Abstract
Objective:
This article traces the influence of early misfortune on somatic and psychological symptoms, examining whether the health disadvantages endure and/or worsen over a decade.
Method:
The study uses two waves of data from the Midlife Development in the United States study. Structural equation models are used to assess change in somatic and psychological symptoms.
Results:
Findings reveal that childhood abuse is associated with more initial somatic and psychological symptoms among American adults, but that family structure and financial strain had little association with baseline adult symptoms. The effects of abuse were not observed at Wave 2 (W2), net of Wave 1 (W1) symptoms.
Discussion:
The results suggest an enduring—but not cascadic—effect of childhood abuse on adult health. There was little evidence that the consequences of early misfortune waned over the course of time or were less substantial for older adults; but neither did these early life experiences contribute to worsened symptoms over a decade of observation.
Keywords: life course epidemiology, childhood adversity, physical health, mental health
It is becoming increasingly clear that early life course conditions set the stage for the full span of human health. Many refer to childhood as a sensitive period of development, as problems experienced during this crucial period of physical development influence the maturation of multiple bodily systems (Kuh & Ben-Shlomo, 2004). Not only are early years crucial for cognitive and physiological development but also behaviors, aspirations, and dispositions emerge as young people form self-identities and begin to negotiate social institutions and peer networks (McLeod & Almazan, 2003). Insults experienced during childhood—interpersonal and material alike—are now widely acknowledged to have long-term impacts on health long before symptoms become manifest as disease (Ferraro & Shippee, 2009; Hayward & Gorman, 2004).
One perspective for understanding the connection between early conditions and later health conditions comes from the stress process model (Pearlin, 2010; Pearlin, Schieman, Fazio, &, Meersman, 2005). The framework posits that problematic conditions threaten people’s adaptive capacities; this process, in turn, unfolds over the life course: “people are never completely separated from the imprint of their origins, even as the world about them may change” (Pearlin, 2010, p. 212). Stressors arising from the social world are expected to inflict harm over long periods of time on physical and mental functioning. Moreover, these challenges to physical and mental health are interrelated, as the effects of stress diffuse across multiple domains of health and well-being (Pearlin, 1989).
Drawing from these insights, the present research examines the relationship between several types of childhood misfortune—abuse, financial strain, and family structure—and the symptoms of one’s somatic and psychological condition. This study has two aims. One objective is to move beyond specific, isolated disease categories and to consider whether early misfortune heightens multiple dimensions of psychosomatic symptoms, which may be precursors to multiple diseases. As we recount below, there is reason to expect that childhood conditions are associated with a range of interconnected physical and mental problems, but few studies make systematic allowance for this likely spillover. The second objective of this article is to examine the longitudinal nature of early misfortune’s influence. Are symptoms of physical and mental duress elevated only initially among those who faced early misfortune, or does misfortune exert additional influence over time? As we suggest below, past research tends to rely on very general language when describing long-term health effects of childhood conditions; we see the importance of clarifying whether “long-term” refers only to the existence of health problems in adulthood or whether it also signifies continued health decline over time. These concerns result in a conceptual distinction we call enduring versus cascadic effects. To study how symptoms may change over the course of a decade, we employ two waves of the Midlife Development in the United States (MIDUS) study (1995 and 2005). Observation spanning 10 years provides an important opportunity to understand the changing nature of psychosomatic well-being among American adults.
Background
Our review of the literature on childhood misfortune and adult physical and psychological health leads us to suggest three important ways that the present research can contribute to the literature: (a) clarifying the meaning of long-term effects, (b) greater attention to the connections between physical and psychological health, and (c) examination of which types of misfortune are most consequential to health.
Clarifying the meaning of long-term effects.
Of foremost concern in this study, there are potentially divergent expectations for the temporal nature of childhood misfortune’s expected effects. Although many studies have revealed important links between childhood misfortune and adult health, relatively little attention has been given to what is meant by “long-term effects.” Some scholars conceptualize the links as quite durable, perhaps indelible, with concepts such as “scarring” (Preston, Hill, & Drevenstedt, 1998) and “biological embedding” (Hertzman & Boyce, 2010). Indeed, in articulating cumulative advantage/disadvantage theory, Dannefer (2003) notes that “resource-based health effects begin early in life and interact continuously with the external circumstances” (p. S331). Ferraro and Shippee’s (2009) recent articulation of cumulative inequality theory also addresses the issue but conveys a more malleable trajectory due to childhood misfortune: “the imprint of early life is substantial but that there are many ways to modify the deleterious chain of events due to early inequalities” (p. 338).
Given distinct views of “long-term” influence, we define and test two related—though critically distinct—models of the phenomena. First, an effect could be enduring: childhood misfortune has long-lasting impact on psychosomatic health, though it does not necessarily pose additional threats for future problems net of the baseline levels. This model implies that childhood misfortune raises the overall level of health dysregulation but that subsequent expression of symptoms may operate through the initial psychosomatic problems themselves. Moreover, any symptom increases from one period to the next could be due to endogenous growth processes (e.g., symptoms beget more symptoms) or result from some factor unrelated to childhood misfortune. Second, an effect could be cascadic: childhood misfortune is associated with higher symptoms during adulthood, but it is also associated with marginal increases net of baseline levels. That is, compounding increases in health dysregulation are also attributable to early life experiences, indicating a cascade of disadvantage over the life course.
Within this framework, an effect of early misfortune must first be enduring before it can be said to be cascadic. To illustrate, if low childhood SES, abuse, or family disruption have a fleeting and reversible influence on psychosomatic symptoms that disappears within a few years, then there are no “long-term” health effects of early misfortune—and naturally no enduring or cascadic effects. It does not follow, however, that any enduring effect will also be a cascadic one. Hence, the former is a necessary but an insufficient condition for the latter.
Figure 1 provides a heuristic tool for thinking about these different processes, with the line segments representing symptom levels occurring for a given person over the course of a decade. The figure implies that the enduring effects are most clearly evidenced when younger people (represented in the dotted line) have similar symptom profiles related to misfortune as somewhat older (sold line) and the oldest adults (broken line).
Figure 1. Schematic figure illustrating enduring and cascadic effects.
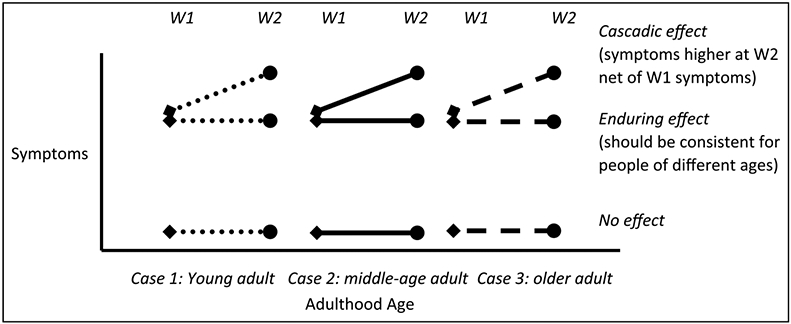
Note: Diamond denotes measurement at W1; Circle denotes measurement at W2. Each line segment illustrates a hypothetical pattern observable for a single study subject.
There are multiple ways to test for enduring and cascadic effects. Many fields of inquiry such as evidence-based medicine have established classes or levels of evidence to be used in developing empirical generalizations (and perhaps clinical guidelines). One may also think of levels of evidence for testing enduring and cascadic effects.
The finest data would be prospective and cover at least three points: childhood and two periods of adulthood. Much more common, however, are studies that retrospectively tap childhood conditions in a cross-sectional design. Of course, the information on childhood in such studies is subject to recall and reporting bias as well as selection processes (e.g., the most severe cases of childhood misfortune may lead to death or incarceration). Still, if one is able to measure childhood misfortune and adult health, one is able to test for enduring effects of the former on the latter. With retrospective data on childhood, such as are used in the present study, one can use cross-sectional data to examine enduring effects. If there is an association between childhood conditions and adult health that is not negatively moderated by age (year of birth), then the effect is said to be enduring. A negative interaction effect would challenge the idea that an effect was enduring because it could suggest that the long-term influence of disadvantage grows weaker as a person ages.1
Enduring effects could indeed be assessed with longitudinal data (e.g., 2 waves of data collected from the same panel), but this would involve examining W2 effects without adjusting for Wave 1 (W1) effects. Assessing Wave 2 (W2) net of lagged W1 effects shifts the question from enduring to cascadic effects.
Evidence required for testing cascadic effects is more demanding than that required for testing enduring effects. One may use cross-sectional data with an interaction between age and childhood misfortune to test for cascadic effects, but this would be less than ideal because there is no way of examining intraindividual change to see how symptoms change for each subject. Rather, one would capitalize on age differences—interindividual variability—to infer observed health changes during adulthood. Still, it is a reasonable approach, and a positive effect on symptoms due to a product term for age and misfortune would be evidence to infer a cascadic effect.
Ideally, however, one would use longitudinal data to test cascadic effects because seeing such an accentuation effect would be stronger with health measured in the same person at two time points. Longitudinal data enable one to estimate the effect of childhood misfortune at one point in time above and beyond the effects demonstrated at an earlier time (i.e., W2 effects net of W1 effects). A cascadic effect refers to this additional change in health, not simply the enduring effect. Of course, cascadic effects, like enduring ones, could also be more or less pronounced with age, so it is important to also consider potential interaction effects of age with the cascadic pattern of health change.2
We are unaware of any studies that make this distinction between enduring and cascadic effects; life course studies instead often invoke more general language about the “long-term” or “long-arm” consequences of childhood conditions. With cross-sectional data that lacks date of onset, one has only point estimates for given ages to address this issue. The present study capitalizes on longitudinal data to determine if childhood misfortune affects only the initial level of somatic and psychological symptoms or extends to a follow-up 10 years later. From another vantage point, one wonders if the latency period of childhood misfortune to influence health is limited or lifelong.
Connections between physical and mental health.
The context in which we will examine potential enduring and cascadic effects is in the realm of psychosomatic symptomology. By now, it is well established that childhood misfortune may affect multiple domains of physical and psychological well-being. Great strides have been made recently to identify some of the varied outcomes—ranging from specific physical (e.g., Stein et al., 2010) to psychological disorders (e.g., McLaughlin et al., 2010)—but few studies examine how early misfortune may influence multiple dimensions of psychosomatic health in simultaneous manner. Moreover, scholars have often focused on diagnosable, life-threatening conditions such as heart disease (Hamil-Luker & O’Rand, 2007), cancer (Fuller-Thompson & Brennenstuhl, 2009), or, in the case of mental health, on major depressive disorder and other forms of serious psychiatric morbidity (Gilman, Kawachi, Fitzmaurice, & Buka, 2003). Less studied is the set of ill-defined, somewhat vague problems lurking at the borderlands of physical and mental disorder. These symptoms—described in more detail in the method section—are important because they are the latent precursors of further difficulties, preceding more serious levels of disability, disease, and mortality (Katon, Sullivan, & Walker, 2001).
Part of the motivation for this study is because research on the etiology of psychosomatic health suggests a reciprocal relationship between physical and mental conditions (Kelley-Moore & Ferraro, 2005; Koopmans & Lamers, 2000; Vilhjalmsson, 1998). Although it is often practical to focus on one outcome at a time, scholars presume that the varied outcomes are related and that problems in one domain may lead to problems in another. Indeed, previous longitudinal studies have identified how physical or psychological problems may accelerate declines in the other domain, leading to cycles of decline (e.g., Gayman, Turner, & Cui, 2008; Kelly-Moore & Ferraro, 2005; Verbrugge & Jette, 1994). The present study systematically examines how childhood misfortune is related to problems in both physical and mental domains, beginning with a measurement model to identify salient dimensions and proceeding to a causal model that investigates the pervasiveness of misfortune on these aspects of health while allowing somatic and psychological domains to be correlated. In light of the stress process model, early misfortune may be expected to have diffuse, proliferative consequences for psychosomatic well-being.
Which types of misfortune are most consequential to health?
Finally, when examining the effects of childhood misfortune, one is faced with different ways to conceptualize misfortune and investigate its relationship with adult health. Different childhood challenges—related to family structure, abuse and trauma, and relative deprivation—each have been linked to adult health problems. For the sake of space, we will not review this large literature here because excellent reviews exist (see Greenfield, 2010, concerning abuse; Cohen, Janicki-Deverts, Chen, & Matthews, 2010, concerning SES; and Amato, 2000, concerning family structure).
Moreover, different forms of misfortune may have distinct long-term effects because they limit the attainment of various forms of life course capital, including human, social, and health capital (Hamil-Luker & O’Rand, 2007; O’Rand, 2006). These forms of life course capital (or their relative absence) comprise the important intervening mechanisms between childhood and adulthood. Distinguishing between these forms of life course capital, for instance, revealed different patterns of heart attack risk between the ages of 51 and 71 (Hamil-Luker & O’Rand, 2007; O’Rand & Hamil-Luker, 2005). Other research finds that different types of misfortune have distinct effects on psychological health, due to the severity of the misfortune (Schilling, Aseltine, & Gore, 2008) or its connection to family functioning (Green et al., 2010). Still other scholars find simple aggregation of childhood misfortune to be predictive of health outcomes (e.g., Edwards, Holden, Felitti, & Anda, 2003; Felitti et al., 1998), a concept which some have referred to as the “joint or cumulative effects of multiple traumas” (Turner & Lloyd, 1995, p. 368). Whereas many studies have focused on one or two particular forms of misfortune such as childhood health problems (Blackwell, Hayward, & Crimmins, 2001) or childhood social class (Langenberg, Kuh, Wadsworth, Brunner, & Hardy, 2006), the present analysis examines multiple indicators of misfortune simultaneously and whether each type is related to adult health.
Conceptual Model and Research Questions
To summarize the preceding discussion, this research examines the effects of childhood misfortune at the intersection of mental and physical health, via symptoms rather than diagnosed conditions. Our approach also emphasizes that multiple domains of early misfortune may elicit these problems, but we emphasize that the temporal nature of these potential effects may take several forms over adulthood. On the basis of exploratory factor analysis and measurement model specification (discussed below), we formulated the structural equation model displayed in Figure 2, simplified for presentation here but described in more detail in the Method section. Two main research questions guide the analysis:
Figure 2. Structural equation model assessed with MIDUS W1 and W2.
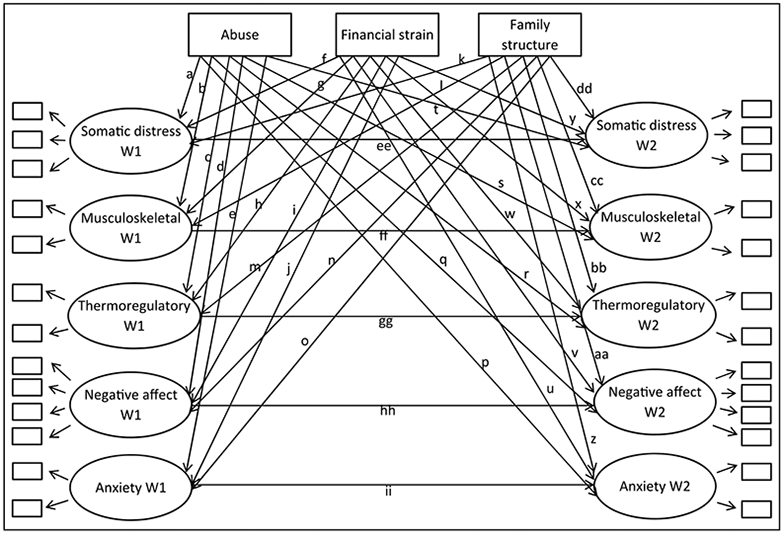
Note: This model conceptually represents the analyses presented in this article, but numerous parameters are not pictured for the sake of clarity. Specifically, the error term of each latent variable from W1 is allowed to correlate with all other latent variables at W1, and latent variables from W2 are treated similarly. The indicator for each manifest variable at W1 has its error term correlated with its counterpart at W2. Finally, the exogenous variables (childhood misfortune plus covariates) are allowed to correlate.
Research Question 1: Is childhood misfortune associated with both somatic and psychological symptoms during adulthood?
This question focuses on whether there are significant regression paths linking any of the domains of psychosomatic symptoms to childhood abuse, low SES, or family structure, while accounting for the correlation between somatic and psychological problems. Though we use childhood misfortune as the conceptual starting point, attention will be given to the consequences of each type of misfortune.
Research Question 2: If childhood misfortune is consequential, are the effects best described as enduring or as cascadic?
Following our discussion above, enduring effects will be demonstrated by significant regression paths from childhood misfortune to W1 symptoms (paths a-o), whereas cascadic effects will be established by significant regression paths from childhood misfortune to W1 and W2 symptoms (paths p-dd). Also as alluded to above, we will consider whether the long-term effects of misfortune are contingent on age, a finding that would call into question how enduring the effects of early misfortune truly are.
Method
Data
Data for the analysis came from the Midlife Development in the United States (MIDUS) study. The MIDUS was undertaken to better understand health and well-being of American adults across a broad range of ages. Data were first collected from 1995 to 1996 by the MacArthur Foundation’s Network on Successful Midlife Development. The survey first used random-digit-dialing to obtain a sampling frame from English-speaking noninstitutionalized adults aged 25 to 74 in the contiguous 48 states. Next, the investigators used disproportionate stratified sampling to oversample males between 65 and 74. The response rate from these initial telephone interviews was 70%. The final stage included a two-part follow-up questionnaire mailed to those who participated in the telephone interview, yielding an 86.6% response rate. Thus the overall response rate was 61% (.70 × .87 = .61), producing a total sample of 3,032 participants who completed both the telephone and mail interview. Respondents from W1 were contacted about 10 years later to secure their participation for W2 in 2005. From the complete W1 sample, 1,748 individuals (58%) completed both the telephone and self-administered follow-up interview.
Measures
Somatic and Psychological Symptoms.
Somatic symptoms were assessed with a 10-item index. During the course of the self-administered questionnaire, respondents were asked how often they experienced the following during the past 30 days: (a) headaches, (b) back aches, (c) frequent sweating, (d) irritability, (e) hot flashes or flushes, (f) aches or stiffness in the joints, (g) troubling getting to or staying asleep, (h) incontinence, (i) pain during sex, and (j) pain in the extremities. The response categories for each item ranged from not at all (coded 1) to almost every day (6). We completed preliminary analyses by averaging responses to the eight items, forming an index with a reliability of .75. However, factor analysis (described below) reveals that there are multiple dimensions to the somatic symptoms measure (labeled somatic distress, musculoskeletal, and thermoregulatory), and these are used in the final analysis. All items were logged to reduce their individual variance.
Psychological symptoms were also assessed within a 30-day window using a multi-item index. Symptoms included feeling (a) so sad nothing could cheer you up, (b) nervous, (c) restless or fidgety, (d) hopeless, (e) that everything was an effort, and (f) worthless. Response options ranged from none of the time (coded 1) to all the time (5). In preliminary analyses, we found that these items can be used as an index (α = .87), yet the results of factor analysis (described below) reveal a two-factor solution to these six items (labeled negative affect and anxiety). As with somatic symptoms, the items were logged to reduce skewness.
Childhood Misfortune.
To measure the extent of trouble experienced early in the life course, we created three summary scores encompassing different domains of childhood misfortune. Indicators of childhood misfortune were (a) selected on the basis of prior literature (Felitti et al., 1998; Turner & Lloyd, 1995) and (b) drawn from the available pool of MIDUS questions on childhood. These items include (a) receipt of welfare, (b) less than a high school education for father (or mother, in households where father was not present), (c) report of being “worse off’ than other families, (d) lack of male in the household, (e) parental divorce, (f) death of a parent, physical abuse at the hands of (g) mother, (h) father, (i) siblings, or (j) other person, (k-n) emotional abuse by any of the same parties. Questions regarding abuse were based on well-validated measures in the Conflict Tactics Scale (Straus, 1979), and abuse was considered an affirmative if it was reported as “often” or “sometimes.”
Following Felitti et al. (1998), each indicator was coded in dichotomous form, reflecting a major insult during childhood (e.g., responses to the eight abuse items ranged from never (coded 1) to often (4), and abuse was coded as present if reported as sometimes or often). Next, we divided the indicators of misfortune into three conceptual categories: abuse (including both physical and emotional maltreatment), family structure (divorce, death, lack of male in household), and financial strain (welfare, low education, worse off than others). These categories were defined on the basis of face validity and in line with past studies that identify the importance of considering how different types of early misfortune influence the accumulation of life course capital (O’Rand, 2006).
Other Covariates.
The analysis also adjusted for basic demographic characteristics: age (years old), education (number of years in school), female (1 = yes, 0 = no), and non-White (1 = non-White, 0 = otherwise). Preliminary analyses considered other demographic controls (e.g., marital status), but they were removed from final models because they did not improve model fit.
Analysis
Before assessing the influence of childhood misfortune on adulthood symptoms, the first step was to examine the factor structure and the interrelation between somatic and psychological symptoms themselves. There may be multiple dimensions underlying the basic somatic and psychological symptom indexes, and, if mental and physical health are intertwined, we should see sizeable correlations between each of the factors.
As a first step, therefore, factor analysis was completed in Stata 12 (StataCorp, 2011) using the principal factor method and a varimax (orthogonal) rotation. Psychological symptoms neatly fell into two factors: (1) negative affect—sadness, hopelessness, the sense of everything being an effort, and worthlessness; (2) anxiety—nervousness and restlessness. Somatic symptom items, on the other hand, demonstrate a three-factor structure: (1) somatic distress—headaches, irritability, and trouble sleeping; (2) musculoskeletal—lower back aches and aches or stiffness in joints; (3) thermoregulatory—frequent sweating and hot flushes/flashes. Two additional items (incontinence and pain or discomfort during sex) were removed from the list of somatic symptoms during preliminary analyses because they failed to load on any factor. Once the basic factor structure was determined for both somatic and psychological symptoms, a full measurement model was assessed. This model allowed all latent factors to be correlated and was used to assess overall model fit.
Finally, structural equation modeling was used to assess the relationship between adverse childhood experiences and the multiple dimensions of somatic and psychological symptoms. Estimation used Stata 12’s Full Information Maximum Likelihood procedure for missing data. Figure 2 (above) shows the conceptual model that is the basis of our analyses. Childhood misfortune—along with age, education, female, and non-White—are treated as exogenous factors; and W1 and W2 symptoms are considered endogenous variables. This figure, however, leaves out many parameters for the sake of space within the graphic. Correlations were estimated between all exogenous variables—indicators of childhood misfortune plus demographic covariates. Error terms of W1 latent variables were correlated, as were those from W2 measurement. Finally, error terms were correlated between W1 manifest indicators and their W2 counterparts (e.g., how often respondent reported “sweating a lot” in the past 30 days, both W1 and W2).
Results
Descriptive Statistics and Measurement Model Results
Table 1 presents the possible range of each explanatory variable, its mean, and its standard deviation (SD; except for binary variables). The next step in the analysis was to assess a measurement model (for W1 and for W2), which treats psychological symptoms as a construct composed of two latent dimensions and somatic symptoms as a three-dimension latent construct. Manifest indicators for each dimension of symptoms correspond with the items used in the factor analysis. On the basis of our assumption that the various types of symptoms are interrelated, we allowed the latent constructs to be correlated. Indeed, the correlations are strong, ranging from .25 at the low end (thermoregulatory with negative affect at W2) to .82 at the high end (somatic distress with anxiety at W1). All 10 W1 and W2 correlations between the five latent factors are significant at the .001 level and are reported in Figures 3 and 4.
Table 1.
Descriptive Statistics for Explanatory Variables From the MIDUS Sample (n = 3,032)
| Range | Mean | SD | |
|---|---|---|---|
| Childhood misfortune | |||
| Abuse | 0-8 | 1.34 | 1.40 |
| Family structure | 0-3 | .26 | .55 |
| Financial strain | 0-3 | .74 | .80 |
| Covariates | |||
| Age | 20-74 | 47.06 | 13.12 |
| Education | 0-20 | 13.78 | 2.62 |
| Female | 0-1 | .51 | |
| Non-White | 0-1 | .15 |
Figure 3. Measurement model results, W1.
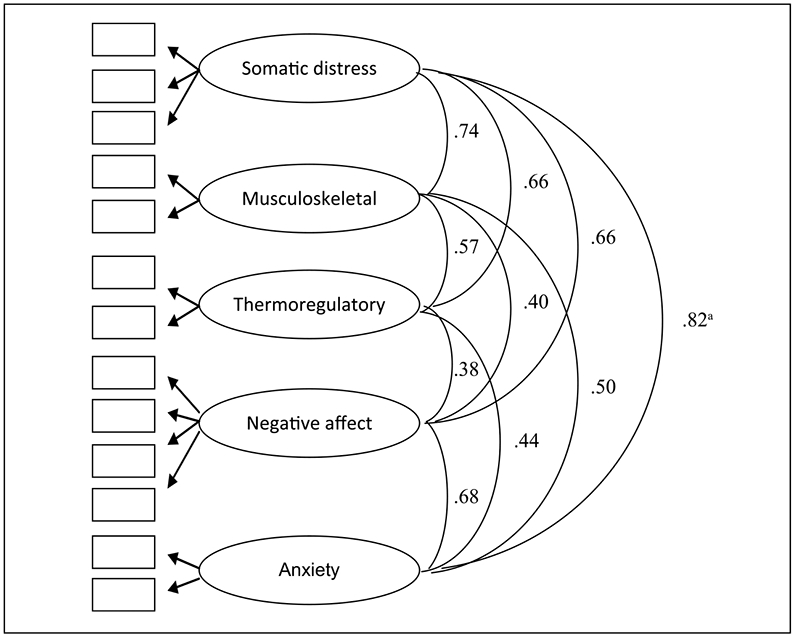
Note: Model fit statistics: χ2 = 475.23, (df = 55); RMSEA = .05; CFI = .97; TLI = .95.
aAll covariances are standardized and significant at p < .001.
Figure 4. Measurement model results, W2.
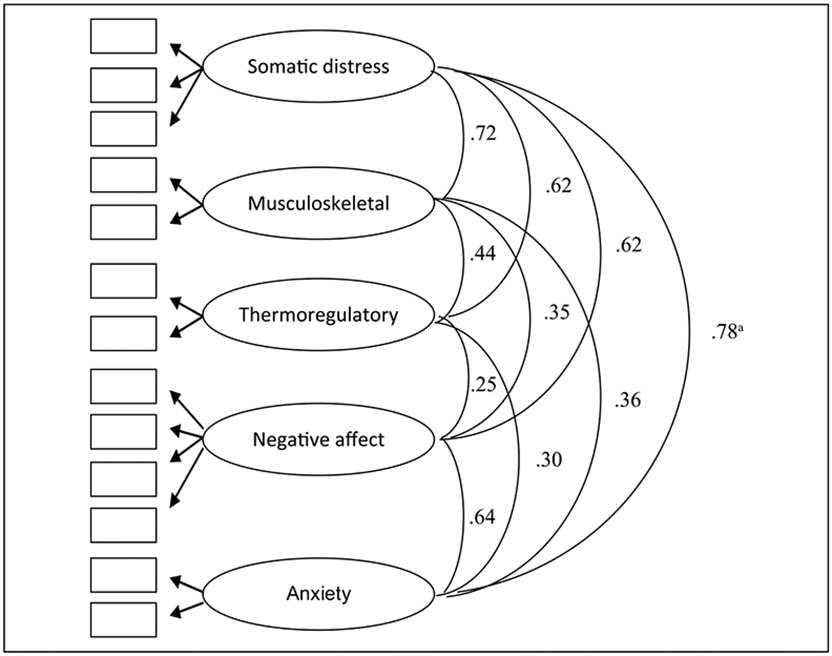
Note: Model fit statistics: χ2 = 333.13, (df = 55); RMSEA = .05; CFI = .96; TLI = .94.
aAll covariances are standardized and significant at p < .001.
In most regards, maximum likelihood estimation of the measurement model revealed acceptable model fit. The χ2values of 475.23 and 333.13 with 55 degrees of freedom for W1 and W2, respectively, are statistically significant, which indicates an unsatisfactory fit to the observed data. With 3,032 observed cases, however, χ2 is not the ideal indication of model fit as it is prone to be inflated for large sample sizes (Bollen, 1989). Other model fit values are respectable. The root mean square error of approximation (RMSEA) value is .05 for W1 and for W2, within the preferred cutoff value. The value of comparative fit index (CFI) and the Tucker-Lewis Index (TLI) are both adequately high, with values ranging from .94 to .97 (1.00 is highest).
Structural Equation Model Results
Having identified the factor structure of the symptoms and evaluated the measurement model, the main and final step of the analysis is to examine whether childhood misfortune contributes to higher levels of psychosomatic symptoms and what the nature of these effects was over both waves of the study. The results of the structural equation model are displayed in Table 2. Overall, the model fits the data fairly well on the basis of RMSEA (.04), CFI (.92), and TLI (.89). The coefficients in Table 3 are standardized effects.
Table 2.
Standardized Coefficients From Structural Equation Model: Predicting Somatic and Psychological Symptoms, MIDUS W1 and W2
| Somatic distress-W1 |
Musculoskeletal -W1 |
Thermoregulatory -W1 |
Negative affect-W1 |
Anxiety -W1 |
Somatic distress-W2 |
Musculoskeletal -W2 |
Thermoregulatory -W2 |
Negative affect-W2 |
Anxiety -W2 |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Childhood misfortune | ||||||||||
| Abuse | .20*** | .16*** | .09*** | .16*** | .18*** | .01 | .07* | −.01 | .03 | .05 |
| Financial strain | .08*** | .04 | .02 | .04* | .03 | .02 | .02 | .02 | .01 | −.02 |
| Family structure | .02 | −.01 | .01 | .03 | .02 | −.04 | .06* | .02 | −.01 | −.04 |
| Covariates | ||||||||||
| Age | −.28*** | .17*** | .06** | −.11*** | −.10*** | −.15*** | .09** | −.07** | −.04 | −.10*** |
| Education | −.03 | −.15*** | −.11*** | −.11*** | −.04 | −.09** | −.07* | −.01 | −.09*** | −.10*** |
| Female | .20*** | .03 | .27*** | .11*** | .11*** | .02 | .03 | .28*** | .03 | .01 |
| Non-White | −.15*** | −.09*** | .03 | .03 | −.07** | .06 | .02 | −.02 | .04 | −.01 |
| Symptoms, W1 | ||||||||||
| Somatic distress-W1 | .60*** | |||||||||
| Orthopedic-W1 | .63*** | |||||||||
| Thermoregulatory-W1 | .38*** | |||||||||
| Negative affect-W1 | .46*** | |||||||||
| Anxiety-W1 | .52*** | |||||||||
| Squared multiple correlation | .18 | .09 | .11 | .08 | .07 | .45 | .48 | .29 | .26 | .32 |
Note: Model fit statistics: χ2 = 2315.55, (df = 374); RMSEA = .04; CFI = .92; TLI = .89.
p < .05.
p < .01.
p < .001.
Table 3.
Standardized Direct and Indirect Effects of Childhood Misfortune on W2 Symptoms, MIDUS
| Somatic distress-W2 |
Musculoskeletal -W2 |
Thermoregulatory -W2 |
Negative affect-W2 |
Anxiety -W2 |
|
|---|---|---|---|---|---|
| Direct effect | |||||
| Abuse | .01 | .07* | −.01 | .03 | .05 |
| Financial strain | .02 | .02 | .02 | .01 | −.02 |
| Family structure | −.04 | .06* | .02 | −.01 | −.04 |
| Indirect effect (through W1 version of latent construct)a | |||||
| Abuse | .10*** | .08*** | .03* | .08*** | .09*** |
| Financial strain | .03 | .03 | .00 | .02 | .02 |
| Family structure | .01 | −.01 | −.01 | .01 | .01 |
An example of such an indirect effect would be abuse → somatic distress W1 → somatic distress W2 (path a → ee in Figure 2)
p < .05.
p < .01.
p < .001.
The five leftmost columns in Table 2 represent W1 estimates. As demonstrated in these columns, reports of child abuse are associated with higher levels of all symptom dimensions with effect sizes ranging from .09 (thermoregulatory) to .20 (somatic distress), and all associations were significant at p < .001). Notably, the indicator of financial strain had far more meager associations with the symptom constructs. The standardized effect was .04 (p < .05) for predicting negative affect and .08 (p < .001) for somatic distress. None of the other associations between financial strain and symptoms were statistically significant. Notable too is the conspicuous lack of effect for family structure; this variable was not associated with any dimension of somatic or psychological symptomology. Most demographic covariates were associated with psychosomatic symptoms. Age, for instance, was associated with less somatic distress, negative affect, and anxiety, but more musculoskeletal and thermoregulatory symptoms. Women tended to report more symptoms than men, with the exception of musculoskeletal symptoms. Higher levels of education and being non-White were associated with reporting fewer symptoms across several of the dimensions.
In summary, the standardized regression weights from the first five columns (representing paths a-o in Figure 2) support the idea that early misfortune—namely abuse—has a robust influence on a range of diffuse symptoms representing psychosomatic health. Moreover, supplementary analyses (reported in the Appendix) indicate that these effects of child abuse are not contingent on age. That is, when interaction models are estimated with each Misfortune × Age term included, there is no significant interaction effect for abuse and age. In these supplementary models, we see the family structure variable emerge as a significant predictor only of W1 somatic distress symptoms (β = .18, p < .05). This effect, however, does not appear to be as enduring because it tapers sharply with increasing age (β = −.16, p < .05). The full interaction model, while in some ways instructive, is not the preferred model for this analysis; inspection of the information criteria reveals that the simpler model without any interaction effects is a better-fitting approach by a considerable margin (Table 2 Model: AIC = 140098.50, BIC = 141422.23; Appendix Table: AIC = 209824.57, BIC = 211509.33).3
All things considered, the findings on regression paths a-o (Figure 2 and in Table 2) suggest that one form of early misfortune—childhood abuse—has an enduring effect on somatic and psychological symptoms. But are its effects also cascadic?
The final five columns in Table 2 continue this line of inquiry, representing paths (p-ii) in Figure 2. The standardized coefficients indicate that childhood misfortune has very limited influence on symptoms at W2, net of its effects on W1 psychosomatic health. Abuse has a modest association with W2 musculoskeletal symptoms (β = .07, p < .05), but has no observed effect on somatic distress, thermoregulatory indicators, negative affect, or anxiety. Likewise, financial strain, which was associated with two symptom dimensions at W1, had no association with the W2 symptoms. Similar to abuse, family structure shows a small association with musculoskeletal symptoms (β = .06, p < .05). This association is curious in that family structure was not associated with any of the symptoms at W1, perhaps suggesting that stressors within the family can have a long period of latency before they influence psychosomatic health in adulthood. Taken together, however, the results are much more consistent in suggesting that abuse and, to a lesser extent, financial strain, have enduring effects on adulthood psychosomatic symptoms. Cascadic effects—a continued marginal influence beyond baseline levels—was only weakly supported for the case of musculoskeletal symptoms. This result should be interpreted with some caution, however, because it was not robust to the inclusion of the full set of age interactions. The abuse coefficient becomes nonsignificant in the supplementary analyses reported in Appendix (β = .16, p = .15).
Another divergent finding that emerges in the supplementary full-interaction model (Appendix) is that childhood financial strain becomes positive and significant as a predictor of musculoskeletal and thermoregulatory symptoms while its corresponding age interaction terms becomes negative, significant, and equal in effect size.4 This was a somewhat unexpected finding, because our conceptualization of cascadic effects was premised on the assumption that health risks must first be enduring to then have a continued cascading effect. Again, however, we hesitate to infer too many firm conclusions about cascadic effects from the interaction findings, as the model was not preferable to the one presented in Table 2 and because the age-contingent effects were neither observable for abuse (the most enduring of childhood health risks) nor were consistently observed for the financial strain indicator.
Finally, it is important to note that the association between childhood misfortune and W2 symptoms did not “disappear”; rather, it was accounted for via the influence of W1 symptoms shown in the bottom rows of Table 2 (paths ee-ii in Figure 2). Indeed, analysis of the direct and indirect effects of childhood misfortune and W2 symptoms reveals that abuse had statistically significant indirect (through corollary W1 measures) effects on all five dimensions of psychosomatic symptoms; W1 symptoms are the conduits through which abuse has lasting influence on W2 symptoms. These results are shown in Table 3.
Discussion
The findings of this study can be summarized around three main themes: (a) distinct types of early misfortune have unique effects on adult health, (b)of the types of misfortune considered, child abuse proved especially consequential on somatic and psychological symptoms, (c) childhood abuse had sizeable effects on W1 symptoms, but not on W2 symptoms net of W1.
Of the three domains of childhood misfortune considered in this study—abuse, financial strain, and family structure—child abuse was the most consequential. Consistent with past research on the epidemiology of social stress and the continuity of interpersonal stressors over the life course (Kessler & Magee, 1993; Turner, Wheaton, & Lloyd, 1995), physical and emotional abuse during childhood were associated with a broad range of adulthood stressors. The effect size of child abuse on nearly all latent dimensions of the symptoms (20% of a SD on somatic distress, 18% of a SD on anxiety, 16% of a SD on musculoskeletal and negative affect, and 9% of a SD on thermoregulatory), suggests that the influence of abuse on adult health is both nontrivial and diffuse across bodily systems (Greenfield, 2010).
Many studies have documented direct and indirect effects of early misfortune on the mental health of young adults (Adkins, Wang, Dupre, van den Oord, & Elder, 2009; Hazel, Hammen, Brennan, & Najman, 2008), while others have assessed these outcomes in middle- or older-age (Clark, Caldwell, Power, & Stansfeld, 2010; Green et al., 2010; McLaughlin et al., 2010; Schilling et al., 2008). The current study attempted to keep the full scope of adulthood in view. With a sample of Americans aged 25 to 74, we see that childhood misfortune—namely abuse—changes the experience of physical and psychological health across the life course.
In terms of psychosomatic processes, such biographical stamps on the life course may leave a “biological residue” and alter stress-responses (Miller et al., 2009). On investigation using factor analysis and a measurement model, we found much interrelation between different dimensions of psychosomatic symptoms. In line with other studies documenting a close connection between mental and physical well-being (e.g., Kelley-Moore & Ferraro, 2005), our analyses reveal that negative affect, anxiety, somatic distress, musculoskeletal discomfort, and thermoregulatory irritation tend to co-occur. Abuse appears to play a substantial role in this vexing complex of symptoms, supporting the thesis that “adverse social conditions yield broad, pluripotential pathogenicity” (Herztman & Boyce, 2010, p. 331).
Unlike some studies that consider the simple accumulation of different adversities (e.g., Felitti et al., 1998), this study revealed that there is some utility to examining domains of misfortune separately. For somatic and psychological symptoms, child abuse seems especially damaging, while meager effects were observed for early financial strain family structure. In this way, abuse appears to constitute a particularly acute and damaging form of childhood misfortune. Recent cellular evidence suggests that early abuse produces accelerated stress-based chromosomal aging and decline (Tyrka et al., 2010); this process is set in motion by particularly intense experiences, which problems in childhood family structure or socioeconomic strain may fall short of precipitating.
The third main and most novel finding of this study is that the effects of one form of childhood misfortune—child abuse—were enduring; that is, the effects were observed across a wide range of adult ages that stretched well beyond the childhood years. Interestingly, however, the influence of childhood abuse on somatic and psychological symptoms did not increase over the course of a decade of observation, failing to support the model of cascadic effects. Though symptom scores were higher at baseline among those who experienced child abuse, effects at the second wave were largely explained by the initial levels of symptoms. This suggests that while the “long arm of childhood” reaches into adulthood (Hayward & Gorman, 2004), it does not necessarily generate a continued marginal decline—at least not for somatic and psychological symptoms. Although few direct effects of childhood misfortune were evident for second wave outcomes net of baseline levels, abuse was associated with indirect effects on the follow-up wave symptoms (via W1 symptoms). This suggests that physical and emotional maltreatment begets a higher baseline level of somatic and psychological symptoms—and these initial levels carry forward in time, inducing more dysregulation a decade later. This finding fits our conceptualization of an enduring effect.
The current study has several important limitations. First is the use of retrospective data. All information about early misfortune was gathered when participants were between 25 and 74 years of age. Any systematic biases in childhood recall (e.g., people with high levels of psychological distress being more inclined to exaggerate the woe of their childhood) would call our findings into question. These biases are always possible when using retrospective questions, but the MIDUS questionnaire was devised to minimize it by asking for specific information on experiences and never mentioning words such as adversity or abuse. For example, the MIDUS questions on abuse relied on the well-validated and widely used Conflict Tactics Scale (Straus 1979), asking about specific acts such as being “pushed, grabbed, or shoved” or “slapped.” To date, most research acknowledges the potential fallibility of retrospective measures, but finds no cause to preemptively disregard their use on the basis of systematic reporting error (Hardt & Rutter, 2004). Nevertheless, these limitations highlight the superiority of prospective longitudinal data in studies of aging and the life course.
A second limitation is the broad age range of respondents included in the study. With adults spanning an age range of nearly 50 years, temporal proximity to childhood conditions is quite far for some people, but quite close for others. In supplementary analyses, we tested Age × Misfortune terms, but found that most of the findings concerning enduring effects were unchanged (the lone exception being a W1 effect of family structure on somatic distress symptoms). Finally, though the wide age range is in some ways a limitation, it offers the strength of ascertaining effects for adults beyond a single birth cohort.
In conclusion, this study provides further evidence that childhood conditions—especially abuse—cast a long shadow over adult somatic and psychological health. The stress process model articulates the role of early misfortune for begetting diffuse and long-lasting health consequences (Pearlin, 2010), a premise that was clearly documented in the current study. By considering both direct and indirect effects, moreover, one sees that maltreatment during childhood has enduring effects on somatic and psychological distress in adulthood. Stated differently, many problems related to negative affect, anxiety, somatic distress, musculoskeletal discomfort, and thermoregulatory unease are rooted in noxious childhood experiences. That being said, the lack of a cascadic influence offers an alternative to the pessimistic notion that an inauspicious start in life permanently “scars” one’s life trajectory and induces a lifelong barrage of unfortunate events.5 Rather, the evidence presented herein reveals a much more contingent and modifiable view of the effects of early misfortune on health (Ferraro & Shippee, 2009). Research that can isolate those contingencies is useful both for developing effective interventions and to avoid self-fulfilling prophecies of cascadic disadvantage.
We welcome further clarification and debate concerning the best way to conceptualize childhood misfortune’s “long arm.” Much ongoing research in the area of childhood events and adult health focuses on the many possible mediating pathways that can explain the association (e.g., Hamil-Luker & O’Rand, 2007; Preston et al., 1998). Other scholars have emphasized personal attributes or resources that can moderate the relationship (e.g., Pitzer & Fingerman, 2010). If our conceptual distinction between enduring and cascadic effects holds any merit, then particular mediating and moderating factors may be more or less important in the context of different temporal processes. For instance, is a sense of personal control or mastery (Pearlin, 2010) most useful for preventing early insults from becoming enduring effects, or is it most crucial for preventing continued, cascadic, adversity-related decline? Perhaps it is equally important for both processes. Likewise, future research should examine gender and racial differences in the health consequences of early misfortune over time, and should give more focused attention to additional forms of adversity (e.g., sexual abuse, neighborhood disorder) that may endure or cascade differently than the conditions examined in this study. We hope that future research will challenge our conceptualization of temporality and risk in the life course, but more importantly, that it will also give more nuanced attention to how additional mediating and moderating variables are involved in the unfolding of long-term health effects related to childhood conditions.
Acknowledgment
We appreciate the constructive comments from JAH reviewers in helping strengthen this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Support for this research was provided by a grant from the National Institute on Aging (R01AG033541).
Appendix
Standardized Coefficients From Alternate Structural Equation Model: Childhood Misfortune and Age Interaction Model Predicting Somatic and Psychological Symptoms, MIDUS W1 and W2
| Somatic distress-W1 |
Musculoskeletal -W1 |
Thermoregulatory -W1 |
Negative affect-W1 |
Anxiety -W1 |
Somatic distress-W2 |
Musculoskeletal -W2 |
Thermoregulatory -W2 |
Negative affect-W2 |
Anxiety -W2 |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Childhood misfortune | ||||||||||
| Abuse | .26** | .28** | .06 | .28*** | .27*** | −.06 | .16 | .01 | .04 | .06 |
| Financial strain | −.04 | −.02 | .17 | .09 | −.04 | .13 | .23* | .22* | −.04 | .02 |
| Family structure | .18* | .11 | .04 | .03 | −.05 | .09 | −.02 | .07 | .04 | −.05 |
| Abuse × Age | −.06 | −.13 | .03 | −.12 | −.09 | .07 | −.09 | −.02 | −.01 | −.01 |
| Financial strain × Age | .14 | −.07 | −.16 | −.05 | .08 | −.12 | −.23* | −.22* | −.04 | −.04 |
| Family structure × Age | −.16* | −.14 | −.03 | −.01 | −.10 | −.14 | .08 | −.06 | −.05 | .02 |
| Covariates | ||||||||||
| Age | −.27*** | .20** | .10** | −.07* | −.08* | −.12* | .10** | −.01 | −.03 | −.09* |
| Education | −.03 | −.15*** | −.11*** | −.11*** | −.04 | −.09** | −.07* | −.01 | −.09*** | −.10*** |
| Female | .20*** | .01 | .27*** | .11*** | .11*** | .03 | .02 | .28*** | .03 | .01 |
| Non-White | −.15*** | −.09*** | .03 | .03 | −.06** | .06 | .03 | −.02 | .04 | −.01 |
| Symptoms, W1 | ||||||||||
| Somatic distress-W1 | .60*** | |||||||||
| Orthopedic-W1 | .63*** | |||||||||
| Thermoregulatory-W1 | .38*** | |||||||||
| Negative affect-W1 | .46*** | |||||||||
| Anxiety-W1 | .52*** | |||||||||
| Squared multiple correlation | .18 | .09 | .11 | .08 | .07 | .45 | .48 | .29 | .26 | .32 |
Note: Model fit statistics: χ2 = 2382.37, (df = 422); RMSEA = .04; CFI = .92;TLI = .88.
p < .05.
p < .01.
p < .001.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Alternatively, such an interaction could reveal something about cohort effects and have little to do with aging per se. Perhaps, for instance, older cohorts are “more hardy” or immune to adversity than recent ones. Regardless of such a possibility, the proposed interaction term (Age × Misfortune) merely serves as a means to cast doubt upon and raise rationale for falsifying the enduring effect explanation, not as a tool to decisively validate it (Popper 1959). The lack of a negative interaction between age and misfortune, however, would imply that neither contingency—age nor cohort—was at play, and it would simply help rule out the possibility that time heals the wounds of early insults. Our aim is to scrutinize the temporal form of symptom expression and knock down false leads, not to pronounce a given pattern as incontestably certain.
Strictly speaking, the potential for age moderation in a cascadic effect does not invalidate it as a concept but provides specificity as to where it can be observed. On the other hand, strong and negative age moderation for the prevalence of baseline health problems directly challenges the idea of an enduring effect, because that concept depends on consistent effects across person-level time (age).
Other model fit comparisons between Table 2 estimates and full-interaction model estimates (Appendix) are as follows: χ2 = 23155.15 (374 df), RMSEA = .04, CFI = .92, TLI = .89 (Table 2); χ2 = 2382.37 (422 df), RMSEA = .04, CFI = .92, TLI = .88 (Appendix).
This could imply that while low childhood SES is not associated in an enduring way with symptoms, it is associated with a more rapid progression of musculoskeletal and thermoregulatory symptoms among relatively young adults.
Indeed, in the instances where cascadic effects could be argued—the association between low childhood SES and musculoskeletal and thermoregulatory symptoms—there was no initial (W1) association with misfortune; and, just as importantly, the observed sharply diminished with age. Given that these two clusters of symptoms are positively associated with age, it appears that they may surface prematurely among people of low SES backgrounds, but do not continue to worsen over the entire course of adulthood due to childhood conditions.
References
- Adkins DE, Wang V, Dupre ME, van den Oord EJ, & Elder GH Jr. (2009). Structure and stress: Trajectories of depressive symptoms across adolescence and young adulthood. Social Forces, 88, 31–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato PR (2000). The consequences of divorce for adults and children. Journal of Marriage and the Family, 62, 1269–1287. [Google Scholar]
- Blackwell DL, Hayward MD, & Crimmins EM (2001). Does childhood health affect chronic morbidity in later life? Social Science & Medicine, 52, 1269–1284. [DOI] [PubMed] [Google Scholar]
- Bollen KA (1989). A new incremental fit index for general structural equation models. Sociological Methods & Research, 17, 303–316. [Google Scholar]
- Clark C, Caldwell T, Power C, & Stansfeld SA (2010). Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Annals of Epidemiology, 20, 385–394. [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Chen E, & Matthews KA (2010). Childhood socioeconomic status and adult health. Annals of the New York Academy of Sciences, 1186, 37–55. [DOI] [PubMed] [Google Scholar]
- Dannefer D (2003). Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and the social science theory. Journal of Gerontology: Social Sciences, 58B, S327–S337. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, & Anda RF (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry, 160, 1453–1460. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, & Shippee TP (2009). Aging and cumulative inequality: How does inequality get under the skin? The Gerontologist, 49, 333–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Thompson E, & Brennenstuhl S (2009). Making a link between childhood physical abuse and cancer. Cancer, 15, 3341–3350. [DOI] [PubMed] [Google Scholar]
- Gayman MD, Turner RJ, & Cui M (2008). Physical limitations and depressive symptoms: Exploring the nature of the association. Journal Gerontology: Social Sciences, 63, S219–S228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice GM, & Buka SL (2003). Family disruption in childhood and risk of adult depression. American Journal of Psychiatry, 160, 939–946. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67, 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA (2010). Child abuse as a life-course determinant of adult health. Maturitas, 66, 51–55. [DOI] [PubMed] [Google Scholar]
- Hamil-Luker J, & O’Rand AM (2007). Gender differences in the link between childhood socioeconomic conditions and heart attack risk in adulthood. Demography, 44, 137–158. [DOI] [PubMed] [Google Scholar]
- Hardt J, & Rutter M (2004). Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Childhood Psychology and Psychiatry, 45, 260–73. [DOI] [PubMed] [Google Scholar]
- Hayward MD, & Gorman BK (2004). The long arm of childhood: The influence of early-life social conditions on men’s mortality. Demography, 41, 87–107. [DOI] [PubMed] [Google Scholar]
- Hazel NA, Hammen C, Brennan PA, & Najman J (2008). Early childhood adversity and adolescent depression: The mediating role of continued stress. Psychologial Medicine, 38, 581–589. [DOI] [PubMed] [Google Scholar]
- Hertzman C, & Boyce T (2010). How experience gets under the skin to create gradients in developmental health. Annual Review of Public Health, 31, 329–347. [DOI] [PubMed] [Google Scholar]
- Katon W, Sullivan M, & Walker E (2001). Medical symptoms without identified pathology: Relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Annals of Internal Medicine, 134, 917–925. [DOI] [PubMed] [Google Scholar]
- Kelley-Moore JA, & Ferraro KF (2005). A 3-D model of health decline: Disease, disability, and depression among black and white older adults. Journal of Health and Social Behavior, 46, 376–391. [DOI] [PubMed] [Google Scholar]
- Kessler RC, & Magee WJ (1993). Childhood adversities and adult depression: Basic patterns of association in a US national survey. Psychological Medicine, 23, 679–690. [DOI] [PubMed] [Google Scholar]
- Koopmans GT, & Lamers LM (2000). Chronic conditions, psychological distress and the use of psychoactive medications. Journal of Psychosomatic Research, 48, 115–123. [DOI] [PubMed] [Google Scholar]
- Kuh D, & Ben-Shlomo Y (2004). A life course approach to chronic disease epidemiology. Oxford, UK: Oxford University Press. [PubMed] [Google Scholar]
- Langenberg C, Kuh D, Wadsworth MEJ, Brunner E, & Hardy R (2006). Social circumstances and education: Life course origins of social inequalities in metabolic risk in a prospective national birth cohort. American Journal of Public Health, 96, 2216–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication II: Associations with persistence of DSM-IV Disorders. Archives of General Psychiatry, 67, 124–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod JD, & Almazan EP (2003). Connections between childhood and adulthood. In Mortimer JT & Shanahan MJ (Eds.), Handbook of the life course (391–411). New York, NY: Kluwer/Plenum. [Google Scholar]
- Miller GE, Chen E, Fok AF, Walker H, Lim A, Nicholls, & Kobor MS (2009). Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proceedings of the National Academy of Sciences, 106, 14716–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Rand AM (2006). Stratification and the life course: Life course capital, life course risks, and social inequality. In Binstock RH, George LK, Cutler SJ, Hendricks J & Schulz JH (Eds.), Handbook of aging and the social sciences (6th ed., pp. 145–162). Boston, MA: Academic Press. [Google Scholar]
- O’Rand AM, & Hamil-Luker J (2005). Processes of cumulative adversity: Childhood disadvantage and increased risk of heart attack across the life course. Journal of Gerontology: Social Sciences, 60B, S117–S124. [DOI] [PubMed] [Google Scholar]
- Pearlin LI (1989). The sociological study of stress. Journal of Health and Social Behavior, 30, 241–256. [PubMed] [Google Scholar]
- Pearlin LI (2010). The life course and the stress process: Some conceptual comparisons. Journal of Gerontology: Social Sciences, 65B, S207–S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, & Meersman SC (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46, 205–219. [DOI] [PubMed] [Google Scholar]
- Pitzer LM, & Fingerman KL (2010). Psychosocial resources and associations between childhood physical abuse and adult well-being. Journal of Gerontology: Social Sciences, 65B, P425–P433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popper K (1959). The logic of scientfic discovery. NY: Basic Books. [Google Scholar]
- Preston SH, Hill ME, & Drevenstedt GL (1998). Childhood conditions that predict survival to advanced ages among African-Americans. Social Science and Medicine, 47, 1231–1246. [DOI] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, & Gore S (2008). The impact of cumulative childhood adversity on young adult mental health: Measures, models, and interpretations. Social Science & Medicine, 66, 1140–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2011). Stata Statistical Software: Release 12. College Station, TX: Stata-Corp LP. [Google Scholar]
- Stein DJ, Scott K, Abad JMH, Aguilar-Gaxiola S, Alonso J, Angermeyer M, & Von Korff M (2010). Early childhood adversity and later hypertension: Data from the World Mental Health Survey. Annals of Clinical Psychiatry, 22, 19–28. [PMC free article] [PubMed] [Google Scholar]
- Straus MA (1979). Measuring intra family conflict and violence: The Conflict Tactics Scale. Journal of Marriage and the Family, 41, 75–88. [Google Scholar]
- Turner RJ, & Lloyd DA (1995). Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior, 36, 360–376. [PubMed] [Google Scholar]
- Turner RJ, Wheaton B, & Lloyd DA (1995). The epidemiology of social stress. American Sociological Review, 60, 104–125. [Google Scholar]
- Tyrka AR, Price LH, Kao HT, Porton B, Marsella SA, & Carpenter LL (2010). Childhood maltreatment and telomere shortening: Prelminary support for an effect of early stress on cellular aging. Biological Psychiatry, 67, 531–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, & Jette AM (1994). The disablement process. Social Science & Medicine, 38, 1–14. [DOI] [PubMed] [Google Scholar]
- Vilhjalmsson R (1998). Direct and indirect effects of chronic physical conditions on depression: A preliminary investigation. Social Science & Medicine, 47, 603–611. [DOI] [PubMed] [Google Scholar]


