Abstract
Background
Following the outbreak of COVID-19, global healthcare systems have had to rapidly adapt. People with multiple sclerosis (pwMS) were required to make decisions about their individual risk and consequent work and social behaviors. This study aimed to evaluate risk perception and patterns of shielding behavior amongst pwMS at the onset of the COVID-19 pandemic and the subsequent impact on patients’ employment and access to disease modifying therapies (DMTs).
Methods
Postal surveys were sent to 1690 people within a UK population-based MS cohort during the first wave of the COVID-19 pandemic. Patients were surveyed on: (i) perceived vulnerability to COVID-19; (ii) isolation behavior; (iii) interruption to DMT; (iv) employment status; (v) level of satisfaction with their current working arrangement.
Results
Responses were received from 1000 pwMS. Two thirds of patients reported isolating at home during the first wave of the pandemic. This behavior was associated with increased age (p<0.0001), higher disability (p<0.0001) and use of high-efficacy DMTs (p = 0.02). The majority of patients reported feeling vulnerable (82%) with perceived vulnerability associated with higher EDSS (p<0.0001) and receiving a high-efficacy DMT (p = 0.04). Clinician-defined risk was associated with shielding behavior, with those at high-risk more likely to self-isolate/shield (p<0.0001). Patients on high-efficacy DMTs were more likely to have an interruption to their treatment (50%) during the first wave of the pandemic. Most pwMS experienced a change to their working environment, and most were satisfied with the adjustments.
Conclusion
This study highlights the risk perception, social behavioral practices and changes to treatment experienced by pwMS during the first wave of the COVID-19 pandemic in a large, well-described UK cohort. The results may help inform management of pwMS during future pandemic waves.
Keywords: Multiple sclerosis, COVID-19, Disease-modifying therapies
1. Introduction
Following the initial identification of COVID-19 in early 2020 (Huang et al., 2020; WHO 2020), governments and healthcare systems around the world were forced to impose public health interventions, including ‘lockdowns’, to protect regional and national populations. At the start of the pandemic, it was unclear whether people with multiple sclerosis (pwMS) would be more at risk of contracting COVID-19 or whether they would experience more severe disease, particularly given the widespread use of immunomodulating disease modifying therapies (DMTs) and the presence of advanced disability in a significant proportion of patients. Previous studies suggested that both factors may be relevant to COVID-19 risk (Wijnands et al., 2018; Luna et al., 2019; Persson et al., 2020).
Consequently, pwMS have had to make difficult individual decisions, aided by national guidance, regarding their social behaviours including the degree of self-isolation/shielding and changes to their working environment. In addition, healthcare provision has had to adapt to minimise risk to patients (Moss and Bermel, 2020). Understanding risk perception, social behaviour and access to treatment amongst pwMS during the pandemic helps to inform future public health and governmental strategies.
This study aimed to evaluate risk perception and patterns of shielding behaviour in pwMS during the COVID-19 pandemic, and the impact of COVID-19 on patients’ employment and access to DMTs.
2. Methods
Between May and November 2020, a postal survey was sent to 1690 pwMS in the Cardiff and Cwm Taf regions of South Wales, UK. The target group was a population-based cohort of pwMS who live in an area of southeast Wales that has a total population of approximately 1 million. Data collection for this population has been conducted by means of a cross-sectional epidemiological study in 1985 (Swingler and Compston, 1988) with periodic updates thereafter (Hennessey et al., 1999, 1989). Since 1999, longitudinal data have been gathered prospectively on this population and is estimated to have captured more than 97% of the MS cases in this region (Hirst et al., 2009). The current study was performed as a service evaluation to understand the impact of COVID-19 on MS service delivery.
The survey contained questions on: (i) perceived vulnerability to COVID-19; (ii) isolation behaviour (social distancing, self-isolation, shielding); (iii) interruption to DMT; (iv) employment status and (v) level of satisfaction with their current working arrangement. Participants were asked to record data referring to the period of lockdown (March – June 2020), when community virus transmission was high. Data on age, disability (last documented Expanded Disability Status Scale (EDSS) score) (Kurtzke, 1983) and DMT were retrieved from medical records and matched with the survey responses from each patient. Non-responders were followed up by telephone where possible. Contemporary data on cumulative COVID-19 incidence was obtained from Public Health Wales (Public Health Wales, 2021) in order to compare contemporaneous incidence of COVID-19 in the UK population with shielding behavior in our cohort.
During the first lockdown, social distancing was recommended for the entire population. Self-isolation was a term used to imply higher vigilance than social distancing alone and was recommended for pwMS. Shielding was defined as not leaving the home and minimising face-to-face contact even with household contacts and was recommended for pwMS thought to be at the highest risk of COVID-19. PwMS were categorised into high- and low-risk according to national guidance from the Association of British Neurologists and UK MS Society at the time (UK Government, 2020). Specifically, pwMS who had received alemtuzumab or cladribine during the last 12 weeks were considered high risk. In addition, those with two or more of the following risk factors were also considered high risk: age greater than 70 years; EDSS ≥6.0; pregnancy; alemtuzumab or cladribine in the past 6 months; ocrelizumab or rituximab in the past 12 months; current use of fingolimod. For the purposes of analysis, high-efficacy DMT was defined as monoclonal antibody treatment, while all other DMTs were considered moderate-efficacy. EDSS was dichotomised into the following categories: <4; 4–5.5; 6–7.5; 8–10.
Statistical analysis was performed in Microsoft Excel and Graphpad Prism. Kruskall-Wallis with Dunn's post-hoc test for multiple comparisons was performed on non-parametric means. Chi-squared tests were used on categorical data.
3. Results
3.1. Demographics
Survey responses were received from 1000 patients (59% response rate). The median age amongst responders was 55 years (range: 21 – 93 years) and 71% were female (age and sex were missing for one respondent). EDSS data was available for 998 patients (99.8%), with a median score of 5.5 (range: 0 - 9.5). The mean time between the last recorded EDSS score (before or after survey date) and survey response was 1.1 years (median 0.6 years, range 0 – 17.9 years) with the date of EDSS and survey response available for 943 patients. Six hundred and seventy-four patients (67%) were not receiving a DMT. Of those 326 pwMS on a DMT, 160 (49.1%) and 166 (50.9%) were receiving high- and moderate-efficacy treatment respectively. The mean age of patients on no DMT, moderate- and high-efficacy DMT was 59.8, 47.4 and 44.2 years respectively.
Two hundred and thirty-eight patients (23.8%) elected to shield during the study period, while 428 (42.8%) and 302 (30.2%) chose to self-isolate or social distance respectively. Twenty-five patients (2.5%) did not regard themselves as complying with any category: either due to their employment circumstances, reliance on residential care or being unaware of the guidance. Data on social behavior was missing for 7 patients (0.7%).
3.2. Age & disability
Mean EDSS was higher in pwMS who were not on any DMT versus those on moderate- and high-efficacy DMTs (5.2 vs. 3.3 vs. 3.5 respectively; p<0.0001). The mean age of those choosing to either self-isolate or shield was significantly higher than those performing social distancing (57.6y vs. 55.0y vs. 51.4y; p<0.0001). In addition, EDSS was higher in those who chose to self -isolate or shield versus those who performed social distancing only (5.0 vs. 5.3 vs. 3.5; p<0.0001).
3.3. DMT usage
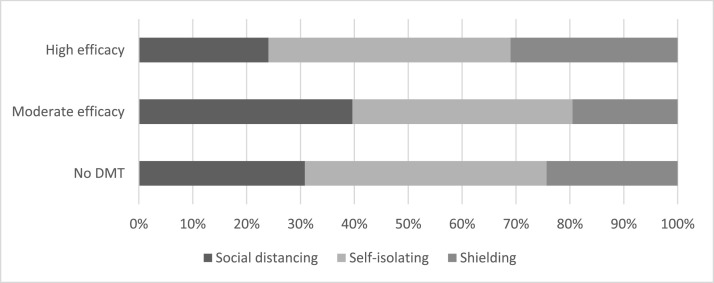
There was no significant difference between DMT exposure in those who chose to socially distance, self-isolate or shield (34% vs. 32% vs. 34%; p = 0.83). However, there was a statistically higher chance of shielding in those on high-efficacy DMT (31%) compared to those taking moderate-efficacy DMT (19%) and those not taking DMT (24%) (p = 0.02). Fig. 1 demonstrates the shielding behaviors according to DMT category.
Fig. 1.
Shielding behavior as a proportion of disease modifying therapy group.
Patients on high-efficacy DMTs were significantly more likely to experience a change or interruption to their treatment compared to those on moderate-efficacy treatment (80/160 (50%) vs. 11/166 (7%) (p<0.0001). The most common reason for treatment change for those on high-efficacy DMTs was a change in dose/frequency or stopping treatment by the MS clinical team (99%); only 1% experienced a change driven by patient choice.
3.4. Clinical risk & vulnerability
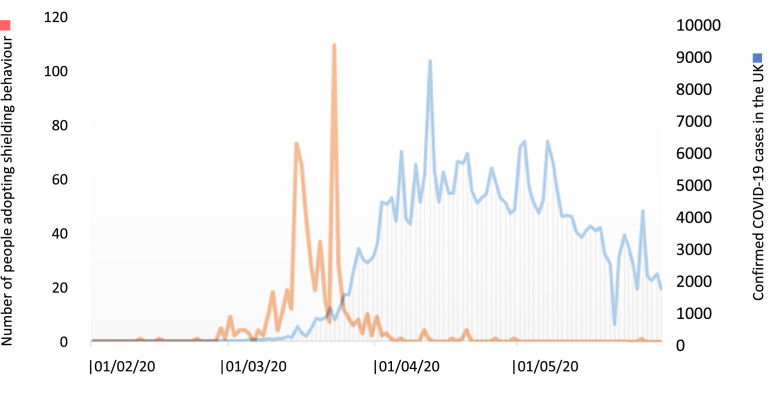
The timing of shielding behavior coincided with the initial surge of cases in the UK (Fig. 2 ).
Fig. 2.
Number of pwMS commencing self-isolating/shielding behavior over time compared to UK COVID-19 incidence in the UK according to viral RNA PCR testing.
An 85.2% agreement was found between clinician-defined risk and shielding behavior (shielding or self-isolation). This was significantly different to the numbers of low-risk patients who elected to shield or self-isolate (64.1%, p<0.0001).
The majority of pwMS felt vulnerable during the first wave of the pandemic (808/988, 82%). There was a statistically significant difference between DMT and perceived vulnerability; a higher proportion of people taking a high-efficacy DMT felt vulnerable compared with people taking a moderate-efficacy DMT or not receiving treatment (88.7% vs. 82.5% and 79.9% respectively) (p = 0.04). However, more pwMS not receiving a DMT felt extremely vulnerable compared with the other groups (p = 0.01).
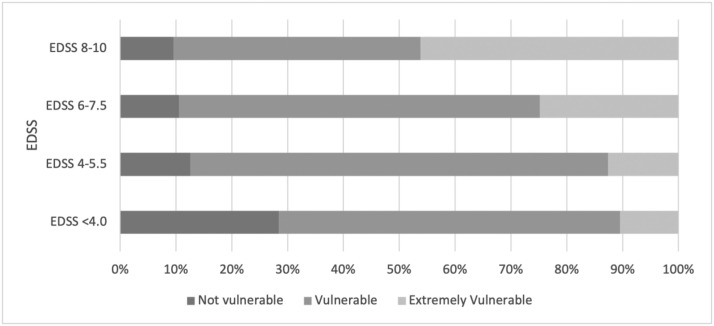
People with higher EDSS were also more likely to feel vulnerable to than those with low EDSS (p<0.0001). Fig. 3 demonstrates levels of self-perceived vulnerability according to disability.
Fig. 3.
Perceived vulnerability by level of disability.
3.5. Working environment
Three hundred and sixty-nine respondents (36.9%) were in employment prior to the COVID-19 pandemic. Of those previously employed, 347 patients responded regarding their current working arrangements: 62% reported to be now working from home, 20% were in their usual environment, 15% were unable to work/furloughed due to lockdown restrictions and 3% were redeployed. Those on high-efficacy DMTs were less commonly working in their usual environment compared to those on moderate-efficacy DMTs and those not on DMTs (14% vs. 24% vs. 24%), although this difference did not reach statistical significance (p = 0.14).
There was a significant association between disability and working environment (p = 0.04), with a lower proportion of pwMS with high EDSS working in their usual workplace, albeit the number of pwMS with EDSS >6.0 in employment was small. Most patients were satisfied with their current working arrangements with the highest rate of satisfaction amongst patients working from home (95%) and the lowest rate in those who were redeployed (70%).
4. Discussion
In March 2020, the UK government recommended that people with chronic health conditions, such as MS, adopt shielding behaviour in order to protect themselves from COVID-19 infection (UK Government, 2020). For pwMS, many of the factors associated with an increased risk of contracting COVID-19 and disease severity were the same as those identified in the general population such as increasing age, male sex, comorbidities and Black/African ethnicity (Chaudhry et al., 2020; Louapre et al., 2020; Parrotta et al., 2020; MS Rb-NBSGFoC-a 2021; Reder et al., 2021; Salter et al., 2021; Sormani et al., 2021). Specific to MS, progressive disease course and increased levels of disability were initially suspected, and have since been shown, to be associated with more severe COVID-19 infection (Chaudhry et al., 2020; Louapre et al., 2020; Parrotta et al., 2020; Salter et al., 2021; Sormani et al., 2021) along with treatment with an anti-CD20 agent (Reder et al., 2021; Salter et al., 2021; Sormani et al., 2021) or recent use of methylprednisolone (Salter et al., 2021; Sormani et al., 2021). Given the risk to pwMS, this study aimed to better understand the perceived level of vulnerability to COVID-19 infection amongst pwMS during the first COVID-19 wave in the UK and whether pwMS altered their social behaviors or experienced a change to their working environment and treatment regime.
Overall, this study demonstrated that over half of pwMS adopted some form of isolation behavior (beyond social distancing) during the first wave of the COVID-19 pandemic. Higher age and disability status were associated with shielding and self-isolating behavior, and patients on high-efficacy DMTs were more likely to shield. In addition, patients on high-efficacy DMTs were more likely to experience an interruption to treatment, mainly due to clinical advice, which has also been demonstrated in other studies (Moss and Bermel, 2020; Lavorgna et al., 2020; Vogel et al., 2020; Zhang et al., 2021).
A high level of risk perception to contracting COVID-19 has previously been found in pwMS - attributed to having MS itself, a higher level of disability, older age and to receiving DMTs (Zhang et al., 2021; Evangelou and dasNair, 2020). As a consequence, this perceived vulnerability has led to postponed appointments, laboratory studies, and imaging (Lavorgna et al., 2020; Vogel et al., 2020; Zhang et al., 2021). In this study, the majority of patients felt vulnerable, but risk perception appeared particularly driven by a higher level of disability and use of high-efficacy DMTs. However, pwMS not on a DMT were more likely to feel extremely vulnerable, which may in part be explained by a higher age and level of disability in this group. In this study, clinician-defined risk was associated with shielding behavior. Of note, although the questionnaire asked about vulnerability to COVID-19 risk, it is acknowledged that this question may not have been able to discriminate between feeling vulnerable to MS disease-related concerns or because of the risk from the virus itself.
Given the requirement for self-isolation and shielding, changes to patients’ working environment have also been described (Vogel et al., 2020). In our cohort, a large proportion of patients were required to work from home albeit with a high level of satisfaction about their current working arrangements. Patients taking high-efficacy DMTs were least commonly working in their usual environment although this was not statistically significant.
There are several limitations to the current study, including the risk of ascertainment and recall bias. Levels of compliance with social distancing guidelines have been shown to be negatively related to various socio-economic factors independent of MS: younger age, a requirement to work on site, lower education levels and residing in a more disadvantaged area (Moss and Bermel, 2020; Evangelou and dasNair, 2020). It is acknowledged that these factors may have had an influence on the results of this study but were not included in the routine data collection.
This study highlights the lived experience of pwMS during the early part of the COVID-19 pandemic. The results of this study should help inform responses to future viral pandemics or further waves of the current pandemic. Specifically, pwMS with higher levels of disability and those on high-efficacy DMTs should be recognised as more liable to feelings of vulnerability, and social isolation is more likely in people deemed at higher risk. PwMS receiving higher-efficacy DMTs may also be more liable to greater treatment disruption.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
R. Beesley: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. M. Cauchi: Investigation. L. Davies: Investigation. M. Upcott: Investigation. E. Norton: Investigation. S. Loveless: Investigation. V. Anderson: Investigation. R. Wynford-Thomas: Investigation. T.P. Pickersgill: Investigation. E. Uzochukwu: Formal analysis. M. Wardle: Resources. N.P. Robertson: Conceptualization, Methodology, Investigation, Writing – review & editing. E. Tallantyre: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. M.D. Willis: Formal analysis, Investigation, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
Author has declared no conflict of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.msard.2022.104121.
Appendix. Supplementary materials
References
- Chaudhry F., Bulka H., Rathnam A.S., Said O.M., Lin J., Lorigan H., et al. COVID-19 in multiple sclerosis patients and risk factors for severe infection. J. Neurol. Sci. 2020;418 doi: 10.1016/j.jns.2020.117147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evangelou N.G.A., dasNair R., et al. Self-diagnosed COVID-19 in people with multiple sclerosis: a community-based cohort of the UK MS register. J. Neurol. Neurosurg. Psychiatry. 2020 doi: 10.1136/jnnp-2020-324449. Aug 27;jnnp-2020-324449Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessey A., Robertson N.P., Swingler R., Compston D.A. Urinary, faecal and sexual dysfunction in patients with multiple sclerosis. J. Neurol. 1999;246(11):1027–1032. doi: 10.1007/s004150050508. [DOI] [PubMed] [Google Scholar]
- Hennessy A.S., Swingler R.J., Compston D.A. The incidence and mortality of multiple sclerosis in south east Wales. J. Neurol. Neurosurg. Psychiatry. 1989;52(9):1027–1032. doi: 10.1136/jnnp.52.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirst C.I.G., Pickersgill T., Swingler R., Compston D.A., Robertson N.P. Increasing prevalence and incidence of multiple sclerosis in South East Wales. J. Neurol. Neurosurg. Psychiatry. 2009;80(4):386–391. doi: 10.1136/jnnp.2008.144667. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtzke J.F. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33(11):1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- Lavorgna L., Alnajashi H., Jabbad R. Behavioral practices of patients with multiple sclerosis during Covid-19 pandemic. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0241103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louapre C., Collongues N., Stankoff B., Giannesini C., Papeix C., Bensa C., et al. Clinical characteristics and outcomes in patients with coronavirus disease 2019 and multiple sclerosis. JAMA Neurol. 2020;77(9):1079. doi: 10.1001/jamaneurol.2020.2581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luna G., Alping P., Burman J., Fink K., Fogdell-Hahn A., Gunnarsson M., et al. Infection risks among patients with multiple sclerosis treated with fingolimod, natalizumab, rituximab, and injectable therapies. JAMA Neurol. 2019 doi: 10.1001/jamaneurol.2019.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss B.P.M.K., Bermel R.A., et al. Multiple sclerosis management during the COVID-19 pandemic. Mult. Scler. 2020;26(10):1163–1171. doi: 10.1177/1352458520948231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MS Rb-NBSGFoC-a Incidence and clinical outcome of Coronavirus disease 2019 in a cohort of 11,560 Brazilian patients with multiple sclerosis. Mult. Scler. 2021 doi: 10.1177/1352458520978354. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Parrotta E., Kister I., Charvet L., Sammarco C., Saha V., Charlson R.E., et al. COVID-19 outcomes in MS. Neurol. Neuroimmunol. Neuroinflamm. 2020;7(5):e835. doi: 10.1212/NXI.0000000000000835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson R., Lee S., Ulcickas Yood M., Wagner Usn Mc C.M., Minton N., Niemcryk S., et al. Infections in patients diagnosed with multiple sclerosis: a multi-database study. Mult. Scler. Relat. Disord. 2020;41 doi: 10.1016/j.msard.2020.101982. [DOI] [PubMed] [Google Scholar]
- Public Health Wales. Rapid COVID-19 virology - Public 2021 [Available from: https://public.tableau.com/app/profile/public.health.wales.health.protection/viz/RapidCOVID-19virology-Public/Headlinesummary.
- Reder A.T.C.D., Naylor M.L., Nagpal A., Rajbhandari R., Altincatal A., Kim M., Berdofe A., Radhakrishnan M., Jung E., Sandrock A.W., Smirnakis K., Popescu C., de Moor C. COVID-19 in patients with multiple sclerosis: associations with disease-modifying therapies. CNS Drugs. 2021 doi: 10.1007/s40263-021-00804-1. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salter A.F.R., Newsome S.D., Halper J., Li D.K.B., Kanellis P., Costello K., Bebo B., Rammohan K., Cutter G.R., Cross A.H. Outcomes and risk factors associated with sars-cov-2 infection in a north american registry of patients with multiple sclerosis. JAMA Neurol. 2021 doi: 10.1001/jamaneurol.2021.0688. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sormani M.P., De Rossi N., Schiavetti I., Carmisciano L., Cordioli C., Moiola L., et al. Disease-modifying therapies and coronavirus disease 2019 severity in multiple sclerosis. Ann. Neurol. 2021;89(4):780–789. doi: 10.1002/ana.26028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swingler R.J., Compston D.A. The prevalence of multiple sclerosis in south east Wales. J. Neurol. Neurosurg. Psychiatry. 1988;51(12):1520–1524. doi: 10.1136/jnnp.51.12.1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UK Government. COVID-19: guidance on shielding and protecting people defined on medical grounds as extremely vulnerable. 21/03/2020 2020 [Available from: https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19.
- Vogel A.C., Schmidt H., Loud S., McBurney R., Mateen F.J. Impact of the COVID-19 pandemic on the health care of >1,000 people living with multiple sclerosis: a cross-sectional study. Mult. Scler. Relat. Disord. 2020;46 doi: 10.1016/j.msard.2020.102512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Novel coronavirus - China 2020 [Available from: http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/.
- Wijnands J.M.A., Zhu F., Kingwell E., Fisk J.D., Evans C., Marrie R.A., et al. Disease-modifying drugs for multiple sclerosis and infection risk: a cohort study. J. Neurol. Neurosurg. Psychiatry. 2018;89(10):1050–1056. doi: 10.1136/jnnp-2017-317493. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Staker E., Cutter G., Krieger S., Miller A.E. Perceptions of risk and adherence to care in MS patients during the COVID-19 pandemic: a cross-sectional study. Mult. Scler. Relat. Disord. 2021;50 doi: 10.1016/j.msard.2021.102856. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.