Summary
Background
There is limited information on the inequity of access to vaccination in low-and-middle-income countries during the COVID-19 pandemic. Here, we described the progression of the Brazilian immunisation program for COVID-19, and the association of socioeconomic development with vaccination rates, considering the potential protective effect of primary health care coverage.
Methods
We performed an ecological analysis of COVID-19 immunisation data from the Brazilian National Immunization Program from January 17 to August 31, 2021. We analysed the dynamics of vaccine coverage in the adult population of 5,570 Brazilian municipalities. We estimated the association of human development index (HDI) levels (low, medium, and high) with age-sex standardised first dose coverage using a multivariable negative binomial regression model. We evaluated the interaction between the HDI and primary health care coverage. Finally, we compared the adjusted monthly progression of vaccination rates, hospital admission and in-hospital death rates among HDI levels.
Findings
From January 17 to August 31, 2021, 202,427,355 COVID-19 vaccine doses were administered in Brazil. By the end of the period, 64·2% of adults had first and 31·4% second doses, with more than 90% of those aged ≥60 years with primary scheme completed. Four distinct vaccine platforms were used in the country, ChAdOx1-S/nCoV-19, Sinovac-CoronaVac, BNT162b2, Ad26.COV2.S, composing 44·8%, 33·2%, 19·6%, and 2·4% of total doses, respectively. First dose coverage differed between municipalities with high, medium, and low HDI (Median [interquartile range] 72 [66, 79], 68 [61, 75] and 63 [55, 70] doses per 100 people, respectively). Municipalities with low (Rate Ratio [RR, 95% confidence interval]: 0·87 [0·85-0·88]) and medium (RR [95% CI]: 0·94 [0·93-0·95]) development were independently associated with lower vaccination rates compared to those with high HDI. Primary health care coverage modified the association of HDI and vaccination rate, improving vaccination rates in those municipalities of low HDI and high primary health care coverage. Low HDI municipalities presented a delayed decrease in adjusted in-hospital death rates by first dose coverage compared to high HDI locations.
Interpretation
In Brazil, socioeconomic disparities negatively impacted the first dose vaccination rate. However, the primary health care mitigated these disparities, suggesting that the primary health care coverage guarantees more equitable access to vaccines in vulnerable locations.
Funding
This work is part of the Grand Challenges ICODA pilot initiative, delivered by Health Data Research UK and funded by the Bill & Melinda Gates Foundation and the Minderoo Foundation. This study was supported by the National Council for Scientific and Technological Development (CNPq), the Coordination for the Improvement of Higher Education Personnel (CAPES) - Finance Code 001, Carlos Chagas Filho Foundation for Research Support of the State of Rio de Janeiro (FAPERJ) and the Pontifical Catholic University of Rio de Janeiro.
Keywords: Socioeconomic factors, Human development, Low-and-middle-income countries, Vaccine, COVID19, Primary healthcare
Research in context.
Evidence before this study
We searched PubMed for nationwide studies on estimating the association of social vulnerability, inequity, and human development with COVID-19 vaccine coverage, focusing on low-income and middle-income countries (LMICs). We searched for studies published in English, from database inception to February 25, 2022, using the following search terms: “SARS-CoV-2” OR “COVID-19” OR “COVID” AND “vaccination” OR “coverage” OR “uptake” OR “vaccination campaign” AND “inequity” OR “socioeconomic” OR “human development”. Four out of five studies used national or regional data from high-income counties. Two studies from the UK analysed cohorts with people over 50 or 70 years old and focused on estimating the association of social vulnerability aspects such as race, skin colour or ethnicity, and living in deprived areas with vaccine uptake. Similarly, one study from Israel analysed differences in vaccine rates among distinct socioeconomic statuses and ethnicity. One study from the US analysed the differences in vaccine coverage among social vulnerability at the municipality and county levels. Regarding LMICs, we found one study on Bangladesh that describes the vaccination campaign in the country, however it was not an ecological design, nor it estimated the association of inequity and vaccination rates directly. Hence, there is scarce information on the inequity of access to COVID-19 vaccination in LMICs.
Added value of this study
We performed an ecological analysis of nationwide COVID-19 immunisation data from the Brazilian National Immunization Program (PNI). The PNI is part of the Brazilian Universal Healthcare system (SUS) and has been recognised as a model of vaccination campaigns and population adhesion, being present in all 5,570 municipalities. During the first seven months of the COVID-19 vaccination campaign, more than 200 million doses were administered with distinct rates throughout the country. We observed that municipalities with low human development index (HDI) were associated with decreased first dose vaccination rates compared to those with higher HDI. The primary health care coverage was associated with increased first dose rates in those municipalities with low HDI, thus reducing the difference among locations. In addition, the progression of the pandemic control was slower in municipalities with low HDI compared to highly developed locations.
Implications of all the available evidence
Socioeconomic disparities have impacted the distribution, access, and administration of COVID-19 vaccine doses worldwide, especially in low-and-middle-income countries. In Brazil, municipalities with low socioeconomic development showed decreased first dose vaccination rates compared to highly developed locations. This low vaccination coverage may be related to limited access to vaccination by socially vulnerable populations. Universal healthcare coverage, with the presence of primary health care in vulnerable communities and cost-free vaccination, is a major driving force guaranteeing equitable access to vaccines by vulnerable populations and effective control of the pandemic.
Alt-text: Unlabelled box
Introduction
Vaccine inequity has contributed to prolonging the pandemic burden and generating new variants of concern (VoC).1,2 Limited access to COVID-19 vaccines by vulnerable populations has marked the vaccination campaign globally.3 High-income countries have concentrated dose acquisition, and poor nations are still struggling to provide their population with access to vaccines and immunisation capacity. Although much has been discussed about differences in access to vaccines between rich and poor countries,4 limited information is available on the inequity of access to vaccination within countries, especially from Low-and-Middle-Income countries (LMIC).
Socioeconomic determinants and the way healthcare systems are organised may impact vaccination coverage. Additionally, the vaccination progression variability may result in delayed mitigation or control of the disease. Access to vaccines is a function of complex chains, including the production, distribution, and administration of this often-scarce resource.5 Characterising potential differences in access to vaccines and identifying their underlying mechanisms is essential to guarantee equitable access to vaccination among nations or within their territory.
Brazil is an upper-middle-income country with a heterogeneous population distribution over an extensive territorial area. The country has substantial inequalities and other socioeconomic vulnerabilities. The presence of a decentralised, universal public health system (Sistema Único de Saúde – SUS) has been an essential factor in reducing inequities and providing the most vulnerable population with access to healthcare resources.6, 7, 8 The system's operation is driven mainly by the primary health care (PHC) services at the municipalities, such as the family health strategy (FHS), which is the main primary health program policy adopted. However, there are still challenges in guaranteeing universal coverage over the country.8
The National Immunization Program (PNI) is part of the SUS and has been recognised as a model of vaccination campaigns and population adhesion.9,10 Immunisation actions are included in prevention activities developed by the PHC, such as managing vaccination rooms and staffing, administering vaccine doses, and reporting and monitoring of adverse events. However, the COVID-19 vaccination campaign has posed new challenges. The campaign started without a nationally coordinated strategy, aiming for a speedy vaccination roll-out, and faced a high burden of the pandemic simultaneously to its execution.
It is unclear whether socioeconomic disparities have affected the vaccination rates in Brazil. We hypothesise that municipalities with low socioeconomic development had an increased hurdle in the progression of the vaccination campaign. Here, we described the progression of the Brazilian immunisation program for COVID-19, the association of socioeconomic development with vaccination rates and the potential protective effect of primary health care coverage.
Methods
Study design and participants
We performed an ecological study to analyse COVID-19 immunisation data from the Brazilian National Immunization Program Information System (Sistema de Informação do Programa Nacional de Imunização [SI-PNI]). The SI-PNI is the main data repository of vaccine doses administered in Brazil. Each record contains information on the person's demographics (age, sex and place of residence), vaccine platform, dose, date of dose administration, place of administration.11
Socioeconomic, demographic, and PHC of Brazilian municipalities was obtained from three public sources (Appendix 2 p 2). The Human Development Index (HDI) data were obtained from the 2010 Brazilian population census. We used PHC coverage data immediately before the pre-pandemic period (December/2019). The PHC has the Family Health Strategy (FHS) as its national expansion policy.12 In this model, FHS teams provide healthcare services to 2000–4000 individuals across a geographic area. In 2019, 98% of the municipalities adopted the FHS model, 60·0% of households were enrolled in the FHS, and the population coverage was 62·6% corresponding to 131,201 million people.13 The PHC coverage is measured by a national, standardised metric used to distribute resources, guide the organization of primary care teams, and monitor evolution of primary care health infrastructure.14 It is expected that each “family-health unit” can attend, or cover, 3450 individuals in their catchment area. Hence, the metric corresponds to the proportion of the municipality population covered by the FHS and FHS-equivalent teams.15,16 Data were obtained from the Ministry of Health's e-Gestor Atenção Básica database. Finally, we used 2020 Population estimates provided by the Health Surveillance Secretary from the Brazilian Ministry of Health stratified by age, sex, and municipality.17
Other data sources
We obtained data on hospitalised adult (≥20 years old) patients with COVID-19 registered in the Influenza Epidemiological Surveillance Information System (Sistema de Informação de Vigilância Epidemiológica da Gripe, SIVEP-Gripe).18 The SIVEP-Gripe is a nationwide surveillance database used to monitor severe acute respiratory infections (SARI) in Brazil since 2009′s H1N1 pandemic and currently is one of the main notification repositories for COVID-19. We analysed patient demographics (age, sex and place of residence), symptom onset, date of the outcome, and the outcome status (death or discharge). A detailed description of the SIVEP-Gripe dataset was provided elsewhere.18,19
All data were already de-identified and publicly available. Following ethically agreed principles on open data, this analysis did not require ethical approval in Brazil.
Study population
We analysed all vaccination records from January 17, the start of the COVID-19 vaccination campaign, to August 31, 2021, before the start of booster doses administration. To describe the progression of the vaccination program, we considered first, second and single doses administered within the study period. We included COVID-19 adult hospital admissions and in-hospital deaths data from the same analysis period.
COVID-19 immunisation in Brazil
The Brazilian national immunisation program (PNI) launched the COVID-19 vaccination campaign on January 17, 2021. The PNI distributed free doses of COVID-19 vaccines on a populational-basis to states and then to the municipalities that managed the local vaccination program in accordance with the available resources. The program followed a national age-based calendar during the whole period, with some local adaptions. It started in parallel vaccinating indigenous, healthcare workers and those aged 90+, then followed exclusively age-based calendar. By the end of April 2021, when almost all elderlies presented fully first dose coverage and the age allowed to vaccinate was 60–64 years, individuals with some comorbidities aged 55–59 years, and Down Syndrome, patients under chronic renal replacement therapy and pregnant women with any comorbidity, independent of age, were considered eligible for vaccination. Some other groups, such as those working on schools, also were prioritized later on, always in parallel with the age-based calendar. Four vaccine platforms were considered in the country: two doses of Sinovac-CoronaVac, ChAdOx1-S/nCoV-19 (Oxford-AstraZeneca), or BNT162b2 (Pfizer/BioNTech); or Ad26.COV2.S (Janssen) single-dose.
Outcome
Our primary outcome is the first dose vaccine coverage at the municipal level measured as the rate of first doses applied per 100 people standardised by age and sex. The standardisation used the Brazilian population as reference. The secondary outcomes are the proportion of people with at least one dose or fully vaccinated, hospital admissions and in-hospital deaths rates per 100,000 population, and the hospital admissions and in-hospital deaths rates per 1000 doses administered at the municipal level. All rates in the secondary outcomes were also standardised by age and sex.
Socioeconomic vulnerability and human development index
We considered the municipality-level Human Development Index (HDI) as a surrogate measure of socioeconomic development (Appendix 2 p 3). The HDI is a well-established international metric for human development and wellbeing conditions, favouring comparative studies with other countries. In addition, it is available at the municipality level in Brazil, being used to guide local policies. The HDI is composed of three main aspects of a location's development: Education, Income and Longevity. We classified municipalities in three main levels of HDI, according to the terciles of its distribution - Low: HDI lower than the first tercile; Medium: HDI between the first and second terciles; High: HDI greater than the third tercile. Classifying the municipalities using the terciles resulted in more balanced groups compared to the traditional HDI strata, which is divided in five groups based on equally distance HDI ranges.20 (Appendix 2 p 3).
Data analysis
The analysis was pre-specified, and the sample size was pragmatic. Data were described using medians and interquartile range (IQR) or means and standard deviations (SDs) for numeric variables and frequency and proportions for categorical variables. We performed the analysis considering complete data, and no missing value imputation was performed.
Our main analysis was conducted in three parts. First, we analysed the daily progression of the COVID-19 pandemic burden (hospital admissions per 100,000 population) and the vaccination coverage. We calculated the vaccination coverage as the number of individuals with a least one dose ("Partially vaccinated") and those with two doses or a single dose ("Fully vaccinated") for the whole country and stratified per age group, state, and platform.
Secondly, we estimated the association of HDI and the vaccination rates using a multivariable Negative Binomial regression model. The dependent variable was the standardised first dose vaccination rate, and the main exposure of interest was the human development index (considering High HDI as reference). As covariates, we considered the municipality's population size, the population density, the degree of urbanisation, the GINI index, the distance to the State capital (in kilometres, measured as the linear distance between the municipalities' and their state capitals' administrative seats), and the rate of COVID-19 hospital admissions in 2020 (previous to the start of the vaccination rollout) (Appendix 2 p 4), the five Brazilian macroregions (North, Northeast, Central-West, Southeast, and South) and the Primary healthcare coverage. A pre-specified interaction term for the HDI level and the PHC coverage was included. Numerical covariates – population, distance to the State capital, and the GINI index - were modelled using restricted cubic splines or using the log transformation when applicable (Appendix 2 p 5). Marginal means were estimated to evaluate the interplay between HDI level and the PHC coverage using averages as the representative values for the other covariates (an “average municipality”).21
Thirdly, we compared the monthly vaccination rates and the COVID-19 pandemic stratified by HDI level from January to August 2021. To evaluate the pandemic progression related to first dose vaccination, we estimated the ratios between the standardised hospital admissions and in-hospital deaths rates and the standardised first dose rates for each municipality and month. We computed the average standardised rates per 1000 doses for each month and stratified by the HDI level and their 95% confidence intervals (95% CI). Using a random-effects log-linear model (Appendix 2 p 6), we estimated each HDI level's average percentage growth rate (AGPR). The response variable was the standardised rate per 1000 doses, the predictor was the month, and the random intercept was the municipality. The APGR was obtained from the interaction term between the HDI level and the month.
We performed three sensitivity analyses to evaluate the estimates of our negative binomial model. First, we evaluated the association between the continuous HDI measure and the standardised first dose rates adjusted by the same covariates. Second, we estimated the association of HDI levels and the standardised first dose rates including the healthcare workers rates per 10,000 population for each municipality in January 2021 as a covariate (data was obtained from the National Registry of Health Facilities - CNES). Third, using the main model, we estimated the association of HDI levels and standardised first dose rates for the subset of doses administered in those older than 60 years old that were eligible by the age-based calendar. The former two analysis were performed to observe the estimated association without the effect of potential priority groups in the vaccination campaign. A significance level of 0.05 was considered for statistical tests. All the analysis was performed in R 4.2.1. We followed STROBE recommendations.
Role of the funding source
The funders had no role in any decision about the manuscript. All authors had full access to all the data in the study, LSLB, SA, BR, and OTR verified the data, and all authors approved the final version of the manuscript for publication
Results
COVID-19 and vaccination in Brazil
The number of vaccine doses for COVID-19 administered, reported by the Brazilian Immunisation program, between January 17, 2021, and August 31, 2021, reached 203,492,355 doses. After removing records with unidentified information on the city of residence and considering only first, second and single doses, 202,427,355 doses remained. Out of these, 135,921,791 (67%) doses corresponded to first, 61,668,575 (30%) to second and 4,836,989 (3%) to single doses (Appendix 2 p 7). Four distinct vaccine platforms were used in the country, ChAdOx1-S/nCoV-19, Sinovac-CoronaVac, BNT162b2, and Ad26.COV2.S (Janssen), composing 44·8%, 33·2%, 19·6%, and 2·4% of total doses, respectively (Appendix 2 p 8).
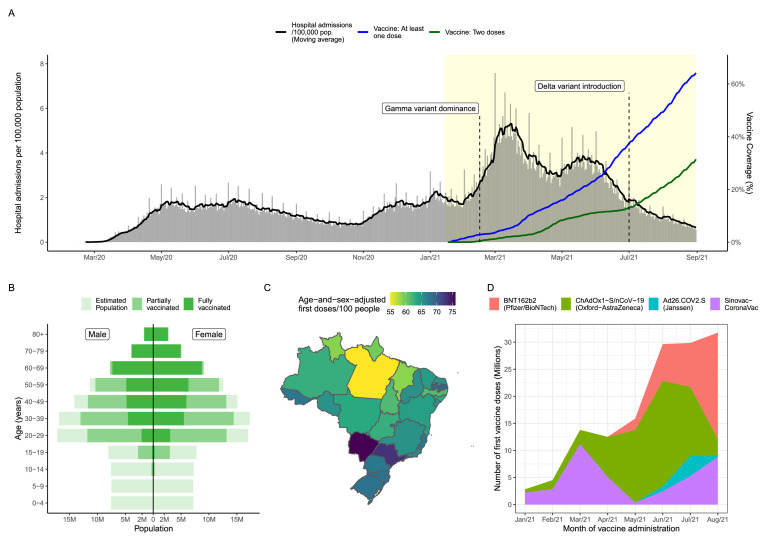
We display an overview of the immunisation program and the pandemic progression in Brazil in Figure 1. The overall first doses coverage was 64·2% and second or single doses coverage was 31·4% by the end of Aug 2021 (Figure 1A). The proportion of adults (≥20 years old) with at least one dose was 85% (129,540,717/151,778,738). Most elders were already fully vaccinated (all age strata over 60 years old with a second dose coverage >=90%, Figure 1B, Appendix 2 p 9). The administration of doses differed geographically (Figure 1C, Appendix 2 p 9): Northern states presented the lower standardised first dose rates (Pará = 54·9 doses per 100 people), compared to higher rates in the Southern states (São Paulo = 73·0 doses per 100 people).
Figure 1.
Number of COVID-19 hospital admissions, vaccine coverage and doses administered in Brazil from January 17 to August 31, 2021 (yellow-shaded area): (A) Daily number of hospital admissions per 100,000 population and vaccine coverage using the Brazilian estimated population in 2020; (B) Vaccine coverage per age and sex; (C) Age-and-sex adjusted first doses rates per 100 people per state; (D) Distribution of vaccine platforms administered per month (first doses include single doses). Reference dates are February 15, 2021, for Gamma variant dominant, and July 01, 2021, for delta variant dominance.
The progression of first doses administration also differed in terms of platforms (Figure 1D). The vaccination started with the administration of Sinovac-CoronaVac and gradually increased in number of doses over the first three months. From March to April 2021, the pace of first dose administration decelerated, with a higher presence of ChAdOx1-S/nCoV-19 compared to Sinovac-CoronaVac. Later, the progression of first doses resumed, with a higher administration of BNT162b2 doses. Ad26.COV2.S doses were less expressive than in June and July 2021 compared to other platforms. In August 2021, approximately 31·7 million doses were administered, of which 62% from BNT162b2 and 28% were from Sinovac-CoronaVac (Appendix 2 p 8).
Vaccination and inequity, the association of HDI and vaccine rates
We described the municipality's socioeconomic characteristics and standardised first dose rates (Table 1). The final sample considered 5565 out of 5570 (99%) municipalities after excluding five with missing HDI values. The Northeast (32%) and Southeast (30%) regions concentrated the majority of municipalities in Brazil. One-quarter of municipalities have more than 25,000 inhabitants. Overall, the median municipal HDI is 0.66 (IQR: 0.60, 0.72), and the median standardised first dose rate is 68 (IQR: 61, 75) doses per 100 people.
Table 1.
Sociodemographic characteristics per municipality stratified by levels of Health Development Index (N = 5565).
| Characteristics | Overall,N = 5565& | Low HDI*,N = 1864 | Medium HDI*,N = 1860 | High HDI*,N = 18411 |
|---|---|---|---|---|
| Population (number of inhabitants), median (IQR) | 11,668 (5444, 25,677) | 12,652 (6708, 21,478) | 8,854 (4648, 19,631) | 15,253 (5315, 45,041) |
| < 5,444 (Q1), N (%) | 1392 (25%) | 329 (18%) | 592 (32%) | 471 (26%) |
| 5444 to 11,665 (Q2) | 1390 (25%) | 538 (29%) | 515 (28%) | 337 (18%) |
| 11,665 to 25,663 (Q3) | 1390 (25%) | 643 (34%) | 396 (21%) | 351 (19%) |
| 25,663 to 12,325,232 | 1,393 (25%) | 354 (19%) | 357 (19%) | 682 (37%) |
| Population density (inhabitants per Km²) | 25 (12, 56) | 22 (10, 45) | 19 (9, 38) | 40 (20, 103) |
| Proportion of self-reported skin colour (%)Ψ, median (IQR) | ||||
| White | 42 (26, 67) | 25 (18, 34) | 43 (29, 64) | 69 (54, 82) |
| Black or Brown | 56 (31, 72) | 73 (64, 79) | 55 (34, 69) | 30 (17, 45) |
| Asian | 0·73 (0·39, 1·25) | 0·90 (0·53, 1·51) | 0·77 (0·41, 1·28) | 0·56 (0·29, 0·97) |
| Indigenous | 0·06 (0·01, 0·14) | 0·04 (0·01, 0·13) | 0·06 (0·02, 0·16) | 0·07 (0·03, 0·13) |
| Region, N (%) | ||||
| North | 449 (8·1%) | 257 (14%) | 171 (9·2%) | 21 (1·1%) |
| Northeast | 1794 (32%) | 1424 (76%) | 340 (18%) | 30 (1·6%) |
| Central-West | 466 (8·4%) | 21 (1·1%) | 275 (15%) | 170 (9·2%) |
| Southeast | 1668 (30%) | 142 (7·6%) | 657 (35%) | 869 (47%) |
| South | 1188 (21%) | 20 (1·1%) | 417 (22%) | 751 (41%) |
| State capital, N (%) | 27 (0·5%) | 0 (0%) | 0 (0%) | 27 (1·5%) |
| Distance to State Capital (Km), median (IQR) | 227 (122, 359) | 220 (116, 354) | 221 (128, 337) | 249 (121, 383) |
| Degree of Urbanisation | ||||
| Rural | 3363 (60%) | 1498 (80%) | 1200 (65%) | 665 (36%) |
| Semi-Urban | 746 (13%) | 220 (12%) | 282 (15%) | 244 (13%) |
| Urban | 1456 (26%) | 146 (7·8%) | 378 (20%) | 932 (51%) |
| GINI Index, median (IQR) | 0·50 (0·46, 0·55) | 0·53 (0·50, 0·57) | 0·50 (0·45, 0·54) | 0·47 (0·43, 0·51) |
| Human Development Index (HDI), median (IQR) | 0·66 (0·60, 0·72) | 0·58 (0·56, 0·60) | 0·67 (0·64, 0·69) | 0·73 (0·72, 0·76) |
| Primary health care coverage (%), median (IQR) | 100 (96, 100) | 100 (100, 100) | 100 (100, 100) | 100 (78, 100) |
| First doses rate per 100 people#, median (IQR) | 68 (61, 75) | 63 (55, 70) | 68 (61, 75) | 72 (66, 79) |
| COVID-19 statistics, median (IQR) | ||||
| Before the vaccination start (2020) | ||||
| Adult Hospital admission rate per 100,000 population#, median (IQR) | 188 (97, 321) | 138 (67, 241) | 164 (90, 287) | 273 (161, 425) |
| Adult In-hospital deaths rate# per 100,000 population#, median (IQR) | 65 (32, 112) | 56 (25, 104) | 60 (29, 107) | 79 (44, 124) |
| At the end of the period (Aug, 2021) | ||||
| Adult Hospital admission rate per 100,000 population#, median (IQR) | 671 (390, 1089) | 409 (260, 619) | 660 (426, 986) | 1085 (742, 1469) |
| Adult In-hospital deaths rate# per 100,000 population#, median (IQR) | 227 (135, 340) | 154 (93, 239) | 227 (146, 326) | 318 (217, 419) |
Five out of 5570 municipalities showed missing HDI values.
HDI levels were defined based on terciles of the Health Development Index (HDI) – Low: HDI < first tercile; Medium: first tercile ≤ HDI < second tercile; High: HDI ≥ second tercile.
Proportion of self-reported skin colour at municipality level obtained from the 2010 Brazilian population Census.
Rates were standardised by age and sex using the overall Brazilian population.
Abbreviations: Q1, first quartile; Q2, second quartile (median); Q3, third quartile; IQR, Interquartile range (first quartile to third quartile).
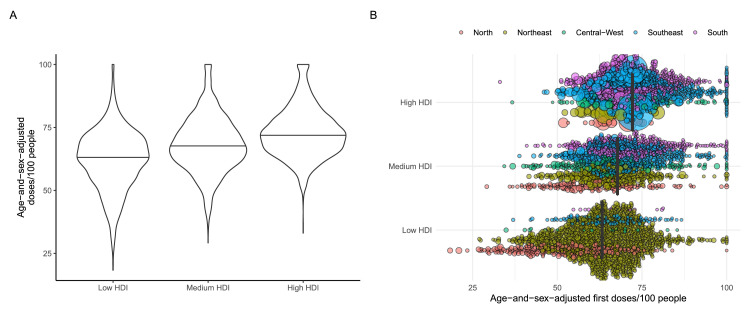
Low HDI municipalities had lower median standardised first dose coverage compared to those with medium and high HDI (63 [IQR: 55, 70] vs 68 [IQR: 61, 75] and 72 [IQR: 66, 79] doses per 100 people; Table 1). Municipalities with low and medium HDI had similar PHC coverage, higher than in high HDI locations (median 95% [IQR: 63%, 100%]). Low HDI municipalities were mainly located in the North and Northeast regions (1681/1864, 90%) and the largest municipalities, mostly from the South and Southeast regions (1620/1841, 88%), including all the State capitals, presented the highest HDIs (Figure 2, Appendix 2 pp 10-14). COVID-19 hospital admission and in-hospital death rates adjusted by age and sex were mostly concentrated in high HDI municipalities (Table 1).
Figure 2.
Distribution of first dose rates per 100 people per municipality (N = 5,565) stratified by Human Development Index [HDI] (A – violin plots) and including estimated population and macroregion (B – bee swarm plots). HDI levels were defined based on terciles of the Health Development Index (HDI) – Low: HDI < first tercile; Medium: first tercile ≤ HDI < second tercile; High: HDI ≥ second tercile. Circle size represents the population of each municipality, coloured by microregion. Solid black lines represent median values.
Association between vaccination rates per HDI level
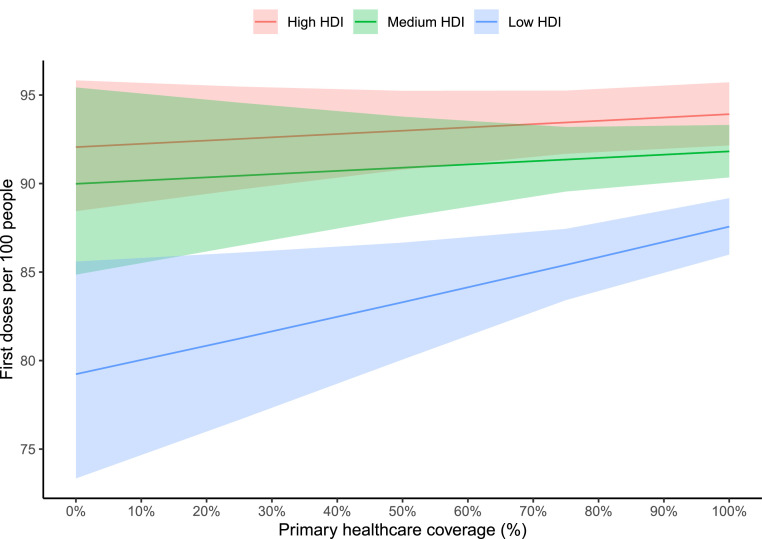
We used the negative binomial regression model to estimate the association between human development with the standardised first dose rates. Municipalities with medium (RR [95% CI]: 0·94 [0·93-0·95]) or low (RR [95% CI]: 0·87 [0·85-0·88]) HDI were associated with decreased rates compared to those with high HDI, considering the average PHC coverage (92·7%), after adjusting by population, distance to capital and region (Appendix 2 pp 15-16). The interaction term represents the association of HDI level, and the vaccination rate is modified by PHC coverage. Municipalities from the low HDI group perform more similar to high HDI levels as the PHC coverage increases (a 2-percentage point increase in doses per each PHC coverage additional 10-percentage point). For instance, the adjusted predictions from marginal means (Figure 3, Appendix 2 pp 16-18) indicate that when PHC coverage was at 50%, the low and medium HDI levels presented approximately 19% and 5% less first doses (RR [95% CI]: 0·81 [0·78-0·84] and 0·95 [0·92-0·97], respectively), compared to the high HDI municipalities, respectively; however, those differences reduce when PHC coverage increases, e.g., at 100% coverage, there were 12% less first doses (RR [95% CI]: 0·88 [0·86-0·89]) in low compared to the high HDI level. The main findings did not change in the three sensitivities analyses (Appendix 2 pp 19-24).
Figure 3.
First doses rates per 100 people according to Health Development Index (HDI) and Primary healthcare coverage estimated from marginal means. First doses rates per 100 people (y-axis) were estimated as marginal means for different Primary healthcare coverage stratified by Human Development Index (HDI) level and according to representative values of other covariates (“average municipality”). Predictions were obtained from the negative binomial regression model.
Temporal differences in vaccination rates and COVID-19 progression per HDI level
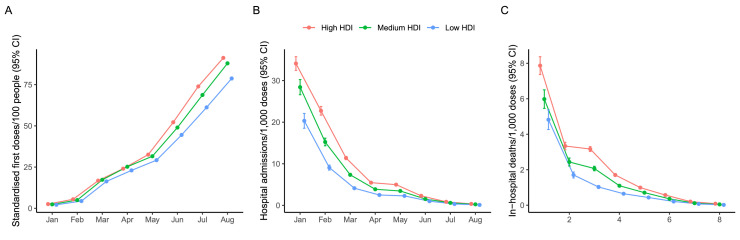
The HDI levels presented different monthly progressions and growths regarding the standardised first dose rates, COVID-19 hospital admissions and in-hospital deaths rates per 1000 doses (Figure 4). From January to April 2021, the progression of the standardised first dose rates was similar among levels (Figure 4A). However, by August 2021, municipalities with low HDI presented a lower average first dose rate than those with medium or high HDI (78·4 vs 87·9 and 91·2 standardised first doses rates per 100 people; Appendix 2 p 25). Furthermore, we evaluated the progression of standardised average hospital admissions and in-hospital deaths rates per 1000 doses. From January to August 2021, there were 1,080,422 hospital admissions and 349,350 in-hospital deaths in Brazil. Although these rates decreased throughout the period for all levels, low HDI municipalities presented a lower average reduction rate for in-hospital deaths per 1000 doses (−33·4%%, 95%CI: −35·2%, −31·6%) compared to those with medium (-36·6%, 95%CI: -38·3%, -34·9%) or high HDI (-39·8%, 95%CI: -41·4%, -38·1%, pinteraction<0·001; Appendix 2 p 26).
Figure 4.
Progression of monthly rates of standardised vaccine first doses, hospital admissions and in-hospital deaths per 1000 doses administered per Human Development Index level. Values (y-axis) correspond to average age-and-sex-adjusted rates for all municipalities (N = 5565) and their respective 95% confidence intervals: (A) cumulative first doses per 100 people; (B) Hospital admissions per 1000 doses administered (month of symptoms onset); and (C) in-hospital deaths per 1000 (month of outcome).
Discussion
We analysed the COVID-19 vaccination coverage progression in all 5570 Brazilian municipalities throughout the first seven months of the national vaccination campaign. At the end of this period, more than 200 million doses were administered, but vaccination coverage differed across the country. Municipalities with low HDI were associated with decreased first dose coverage and presented a slower progression in pandemic control than highly developed locations. Furthermore, in municipalities with low HDI, the primary care coverage was associated with an increased first dose coverage.
A few studies have analysed national data to determine social and economic factors related to differences in vaccine coverage.22, 23, 24, 25 These studies are limited to high-income countries or specific age groups. However, those analyses would be essential in low-income countries, where socioeconomic differences are expected to be more significant. Our study was the first to analyse the dynamics and inequity of vaccine coverage using nationwide data from a large LMIC. HDI was used as a surrogate measure of social vulnerability and poverty, an internationally accepted and comparable metric, and available for all Brazilian municipalities. National vaccination data were analysed dynamically and adjusted by age and sex for each municipality throughout the study period. Modelling the association of human development and vaccination coverage, we identified that municipalities with low development were associated with lower vaccination coverage after seven months compared to highly developed locations, after adjusting for population size, distance to State capitals, and region. Those differences were also observed dynamically, in which municipalities with low development presented a lower monthly coverage rate growth than highly developed locations.
One potential factor in explaining the observed difference across HDI is the logistic of dose distribution to the municipalities. The National authority centralised the distribution of vaccine doses to the states and then to the municipalities. The differences in vaccine coverage remained after adjusting for the distance to state capitals, which were the main entrance hubs of vaccine doses. Another potential factor for low vaccination coverage is vaccine hesitancy, a significant factor in high-income countries,26 particularly for a more vulnerable population. In Brazil, there was a large concern regarding a potential impact of COVID-19 vaccine hesitancy leveraged by the country's leadership and political polarity.27 However, surveys conducted previous to the COVID-19 vaccination program start showed a high willingness to take a COVID-19 vaccine in Brazil,28 similar as described in other LMIC.29,30 Additionally, we observed a high average vaccination coverage in the country with low hesitancy.31
Another factor to explain differences among municipalities are the role of primary health care teams on the management and administration of vaccine doses. For instance, the PNI demands PHC units to have vaccination rooms and supports the access to equipment and trained personnel for vaccine administration, including a cold-chain that is important to manage new vaccine platform technologies, such as the BNT162b2 (Pfizer/BioNTech). The PHC coverage metric used in this study is based on the catchment area of FHS teams, thus representing the coverage from a theoretical demand of a population within a municipality. Thus, we cannot ascertain directly the access and engagement of the population, nor performance of PHC services. Nevertheless, increased PHC coverage has been associated with better health outcomes in several domains.16 Here, it was associated with higher vaccination coverage in low HDI municipalities, suggesting that investments in primary health care might support for a better structure and organisation of the vaccination program, guaranteeing equitable access to vaccines by vulnerable populations and effective control of the pandemic.
The vaccination campaign progression was not steady over the first seven months. Although there was a slow increase in vaccine coverage in the first three months, there was a deacceleration in vaccine administration between March and April 2021. The shortage of inputs and supplies for vaccines impacted the production of new doses of Sinovac–CoronaVac and ChAdOx1-S/nCoV-19, the main platforms used in the country at this period and produced by the Butatan Institute and FIOCRUZ. The vaccine campaign regained momentum with the arrival of BNT162b2 doses after May 2021. From this moment, the administration of doses began to differ between locations, potentially indicating logistic challenges from the handling of this vaccine platform. Therefore, low HDI municipalities showed lower vaccination rates compared to higher HDI from May to August 2021. To understand the challenges in the start of the vaccination rollout during the pandemic, we restricted the analysis to the initial phase, when the system was under high pressure to vaccinate the maximum of individuals in a short time aiming to reduce the burden of disease and the impacts in mortality for the Brazilian population.19
Additionally, we observed that hospital admission and in-hospital deaths rates adjusted by doses decreased over the seven months. Low HDI municipalities showed a slower decrease in in-hospital death rates compared to higher developed locations. However, the interpretation should be cautious. Due to the ecological design, we cannot infer that the reduction in COVID-19 hospital admissions and in-hospital deaths is only due to the vaccination. In addition, we analysed the vaccination rates at municipal level, and to estimate the direct impact of the vaccination program on the control of the pandemic requires additional information (e.g., the follow-up vaccinated people, testing data, the vaccine platform used, different doses and time from vaccination) and specific study designs, such as a counterfactual analysis.
The findings of this study have to be interpreted in light of some additional limitations. First, this is an ecological analysis and we cannot translate these findings directly to the individuals in each one of the municipalities. We aggregated the data at the municipal level, so did not consider inequities within each municipality; even in high HDI locations, vulnerable populations might have difficulties accessing vaccination. Second, the process of notifying vaccine doses, hospital admissions and in-hospital deaths may be different among municipalities. For instance, low-resource locations may have higher delays or issues in releasing data in the systems compared to more developed municipalities. However, we exported the data on January 14, 2022, which minimised any potential delay from data from August 2021.32 Third, the proportion of priority groups for the vaccination schedule at municipal level might be correlated with HDI, which could led to over- or under-estimation of the association between vaccination efficiency and HDI. However, the Brazilian program in the study period was mainly based on age, and our sensitivity analysed yielded comparable results. Finally, we have no data on the supply of doses at the municipal level, nor additional local strategies for vaccination, such as the use mobile units, adapted places for vaccination beyond the PHC structure, such as churches and sports clubs, and active vaccination programs during weekends, additional efforts that some municipalities organised during 2021 in Brazil.
Our finding indicates that low socioeconomic development was associated with decreased first dose vaccination rates in Brazil, a large LMIC with significant inequality. Additionally, it reinforces the power of the universal healthcare coverage, with the presence of primary health care in vulnerable communities and cost-free vaccination, as a major component guaranteeing equitable access to vaccines by vulnerable populations and effective control of the pandemic.
Contributors
LSLB, PM, FB, SH, JCN, OTR and FAB participated in the design and concept of the study. LSLB and RR did the data curation. LSLB, SA, BR, RR, PM, FB and OTR designed the data analysis. LSLB, SA, BR, PM and FB performed the data analysis. LSLB, SA, OTR and FAB wrote the first version of the manuscript. RR, SH, OTR and FAB supervised the study. OTR and FAB are co-seniors and corresponding authors of this manuscript. All authors had full access to data, participated in data interpretation, revised the manuscript, and approved the final version of the manuscript.
Data sharing statement
All data, including individual participant data, is publicly available with de-identification and anonymisation of patients. The data sources are described in the manuscript and in the supplementary material (Appendix p 2). The raw data, dictionary, and code used for the analysis are available in a GitHub repository (https://github.com/noispuc/ICODA_BR_Vaccine_Socioeconomic).
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
SH (Silvio Hamacher) and FAB are funded by the CNPq and FAPERJ. PM is funded by CNPq (422470/2021-0) and FAPERJ (E-26/211.645/2021 and E-26/201.348/2022). OTR is funded by a Sara Borrell fellowship from the Instituto de Salud Carlos III (CD19/00110), acknowledges support from the Spanish Ministry of Science and Innovation and State Research Agency through the “Centro de Excelencia Severo Ochoa 2019–2023” Program (CEX2018-000806-S), support from the Generalitat de Catalunya through the CERCA Program, and received a research grant from the Health Effects Institute for research unrelated to this manuscript. OTR was also member of the Data Safety Monitoring Board in the REVOLUTION and STOP-COVID trials, testing treatments against COVID-19, and is currently member of the Data Safety Monitoring Board of the RENOVATE trial, testing respiratory support strategies in patients with acute respiratory hypoxaemic failure. The other authors declare that they have no conflict of interest.
All authors carried out the research independently of the funding bodies. The findings and conclusions in this manuscript reflect the opinions of the authors alone.
Acknowledgements
This work is part of the Grand Challenges ICODA pilot initiative, delivered by Health Data Research UK and funded by the Bill & Melinda Gates Foundation and the Minderoo Foundation. This study was also supported by the National Council for Scientific and Technological Development (CNPq), the Coordination for the Improvement of Higher Education Personnel (CAPES) - Finance Code 001, Carlos Chagas Filho Foundation for Research Support of the State of Rio de Janeiro (FAPERJ), the Pontifical Catholic University of Rio de Janeiro. OTR is funded by a Sara Borrell grant from the Instituto de Salud Carlos III (CD19/00110), acknowledges support from the Spanish Ministry of Science and Innovation and State Research Agency through the “Centro de Excelencia Severo Ochoa 2019–2023” Program (CEX2018-000806-S), support from the Generalitat de Catalunya through the CERCA Program received a research grant from the Health Effects Institute for research unrelated to this manuscript.
We are grateful to all healthcare workers for their endless efforts to tackle COVID-19 pandemic in Brazil. We thank the NOIS research group and the ICODA driver project EFFECT-Brazil team members for the discussions and collaborative production during the COVID-19 pandemic. All authors carried out the research independently of the funding body. The findings and conclusions in this manuscript reflect the opinions of the authors alone.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2022.100335.
Contributor Information
Otavio T. Ranzani, Email: otavio.ranzani@isglobal.org.
Fernando A. Bozza, Email: fernando.bozza@ini.fiocruz.br, bozza.fernando@gmail.com.
Appendix. Supplementary materials
References
- 1.Ye Y, Zhang Q, Wei X, Cao Z, Yuan H-Y, Zeng DD. Equitable access to COVID-19 vaccines makes a life-saving difference to all countries. Nat Hum Behav. 2022;6:207–216. doi: 10.1038/s41562-022-01289-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saha S, Tanmoy AM, Tanni AA, et al. New waves, new variants, old inequity: a continuing COVID-19 crisis. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2021-007031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Binagwaho A, Mathewos K, Davis S. Time for the ethical management of COVID-19 vaccines. Lancet Glob Health. 2021;9:e1169–e1171. doi: 10.1016/S2214-109X(21)00180-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bajaj SS, Maki L, Stanford FC. Vaccine apartheid: global cooperation and equity. Lancet. 2022;399:P1452–P1453. doi: 10.1016/S0140-6736(22)00328-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asundi A, O'Leary C, Bhadelia N. Global COVID-19 vaccine inequity: the scope, the impact, and the challenges. Cell Host Microbe. 2021;29:1036–1039. doi: 10.1016/j.chom.2021.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gurgel GD, de Sousa IMC, de Araujo Oliveira SR, de Assis, da Silva Santos F, Diderichsen F. The national health services of brazil and northern europe: universality, equity, and integrality—time has come for the latter. Int J Health Serv. 2017;47:690–702. doi: 10.1177/0020731417732543. [DOI] [PubMed] [Google Scholar]
- 7.Atun R, de Andrade LOM, Almeida G, et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015;385:1230–1247. doi: 10.1016/S0140-6736(14)61646-9. [DOI] [PubMed] [Google Scholar]
- 8.Castro MC, Massuda A, Almeida G, et al. Brazil's unified health system: the first 30 years and prospects for the future. Lancet. 2019;394:345–356. doi: 10.1016/S0140-6736(19)31243-7. [DOI] [PubMed] [Google Scholar]
- 9.Peres KC, Buendgens FB, Prates EA, et al. Vacinas no Brasil: análise histórica do registro sanitário e a disponibilização no Sistema de Saúde. Ciênc saúde coletiva. 2021;26:5509–5522. doi: 10.1590/1413-812320212611.13932021. [DOI] [PubMed] [Google Scholar]
- 10.Domingues CMAS, Maranhão AGK, Teixeira AM, Fantinato FFS, Domingues RAS. 46 anos do Programa Nacional de Imunizações: uma história repleta de conquistas e desafios a serem superados. Cad Saúde Pública. 2020;36 doi: 10.1590/0102-311X00222919. [DOI] [PubMed] [Google Scholar]
- 11.DATASUS. Brazilian Ministry of Health. National Immunisation Program Information System (SI-PNI) - SI-PNI. 2021. http://sipni.datasus.gov.br/. Accessed 13 September 2021.
- 12.Macinko J, Harris MJ. Brazil's family health strategy — delivering community-based primary care in a universal health system. N Engl J Med. 2015;372:2177–2181. doi: 10.1056/NEJMp1501140. [DOI] [PubMed] [Google Scholar]
- 13.Giovanella L, Bousquat A, Schenkman S, de Almeida PF, Sardinha LMV, Vieira MLFP. Cobertura da Estratégia Saúde da Família no Brasil: o que nos mostram as Pesquisas Nacionais de Saúde 2013 e 2019. Ciênc Saúde Coletiva. 2021;26:2543–2556. doi: 10.1590/1413-81232021266.1.43952020. [DOI] [PubMed] [Google Scholar]
- 14.DATASUS. Brazilian Ministry of Health. Technical note - primary health care coverage teams supported by the Ministry of health. 2021. https://egestorab.saude.gov.br/image/?file=20211119_O_notacoberturaapspns_4413967205649403244.pdf. Accessed 25 May 2022.
- 15.Jesus GS, Pescarini JM, Silva AF, et al. The effect of primary health care on tuberculosis in a nationwide cohort of 7·3 million Brazilian people: a quasi-experimental study. Lancet Glob Health. 2022;10:e390–e397. doi: 10.1016/S2214-109X(21)00550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ. 2014;349:g4014. doi: 10.1136/bmj.g4014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DATASUS. Brazilian Ministry of Health. Population estimates. http://tabnet.datasus.gov.br/cgi/deftohtm.exe?popsvs/cnv/popbr.def. Accessed 7 February 2022.
- 18.Ranzani OT, Bastos LSL, Gelli JGM, et al. Characterisation of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respiratory Med. 2021;9:407–418. doi: 10.1016/S2213-2600(20)30560-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bastos LS, Ranzani OT, Souza TML, Hamacher S, Bozza FA. COVID-19 hospital admissions: Brazil's first and second waves compared. Lancet Respiratory Med. 2021;9:e82–e83. doi: 10.1016/S2213-2600(21)00287-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United Nations Development Programme. Human Development Reports - Brasil. Municipality Human Development Index 2010. https://www.undp.org/pt/brazil/idhm-munic%C3%ADpios-2010. Accessed 3 October 2022.
- 21.Norton EC, Dowd BE, Maciejewski ML. Marginal effects—quantifying the effect of changes in risk factors in logistic regression models. JAMA. 2019;321:1304. doi: 10.1001/jama.2019.1954. [DOI] [PubMed] [Google Scholar]
- 22.Barry V, Dasgupta S, Weller DL, et al. Patterns in COVID-19 vaccination coverage, by social vulnerability and urbanicity — United States, December 14, 2020–May 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:818–824. doi: 10.15585/mmwr.mm7022e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nafilyan V, Dolby T, Razieh C, et al. Sociodemographic inequality in COVID-19 vaccination coverage among elderly adults in England: a national linked data study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-053402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perry M, Akbari A, Cottrell S, et al. Inequalities in coverage of COVID-19 vaccination: a population register based cross-sectional study in Wales, UK. Vaccine. 2021;39:6256–6261. doi: 10.1016/j.vaccine.2021.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saban M, Myers V, Ben-Shetrit S, Wilf-Miron R. Socioeconomic gradient in COVID-19 vaccination: evidence from Israel. Int J Equity Health. 2021;20:242. doi: 10.1186/s12939-021-01566-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stojanovic J, Boucher VG, Gagne M, et al. Global trends and correlates of COVID-19 vaccination hesitancy: findings from the iCARE study. Vaccines. 2021;9:661. doi: 10.3390/vaccines9060661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xavier DR, Lima e Silva E, Lara FA, et al. Involvement of political and socio-economic factors in the spatial and temporal dynamics of COVID-19 outcomes in Brazil: a population-based study. Lancet Reg Health - Am. 2022;10 doi: 10.1016/j.lana.2022.100221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moore DCBC, Nehab MF, Camacho KG, et al. Low COVID-19 vaccine hesitancy in Brazil. Vaccine. 2021;39:6262–6268. doi: 10.1016/j.vaccine.2021.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bono SA, Edlaine Faria de Moura V, Siau CS, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low- and middle-income countries. Vaccines. 2021;9:515. doi: 10.3390/vaccines9050515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solís Arce JS, Warren SS, Meriggi NF, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27:1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lotta G, Fernandez M, Kuhlmann E, Wenham C. COVID-19 vaccination challenge: what have we learned from the Brazilian process? Lancet Glob Health. 2022;10:e613–e614. doi: 10.1016/S2214-109X(22)00049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rocha R, Atun R, Massuda A, et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health. 2021;9:e782–e792. doi: 10.1016/S2214-109X(21)00081-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.