10 Although thoracic surgery has been included in some multispecialty studies of the effect of duration on perioperative outcome, there has not been a focused study on the effects of operative duration of lung resection. Lobectomy remains the standard of care for medically operable early-stage lung cancer and is one of the most common thoracic procedures in the United States. 11,12
Due to the unique physiology sustained by patients undergoing lung resection with single lung ventilation, we hypothesized that increased surgical duration would increase the incidence of pulmonary complications. Therefore, the aim of this study was to determine whether increased surgical duration for lung resection is associated with increased perioperative morbidity and mortality, particularly for pulmonary complications.
PATIENTS AND METHODS
Case Selection
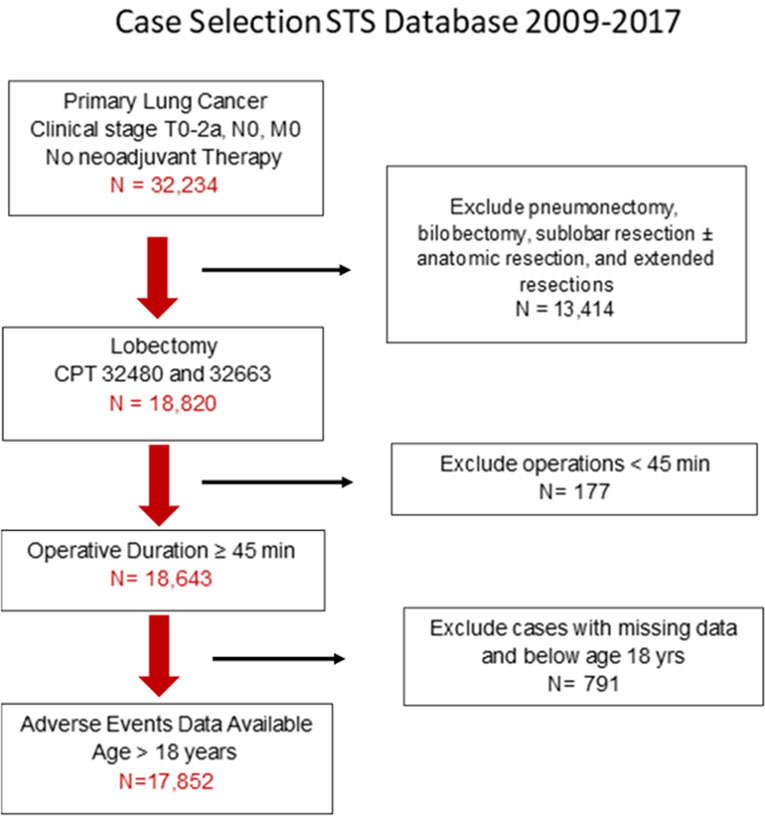
The Society of Thoracic Surgeons General Thoracic Surgery Database is comprised of validated risk adjusted data from more than 1000 participating surgeons for thoracic surgical procedures. The data are prospectively collected for quality improvement and patient safety purposes. The STS GTS database from 2009–2017 was queried for patients who had a diagnosis of primary lung cancer of clinical stage ≤T2aN0M0 (Figure 1). The sample included patients who had lung lobectomy (Current Procedural Terminology 32480 and 32663). Sublobar resection, wedge resection followed by anatomic resection, extended resection (chest wall, sleeve resection), bilobectomy, and pneumonectomy were excluded to limit the variability of oncologic severity and extent of resection between patients on outcome. Cases with operative duration < 45 minutes (an estimate of the shortest duration for anatomic lung lobectomy), patient age < 18 years, and neoadjuvant therapy were excluded, Because this study focused on operative duration and outcomes, lobectomy cases missing all adverse outcome data were excluded. Lung cancer was staged according to the 7th edition of the AJCC.13
Figure 1:
Diagram of Patient Selection 2009–2017 STS GTSD
Parameters
For calculation of surgical duration, the STS database “Procedure” time was utilized as procedure duration is designated as the “Time procedure started” to the “Time procedure ended”. STS “Operative time” was not utilized as this captured the “Time patient enters OR room” to the “Time patient exits OR room” and would include all activity prior to incision and after closure such as anesthesia administration, positioning, and emergence from anesthesia. In this manuscript, “operation” or “procedure” and “time” or “duration” will be combined interchangeably to designate the temporal length of the surgical procedure.
Statistics
Procedure duration was treated as a continuous variable. The procedure time (in minutes) was summarized by patient demographic and clinical characteristics using the mean, standard deviation, median, and interquartile ration (IQR). Patient characteristics continuous in nature (i.e. age) were dichotomized at (or near) the median. Thoracoscopic (VATS) and robotic (RATS) lobectomy cases were combined into the minimally invasive (MITS) lobectomy group for analyses due to the low number (N=1393) of robotic cases. VATS and RATS lobectomy converted to thoracotomy were analyzed in the thoracotomy (OPEN) group. Univariate associations were evaluated using the Mann-Whitney U or Kruskal-Wallis tests, as appropriate. Patient and operative characteristics were compared between OPEN and MITS lobectomy cohorts.
Univariate association between procedure time and preoperative and operative characteristics were evaluated. Association between procedure duration and intra- and post-operative outcomes were evaluated using logistic regression models. The first model evaluated the overall effect of time and included time and time-squared (to account for the non-linear association between the log-odds of the outcomes and time) as predictors. The second model evaluated the potential interaction between time and procedure type (OPEN versus MITS) and included procedure type as a main effect and interaction with the time variables. The appropriate F-tests about model coefficients were used. To evaluate the effect of mediastinal staging, the above analyses were repeated excluding cases with concurrent EBUS, mediastinotomy and/or mediastinoscopy (Supplement Tables S3 and S4). Cases missing relevant data for a given analysis or model were excluded for that analysis (Supplement Tables S7–S8). Univariate association between hospital volume with patient demographics and operative characteristics and surgical outcomes was evaluated (Appendix A). The 90th percentile of lobectomy cases performed per year was used to determine high volume (≥ 20 cases/year) versus low volume (< 20 cases/year) institutions.
Multivariate logistic regression was performed for outcomes that had significant association with duration at the <0.001 p-value on univariate analysis or pulmonary related outcomes to increase the stringency of significance which was of concern due to the multiple variables and comparisons that were made. Analysis to determine the overlap between the patient cohort with pneumonia and the cohort with other outcomes was performed using Cramer’s V (Supplement Table S6). All analyses were conducted in SAS v9.4 (Cary, NC) at a significance level of 0.05.
RESULTS
There were 17,852 lobectomy patients (45% male) who met inclusion criteria (Figure 1) with a mean age of 67.1±9.6 years. (Supplement Table S1) Most cases had comorbidities (ASA 3, 73.9%) and were former (58.4%) or current (26%) smokers. There were 11,955 thoracotomy (67.0%), 4,504 thoracoscopic (25.2%) and 1393 (7.8%) robotic lobectomy approaches. Of attempted RATS lobectomy, 12 (0.8%) were converted to VATS while 160 (11.5%) were converted to OPEN. Over time, minimally invasive lobectomy (MITS) cases increased from 68 (1.4%; 2009–2011) to 3252 (47.1%; 2015–2017). Mean operative durations for OPEN, VATS, and RATS lobectomy were 178±84 min, 185±73 min, and 214±82 min respectively (Supplement Table S2). Concomitant endobronchial ultrasound (EBUS; N=124), mediastinotomy (N=236) or mediastinoscopy (N=1546) increased mean operative time by 53 min, 39 min, and 67 min respectively. Mean and median length of stay were 7.2 and 5.0 days (OPEN) and 4.7 and 4.0 days (MITS) respectively. Although multiple patient and operative characteristics were associated with longer procedure duration on univariate analysis (Supplement Table S2); only preoperative ventilator support, robotic approach, and concurrent mediastinal staging had duration differentials ≥ 30 minutes.
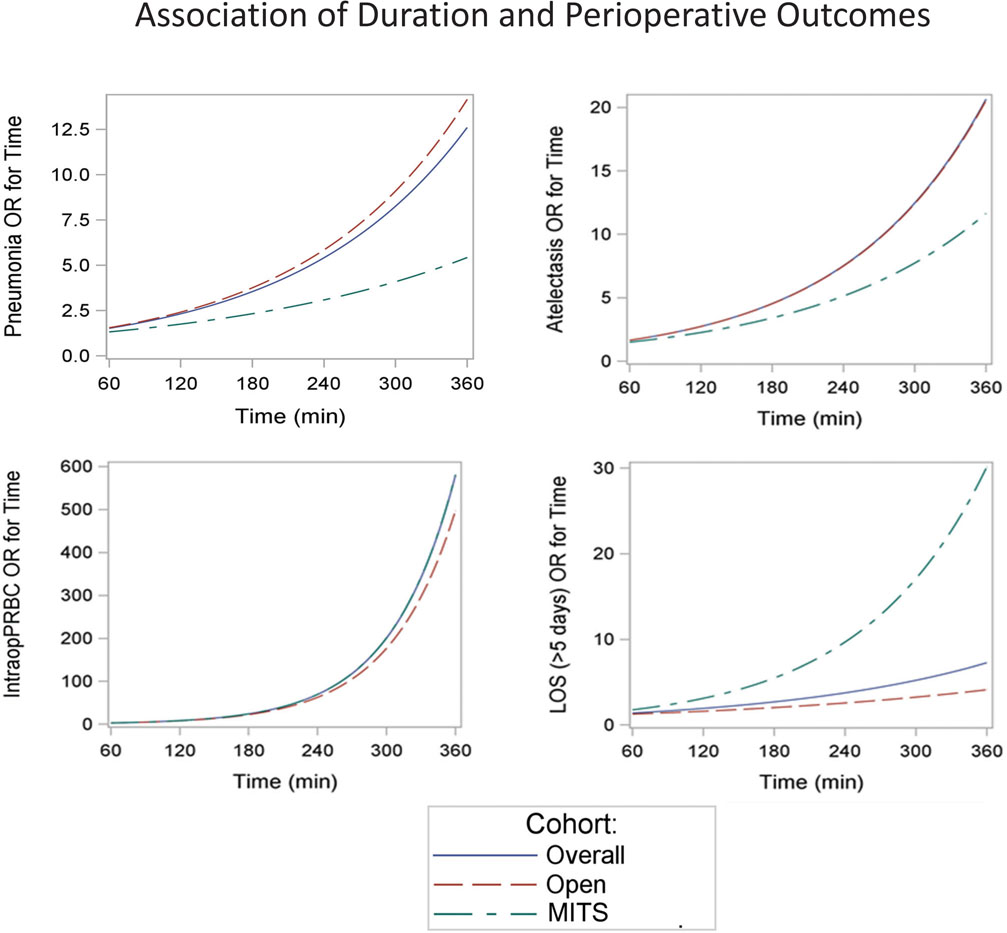
Perioperative outcomes associated with increased operative duration by univariate analysis (Table 1) were prolonged air leak, atrial fibrillation pneumonia, reintubation, ARDS, pleural effusion, atelectasis, pneumothorax, surgical site infection, UTI, sepsis, DVT, need for other surgery, unexpected ICU admission, OR return, length of stay (LOS) longer than 5 days and thirty day mortality. The only statistical interaction between duration and operative approach (OPEN or MITS) was for LOS (Table 1). The odds of pneumonia, atelectasis, unexpected ICU admission, intraoperative blood transfusion, need for another surgery, and LOS > 5 days increased as procedure duration increased with multivariate analysis (Table 2). Analysis by surgical approach showed that OPEN lobectomy duration was associated with increased odds of pneumonia (p<0.001) and unexpected ICU admission (p=0.008). Both OPEN and MITS lobectomy had increased odds of atelectasis (p<0.001 and p=0.017 respectively), intraoperative PRBC transfusion (p<0.001 both) and LOS > 5 days (p<0.001 both) as procedure duration increased. There was no association of procedure duration with readmission or 30-day mortality. When cases with concurrent mediastinal staging were removed from the analyses, the univariate and multivariate associations of increased operative duration with complications and outcomes were similar to those of the whole cohort (Supplement Tables S3 and S4).
Table 1.
Univariate Associations of Duration and Perioperative Outcomes
| Outcomes | N (%) | Operative Duration p value | Interaction by Operative Approach p value |
|---|---|---|---|
| Pneumonia | 786 (4.4%) | <.001 | 0.553 |
| Pulmonary Embolus | 90 (0.5%) | 0.036 | 0.972 |
| Intraoperative Packed Red Blood Cells | 301 (1.7%) | <.001 | 0.130 |
| UTI | 417 (2.3%) | <.001 | 0.319 |
| Wound Infection | 22 (0.2%) | 0.235 | 1.000 |
| Sepsis | 118 (0.7%) | 0.006 | 0.350 |
| New Renal Fail | 82 (0.7%) | 0.583 | 0.389 |
| DVT | 104 (0.6%) | 0.023 | 0.274 |
| Air Leak (>5 days) | 2187 (12.3%) | <.001 | 0.275 |
| Reintubation | 435 (2.9%) | <.001 | 0.246 |
| Pneumothorax | 638 (3.6%) | <.001 | 0.568 |
| Chylothorax | 86 (0.5%) | 0.118 | 0.277 |
| Surg Site Infection | 108 (0.6%) | 0.004 | 0.901 |
| Unexpected ICU | 709 (4.0%) | <.001 | 0.972 |
| Return to OR | 651 (3.7%) | <.001 | 0.203 |
| Readmission (30 days) | 215 (1.7%) | 0.317 | 0.802 |
| Other Cardiovascular Events | 312 (1.8%) | 0.003 | 0.979 |
| Other Pulmonary Events | 578 (3.3%) | <.001 | 0.368 |
| Other Gastrointestinal Events | 207 (1.2%) | 0.138 | 0.696 |
| Other Surg | 192 (1.1%) | <.001 | 0.533 |
| LOS > 5 days | 7357 (41.8%) | <.001 | <.001 |
| 30-day Mortality | 236 (1.4%) | 0.009 | 0.950 |
| Atrial fibrillation | 2129 (12.0%) | <.001 | 0.131 |
| ARDS | 140 (0.8%) | <.001 | 0.475 |
| Pleural Effusion | 220 (1.4%) | <.001 | 0.325 |
| Atelectasis | 729 (4.1%) | <.001 | 0.200 |
Table 2.
Multivariate Associations of Duration and Perioperative Outcomes by Surgical Approach
| p value | |||
|---|---|---|---|
| Outcomes | Overall | Open | MITS |
| Pneumonia | <.001 | <.001 | 0.078 |
| Intraoperative Packed Red Blood Cells | <.001 | <.001 | <.001 |
| Air Leak (>5 days) | 0.116 | 0.526 | 0.054 |
| Reintubation | 0.024 | 0.083 | 0.160 |
| Pneumothorax | 0.025 | 0.016 | 0.895 |
| Unexpected ICU | 0.011 | 0.008 | 0.985 |
| Return to OR | 0.140 | 0.165 | 0.362 |
| Readmission (30 days) | 0.549 | 0.729 | 1.000 |
| Other Surg | 0.004 | 0.055 | 0.028 |
| LOS | <.001 | <.001 | <.001 |
| 30-day Mortality | 0.208 | 0.289 | 0.330 |
| Atrial fibrillation | 0.241 | 0.783 | 0.115 |
| ARDS | 0.155 | 0.202 | 0.193 |
| Pleural Effusion | 0.805 | 0.802 | 0.953 |
| Atelectasis | <.001 | <.001 | 0.017 |
”Cut point “ operative duration after which odds of morbidity increased were modeled from the data (Supplement Table S5, Figure 2). Cut point duration was shorter than mean operative duration for both OPEN and MITS lobectomy for pneumonia, pneumothorax, reintubation, ARDS, unexpected ICU admission, need for other surgery and increased LOS. Cut point duration was longer than mean operative duration for both OPEN and MITS lobectomy for wound infection, DVT, and intraoperative packed red blood cell transfusion.
Figure 2:
Risk of Perioperative Outcomes by Operative Duration and Procedure Type
There was moderate overlap of patients who had pneumonia and reintubation, unexpected admission to the ICU, ARDS, and atelectasis (Supplement Table S6). Low volume hospitals had a higher percentage of LOS > 5 days versus high volume hospitals (43% vs 40%, p <0.001). High volume hospitals showed a trend of lower mortality rate than low volume hospitals (1.2% vs 1.6%; p = 0.058, Appendix A). There was no other significant difference in morbidity between high and low volume hospitals.
COMMENT
Longer operations increased postoperative complications in retrospective studies of single specialty procedures or studies that included multiple surgical specialty operations.1,5,6,8–10,14 Although some studies included thoracic surgery patients, to our knowledge lung resection duration effects on outcome have never been the primary focus of a study. We hypothesized that longer duration lung lobectomy would be more likely associated with pulmonary complications such as pneumonia, ARDS. reintubation, readmission to the ICU, and resultant increased LOS. We reasoned this since lung resection patients undergo unique physiologic changes from single lung ventilation including atelectasis/reinflation, hypoperfusion/ischemia and reperfusion, and increase in inflammatory mediators.15 Additionally, lung resection patients are prone to emphysema/smoking,16 age-related lung function reduction, 17 sarcopenia,18,19 and incisional chest wall pain causing splinting with impaired cough.20,21
Average operative duration of lobectomy for stage I non-small cell lung cancer listed by Chen et al22 in a meta-analysis ranged from 78–288 minutes for VATS lobectomy and 82–293 min for OPEN lobectomy. Those operative durations are consistent with mean operative duration of OPEN, VATS and RATS lobectomy for early-stage lung cancer in this current study using the STS GTSD. There is an association of longer operation duration and respiratory complications of pneumonia, atelectasis, reintubation, and unexpected ICU admission.
No difference in association of operative duration with complications and outcomes was seen when the additional time of concomitant mediastinal staging was excluded except that reintubation was no longer associated. The lack of difference in outcomes with the longer duration may be secondary to the low proportion of concurrent mediastinal staging (10.7%). Preoperative ventilator use implies respiratory compromise which may require time during operation for patient stabilization or altered anatomy from empyema, pneumonia or bronchial obstruction. Longer duration of VATS and RATS lobectomy may be due to learning curves of both the surgeon and operative team. MITS lobectomy increased by 48-fold over the 8 years of the study. As more surgeons adopt MITS lobectomy, increased duration due to learning curve may decrease until another technology emerges.
The increased odds of intraoperative PRBC transfusion and need for other surgery associated with operative duration may be indicative of bleeding or other complications prolonging lobectomy and leading to the need for other operative procedures during the hospital stay.
Licker and colleagues reviewed thoracotomy lung resections retrospectively and found operative time great than 120 min was associated with postoperative cardiopulmonary complications.23 This current study used operative duration as a continuous independent variable and similarly found higher odds of pneumonia in OPEN lobectomy patients and a trend in MITS lobectomy patients as operative duration increased. The operative time found to be a threshold for increased odds of pneumonia in OPEN lobectomy in this current study was 177 minutes (Supplement Table S5). It is notable that this duration is nearly equal the mean duration of OPEN lobectomy of 178 minutes in this study. Although the mean duration of MITS lobectomy (185 minutes) is longer than the 173 minute “cutoff”, the number of MITS lobectomy patients with pneumonia may have been too low for statistical significance (Table 2). The difference between this study and Licker et al, is that Licker utilized data from a single center performing only OPEN lobectomy and without resident physicians. Involvement of trainees is not delineated in the STS GTSD. Previous analysis of NSQIP data by our group showed increased mean operative time of 33.3 min with trainee participation. However, no difference in morbidity except decreased risk of ventilation >48 hours with trainee participation was found (Appendix B)24.
Pei et al studied patients over 70 yrs of age undergoing lung resection. Multivariate analysis revealed that surgical duration over 180 minutes was associated with occurrence of postoperative complication (OR 1.93).25 The investigators performed an analysis matching cases by age, sex, comorbidity index, pathologic stage and type of lung resection (wedge, segment, lobectomy, extended resection or pneumonectomy) to determine if there was a difference in outcomes between thoracoscopic and thoracotomy resection. They found fewer complications in the VATS group and a shorter LOS. This current study similarly showed an association of increased duration for OPEN lobectomy with pneumonia, atelectasis, unexpected ICU admission, and LOS. However, the only association of procedure duration with respiratory morbidity or mortality in MITS lobectomy was with atelectasis, and a trend for pneumonia. This study included patients younger than 70 years of age while pneumonectomy and extended resections were excluded which likely decreased risk for the cohort. Univariate analysis showed that longer LOS associated with increased operative duration may be influenced by the surgical approach. Against intuition, this analysis shows higher risk of LOS > 5 days for MITS lobectomy than for OPEN lobectomy as operative duration increases. Since the mean LOS for OPEN lobectomy is 7.2 days, (already more than 5 days), there is a greater proportion of MITS patients with LOS less than 5 days and therefore at risk of developing LOS greater than 5 days with longer operative duration.
Logic would associate pneumonia with increased risk of reintubation and unexpected ICU admission and analysis revealed moderate commonality in these patient cohorts (Supplement Table S6).
This current study found increased odds of ICU admission in OPEN lobectomy patients as operative duration increased. Two previous studies evaluating readmission to the ICU after thoracic surgery found ARDS and pneumonia to be the most common causes. Both found increased hospital mortality associated with ICU readmission.26,27 These studies had comparable unexpected ICU admission rates of 8.6% and 2.7% compared to the unexpected ICU admission rate in this study of 4.0%.
Brunelli et al 28 evaluated risk factors for 90-day mortality after VATS lobectomy or segmentectomy for stage I and II non-small cell lung cancer. Operative duration longer than 150 minutes was found to be independently associated with 90-day mortality. Patients who died within 90 days (N=18) had mean operative duration of 217 ± 114 min while patients who survived more than 90 days had a mean operative time of 151.6 ± 49.3 min. On multivariate analysis we found no association between operative duration and 30-day mortality. Brunelli et al used data from a single surgical group at a single institution from the years 2012–2016. This study includes lobectomy data from a multitude of institutions by different surgeons and both thoracotomy and minimally invasive approaches which likely accounts for the difference in findings.
The influence of hospital volume on outcomes was evaluated by two studies of VATS lobectomy29 and RATS lobectomy.30 Using HCUP-NIS data, shorter LOS, but higher complication rates at high volume VATS (>20 cases/year) institutions and shorter LOS and lower mortality rate at higher volume RATS lobectomy centers were reported. In this current study, high volume hospitals had shorter LOS and a trend of lower 30-day mortality than low volume hospitals. However, there was no other difference in perioperative outcomes between the high and low volume hospitals (Appendix A). This is notable because the patients at low volume hospitals had more comorbidities.
One limitation of this study is the retrospective analyses which may introduce misclassification, miscoding, selection bias and missing data.
Although it is advantageous to have the larger number of subjects from the 8-year span of this study, the long timespan resulted in changes in surgical approach and techniques, patient selection and preoperative evaluation, and postoperative care. Additionally, different versions of the STS data variables and multiple versions of lung cancer staging led to unavoidable inconsistencies in data.
Data about experience, training and case volume of each surgeon, and the designation of academic or non-academic hospital were not available from the STS GTSD. During the learning curve of VATS or RATS lobectomy, operative time is longer, but improves with repetition and experience. Yet another limitation is the inability to determine case complexity. Although we included only stage I tumors and single lobectomy, adhesions, anatomical variants, difficulty with single lung ventilation, equipment failures and other unanticipated occurrences can all add to operative duration or morbidities and are not captured by the database.
Conclusion
Longer early-stage lung cancer lobectomy durations are associated postoperative morbidities and increased LOS. Odds of postoperative pneumonia and ICU admission are decreased in MITS lobectomy. Although effects of longer operation on long-term survival are unknown, short-term mortality differences were not detected. Measures that decrease operative durations without sacrificing safety and oncologic outcome should be undertaken by surgeons and their hospital systems. These may include avoidance of concurrent mediastinal staging or operation on patients currently on the ventilator. As surgeons gain experience with new technology, operative duration should decrease.
Supplementary Material
Acknowledgments
This work was supported by the Roswell Park Comprehensive Cancer Center and National Cancer Institute (NCI) grant P30CA016056.
Abbreviations
- ARDS
acute respiratory distress syndrome
- AJCC
American Joint Committee on Cancer
- BMI
body mass index
- COPD
chronic obstructive pulmonary disease
- DLCO
Diffusion capacity of carbon monoxide
- EBUS
endobronchial ultrasound
- FEV1
forced expiratory volume in 1 second
- Hr
hour
- ICU
intensive care unit
- IQR
interquartile ratio
- GTS
General Thoracic Surgery
- LOS
length of hospital stay
- Min
minutes
- MITS
minimally invasive thoracic surgery
- N
number
- OPEN
thoracotomy
- OR
operating room
- PRBC
packed red blood cells
- RATS
robotic assisted thoracic surgery
- STS GTS
Society for Thoracic Surgeons General Thoracic Surgery
- UTI
urinary tract infection
- VATS
video assisted thoracic surgery
Footnotes
Disclosures: Dr. Demmy and Dr. Dexter receive royalties from Up To Date™
This manuscript was accepted for ePoster at the Annual Meeting of the STS 2021
The data for this research were provided by The Society of Thoracic Surgeons’ National Database Participant User File Research Program. Data analysis was performed at the investigators’ institution.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Routh JC, Bacon DR, Leibovich BC, Zincke H, Blute ML, Frank I. How long is too long? The effect of the duration of anaesthesia on the incidence of non-urological complications after surgery. BJU Int. 2008;102(3):301. [DOI] [PubMed] [Google Scholar]
- 2.Valentini LG, Casali C, Chatenoud L, Chiaffarino F, Uberti-Foppa C, Broggi G. Surgical site infections after elective neurosurgery: a survey of 1747 patients. Neurosurgery. 2008;62(1):88. [DOI] [PubMed] [Google Scholar]
- 3.Bernatz JT, Anderson PA. Thirty-day readmission rates in spine surgery: systematic review and meta-analysis. NeurosurgFocus. 2015;39(4):E7. [DOI] [PubMed] [Google Scholar]
- 4.Polites SF, Potter DD, Glasgow AE, et al. Rates and risk factors of unplanned 30-day readmission following general and thoracic pediatric surgical procedures. JPediatrSurg. 2016. [DOI] [PubMed] [Google Scholar]
- 5.Daley BJ, Cecil W, Clarke PC, Cofer JB, Guillamondegui OD. How slow is too slow? Correlation of operative time to complications: an analysis from the Tennessee Surgical Quality Collaborative. JAmCollSurg. 2015;220(4):550. [DOI] [PubMed] [Google Scholar]
- 6.Kim BD, Hsu WK, De Oliveira GS Jr., Saha S, Kim JY. Operative duration as an independent risk factor for postoperative complications in single-level lumbar fusion: an analysis of 4588 surgical cases. Spine (Phila Pa1976). 2014;39(6):510. [DOI] [PubMed] [Google Scholar]
- 7.McAlister FA, Bertsch K, Man J, Bradley J, Jacka M. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. AmJRespirCritCare Med. 2005;171(5):514. [DOI] [PubMed] [Google Scholar]
- 8.Owen RM, Perez SD, Lytle N, et al. Impact of operative duration on postoperative pulmonary complications in laparoscopic versus open colectomy. SurgEndosc. 2013;27(10):3555. [DOI] [PubMed] [Google Scholar]
- 9.Qin C, de Oliveira G, Hackett N, Kim JY. Surgical duration and risk of Urinary Tract Infection: An analysis of 1,452,369 patients using the National Surgical Quality Improvement Program (NSQIP). IntJSurg. 2015;20:107. [DOI] [PubMed] [Google Scholar]
- 10.Reames BN, Bacal D, Krell RW, Birkmeyer JD, Birkmeyer NJ, Finks JF. Influence of median surgeon operative duration on adverse outcomes in bariatric surgery. SurgObesRelatDis. 2015;11(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ettinger DS, Wood DE, Aggarwal C, et al. NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 1.2020. J Natl Compr Canc Netw. 2019;17(12):1464–1472. [DOI] [PubMed] [Google Scholar]
- 12.Howington JA, Blum MG, Chang AC, Balekian AA, Murthy SC. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e278S. [DOI] [PubMed] [Google Scholar]
- 13.Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. [DOI] [PubMed] [Google Scholar]
- 14.Hardy KL, Davis KE, Constantine RS, et al. The impact of operative time on complications after plastic surgery: a multivariate regression analysis of 1753 cases. AesthetSurgJ. 2014;34(4):614. [DOI] [PubMed] [Google Scholar]
- 15.Lohser J, Slinger P. Lung Injury After One-Lung Ventilation: A Review of the Pathophysiologic Mechanisms Affecting the Ventilated and the Collapsed Lung. Anesth Analg. 2015;121(2):302–318. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Chronic Disease P, Health Promotion Office on S, Health. Reports of the Surgeon General. In: The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. [Google Scholar]
- 17.Skloot GS. The Effects of Aging on Lung Structure and Function. Clin Geriatr Med. 2017;33(4):447–457. [DOI] [PubMed] [Google Scholar]
- 18.Choe EK, Lee Y, Kang HY, Choi SH, Kim JS. Association between CT-Measured Abdominal Skeletal Muscle Mass and Pulmonary Function. J Clin Med. 2019;8(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nagano A, Wakabayashi H, Maeda K, et al. Respiratory Sarcopenia and Sarcopenic Respiratory Disability: Concepts, Diagnosis, and Treatment. J Nutr Health Aging. 2021;25(4):507–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ballantyne JC, Carr DB, deFerranti S, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. AnesthAnalg. 1998;86(3):598. [DOI] [PubMed] [Google Scholar]
- 21.Richardson J, Sabanathan S, Shah R. Post-thoracotomy spirometric lung function: the effect of analgesia. A review. J Cardiovasc Surg (Torino). 1999;40(3):445–456. [PubMed] [Google Scholar]
- 22.Chen FF, Zhang D, Wang YL, Xiong B. Video-assisted thoracoscopic surgery lobectomy versus open lobectomy in patients with clinical stage Ⅰ non-small cell lung cancer: a meta-analysis. Eur J Surg Oncol. 2013;39(9):957–963. [DOI] [PubMed] [Google Scholar]
- 23.Licker M, Spiliopoulos A, Frey JG, De Perrot M, Chevalley C, Tschopp JM. Management and outcome of patients undergoing thoracic surgery in a regional chest medical centre. EurJAnaesthesiol. 2001;18(8):540. [DOI] [PubMed] [Google Scholar]
- 24.Dexter EUAK, Demmy TL,Hennon MW, Huang M, Nwogu CE, Picone AL, Yendamuri SS. JACS; 2017. [Google Scholar]
- 25.Pei G, Zhou S, Han Y, Liu Z, Xu S. Risk factors for postoperative complications after lung resection for non-small cell lung cancer in elderly patients at a single institution in China. JThoracDis. 2014;6(9):1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song SW, Lee HS, Kim JH, Kim MS, Lee JM, Zo JI. Readmission to intensive care unit after initial recovery from major thoracic oncology surgery. Ann Thorac Surg. 2007;84(6):1838–1846; discussion 1838–1846. [DOI] [PubMed] [Google Scholar]
- 27.Jung JJ, Cho JH, Hong TH, et al. Intensive care unit (ICU) readmission after major lung resection: Prevalence, patterns, and mortality. Thorac Cancer. 2017;8(1):33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brunelli A, Dinesh P, Woodcock-Shaw J, Littlechild D, Pompili C. Ninety-Day Mortality After Video-Assisted Thoracoscopic Lobectomy: Incidence and Risk Factors. Ann Thorac Surg. 2017;104(3):1020–1026. [DOI] [PubMed] [Google Scholar]
- 29.Park HS, Detterbeck FC, Boffa DJ, Kim AW. Impact of hospital volume of thoracoscopic lobectomy on primary lung cancer outcomes. AnnThoracSurg. 2012;93(2):372. [DOI] [PubMed] [Google Scholar]
- 30.Tchouta LN, Park HS, Boffa DJ, Blasberg JD, Detterbeck FC, Kim AW. Hospital Volume and Outcomes of Robot-Assisted Lobectomies. Chest. 2017;151(2):329–339. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.