Abstract
Affective dynamics have been increasingly recognized as important indicators of emotional health and well-being. Depression has been associated with altered affective dynamics, but little is known about how daily life affective dynamics predict depression’s naturalistic course. We investigated positive and negative affective dynamics (e.g., inertia, variability, and instability) among adults with depressive disorders (N = 60) and healthy controls (N = 38) in both cross-sectional and prospective analyses predicting weekly depression symptoms over 6 months. Relative to controls, depressed individuals showed elevated daily negative affect (NA) and NA variability along with decreased positive affect (PA). However, groups did not significantly differ on other affective dynamic indices. Based on multivariate prospective analyses of depressed individuals (follow-up N = 36), higher daily NA and lower daily PA were independently associated with higher and average weekly depressive symptom severity over the subsequent 6 months. Exploratory analyses of depression symptom trajectory shape revealed that higher NA and PA variability, NA inertia, and NA instability all predicted an initial increase and eventual return to higher depression symptom levels over the 6-month follow-up period. Daily life affective dynamics may have utility for predicting the naturalistic course of depression, which may help guide interventions targeting affective dynamics in vulnerable individuals.
Electronic supplementary material
The online version of this article (10.1007/s42761-020-00014-w) contains supplementary material, which is available to authorized users.
Keywords: Depression, Affective dynamics, Symptom trajectory, Depression severity
The dynamic nature of emotions (Frijda, 2007) has been conceptualized as a key aspect of psychological flexibility, which reflects the capacity to respond appropriately to environmental challenges and opportunities (Kashdan & Rottenberg, 2010). Affective dynamics, or the fluctuations in emotions over time to meet environmental needs, are consistently related to well-being and mental health in cross-sectional studies (e.g., see Houben, Van den Noortgate, & Kuppens, 2015 meta-analysis). However, less is known about how day-to-day emotional fluctuations might impact well-being and psychopathology over longer periods of time (e.g., months and years). Theoretical reviews by Hollenstein, Lichtwarck-Aschoff, and Potworowski (2013) and Hollenstein (2015) suggest a dynamic interplay between real-time affective dynamics and adaptive development over longer periods of time, such as moods, personality traits, and psychopathology (e.g., Koval, Kuppens, Allen, & Sheeber, 2012). Therefore, understanding the nature of affective dynamics not only reveals information about normative variation in emotional health (e.g., Koval et al., 2015; Suls, Green, & Hillis, 1998), but also helps elucidate the nature and course of affective disorders, such as depression. Specifically, experience sampling methodologies (ESM) can clarify what aspects of daily affective dynamics are implicated in depression course in an ecologically valid and clinically relevant naturalistic context.
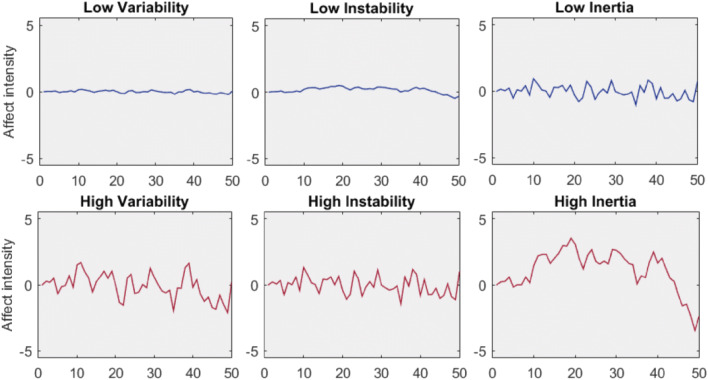
While operationalizations of affective dynamics are not always consistent, variability, instability, and inertia have emerged as potentially the most relevant indices for understanding the role of emotion in mental health and well-being (e.g., Houben et al., 2015; Koval, Pe, Meers, & Kuppens, 2013). Variability (i.e., indexed as within-person standard deviation, SD, or variance) captures the overall range of affect levels a person may experience across a particular time period, while instability (i.e., indexed as mean square successive difference between adjacent time points within person, MSSD; Jahng, Wood, & Trull, 2008) is an index of sudden and large changes from one time point to the next that takes into account temporal dependency (Koval et al., 2013). Inertia (i.e., autocorrelation between adjacent time points within person) captures the predictability of affective states from any given time point to the next (Koval et al., 2013) and also takes into account temporal dependency. To illustrate these three indices, Fig. 1 displays data simulations of low (top panels) and high (bottom panels) levels of the three dynamic measures.
Fig. 1.
Low versus high affective dynamics from left to right: variability (variance or square root of the standard deviation, SD), instability (MSSD), and inertia (autocorrelation). Figures are based on simulated data for illustration with dynamic variables set at .01 for low and .99 for high values. The x-axis represents hypothetical time points for 0 to 50, and the y-axis represents hypothetical affect intensity set to range from − 5 to 5. Variability captures the overall range of affect levels experienced across a period of time, instability is an index of sudden and large changes from one time point to the next that takes into account temporal dependency, and inertia captures the predictability of affective states from any given time point to the next and also takes into account temporal dependency
A growing number of studies have investigated how affective dynamics relate to well-being in non-clinical samples. Overall, normative data suggest that lower well-being is associated with affective dynamics characterized by higher variability, higher instability, and greater inertia across positive and, especially, negative emotions (see Houben et al., 2015 for meta-analysis). Along these lines, high levels of neuroticism (generally associated with lower well-being) in non-clinical samples have been associated with greater negative affect (NA) inertia (e.g., Suls et al., 1998), and NA inertia has been associated with regularity with difficulty in recovery of NA (e.g., Koval et al., 2015). Taken together, these findings indicate that affective dynamics may be important predictors of emotional health and well-being across populations.
Affective dynamics also have likely utility in understanding affective dysfunction in individuals with psychopathology. The study of affective dynamics is particularly relevant for understanding affective disturbance in major depressive disorder (MDD) given the nature of the disorder. Specifically, MDD is a chronic and debilitating disorder that is characterized by prevalent NA (i.e., sadness) and decreased positive affect (PA) (i.e., anhedonia) (APA, 2000). Depression is highly prevalent, especially among women (10–25%), and is the leading cause of disability (WHO, 2017). Despite the centrality of affective dysfunction to depression, we continue to have an incomplete understanding of how depression influences affective dynamics and how daily variations in affect may track the course of the disorder.
Perhaps the most consistent cross-sectional finding is that depressed individuals are typically characterized by heightened NA dynamics, including higher levels of NA inertia (e.g., Koval et al., 2013; Kuppens, Allen, & Sheeber, 2010), higher NA variability (e.g., Peeters, Berkhof, Delespaul, Rottenberg, & Nicolson, 2006; Wichers et al., 2010), and higher NA instability (e.g., Demiralp et al., 2012; Neumann, van Lier, Frijns, Meeus, & Koot, 2011; Thompson et al., 2012) relative to healthy individuals. One notable tension in depression findings is that this condition has been characterized by both high NA instability and NA inertia. Some commentators have attempted to reconcile this tension by describing depression as a state of systemic inflexibility characterized by occasional spikes in NA (contributing to higher MSSD), which are followed by a protracted period of recovery (i.e., impaired recovery) in subsequent time points (reflected in greater inertia) (e.g., Bos, de Jonge, & Cox, 2019; Koval et al., 2013).
Although depression is also typically characterized by low levels of PA (i.e., anhedonia; 70% of cases; Shankman et al., 2014) and the presence of anhedonia increases risk for chronic depression over the long term (e.g., Moos & Cronkite, 1999), less effort has focused on understanding the role of PA dynamics in depression. Characterizations of PA dynamics in depression appear to be less consistent than those of NA dynamics and may show nonlinear relationships with depression severity (see Houben et al., 2015). For example, in their meta-analytic review, Houben et al. (2015) observed that alterations in PA dynamics vary between symptomatic and diagnosed samples, such that while those with subclinical depression (i.e., minor depression and non-clinical symptomatic individuals) primarily exhibited high PA variability, instability, and inertia, a diagnosis of MDD was associated with only low PA variability. Along these lines, Heininga et al. (2019) did not find any differences between clinically depressed and non-depressed on PA dynamics (i.e., PA variability, instability, and inertia). Similar to findings with subclinical adults, depression symptoms in adolescence also have been associated with greater PA variability (van Roekel et al., 2016). In addition, while low PA variability has not been consistently observed in depression, it has been retrospectively associated with longer depressive episodes among depressed individuals (Peeters et al., 2006). Overall, findings suggest that relationships between PA dynamics and depression symptoms may be complex, and most prior work has focused on cross-sectional relationships between affective characteristics and depression.
Considering the nature of depression and data from laboratory findings comparing individuals with current or remitted MDD (e.g., Bylsma, Taylor-Clift, & Rottenberg, 2014; Salomon et al., 2013), it is expected that affective characteristics may fluctuate with depressive mood states. At the same time, little is known about how affective dynamics may prospectively predict depressive course longitudinally. While it has been established that positive and negative emotions can predict depression course more generally, based on laboratory findings and questionnaires (see Morris, Bylsma, & Rottenberg, 2009, for review), only a handful of studies have examined how daily life affective dynamics predict depression longitudinally, and none have examined how affective dynamics predict the long-term shape of depression symptom trajectories.
For example, higher NA instability, but not mean NA or PA dynamics, predicted slower early treatment response among depressed adults receiving cognitive behavioral therapy (CBT) over 5 weeks (Husen, Rafaeli, Rubel, Bar-Kalifa, & Lutz, 2016). Most recently, an evaluation of affective dynamics in the context of treatment for MDD and other emotional disorders found no association between NA affect dynamic measures and treatment outcomes (Bosley, Soyster, & Fisher, 2019). However, these authors did find an association between PA dynamics and treatment response, such that greater PA variability (but not PA instability or inertia) was associated with lower depressive symptoms posttreatment (Bosley et al., 2019). Further, in a study of the naturalistic course of depression, higher daily NA and NA variability, but not PA variability, independently predicted future MDD recurrence and future higher depressive symptoms over 4 follow-up symptom assessments completed over a 14-month period among women with current or lifetime MDD (Wichers et al., 2010). Affective inertia in daily life has not been examined as a predictor of MDD course, although one laboratory assessment of NA inertia found that affective behavior during a dyadic interaction task predicted depression onset in initially healthy adolescent girls (Kuppens et al., 2012). Therefore, despite inconsistent cross-sectional associations between PA dynamics and depression, PA dynamics may be important for predicting the course of depression.
The current study is the first to examine four daily life affective dynamic measures as predictors of the naturalistic course of weekly depressive symptoms assessed via structured retrospective clinical interviews at a 6-month follow-up. First, we examined group differences (i.e., depressed vs. controls) in daily affect levels, instability (MSSD), variability (SD), and inertia of both PA and NA in healthy controls and individuals with depressive disorders (i.e., MDD and minor depression, mD). Based on prior findings, we hypothesized that a current depression diagnosis (i.e., MDD or mD) would be associated with altered daily life NA dynamics, including higher levels of NA variability, NA instability, and NA inertia. By contrast, given inconsistent findings in the literature, we did not expect to find robust group differences for PA dynamics (variability, instability, inertia). Second, among those depressed at baseline (i.e., both MDD and mD), we examined NA and PA affective dynamics as predictors of weekly depression symptom trajectories over 6 months. For these analyses, we had two related sets of hypotheses: (1) NA dynamics (i.e., high NA variability, high NA instability, and high NA inertia) would be associated with high depression severity over time; (2) PA dynamics (i.e., low PA variability, low PA instability, and low PA inertia) would be associated with high depression severity over time. Finally, we explored how PA and NA dynamic indices predicted the shape of depression trajectories (i.e., linear and nonlinear changes in symptoms over time).
Method
As we describe in detail in Bylsma et al. (2011), participants were recruited from the community and were initially screened by phone and then invited for a diagnostic interview if eligible when participants provided informed consent. The Structured Clinical Interview for DSM-IV Disorders (SCID-I/P) was used to determine depression diagnostic status and history of other Axis-I disorders. Included participants met the current criteria for MDD (N = 35), mD (N = 25),1 or were healthy controls (i.e., no lifetime history of Axis-I disorders, N = 38). The mD group (a disorder included in the DSM-IV appendix) was included in the original study to determine if clinically depressed individuals with fewer symptoms also show similar alterations in affective functioning. This variability in weekly symptom severity among our depressed individuals was advantageous to our design, as it improved our ability to examine predictors of depressive symptom changes (i.e., increases or decreases) longitudinally. Participants across all groups were excluded for any of the following: history of a major head injury, hearing impairment, diagnosis of bipolar disorder, substance abuse occurring within 6 months prior to entry into the study, or any history of primary psychotic symptoms, as assessed by the telephone screen and the SCID diagnostic interviews.
The computerized ESM procedure was scheduled to begin within a week after baseline data was collected, using Palm Pilots and ESP software (Barrett & Barrett, 2001). Participants carried a study-provided Palm Pilot with them as they engaged in their daily activities over 3 weekdays (always Tuesday–Thursday). The devices were programmed to alarm 10 times a day semi-randomly. Participants first reported on their current mood by rating on a 0–100 scale 7 positive (talkative, enthusiastic, confident, cheerful, energetic, satisfied, and happy) and 7 negative (tense, anxious, distracted, restless, irritated, depressed, and guilty) mood adjectives which were summed to compute PA and NA composites at each time point. We used a multilevel approach described by Nezlek (2001) to calculate reliability of NA and PA. Person-level reliability estimates above .90 for both NA and PA confirmed that the scales had high internal consistency (see also Bylsma et al., 2011).
Depression symptoms and diagnostic status were re-assessed retrospectively after 6 months using a modified version of the SCID-I/P, which assessed symptoms week by week for the 6-month period since the last interview. In the introduction to this assessment, the interviewer worked with the participant to construct a life events timeline to aid recall. This depression re-assessment procedure was modeled after the well-established Longitudinal Interval Follow-up Evaluation (Keller et al., 1987). We and other groups have used similar procedures successfully to reconstruct depression course (e.g., Panaite et al., 2016; Lewinsohn, Joiner Jr, & Rohde, 2001). Retrospective symptom assessments have been noted to have good interrater reliability: Warshaw, Dyck, Allsworth, Stout, and Keller (2001) found substantial interrater reliability of symptom reports at 25–28 weeks post-baseline (ICC = .69) and comparative reliability of bi-monthly symptom reports with 6-month symptom reports among MDD participants (ICC = .76). We used strict criteria for remission, which we defined as no more than 1 clinically significant subthreshold symptom for the past 4 consecutive weeks. Weekly symptoms were summed to create a continuous weekly severity score used for the longitudinal analyses.
Compliance and Missing Data
A total of 98 participants completed the ESM protocol and met all baseline study inclusion and exclusion criteria. Two participants (both in the control group) were excluded from the ESM data for failing to complete at least five questionnaires (due to concerns about the validity of these participants’ data), and one person’s ESM data was lost due to a technical problem. There were no differences in ESM protocol compliance across groups, and the mean number of completed reports was 19.59 (SD = 5.56) out of a possible 30 for the included participants. Our compliance rate of 65% is comparable with other published ESM studies with clinical samples (e.g., 75%, Myin-Germeys, Krabbendam, Delespaul, & van Os, 2004). Compliance may have been diminished by our requirement that participants respond to ESM prompts within 15 min. Since most participants were employed or enrolled in school (86%), we recognized that timely responses to prompts would periodically be impossible (i.e., while driving or during a business meeting or classes). Final data included 1903 ESM episodes. However, 30 ESM episodes were discarded as invalid because participants selected the default option for all answers, leaving a total of 1873 valid entries (see Bylsma et al., 2011).
For the follow-up analyses, of the 60 participants that met baseline study mood criteria and completed the ESM protocol, 24 did not complete the 6-month follow-up. Among those that completed the follow-up visit (N = 36), on average, participants had a follow-up visit after 29 weeks (SD = 5.2 weeks, range = 23–52 weeks). There were no baseline differences in demographic characteristics, depression severity, or affective dynamic indices between study completers and non-completers (ps > .05). Because our previously reported findings revealed that MDD and mD groups were similar in terms of overall daily affect (see Bylsma et al., 2011), we combine these two groups in the current analyses into one mood-disordered group in order to allow us to examine the impact of depression symptom severity using a broader range of symptoms and to improve power for predicting longitudinal trajectories.
Computation of Affect Dynamic Measures
Within-person standard deviation (SD) was computed as an overall measure of PA and NA variability over time. Successive squared differences of PA and NA were computed between adjacent time points within person and day, which were used to evaluate multilevel estimates of mean squared successive difference (MSSD) in the models described below. Inertia was modeled as the autocorrelation of affect at lagged consecutive time points within person and day, where current affect is a function of affect at the previous time point (Koval et al., 2013).
Overview of Statistical Approach
Given the clustered, non-independent nature of ESM data (i.e., multiple measures within person), analyses were performed using multilevel modeling (MLM) in SPSS Version 24 (IBM, 2018), as MLM can accommodate for non-independence of clustered data as well as unequal spacing between time interviews and unbalanced data (Nezlek, 2001). Given that the data appear to be missing at random, MLM’s default maximum likelihood (ML) estimates are appropriate for dealing with missing data in the current study, which uses all available data to compute ML estimates and gives unbiased parameter estimates and standard errors. Of note, we used ML rather than restricted maximum likelihood (RML) given the appropriateness of ML to compare nested models (i.e., testing incremental value of additional higher order predictors). All models used unstructured covariance matrices and included random intercepts, and trajectory analyses included both random slopes and intercepts. ICCs indicated adequate variability to explore interindividual differences (NA = .76, PA = .56, weekly symptoms = .62).
Evaluation of Control Variables
In preliminary analyses, we investigated clinical (baseline BDI-II depression symptoms, mD vs MDD diagnosis) and demographic (age, sex, education) characteristics that may impact the shape of individual depression trajectories. Only age (B = .17, SE = .05, t = 3.62, p = .001) and baseline depression symptom severity (B = .18, SE = .05, t = 3.48, p = .001) were retained as significant covariates as they both predicted increased average 6-month depression severity.
Group Differences in Daily Affect Dynamics
Daily PA and NA dynamics were modeled as a function of group membership by regressing each person i’s outcome level onto a variable indicating the depression group membership (group: 0 = no depression; 1 = depression). At level 2, the level 1 intercept was allowed to vary randomly across participants and modeled as a function of individual differences established by group membership, as shown in the level 2 basic model equations below, where i represents person and j represents group (Tabachnick, Fidell, & Ullman, 2007). We use NA for illustrative purposes, as the PA models were parallel to the NA models.
Level 1 models:
Level 2 models:
Linear regression (i.e., general linear models) were used to identify group differences in affective variability measured by SD while controlling for identified covariates. Finally, two MANOVAs (one for PA and one for NA) evaluated whether affective dynamic indices significantly varied by group.
Longitudinal Models: Daily Affect Dynamics Predicting Depression Symptom Trajectory over 6 Months Among Those with Minor and Major Depression
These analyses followed a two-step procedure (for a similar approach, see Kuppens et al., 2012). In the first step, estimates of person-level mean PA (or mean NA), PA MSSD (or NA MSSD), and PA inertia (or NA inertia) were computed from two-level multilevel analyses performed separately and saved for each variable. At level 2 of the models, person-specific intercept and slope values were estimated (intercept and slope estimates were allowed to vary at random across participants, as appropriate).
In the next step, the computed estimates and SD were used to predict depressive symptoms over time, controlling for age and baseline depression severity. Assessment week was included both as a fixed and random time effect. Four separate models were run using the following formula for each affect dynamic measure in turn. A final multivariable model tested the four measures concurrently.
Level 1 model:
Level 2 model:
Correction for Multiple Hypothesis Testing
We corrected for multiple hypothesis testing using the Benjamini and Hochberg (1995) approach. Following recommendations, we applied this approach to the two families of hypotheses separately, identifying corrected p values for hypotheses concerning group differences (p < .019) and longitudinal analyses (p < .025) (Benjamini & Hochberg, 1995). This allows for correction of type I error while suppressing inflation of type II error, relative to other approaches, such as Bonferroni correction.
Results
Clinical Characteristics
Clinical characteristics of the groups (see Supplementary Table 1) followed expected patterns (see parent study, Bylsma et al., 2011). Analyses of demographic characteristics, treatment use at baseline, and comorbid diagnoses revealed no differences between MDD and mD groups. Further areas where those with MDD and mD did not differ, such as follow-up rates of experiencing an episode or remission (ps > .05), are highlighted in Supplementary Table 1.
Group Differences in Individual Daily Affect Dynamics
Our first set of results evaluating group differences in affective dynamics are presented in Table 1. We first re-examined group differences (depressed vs. controls) in the overall means for PA and NA, in order to establish replication of our prior study findings (i.e., given that prior analyses were completed with a different statistical package; see Bylsma et al., 2011). To ensure replication of prior analyses, we retained the original model specifications described in the parent project (see Bylsma et al., 2011). Therefore, separate multilevel models were conducted for PA and NA with group status as a level 2 predictor. As reported in Bylsma et al. (2011), follow-up analyses demonstrated that both depressed groups reported reduced daily PA relative to healthy controls (p < .001) and both depressed groups reported greater overall daily NA compared with healthy controls (p < .001). Of note, no differences were recorded between the two depressed groups (MDD vs. mD, ps > .05). Furthermore, given that no differences were recorded between the two depressed groups across all dynamic measures (ps > .05), we collapsed the MDD and mD groups into one depressed group for all subsequent analyses.
Table 1.
Dynamics of positive and negative daily affect across groups
| Fixed effects | B | SE | t | p | B | SE | t | p |
|---|---|---|---|---|---|---|---|---|
| Mean PA | Mean NA | |||||||
| Intercept | 416.15 | 15.98 | 26.03 | < .001 | 147.48 | 17.03 | 8.66 | < .001 |
| Group | − 156.79 | 20.29 | − 7.73 | < .001* | 214.77 | 21.62 | 9.93 | < .001* |
| PA MSSD | NA MSSD | |||||||
| Intercept | 13,207.98 | 1981.95 | 85.36 | < .001 | 8263.13 | 1484.55 | 5.57 | < .001 |
| Group | 1851.35 | 2515.10 | 85.76 | .464 | 3117.71 | 1883.63 | 1.66 | .101 |
| PA inertia | NA inertia | |||||||
| Intercept | 247.92 | 18.67 | 13.28 | < .001 | 103.68 | 13.90 | 7.46 | < .001 |
| Group | − .05 | .05 | − 1.02 | .308 | < .01 | .05 | .09 | .933 |
| PA SD | NA SD | |||||||
| Constant | 91.76 | 6.78 | 13.54 | < .001 | 68.22 | 5.04 | 13.54 | < .001 |
| Group | 7.44 | 8.61 | .86 | .390 | 13.86 | 6.41 | 2.16 | .033 |
Note: Group: healthy = 0, depressed = 1
*Based on Benjamini-Huchberg multiple testing correction, α < .019 was used for significance testing
Next, we evaluated group differences (depressed vs control) in PA and NA dynamics (see Table 1). Separate multilevel models were conducted for PA and NA inertia and MSSD with group status as a level 2 predictor. Linear regression analyses were used to evaluate group differences in SD (variability) of NA and PA. No group effects were observed for PA SD or NA SD after controlling for multiple hypothesis testing (see Table 1). In summary, the groups differed in their overall affect levels for PA and NA (as previously reported in Bylsma et al., 2011). However, partially countering expectations, there were no group differences in any of the other PA or NA affective dynamics (i.e., SD, MSSD, or autocorrelation).
Group Differences Across Affect Dynamics Using a Multivariate Model
Given prior work showing shared variance among dynamic measures (e.g., Dejonckheere et al., 2019), we evaluated the independent group effect on the four affective dynamic measures concurrently. Two MANOVAs evaluated group effect on NA and PA2 dynamics separately. The multivariate tests indicated a group effect for both PA and NA affective dynamic measures (PA, F (4.91) = 15.77, p < .001; Wilk’s Λ = 0.591, partial η2 = .41; NA, F (4.91) = 25.83, p < .001; Wilk’s Λ = 0.468, partial η2 = .53). The tests of between-subjects effects indicated a specific group effect on mean PA (F (1.94) = 59.67, p < .001; partial η2 = .39). For NA, both mean NA (F (1.94) = 99.91, p < .001; partial η2 = .52) and NA SD (F (1.94) = 5.38, p = .023; partial η2 = .05) were significant controlling for all other dynamic measures, with depressed persons reporting higher NA and lower PA on average, as well as higher NA variability (SD) relative to healthy controls. In sum, univariate and multivariate dynamic models reveal that group differences are relatively stable, suggesting that mean NA and PA levels and NA variability (but not PA variability) consistently differentiate depressed and healthy individuals.
Do Individual Affective Dynamics Predict Average Future Depression Severity?
Our second set of hypotheses focused on whether PA and NA mean levels, variability, instability, and inertia were predictive of follow-up symptom severity among depressed (MDD and mD) individuals. MLM random intercept models were built to test whether level 2 computed person-level estimates of each of the dynamic indices predicted weekly depression symptom severity. These analyses were performed with and without significant covariates (age, baseline depression severity) (Table 2). As expected, higher NA and lower PA levels predicted higher average depression symptoms over time (ps < .025). Neither NA nor PA variability, instability, or inertia were related to average depression symptom severity over time (p > .025) (Table 2).
Table 2.
Daily affect dynamics, overall symptom severity, and trajectory shape of weekly total depression symptom severity over 6 months
| B | SE | t | p | |
|---|---|---|---|---|
| Mean Models | ||||
| Unconditional: | ||||
| Intercept Only | 7.23 | .59 | 12.29 | <.001** |
| With predictors: | ||||
| Mean PA | –.01 | .01 | –2.34 | .025** |
| Mean NA | .01 | .01 | 2.51 | .017** |
| PA MSSD | <–.01 | <.01 | –1.85 | .073 |
| NA MSSD | <.01 | <.01 | .27 | .785 |
| PA Inertia | 1.78 | 1.93 | .92 | .361 |
| NA Inertia | 2.44 | 1.66 | 1.47 | .150 |
| PA SD | –.02 | .01 | –1.41 | .167 |
| NA SD | <.01 | .02 | .12 | .908 |
| Cubic Growth Curve Models (Higher–Order Change Trajectories) | ||||
| Unconditional: | ||||
| Week | –.22 | .13 | –1.65 | .100 |
| Week2 | –.01 | .01 | –1.17 | .242 |
| Week3 | <.01 | <.01 | 3.03 | .003** |
| With predictors: | ||||
| Mean PA* Week | <–.01 | <.01 | –.74 | .461 |
| Mean PA* Week2 | <.01 | <.01 | .22 | .828 |
| Mean PA* Week3 | <.01 | <.01 | .12 | .904 |
| Mean NA* Week | <–.01 | <.01 | –.06 | .953 |
| Mean NA* Week2 | <.01 | <.01 | .35 | .723 |
| Mean NA* Week3 | <–.01 | <.01 | –.63 | .530 |
| PA MSSD* Week | <.01 | <.01 | .59 | .556 |
| PA MSSD* Week2 | <–.01 | <.01 | –.81 | .418 |
| PA MSSD* Week3 | <.01 | <.01 | 1.20 | .230 |
| NA MSSD* Week | <.01 | <.01 | 2.47 | .014** |
| NA MSSD* Week2 | <–.01 | <.01 | –2.98 | .003** |
| NA MSSD* Week3 | <.01 | <.01 | 3.20 | .001** |
| PA Inertia* Week | .78 | .56 | 1.40 | .163 |
| PA Inertia* Week2 | –.04 | .04 | –.86 | .391 |
| PA Inertia* Week3 | <.01 | <.01 | .55 | .583 |
| NA Inertia* Week | 1.43 | .56 | 2.58 | .010** |
| NA Inertia* Week2 | –.10 | .05 | –2.19 | .029 |
| NA Inertia* Week3 | <.01 | <.01 | 2.18 | .029 |
| PA SD* Week | .01 | .01 | 2.23 | .026 |
| PA SD* Week2 | <–.01 | <.01 | –2.13 | .033 |
| PA SD* Week3 | <.01 | <.01 | 2.26 | .024** |
| NA SD* Week | .02 | .01 | 2.79 | .005** |
| NA SD* Week2 | <–.01 | <.01 | –2.73 | .006** |
| NA SD* Week3 | <.01 | <.01 | 2.59 | .010** |
Note: Results reflect inclusion of week of assessment (both as fixed and random effects), age, and baseline BDI–II as fixed covariates. Week2 = quadratic time effect; Week3 = cubic time effect. **Based on Benjamini/Huchberg multiple testing correction, α < .025 for significance testing
Multivariate Affective Dynamic Model Predicting Average Future Depression Severity
When all four affective dynamic indices were entered simultaneously in a multilevel model predicting depression symptom severity over time, mean affect for both PA (B = − .01, SE = .01, t = − 2.42, p = .021) and NA (B = .01, SE = .01, t = 2.62, p = .013) remained a robust predictor of depression symptom severity longitudinally. These results persisted with the inclusion of age and baseline depression severity as covariates. Overall, consistent with our group differences reported above, average daily NA and PA (but none of the other affective dynamic indices) persisted across single and multivariable models in predicting longitudinal depression symptom severity.
Trajectory of Symptom Severity: Preliminary Testing of Time Effects
Our last set of analyses explored whether affective dynamics are associated with shape of depression symptom trajectories (i.e., based on the weekly depression symptoms assessed retrospectively at the 6-month follow-up visit using the modified SCID interview). First, we present preliminary analyses used to evaluate whether an investigation of trajectory shape is warranted. An unconditional model showed that 43.6% of variance within depression symptom severity scores stems from interindividual variability, suggesting the presence of considerable individual variability in depression severity trajectories. Therefore, our investigation of depression symptom trajectories was warranted.
First, investigation of an unconditional linear growth model suggested that linear growth rate in depression symptoms was not constant: Although there was evidence of a significant linear decrease in depression severity over time (B = − .09, SE = .02, t = − 5.45, p < .001), a decline in residual (unexplained) variance with the inclusion of linear time as a predictor indicated that only 3.9% of the within-individual variation of depression symptom severity was associated with linear rate of change. Thus, we next explored quadratic and cubic models to determine whether they may provide additional information about depression symptom trajectory.
Next, we investigated a quadratic growth curve model of depression symptom change trajectories. The model indicated a small positive quadratic effect (B = .02, SE = .002, t = 8.49, p < .001), suggesting that the initial decrease in depression symptom severity (i.e., negative linear effect: B = − .56, SE = .07, t = − 7.97, p < .001) diminished over time. Next, we examined change trajectories with a cubic growth curve model that would capture repeated changes or variability in change of depressive symptoms over time. This model indicated a small positive cubic effect (B = .001, SE < .001, t = 3.03, p < .01), suggesting that the initial deceleration in decrease in depression severity continues over time with participants continuing to exhibit an eventual increase in depression severity (i.e., U-shaped trajectory of depression symptoms over time). Model fit criteria (see Table 3) demonstrated improvements in model estimation gained by adding the quadratic (χ2 (1) = 5466.09–5396.74 = 68.35, p < 0.01; Δ AIC = 5478.09–5410.74 = 67.35, p < 0.01; Δ BIC = 5507.44–5444.98 = 62.46) and cubic (χ2 (1) = 5396.74–5387.63 = 9.11, p < 0.05; Δ AIC = 5410.74–5403.63 = 7.11, p < 0.05; Δ BIC = 5444.98–5442.76 = 2.22) effects.3 Therefore, a model including all three effects was retained (Table 2). Taken together, our initial evaluations of depression symptom trajectory suggested an evaluation of nonlinear trajectories was warranted.
Table 3.
Model fit information for our preliminary models testing linear, quadratic, and cubic time trajectories
| Model | Goodness of fit | # of parameters | df | -2LL | χ2 | p | AIC | ΔAIC | p | BIC | ΔBIC |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Linear model 1 | 6 | 5466.09 | 5478.09 | 5507.44 | |||||||
| Linear + quadratic model 2 | M1-M2 | 7 | 1 | 5396.74 | 68.35 | < .01 | 5410.74 | 67.35 | < .01 | 5444.98 | 62.46 |
| Linear + quadratic + cubic model 3 | M2-M3 | 8 | 1 | 5387.63 | 9.11 | < .05 | 5403.63 | 7.11 | < .05 | 5442.76 | 2.22 |
Multilevel Models of Individual Daily Affect Dynamics Predicting 6-Month Depression Symptom Trajectory
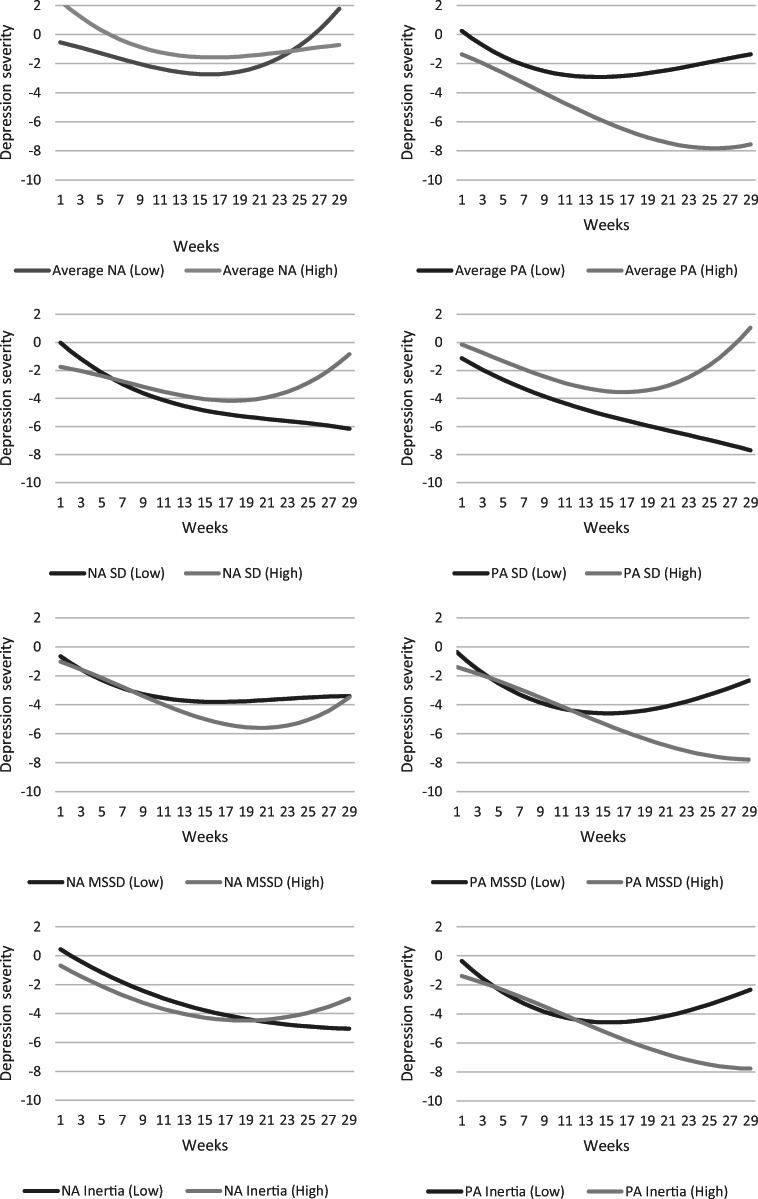
Next, we employed growth curve models to evaluate whether PA and NA dynamic indices predict the shape of depression symptom trajectories (see Table 2). Daily NA instability, inertia, and variability were all associated with cubic trajectories. The shape of the cubic trajectories was characterized by an initial elevated level in symptom severity, followed by a temporary decrease in symptom severity and an eventual return to heightened depression severity. In sum, greater NA variability, inertia, and instability predicted a longer term increase in depression symptoms over time. Although PA variability was also associated with a similar U-shaped cubic trajectory, our sample size did not allow to establish whether findings across PA and NA variability were comparable or meaningfully different. None of the other affect dynamic indices predicted the shape of depression symptom trajectories. Results were robust to control of age and baseline depression severity (see Table 2). To further illustrate these findings, see cubic effects illustrated in Fig. 2.
Fig. 2.
The association between low versus high NA and PA dynamic measures (calculated by mean split) and depression severity rate of change over time
Discussion
Affective dynamics, or the fluctuations in emotional states over time to meet environmental needs, have been consistently related to well-being and mental health (see Houben et al., 2015). Although there is accumulating cross-sectional evidence that affect dynamics relate to emotional health and well-being (e.g., Koval et al., 2015; Suls et al., 1998), less is known about how day-to-day emotional fluctuations might be predictive of well-being and psychopathology over longer periods of time (e.g., months). Depression has been associated with affective dynamic characteristics cross-sectionally, particularly for NA, but it is less clear how affective dynamics predict depression course. Our study was the first to examine the naturalistic course of affective dynamics and depressive symptoms in individuals with depressive disorders.
Consistent with prior literature, we did not find group differences between depressed and controls for any of our PA dynamic measures at baseline. In contrast to cross-sectional studies linking affective dynamics to depression and well-being (e.g., Dejonckheere et al., 2019; Houben et al., 2015; Peeters et al., 2006), we also did not observe higher NA inertia cross-sectionally among depressed individuals relative to healthy controls. At the same time, our results have precedent as not all studies find an association between NA inertia and depression (e.g., Houben & Kuppens, 2020; Thompson et al., 2012). Even when group differences are observed in the literature, other recent findings question whether NA inertia contributes unique variance in predicting current depression or well-being above and beyond non-dynamic measures (i.e., mean affect or affect variance) (Dejonckheere et al., 2019). The timescale at which inertia is measured or environmental context may further contribute to heterogeneity in findings.
Our study was novel in examining both daily life PA and NA levels and dynamics in predicting the naturalistic course of weekly depression symptoms sampled retrospectively at the 6-month follow-up using a rigorous mixed-methods design. Our sample of individuals with both MDD and mD allowed us to use stringent diagnostic criteria to establish a clinical diagnosis of depression while also increasing the range of possible depressive symptoms among participants over the follow-up period (i.e., participants could have anywhere from 2 to 9 DSM symptoms of depression at a clinical level). We found that higher mean NA was the most robust in predicting an adverse course of depression, while mean PA was a predictor of a more benign course defined by decreasing average symptom severity over time. Furthermore, multiple NA measures were related to shape of trajectory of depression over time: NA variability, NA instability, and NA inertia all predicted a more deleterious depression course characterized by increased and sustained depression symptom severity over time.
Longitudinal findings for PA dynamics were more equivocal: only PA variability predicted depression trajectories. The specific relationship between PA and depression symptom trajectory shape was also unexpected, such that high PA variability did not appear to protect against the experience of depression symptoms over time. Because anhedonia (i.e., inability to experience PA) is a core symptom of depression that is present in over 70% of cases (Shankman et al., 2014), this may constrain the predictive power of PA variability, whereas high levels of PA are more consistently linked to well-being (Diener, 2000; Kahneman et al., 1999). Despite our results, additional future work should test the possibility that more variable PA could still occur against a backdrop of low PA, and such a pattern may reflect more appropriate and flexible responsiveness to environmental rewards, consistent with increased psychological flexibility (Kashdan & Rottenberg, 2010).
Most notably, ours is the first study to demonstrate that longitudinal effects for NA dynamics follow a similar pattern to findings from cross-sectional studies (e.g., Dejonckheere et al., 2019). Specifically, when tested separately, NA variability, NA inertia, and NA instability were all associated with depression symptom variability longitudinally and, more specifically, with a deteriorating clinical state (i.e., increases in depression symptoms) over time. We should note that, in our conservative multivariate analysis, mean NA survived as a predictor of longitudinal depression symptoms, in line with findings by Dejonckheere et al. (2019). It may be that larger samples are needed to detect dynamic effects or that heightened mean NA may be better at reflecting the diverse mechanisms that lead to sustained or worsening depression. Affect dynamics, whether individually or under the umbrella of mean NA, may be capturing mechanisms that are likely to sustain depression over time. For example, NA inertia may contribute to sustained NA via poor emotion regulation or a perseverative cognitive style (e.g., rumination, Koval et al., 2012). Further, NA variability and instability may contribute to sustained NA via heightened sensitivity to emotional stimuli, which has been observed in some samples of depressed individuals who responded with increased NA in response to small daily life stressors (Myin-Germeys et al., 2003; Wichers et al., 2007a, 2007b). Finally, heightened NA instability, but not mean NA, has been shown to predict a slower treatment response among patients completing (CBT) for depression (Husen et al., 2016), further highlighting the possible added value of continuing to evaluate affective dynamics to understand clinical outcomes.
As this was a first investigation of how affective dynamics predict depression symptoms longitudinally, results should be considered with some limitations in mind. For example, we did not explore several individual difference variables that may play a role in the relationship between affective dynamics and depression. Thus, it is possible that these affective characteristics may reflect trait neuroticism, which has been linked to more severe depression over time (e.g., Morris et al., 2009), although prior work has not found neuroticism to independently predict depression trajectories beyond the effect of daily affective dynamics (Wichers et al., 2010). Future work should examine the contribution of personality and other individual difference variables such as neuroticism to alterations in affective dynamics associated with depression over time. Finally, both our sample size and the retrospective nature of our 6-month symptom assessment may have limited further evaluation of impact of dynamics on depression symptom trajectories of those with preclinical and subclinical symptoms of depression; such evaluations may have value in better understanding risk for depression and recurrence. Future work using both a larger sample and weekly symptom ratings will help evaluate theories about how affective dynamics relate to long-term adaptational outcomes (Hollenstein, 2015; Hollenstein et al., 2013).
Daily life affective dynamics may have merit as an inexpensive and noninvasive predictor of the naturalistic course of mood disorders or markers of response to interventions (e.g., Husen et al., 2016). Further work is needed to clarify whether mean affective measures are sufficient in capturing the impact of affect dynamics on longitudinal course of depression. Predicting which patients do well in the longer term is notoriously difficult, although early improvement has been shown to predict sustained recovery over the long term (Ghio, Gotelli, Marcenaro, Amore, & Natta, 2014). Affective dynamics may help predict which individuals may continue to need additional support even following an initial improvement in symptoms (e.g., Husen et al., 2016), and may also identify potential modifiable targets for depression prevention and intervention.
Electronic Supplementary Material
(DOCX 15 kb)
Additional Information
Acknowledgments
We thank Marlies Houben and Merijn Mestdagh for providing the code used to produce the simulated affective dynamic data used in Fig. 1.
Authors’ Contributions
LMB and JR contributed to the study design; LMB collected the data; LMB performed preliminary data analyses and contributed to the literature review; VP and LMB contributed to the concept of this secondary data analysis; VP performed the current data analyses and drafted the manuscript. JR and LMB provided substantive edits and feedback throughout the development of this manuscript.
Funding
LMB received support from American Psychological Association of Graduate Students (APAGS) Nancy B. Forest & L. Michael Honaker Master’s Scholarship for Research in psychology to support data collection and preliminary analyses of this research. LMB also was supported by MH104325 and MH118218 during the preparation of this manuscript.
Data Availability
The data used to prepare this article can be found at https://osf.io/cepr4/.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All data were collected in accordance with the rules and regulations of the University of South Florida Internal Review Board.
Informed Consent
Completed by all participants prior to enrollment.
Disclaimer
The contents of this publication do not represent the views of the Department of Veterans Affairs or the US Government.
Footnotes
One participant was excluded at follow-up after publication of ESM findings (Bylsma et al., 2011) due to no longer meeting study inclusion criteria.
In testing for multicollinearity, we evaluated several indices of multicollinearity possibly being present. First correlation matrices for NA and PA identified two elevated correlations among variability and instability dynamics measures, specifically, rNA = .64 and rPA = .78. This suggested that further evaluation of multicollinearity may be warranted. Indeed, multicollinearity is suspected between PA MSSD and PA SD based on the two indices that were elevated beyond acceptable boundaries: PA MSSD VIF = 5.4 and PA MSSD variance proportion = .80; PA SD VIF = 4.8 and PA SD variance proportion = .96. Specificity analyses were therefore re-run excluding PA SD from the model and results remained unchanged.
References
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: Author.
- Barrett LF, Barrett DJ. An introduction to computerized experience sampling in psychology. Social Science Computer Review. 2001;19(2):175–185. doi: 10.1177/089443930101900204. [DOI] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B: Methodological. 1995;57(1):289–300. [Google Scholar]
- Bos EH, de Jonge P, Cox RF. Affective variability in depression: revisiting the inertia–instability paradox. British Journal of Psychology. 2019;110(4):814–827. doi: 10.1111/bjop.12372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosley HG, Soyster PD, Fisher AJ. Affect dynamics as predictors of symptom severity and treatment response in mood and anxiety disorders: evidence for specificity. Journal for Person-Oriented Research. 2019;5(2):101–113. doi: 10.17505/jpor.2019.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bylsma LM, Taylor-Clift A, Rottenberg J. Emotional reactivity to daily events in major and minor depression. Journal of Abnormal Psychology. 2011;120:155–167. doi: 10.1037/a0021662. [DOI] [PubMed] [Google Scholar]
- Bylsma, L. M., Salomon, K., Taylor-Clift, A., Morris, B. H., & Rottenberg, J. (2014). RSA reactivity in current and remitted major depressive disorder. Psychosomatic medicine, 76(1), 66. [DOI] [PMC free article] [PubMed]
- Dejonckheere E*, Mestdagh M*, Houben M, Rutten I, Sels L, Kuppens P, Tuerlinckx F. Complex affect dynamics add limited information to the prediction of psychological well-being. Nature Human Behaviour. 2019;3:478–491. doi: 10.1038/s41562-019-0555-0. [DOI] [PubMed] [Google Scholar]
- Demiralp E, Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Barrett LF, Jonides J. Feeling blue or turquoise? Emotional differentiation in major depressive disorder. Psychological Science. 2012;23:1410–1416. doi: 10.1177/0956797612444903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener, E. (2000). Subjective well-being: The science of happiness and a proposal for a national index. American psychologist, 55(1), 34. [PubMed]
- Frijda NH. The laws of emotion Mahwah. NJ: Lawrence Erlbaum Associates; 2007. [Google Scholar]
- Ghio L, Gotelli S, Marcenaro M, Amore M, Natta W. Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta-analysis. Journal of Affective Disorders. 2014;152–154:45–51. doi: 10.1016/j.jad.2013.10.002. [DOI] [PubMed] [Google Scholar]
- Heininga VE, Dejonckheere E, Houben M, Obbels J, Sienaert P, Leroy B, van Roy J, Kuppens P. The dynamical signature of anhedonia in major depressive disorder: positive emotion dynamics, reactivity, and recovery. BMC Psychiatry. 2019;19(1):59. doi: 10.1186/s12888-018-1983-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollenstein T. This time, it’s real: affective flexibility, time scales, feedback loops, and the regulation of emotion. Emotion Review. 2015;7(4):308–315. doi: 10.1177/1754073915590621. [DOI] [Google Scholar]
- Hollenstein T, Lichtwarck-Aschoff A, Potworowski G. A model of socioemotional flexibility at three time scales. Emotion Review. 2013;5(4):397–405. doi: 10.1177/1754073913484181. [DOI] [Google Scholar]
- Houben M, Kuppens P. Emotion dynamics and the association with depressive features and borderline personality disorder traits: unique, specific and prospective relationships. Clinical Psychological Science. 2020;8:226–239. doi: 10.1177/2167702619871962. [DOI] [Google Scholar]
- Houben M, Van den Noortgate W, Kuppens P. The relation between short-term emotion dynamics and psychological well-being: a meta-analysis. Psychological Bulletin. 2015;141:901–930. doi: 10.1037/a0038822. [DOI] [PubMed] [Google Scholar]
- Husen K, Rafaeli E, Rubel JA, Bar-Kalifa E, Lutz W. Daily affect dynamics predict early response in CBT: feasibility and predictive validity of EMA for outpatient psychotherapy. Journal of Affective Disorders. 2016;206:305–314. doi: 10.1016/j.jad.2016.08.025. [DOI] [PubMed] [Google Scholar]
- IBM Corp. (2018). IBM SPSS statistics for windows, version 26.0. Armonk, NY: IBM Corp.
- Jahng S, Wood PK, Trull TJ. Analysis of affective instability in ecological momentary assessment: indices using successive difference and group comparison via multilevel modeling. Psychological Methods. 2008;13(4):354–375. doi: 10.1037/a0014173. [DOI] [PubMed] [Google Scholar]
- Kahneman, D., Diener, E., & Schwarz, N. (Eds.). (1999). Well-being: Foundations of hedonic psychology. Russell Sage Foundation.
- Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44(6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Koval P, Kuppens P, Allen NB, Sheeber LB. Getting stuck in depression: the roles of rumination and emotional inertia. Cognition & Emotion. 2012;26:1412–1427. doi: 10.1080/02699931.2012.667392. [DOI] [PubMed] [Google Scholar]
- Koval P, Pe ML, Meers K, Kuppens P. Affect dynamics in relation to depressive symptoms: variable, unstable or inert? Emotion. 2013;13:1132–1141. doi: 10.1037/a0033579. [DOI] [PubMed] [Google Scholar]
- Koval P, Brose A, Pe ML, Houben M, Erbas Y, Champagne D, Kuppens P. Emotional inertia and external events: the roles of exposure, reactivity, and recovery. Emotion. 2015;15(5):625–636. doi: 10.1037/emo0000059. [DOI] [PubMed] [Google Scholar]
- Kuppens P, Allen NB, Sheeber LB. Emotional inertia and psychological maladjustment. Psychological Science. 2010;21(7):984–991. doi: 10.1177/0956797610372634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuppens P, Sheeber LB, Yap MBH, Whittle S, Simmons JG, Allen NB. Emotional inertia prospectively predicts the onset of depressive disorder in adolescence. Emotion. 2012;12:283–289. doi: 10.1037/a0025046. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Joiner TE, Jr, Rohde P. Evaluation of cognitive diathesis-stress models in predicting major depressive disorder in adolescents. Journal of Abnormal Psychology. 2001;110(2):203–215. doi: 10.1037/0021-843X.110.2.203. [DOI] [PubMed] [Google Scholar]
- Moos RH, Cronkite RC. Symptom-based predictors of a 10-year chronic course of treated depression. The Journal of Nervous and Mental Disease. 1999;187(6):360–368. doi: 10.1097/00005053-199906000-00005. [DOI] [PubMed] [Google Scholar]
- Morris BH, Bylsma LM, Rottenberg J. Does emotion predict the course of major depressive disorder? A review of prospective studies. British Journal of Clinical Psychology. 2009;48:255–273. doi: 10.1348/014466508X396549. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I, Peeters FPML, Havermans R, Nicolson NA, DeVries MW, Delespaul PAEG, Van Os J. Emotional reactivity to daily life stress in psychosis and affective disorder: an experience sampling study. Acta Psychiatrica Scandinavica. 2003;107(2):124–131. doi: 10.1034/j.1600-0447.2003.02025.x. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I, Krabbendam L, Delespaul PA, van Os J. Sex differences in emotional reactivity to daily life stress in psychosis. Journal of Clinical Psychiatry. 2004;65:805–809. doi: 10.4088/JCP.v65n0611. [DOI] [PubMed] [Google Scholar]
- Neumann A, van Lier PA, Frijns T, Meeus W, Koot HM. Emotional dynamics in the development of early adolescent psychopathology: a one-year longitudinal study. Journal of Abnormal Child Psychology. 2011;39(5):657–669. doi: 10.1007/s10802-011-9509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezlek JB. Multilevel random coefficient analyses of event-and interval-contingent data in social and personality psychology research. Personality and Social Psychology Bulletin. 2001;27(7):771–785. doi: 10.1177/0146167201277001. [DOI] [Google Scholar]
- Panaite V, Hindash AC, Bylsma LM, Small BJ, Salomon K, Rottenberg J. Respiratory sinus arrhythmia reactivity to a sad film predicts depression symptom improvement and symptomatic trajectory. International Journal of Psychophysiology. 2016;99:108–113. doi: 10.1016/j.ijpsycho.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters F, Berkhof J, Delespaul P, Rottenberg J, Nicolson NA. Diurnal mood variation in major depressive disorder. Emotion. 2006;6:383–391. doi: 10.1037/1528-3542.6.3.383. [DOI] [PubMed] [Google Scholar]
- Salomon, K., Bylsma, L. M., White, K. E., Panaite, V., & Rottenberg, J. (2013). Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major depressive disorder remitted depression and healthy controls. International Journal of Psychophysiology, 90(1), 50–57. [DOI] [PMC free article] [PubMed]
- Shankman SA, Katz AC, DeLizza AA, Sarapas C, Gorka SM, Campbell ML. Anhedonia: a comprehensive handbook. Dordrecht: Springer; 2014. The different facets of anhedonia and their associations with different psychopathologies; pp. 3–22. [Google Scholar]
- Shek DT, Ma C. Longitudinal data analyses using linear mixed models in SPSS: concepts, procedures and illustrations. The Scientific World Journal. 2011;11:42–76. doi: 10.1100/tsw.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J, Green P, Hillis S. Emotional reactivity to everyday problems, affective inertia, and neuroticism. Personality and Social Psychology Bulletin. 1998;24:127–136. doi: 10.1177/0146167298242002. [DOI] [Google Scholar]
- Tabachnick BG, Fidell LS, Ullman JB. Using multivariate statistics. Boston: Pearson; 2007. [Google Scholar]
- Thompson, R. J., Mata, J., Jaeggi, S. M., Buschkuehl, M., Jonides, J., & Gotlib, I. H. (2012). The everyday emotional experience of adults with major depressive disorder: examining emotional instability, inertia, and reactivity. Journal of Abnormal Psychology, online, 1–11. [DOI] [PMC free article] [PubMed]
- van Roekel E, Bennik EC, Bastiaansen JA, Verhagen M, Ormel J, Engels RC, Oldehinkel AJ. Depressive symptoms and the experience of pleasure in daily life: an exploration of associations in early and late adolescence. Journal of Abnormal Child Psychology. 2016;44(5):999–1009. doi: 10.1007/s10802-015-0090-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: an ongoing inter-rater reliability monitoring program using the Longitudinal Interval Follow-up Evaluation. Journal of Psychiatric Research. 2001;35(5):297–305. doi: 10.1016/S0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Wichers M, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, et al. Genetic risk of depression and stress-induced negative affect in daily life. The British Journal of Psychiatry. 2007;191(3):218–223. doi: 10.1192/bjp.bp.106.032201. [DOI] [PubMed] [Google Scholar]
- Wichers MC, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, et al. Evidence that moment-to-moment variation in positive emotions buffer genetic risk for depression: a momentary assessment twin study. Acta Psychiatrica Scandinavica. 2007;115(6):451–457. doi: 10.1111/j.1600-0447.2006.00924.x. [DOI] [PubMed] [Google Scholar]
- Wichers M, Peeters F, Geschwind N, Jacobs N, Simons CJP, Derom C, Thiery E, Delespaul PH, van Os J. Unveiling patterns of affective responses in daily life may improve outcome prediction in depression: a momentary assessment study. Journal of Affective Disorders. 2010;124(1):191–195. doi: 10.1016/j.jad.2009.11.010. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017). Depression and other common mental disorders: Global health estimates: https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 15 kb)
Data Availability Statement
The data used to prepare this article can be found at https://osf.io/cepr4/.