Abstract
Background:
Both natural grass (NG) and artificial turf (AT) are popular playing surfaces for soccer. Biomechanical studies have found increased frictional forces on AT that may lead to anterior cruciate ligament (ACL) injury. The increased risk of ACL injury during soccer in female participants may amplify this effect.
Purpose:
To systematically review the literature for studies comparing ACL injury risk in soccer players on AT versus NG and to specifically determine whether there were differences in injury risk in male versus female players when considering the playing surface.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
A systematic review was performed using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Three databases were searched for studies with evidence level 1 to 3 that compared the incidence of ACL injuries on AT versus NG in soccer players. Data recorded included study characteristics, sex, competition level, exposure setting (games or practices), turf type, and ACL injury information. Study methodological quality was analyzed using the methodological index for non-randomized studies (MINORS) score, and incidence rate ratios (IRRs) were calculated.
Results:
Included were 7 articles (3 studying professional soccer, 3 collegiate soccer, 1 youth-level soccer; 4 male cohorts, 2 female cohorts, and 1 male and female cohort; mean MINORS score, 20 ± 0.8). Pooled ACL injury IRRs demonstrated no significant differences in overall ACL injury risk when playing soccer on AT compared with NG (IRR = 0.57 [95% CI, 0.21-1.53]; P = .31). A significantly increased risk of ACL injury in games played on AT compared with NG was detected for female (IRR = 1.18 [95% CI, 1.05-1.31]; P = .004) but not for male players (IRR = 1.18 [95% CI, 0.97-1.42]; P = .09). Subgroup analyses showed no significant differences in injury risk for games (IRR = 1.07 [95% CI, 0.97-1.18]; P = .20) or practices (IRR = 0.21 [95% CI, 0.04-1.23]; P = .09).
Conclusion:
Findings indicated that female soccer players had a significantly higher risk of ACL injury when playing games on AT versus NG, whereas no significant difference was seen in male players. No differences were found for the combined male/female cohort or for soccer games or training sessions played on AT compared with NG.
Keywords: ACL, artificial turf, female, gender, injury risk, natural grass, playing surface, sex, soccer
Soccer is the most popular sport in the world, with >265 million athletes playing globally. 25 While soccer is most often played on natural grass (NG) surfaces, artificial turf (AT) surfaces have become increasingly popular because of their ease of maintenance, durability, and consistent field conditions. 13,48 However, since the introduction of AT fields in the 1960s, there has been controversy over the effect on injury of this playing surface. First- and second-generation ATs were known to cause increased injury risk when compared with NG. 35 Newer, third-generation AT is composed of longer fibers and a sand and/or rubber infill that more closely mimic the properties of NG. 48 Therefore, with these improvements in AT characteristics, injury risk on AT may be comparable with that on NG. Nevertheless, biomechanical studies have found increased frictional forces on AT that may lead to increased lower extremity injury, specifically to the anterior cruciate ligament (ACL). 10,12
Soccer players have been shown to overwhelmingly favor playing soccer on NG compared with AT. 34,38 Increased risk of ACL injury on AT surfaces is a concern cited frequently by players because of perceived higher surface stiffness and friction. 34 ACL injuries can be devastating for soccer players, as return to play requires lengthy and extensive rehabilitation and some athletes do not return to their previous level of competition. 2,3,6,45 While ACL injuries may occur via contact mechanisms, they are also commonly caused by noncontact cutting and pivoting mechanisms, extremely prevalent in soccer, and can be related to playing surface. 9
Despite these perceptions, limited studies have been conducted to specifically investigate the effects of playing surface on ACL injury risk in soccer players. The majority of studies on the topic of playing surface and injury risk have sought to characterize overall lower extremity injury risk or have combined multiple sports in their analyses rather than examining ACL injuries in soccer players specifically. 8,13,17,26,27 –29 Furthermore, few studies have examined the differences between ACL injury risk in male and female soccer athletes playing on AT versus NG. Given the higher risk for female ACL injury in sports, 36 and soccer in particular, 31,46 it is important to define whether AT may compound this injury risk.
The purpose of this investigation was to systematically review the literature for studies comparing ACL injury risk on AT versus NG in soccer and to specifically determine whether there were differences in injury risk in male versus female soccer players when considering the playing surface. We hypothesized that no difference in ACL injuries would be seen between playing on AT and NG and that male and female players would have similar risk of ACL injury despite the playing surface.
Methods
Literature Review and Search Strategy
This systematic review was performed according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines 30 and was registered with PROSPERO (CRD42021238137) on March 22, 2021. Two authors (M.X., J.L.L.) conducted separate searches of the following medical databases: PubMed, SCOPUS, and Cochrane Central Register of Controlled Trials. The searches were performed on August 12, 2021. The search string used was ((ACL OR anterior cruciate ligament) OR (injury)) AND (turf OR surface OR ((synthetic OR natural) AND grass)) AND (soccer OR football). Articles published between database inception and August 12, 2021, were included for screening.
Eligibility Criteria
Eligible studies were published in the English language, had an evidence level of 1 to 3 (per Oxford Centre for Evidence-Based Medicine), and compared the incidence of ACL injuries on AT versus NG in soccer players. Exclusion criteria included (1) animal studies, basic science studies, review articles, case reports, book chapters, and technique papers; (2) studies published before 2000; (3) studies that reported on lower extremity injury without specifying ACL injuries specifically; and (4) studies where an incidence rate ratio (IRR) was unable to be calculated. In the event of different studies with duplicate (or overlapping) patient populations, the study with the largest number of patients or greatest clarity of methods and results was included if the participants could not be separated. After removal of duplicates, titles and/or abstracts were screened, and full-text articles were further assessed based on inclusion and exclusion criteria by 2 independent reviewers (M.X., J.L.L.). All references were cross-referenced for inclusion if missed by the initial search. The search results were reviewed for duplicates and the inclusion criteria to determine the articles that were included in the final analysis.
Data Extraction
All study, participant, and ACL injury information were collected. Study and participant characteristics extracted included year of publication, journal, country where the study was conducted, years of included seasons, sex of included players, level of competition (youth, collegiate, or professional), exposure setting (games or practices), denominator for incidence (per game, per hour, or per athlete-exposure), and turf type. ACL injury information recorded included the total number of injuries, injuries on NG, injuries on AT, and total exposures. When feasible, these data were subgrouped by sex and exposure setting. Extracted data were cross-checked for accuracy by the 2 reviewers and recorded onto a shared spreadsheet (Microsoft Excel, Microsoft Corporation).
Quality Assessment
The risk of study bias and methodological quality was analyzed using the methodological index for non-randomized studies (MINORS) score, which has been shown to be a reliable and valid assessment of comparative and noncomparative outcome studies. 42 The maximum possible score is 24 points for comparative studies and 16 points for noncomparative studies, with maximum scores representing the highest methodological quality for nonrandomized studies and a low risk of bias. Two authors (M.X., J.L.L.) independently scored the studies. Disagreements were resolved between the 2 reviewers and confirmed by the senior author (G.D.A.).
Statistical Analysis
IRRs and their 95% CIs were calculated by comparing ACL injuries on AT versus NG, where IRRs <1 indicated a lower incidence of ACL injuries on AT compared with NG and IRRs >1 signified a higher incidence of ACL injuries on AT compared with NG. Mantel-Haenszel random-effects model was used for meta-analyses of IRRs using the metainc function from the metafor package, 44 and forest plots were generated for the pooled IRR for ACL injuries in game and training settings. In addition, subanalyses based on athlete sex were conducted for IRRs of ACL injuries in games. Heterogeneity was quantified using the I 2 statistic, which describes the proportion of total variation in study estimates that is due to heterogeneity, ranging from 0% to 100%. 22 A P value of <.05 was set as significant. R (Version 4.03; R Foundation for Statistical Computing) was used for all analyses.
Results
Characteristics of Included Studies
The initial search yielded 1010 articles. After removing duplicates, 644 records were screened for eligibility. Of these, 26 articles underwent full-text review, resulting in 7 articles that were included and analyzed (Figure 1). 5,8,19,23,26,28,29 Three articles were level 2 evidence, 19,28,29 and 4 articles were level 3 evidence. 5,8,23,26 The MINORS score ranged from 19 to 21 (fair quality), with a mean score of 20 ± 0.8. Soccer players from the United States comprised 4 studies, 8,23,28,29 and players from Europe (Sweden, Norway, and Italy) were represented in 3 studies. 5,19,26 There were 2 studies that investigated ACL injuries in a female-only cohort, 19,29 4 studies that included a male-only cohort, 5,8,26,28 and 1 study that included both male and female participants (Table 1). 23 Included seasons were between 2004 and 2016 and, in the 5 studies that specified turf type, 5,8,26,28,29 all athletes competed on third-generation turf. Levels of play included professional (n = 3 studies) 5,8,26 college (n = 3 studies), 23,28,29 and youth (n = 1 study). 19 Four articles reported ACL injury for only games played on AT and NG, 8,26,28,29 whereas 3 studies included data on both games and training on the 2 field types (Table 1). 5,19,23 The majority (97%) of ACL injuries included were from the study by Howard et al 23 (Table 2).
Figure 1.
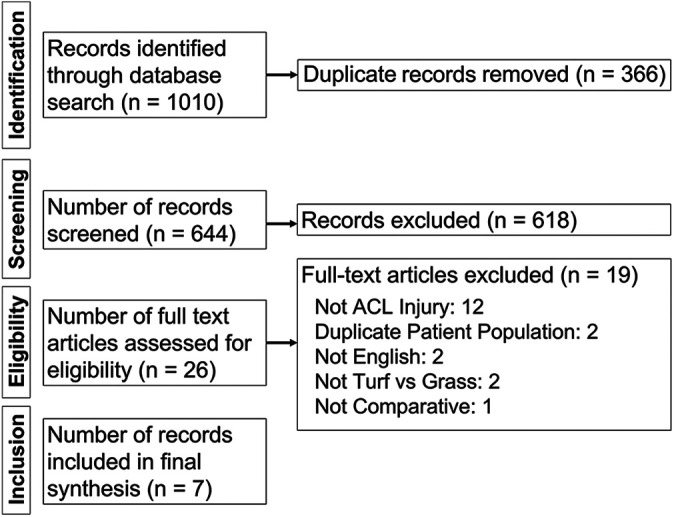
Flow diagram summarizing the literature search, screening, and review. ACL, anterior cruciate ligament.
Table 1.
Summary of Study Characteristics for Included Articles a
| Lead Author (Year) | Journal | LOE | MINORS Score | Country | Sex | Competition Level | Exposure Setting | Turf Type | Years Included |
|---|---|---|---|---|---|---|---|---|---|
| Bjørneboe (2010) 5 | BJSM | 3 | 21 | Norway | Male | Professional | Games and training | 3rd generation | 2004-2007 |
| Calloway (2019) 8 | AJSM | 3 | 20 | USA | Male | Professional | Games | 3rd generation | 2013-2016 |
| Hägglund (2016) 19 | KSSTA | 2 | 21 | Sweden | Female | Youth | Games and training | NS | 2009 |
| Howard (2020) 23 | OJSM | 3 | 20 | USA | Male and female | College | Games and training | NS | 2004-2014 |
| Lanzetti (2017) 26 | SJMSS | 3 | 19 | Italy | Male | Professional | Games | 3rd generation | 2011-2012 |
| Meyers (2013) 29 | AJSM | 2 | 21 | USA | Female | College | Games | 3rd generation | 2007-2011 |
| Meyers (2017) 28 | AJSM | 2 | 21 | USA | Male | College | Games | 3rd generation | 2007-2012 |
a AJSM, American Journal of Sports Medicine; BJSM, British Journal of Sports Medicine; KSSTA, Knee Surgery, Sports Traumatology, Arthroscopy; LOE, level of evidence; MINORS, methodological index for non-randomized studies; NS, not specified; OJSM, Orthopaedic Journal of Sports Medicine; SJMSS, Scandinavian Journal of Medicine and Science in Sports.
Table 2.
Summary of ACL Injury Collection and Information for Included Studies a
| Lead Author (Year) | Denominator for Exposure Incidence | No. of ACL Injuries | ACL Injury Incidence | |||
|---|---|---|---|---|---|---|
| Exposures on NG, % | On NG | On AT | On NG | On AT | ||
| Bjørneboe (2010) 5 | 71.47 | Hours | 11 | 3 | 0.075 per 1000 h | 0.04 per 1000 h |
| Calloway (2019) 8 | 75.95 | Games | 30 | 9 | 0.027 per game | 0.026 per game |
| Hägglund (2016) 19 | 85.74 | Hours | 19 | 2 | 0.084 per 1000 h | 0.084 per 1000 h |
| Howard (2020) 23 | 81.36 | AE b | 2947 | 502 | 1.16 per 10,000 AE | 0.92 per 10,000 AE |
| Lanzetti (2017) 26 | 50.78 | Hours | 1 | 0 | 0.76 per 1000 h | 0 per 1000 h |
| Meyers (2013) 29 | 55.46 | Games | 13 | 9 | 0.294 per 10 games | 0.254 per 10 games |
| Meyers (2017) 28 | 50.33 | Games | 2 | 1 | 0.052 per 10 games | 0.026 per 10 games |
a ACL, anterior cruciate ligament; AE, athlete-exposures; AT, artificial turf; NG, natural grass.
b AE was defined as 1 student-athlete participating in 1 National Collegiate Athletic Association–sanctioned practice or competition.
ACL Injuries on AT Versus NG
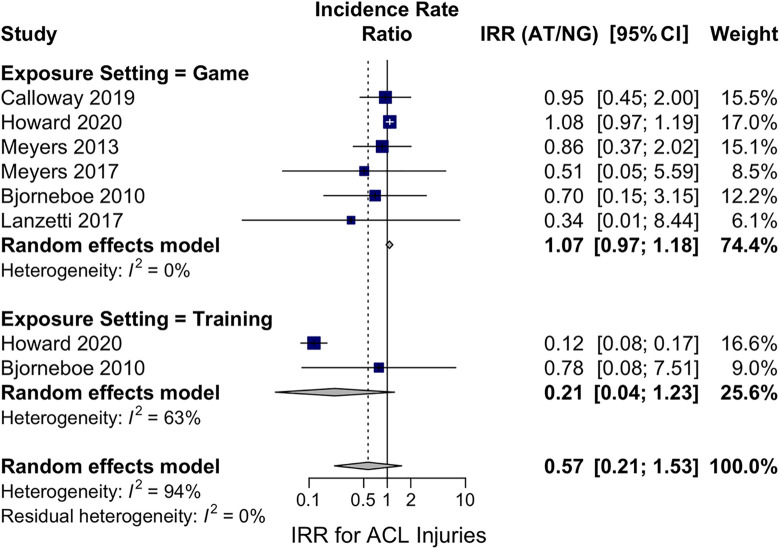
Pooling of ACL injury IRRs (incidence on AT divided by incidence on NG) demonstrated no significant differences in overall ACL injury risk when playing soccer on AT compared with playing on NG (IRR = 0.57 [95% CI, 0.21-1.53]; P = .31) (Figure 2).
Figure 2.
Forest plot of pooled IRRs for ACL injury on AT versus NG in soccer players with subanalysis by exposure setting (game vs training). ACL, anterior cruciate ligament; AT, artificial turf; IRR, incidence rate ratio; NG, natural grass.
ACL Injuries by Sex and Exposure Setting
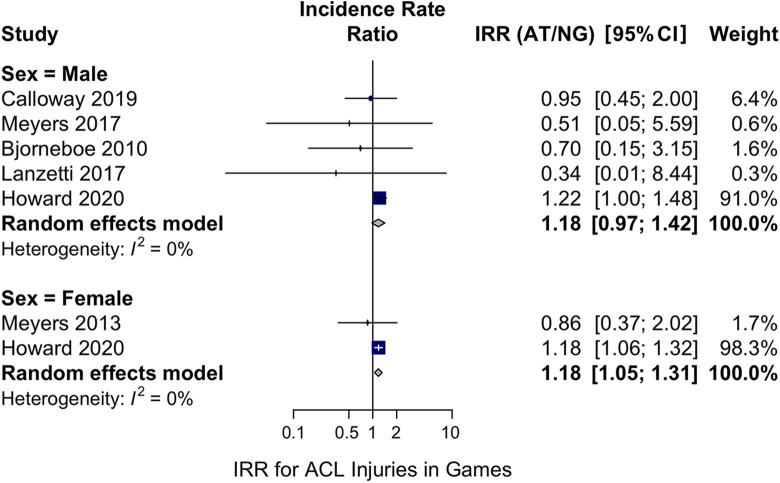
When stratifying game data by sex, we observed no significant differences in ACL injury risk on AT and NG for male players (IRR = 1.18 [95% CI, 0.97-1.42]; P = .09) but a significantly increased risk of ACL injury on AT compared with on NG for female players (IRR = 1.18 [95% CI, 1.05-1.31]; P = .004) (Figure 3).
Figure 3.
Forest plot of the subanalysis based on sex (male or female) of pooled IRRs for ACL injury in soccer games played on AT versus NG. ACL, anterior cruciate ligament; AT, artificial turf; IRR, incidence rate ratio; NG, natural grass.
In addition, subgroup analyses by exposure setting (game or practice) showed no significant differences in ACL injury risk during soccer games (IRR = 1.07 [95% CI, 0.97-1.18]; P = .20) and soccer practices (IRR = 0.21 [95% CI, 0.04-1.23]; P = .09) played on AT and NG (Figure 2).
Exposure Settings
There were variations in how studies documented soccer exposures for calculating the ACL injury incidences on AT and NG. Three studies reported exposures in the number of hours athletes trained or played in games, 5,19,26 resulting in an incidence of injuries per 1000 hours. Three studies tracked ACL injury incidences per team game, 8,28,29 and 1 study measured exposure via the number of athlete-exposures, 23 defined as 1 athlete participating in 1 National Collegiate Athletic Association (NCAA)–sanctioned practice or competition. A total of 3023 ACL injuries occurred on NG, and 526 ACL injuries happened on AT. The majority of soccer exposures in each study were on NG (range, 50.33%-85.74%) (Table 2).
Discussion
The present systematic review included 7 studies that compared ACL injury risk in soccer players on AT and NG. The studies varied with respect to the exposure setting (game or training), sex, competition level, and definition of measures of exposure, but all studies provided an incidence of ACL injury on AT and NG to allow for the calculation of an IRR as a measure of injury risk. There were no significant differences in the pooled ACL injury risk on AT compared with NG in soccer games and training and no significant differences in ACL injury risk for male athletes playing games on AT compared with NG. However, subgroup analysis showed that the incidence of ACL injuries for female players in soccer games on AT was 1.18 times higher than that on NG.
It is well known that risk factors for ACL injury are multifactorial. One of the biggest risk factors is female sex, as female soccer players are 2 to 9 times more likely to sustain an ACL injury compared with their male counterparts. 36,47 It has been shown that 18.3% of current collegiate and professional women’s soccer players have a history of at least 1 ACL injury. 50 Risk factors associated with ACL injury in female athletes include neuromuscular imbalances, 21 hormonal fluctuations, 11,20 narrower intercondylar notch width, 39,40,42 joint laxity, 32,43 workload, 51 and landing mechanics. 24,33 Our investigation demonstrated that playing soccer games on AT may be an additional risk factor for ACL injury specifically for female athletes. Previous studies have shown that differences in field and playing conditions, such as weather, field maintenance, cleat pattern, and season, may also affect injury rates. 1,4 Therefore, field conditions combined with intrinsic risk factors for female soccer players may cause an increased risk for ACL injury not seen in male athletes.
In all included studies, most of the soccer exposures were on NG, but, as AT is becoming more popular because of lower maintenance costs, higher field consistency, and the ability to be played on year-round, it is important to understand its effects on injury. 13,48 Although the Fédération Internationale de Football Association has approved certain third-generation AT fields for professional games, perceptions around playing soccer on AT are still controversial, especially at the professional level. Poulos et al 34 surveyed 99 Major League Soccer (MLS) athletes and found that 94% of players believed that AT surfaces were most likely to increase the risk of sustaining an injury because of higher surface stiffness and friction. Moreover, Roberts et al 38 found that the majority of professional soccer players in Europe prefer playing on NG over AT and perceived that they had a higher risk of sustaining an injury on AT. Despite these perceptions, our study demonstrated that playing games on AT is comparable with playing games on NG in terms of ACL injury risk for men but not for women.
A previous systematic review on the effects of playing surface on ACL injury in American football and soccer concluded that AT surfaces increased the rate of ACL injury in football but not in soccer. 4 In addition, a meta-analysis of all lower extremity injuries on AT versus NG in soccer found a pooled IRR of 0.86 (P < .05), suggesting that injury incidence may be lower on AT. 48 Our study incorporated more recent literature and focused specifically on ACL injuries in soccer players, as movement and fatigue patterns differ among sports. Further, our investigation included separate subgroup analyses on pooled ACL injury IRRs for sex (male or female) and exposure setting (training or games), which are variables that affect ACL injury risk. It has been shown that soccer players are significantly more likely to sustain an injury during games compared with in training. 14 –16,18,37,45 Waldén and colleagues 45 found that men’s professional soccer players in Europe had a 20-fold higher rate of ACL injury in games compared with in training and only 65% of players still played at the top level 3 years after injury. Although none of the included studies tracked the mechanism of injury, studies have demonstrated that both male and female soccer players are most at risk for ACL injury when defending. 7,9
The majority of studies included in the present review only reported on game injuries, and most had a primary aim of analyzing overall injury rates rather than ACL injuries specifically. In MLS players, Calloway et al 8 studied all in-game injuries and found that the overall rate of injury on AT was not inferior to that on NG, and the type of playing surface also did not influence ACL injury rates in their subgroup analysis. Further, Meyers 28,29 found a significantly lower total injury incidence rate for men’s and women’s collegiate soccer athletes playing on FieldTurf compared with NG, although no significant differences in ACL injury risk was seen between playing surfaces. The studies by Meyers 28,29 were funded by the FieldTurf company, and results may not be generalizable to other AT types.
The cohort from Howard et al 23 comprised the largest number of ACL injuries in the current investigation, as their primary aim was to compare ACL injuries on NG and AT in collegiate soccer using the NCAA Injury Surveillance System (ISS) database. The authors retrospectively reviewed 10 seasons of men’s and women’s collegiate soccer game and practice data. Interestingly, they found that practicing on NG was associated with a significantly higher risk of ACL injury compared with practicing on AT for both men (IRR = 3.03 NG/AT) and women (IRR = 11.13 NG/AT) whereas playing games on AT was associated with increased risk of ACL injury compared with games on NG for both sexes. The other study to include separate training data reported no significant differences in ACL injury rates between training on AT and NG. 5
Limitations
There were limitations to the current investigation, reflecting the underlying limitations of the included studies and available data. The studies differed in regard to exposure definition, which limited the ability to calculate a pooled incidence rate of ACL injuries on AT and NG separately. ACL injury rates were not able to be stratified by player position or level of play, and field conditions most likely differed among studies. Five studies conducted their studies on third-generation turf, whereas the other 2 studies did not include the turf type, which may have affected these results. In addition, the retrospective nature of some studies and the heterogeneity in level of play and sex may have affected pooled IRRs and resulted in a higher risk of bias. Two studies by Meyers 28,29 collected data prospectively from collegiate men’s and women’s soccer players, whereas Howard et al 23 used retrospective data from the NCAA ISS database to conduct their analyses. Therefore, it is unknown if there was overlap in data between these studies, as the NCAA ISS is based on a convenience sample and is not representative of all NCAA collegiate soccer programs in the United States. In addition, data are contributed voluntarily to the NCAA ISS. Thus, not all NCAA programs are represented, and not all injuries from a single institution are included. Further, due to its large sample size, the study data from Howard et al comprised the majority of ACL injuries included in this investigation, which may have biased results. Moreover, the primary aim of all but 1 of the included studies was to look at overall or lower extremity injury rates rather than focusing specifically on ACL injury. Therefore, the total number of ACL injuries was small in some of these studies, which may have resulted in individual studies being underpowered to detect differences in injury rates between cohorts.
Conclusion
This investigation found that female soccer players had a significantly higher risk of ACL injury when playing games on AT versus NG, whereas no significant difference was seen in their male counterparts. No differences were found for the combined male/female population or soccer games or training sessions played on AT compared with NG. Because ACL injury risk is multifactorial, future studies on the sex-specific differences in playing surface on injury risk are warranted.
Footnotes
Final revision submitted April 1, 2022; accepted May 12, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.L.S. has received research support from Arthrex and DJO; education payments from Elite Orthopedics and Evolution Surgical; consulting fees from Arthrex, Bioventus, Ceterix, ConMed Linvatec, Flexion Therapeutics, GLG Consulting, JRF Ortho, Moximed, Olympus America, Smith & Nephew, and Vericel; speaking fees from Arthrex, Smith & Nephew, and Vericel; and honoraria from Flexion Therapeutics and Vericel. M.R.S. has received research support from Smith & Nephew; consulting fees from Anika Therapeutics, Medacta, and Smith & Nephew; speaking fees from Medacta and Smith & Nephew; royalties from DJO, Saunders/Mosby-Elsevier, Smith & Nephew, Stryker, and Wolters Kluwer Health-Lippincott Williams & Wilkins; honoraria from Medacta; and stock/stock options from Biomimedica. G.D.A. has received education payments from Evolution Surgical; consulting fees from Cytonics, Fidia Pharma, RubiconMD, and Sideline Sports Doc; nonconsulting fees from Arthrex and Stryker; royalties from Orthofix; and stock/stock options from Cytonics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players, part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):705–729. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 4. Balazs GC, Pavey GJ, Brelin AM, Pickett A, Keblish DJ, Rue J-PH. Risk of anterior cruciate ligament injury in athletes on synthetic playing surfaces. Am J Sports Med. 2015;43(7):1798–1804. [DOI] [PubMed] [Google Scholar]
- 5. Bjørneboe J, Bahr R, Andersen TE. Risk of injury on third-generation artificial turf in Norwegian professional football. Br J Sports Med. 2010;44(11):794–798. [DOI] [PubMed] [Google Scholar]
- 6. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brophy RH, Stepan JG, Silvers HJ, Mandelbaum BR. Defending puts the anterior cruciate ligament at risk during soccer. Sports Health. 2015;7(3):244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Calloway SP, Hardin DM, Crawford MD, et al. Injury surveillance in major league soccer: a 4-year comparison of injury on natural grass versus artificial turf field. Am J Sports Med. 2019;47(10):2279–2286. [DOI] [PubMed] [Google Scholar]
- 9. Della Villa F, Buckthorpe M, Grassi A, et al. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br J Sports Med. 2020;54(23):1423–1432. [DOI] [PubMed] [Google Scholar]
- 10. Dowling AV, Corazza S, Chaudhari AM, Andriacchi TP. Shoe-surface friction influences movement strategies during a sidestep cutting task: implications for anterior cruciate ligament injury risk. Am J Sports Med. 2010;38(3):478–485. [DOI] [PubMed] [Google Scholar]
- 11. Dragoo JL, Castillo TN, Braun HJ, Ridley BA, Kennedy AC, Golish SR. Prospective correlation between serum relaxin concentration and anterior cruciate ligament tears among elite collegiate female athletes. Am J Sports Med. 2011;39(10):2175–2180. [DOI] [PubMed] [Google Scholar]
- 12. Drakos MC, Hillstrom H, Voos JE, et al. The effect of the shoe-surface interface in the development of anterior cruciate ligament strain. J Biomech Eng. 2010;132(1):011003. [DOI] [PubMed] [Google Scholar]
- 13. Ekstrand J, Hägglund M, Fuller CW. Comparison of injuries sustained on artificial turf and grass by male and female elite football players. Scand J Med Sci Sports. 2011;21(6):824–832. [DOI] [PubMed] [Google Scholar]
- 14. Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553–558. [DOI] [PubMed] [Google Scholar]
- 15. Engström B, Johansson C, Tornkvist H. Soccer injuries among elite female players. Am J Sports Med. 1991;19(4):372–375. [DOI] [PubMed] [Google Scholar]
- 16. Faude O, Junge A, Kindermann W, Dvorak J. Injuries in female soccer players. Am J Sports Med. 2005;33(11):1694–1700. [DOI] [PubMed] [Google Scholar]
- 17. Fuller CW, Dick RW, Corlette J, Schmalz R. Comparison of the incidence, nature and cause of injuries sustained on grass and new generation artificial turf by male and female football players, part 1: match injuries. Br J Sports Med. 2007;41(suppl 1):i20–i26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Giza E, Mithöfer K, Farrell L, Zarins B, Gill T. Injuries in women’s professional soccer. Br J Sports Med. 2005;39(4):212–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hägglund M, Waldén M. Risk factors for acute knee injury in female youth football. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):737–746. [DOI] [PubMed] [Google Scholar]
- 20. Herzberg SD, Motu’apuaka ML, Lambert W, Fu R, Brady J, Guise JM. The effect of menstrual cycle and contraceptives on ACL injuries and laxity: a systematic review and meta-analysis. Orthop J Sports Med. 2017;5(7):2325967117718781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hewett TE, Ford KR, Hoogenboom BJ, Myer GD. Understanding and preventing ACL injuries: current biomechanical and epidemiologic considerations–-update 2010. N Am J Sports Phys Ther. 2010;5(4):234–251. [PMC free article] [PubMed] [Google Scholar]
- 22. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 23. Howard M, Solaru S, Kang HP, et al. Epidemiology of anterior cruciate ligament injury on natural grass versus artificial turf in soccer: 10-year data from the National Collegiate Athletic Association Injury Surveillance System. Orthop J Sports Med. 2020;8(7):2325967120934434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kernozek TW, Torry MR, Iwasaki M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am J Sports Med. 2008;36(3):554–565. [DOI] [PubMed] [Google Scholar]
- 25. Kunz M. Big count: 265 million playing football. FIFA Magazine. 2007:10–15. [Google Scholar]
- 26. Lanzetti RM, Ciompi A, Lupariello D, Guzzini M, De Carli A, Ferretti A. Safety of third-generation artificial turf in male elite professional soccer players in Italian major league. Scand J Med Sci Sports. 2017;27(4):435–439. [DOI] [PubMed] [Google Scholar]
- 27. Lucarno S, Zago M, Buckthorpe M, et al. Systematic video analysis of anterior cruciate ligament injuries in professional female soccer players. Am J Sports Med. 2021;49(7):1794–1802. [DOI] [PubMed] [Google Scholar]
- 28. Mack CD, Hershman EB, Anderson RB, et al. Higher rates of lower extremity injury on synthetic turf compared with natural turf among National Football League athletes: epidemiologic confirmation of a biomechanical hypothesis. Am J Sports Med. 2019;47(1):189–196. [DOI] [PubMed] [Google Scholar]
- 29. Meyers MC. Incidence, mechanisms, and severity of match-related collegiate men’s soccer injuries on FieldTurf and natural grass surfaces: a 6-year prospective study. Am J Sports Med. 2017;45(3):708–718. [DOI] [PubMed] [Google Scholar]
- 30. Meyers MC. Incidence, mechanisms, and severity of match-related collegiate women’s soccer injuries on FieldTurf and natural grass surfaces: a 5-year prospective study. Am J Sports Med. 2013;41(10):2409–2420. [DOI] [PubMed] [Google Scholar]
- 31. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. BMJ. 2009;339:B2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Montalvo AM, Schneider DK, Yut L, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sports Med. 2019;53(16):1003–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36(6):1073–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Peebles AT, Dickerson LC, Renner KE, Queen RM. Sex-based differences in landing mechanics vary between the drop vertical jump and stop jump. J Biomech. 2020;105:109818. [DOI] [PubMed] [Google Scholar]
- 35. Poulos CC, Gallucci J, Gage WH, Baker J, Buitrago S, Macpherson AK. The perceptions of professional soccer players on the risk of injury from competition and training on natural grass and 3rd generation artificial turf. BMC Sports Sci Med Rehabil. 2014;6(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Powell JW, Schootman M. A multivariate risk analysis of selected playing surfaces in the National Football League: 1980 to 1989. An epidemiologic study of knee injuries. Am J Sports Med. 1992;20(6):686–694. [DOI] [PubMed] [Google Scholar]
- 37. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320–1325.e1326. [DOI] [PubMed] [Google Scholar]
- 38. Rekik RN, Tabben M, Eirale C, et al. ACL injury incidence, severity and patterns in professional male soccer players in a Middle Eastern league. BMJ Open Sport Exerc Med. 2018;4(1):e000461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Roberts JR, Osei-Owusu P, Mears AC, Harland AR. Elite players’ perceptions of football playing surfaces: a qualitative study. Res Q Exerc Sport. 2020;91(2):239–251. [DOI] [PubMed] [Google Scholar]
- 40. Shelbourne KD, Facibene WA, Hunt JJ. Radiographic and intraoperative intercondylar notch width measurements in men and women with unilateral and bilateral anterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):229–233. [DOI] [PubMed] [Google Scholar]
- 41. Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 43. Souryal TO, Freeman TR. Intercondylar notch size and anterior cruciate ligament injuries in athletes: a prospective study. Am J Sports Med. 1993;21(4):535–539. [DOI] [PubMed] [Google Scholar]
- 44. Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31(6):831–842. [DOI] [PubMed] [Google Scholar]
- 45. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Soft. 2010;36:1–48. [Google Scholar]
- 46. Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50(12):744–750. [DOI] [PubMed] [Google Scholar]
- 47. Waldén M, Hägglund M, Werner J, Ekstrand J. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc. 2011;19(1):3–10. [DOI] [PubMed] [Google Scholar]
- 48. Williams JH, Akogyrem E, Williams JR. A meta-analysis of soccer injuries on artificial turf and natural grass. Sports Med. 2013;2013:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Williams S, Hume PA, Kara S. A review of football injuries on third and fourth generation artificial turfs compared with natural turf. Sports Med. 2011;41(11):903–923. [DOI] [PubMed] [Google Scholar]
- 50. Xiao M, Lemos JL, Hwang CE, Sherman SL, Safran MR, Abrams GD. High specialization among female youth soccer players is associated with an increased likelihood of serious injury. Med Sci Sports Exerc. 2021;53(10):2086–2092. [DOI] [PubMed] [Google Scholar]
- 51. Xiao M, Nguyen JN, Hwang CE, Abrams GD. Increased Lower Extremity Injury Risk Associated With Player Load and Distance in Collegiate Women's Soccer. Orthop J Sports Med. 2021;9(10):23259671211048248. [DOI] [PMC free article] [PubMed] [Google Scholar]