Abstract
Background:
High cost of eight-plate makes it unavailable in many countries; therefore, developing an alternative device for temporary hemiepiphysiodesis of knee deformities in pediatrics is valuable. In this study, we compared the outcome of the eight-plate with the reconstruction-plate in this setting.
Methods:
In this retrospective study, 109 skeletally immature patients (212 physes) who underwent temporary hemiepiphysiodesis to correct idiopathic genu valgum were included. The eight-plate and reconstruction-plate were used in 47 patients (90 physes) and 62 patients (122 physes), respectively. Outcome measures were the valgus angle, medial proximal tibial angle (MPTA), the lateral distal femoral angle (LDFA), the joint-line convergence angle (JLCA), and lower limb mechanical axis (LLMA).
Results:
The baseline characteristics of the patients were comparable between the two plate groups. The mean follow-up of the patients was 32.9 ± 15.1 months. The mean MPTA change was 2.7 ± 3.7º in the eight-plate group and 2.1 ± 3.4º in the reconstruction-plate group (P=0.2). The mean LDFA improvement was 8 ± 3.7º in the eight-plate group and 7.9 ± 3.5º in the reconstruction-plate group (P=0.61). The mean valgus correction was 10.7 ± 4.4º in the eight-plate group and 10.4 ± 4.6º in the reconstruction-plate group (P=0.74). Moreover, the mean change of JLCA was 0.7 ± 1.3º in the eight-plate group and 0.8 ± 1.3º in the reconstruction-plate group (P=0.58). The postoperative LLMA was comparable between the two study groups as well. In total, five postoperative complications were recorded in this series, which included one case of screw loosening in each group, two cases of overcorrection, and one screw breakage in the reconstruction-plate group.
Conclusion:
The radiologic results and complications of the reconstruction-plate are comparable with the eight-plate. Therefore, it can be safely and efficiently used in hemiepiphysiodesis to correct idiopathic genu valgum.
Key Words: Eight-plate, Hemiepiphysiodesis, Idiopathic genu valgum, Reconstruction-plate, Pediatrics
Introduction
Idiopathic genu valgum is a frequent deformity of the knee in adolescence that generally occurs between 2 to 11 years of age (1). The true incidence of this deformity is not apparent. However, its association with obesity has been demonstrated in several studies, and the rate of obesity is significantly higher in genu valgum patients (2, 3). Along with the industrialization of societies, the rate of obesity also continuously increases, therefore, increasing the risk of idiopathic genu valgum and its consequences, such as osteoarthritis in adulthood (4). As a result, optimizing the available therapeutic approach for the patients and the healthcare system is critical.
While the idiopathic genu valgum in adolescence usually resolves spontaneously or through conservative treatment, surgical intervention might be required in some patients (5). Temporary hemiepiphysiodesis is a widely accepted method and a valuable alternative to realignment osteotomy in adolescent genu valgum (6), which could be performed with several devices, including screws, staples, and wires (7-9). However, the high complication rates of these devices (7-10) led to the development of the eight-plate by Stevens in 2007, which is based on the tension band principle instead of physeal compression. (11). Subsequent studies revealed promising results, a lower rate of rebound, and fewer postoperative complications using eight-plate for temporary hemiepiphysiodesis of the idiopathic genu valgum (12, 13).
While eight-plate is accepted as a safe and effective device for temporary hemiepiphysiodes is of the idiopathic genu valgum, its high failure rate in obese patients has been reported (14). In addition, it is an expensive device in many countries, including Iran (almost $250). With the growing number of genu valgum patients triggered by the increased rate of obesity, less expensive devices are essential to reduce the economic burden on the patients and healthcare systems, particularly in developing countries (15).
Preliminary evidence shows that temporary hemiepiphysiodesis with reconstruction-plate could provide similar results to eight-plate, with significantly lower expenses (almost $6 in Iran) (15, 16). This study aimed to compare the outcome of eight-plate hemiepiphysiodesis with reconstruction-plate hemiepi-physiodesis to find if they could be implemented interchangeably.
Materials and Methods
The review board of our institute approved this retrospective study under the code of IR.IUMS.FMD.REC.1398.521. Between 2009 and 2018, patients with idiopathic genu valgum who underwent temporary hemiepiphysiodesis using either an eight-plate or a reconstruction-plate were evaluated for the inclusion and exclusion criteria. Indications for surgery were the clinical appearance of the knees, gating impairment, genu valgum deformity of ≥ 6º, or lower but progressive valgus angles. Inclusion criteria were genu valgum deformity nonresponsive to conservative treatment, age of ≤ 16 years for males, and ≤ 15 years for females. Conservative treatment mainly included using a knee brace for patients under the age of six years and administering NSAIDs for pain relief, if needed. Patients with a history of surgery to correct genu valgum and patients with metabolic bone disorders were excluded from the study. Patients who lost follow-ups were excluded from the study, as well. Finally, 109 patients (212 knees) were included in the study. Hemiepiphysiodesis was performed bilaterally in 103 patients and unilaterally in six patients. The study population included 51 (46.8%) males and 58 (53.2%) females with a mean age of 11.9 ± 5 years (range 9-16). The patients’ mean body mass index (BMI) was 22.4 ± 1.8 kg/m2 (range 19-26.5). The mean follow-up of the patients was 32.9 ± 15.1 months (range 7-74). The mean time interval for plate removal was 11.3±3 months (range 5-18). Indications for plate removal were some degree of overcorrection in patients with more than two years to skeletal maturity (to reduce the risk of recurrence) and achieving a neutral mechanical axis in patients with less than two years to skeletal maturity. The degree of genu valgum did not change from plate removal to the final follow-up. No premature physeal plate closure was recorded.
Surgical Technique
Under general anesthesia, the patient was placed on a radiolucent operating table. After prepping and draping, the patient received intravenous antibiotics, and the tourniquet was inflamed. First, the medial epicondyle was identified, and through a small incision, one 1.5 mm smooth guide pin was placed on the medial cortex of the distal femur. The distance between the pin insertion site and distal femur physis was checked to avoid Physeal injury. Then, either an eight-plate (Marquardt, Germany; Figure 1) or a 3.5-mm reconstruction-plate (Mork-Med, Germany; Figure 2) was placed at the location indicated by the guide pin with a minimally invasive method without damaging the periosteum and perichondrial ring. The screws were inserted under the fluoroscopic guide. In patients of higher age, the screws were placed divergently to achieve faster correction and prevent the screw divergence with bone growth. The screws were placed parallel to the growth plate in younger patients because they will be corrected during the growth. We used three-hole reconstruction-plates. The length of the selected screw was generally one-third of the width of the bone. Following the screw insertions, the physis was re-checked under fluoroscopy. After irrigation and closure of the incision site, the wound was dressed. The patients were discharged one day after the surgery and returned to normal activities without restrictions, showing no sign of pain.
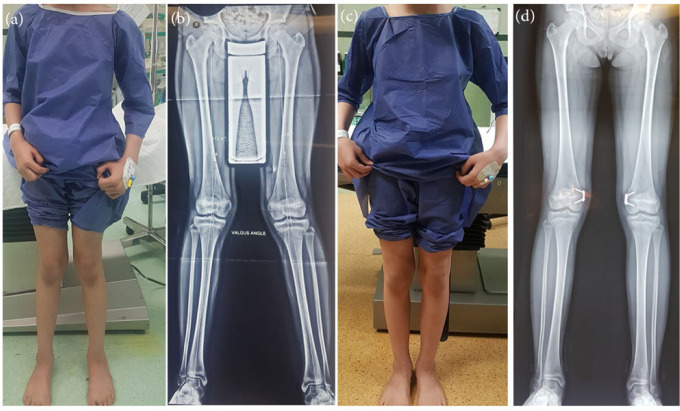
Figure 1.
Preoperative photograph (a) and anteroposterior radiograph (b) of an 11-year old girl with idiopathic genu valgum; Postoperative photograph (c) and radio graph (d) of the same patients after correction of deformity by medial temporary hemiepiphysiodesis using an eight-plate
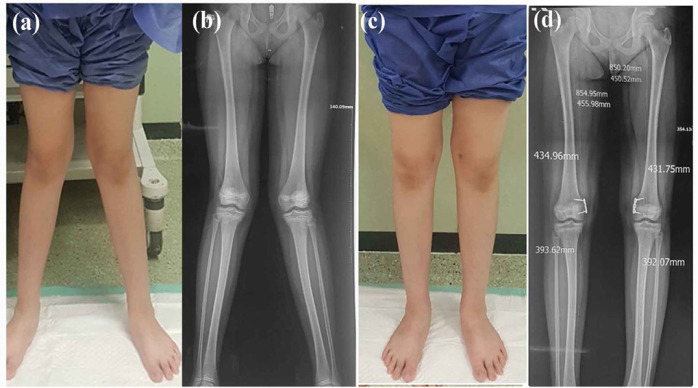
Figure 2.
Preoperative photograph (a) and anteroposterior radiograph (b) of a 10-year old girl with idiopathic genu valgum; Postoperative photograph (c) and radiograph (d) of the same patient after correction of deformity by medial temporary hemiepiphysiodesis using reconstruction plate
The first follow-up of patients was two weeks after the surgery. The subsequent follow-ups were every two months, and radiographic evaluations were performed every two months after the surgery. Furthermore, hardware was removed before skeletal maturity.
Outcome measures
The outcome of hemiepiphysiodesis was evaluated using radiographic measures, including the medial proximal tibial angle (MPTA), the lateral distal femoral angle (LDFA), the joint-line convergence angle (JLCA), and the valgus angle [Figure 3].
Figure 3.
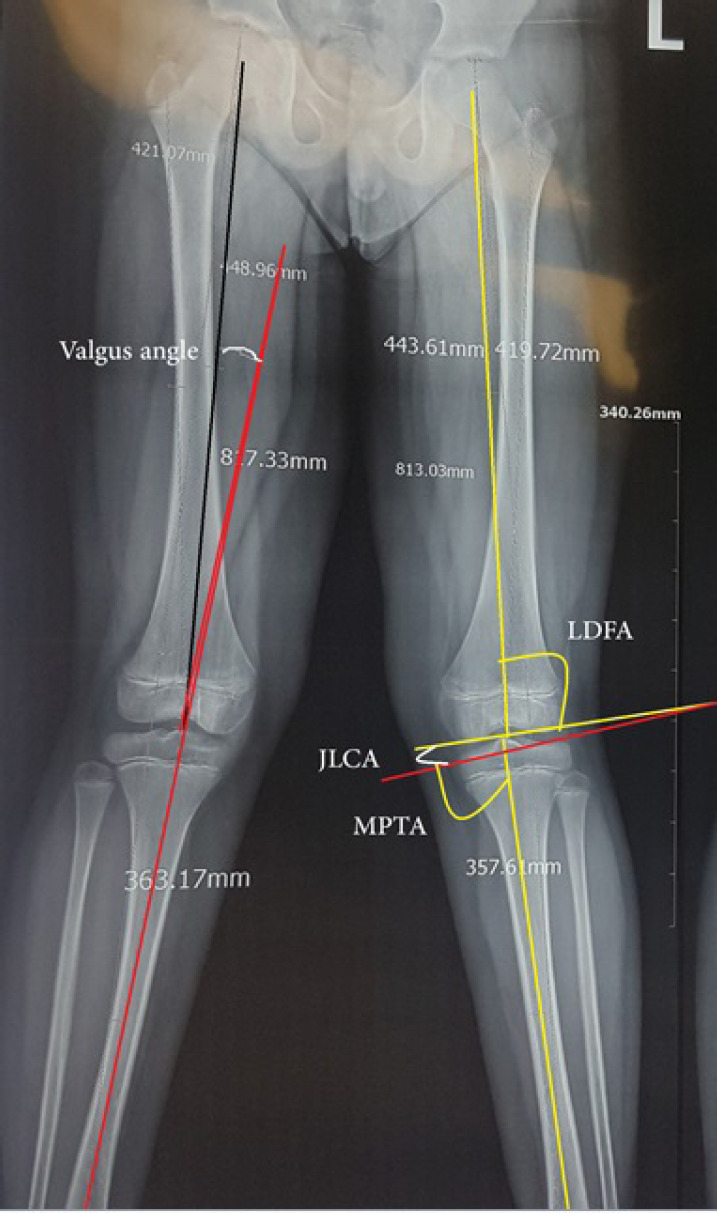
Calculation of MPTA, LDFA, JLCA, and valgus angle on standing radiographs
The lower limb mechanical axis (LLMA) was also assessed. For this purpose, a line was drawn from the femoral head’s center to the talus bone’s center. If the line crossed the middle of the tibial eminence, it was considered a neutral axis. If the line intersected the medial plateau LLMA was presented in three categories according to its distance from the center of the medial plateau: M1 (between the tibial eminence and middle point of the medial plateau), M2 (between the middle point of the medial plateau and the articular surface of the medial plateau), and M3 (the line protrudes the edge of the tibial bone, so that the axis line locates outside or more medial to the medial edge of the medial plateau). The LLMA was also presented in three categories (L1, L2, and L3) using the same categorization pattern if the line was located between the tibial eminence and lateral plateau.
Statistical analysis
Statistical evaluations were performed using SPSS software (version 16) for Windows, (SPSS Inc., Chicago, Ill., USA). Descriptive statistics were provided by mean ± standard deviation for numeric variables and number and percentage for categorical variables. The normal distribution of data was checked with the Kolmogorov-Smirnov test. Comparison of before-after radiographic measures was performed using a paired t-test or its nonparametric counterpart (Wilcoxon signed-rank test). The mean improvement of radiographic measures was compared between the two study groups using either an independent t-test or its nonparametric counterpart (Mann–Whitney U test). A P-values of less than 0.05 was considered statistically significant.
Results
Hemiepiphysiodesis was performed using eight-plate in 47 patients (90 physes) and using reconstruction-plate in 62 patients (122 physes). The mean age of the patients was 11.8 ± 1.3 years in the eight-plate group and 12 ± 1.6 years in the reconstruction-plate group (P=0.68). The mean follow-up of the patients was 31.3 ± 12.1 months in the eight-plate group and 34.2 ± 17 months in the reconstruction-plate group (P=0.31). The mean BMI of the patients was 22.7 ± 1.9 kg/m2 in the eight-plate and 22.2 ± 1.7 kg/m2 in the reconstruction-plate group (P=0.08). The sex distribution was not significantly different between the two study groups (61.1% vs. 46.7% female, P=0.18; Table 1).
Table 1.
The demographic characteristics of the patients of the two study groups
| Variable | Eight-plate (n=90 physes) | Reconstruction-plate (n=122 physes) | P value |
|---|---|---|---|
| Age (year) | 11.8±1.3 | 12±1.6 | 0.68 |
| Sex Male Female |
35 (38.9) 55 (61.1) |
65 (53.3) 57 (46.7) |
0.18 |
| Body mass index (kg/m2) | 22.7±1.9 | 22.2±1.7 | 0.08 |
| Follow-up (month) | 31.3±12.1 | 34.2±17 | 0.31 |
Data are presented as mean ± standard deviation or number (%)
The mean MPTA, LDFA, and varus angle were significantly corrected after the operation (P<0.001 for all) in the eight-plate group. The mean JLCA was not significantly changed after the surgery (P=0.52). Before the hemiepiphysiodesis, the LLMA was L1 in 50 (55.5%) physes, L2 in 35 (38.9%) physes, and L3 in 5 (5.6%) physes. After the surgery, the LLMA was neutral in 17 (18.9%) physes, M1 in 51 (56.7%) physes, M2 in 19 (21.1%) physes, and M3 in 3 (3.3%) physes [Table 2].
Table 2.
Comparison of preoperative and postoperative measures in patients undergoing hemiepiphysiodesis using eight-plate
| Variable | Preoperative (n=90 physes) | Postoperative (n=90 physes) | P-value |
|---|---|---|---|
| MPTA (º) | 91.1±1.9 | 88.4±2.9 | <0.001 |
| LDFA (º) | 84.2±2.5 | 92.3±2.9 | <0.001 |
| JLCA (º) | 0.17±1.2 | 0.27±1 | 0.52 |
| Valgus angle (º)* | -6.7±2.7 | +4.3±3.3 | <0.001 |
| LLMA | L1 (n=50) L2 (n=35) L3 (n=5) |
Neutral (n=17) M1 (n=51) M2 (n=19) M3 (n=3) |
<0.001 |
MPTA: Medial proximal tibial angle; LDFA: lateral distal femoral angle; JLCA: Joint line congruency angle; LLMA: Lower limb mechanical axis. A P<0.05 is considered statistically significant.
*A “-” means a valgus angle, and a “+” means a varus angle.
In the reconstruction-plate group, the mean MPTA, LDFA, and varus angle were significantly improved after the operation (P<0.001 for all). The mean change of JLCA was not significant after the surgery (P=0.33). Before the hemiepiphysiodesis, the LLMA was L1 in 75 (61.5%) physes, L2 in 32 (26.2%) physes, and L3 in 15 (12.3%) physes. After the surgery, the LLMA was neutral in 34 (27.9%) physes, M1 in 62 (50.8%) physes, M2 in 23 (18.9%) physes, and M3 in 3 (2.5%) physes [Table 3].
Table 3.
Comparison of preoperative and postoperative measures in patients undergoing hemiepiphysiodesis using reconstruction-plate
| Variable |
Preoperative
(n=122 physes) |
Postoperative
(n=122 physes) |
P-value |
|---|---|---|---|
| MPTA (º) | 90.4±3.2 | 88.3±3 | <0.001 |
| LDFA (º) | 83.4±2.7 | 91.2±3.1 | <0.001 |
| JLCA (º) | 0.09±1.4 | 0.23±1.3 | 0.33 |
| Valgus angle (º)* | -7±3.7 | +3.4±3.3 | <0.001 |
| LLMA | L1 (n=75) L2 (n=32) L3 (n=15) |
Neutral (n=37) M1 (n=62) M2 (n=23) |
<0.001 |
MPTA: Medial proximal tibial angle; LDFA: Lateral distal femoral angle; JLCA: Joint line congruency angle; LLMA: Lower limb mechanical axis. A P<0.05 is considered statistically significant.
*A “-” means a valgus angle, and a “+” means a varus angle.
The mean improvement of MPTA was 2.7 ± 3.7º in the eight-plate group and 2.1 ± 3.4º in the reconstruction-plate group (P=0.2). The mean improvement of LDFA was 8 ± 3.7º in the eight-plate group and 7.9 ± 3.5º in the reconstruction-plate group (P=0.61). The mean valgus correction was 10.7 ± 4.4º in the eight-plate group and 10.4 ± 4.6º in the reconstruction-plate group (P=0.74). In this respect, the knee angulation was changed from a valgus degree of 6.7 ± 2.7º to a varus degree of 4.3 ± 3.3º in the eight-plate group and from a valgus degree of 7 ± 3.7º to a varus degree of 3.4 ± 3.3º in the reconstruction-plate group.The mean change of JLCA was 0.7 ± 1.3º in the eight-plate group and 0.8 ± 1.3º in the reconstruction-plate group (P=0.58). The preoperative and postoperative LLMA was comparable between the two study groups [Table 4].
Table 4.
Comparison of change of outcome measures between patients undergoing hemiepiphysiodesis using eight-plate and reconstruction-plate
| Variable | Eight-plate (n=90 physes) | Reconstruction-plate (n=122 physes) | P-value |
|---|---|---|---|
| MPTA (º) | 2.7±3.7 | 2.1±3.4 | 0.2 |
| LDFA (º) | 8±3.7 | 7.9±3.5 | 0.61 |
| JLCA (º) | 0.7±1.3 | 0.8±1.3 | 0.58 |
| Valgus angle (º) | 10.7±4.4 | 10.4±4.6 | 0.74 |
| Preoperative LLMA L1 L2 L3 |
50 (55.5) 35 (38.9) 5 (5.6) |
75 (61.5) 32 (26.2) 15 (12.3) |
0.63 |
| Postoperative LLMA Neutral M1 M2 M3 |
17 (18.9) 51 (56.7) 19 (21.1) 3 (3.3) |
34 (27.9) 62 (50.8) 23 (18.9) 3 (2.5) |
0.5.6 |
MPTA: Medial proximal tibial angle; LDFA: Lateral distal femoral angle; JLCA: Joint line congruency angle; LLMA: Lower limb mechanical axis. A P<0.05 is considered statistically significant. Data is presented by mean ± standard deviation or number (%).
In total, five postoperative complications were recorded in this series, which included one case of screw loosening in each group, two cases of overcorrection, and one screw breakage in the reconstruction-plate group. Patients with screw loosening underwent revision surgery, and the screw was changed. Patients with overcorrection were monitored, and no rebound was observed; therefore, no intervention was required. No intervention was performed for the patients with screw breakage.
Discussion
This study compared the radiologic outcomes and complications of eight-plate with reconstruction-plate in temporary hemiepiphysiodesis performed to correct idiopathic genu valgum. Based on the findings of the current study, the radiologic outcomes and complications of the two plates were not statistically different. In addition, the obtained correction of valgus angle was not significantly different when the eight-plate or the reconstruction-plate was used.
Favorable results of Eight-plate for temporary hemiepiphysiodesis of genu valgum patients have been reported in some studies (12, 13). Sawiris et al. performed a systematic review and meta-analysis to investigate guided growth to correct coronal knee deformity in skeletally immature patients. According to their study, the success rate of eight-plate in correcting angular knee deformities was almost 85%. The rate of inadequate correction, rebound, implant breakage, and implant migration by eight-plate was 3%, 4%, 4%, and 2%, respectively. In addition, they suggested an eight-plate as a safe and efficient device for coronal knee deformity-guided correction (17). According to the study of Jelinek et al., the operating time for implantation and explantation was shorter with eight-plate compared to Blount stapling for correction of genu varum and valgum deformity in skeletally immature patients (18). Despite these advantages, more recent studies have reported a high failure rate of eight-plate, particularly in overweight patients and patients with Blount disease (14, 19). Based on a study carried out by Burghardt et al., eight-plate failure was generally observed in overweight patients with a mean BMI of 37.8 kg/m2. The BMI of patients who experienced an eight-plate failure in the study of Schroerlucke et al. was >30 kg/m2. In addition, the high cost of eight-plate makes it unavailable in many countries (15). Therefore, a more secure and affordable device for hemiepiphysiodesis of genu valgum patients is demanding.
Reconstruction-plate has been suggested as an alternative for eight-plate in some studies. Aslani et al. used 3.5mm reconstruction-plates for tension-band temporary hemiepiphysiodesis of angular knee deformity in 21 patients (42 knees). The mean follow-up of the patients after plate removal was 17 months. Complete correction of deformity was observed in 86% of patients. Screw breakage was seen in 10% of cases and was more frequent in the genu varum group (40% vs. 6.3%). They concluded that a 3.5mm reconstruction-plate provides a safe and efficient hemiepiphysiodesis, with a lower cost than eight-plate (15). Ghaffari and Mohammad Amini successfully used a 3.5 mm reconstruction-plate for the temporary hemiepiphysiodesis of genu valgum in two twin sisters associated with no postoperative complications (20).
Comparison of eight-plate with reconstruction-plate in guided growth has only been performed in one earlier study. In this comparative study, park et al. compared the outcome of eight-plate (31 physes, 20 patients) with reconstruction-plate (61 physes, 35 patients) in correcting knee deformities with different etiologies. The angular correction was achieved in all patients of the eight-plate and reconstruction-plate at a mean period of 13.7 months and 19.7 months, respectively. The mean correction of MPTA, LDFA, and angular deformity were comparable between the two plates. The rate of complications was also similar between the two plates (16). Similarly, the correction of MPTA, LDFA, varus angle, and LLMA was comparable between the eight-plate and reconstruction-plate groups of the present study. The rate of postoperative complications was not different, as well.
In total, the results of this study revealed that eight-plate and reconstruction-plate could be used interchangeably for temporary hemiepiphysiodesis of genu valgum, at least in non-obese patients. The present study was not without limitations. The main limitation of the study was its retrospective design. In addition, the clinical outcomes of the patients were not evaluated in this study. Furthermore, we did not compare the results of the eight-plate and reconstruction-plate in obese patients, which could be of more interest in future investigations.
Both eight-plate and reconstruction-plate are safe and efficient devices for temporary hemiepiphysiodesis of idiopathic genu valgum in skeletally immature patients. They can be used interchangeably, particularly in countries where eight-plate is not easily accessible due to its high cost.
Patient consent:
Informed consent was obtained from the patients’ parents to use their medical data for publication.
Disclosure:
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Westhoff B, Jäger M, Krauspe R. Axes of the legs in childhood What is pathologic? Der Orthopade. 2007;36(5):485–98. doi: 10.1007/s00132-007-1088-1. [DOI] [PubMed] [Google Scholar]
- 2.Soheilipour F, Pazouki A, Mazaherinezhad A, Yagoubzadeh K, Dadgostar H, Rouhani F. The prevalence of genu varum and genu valgum in overweight and obese patients: assessing the relationship between body mass index and knee angular deformities. Acta Bio Medica: Atenei Parmensis. 2020;91:4. doi: 10.23750/abm.v91i4.9077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shapouri J, Aghaali M, Aghaei M, Iranikhah A, Ahmadi R, Hovsepian S. Prevalence of lower extremities’ postural deformities in overweight and normal weight school children. Iranian Journal of Pediatrics. 2019;29:5. [Google Scholar]
- 4.Walker JL, Hosseinzadeh P, White H, Murr K, Milbrandt TA, Talwalkar VJ, et al. Idiopathic Genu Valgum and Its Association With Obesity in Children and Adolescents. J Pediatr Orthop. 2019;39(7):347–52. doi: 10.1097/BPO.0000000000000971. [DOI] [PubMed] [Google Scholar]
- 5.White GR, Mencio GA. Genu valgum in children: diagnostic and therapeutic alternatives. J Am Acad Orthop Surg. 1995;3(5):275–83. doi: 10.5435/00124635-199509000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling: a preliminary report. J Bone Joint Surg. 1949;31(3):464–78. [PubMed] [Google Scholar]
- 7.Eidelman M, D’Agostino P. Hemiepiphysiodesis around the knee by percutaneously guided and grooved staple. J Pediatr Orthop B. 2005;14(6):434–5. doi: 10.1097/01202412-200511000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Nouth F, Kuo LA. Percutaneous epiphysiodesis using transphyseal screws (PETS): prospective case study and review. J Pediatr Orthop. 2004;24(6):721–5. [PubMed] [Google Scholar]
- 9.Horton GA, Olney BW. Epiphysiodesis of the lower extremity: results of the percutaneous technique. J Pediatr Orthop. 1996;16(2):180–2. doi: 10.1097/00004694-199603000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Khoury JG, Tavares JO, McConnell S, Zeiders G, Sanders JO. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27(6):623–8. doi: 10.1097/BPO.0b013e318093f4f4. [DOI] [PubMed] [Google Scholar]
- 11.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27(3):253–9. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 12.Stevens PM, Klatt JB. Guided growth for pathological physes: radiographic improvement during realignment. J Pediatr Orthop. 2008;28(6):632–9. doi: 10.1097/BPO.0b013e3181841fda. [DOI] [PubMed] [Google Scholar]
- 13.Burghardt RD, Herzenberg JE. Temporary hemiepiphysiodesis with the eight-Plate for angular deformities: mid-term results. J Orthop Sci. 2010;15(5):699–704. doi: 10.1007/s00776-010-1514-9. [DOI] [PubMed] [Google Scholar]
- 14.Burghardt RD, Specht SC, Herzenberg JE. Mechanical failures of eight-plateguided growth system for temporary hemiepiphysiodesis. J Pediatr Orthop. 2010;30(6):594–7. doi: 10.1097/BPO.0b013e3181e4f591. [DOI] [PubMed] [Google Scholar]
- 15.Aslani H, Panjavy B, Bashy RH, Tabrizi A, Nazari B. The efficacy and complications of 2-hole 3 5 mm reconstruction plates and 4 mm noncanulated cancellous screws for temporary hemiepiphysiodesis around the knee. J Pediatr Orthop. 2014;34(4):462–6. doi: 10.1097/BPO.0000000000000115. [DOI] [PubMed] [Google Scholar]
- 16.Park KH, Oh CW, Kim JW, Park IH, Kim HJ, Choi YS. Angular deformity correction by guided growth in growing children: Eight-plate versus 3 5-mm reconstruction plate. J Orthop Sci. 2017;22(5):919–23. doi: 10.1016/j.jos.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Sawiris Y, Abo-Seif S, Aly A. The Using of ‘Guided Growth’for Correction of Coronal Deformities around the Knee in Skeletally Immature Children (Systematic review and Meta-analysis) Med Clin Rev. 2018;4(03):1–10. [Google Scholar]
- 18.Jelinek EM, Bittersohl B, Martiny F, Scharfstädt A, Krauspe R, Westhoff B. The 8-plate versus physeal stapling for temporary hemiepiphyseodesis correcting genu valgum and genu varum: a retrospective analysis of thirty five patients. Int Orthop. 2012;36(3):599–605. doi: 10.1007/s00264-011-1369-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schroerlucke S, Bertrand S, Clapp J, Bundy J, Gregg FO. Failure of Orthofix eight-Plate for the treatment of Blount disease. J Pediatr Orthop. 2009;29(1):57–60. doi: 10.1097/BPO.0b013e3181919b54. [DOI] [PubMed] [Google Scholar]
- 20.Ghaffari S, Mohammad amini P. Growth Modulation With Reconstruction Plate for Genu Valgum Deformity in Twins: A Case Report and Literature Review. J Pediatr Rev. 2020;8(3):189–94. [Google Scholar]