Abstract
Microblading is a novel method of semi-permanent makeup, which has achieved popularity in the last few years. We present the case of a patient who developed cutaneous sarcoidosis after microblading of her eyebrows. A 45-year-old female presented with a 6-month history of pruritic erythematous granulomatous plaques on bilateral eyebrows corresponding to the site of microblading 1.5 years prior. A tissue biopsy was preformed which was consistent with cutaneous sarcoidosis. An extensive work-up including assessment by respirology, rheumatology, and ophthalmology did not reveal any evidence of systemic sarcoidosis. The patient was treated with intralesional triamcinolone injections and tacrolimus ointment twice daily, with complete resolution. To our knowledge, this is the first case of cutaneous sarcoidosis associated with microblading in the literature. Dermatologists should be aware of popular and novel cosmetic procedures and the potential complications that arise from these interventions.
Keywords: Microblading, sarcoidosis, cosmetic dermatology, eyebrow tattoos
Introduction
Microblading, also known as eyebrow feathering/eyebrow embroidery, is a method of semi-permanent makeup, which has achieved popularity in the last few years. 1 Using this technique, pigment is introduced into the skin until the level of the papillary dermis using linear rows of needles.1,2 This technique results in the appearance of natural feathery-appearing hairs.1,2 Although most commonly used for eyebrow pigmentation, this technique has also been employed in scalp pigmentation for alopecia. Unlike traditional permanent tattooing, pigmentation lasts 1–3 years, largely due to the shallower depth of pigment deposition.1–3 Several risks have been associated with this cosmetic procedure including allergic contact dermatitis and skin and soft tissue infections. 2 We present the case of a patient who developed a cutaneous sarcoidosis to microblading of her eyebrows.
Case report
A 45-year-old female presented with a 6-month history of a pruritic erythematous granulomatous plaques on the bilateral eyebrows corresponding to the site of microblading 1.5 years prior (Figure 1). She had a prior medical history of hypothyroidism and migraines which were being managed with levothyroxine and eletriptan, respectively. Physical examination showed firm erythematous to beige granulomatous linear plaques affecting the length of bilateral eyebrows. A punch biopsy was performed to evaluate differential diagnoses which included sarcoidosis or allergic contact dermatitis. Tissue biopsy showed sarcoidal granulomas throughout the dermis with multinucleated giant cells. There was stippling of exogenous pigment throughout, which was more prominent within superficial macrophages. Spongiosis was also identified in the epidermis. The patient was also referred for allergic patch testing using Chemotechnique diagnostics’ North American 80 Comprehensive series, which identified a 2+ reaction to 4-tert-butylphenol formaldehyde resin. This allergen is a shoe adhesive used to glue leather parts together and is unrelated to dyes used in microblading. Her presentation was consistent with cutaneous sarcoidosis, and the patient was treated with intralesional triamcinolone 2.5 mg/mL injections and tacrolimus 0.1% ointment twice daily as needed, with complete resolution (Figure 2).
Figure 1a,b,c.
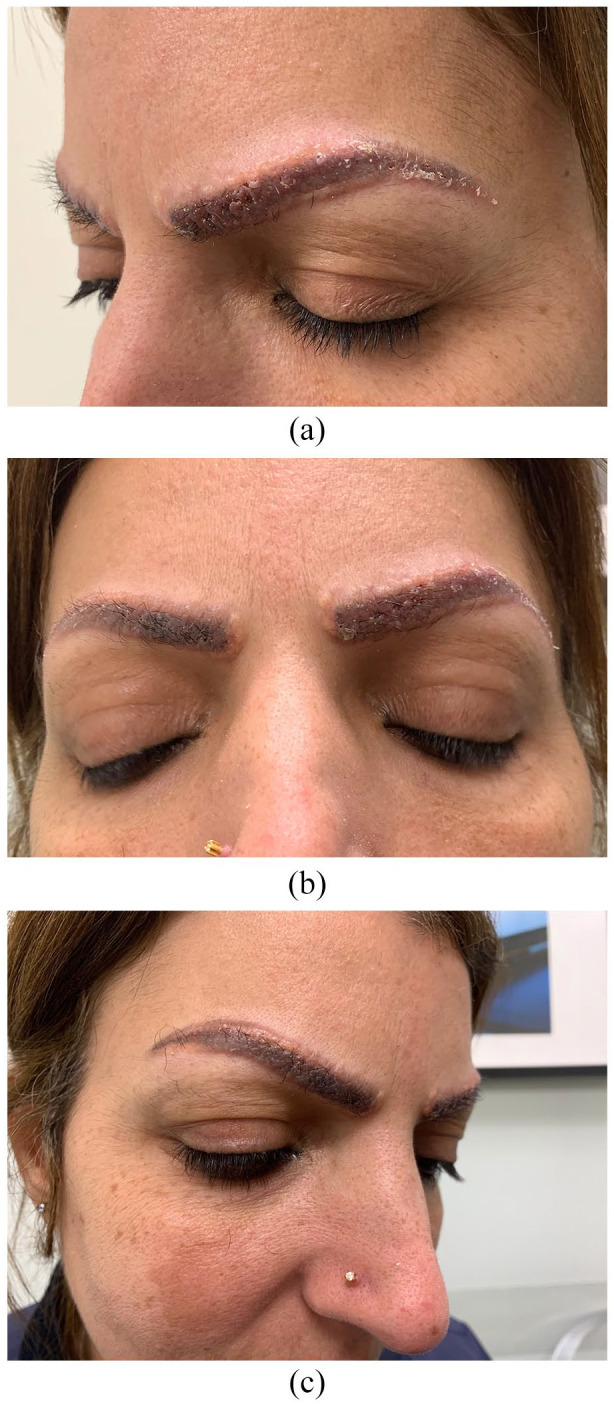
Baseline photos before treatment on 9 October 2019.
Figure 2a & b.

Photos after treatment on 4 November 2020.
A work-up for systemic sarcoidosis was subsequently preformed. The patient denied symptoms of systemic sarcoidosis including fever, night sweats, chills, ocular irritation/dryness, oral ulcers, chest pain, or shortness of breath. However, she endorsed arthralgia in wrists with morning stiffness lasting longer than 30 min. The results of hematological, biochemical, and inflammatory tests were unremarkable aside from Anti-ds DNA, which was found to be borderline positive with titer of 5. She had normal renal function, and there was no evidence of hypercalcemia. Imaging results including chest X-ray, echocardiogram, and X-rays of the hands, knees, ankles, and feet were unremarkable, suggesting no systemic involvement. She was seen by respirology who found no evidence of pulmonary sarcoidosis. She had normal pulmonary function tests (PFTs) with Diffusion Capacity of the Lungs for Carbon Monoxide (DLCO). She was referred to ophthalmology who found no evidence of ocular sarcoidosis. She was seen by rheumatology who found no evidence of internal or joint involvement. At one-year follow-up, there were still no signs of systemic sarcoidosis.
Discussion
Cutaneous sarcoidosis following tattooing has been described numerous times in the literature. 4 We performed a literature review of cases of cutaneous eyebrow sarcoidosis in the context of permanent or semi-permanent cosmetic tattooing. The results of this review are summarized in Table 1. In total, there were 21 cases (15 studies) identified in the literature. All of the identified cases occurred after permanent eyebrow tattooing. There were no cases of cutaneous sarcoidosis described following microblading (semi-permanent method) of the eyebrows. Onset of tattoo sarcoidosis from permanent or semi-permanent pigmentation varied significantly from 4 months to 25 years. There were also several cases which developed after multiple tattoo applications.
Table 1.
Summary of literature describing cutaneous sarcoidosis in permanent or semi-permanent cosmetic eyebrow tattoos.
| Study | n | Type of permanent/semi-permanent pigmentation | Onset after procedure | Morphology of eyebrow lesions | Histology | Systemic sarcoidosis | Treatment |
|---|---|---|---|---|---|---|---|
| Wang et al. 5 | 1 | Permanent cosmetic tattooing | 20 years | Scaly erythema and edema | Non-caseating epithelioid granulomas surrounded by lymphocytic infiltrate | Yes | Unknown |
| Demirci et al. 6 | 1 | Permanent cosmetic tattooing | Multiple procedures in last 10 years (most recent 2 years ago) | Hard, shiny yellowish papules arranged in a linear pattern along eyebrows and upper vermillion border | Non-caseating histiocyte granulomas surrounded by infiltrate of lymphocytes with foreign body-type giant cells | No, but increased serum ACE level | Clobetasol propionate 0.1% ointment |
| Mirzaei et al. 7 | 1 | Permanent cosmetic tattooing | Multiple procedures, most recent 4 months | Red papules | No biopsy | Yes | Adalimumab and prednisolone |
| Antonovich and Callen 8 | 1 | Permanent cosmetic tattooing | 3 years | Translucent skin-colored papules arranged linearly along eyebrows | Sarcoidal granulomas and scattered pigment granules | No, but hilar adenopathy | Doxycycline hyclate, mid-potency topical corticosteroid |
| Ebrahimiadib et al. 9 | 2 | Permanent cosmetic tattooing | 4–6 months | Red papules with associated swelling and scaling | Non-caseating granuloma | Yes | Methotrexate, systemic and topical corticosteroid |
| Monroe 10 | 1 | Permanent cosmetic tattooing | 15 years | Coalescent papules in linear pattern along the left brow | Granulomatous dermatitis consisting of nodular collections of epithelioid histiocytes and multinucleated giant cells | No | Intralesional triamcinolone |
| Landers et al. 11 | 1 | Permanent cosmetic tattooing | 25 years | Erythematous brown plaques with rolled borders surrounding eyebrow tattoos | Non-caseating granulomas with large, pale-staining, epithelioid histiocytes | Yes, pulmonary sarcoidosis | Prednisone, tacrolimus 0.1% ointment |
| Naeini et al. 12 | 1 | Permanent cosmetic tattooing | 10 years | Red, scaly patches | Non-necrotizing granulomas with a few lymphocytes | Yes, pulmonary sarcoidosis | Prednisone, topical steroid, pimecrolimus 1% |
| Huisman et al. 13 | 5 | Permanent cosmetic tattooing | Multiple treatments in 4–15 years (last treatment 1–18 months) | Not described | Granulomatous inflammation | Yes, in 2/5 | Potent topical steroids, intralesional corticosteroids |
| Vera et al. 14 | 1 | Permanent cosmetic tattooing | 7 years | Red, and itchy supraorbital skin swellings and loss of both eyebrows | Dense nodular infiltrate with epithelioid nodules, histiocytes, many giant multinucleated Langerhans cells as well as intra and extracellular foreign body-like black granulomas | Yes | Intralesional triamcinolone |
| Miguel-Gómez et al. 15 | 1 | Permanent cosmetic tattooing | 10 years | Reddish papules and nodules | Non-caseating epithelioid cell granulomas with foreign material and pigmented granules | Yes | Prednisone, intralesional injections |
| Hinojosa et al. 16 | 1 | Permanent cosmetic tattooing | 3 years | Brown-pink verrucous plaques with overlying crusting on tattooed eyebrows | Nodular collections of epithelioid histiocytes surrounded by sparse infiltrate of lymphocytes in the dermis with the presence of asteroid body | Yes | Intralesional corticosteroids |
| Valbuena et al. 4 | 1 | Permanent cosmetic tattooing | 16 years | Yellow infiltrated plaques on bilateral ciliary lesions | Thick dermis with epithelioid granulomas involving the entire dermis surrounded by lymphocytic infiltrates | No | Intralesional triamcinolone |
| Bombonato et al. 17 | 1 | Permanent cosmetic tattooing | Unknown | Coalescing hard yellow-red papules located on eyebrows | Superficial and deep dermal non-necrotizing granulomatous inflammation with few giant cells | Unknown | Unknown |
| Martìn et al. 18 | 2 | Permanent cosmetic tattooing | 2–6 years | Firm, elevated erythematous nodules | Non-caseous epithelioid and Langerhans cells granulomata in reticular dermis, without/with lymphocytic component | No | Allopurinol, mometasone furoate, topical clobetasol propionate |
ACE: angiotensin-converting enzyme.
Of the 21 patients with cutaneous eyebrow sarcoidosis, 10 were found to have systemic sarcoidosis, or to subsequently develop systemic sarcoidosis. After full work-up of our patient, there was no evidence of systemic sarcoidosis, which persisted at 1-year follow-up. Nonetheless, several patients with permanent tattoos developed systemic sarcoidosis years after initial presentation with cutaneous sarcoidosis. This may possibly be due to an immune response to ongoing exposure to foreign materials in the skin, which is a known etiology of systemic sarcoidosis.6,12,19,20 However, because the pigmentation in microblading is non-dispersible, and hence difficult to retain for more than a few years, the theoretical risk of this is less than in permanent tattoos.1,21 Nevertheless, in patients who have granulomatous reactions to microblading, it may be reasonable to recommend against future pigmentation to avoid the risk of developing systemic manifestations of sarcoidosis.
To our knowledge, this is the first case of cutaneous sarcoidosis associated with microblading in the literature. With the expansion of the cosmetic procedure industry, dermatologists should be aware of popular and novel cosmetic procedures and the potential complications that arise from these interventions to facilitate appropriate management.22,23 It is also important to note that there is significant influence of social media on the public’s interest in cosmetic procedures. 24 As such, the focus of future research should be to characterize social media and public interest in cosmetic procedures and to outline the medical considerations for these procedures.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Patient provided written informed consent to publish case report and images.
ORCID iDs: Alison Spurr  https://orcid.org/0000-0001-7109-7063
https://orcid.org/0000-0001-7109-7063
Sophia Colantonio  https://orcid.org/0000-0003-4297-2337
https://orcid.org/0000-0003-4297-2337
References
- 1. Marwah MK, Kerure AS, Marwah GS. Microblading and the science behind it. Indian Dermatol Online J 2021; 12(1): 6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wong E, Environmental Health BCIT School of Health Sciences and Heacock H. Biological hazards associated with microblading and evaluation of its infection control procedures and wound care. BCIT Environ Public Heal J. Epub ahead of print April 2018. DOI: 10.47339/EPHJ.2018.56. [DOI] [Google Scholar]
- 3. Tierney E, Kavanagh GM. Koebnerization secondary to microblading. J Cosmet Dermatol 2021; 20(4): 1040–1041. [DOI] [PubMed] [Google Scholar]
- 4. Valbuena MC, Franco VE, Sánchez L, et al. Sarcoidal granulomatous reaction due to tattoos: report of two cases. An Bras Dermatol 2017; 92(5, Suppl. 1): 138–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang WM, Zhu CY, Jin HZ, et al. Systemic sarcoidosis revealed by sarcoidal granulomas on eyebrow tattoos. Eur J Dermatol 2018; 28(4): 561–562. [DOI] [PubMed] [Google Scholar]
- 6. Demirci GT, Mansur AT, Yildiz S, et al. Is it a sarcoidal foreign-body granuloma or a cutaneous sarcoidosis on a permanent eyebrow make-up? J Cosmet Laser Ther 2016; 18(1): 50–52. [DOI] [PubMed] [Google Scholar]
- 7. Mirzaei A, Joharimoghadam MM, Zabihiyeganeh M. Adalimumab-responsive refractory sarcoidosis following multiple eyebrow tattoos: a case report. Tanaffos 2017; 16(1): 80–83, https://pubmed-ncbi-nlm-nih-gov.proxy.bib.uottawa.ca/28638429/ (accessed 5 December 2021). [PMC free article] [PubMed] [Google Scholar]
- 8. Antonovich DD, Callen JP. Development of sarcoidosis in cosmetic tattoos. Arch Dermatol 2005; 141(7): 869–872. [DOI] [PubMed] [Google Scholar]
- 9. Ebrahimiadib N, Adelpour F, Ghahari M, et al. Intermediate uveitis associated with tattooing of eyebrows as a manifestation of systemic sarcoidosis: report of two cases. Ocul Immunol Inflamm 2021; 29: 902–905. [DOI] [PubMed] [Google Scholar]
- 10. Monroe JR. What caused these unusual bumps on the left eyebrow? Sarcoidosis. JAAPA 2011; 24(3): 18. [DOI] [PubMed] [Google Scholar]
- 11. Landers MC, Skokan M, Law S, et al. Cutaneous and pulmonary sarcoidosis in association with tattoos. Cutis 2005; 75(1): 44–48, https://pubmed-ncbi-nlm-nih-gov.proxy.bib.uottawa.ca/15732434/ (accessed 5 December 2021). [PubMed] [Google Scholar]
- 12. Naeini FF, Pourazizi M, Abtahi-Naeini B, et al. Looking beyond the cosmetic tattoo lesion near the eyebrow: screening the lungs. J Postgrad Med 2017; 63(2): 132–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huisman S, van der Bent SAS, Wolkerstorfer A, et al. Granulomatous tattoo reactions in permanent makeup of the eyebrows. J Cosmet Dermatol 2019; 18(1): 212–214. [DOI] [PubMed] [Google Scholar]
- 14. Vera C, Vera J, Ball E, et al. Red and itchy bilateral supraorbital swellings. J Dtsch Dermatol Ges 2018; 16(12): 1503–1506. [DOI] [PubMed] [Google Scholar]
- 15. Miguel-Gómez L, Vañó-Galván S, Sido-Ahmed B, et al. Sarcoidal infiltration of tattoos. Cleve Clin J Med 2014; 81(12): 717–718. [DOI] [PubMed] [Google Scholar]
- 16. Hinojosa T, Lewis DJ, Sharghi KG, et al. Verrucous eyebrows: a cutaneous manifestation of a systemic disease. J Eur Acad Dermatol Venereol 2017; 31(10): e430–e432. [DOI] [PubMed] [Google Scholar]
- 17. Bombonato C, Argenziano G, Lallas A, et al. Orange color: a dermoscopic clue for the diagnosis of granulomatous skin diseases. J Am Acad Dermatol 2015; 72(Suppl. 1): S60–S63. [DOI] [PubMed] [Google Scholar]
- 18. Martín JM, Revert Á, Monteagudo C, et al. Granulomatous reactions to permanent cosmetic tattoos successfully treated with topical steroids and allopurinol. J Cosmet Dermatol 2007; 6(4): 229–231. [DOI] [PubMed] [Google Scholar]
- 19. Marcoval J, Maná J, Moreno A, et al. Foreign bodies in granulomatous cutaneous lesions of patients with systemic sarcoidosis. Arch Dermatol 2001; 137: 427–430, https://jamanetwork.com/journals/jamadermatology/article-abstract/478298 (accessed 4 December 2021). [PubMed] [Google Scholar]
- 20. Morales-Callaghan AM, Aguilar-Bernier M, Martínez-García G, et al. Sarcoid granuloma on black tattoo. J Am Acad Dermatol 2006; 55(Suppl. 5): S71–S73. [DOI] [PubMed] [Google Scholar]
- 21. Haney B. Permanent and semi-permanent micro-pigment treatments. In: Aesthetic procedures: nurse practitioner’s guide to cosmetic dermatology. 2020, pp. 59–66. DOI: 10.1007/978-3-030-19948-7_7. [DOI] [Google Scholar]
- 22. Tierney EP, Hanke CW. Recent trends in cosmetic and surgical procedure volumes in dermatologic surgery. Dermatol Surg 2009; 35(9): 1324–1333. [DOI] [PubMed] [Google Scholar]
- 23. Wang JV, Akintilo L, Geronemus RG. Growth of cosmetic procedures in millennials: a 4.5-year clinical review. J Cosmet Dermatol 2020; 19(12): 3210–3212. [DOI] [PubMed] [Google Scholar]
- 24. Hopkins ZH, Moreno C, Secrest AM. Influence of social media on cosmetic procedure interest. J Clin Aesthet Dermatol 2020; 13(1): 28–31, https://pubmed-ncbi-nlm-nih-gov.proxy.bib.uottawa.ca/32082468/ (accessed 4 December 2021). [PMC free article] [PubMed] [Google Scholar]


