Key Points
Question
Are female surgeons at increased risk of infertility and pregnancy complications?
Findings
In this national survey study of 850 US surgeons, female surgeons were more likely to delay pregnancy because of training, use assisted reproductive technology, and experience pregnancy complications compared with the female partners of their nonchildbearing colleagues. Surgeons operating more than 12 hours per week during pregnancy also had increased risk of pregnancy complications.
Meaning
Female surgeons may be at increased risk of infertility and pregnancy complications; changing surgical culture and enacting policies that support pregnancy may reduce risk of adverse obstetric outcomes.
This survey study describes the incidence of infertility and pregnancy complications among female surgeons in the US and identifies workplace factors that may be associated with increased risk compared with a sociodemographically similar nonsurgeon population.
Abstract
Importance
While surgeons often delay pregnancy and childbearing because of training and establishing early careers, little is known about risks of infertility and pregnancy complications among female surgeons.
Objective
To describe the incidence of infertility and pregnancy complications among female surgeons in the US and to identify workplace factors associated with increased risk compared with a sociodemographically similar nonsurgeon population.
Design, Setting, and Participants
This self-administered survey questionnaire was electronically distributed and collected from November 2020 to January 2021 through multiple surgical societies in the US and social media among male and female attending and resident surgeons with children. Nonchildbearing surgeons were asked to answer questions regarding the pregnancies of their nonsurgeon partners as applicable.
Exposures
Surgical profession; work, operative, and overnight call schedules.
Main Outcomes and Measures
Descriptive data on pregnancy loss were collected for female surgeons. Use of assisted reproductive technology was compared between male and female surgeons. Pregnancy and neonatal complications were compared between female surgeons and female nonsurgeon partners of surgeons.
Results
A total of 850 surgeons (692 women and 158 men) were included in this survey study. Female surgeons with female partners were excluded because of lack of clarity about who carried the pregnancy. Because the included nonchildbearing population was therefore made up of male individuals with female partners, this group is referred to throughout the study as male surgeons. The median (IQR) age was 40 (36-45) years. Of 692 female surgeons surveyed, 290 (42.0%) had a pregnancy loss, more than twice the rate of the general population. Compared with male surgeons, female surgeons had fewer children (mean [SD], 1.8 [0.8] vs 2.3 [1.1]; P < .001), were more likely to delay having children because of surgical training (450 of 692 [65.0%] vs 69 of 158 [43.7%]; P < .001), and were more likely to use assisted reproductive technology (172 of 692 [24.9%] vs 27 of 158 [17.1%]; P = .04). Compared with female nonsurgeon partners, female surgeons were more likely to have major pregnancy complications (311 of 692 [48.3%] vs 43 of 158 [27.2%]; P < .001), which was significant after controlling for age, work hours, in vitro fertilization use, and multiple gestation (odds ratio [OR], 1.72; 95% CI, 1.11-2.66). Female surgeons operating 12 or more hours per week during the last trimester of pregnancy were at higher risk of major pregnancy complications compared with those operating less than 12 hours per week (OR, 1.57; 95% CI, 1.08-2.26). Compared with female nonsurgeon partners, female surgeons were more likely to have musculoskeletal disorders (255 of 692 [36.9%] vs 29 of 158 [18.4%]; P < .001), nonelective cesarean delivery (170 of 692 [25.5%] vs 24 of 158 [15.3%]; P = .01), and postpartum depression (77 of 692 [11.1%] vs 9 of 158 [5.7%]; P = .04).
Conclusions and Relevance
This national survey study highlighted increased medical risks of infertility and pregnancy complications among female surgeons. With an increasing percentage of women representing the surgical workforce, changing surgical culture to support pregnancy is paramount to reducing the risk of major pregnancy complications, use of fertility interventions, or involuntary childlessness because of delayed attempts at childbearing.
Introduction
As medical school graduate rates approach sex parity,1 women are entering the surgical profession in greater numbers, making up 38% of residents2 and 21% of practicing surgeons in the US.3 Despite increasing numbers, female surgeons continue to face challenges in reconciling work and family demands, particularly early in their careers. Among US surgical residents, national surveys describe pregnancy-related stigma, unmodified work schedules during pregnancy, inconsistent and brief maternity leave options of usually 6 weeks or shorter, and little support for childcare and lactation needs after delivery.4,5 As a result, most female surgeons postpone starting a family until after training.6,7 This timeline coincides with acquiring the diagnosis of advanced maternal age at age 35 years, when the risks of infertility and adverse pregnancy outcomes rise sharply.8 Compared with their male counterparts, female surgeons are more likely to be childless9 but little is known about the risks of infertility and pregnancy complications for female surgeons.
Although prior studies report increased risk of infertility and adverse pregnancy outcomes for physicians, the results are difficult to extrapolate to surgeons, as they do not account for the duration, intensity, and physical nature of surgical training and practice.10,11 The goal of this study is to assess the risk of infertility and pregnancy complications in US female surgeons compared with sociodemographically similar female nonsurgeons, to identify workplace factors that may contribute to increased risk of complications, and to identify areas with the greatest potential for improvement.
Methods
Survey Development
An electronic survey was developed using a cognitive testing approach. Focus groups of male and female faculty and resident surgeons were held at 2 academic teaching hospitals using open-ended scripted questions to solicit views on infertility, barriers to early childbearing, and pregnancy complications. Additional topics were identified through MEDLINE searches combining the keywords pregnancy, childbearing, infertility, assisted reproduction, obstetric outcomes, and pregnancy complications in any specialty. Questions were developed with content expertise from a maternal-fetal medicine specialist (S.R.E.) and validated by collaborators with expertise in qualitative and survey research (E.L.R., M.C-A., Y-Y.H.). The survey instrument was tested with male and female surgeons from multiple institutions and iteratively revised. Participation was voluntary and uncompensated, and completion of the survey was considered implied consent. The survey was approved by the Massachusetts General Brigham institutional review board. All data were deidentified.
Survey Content
The survey (eMethods in the Supplement) collected demographic characteristics, practice information, and work hours. To better understand the impact of race and ethnicity on fertility and pregnancy and neonatal outcomes, participants were asked to report their race and ethnicity using categories defined by the US Office of Civil Rights,12 with options to select multiple categories or to self-report. Personal family goals were assessed by asking participants how many children they had, whether they delayed having children because of training, and if they had the number of children they wanted. Evaluation for and use of assisted reproductive technology (ART), including intrauterine insemination, in vitro fertilization (IVF), and embryo freezing, were assessed.
Factors associated with adverse pregnancy outcomes, including maternal age, work hours, use of IVF, and multiple gestation, were assessed. IVF was selected over other forms of ART because of its association with pregnancy complications related to placental dysfunction.13 Childbearing surgeons answered additional questions regarding call schedules and time spent in the operating room during pregnancy.
The survey explored a range of antepartum, intrapartum, and postpartum complications with associated neonatal outcomes. Complications were grouped into 4 categories based on biologic plausibility and potential impact on the patient and health care system. Major pregnancy complications were defined as those with a need for increased surveillance, with a known association with preterm birth, and for which placental dysfunction is an underlying etiology. Minor pregnancy complications, including musculoskeletal disorders, were defined as non–life-threatening conditions that may have been affected by the physical demands of a surgeon’s work and may have a lasting impact on future health and professional longevity. Intrapartum and postpartum complications were grouped together, given events of labor and delivery may be associated with postpartum complications, including mood disorders.14,15,16 Neonatal complications captured the most serious complications of preterm delivery and unanticipated complications that may occur at term.
Survey Distribution
Survey links were distributed via 7479 emails and approximately 72 000 newsletters from surgical societies between November 2020 and February 2021 to members of the Association of Women Surgeons, Association for Academic Surgery, Society of Asian Academic Surgeons, Society of Black Academic Surgeons, Women in Thoracic Surgery, American College of Surgeons, American College of Surgeons Young Fellows Association, and through targeted social media platforms (a Facebook group of 2700 surgeon mothers and Twitter). The survey was available online for 12 weeks.
Study Participants
Male and female surgeons and surgical trainees in the US were invited to participate. Nonchildbearing surgeons were asked to answer questions regarding their partners’ pregnancies (referred to as female nonsurgeon partners in this study). These women served as a sociodemographically similar control group for pregnancy outcomes because couples with at least 1 surgeon partner share similarities beyond socioeconomic status that carry implications for the timing of childbearing, family planning decisions, and access to ART. Despite a strong medical knowledge base and easy access to health care, surgeons often postpone starting a family and take little time off for childbearing. Long, irregular work hours, prolonged training with little financial compensation during residency, and a professional identity that traditionally minimizes personal life responsibilities17 may contribute to differences in family planning compared with other educated groups.9,18,19 Surgeons who had never attempted pregnancy, male surgeons with female surgeon partners, and female surgeons in same-sex relationships in which the gestational carrier could not be ascertained were excluded.
Statistical Analysis
Hypertensive disorders of pregnancy are a considerable contributor to morbidity and cost, and are associated with many complications explored in this survey.20 To calculate sample size, the risk of hypertensive disorders of pregnancy in female nonsurgeon partners was estimated to be 7.2% based on the risk in the general population in the US Centers for Disease Control and Prevention natality files.21 To detect a difference of 8% among primiparous female surgeons, a sample size of 794 respondents was required to achieve 80% power. A 2-sided z test with pooled variance was used as the test statistic.
To account for differences in factors associated with adverse pregnancy outcomes among nulliparous vs multiparous women, pregnancies resulting in a first live birth were used for comparison between groups. A χ2 analysis was used for categorical variables and t test for continuous variables. Univariate and multivariate logistic regression were used to determine factors associated with having a major pregnancy complication. Variables with a P value less than or equal to .20 were included in multivariate models, and multicollinearity was evaluated using the variance inflation factor. Significance was set at P < .05. Data were analyzed using Stata version 14.0 (StataCorp).
Results
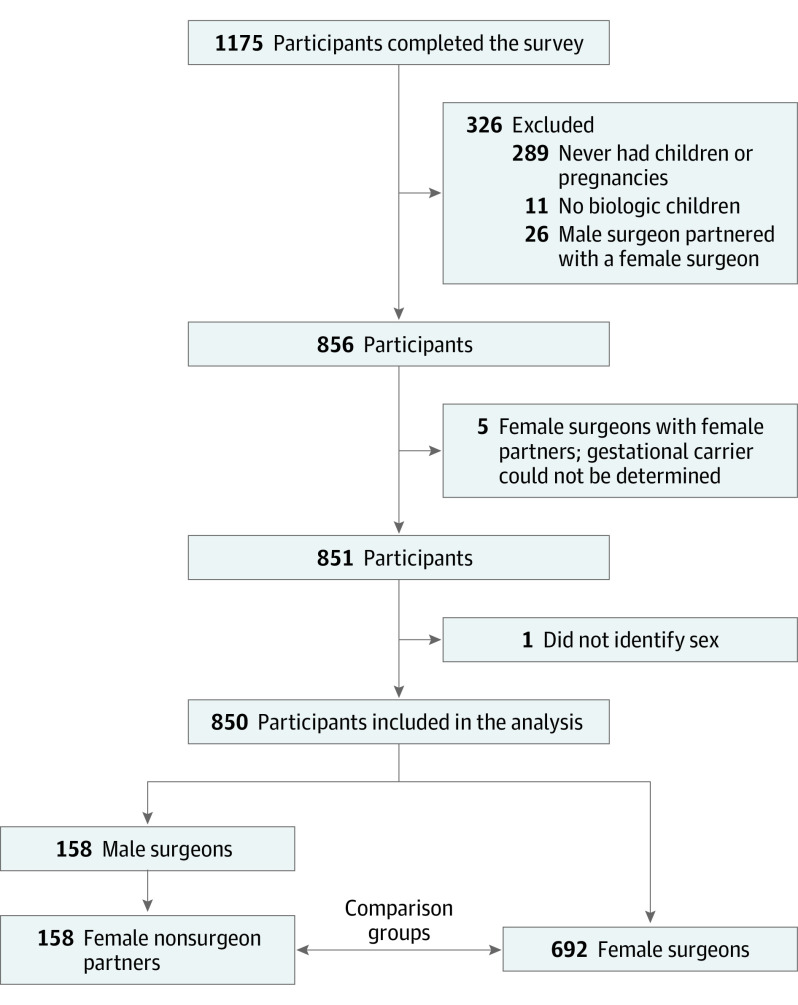
A total of 1175 surveys were completed, and 850 respondents were included in the final analysis (Figure). The median (IQR) age was 40 (36-45) years, and 692 respondents (81.4%) were female. After exclusions, the control group only included childbearing partners of male surgeons. Therefore nonchildbearing surgeons are referred to as male surgeons throughout the study. Of the 692 female surgeons included, 1266 live-birth pregnancies were reported, and 158 male surgeons reported 366 live-birth pregnancies in their female nonsurgeon partners.
Figure. Survey Participants and Exclusion Criteria.
Numbers do not add up due to the intersection of some of the exclusion criteria.
Survey response rate could not be calculated, as 61.2% of respondents accessed the survey through social media or personal communication. Additionally, the number of society-distributed links considerably overestimates the number of potential respondents, as many surgeons are members of multiple societies. Among societies with metrics for email click rates, there were 250 respondents and 533 clicks (46.9%). Compared with male surgeons, female surgeons had fewer biologic children (mean [SD], 1.8 [0.8] vs 2.3 [1.1]; P < .001), were more likely to delay having children because of surgical training (450 of 692 [65.0%] vs 69 of 158 [43.7%]; P < .001), and were more likely to use ART (172 of 692 [24.9%] vs 27 of 158 [17.1%]; P = .04) (Table 1). Compared with female nonsurgeon partners, female surgeons were older at first birth (median [IQR] age, 33 [31-36] years vs 31 [29-34] years; P < .001) and were more likely to work more than 60 hours a week during pregnancy (14 of 158 [56.6%] vs 380 of 692 [10.0%]; P < .001). Among women who reported pregnancy complications, surgeons were less likely to take time off for bed rest (115 of 692 [22.1%] vs 30 of 158 [36.1%]; P = .005). Only 111 female surgeons (16.5%) reduced their work schedules during pregnancy at a mean (SD) of 28.6 (9.3) weeks’ gestation (Table 1). Moreover, 380 of 692 (56.6%) worked more than 60 hours per week and 248 of 671 (37.0%) took more than 6 overnight calls per month during pregnancy. Among female surgeons, 290 (42.0%) experienced a pregnancy loss; among these, 244 (84.4%) had a loss at less than 10 weeks’ gestation, 92 (31.8%) had a loss between 10 and 20 weeks’ gestation, and 11 (3.8%) had a stillbirth (loss at 20 weeks or later). Following a miscarriage, 225 of 336 women (75%) took no time off work, and after a stillbirth, 5 of 11 (45%) took off 1 week or less (Table 2).
Table 1. Characteristics of Female Surgeons vs Male Surgeons and Obstetric Factors Among Female Nonsurgeons vs Female Surgeons.
| Characteristic | No. (%) | P value | |
|---|---|---|---|
| Male surgeons (n = 158) | Female surgeons (n = 692) | ||
| Sociodemographic characteristics of female surgeons and male surgeons (n = 850) | |||
| Relationship status | .59 | ||
| Single, never married | 0 | 4 (0.6) | |
| Married or domestic partnership | 153 (96.8) | 661 (95.5) | |
| Significant other | 0 | 6 (0.9) | |
| Widowed, divorced, or separated and single | 5 (3.2) | 21 (3.0) | |
| Partner occupation | <.001 | ||
| Physician | 51 (33.3) | 88 (13.2) | |
| Surgeon | NAa | 119 (17.2) | |
| Other | 63 (41.2) | 389 (58.3) | |
| Unemployed | 39 (25.5) | 71 (10.6) | |
| Race or ethnicityb | |||
| White | 117 (74.1) | 540 (78.0) | .28 |
| African American/Black | 5 (3.2) | 38 (5.5) | .23 |
| Asian | 25 (15.8) | 109 (15.8) | .98 |
| Native Hawaiian/Pacific Islander | 1 (0.6) | 1 (0.1) | .25 |
| Native American | 2 (1.3) | 0 | .003 |
| Hispanic/Latinx | 8 (5.1) | 24 (3.5) | .34 |
| Otherc | 4 (2.5) | 9 (1.3) | .26 |
| Age, median (IQR), y | 45 (38-52) | 39 (36-44) | <.001 |
| Time since residency, median (IQR), y | 13 (5-18) | 7 (4-12) | <.001 |
| Delayed having children because of surgical training | 69 (43.7) | 450 (65.0) | <.001 |
| No. of biologic children | <.001 | ||
| 1 | 37 (23.4) | 247 (35.7) | |
| 2 | 61 (38.6) | 339 (49.0) | |
| ≥3 | 60 (38.0) | 106 (15.3) | |
| Used ARTd | 27 (17.1) | 172 (24.9) | .04 |
| Title | <.001 | ||
| Instructor | 4 (2.5) | 19 (2.8) | |
| Assistant professor | 42 (26.6) | 224 (32.4) | |
| Associate professor | 31 (19.6) | 85 (12.3) | |
| Full professor | 36 (22.8) | 30 (4.3) | |
| Practicing surgeon in nonacademic setting | 19 (12.0) | 209 (30.2) | |
| Fellow | 9 (5.7) | 46 (6.7) | |
| Resident | 17 (10.8) | 79 (11.4) | |
| Method of survey access | <.001 | ||
| Association of Women Surgeons | 15 (9.5) | 98 (14.2) | |
| Association of Academic Surgery | 52 (32.9) | 70 (10.1) | |
| Society of Asian Academic Surgeons | 7 (4.4) | 8 (1.2) | |
| Society of Black Academic Surgeons | 1 (0.6) | 6 (0.9) | |
| Women in Thoracic Surgery | 1 (0.6) | 13 (1.9) | |
| American College of Surgeons Young Fellows Association | 4 (2.5) | 14 (2.0) | |
| American College of Surgeons bulletin | 8 (5.1) | 33 (4.8) | |
| Facebook surgeon moms’ group | 0 | 334 (48.27) | |
| 11 (7.0) | 37 (5.4) | ||
| Personal communication/notification | 59 (37.3) | 79 (11.4) | |
| Specialty | <.001 | ||
| Breast | 0 | 65 (9.4) | |
| Cardiothoracic | 7 (4.4) | 32 (4.6) | |
| Colorectal | 15 (9.5) | 42 (6.1) | |
| Otolaryngology | 0 | 20 (2.9) | |
| Endocrine | 3 (1.9) | 15 (2.2) | |
| General | 15 (9.5) | 90 (13.0) | |
| Hepatobiliary | 3 (1.9) | 5 (0.7) | |
| Minimally invasive/bariatric | 9 (5.7) | 50 (7.2) | |
| Neurosurgery | 0 | 5 (0.7) | |
| Orthopedic | 4 (2.5) | 18 (2.6) | |
| Pediatric | 30 (19.0) | 46 (6.7) | |
| Plastic | 7 (4.4) | 46 (6.7) | |
| Oncology | 15 (9.5) | 39 (5.6) | |
| Transplant | 3 (1.9) | 10 (1.5) | |
| Trauma/critical care | 19 (12.0) | 87 (12.6) | |
| Urology | 10 (6.3) | 34 (4.9) | |
| Vascular | 6 (3.8) | 34 (4.9) | |
| Resident (not in subspecialty track) | 12 (7.6) | 54 (7.8) | |
| Practice setting | <.001 | ||
| Academic | 123 (77.9) | 392 (56.7) | |
| Community/private practice | 13 (8.2) | 196 (28.3) | |
| Affiliated with academic hospital | 9 (5.7) | 72 (10.4) | |
| Military | 5 (3.2) | 12 (1.7) | |
| Other | 8 (5.1) | 20 (2.9) | |
| Region where child(ren) was/were conceived | .003 | ||
| Northeast | 67 (42.9) | 191 (27.8) | |
| Midwest | 30 (19.1) | 149 (21.7) | |
| South | 39 (24.8) | 208 (30.3) | |
| West | 21 (13.4) | 139 (20.2) | |
| Obstetric factors during pregnancy among female nonsurgeons and female surgeons (n = 850) | |||
| Maternal age at first live birth, median (IQR), ye | 31 (29-34) | 33 (31-36) | <.001 |
| Multiple gestatione | 4 (2.5) | 30 (4.3) | .30 |
| Maternal work hours >60 h/wk during first pregnancye | 14 (10.0) | 380 (56.6) | <.001 |
| Mother took time off for bed rest during first pregnancye,f | 30 (36.1) | 115 (22.1) | .005 |
| Questions for female surgeons only | NA | ||
| Reduced work hours for obstetric indication | NA | 111 (16.5) | |
| No. of overnight calls/mo during pregnancy | NA | ||
| 0 | NA | 66 (9.8) | |
| 2-4 | NA | 156 (23.3) | |
| 4-6 | NA | 201 (30.0) | |
| >6 | NA | 248 (37.0) | |
| Time in operating room/wk during last trimester, h | NA | NA | |
| 0-<8 | NA | 155 (23.1) | |
| 8-<12 | NA | 113 (16.8) | |
| 12-<16 | NA | 138 (20.6) | |
| ≥16 | NA | 265 (39.5) | |
Abbreviations: ART, assisted reproductive technology; IQR, interquartile range; NA, not applicable.
Male surgeons with female surgeon partners were excluded.
To better understand the impact of race and ethnicity on fertility and pregnancy and neonatal outcomes, participants were asked to report their race and ethnicity using categories defined by the US Office of Civil Rights,12 with options to select multiple categories or to self-report.
This category allowed participants to write their own responses. For male surgeons, this category included Iranian American, Middle Eastern, and South Asian. For female surgeons, this category included Arabic, South Asian, Iranian/Pakistani, and Middle Eastern.
ART included intrauterine insemination, in vitro fertilization, and embryo freezing.
Male surgeons reporting on behalf of their female nonsurgeon partners.
Among 83 nonsurgeons and 520 surgeon respondents who reported pregnancy complications.
Table 2. Pregnancy Losses, Pregnancy Complications, and Neonatal Complications Among Female Nonsurgeons and Female Surgeons.
| Variable | No. (%) | P value | |
|---|---|---|---|
| Female nonsurgeons (n = 158) | Female surgeons (n = 692) | ||
| Miscarriages | |||
| Pregnancy loss at <10 wk, mean (SD) | NA | 1.65 (1.37) | NA |
| No. | NA | 244 | |
| Amount of time off work following loss at <10 wk | NA | ||
| 0 d | NA | 196 (80.3) | |
| 1-7 d | NA | 42 (17.2) | |
| 1-2 wk | NA | 3 (1.2) | |
| 3-4 wk | NA | 3 (1.2) | |
| >4 wk | NA | 0 | |
| Pregnancy loss at 10-20 wk, mean (SD) | NA | 1.10 (0.43) | NA |
| No. | NA | 92 | |
| Amount of time off work following loss at 10-20 wk | NA | ||
| 0 d | NA | 56 (60.9) | |
| 1-7 d | NA | 33 (35.9) | |
| 1-2 wk | NA | 0 | |
| 3-4 wk | NA | 2 (2.2) | |
| >4 wk | NA | 1 (1.1) | |
| Pregnancy loss at >20 wk (stillbirth or neonatal demise), mean (SD) | NA | 1.09 (0.30) | NA |
| No. | NA | 11 | |
| Amount of time off work following loss at >20 wk | NA | ||
| 0 d | NA | 2 (18.2) | |
| 1-7 d | NA | 3 (27.3) | |
| 1-2 wk | NA | 1 (9.1) | |
| 3-4 wk | NA | 3 (27.3) | |
| >4 wk | NA | 2 (18.2) | |
| Pregnancy complications | |||
| Major complications | |||
| Preeclampsia | 10 (6.3) | 115 (16.6) | .001 |
| Placental abruption | 9 (5.7) | 30 (4.3) | .46 |
| Placenta previa or accreta | 3 (1.9) | 12 (1.7) | .89 |
| Intrauterine growth restriction | 7 (4.4) | 57 (8.2) | .10 |
| Preterm labor/PPROM | 13 (8.2) | 82 (11.9) | .19 |
| Placental insufficiency/oligohydramnios | 3 (1.9) | 25 (3.6) | .28 |
| Intrapartum and postpartum complications | |||
| Cesarean deliverya | 24 (15.3) | 170 (25.5) | .007 |
| Postpartum hemorrhage | 3 (1.9) | 30 (4.3) | .15 |
| Postpartum depression | 9 (5.7) | 77 (11.1) | .04 |
| Minor complications | |||
| Hyperemesis | 12 (7.6) | 53 (7.7) | .98 |
| Musculoskeletal complaints | 29 (18.4) | 255 (36.9) | <.001 |
| Low back pain | 18 (11.4) | 184 (26.6) | <.001 |
| Carpal tunnel syndrome | 6 (3.8) | 85 (12.3) | .002 |
| Other musculoskeletal pain | 14 (8.9) | 117 (16.9) | .01 |
| Other complication | 15 (9.5) | 90 (13.0) | .23 |
| Neonatal complications | |||
| Preterm delivery <37 wk, No./total No. (%) | 13/71 (18.3) | 69/541 (15.2) | .51 |
| Gestational age at preterm delivery, mean (SD), y | 34.30 (2.65) | 34.35 (2.33) | .95 |
| NICU stay with complication | 25 (15.8) | 108 (15.6) | .95 |
| Blood transfusion | 3 (1.9) | 7 (1.0) | .35 |
| Congenital anomalies | 3 (1.9) | 14 (2.0) | .92 |
| Hypoxia requiring supplemental oxygen | 8 (5.1) | 51 (7.4) | .30 |
| Intraventricular hemorrhage | 0 | 2 (0.3) | .50 |
| Intubation | 6 (3.8) | 17 (2.5) | .35 |
| Meconium aspiration | 2 (1.3) | 4 (0.6) | .35 |
| Necrotizing enterocolitis | 0 | 0 | NA |
| Neonatal sepsis | 1 (0.6) | 0 | .04 |
| Nerve palsy | 1 (0.6) | 2 (0.3) | .51 |
| Pneumothorax | 0 | 5 (0.7) | .28 |
| Seizures | 1 (0.6) | 1 (0.1) | .25 |
| Skeletal fracture | 0 | 0 | NA |
| Therapeutic hypothermia | 1 (0.6) | 2 (0.3) | .51 |
| NICU stay with no complications | 5 (3.2) | 29 (4.2) | .55 |
| Other | 7 (4.4) | 32 (4.6) | .92 |
Abbreviations: NA, not applicable; NICU, neonatal intensive care unit; PPROM, preterm premature rupture of membranes.
Elective cesarean sections were excluded.
Compared with female nonsurgeon partners, female surgeons were more likely to have major pregnancy complications (311 of 692 [48.3%] vs 43 of 158 [27.2%]; P < .001), and this remained significant after controlling for age, hours worked per week, race and ethnicity, IVF usage, and multiple gestation (odds ratio [OR], 1.72; 95% CI, 1.11-2.66; P = .02). Among female surgeons, operating 12 or more hours per week during the last trimester (OR, 1.57; 95% CI, 1.08-2.26; P = .02), maternal age of 35 years or older (OR, 1.66; 95% CI, 1.18-2.32; P = .03), multiple gestation (OR, 3.86; 95% CI, 1.59-9.34; P = .003), and requiring bed rest (OR, 2.33; 95% CI, 1.48-3.67; P < .001) were associated with major pregnancy complications (Table 3).
Table 3. Factors Associated With Major Pregnancy Complications Among Female Nonsurgeons and Female Surgeons and Among Female Surgeons Onlya.
| Variable | Odds ratio (95% CI) | P value |
|---|---|---|
| Factors associated with major pregnancy complications among female nonsurgeons and female surgeons (n = 850) | ||
| Female nonsurgeons | 1 [Reference] | NA |
| Female surgeons | 1.72 (1.11-2.66) | .02 |
| Age, y | ||
| <35 | 1 [Reference] | NA |
| ≥35 | 1.54 (1.12-2.12) | .007 |
| Hours of work/wk | ||
| ≤60 | 1 [Reference] | NA |
| >60 | 1.29 (0.94-1.77) | .11 |
| Race or ethnicityb | ||
| White | 1 [Reference] | NA |
| Asian/Pacific Islander | 1.05 (0.71-1.56) | .44 |
| Underrepresented groupsc | 1.09 (0.64-1.84) | .74 |
| Having used IVF | 1.45 (0.97-2.16) | .06 |
| Having multiple gestation | 3.56 (1.55-8.19) | .003 |
| Subgroup analysis of female surgeons: factors associated with major pregnancy complications (n = 692) a | ||
| Age, y | ||
| <35 | 1 [Reference] | NA |
| ≥35 | 1.66 (1.18-2.32) | .003 |
| Hours of work/wk | ||
| ≤60 | 1 [Reference] | NA |
| >60 | 1.25 (0.87-1.79) | .23 |
| Frequency of overnight call during pregnancy/mo, No. | ||
| <4 | 1 [Reference] | NA |
| ≥4 | 0.96 (0.67-1.38) | .85 |
| Hours/wk operating during last trimester | ||
| <12 | 1 [Reference] | NA |
| ≥12 | 1.57 (1.08-2.26) | .02 |
| Practice setting | ||
| Community/private practice/military/other | 1 [Reference] | NA |
| Academic/affiliated with academic center | 0.87 (0.62-1.22) | .43 |
| Race or ethnicityb | ||
| White | 1 [Reference] | NA |
| Asian/Pacific Islander | 0.92 (0.54-1.43) | .72 |
| Underrepresented groupsc | 0.80 (0.43-1.46) | .47 |
| Required bed rest during pregnancy | 2.33 (1.48-3.67) | <.001 |
| Multiple gestation | 3.86 (1.59-9.34) | .003 |
Abbreviation: IVF, in vitro fertilization; NA, not applicable.
Major pregnancy complications included preeclampsia, placental abruption, placenta previa or accreta, intrauterine growth restriction, placental insufficiency or oligohydramnios, spontaneous preterm labor, or preterm premature rupture of membranes.
To better understand the impact of race and ethnicity on fertility and pregnancy and neonatal outcomes, participants were asked to report their race and ethnicity using categories defined by the US Office of Civil Rights,12 with options to select multiple categories or to self-report.
For the adjusted analysis, race and ethnicity groups were consolidated to evaluate whether being part of an underrepresented racial or ethnic group had an affect on outcomes. This item includes individuals who identified as Black, Hispanic or Latinx, Native American, Iranian American, Middle Eastern, South Asian, Arabic, Iranian/Pakistani, and Middle Eastern. These groups have been identified by the Association of American Medical Colleges as underrepresented in medicine.
Compared with female nonsurgeon partners, female surgeons were more likely to have musculoskeletal disorders (255 of 692 [36.9%] vs 29 of 158 [18.4%]; P < .001), nonelective cesarean delivery (170 of 692 [25.5%] vs 24 of 158 [15.3%]; P = .01), and postpartum depression (77 of 692 [11.1%] vs 9 of 158 [5.7%]; P = .04) (Table 2). Among female surgeons, postpartum depression was independently associated with having a major pregnancy complication (OR, 2.23; 95% CI, 1.35-3.69) after controlling for age, race and ethnicity, practice setting, and weekly work hours. Neonatal outcomes were similar between groups, with 69 of 692 (15.2%) having a preterm birth at less than 37 weeks’ gestation and 108 of 692 (15.6%) having an infant requiring neonatal intensive care unit admission for a complication.
Discussion
In this survey study, female surgeons reported high rates of miscarriage, following which few took time off from work. This study revealed a higher use of ART and greater number of pregnancy complications among female surgeons compared with sociodemographically similar female nonsurgeons. Although long operative hours were found to be independently associated with pregnancy complications, few female surgeons reduced their work schedules. Challenges associated with childbearing may negatively impact the workforce, with surgeons who perceive a conflict between work life and home life having lower career satisfaction and professional longevity.22 To our knowledge, this is the first study of infertility and pregnancy complications in surgeons that controls for the sociodemographic characteristics of a surgeon household by comparing outcomes of female surgeons with those of nonsurgeon partners of surgeons.
Despite recognized infertility and obstetric risks after age 35 years,8 female physicians have historically delayed pregnancy until completion of training.7,23 In this study, women were more likely than their male colleagues to postpone having children until after surgical training, well past the national median age at first birth (30 years) among mothers with advanced degrees.24 Given the length of surgical training, older maternal age likely contributes to the disproportionate number of female surgeons using ART. In previous generations, male surgeons more commonly had stay-at-home spouses who provided childcare, perhaps explaining historic differences in childbearing patterns between male surgeons and female surgeons.9 With dual-career couples now representing most of the professional sector,25 the disparity in age at first pregnancy between female surgeons and nonsurgeon partners of male surgeons can no longer be explained solely by differences in access to childcare and professional goals. The US and Papua New Guinea are the only 2 countries without federally mandated paid parental leave.26 Most US female surgeons rely on their employer for this benefit, but only half of top-ranked medical schools offer paid leave27 and 33% to 65% of US surgical training programs lack clear maternity leave policies.4,5 The absence of compensated leave may discourage young female surgeons from having children until later in their career when they can shoulder the monetary burden. Cultural barriers against childbearing compound these constraints and are also observed in countries with statutory paid leave, suggesting that pregnant residents may be concerned about damage to their professional reputation,23,28 negative perceptions of childbearing trainees by surgical program directors,5 inadequate lactation support,4,29,30 loss of referral patterns for practicing surgeons,29 and perceived loss of career opportunities after parental leave.30,31
In this study, 42% of female surgeons reported at least 1 pregnancy loss, more than double the rate reported in the general population of women aged 30 to 40 years.32 This higher incidence cannot likely be explained by increased ART use, as ART is not clearly associated with early pregnancy loss.33 Studies suggest consistent night shift work and working more than 40 hours a week are associated with higher risks of miscarriage.34,35 Although work schedules prior to miscarriage were not specifically evaluated, it is likely that many female surgeons exceeded these parameters, given the substantial duty hours and call obligations that were reported during first pregnancies. Limiting overnight shifts and work hours for pregnant surgeons may mitigate pregnancy losses. Moreover, perinatal loss is associated with considerable psychologic impact, similar to complicated grief experienced after the loss of a first-degree relative.36,37,38,39 However, 75% of female surgeons in this study took no time off work after miscarriages and nearly half took off 1 week or less after a stillbirth. Women physicians may be reticent to request time off to cope with pregnancy losses because of concern for loss of reputation or burdening their colleagues.40 Surgical practices and training programs should support bereavement after pregnancy loss by assuring an empathic environment and appropriate time off work to process grief and seek support.
Women working in physically demanding environments are known to have higher rates of pregnancy complications. Large multicenter studies and meta-analyses suggest adverse pregnancy outcomes are associated with working more than 40 hours a week, prolonged standing, high fatigue scores, and shift and night work.41,42,43 Similar findings were identified among surgical subspecialists. Orthopedic surgeons working more than 60 hours a week were shown to have a greater risk of preterm delivery compared with age-matched population controls.44 Female urologists have been shown to have a higher prevalence of pregnancy complications compared with women in the lowest income bracket in the US.45 These findings are notable given that higher education levels and socioeconomic status are typically associated with decreased pregnancy complications.46 Despite using a narrower definition of major pregnancy complications (ie, excluding obstetric complications like postpartum hemorrhage, non–life-threatening conditions like hyperemesis, and conditions unlikely to be related to work environment like gestational diabetes), the current study demonstrates a higher major pregnancy complication rate (48.3%) than that observed in both subspecialty studies (31% in orthopedic surgeons and 25% in urologists).44,45 This may be explained by an a priori approach limiting analysis to nulliparous women who inherently carry higher risk of complications and are physiologically different from multiparous women.47,48 Compared with female nonsurgeon partners, female surgeons had 1.7 higher odds of pregnancy complications, with the greatest risk observed in women operating 12 or more hours per week. With US surgeons averaging 16 operative hours weekly,49 the physical working conditions of the profession likely have a substantial impact on pregnancy outcomes. This study demonstrates that female surgeons may be at higher risk of postpartum depression after major pregnancy complications, a condition that carries long-term effects for child development and maternal mental health.50 It is essential for institutions to have heightened awareness for surgeons at risk and be prepared to offer time away from training and practice as well as support through timely referrals to mental health resource.
Although few data have been published on musculoskeletal pain in pregnant surgeons,43 this study demonstrates that more than one-third of gravid surgeons experience musculoskeletal disorders. This finding is expected given that the frequency of low back and pelvic pain in the general obstetric population51 is superimposed on a high background prevalence of musculoskeletal injuries among nonpregnant surgeons.52 An evidence-based applied ergonomic program is critical to optimize modifiable factors in the operating room.52 Surgeons who do not have sustained benefit from ergonomic intervention may need to reduce or cease operating time during pregnancy to ensure musculoskeletal injuries do not result in long-term disability.52
Preterm birth was higher in both groups compared with the rate of 9.3% in the general population of similar maternal age.53 This may be explained in part by greater use of ART services among surgeon couples, with rates 30% to 90% higher than the national mean of 13%.54 ART, particularly IVF, is known to contribute to worse neonatal outcomes, including infants with very low birthweight and infants who are small for gestational age, preterm deliveries, and need for neonatal intensive care unit admissions.55 This underscores the considerable morbidity associated with delayed childbearing, which may carry long-term implications for the health of the child.
Limitations
This study had limitations. An a priori decision was made to use a multimodal approach to reach as many surgeons as possible, focusing on groups and societies with ethnic and racial diversity and younger membership to broadly canvass surgeons likely to be in their childbearing years. This distribution method precludes calculation of a response rate and may be subject to sampling bias. However, the balanced geographic distribution, practice settings, and subspecialty types of the respondent cohort suggest it is a contemporary cross-section of the US surgeon community. Recall bias, specifically regarding details of the pregnancy experience, may have resulted in reporting inaccuracies, particularly for nonchildbearing surgeons reporting on behalf of their partners. Musculoskeletal disorders may have been underreported for female nonsurgeons, who may have been less likely to have these complications impact their work performance compared with female surgeons. This was mitigated by limiting questions asked of nonsurgeon participants to significant clinical outcomes, such as infertility treatments, pregnancy complications, and neonatal complications. Details regarding reduction in work schedules and miscarriages were limited to childbearing participants. Maternal recall of obstetric complications is typically excellent with high correlation with medical records (r, 0.89-0.95).56,57 Additionally, obstetric care has advanced over time, and it is possible that treatment has changed for recent pregnancies compared with earlier ones. However, the difference between respondents’ median current age and age at first birth is small enough that major changes in care that impact outcome are unlikely.
Conclusions
This study highlights the increased risks of infertility and major pregnancy complications among childbearing surgeons. With a lack of clear standardized guidelines or federally mandated paid maternity leave, we propose recommendations for US residency programs and surgical departments to facilitate pregnancy earlier in a surgeon’s career to reduce pregnancy-related health risks (Box).5,43,58,59,60,61 The monetary costs associated with these proposed solutions must be weighed against the human and workforce costs of maintaining the status quo. Importantly, changing surgical culture to legitimize pregnancy and motherhood is paramount to reducing the risk of major pregnancy complications, use of fertility interventions, or involuntary childlessness associated with delayed attempts at childbearing.
Box. Recommendations for Residency Programs and Surgical Departments and Practices to Address the Needs of Early-Career Surgeon Mothers and Mitigate Pregnancy-Associated Health Risks.
Recommendations and Practices
-
Training programs should include policies to support pregnant and expecting trainees and should be clearly written and openly discussed to avoid misunderstandings from other members of the surgical team. Provision of such support during residency demonstrates a commitment from the department to support parenthood during training, enforces that time for parental bonding is an expectation, and encourages trainees that are ready to start families that they do not need to wait until the end of a 5- to 7-y residency to have children, as younger maternal age may reduce use of assisted reproductive technology and lower future complication rates. These policies should include:
Schedule flexibility for pregnant trainees, including less demanding rotations scheduled close to term and on initial return after childbirth. This may mitigate potential risks to maternal and fetal health for pregnant residents and help returning trainees adjust to balancing new family and work priorities.
At least 6 wk of paid parental leave exclusive of vacation time and consistent with new recommendations from the American Board of Medical Specialties and the Accreditation Council for Graduate Medical Education58 without need to extend training should be provided. To allow healthy time for maternal care and parental bonding, residents should be encouraged to take the full 12 wk of leave recommended by the American Academy of Pediatrics.59 To avoid compromising education requirements and meet American Board of Surgery eligibility,60 extension of training may be necessary and should be facilitated.
Nonchildbearing residents should be encouraged to take full parental leave. All parents should have time off to bond with a new infant, including those who have children by adoption or surrogacy. Normalization of parental leave for both male residents and female residents helps override the narrative that parenting is an issue exclusive to women and changes surgical culture to accept time away for family needs.
Fellowship programs should be prepared to delay the start of training for trainees who need to extend training after maternity leave. For a 12-wk maternity leave, such a delay would be unlikely to exceed several weeks, given most fellowships start August 1 of each year.
Service coverage during leave should be provided by moonlighting physicians or advance practice clinicians while residents are on leave to avoid resentment from colleagues asked to take over additional work and to facilitate culture change to reduce stigma associated with childbearing.
Pregnant residents should not be asked to make up call shifts missed during maternity leave, as increased work hours or overnight shifts may heighten risk of pregnancy complications.
Nursing residents should be supported after delivery with written policies that permit cross-coverage during long cases and education for faculty regarding the duration and frequency new mothers require to pump milk.
The American Board of Surgery requires residents to complete training by August 31 to take the qualifying examination, which is currently only offered once a year.61 Offering the examination more than once a year would reduce delays in board certification because of childbearing and parental leave.
Many academic research programs require research in the middle of clinical training. Although many program directors and trainees consider this an ideal time to start a family,5 pregnancies cannot be precisely scheduled, and this timeline may not align with residents’ personal circumstances. For female trainees who choose to have children after residency, research prolongs training and may increase risk of infertility. Research during residency should be optional and timing should be flexible.
Mentors of the same sex, ideally another surgeon mother, can offer experience-based advice in balancing professional and personal commitments, help set realistic expectations, and provide a safe setting to discuss challenges.
-
Institutions and practices should foster a supportive work environment through coverage plans for pregnancy and leave for practicing physicians. These policies should be clearly outlined in a surgeons’ contracts and should include the following:
Pregnant surgeons may reduce their operative commitments in their third trimester without financial penalty. Multiple-gestation pregnancies may require reduction in operative schedules earlier in the pregnancy.
A minimum of 12 wk of paid parental leave should be offered, exclusive of vacation time. This should be a separate allocation than the disability that may be required during pregnancy.
Surgeons should not be required to make up missed calls or sustain revenue losses that result from leave. Productivity bonuses, which may constitute a considerable portion of take-home wages, should reflect prepregnancy performance.
Additional clinical duties taken by colleagues should be compensated to avoid resentment.
Surgeons returning to clinical practice after maternity leave should have a defined plan to restore clinical work after leave.
-
Both trainees and practicing physicians should be provided with the following:
A substantial proportion of surgeons require ART, which involves considerable expense and frequent imaging, procedures, and laboratory work. Surgeons should be encouraged to take appropriate time off from clinical duties during such treatment. Institutions in states without mandatory comprehensive ART insurance coverage should offer financial aid or additional insurance coverage for ART.
Mothers who choose to breastfeed should be supported with dedicated private lactation space with proximity to the operating room and clinical spaces. These facilities should include a high-speed pump, sink, microwave, and a refrigerator for storing milk. Operative and clinic schedules should be adjusted to accommodate time for postpartum surgeons to pump and store milk.
Teaching hospitals and larger institutions should provide onsite childcare with priority for trainees who have the longest workhours and the least scheduling flexibility. The fee schedule should be prorated to better accommodate trainees’ salaries.
Formal ergonomic consultation should be obtained for pregnant surgeons to avoid musculoskeletal injury in the operating room.
Fetal dosimeters should be provided and checked monthly to demonstrate adherence to established limits of less than 5 millisieverts for the gestation. Pregnant surgeons should not participate in hyperthermic intraperitoneal chemotherapy operating rooms and should use 3 layers of gloves when handling chemotherapeutics. Surgeons using methyl methacrylate should be provided surgical hooded helmets in operating rooms with laminar airflow for proper ventilation.43
Timely referral to mental health resources for postpartum depression, with appropriate time away from practice or training for treatment, should be provided.
eMethods. Sample survey
References
- 1.Association of American Medical Colleges . US medical school applicants, matriculants, and graduates by gender, academic year, 2018-2019. Accessed February 27, 2021. https://www.aamc.org/media/43351/download
- 2.Association of American Medical Colleges . The state of women in academic medicine 2018-2019: percentage of women residents by specialty, 2018. Accessed February 27,2021. https://www.aamc.org/data-reports/data/2018-2019-state-women-academic-medicine-exploring-pathways-equity
- 3.American College of Surgeons. 2018 ACS governors survey: gender inequality and harassment remain a challenge in surgery. Accessed March 1, 2021. https://bulletin.facs.org/2019/09/2018-acs-governors-survey-gender-inequality-and-harassment-remain-a-challenge-in-surgery/
- 4.Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surg. 2018;153(7):644-652. doi: 10.1001/jamasurg.2018.0153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandler BJ, Tackett JJ, Longo WE, Yoo PS. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program directors. J Am Coll Surg. 2016;222(6):1090-1096. doi: 10.1016/j.jamcollsurg.2015.12.004 [DOI] [PubMed] [Google Scholar]
- 6.Turner PL, Lumpkins K, Gabre J, Lin MJ, Liu X, Terrin M. Pregnancy among women surgeons: trends over time. Arch Surg. 2012;147(5):474-479. doi: 10.1001/archsurg.2011.1693 [DOI] [PubMed] [Google Scholar]
- 7.Pham DT, Stephens EH, Antonoff MB, et al. Birth trends and factors affecting childbearing among thoracic surgeons. Ann Thorac Surg. 2014;98(3):890-895. doi: 10.1016/j.athoracsur.2014.05.041 [DOI] [PubMed] [Google Scholar]
- 8.Berkowitz GS, Skovron ML, Lapinski RH, Berkowitz RL. Delayed childbearing and the outcome of pregnancy. N Engl J Med. 1990;322(10):659-664. doi: 10.1056/NEJM199003083221004 [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146(2):211-217. doi: 10.1001/archsurg.2010.310 [DOI] [PubMed] [Google Scholar]
- 10.Scully RE, Stagg AR, Melnitchouk N, Davids JS. Pregnancy outcomes in female physicians in procedural versus non-procedural specialties. Am J Surg. 2017;214(4):599-603. doi: 10.1016/j.amjsurg.2017.06.016 [DOI] [PubMed] [Google Scholar]
- 11.Miller NH, Katz VL, Cefalo RC. Pregnancies among physicians. a historical cohort study. J Reprod Med. 1989;34(10):790-796. [PubMed] [Google Scholar]
- 12.US Department of the Interior Office of Civil Rights . Standards for maintaining, collecting, and presenting federal data on race and ethnicity. Accessed April 30, 2021. https://www.doi.gov/pmb/eeo/directives/race-data
- 13.Johnson KM, Hacker MR, Thornton K, Young BC, Modest AM. Association between in vitro fertilization and ischemic placental disease by gestational age. Fertil Steril. 2020;114(3):579-586. doi: 10.1016/j.fertnstert.2020.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bonacquisti A, Geller PA, Patterson CA. Maternal depression, anxiety, stress, and maternal-infant attachment in the neonatal intensive care unit. J Reprod Infant Psychol. 2020;38(3):297-310. doi: 10.1080/02646838.2019.1695041 [DOI] [PubMed] [Google Scholar]
- 15.American College of Obstetricians and Gynecologists . ACOG Committee opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;131(5):e140-e150. doi: 10.1097/AOG.0000000000002633 [DOI] [PubMed] [Google Scholar]
- 16.Kendig S, Keats JP, Hoffman MC, et al. Consensus bundle on maternal mental health: perinatal depression and anxiety. Obstet Gynecol. 2017;129(3):422-430. doi: 10.1097/AOG.0000000000001902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kellogg KC, Breen E, Ferzoco SJ, Zinner MJ, Ashley SW. Resistance to change in surgical residency: an ethnographic study of work hours reform. J Am Coll Surg. 2006;202(4):630-636. doi: 10.1016/j.jamcollsurg.2005.11.024 [DOI] [PubMed] [Google Scholar]
- 18.Pew Research Center . The educational gap in motherhood is shrinking. Accessed March 4, 2021. https://www.pewresearch.org/social-trends/2018/01/18/theyre-waiting-longer-but-u-s-women-today-more-likely-to-have-children-than-a-decade-ago/pstl_1-18-18-motherhood-04//
- 19.Simoni MK, Mu L, Collins SC. Women’s career priority is associated with attitudes towards family planning and ethical acceptance of reproductive technologies. Hum Reprod. 2017;32(10):2069-2075. doi: 10.1093/humrep/dex275 [DOI] [PubMed] [Google Scholar]
- 20.Hao J, Hassen D, Hao Q, et al. Maternal and infant health care costs related to preeclampsia. Obstet Gynecol. 2019;134(6):1227-1233. doi: 10.1097/AOG.0000000000003581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Centers for Disease Control and Prevention . Natality information: live births. Accessed February 15, 2021. https://wonder.cdc.gov/natality.html
- 22.Dyrbye LN, Freischlag J, Kaups KL, et al. Work-home conflicts have a substantial impact on career decisions that affect the adequacy of the surgical workforce. Arch Surg. 2012;147(10):933-939. doi: 10.1001/archsurg.2012.835 [DOI] [PubMed] [Google Scholar]
- 23.Kin C, Yang R, Desai P, Mueller C, Girod S. Female trainees believe that having children will negatively impact their careers: results of a quantitative survey of trainees at an academic medical center. BMC Med Educ. 2018;18(1):260. doi: 10.1186/s12909-018-1373-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Livingston G. For most highly educated women, motherhood doesn’t start until the 30s. Accessed February 14, 2021. https://www.pewresearch.org/fact-tank/2015/01/15/for-most-highly-educated-women-motherhood-doesnt-start-until-the-30s/
- 25.Azil A, Bennett B, Nadeau, M-C, Zucker J. How dual-career couples find fulfillment at work. Accessed February 13, 2021. https://www.mckinsey.com/business-functions/organization/our-insights/how-dual-career-couples-find-fulfillment-at-work#
- 26.Rubin R. Despite potential health benefits of maternity leave, US lags behind other industrialized countries. JAMA. 2016;315(7):643-645. doi: 10.1001/jama.2015.18609 [DOI] [PubMed] [Google Scholar]
- 27.Itum DS, Oltmann SC, Choti MA, Piper HG. Access to paid parental leave for academic surgeons. J Surg Res. 2019;233:144-148. doi: 10.1016/j.jss.2018.01.001 [DOI] [PubMed] [Google Scholar]
- 28.Willett LL, Wellons MF, Hartig JR, et al. Do women residents delay childbearing due to perceived career threats? Acad Med. 2010;85(4):640-646. doi: 10.1097/ACM.0b013e3181d2cb5b [DOI] [PubMed] [Google Scholar]
- 29.Scully RE, Davids JS, Melnitchouk N. Impact of procedural specialty on maternity leave and career satisfaction among female physicians. Ann Surg. 2017;266(2):210-217. doi: 10.1097/SLA.0000000000002196 [DOI] [PubMed] [Google Scholar]
- 30.Merchant SJ, Hameed SM, Melck AL. Pregnancy among residents enrolled in general surgery: a nationwide survey of attitudes and experiences. Am J Surg. 2013;206(4):605-610. doi: 10.1016/j.amjsurg.2012.04.005 [DOI] [PubMed] [Google Scholar]
- 31.Rogers AC, Wren SM, McNamara DA. Gender and specialty influences on personal and professional life among trainees. Ann Surg. 2019;269(2):383-387. doi: 10.1097/SLA.0000000000002580 [DOI] [PubMed] [Google Scholar]
- 32.Magnus MC, Wilcox AJ, Morken N-H, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019;364:l869. doi: 10.1136/bmj.l869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Torrealday S. Is the fertility treatment itself a risk factor for early pregnancy loss? Curr Opin Obstet Gynecol. 2014;26(3):174-180. doi: 10.1097/GCO.0000000000000064 [DOI] [PubMed] [Google Scholar]
- 34.Cai C, Vandermeer B, Khurana R, et al. The impact of occupational shift work and working hours during pregnancy on health outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol. 2019;221(6):563-576. doi: 10.1016/j.ajog.2019.06.051 [DOI] [PubMed] [Google Scholar]
- 35.Zhu JL, Hjollund NH, Andersen AM, Olsen J. Shift work, job stress, and late fetal loss: the National Birth Cohort in Denmark. J Occup Environ Med. 2004;46(11):1144-1149. doi: 10.1097/01.jom.0000145168.21614.21 [DOI] [PubMed] [Google Scholar]
- 36.Farren J, Jalmbrant M, Ameye L, et al. Post-traumatic stress, anxiety and depression following miscarriage or ectopic pregnancy: a prospective cohort study. BMJ Open. 2016;6(11):e011864. doi: 10.1136/bmjopen-2016-011864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kulathilaka S, Hanwella R, de Silva VA. Depressive disorder and grief following spontaneous abortion. BMC Psychiatry. 2016;16:100. doi: 10.1186/s12888-016-0812-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hunfeld JA, Wladimiroff JW, Passchier J. The grief of late pregnancy loss. Patient Educ Couns. 1997;31(1):57-64. doi: 10.1016/S0738-3991(97)01008-2 [DOI] [PubMed] [Google Scholar]
- 39.Kersting A, Wagner B. Complicated grief after perinatal loss. Dialogues Clin Neurosci. 2012;14(2):187-194. doi: 10.31887/DCNS.2012.14.2/akersting [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glauser W. Is the culture of medicine contributing to miscarriages among female physicians? CMAJ. 2019;191(44):E1229-E1230. doi: 10.1503/cmaj.1095821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saurel-Cubizolles MJ, Zeitlin J, Lelong N, Papiernik E, Di Renzo GC, Bréart G; Europop Group . Employment, working conditions, and preterm birth: results from the Europop case-control survey. J Epidemiol Community Health. 2004;58(5):395-401. doi: 10.1136/jech.2003.008029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mozurkewich EL, Luke B, Avni M, Wolf FM. Working conditions and adverse pregnancy outcome: a meta-analysis. Obstet Gynecol. 2000;95(4):623-635. doi: 10.1097/00006250-200004000-00029 [DOI] [PubMed] [Google Scholar]
- 43.Anderson M, Goldman RH. Occupational reproductive hazards for female surgeons in the operating room: a review. JAMA Surg. 2020;155(3):243-249. doi: 10.1001/jamasurg.2019.5420 [DOI] [PubMed] [Google Scholar]
- 44.Hamilton AR, Tyson MD, Braga JA, Lerner LB. Childbearing and pregnancy characteristics of female orthopaedic surgeons. J Bone Joint Surg Am. 2012;94(11):e77-e79. doi: 10.2106/JBJS.K.00707 [DOI] [PubMed] [Google Scholar]
- 45.Lerner LB, Stolzmann KL, Gulla VD. Birth trends and pregnancy complications among women urologists. J Am Coll Surg. 2009;208(2):293-297. doi: 10.1016/j.jamcollsurg.2008.10.012 [DOI] [PubMed] [Google Scholar]
- 46.Hegelund ER, Poulsen GJ, Mortensen LH. Educational attainment and pregnancy outcomes: a Danish register-based study of the influence of childhood social disadvantage on later socioeconomic disparities in induced abortion, spontaneous abortion, stillbirth and preterm delivery. Matern Child Health J. 2019;23(6):839-846. doi: 10.1007/s10995-018-02704-1 [DOI] [PubMed] [Google Scholar]
- 47.Bai J, Wong FW, Bauman A, Mohsin M. Parity and pregnancy outcomes. Am J Obstet Gynecol. 2002;186(2):274-278. doi: 10.1067/mob.2002.119639 [DOI] [PubMed] [Google Scholar]
- 48.Chauhan SP, Rice MM, Grobman WA, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network . Neonatal and maternal composite adverse outcomes among low-risk nulliparous women compared with multiparous women at 39-41 weeks of gestation. Obstet Gynecol. 2020;136(3):450-457. doi: 10.1097/AOG.0000000000003951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463-471. doi: 10.1097/SLA.0b013e3181ac4dfd [DOI] [PubMed] [Google Scholar]
- 50.Pearlstein T, Howard M, Salisbury A, Zlotnick C. Postpartum depression. Am J Obstet Gynecol. 2009;200(4):357-364. doi: 10.1016/j.ajog.2008.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Richards E, van Kessel G, Virgara R, Harris P. Does antenatal physical therapy for pregnant women with low back pain or pelvic pain improve functional outcomes? a systematic review. Acta Obstet Gynecol Scand. 2012;91(9):1038-1045. doi: 10.1111/j.1600-0412.2012.01462.x [DOI] [PubMed] [Google Scholar]
- 52.Epstein S, Sparer EH, Tran BN, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. 2018;153(2):e174947. doi: 10.1001/jamasurg.2017.4947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ferré C, Callaghan W, Olson C, Sharma A, Barfield W. Effects of maternal age and age-specific preterm birth rates on overall preterm birth rates—United States, 2007 and 2014. MMWR Morb Mortal Wkly Rep. 2016;65(43):1181-1184. doi: 10.15585/mmwr.mm6543a1 [DOI] [PubMed] [Google Scholar]
- 54.US Centers for Disease Control and Prevention . 2018Assisted Reproductive Technology Fertility Clinic Success Rates Report. Accessed March 3, 2021. https://www.cdc.gov/art/pdf/2018-report/ART-2018-Clinic-Report-Full.pdf
- 55.Mukhopadhaya N, Arulkumaran S. Reproductive outcomes after in-vitro fertilization. Curr Opin Obstet Gynecol. 2007;19(2):113-119. doi: 10.1097/GCO.0b013e32807fb199 [DOI] [PubMed] [Google Scholar]
- 56.Bat-Erdene U, Metcalfe A, McDonald SW, Tough SC. Validation of Canadian mothers’ recall of events in labour and delivery with electronic health records. BMC Pregnancy Childbirth. 2013;13(suppl 1):S3. doi: 10.1186/1471-2393-13-S1-S3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sou SC, Chen WJ, Hsieh WS, Jeng SF. Severe obstetric complications and birth characteristics in preterm or term delivery were accurately recalled by mothers. J Clin Epidemiol. 2006;59(4):429-435. doi: 10.1016/j.jclinepi.2005.08.010 [DOI] [PubMed] [Google Scholar]
- 58.Buyske, J. Supporting early career physicians by collaborating with stakeholders. Accessed March 3, 20201. https://www.abms.org/news-events/supporting-early-career-physicians-by-collaborating-with-stakeholders/.
- 59.Dodson NA, Talib HJ. Paid parental leave for mothers and fathers can improve physician wellness. Accessed March 3, 2021. https://www.aappublications.org/news/2020/07/01/wellness070120/.
- 60.The American Board of Surgery . Leave policy-general surgery. Accessed March 3, 2021. https://www.absurgery.org/default.jsp?policygsleave
- 61.The American Board of Surgery . Qualifying exam. Accessed March 3, 2021. https://www.absurgery.org/default.jsp?certgsqe.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Sample survey