Abstract
Touch associated with sleep (sleep-touch; reported physical contact during or shortly before/after sleep) is underexplored as a distinct contributor to affect regulatory processes associated with adult sleep. Given the affect-regulating effects of interpersonal touch, we theorized that among healthy co-sleeping adults, sleep-touch would add to sleep-related effects on affective “resetting,” resulting in the experience of calmer, more regulated states. We studied 210 married heterosexual couples (aged 20–67 years, 79% non-Hispanic white, 13% Latinx) assigned 14 days of twice-daily (morning/evening) sleep/mood diaries. Multilevel daily (within-couple) mediation analyses showed that as hypothesized, more reported sleep-touch was associated with happier/calmer and less angry/irritable morning mood. In turn, happier/calmer mood was associated with greater enjoyment of time with spouse (for both spouses). Sleep-touch also was linked directly to both evening positive spousal events and enjoyment ratings. Sleep-touch was associated indirectly with fewer negative spousal events and less spouse-related stress via less angry/irritable morning mood (both spouses). Further, wives’ sleep-touch was related to happier/calmer husband mood and evening enjoyment; husbands’ sleep-touch was unrelated to wives’ reports. All associations with sleep-touch were present while accounting for subjective sleep quality, prior evening mood, non-sleep-related physical affection, day in study, and weekend versus weekday. We speculate that among relatively healthy satisfied couples, physical touch during and surrounding sleep may add to sleep’s restorative and affect-regulatory functions, suggesting a pathway through which co-sleeping can improve affect regulation and ultimately relationships and health.
Keywords: Emotion, Emotion regulation, Sleep, Affectionate touch, Couples, Positive affect
Alongside its well-established benefits for cognition (e.g., memory consolidation, Stickgold, 2005) and health (e.g., immune functioning, Besedovsky et al., 2012; Prather et al., 2015), sleep is now recognized for its emotion processing/emotion regulation (Ben Simon et al., 2020; Cartwright et al., 1998; Krause et al., 2017; van der Helm & Walker, 2011; Walker & van der Helm, 2009) and social functions (Gordon et al., 2017, 2021). Interpersonal touch has similar socioemotional functions (Jakubiak & Feeney, 2017). Here, we focus on sleep-touch, which we operationalize as self-reported physical contact during or shortly before/after sleep and which may intersect with the aforementioned processes.
Sleep has the potential to consolidate emotional memories (Payne et al., 2008) and “reset” or “recalibrate” (Goldstein-Piekarski et al., 2015) affect, shifting mood in a positive direction (Bouwmans et al., 2017). Although the processes through which this occurs are still emerging, sleep may shape affect by enhancing self-regulatory capacity (Barber et al., 2013), such as through inhibitory control (Chuah et al., 2006) or increased ability for cognitive shifting (reappraisal, Mauss et al., 2013), or by changing the very nature of affective processing, as evidenced by neuroimaging after sleep deprivation (Yoo et al., 2007) and by close links between sleep disruption and psychopathology (Benca et al., 1992; Krystal, 2020; Wassing et al., 2019).
Sleep’s ability to reset mood may be especially beneficial for spouses/romantic partners (Maranges & McNulty, 2017; reviewed in Richter et al., 2016 and Troxel et al., 2007), which was the focus of the present study. The balance of positive and negative affect (particularly hostility) predicts marital quality and stability (Gottman & Levenson, 1992; Waldinger et al., 2004). Relationship quality and sleep quality covary over time (Lee et al., 2017). One partner’s well-being can suffer due to the other’s disrupted sleep, even accounting for the person’s own sleep quality (Strawbridge et al., 2004). In healthy couples, sleep concordance correlates with subjective (Spiegelhalder et al., 2017) and objective sleep quality (Drews et al., 2017; Troxel et al., 2010); health indicators (Gunn et al., 2017); and relationship satisfaction (Elsey et al., 2019; Hasler & Troxel, 2010). For example, co-sleeping with a partner versus sleeping alone is associated with more (and less fragmented) REM sleep (Drews et al., 2020).
One key aspect of co-sleeping is physical touch (Rosenblatt, 2006). Although partner touch during sleep is noted in some studies (Izci et al., 2005; McFadyen et al., 2001), it is often overlooked as a distinct contributor to affect regulatory processes. There is reason to believe sleep-touch is an important facet of co-sleeping. Touch is central to affect regulation and distress mitigation, not only between infants and caregivers (Cascio et al., 2019; Waters et al., 2014) but also in adult relationships (Burleson et al., 2021; Jakubiak & Feeney, 2017). As with sleep, these effects potentially occur indirectly by enhancing regulatory capacity and directly via neural/physiological processes (Coan et al., 2006; Ditzen et al., 2007; Holt-Lunstad et al., 2008). In couples, affect regulation and touch can have synergistic effects and reciprocal associations with relationship satisfaction. For example, partners’ morning positive mood is associated with affectionate touch frequency within the prior 24 h, and affectionate touch mediates the positive relationship between sexual contact and well-being (Debrot et al., 2017). Couples report lower negative affect after conflict if they hugged the prior day (Murphy et al., 2018). Overall, partners’ satisfaction with affectionate touch in their relationship is associated with better perceived relationship quality (Dainton et al., 1994; Wagner et al., 2020).
We posit that in healthy adults, touch during and surrounding sleep may add to restorative and affect resetting/regulatory functions of touch or sleep alone. The intersection of these, especially in a meaningful social context (e.g., marriage), may have synergistic effects to enhance positive mood, reduce negative mood, and benefit dyadic interactions post-waking. We note that although subjective reports cannot pinpoint the extent of actual touch during sleep, perceptions of sleep-touch reported upon awakening can capture the experience of touch during hypnagogic (falling asleep) and hypnopompic (waking up) states. Thus, we examined how subjective reports of sleep-touch were associated with subjective reports of next-day affect upon awakening and during spousal interactions. We focused on calm/happy mood (a low-arousal positive state to start the day or engage with a partner) and angry/irritable mood, given associations of anger with disrupted sleep (Krizan & Hisler, 2019; Minkel et al., 2012) and problematic marital interactions.
Current Study
For the current study, we asked married heterosexual couples to provide 14 days of twice-daily diary submissions, including morning sleep-touch and mood reports and evening reports of positive and negative spousal events and quality of spousal interactions. We hypothesized that morning reports of more sleep-touch would be associated with morning reports of (H1) happier/calmer mood and (H2) less angry/irritable mood, which would in turn be associated respectively with evening reports of (H3) more positive and (H4) fewer negative events with their spouse, and with evening ratings of (H5) more enjoyable and (H6) less stressful spousal interactions.
To test direct and indirect (via morning mood) effects of sleep-touch, we proposed two dyadic mediated models (one each for positively valenced and negatively valenced variables; see Fig. 1). We controlled for prior evening reports of mood, morning reports of subjective sleep quality and non-sleep-related physical affection, day in study, and weekend versus weekday. We hypothesized similar actor and partner effects, with own (actor) sleep-touch expected to be a more consistent predictor of outcomes. Finally, we expected these processes to operate similarly for both spouses.
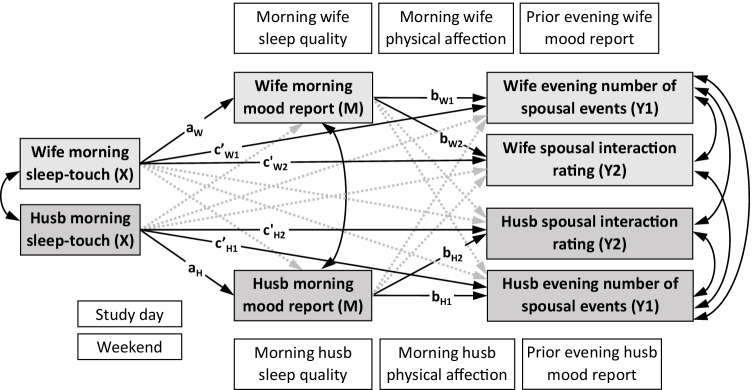
Fig. 1.
Dyadic mediation model. Note. Husb, husband; X, exogenous predictor; M, mediator; Y, final outcome. Gray boxes represent exogenous predictors, mediators, and final outcomes. Subscript H, husband; subscript W, wife. White boxes represent covariates. Black solid arrows represent hypothesized actor effects and correlations. Gray dashed arrows represent hypothesized partner effects. Paths representing effects of covariates are omitted for clarity
Method
Participants
Recruitment and Inclusion Criteria
Married couples were recruited locally using flyers, advertisements on Facebook, Craigslist, a graduate student listserv at the university, and referrals from previous participants. The “Healthy Couples Project” was described as a study of relationships involving twice-daily online questionnaires from both spouses for two weeks, followed by an online survey and a one-time session in the laboratory. Eligibility for the diary portion of the study required (1) 6 months in current marriage; (2) age between 21 and 70 years old; (3) internet access shortly after waking and prior to going to bed; (4) marital happiness rating of 2 or above on a scale ranging from 0 (very unhappy) to 6 (perfectly happy); and (5) score below 14 on the Public Health Questionnaire 8-item version (PHQ-8, Kroenke et al., 2009), a measure of ongoing depressive symptoms (the 8-item version parallels the original PHQ-9 [Kroenke et al., 2001] but omits the item concerning suicidal ideation).
We enrolled 277 couples. Forty-seven couples were omitted either for submission of data for fewer than seven consecutive days or for substantial backfilling of the diaries as detected from timestamps. For these 47 couples, both husbands, F(1,229) = 6.21, p = 0.013, and wives, F(1,236) = 9.736, p = 0.002, in the excluded group were older than those who were retained; excluded group husbands, M = 40.3, SD = 11.9; wives, M = 39.7, SD = 12.2. No other demographics differed between the excluded and retained participants.
Five additional couples were excluded for insufficient co-sleeping (i.e., reporting that they sometimes or often slept in separate beds in the same room or in separate rooms). Thus, 225 couples provided data for the current report.
Sample Characteristics
Ages ranged from 23 to 67 years (husbands M = 35.1, SD = 9.2, median = 32; wives M = 33.2, SD = 9.0, median = 31); 80.6% identified as non-Hispanic White, 13.0% as Latinx, 3.7% as Asian-American, 2.2% as African-American, and 0.5% as other. The majority of participants (64.8%) reported attending some college or trade school, and an additional sizeable minority (29.7%) had at least some postgraduate education. Median annual household income was slightly below $60,000, with 81.5% of participants in full- or part-time employment.
Marital duration ranged from 6 months to 40 years (M = 7.9, SD = 8.5, median = 9.5). Marital quality, as assessed with the RDAS (see 8), was relatively high (range: 23 to 67 out of 69 possible; wives: M = 53.2, SD = 6.6, median = 54; husbands: M = 52.4, SD = 7.3, median = 53). Couples included in our analyses reported sharing a bed either every night (89.5%) or most nights (10.5%). Typical sleep quality was good on average per the PSQI (see 8; range: 0 to 17, where 5 or below indicates good sleep quality [Buysse et al., 1989]; wives: M = 5.1, SD = 2.7, median = 5.0; husbands: M = 5.7, SD = 2.9, median = 5.0).
Finally, ratings at screening suggested that depressive symptoms (PHQ-8 scores) were low (range: 0 to 11, where below 10 indicates no clinical depression [Kroenke et al., 2009]; wives: M = 1.5, SD = 2.0; husbands: M = 1.4, SD = 2.0). Depressive symptoms, subsequently measured using the full CES-D (see 8), also were low (range 0 to 51; wives: M = 8.4, SD = 7.2, median = 7.0; husbands: M = 8.7, SD = 6.4, median = 7.0) where 16 or greater indicates risk for clinical depression [Radloff, 1977]).
Procedure
All procedures were approved by the university’s institutional review board and followed APA ethical guidelines for the protection of human subjects. This study was not pre-registered; data are available via https://osf.io/c4sw5/. After enrolling, spouses were assigned separate userIDs in the study’s Google domain (e.g., 185wife, 185husband), enabling them to receive emails and submit diary information separately. Both were asked to fill out morning assessments (within the first hour or so of arising) and evening assessments (within an hour or so of retiring for the night) each day for 14 days. The morning and evening assessments were not identical, and were accessed using individual links to two Google forms. Informed consent was presented when participants opened each assessment; submission of data was considered consent. In addition to standard confidentiality assurances, the consent form specified that data submitted by one spouse would not be shared with the other spouse by study staff.
When submitted by a participant, the data (along with a time and date stamp) were automatically added to the morning or evening assessment database under his or her userID. Trained research personnel checked approximately daily for missing diary entries and sent email reminders when needed. After spouses completed diary data collection, each was sent an individual link to a SurveyMonkey online survey (“Healthy Couples Questionnaire” or HCQ). At the end of their participation, the spouses received their payment separately. Couples were compensated for diary participation with $35 per spouse in Target gift cards.
Measures
Morning Diary Assessments
Bedtime and Waketime
Participants reported the time they went to bed on the previous evening and the time they awoke on the current morning.
Sleep Quality
Subjective sleep quality was measured with a single item, “On a scale of zero to ten, please rate your overall sleep quality last night” (anchored by 0 = extremely poor and 10 = extremely good).
Sleep-Touch
Sleep-touch was measured with a single item, “How much physical contact did you have with your partner during sleep last night?” Response choices were none, a little, a moderate amount, quite a bit, and a great deal (coded as 0 to 4).
Physical Affection
Participants indicated whether or not they had exchanged physical affection and/or had sexual relations with their spouse since the previous evening’s diary submission (both coded as 0 = no, 1 = yes).
Moods/Emotions
Using the response options not at all, a little bit, moderately, quite a bit, and extremely (coded as 0 to 4), participants were asked to “rate the extent to which you felt the following emotions or moods since last night’s diary.” We used ratings of calm, happy, and relaxed to indicate calm/happy mood states and ratings of angry and irritable to indicate angry/irritable mood states. Other adjectives (afraid, enthusiastic, lonely, loved, loving, nervous, and sad) were also rated, but were not used in the current study.
Evening Diary Assessments
Event Checklist
The checklist included the following 10 positive or negative events that could have occurred with the participant’s spouse since the previous evening’s diary submission, as follows. Positive events: received a special gift from (or gave a gift to) your spouse; you verbally expressed love to your spouse; celebrated special occasion with spouse; your spouse verbally expressed love to you; relations with spouse changed for the better. Negative events: argued with your spouse; critical of spouse; criticized by spouse; ignored by spouse; spouse turned down an opportunity to spend time with you. Separate sums were derived for positive and negative events (resulting in scores from 0 to 5).
Interaction Ratings
Enjoyment (spousal enjoyment) was rated using a single item, “Overall, how enjoyable was the time you spent with your spouse since last night’s diary?” Perceived stress (spousal stress) was also rated using a single item, “Overall, how stressful were your relations with your spouse since last night’s diary?” Response choices for both items were no contact with spouse (scored as missing), not at all, a little bit, moderately, quite a bit, and extremely (coded as 0 to 4).
Moods/emotions
Using the format described above, we obtained mood ratings “since this morning’s diary.”
Healthy Couples Questionnaire
The HCQ included demographics, assessments of marital quality and typical sleep quality, co-sleeping (bed sharing) frequency, depressive symptoms, and measures of other individual differences that are not included in the current report.
Marital Quality
Marital quality was assessed using the Revised Dyadic Adjustment Scale (RDAS, Busby et al., 1995). The RDAS is a 14-item questionnaire with subscales measuring dyadic consensus, satisfaction, and cohesion. Scores can range from 1 to 69. Cronbach’s alpha was 0.84 for wives and 0.86 for husbands.
Typical Sleep Quality
Typical subjective sleep quality (during the past month) was assessed with the Pittsburgh Sleep Quality Index (PSQI, Buysse et al., 1989), a 24-item questionnaire (19 self-rated items, five partner-provided ratings) assessing seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The sum of these component scores yield one global sleep quality score, with higher scores reflecting worse sleep quality. Cronbach’s alpha for the seven component scores was 0.63 for wives and 0.66 for husbands.
Co-sleeping
Participants responded to three items generated in our laboratory: “How often do you and your spouse…sleep in the same bed?”; “…sleep in different beds in the same room?”; and “…sleep in different rooms?” Answer choice options were every night, most nights, sometimes, rarely, and never.
Depressive Symptoms
The Center for Epidemiological Studies Depression Scale (CES-D, Radloff, 1977) assesses the frequency of occurrence of both feelings and behaviors typical of depression. It comprises 20 items reported on a 4-point scale reflecting frequency of occurrence during the past week; the scale ranges from 1 (rarely or less than one day) to 4 (most of the time or 5–7 days); higher sums represent more frequent symptoms. Cronbach’s alpha was 0.88 for wives and 0.85 for husbands.
Data Analysis
The primary goal of the current study was to investigate whether spouses’ experiences of physical contact with each other during and surrounding sleep (sleep-touch, as reported in the morning) carried forward in time, potentially influencing their own and each other’s concurrent morning mood and subsequent positive and negative spousal experiences on that day. Given this focus on daily effects and the hierarchical data structure, with individual daily reports (Level 1) nested within couples (Level 2), we analyzed the data using multilevel path analysis with observed variables, under Mplus Version 8.4 (Muthen & Muthen, ©1998–2019).
Distinguishability
Although we did not make directional predictions regarding differences between spouses, we conducted preliminary tests for such differences to evaluate dyad distinguishability. Three significant spouse differences were found in each of the models (see Preliminary Analyses). Given conceptual and theoretical reasons supporting distinguishability, the fact that previous researchers have found gender differences in touch- and sleep-related constructs such as desire for touch in relationships (Jakubiak et al., 2021) and subjective sleep quality (Fatima et al., 2016), and the empirical differences we uncovered, we opted to treat the dyads as distinguishable. We used a dual-intercept framework, in which separate parameters were specified for each spouse at Level 1.
Data Inclusion
In the mornings, our participants self-reported the times at which they woke up that day and at which they went to bed on the prior evening. Their diary submissions were timestamped automatically by Google Forms. We defined the “gap” as the time between the timestamp on the relevant diary submission and a participant’s reported time of awakening (morning gap) or retiring (evening gap). As noted above, couples were excluded at the outset if they submitted fewer than seven consecutive days of diary entries or for substantial backfilling (long gaps). Within the 225 couples who were included in the analyses, individual couple-days were rejected if either the morning gap or the evening gap was greater than 4 h for either spouse. These exclusion rules resulted in the following: for morning gaps (husbands M = 64 min, SD = 53, median = 47; wives M = 60 min, SD = 51; median = 50) and for evening gaps (husbands M = 53 min, SD = 49, median = 37; wives M = 52 min, SD = 47, median = 38).
Missing Data
The 225 couples included in the current study submitted 3,510 couple-days of data. Of those days, 2,699 (76.9%) included both morning and evening submissions from both spouses. Wives submitted data at both mornings and evenings on 2,990 (85.2%) of days, whereas husbands did so on 2,873 (81.9%) of days. Within the couple-days used in the analyses, the average missingness rate for study variables measured in the morning was 11.1%, whereas for study variables measured in the evening, it was 15.8%. The average missingness rate across all of the study variables was 13.7%.
Parameter estimates were obtained using Bayesian estimation. Analogous to full information maximum likelihood treatment of missing data, this procedure provides for unbiased parameter estimates and accurate standard error equivalents (defined as the standard deviations of the posterior distributions) when data are missing either completely at random or at random. As such, Bayesian estimation provides for optimal treatment of incomplete data even when there is a larger proportion of missingness than in the current dataset (Asparouhov & Muthen, 2010; Asparouhov et al., 2018; Rubin, 1976).
Estimation
Bayesian estimation methods were implemented without thinning using the Markov Chain Monte Carlo procedure via the Gibbs sampler with two chains. We used non-informative prior distributions, so that the data at hand largely determined the final set of parameter values in the posterior parameter distributions. Convergence was assessed by the Potential Scale Reduction (PSR) values (Gelman & Rubin, 1992) using the Mplus default value of 1.10; both models initially converged with 500 or fewer iterations. Because use of the PSR values in this way can sometimes prematurely terminate estimation, final parameter estimates for all models were based on 30,000 iterations (15,000 burn-in). With longer chains, PSR values for all parameters in both models remained below 1.01 during the final 15,000 iterations.
Regarding centering, with Bayesian estimation, Mplus (versions 8.1 and above) automatically uses latent variable centering for both predictors and mediators in multilevel models. Simulation research shows that this form of centering performs better than observed variable centering, to which it is directly analogous (Asparouhov & Muthén, 2019). The significance of all effects, including indirect effects, was assessed using 95% Bayesian credibility intervals, which show excellent performance for mediation analysis (Biesanz et al., 2010; Wang & Preacher, 2015). Such intervals, like those obtained with bootstrapping methods, provide appropriate inference for indirect effects because they require no distributional assumptions for these effects and accordingly yield non-symmetric intervals. Exact one-tailed p-values given in the manuscript are derived from the posterior distributions.
Results
Preliminary Analyses
Model-estimated means, standard deviations, and within-level bivariate correlations for the variables of interest, separately for husbands and wives, are shown in Table 1. We note that for both spouses, mean subjective sleep quality was relatively high. Mean subjective sleep-touch was relatively low, perhaps because participants were uncertain about how much they touched during the night. Table 2 illustrates cross-correlations of the study variables between husbands and wives.
Table 1.
Means, standard deviations, and correlations of daily study variables, separately for husbands and wives
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Morning sleep-toucha | .18** | − .09** | .16** | − .02 | .08** | − .02 | .06* | .31** | .09** | − .06* | − .09** | .04 | ||
| 2 Morning happy/calm mooda | .29** | − .41** | .12** | − .09** | .05* | − .03 | .32** | .17** | .28** | − .09** | − .12** | .07** | ||
| 3 Morning angry/irrit mooda | − .13** | − .38** | − .10** | .20** | − .00 | .16** | − .27** | − .06* | − .11** | .14** | − .08** | − .01 | ||
| 4 Evening enjoyment spousea | .14** | .14** | − .05 | − .22** | .32** | − .23** | .02 | .08** | .08** | − .00 | − .08** | .14** | ||
| 5 Evening stress spousea | − .02 | − .06** | .09** | − .26** | − .03 | .48** | − .02 | − .01 | − .04 | .02 | .01 | .04 | ||
| 6 Evening spouse positive eventsb | .11** | .09** | .00 | .29** | − .04 | .07** | .05* | .07** | .05* | .05 | − .12** | .06** | ||
| 7 Evening spouse negative eventsb | .03 | − .02 | .14** | − .18** | .46** | .08** | .05* | − .03 | .01 | .00 | − .07** | .07** | ||
| 8 Morning sleep qualityc | .15** | .31** | − .20** | .06* | − .02 | .03 | − .01 | .04* | .06* | .02 | − .09** | .06* | ||
| 9 Morning physical affectiond | .36** | .26** | − .08** | .15** | − .02 | .13** | − .01 | .12** | .07** | .02 | − .19** | − .01 | ||
| 10 Prior evening happy/calm mooda | .08** | .30** | − .13** | .06* | − .04 | .08** | − .00 | .07* | .07** | − .35** | − .12** | .06** | ||
| 11 Prior evening angry/irrit mooda | − .04 | − .11** | .18** | .00 | .01 | .03 | .04 | − .00 | − .01 | − .33** | − .11** | − .01 | ||
| 12 Study daye | − .11** | − .16** | − .04 | − .09** | .04 | − .12** | − .07** | − .08** | − .23** | − .16** | − .10** | .02 | ||
| 13 Weekendf | .02 | .07** | − .03 | .16** | .06* | .11** | .09** | .07** | − .01 | .06* | .01 | .02 | ||
| Husband mean | 1.20 | 2.12 | 0.30 | 2.74 | 0.50 | 1.87 | 0.45 | 7.09 | 0.55 | 2.04 | 0.56 | 7.93 | 0.28 | |
| Husband standard deviation | 0.07 | 0.06 | 0.03 | 0.05 | 0.05 | 0.07 | 0.05 | 0.12 | 0.03 | 0.06 | 0.04 | 0.16 | 0.01 | |
| Wife mean | 1.19 | 2.13 | 0.32 | 2.79 | 0.50 | 1.95 | 0.63 | 7.21 | 0.61 | 2.02 | 0.65 | 7.93 | 0.28 | |
| Wife standard deviation | 0.07 | 0.06 | 0.03 | 0.05 | 0.04 | 0.08 | 0.06 | 0.10 | 0.03 | 0.06 | 0.04 | 0.16 | 0.01 | |
Estimates derived using Bayes estimator; N(couple-days) = 2,128; N(couples) = 222. Correlations are standardized within-person covariances. Correlation estimates for husbands in lower triangle; estimates for wives in upper triangle. Morning = morning report, evening = evening report, prior evening = report from prior evening. Irrit = irritable; enjoyment spouse = enjoyment of time spent with spouse; stress spouse = stressfulness of relations with spouse; spouse positive events = positive events with spouse; spouse negative events = negative events with spouse. aRatings, range = 0 to 4; bSum of events, range = 0 to 5; cRatings, range = 0 to 10; d0 = did not occur, 1 = did occur; eRange = 7 to 30; f0 = weekday, 1 = Saturday or Sunday
*p < .05. **p < .01
Table 2.
Correlations between husbands’ and wives’ values of daily study variables
| Study variables | W1 | W2 | W3 | W4 | W5 | W6 | W7 | W8 | W9 | W10 | W11 | W12 | W13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | H Morning sleep-toucha | .53** | .16** | − .06** | .10** | .015 | .07** | .01 | .06* | .31** | .07** | − .04 | − .11** | .02 |
| 2 | H Morning happy/calm mooda | .21** | .24** | − .13** | .05 | − .07** | .04 | − .01 | .11** | .15** | .14** | − .11** | − .16** | .07** |
| 3 | H Morning angry/irrit mooda | − .09** | − .18** | .26** | − .04 | .10** | .01 | .09** | − .07* | − .07** | − .07* | .12** | − .04 | − .03 |
| 4 | H Evening enjoyment spousea | .13** | .08** | − .11** | .42** | − .17** | .20** | − .14** | .04 | .11** | .04 | − .01 | − .09** | .16** |
| 5 | H Evening stress spousea | − .02 | − .07** | .13** | − .19** | .37** | − .02 | .35** | .01 | − .02 | − .01 | − .02 | .04 | .06* |
| 6 | H Evening positive spouse eventsb | .09** | .06* | − .01 | .22** | .01 | .33** | .05* | .01 | .09** | .02 | .03 | − .12** | .11** |
| 7 | H Evening negative spouse eventsb | − .01 | − .03 | .16** | − .14** | .37** | .01 | .50** | .03 | − .01 | .00 | − .01 | − .07** | .09** |
| 8 | H Morning sleep qualityc | .09** | .11** | − .09** | .01 | − .04 | .04 | − .00 | .22** | .04 | .06* | − .04 | − .08** | .07** |
| 9 | H Morning physical affectiond | .28** | .14** | − .06* | .10** | − .01 | .11** | − .00 | .04 | .36** | .06** | − .02 | − .23** | − .01 |
| 10 | H Prior evening happy/calm mooda | .05* | .14** | − .06* | .02 | − .03 | .02 | − .01 | .03 | .05* | .21** | − .13** | − .16** | .06* |
| 11 | H Prior evening angry/irrit mooda | − .02 | − .10** | .08** | − .01 | .04 | .00 | .05 | − .01 | .02 | − .21** | .29** | − .10** | .01 |
| 12 | H Study daye | − .09** | − .12** | − .08** | − .08** | .01 | − .12** | − .07** | − .09** | − .19** | − .12** | − .11** | 1.00 | .02 |
| 13 | H Weekendf | .04 | .07** | − .01 | .14** | .04 | .06** | .07** | .06* | − .01 | .06** | − .01 | .02 | 1.00 |
Estimates derived using Bayes estimator; N(couple-days) = 2,128; N(couples) = 222. Correlations are standardized Level 1 covariances. Bold estimates on diagonal = cross-correlations between husbands’ and wives’ values of the same variables. H, husband value; W, wife value. Morning = morning report, evening = evening report, prior evening = report from prior evening. Enjoyment spouse = enjoyment of time spent with spouse; stress spouse = stressfulness of relations with spouse
aRatings, range = 0 to 4; bSum of events, range = 0 to 5; cRatings, range = 0 to 10; d0 = did not occur, 1 = did occur; eRange = 7 to 30; f0 = weekday, 1 = Saturday or Sunday
*p < .05. **p < .01
As noted above, differences between spouses were found in each of the two models during assessment for dyad distinguishability (see Table 3).
Table 3.
Differences between spouses of estimated path coefficients and means in positively and negatively valenced models
| Estwife | Esthusb | Estdiff | SDdiff | p1-tail | 95% CIdiff | ||
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Positively valenced model | |||||||
| Evening spouse positive events ON weekend | 0.104 | 0.219 | 0.116 | 0.048 | .008 | 0.022 | 0.209 |
| Evening spouse positive events ON sleep quality | 0.026 | − 0.016 | − 0.042 | 0.018 | .012 | − 0.078 | − 0.006 |
| Physical affection | 0.609 | 0.553 | − 0.056 | 0.027 | .022 | − 0.110 | − 0.001 |
| Negatively valenced model | |||||||
| Morning angry-irritable mood ON sleep quality | − 0.095 | − 0.072 | 0.023 | 0.009 | .006 | 0.005 | 0.041 |
| Evening stress spouse ON angry-irritable mood | 0.228 | 0.093 | − 0.135 | 0.051 | .005 | − 0.234 | − 0.034 |
| Physical affection | 0.610 | 0.554 | − 0.056 | 0.027 | .021 | − 0.109 | − 0.002 |
Estwife and esthusb, parameter estimates for wife and husband, respectively; estdiff, difference between spouses’ parameter estimates; SDdiff, standard deviation of posterior distribution of difference estimates; CI, credibility interval for differences estimates; LL, lower limit; UL, upper limit. Evening = evening report; morning = morning report. Spouse positive events = positive events with spouse; stress spouse = stressfulness of relations with spouse
Testing the Models
Results are displayed in Table 4 (for positively valenced models) and Table 5 (for negatively valenced models). Actor and partner within-person effects of morning-reported sleep-touch on morning mood reports (mediators) and evening variables (final outcomes), along with actor and partner effects of mediators on final outcomes, are described for both models. All results presented refer to associations relative to that individual’s own mean.
Table 4.
Unstandardized coefficients, standard deviations of posterior distributions, significance levels, and upper and lower 95% credibility intervals for total, direct, indirect, and covariate effects in positively valenced model
| Antecedent variables | A/P | Mediator (M) | Final outcomes (Y1, Y2) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Morning happy/calm mooda | Evening positive eventsb (Y1) | Evening enjoymentb (Y2) | ||||||||||||||
| Coeff | SDp | β | p1-tail | CI [LL,UL] | Coeff | SDp | β | p1-tail | CI [LL,UL] | Coeff | SDp | β | p1-tail | CI [LL,UL] | ||
| Effects for wives | ||||||||||||||||
| Total effects (path c) | .067 | .026 | .065 | .006 | .015, .119 | .132 | .023 | .151 | .000 | .087, .177 | ||||||
| Hypothesized direct effects | ||||||||||||||||
| Sleep-toucha (path a; path c′) | A | .086 | .017 | .118 | .000 | .053, .119 | .068 | .027 | .066 | .006 | .015, .120 | .123 | .023 | .141 | .000 | .078, .168 |
| Sleep-toucha | P | .032 | .017 | .044 | .030 | − .001, .067 | .007 | .028 | .007 | .395 | − .047, .061 | .013 | .024 | .015 | .285 | − .034, .060 |
| Happy/calm mooda (path b) | A | − .007 | .034 | − .005 | .418 | − .074, .0059 | .099 | .030 | .084 | .000 | .041, .158 | |||||
| Happy/calm mooda | P | .009 | .033 | .006 | .389 | − .055, .073 | .013 | .029 | − .005 | .413 | − .062, .050 | |||||
| Hypothesized indirect effects (path ab) | − .001 | .003 | − .001 | .418 | − .007, .005 | .008 | .003 | .010 | .000 | .003, .015 | ||||||
| Covariates | ||||||||||||||||
| Subjective sleep qualitya | A | .126 | .008 | .292 | .000 | .110, .140 | .026 | .013 | .043 | .023 | .000, .051 | − .006 | .011 | − .011 | .306 | − .028, .017 |
| Occurrence of physical affectiona | A | .165 | .032 | .105 | .000 | .103, .226 | .092 | .048 | .042 | .026 | − .001, .186 | .004 | .041 | .002 | .462 | − .075, .086 |
| Prior evening happy/calm moodc | A | .266 | .023 | .235 | .000 | .220, .311 | .062 | .035 | .039 | .037 | − .006, .130 | .033 | .029 | .025 | .128 | − .023, .091 |
| Study day | − .004 | .003 | − .030 | .068 | − .009, .001 | − .019 | .004 | − .105 | .000 | − .027, − .011 | − .010 | .004 | − .061 | .003 | − .017, − .002 | |
| Weekend | .046 | .026 | .032 | .037 | − .005, .067 | .104 | .039 | .052 | .005 | .026, .181 | .221 | .035 | .130 | .000 | .153, .290 | |
| Explained variance | .177 | .013 | − | .000 | .152, .205 | .028 | .006 | − | .000 | .017, .041 | .059 | .010 | − | .000 | .042, .080 | |
| Effects for husbands | ||||||||||||||||
| Total effects (path c) | .063 | .028 | .061 | .011 | .009, .118 | .072 | .023 | .088 | .001 | .028, .117 | ||||||
| Hypothesized direct effects | ||||||||||||||||
| Sleep-toucha (path a; path c′) | A | .106 | .017 | .149 | .000 | .073, .138 | .059 | .028 | .057 | .017 | .005, .115 | .064 | .023 | .078 | .002 | .019, .109 |
| Sleep-toucha | P | .041 | .016 | .058 | .007 | .009, .073 | .029 | .026 | .028 | .134 | − .022, .080 | .043 | .022 | .053 | .023 | .001, .086 |
| Happy/calm mooda (path b) | A | .034 | .037 | .024 | .173 | − .037, .106 | .078 | .030 | .068 | .004 | .019, .136 | |||||
| Happy/calm mooda | P | .015 | .031 | .011 | .311 | − .046, l007 | .028 | .026 | .025 | .146 | − .024, .079 | |||||
| Hypothesized indirect effects (path ab) | .004 | .004 | .004 | .173 | − .004, .012 | .008 | .003 | .010 | .004 | .002, .016 | ||||||
| Covariates | ||||||||||||||||
| Subjective sleep qualitya | A | .115 | .008 | .275 | .000 | .099, .131 | − .016 | .014 | − .026 | .132 | − .042, .012 | − .005 | .011 | − .011 | .312 | − .024, .016 |
| Occurrence of physical affectiona | A | .202 | .030 | .141 | .000 | .143, .260 | .161 | .048 | .042 | .000 | .066, .254 | .106 | .037 | .064 | .003 | .031, .178 |
| Prior evening happy/calm moodc | A | .272 | .023 | .245 | .000 | .227, .316 | .064 | .036 | .039 | .040 | − .007, .135 | .020 | .029 | .015 | .250 | − .037, .077 |
| Study day | − .006 | .003 | − .050 | .006 | − .011, − .001 | − .016 | .004 | − .089 | .000 | − .024, − .008 | − .007 | .003 | − .051 | .014 | − .014, − .001 | |
| Weekend | .045 | .025 | .032 | .038 | − .005, .093 | .219 | .040 | .109 | .000 | .139, .298 | .248 | .033 | .130 | .000 | .184, .312 | |
| Explained variance | .196 | .014 | − | .000 | .152, .205 | .040 | .007 | − | .000 | .027, .056 | .061 | .009 | − | .000 | .044, .080 | |
N = 2,851 couple-days; N = 225 couples. A, actor effect on actor; P, partner effect on actor; Coeff, unstandardized regression coefficient; SDp, standard deviation of posterior distribution; β, standardized regression coefficient; p1-tail, one-tailed p value; CI [LL,UL], 95% credibility interval (lower limit, upper limit). Effects in bold font are statistically significant at two-tailed p < .05 or less
aFrom morning assessment; refers to time since prior evening assessment; bFrom evening assessment of positive events and enjoyment; refers to time since prior evening assessment; cFrom prior evening assessment of mood; refers to time since prior morning assessment
Table 5.
Unstandardized coefficients, standard deviations of posterior distributions, standardized coefficients, significance levels, and upper and lower 95% credibility intervals for total, direct, indirect, and covariate effects in negatively valenced model (fully updated 7/11/21)
| Antecedent variables | A/P | Mediator (M) | Final outcomes (Y1, Y2) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Morning angry/irritable mooda | Evening negative eventsb (Y1) | Evening stressb (Y2) | ||||||||||||||
| Coeff | SDp | β | p1-tail | CI [LL,UL] | Coeff | SDp | β | p1-tail | CI [LL,UL] | Coeff | SDp | β | p1-tail | CI [LL,UL] | ||
| Effects for wives | ||||||||||||||||
| Total effects (path c) | − .010 | .029 | − .009 | .367 | − .066, .046 | − .007 | .022 | − .009 | .369 | − .051, .036 | ||||||
| Hypothesized direct effects | ||||||||||||||||
| Sleep-toucha (path a; path c′) | A | − .037 | .014 | − .063 | .004 | − .064, − .009 | .000 | .029 | .000 | .493 | − .056, .056 | .001 | .022 | .001 | .482 | − .042, .044 |
| Sleep-toucha | P | − .016 | .021 | − .027 | .226 | − .057, .025 | .030 | .030 | .026 | .156 | − .027, .089 | .041 | .022 | .050 | .033 | − .003, .085 |
| Angry/irritable mooda (path b) | A | .276 | .043 | .145 | .000 | .192, .360 | .228 | .034 | .163 | .000 | .162, .294 | |||||
| Angry/irritable mooda | P | .122 | .045 | .061 | .004 | .033, .209 | .076 | .035 | .052 | .015 | .007, .145 | |||||
| Hypothesized indirect effects (path ab) | − .010 | .004 | − .009 | .004 | − .019, − .002 | − .008 | .003 | − .010 | .004 | − .016, − .002 | ||||||
| Covariates | ||||||||||||||||
| Subjective sleep qualitya | A | − .095 | .007 | − .272 | .000 | − .108, − .082 | .042 | .013 | .063 | .001 | .016, .068 | .000 | .011 | .001 | .485 | − .021, .022 |
| Occurrence of physical affectiona | A | − .049 | .026 | − .039 | .031 | − .101, .003 | − .073 | .049 | − .030 | .068 | − .170, .023 | − .011 | .040 | − .006 | .393 | − .088, .068 |
| Prior evening angry/irritable moodc | A | .079 | .016 | .106 | .000 | .049, .110 | − .041 | .028 | − .029 | .070 | − .097, .013 | .005 | .023 | .005 | .412 | − .039, .049 |
| Study day | − .011 | .002 | − .100 | .000 | − .015, − .006 | − .014 | .004 | − .072 | .000 | − .023, − .006 | .002 | .003 | .012 | .298 | − .005, .008 | |
| Weekend | − .002 | .022 | − .002 | .456 | − .044, .040 | .119 | .043 | .054 | .003 | .035, .202 | .065 | .033 | .040 | .024 | .001, .129 | |
| Explained variance | .090 | .011 | − | .000 | .084, .130 | .043 | .008 | − | .000 | .028, .060 | .040 | .008 | − | .000 | .025, .058 | |
| Effects for husbands | ||||||||||||||||
| Total effects (path c) | .042 | .028 | .040 | .071 | − .013, .097 | .011 | .023 | .014 | .321 | − .033, .056 | ||||||
| Hypothesized direct effects | ||||||||||||||||
| Sleep-toucha (path a; path c′) | A | − .046 | .014 | − .081 | .001 | − .073, − .018 | .050 | .028 | .048 | .038 | − .005, .105 | .015 | .023 | .019 | .257 | − .029, .060 |
| Sleep-toucha | P | − .032 | .025 | − .024 | .094 | − .081, .016 | − .006 | .026 | − .006 | .405 | − .058, .045 | − .016 | .021 | − .019 | .226 | − .057, .025 |
| Angry/irritable mooda (path b) | A | .180 | .043 | .098 | .000 | .094, .265 | .093 | .036 | .065 | .005 | .021, .164 | |||||
| Angry/irritable mooda | P | .184 | .039 | .105 | .000 | .107, .262 | .134 | .032 | .098 | .000 | .071, .197 | |||||
| Hypothesized indirect effects (path ab) | − .008 | .003 | − .008 | .001 | − .015, − .003 | − .004 | .002 | − .005 | .006 | − .009, − .001 | ||||||
| Covariates | ||||||||||||||||
| Subjective sleep qualitya | A | − .072 | .007 | − .214 | .000 | − .085, − .059 | .013 | .013 | .021 | .154 | − .012, .038 | − .003 | .011 | − .006 | .398 | − .024, .019 |
| Occurrence of physical affectiona | A | − .047 | .025 | − .041 | .028 | − .096, .001 | − .027 | .045 | − .013 | .268 | − .118, .059 | − .011 | .040 | .003 | .393 | − .088, .068 |
| Prior evening angry/irritable moodc | A | .122 | .017 | .157 | .000 | .089, .155 | − .002 | .029 | − .001 | .476 | − .059, .055 | − .019 | .024 | − .017 | .213 | − .066, .028 |
| Study day | − .007 | .002 | − .065 | .001 | − .011, − .002 | − .012 | .004 | − .067 | .000 | .082, .236 | .005 | .003 | .034 | .079 | − .002, .012 | |
| Weekend | − .010 | .021 | − .009 | .312 | − .052, .031 | .119 | .043 | .079 | .003 | .035, .202 | .096 | .033 | .061 | .002 | .030, .160 | |
| Explained variance | .106 | .012 | − | .000 | .084, .130 | .042 | .008 | − | .000 | .027, .060 | .025 | .007 | − | .000 | .014, .040 | |
N = 2,851 couple-days; N = 225 couples. A, actor effect on actor; P, partner effect on actor; Coeff, unstandardized regression coefficient; SDp, standard deviation of posterior distribution; β, standardized regression coefficient; p1-tail, one-tailed p value; CI [LL, UL], 95% credibility interval (lower limit, upper limit). Effects in bold font are statistically significant at two-tailed p < .05 or less
aFrom morning assessment; refers to time since prior evening assessment; bFrom evening assessment of negative events and stress; refers to time since prior evening assessment; cFrom prior evening assessment of mood; refers to time since prior morning assessment
Positively Valenced Model
Sleep-Touch → Happy/Calm Mood → Positive Spousal Events
The total effects (ab + c′) for evening positive spousal events regressed on morning sleep-touch were significant for both wives and husbands (see Table 4 for full results; see Fig. 2 for illustrated path model).
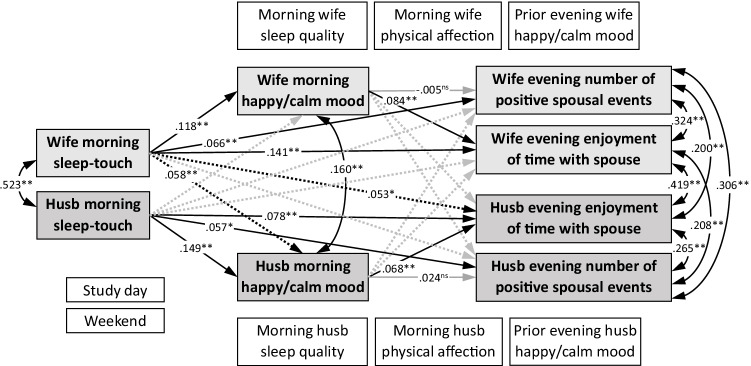
Fig. 2.
Positively valenced model. Note. Standardized estimates. Husb, husband. Gray boxes represent exogenous predictors, mediators, and final outcomes. White boxes represent covariates. Black arrows represent significant hypothesized paths and correlations. Gray arrows represent non-significant hypothesized paths. Solid arrows represent actor effects on actor; dashed arrows represent partner effects on actor. Coefficients for non-significant partner effects, along with all paths representing actor effects of covariates, are omitted for clarity (see Table 4 for results)
Furthermore, as predicted in H1, greater reported sleep-touch (relative to each spouse’s own mean) was significantly associated directly with morning reports of happier/calmer mood (path a) for both spouses. Contrary to H3, however, morning happy/calm mood was not significantly associated with the number of positive spousal events reported in the evening of the same day (path b) either for wives or for husbands. Accordingly, the predicted indirect paths (path ab) also were non-significant for both spouses. The direct paths (path c′), however, were significant for both spouses, such that greater sleep-touch predicted more positive spousal events. In short, there were significant overall positive associations between morning sleep-touch and evening positive events for both spouses, but these associations were not fully mediated by morning happy/calm mood.
No partner effects were found for wives. For husbands, there was a significant partner effect on morning happy/calm mood in the predicted direction, such that wives’ reports of more sleep-touch were associated with happier/calmer mood reported by husbands. The difference between these partner effects was not significant; therefore, the results cannot be interpreted as a gender difference.
Sleep-Touch → Happy/Calm Mood → Spousal Enjoyment
The total effects (ab + c′) for evening spousal enjoyment regressed on morning sleep-touch were significant for both wives and husbands (see Table 4 for full results; see Fig. 2 for illustrated path model). Furthermore, as noted above for H1, greater reported sleep-touch was significantly associated with morning reports of happier/calmer mood (path a) for both wives and husbands. As predicted in H5, greater evening spousal enjoyment was significantly related to happier/calmer morning mood (path b) for both spouses. Consequently, the predicted indirect paths (path ab) also were significant for both spouses. The direct paths (path c′) also were significant for both spouses. In sum, there were significant overall positive associations between morning sleep-touch and evening reports of greater spousal enjoyment for both spouses. The indirect paths through morning happy/calm mood, although significant, explained only a small portion of this association, as the direct paths from sleep-touch to evening spousal enjoyment also remained significant.
Again, no partner effects were found for wives. For husbands, there was a significant partner effect on spouse enjoyment, such that wives’ reports of more sleep-touch were directly associated with greater spouse enjoyment reported by husbands. The difference between these partner effects was not significant; therefore, the results cannot be interpreted as a gender difference.
Positive Model Covariates
Associations of covariates with morning reports of happy/calm mood followed similar, but not identical, patterns for wives and husbands (see Table 4 for full results). Morning reports of better subjective sleep quality and occurrence of non-sleep-related physical affection, along with prior evening reports of happier/calmer mood, were significantly related to happier/calmer morning mood. Weekend versus weekday was unrelated to morning mood for both spouses. Later day in the study predicted lower happy/calm mood reports for husbands but not wives.
Associations of the covariates with evening outcomes were similar between spouses in the following ways: Both spouses reported more positive spousal events and greater spouse enjoyment on weekends than on weekdays, and later day in the study predicted reports of fewer positive spousal events and less spouse enjoyment for both husbands and wives. Happy/calm mood reported on the prior evening did not predict evening positive spousal events or spouse enjoyment for either spouse. Finally, subjective sleep quality was not related to spouse enjoyment ratings for either spouse. On the other hand, covariate associations differed between spouses as follows: Better subjective sleep quality was significantly associated with more evening positive spousal events for wives but not husbands, whereas occurrence of non-sleep-related physical affection was significantly associated with more evening positive spousal events for husbands but not wives. Occurrence of non-sleep-related physical affection also predicted greater spousal enjoyment ratings for husbands, but not for wives.
Negatively Valenced Model
Sleep-Touch → Angry/Irritable Mood → Negative Spousal Events
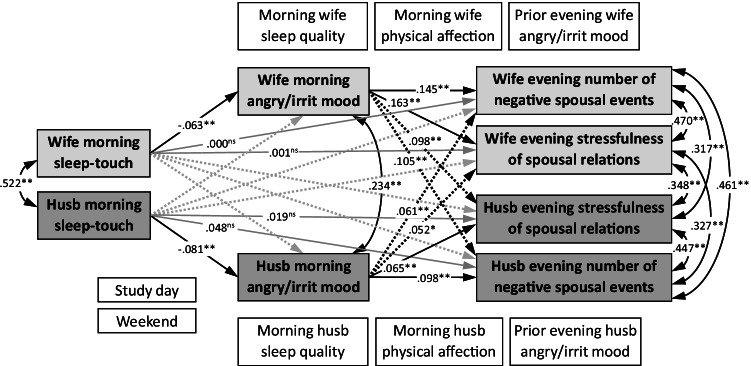
The total effects (ab + c′) for evening positive spousal events regressed on morning sleep-touch were non-significant for both wives and husbands (see Table 5 for full results; see Fig. 3 for illustrated path model). Nevertheless, as predicted in H2, greater reported sleep-touch was significantly associated with morning reports of less angry/irritable mood (path a) for both spouses. Also as predicted in H4, morning angry/irritable mood was significantly associated with fewer negative spousal events reported in the evening of the same day (path b) for both spouses. Accordingly, the predicted indirect paths (path ab) also were significant for both spouses, such that greater sleep-touch predicted evening reports of fewer negative spousal events. The direct paths (path c′), however, were not significant for either wives or husbands. To summarize, the overall associations between morning sleep-touch and evening negative spousal events were not significant for either spouse, but there were significant indirect effects in the predicted direction: greater sleep-touch was associated with fewer negative spousal events via less angry/irritable mood reported on the morning of the same day for both husbands and wives.
Fig. 3.
Negatively valenced model. Note. Standardized estimates. Husb, husband. Gray boxes represent exogenous predictors, mediators, and final outcomes. White boxes represent covariates. Black arrows represent correlations and significant hypothesized paths. Gray arrows represent non-significant hypothesized paths. Solid arrows represent actor effects on actor; dashed arrows represent partner effects on actor. Coefficients for non-significant partner effects, along with all paths representing actor effects of covariates are omitted for clarity (see Table 5 for results)
Partner effects were found for both spouses, in which one spouse’s reports of angrier/more irritable mood in the morning were associated with the other spouse’s evening reports of more negative spousal events.
Sleep-Touch → Angry/Irritable Mood → Spousal Stress
The total effects (ab + c′) for evening ratings of stress of spousal interactions regressed on morning sleep-touch were not significant for either wives or husbands (see Table 5 for full results; see Fig. 3 for illustrated path model). However, as described above for H2, greater reported sleep-touch was significantly associated with morning reports of less angry/irritable mood (path a) for both wives and husbands. As predicted in H6, more angry/irritable morning mood was significantly related to greater evening spousal stress (path b) for both spouses. Consequently, the predicted indirect paths (path ab) also were significant for both wives and husbands, such that more angry/irritable morning mood was linked with greater spousal stress reported in the evening. The direct paths (path c′) were not significant for either spouse. In short, although the overall associations between morning sleep-touch and evening negative spousal events were not significant, there were significant indirect effects in the predicted direction: for both spouses, more sleep-touch was associated with lower evening ratings of spouse-associated stress via less angry/irritable mood reported on the morning of the same day.
Similar to those described above, partner effects were found for both spouses, in which one spouse’s reports of angrier/more irritable mood in the morning were associated with the other spouse’s evening reports of more spousal stress.
Negative Model Covariates
The patterns of associations of the covariates with morning reports of angry/irritable mood were identical for wives and husbands. Greater angry/irritable mood in the morning was significantly related to morning reports of worse subjective sleep quality and to prior evening reports of more angry/irritable mood for both spouses. Morning reports of non-sleep-related physical affection were not significantly related to morning angry/irritable mood for either wives or husbands.
The patterns of associations of the covariates with evening outcomes were also identical; neither negative spousal events nor spousal stress were significantly related to subjective sleep quality, occurrence of non-sleep-related physical affection, or prior evening reports of angry/irritable mood for either wives or husbands. Later day in the study was associated with fewer reported negative spousal events for both spouses. Finally, both spouses reported more negative spousal events and greater spousal stress on weekends than on weekdays.
Discussion
Co-sleeping is common; yet, the role of physical contact during sleep remains underexplored. We examined sleep-touch, the extent to which partners reported touching during sleep, and its links to mood and spouses’ experience of marital interactions. Diary ratings revealed that on mornings when spouses reported more sleep-touch, they each reported happier/calmer and less angry/irritable morning mood. More sleep-touch also was directly linked to evening reports of more positive spousal events and enjoyment. Husbands reported better morning mood and more evening enjoyment when wives reported more sleep-touch (but not vice-versa).
As predicted, sleep-touch linked indirectly with spousal enjoyment via happy/calm morning mood for both spouses. Surprisingly, despite these links, most of the association between sleep-touch and the two positive relational outcomes was not accounted for by differences in morning mood, suggesting that sleep-touch benefits may be incurred instead via physiological or marital/relationship changes. In contrast, sleep-touch was related only indirectly to spouse-related stress and negative spousal events, suggesting that a relative lack of sleep-touch may be unrelated to relationship problems unless mood effects take hold. Indeed, both spouses’ negative evening outcomes were predicted not only by their own, but even by their partner’s angry/irritable morning mood.
Notably, the aforementioned associations held even after accounting for effects of sleep quality, physical affection, and other covariates. Consistent with prior findings, better subjective sleep quality was associated with happier/calmer and less angry/irritable morning mood, and non-sleep-related physical affection was associated with happier/calmer mood. Fewer associations occurred with evening outcomes. For wives, better subjective sleep quality was related to more positive and negative spousal events, perhaps because wives had more energy to engage in spousal interactions of all kinds. For husbands, non-sleep physical affection was related to more positive spousal events and enjoyment.
Thus, in this sample of relatively healthy, satisfied couples, sleep-touch, rather than sleep quality or waking physical affection, showed the most consistent associations with relationship-related affective experiences/events. All effects were at the daily (within-subjects) level, revealing that benefits of sleep-touch were incurred when spouses had more sleep-touch relative to their own typical amount.
Potential Sleep-Touch Mechanisms
The fact that sleep-touch is linked with better morning mood after accounting for mood at bedtime, sleep quality, and non-sleep physical affection underscores the importance of this phenomenon. The findings suggest sleep-touch may be a key means through which healthy adults benefit from co-sleeping, and that individual mood regulation provided by sleep may be even more powerful in a context of co-regulation. While transitioning to sleep, partner presence may enhance feelings of safety and security (Troxel et al., 2007). Touch may facilitate falling and staying asleep by conveying intimacy/relationship reassurance (Rosenblatt, 2006) or embodying the presence of available social resources (Beckes et al., 2015), or even directly via arousal reduction (Ditzen et al., 2019; Holt-Lunstad et al., 2008). Like non-sleep-related touch, sleep-touch may alter physiological processes such as greater heart rate variability (Triscoli et al., 2017) that augment affect regulatory or resetting functions of sleep—which in itself is associated with such physiological changes (e.g., Stein & Pu, 2012).
In healthy sleepers, descent into sleep involves reductions in cortical and autonomic arousal (lower-frequency EEG [Saper et al., 2010], lower heart rate and blood pressure [Van Cauter et al., 2008], HPA de-activation [Nicolaides et al., 2000]). Transition to sleep may create a more vulnerable or susceptible state than during waking, whereby fewer competing intero- or exteroceptive stimuli could allow for better attention to and integration of touch experience. In other words, the peri-sleep-period may provide an opportunity to attend to or savor touch experiences, or simply to process (implicitly) touch inputs more fully, integrating touch into how one “feels” (e.g., via insular inputs; Burleson & Quigley, 2021; Craig, 2009; Davidovic et al., 2019). Finally, touch experiences just prior to sleep onset are temporally proximate to the onset of sleep-facilitated consolidation of emotion, memory, and emotional memory (Payne et al., 2008). Thus, sleep-touch-related pleasant sensations and/or emotional meaning should be encoded especially strongly during sleep, potentially leading to affective carryover of happy/calm mood the next day, and perhaps overshadowing negative emotional experiences and resultant angry/irritable mood.
Limitations and Implications
This study was solely self-report. Morning diary items (e.g., sleep quality, sleep-touch) were assessed at the same time, preventing causal inferences. Sleep-touch, our key independent variable, was a single-item measure, and our initial attempt to evaluate sleep-touch was deliberately non-specific. We did not measure how much partners touched before, during, and/or after sleep, nor capture the trajectory and influence of touch at different points during the night or whether one versus both partners were awake. We did not examine different kinds of touch (e.g., prolonged close-body contact vs. brief shoulder massage), nor the potential influence from other sleep-touch sources (children, pets). Reports of all study variables were only modestly correlated between partners, suggesting the importance in future studies of examining how partners attend to, define/label, experience, recall, and report touch.
Our sample comprised relatively satisfied, mostly White, married heterosexual couples conscientious and unburdened enough to complete daily diaries. Touch attitudes and behaviors vary among groups (Burleson et al., 2019), highlighting the need to examine sleep-touch in diverse couples. Evidence suggests touch (Debrot et al., 2020) and sleep concordance (Elsey et al., 2019) are beneficial for well-being and sleep quality, respectively, even among those with relationship concerns (i.e., attachment anxiety/avoidance). In our sample of healthy, satisfied couples, we found sleep-touch effects despite relatively low levels of sleep-touch on average. Nevertheless, sleep-touch may operate differently for couples with more substantial mood-, relationship-, and/or sleep-related distress. Examining sleep-touch effects over time, alongside contextual and relationship factors, will be important.
Previously we found that individual differences in use of touch for affect regulation (TAR) moderated links between touch and psychological distress (Burleson et al., 2021). Benefits of sleep-touch similarly may be more potent among higher-TAR individuals. Alternatively, transitions between waking and sleep are unique states where physical touch may have implicit calming and regulatory effects regardless; our findings of associations with sleep-touch above and beyond non-sleep physical affection support this possibility.
In sum, we suggest that environmental and physiological contexts surrounding sleep-touch may allow it to augment the restorative and regulatory effects of sleep and of touch on affective states. We found that on a day-to-day basis, more sleep-touch was associated (either directly or indirectly via mood) with more positive spouse-related events and enjoyment, and with less spouse-related negative events and stress, all of which could strengthen relationships. Further study will be needed to ascertain the extent of this phenomenon and its implications for relationships and well-being.
Additional Information
Funding
This research was supported by grants R21HL088612-01A1 and R21HL088612-01A1S1 awarded to Mary H. Burleson by the National Heart, Lung, and Blood Institute.
Data Availability
All materials, syntax and data are available here: https://osf.io/c4sw5/.
Ethical Approval
Not applicable.
Conflict of interest
The authors declare no competing interests.
Informed Consent
Not applicable.
Footnotes
Nicole A. Roberts and Mary H. Burleson shared first authorship.
Handling Editor: Aric Prather
References
- Asparouhov T, Hamaker EL, Muthén B. Dynamic structural equation models. Structural Equation Modeling: A Multidisciplinary Journal. 2018;25:359–388. doi: 10.1080/10705511.2017.1406803. [DOI] [Google Scholar]
- Asparouhov, T., & Muthen, B. (2010). Bayes analysis using Mplus: Technical implementation. Technical report, Version 3 https://www.statmodel.com/papers.shtml
- Asparouhov T, Muthén B. Latent variable centering of predictors and mediators in multilevel and time-series models. Structural Equation Modeling: A Multidisciplinary Journal. 2019;26(1):119–142. doi: 10.1080/10705511.2018.1511375. [DOI] [Google Scholar]
- Barber L, Grawitch MJ, Munz DC. Are better sleepers more engaged workers? A self-regulatory approach to sleep hygiene and work engagement. Stress and Health. 2013;29(4):307–316. doi: 10.1002/smi.2468. [DOI] [PubMed] [Google Scholar]
- Beckes L, IJzerman H, Tops M. Toward a radically embodied neuroscience of attachment and relationships. Frontiers in Human Neuroscience. 2015;9:266. doi: 10.3389/fnhum.2015.00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Simon E, Vallat R, Barnes CM, Walker MP. Sleep loss and the socio-emotional brain. Trends in Cognitive Science. 2020;24(6):435–450. doi: 10.1016/j.tics.2020.02.003. [DOI] [PubMed] [Google Scholar]
- Benca, R. M., Obermeyer, W. H., Thisted, R. A., & Gillin, J. C. (1992). Sleep and psychiatric disorders. A meta-analysis. Archives of General Psychiatry, 49(8), 651–668; discussion 669–670. 10.1001/archpsyc.1992.01820080059010 [DOI] [PubMed]
- Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Archiv European Journal of Physiology. 2012;463(1):121–137. doi: 10.1007/s00424-011-1044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biesanz JC, Falk CF, Savalei V. Assessing mediational models: Testing and interval estimation for indirect effects. Multivariate Behavioral Research. 2010;45:661–701. doi: 10.1080/00273171.2010.498292. [DOI] [PubMed] [Google Scholar]
- Bouwmans MEJ, Bos EH, Hoenders HJR, Oldehinkel AJ, de Jonge P. Sleep quality predicts positive and negative affect but not vice versa. An electronic diary study in depressed and healthy individuals. Journal of Affective Disorders. 2017;207:260–267. doi: 10.1016/j.jad.2016.09.046. [DOI] [PubMed] [Google Scholar]
- Burleson MH, Quigley KS. Social interoception and social allostasis through touch: Legacy of the Somatovisceral Afference Model of Emotion. Social Neuroscience. 2021;16(1):92–102. doi: 10.1080/17470919.2019.1702095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burleson MH, Roberts NA, Coon DW, Soto JA. Perceived cultural acceptability and comfort with affectionate touch: Differences between Mexican Americans and European Americans. Journal of Social and Personal Relationships. 2019;36(3):1000–1022. doi: 10.1177/0265407517750005. [DOI] [Google Scholar]
- Burleson, M. H., Roberts, N. A., Munson, A. A., Duncan, C. J., Randall, A. K., Ha, T., Sioni, S., & Mickelson, K. D. (2021). Feeling the absence of touch: Distancing, distress, regulation, and relationships in the context of COVID-19. Journal of Social and Personal Relationships. 10.1177/02654075211052696
- Busby DM, Crane DR, Larson JH, Christensen C. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: Construct hierarchy and multidimensional scales. Journal of Marital and Family Therapy. 1995;21(3):289–308. doi: 10.1111/j.1752-0606.1995.tb00163.x. [DOI] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cartwright R, Luten A, Young M, Mercer P, Bears M. Role of REM sleep and dream affect in overnight mood regulation: A study of normal volunteers. Psychiatry Research. 1998;81(1):1–8. doi: 10.1016/s0165-1781(98)00089-4. [DOI] [PubMed] [Google Scholar]
- Cascio CJ, Moore D, McGlone F. Social touch and human development. Developmental Cognitive Neuroscience. 2019;35:5–11. doi: 10.1016/j.dcn.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuah YM, Venkatraman V, Dinges DF, Chee MW. The neural basis of interindividual variability in inhibitory efficiency after sleep deprivation. Journal of Neuroscience. 2006;26(27):7156–7162. doi: 10.1523/jneurosci.0906-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coan JA, Schaefer HS, Davidson RJ. Lending a hand: Social regulation of the neural response to threat. Psychological Science. 2006;17(12):1032–1039. doi: 10.1111/j.1467-9280.2006.01832.x. [DOI] [PubMed] [Google Scholar]
- Craig AD. How do you feel–now? The anterior insula and human awareness. Nature Reviews Neuroscience. 2009;10(1):59–70. doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- Dainton M, Stafford L, Canary DJ. Maintenance strategies and physical affection as predictors of love, liking, and satisfaction in marriage. Communication Reports. 1994;7(2):88–98. doi: 10.1080/08934219409367591. [DOI] [Google Scholar]
- Davidovic M, Starck G, Olausson H. Processing of affective and emotionally neutral tactile stimuli in the insular cortex. Developmental Cognitive Neuroscience. 2019;35:94–103. doi: 10.1016/j.dcn.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debrot A, Meuwly N, Muise A, Impett EA, Schoebi D. More than just sex: Affection mediates the association between sexual activity and well-being. Personality and Social Psychology Bulletin. 2017;43(3):287–299. doi: 10.1177/0146167216684124. [DOI] [PubMed] [Google Scholar]
- Debrot, A., Stellar, J. E., MacDonald, G., Keltner, D., & Impett, E. A. (2020). Is touch in romantic relationships universally beneficial for psychological well-being? The role of attachment avoidance. Personality and Social Psychology Bulletin, online before print. 10.1177/0146167220977709 [DOI] [PubMed]
- Ditzen B, Neumann ID, Bodenmann G, von Dawans B, Turner RA, Ehlert U, Heinrichs M. Effects of different kinds of couple interaction on cortisol and heart rate responses to stress in women. Psychoneuroendocrinology. 2007;32(5):565–574. doi: 10.1016/j.psyneuen.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Ditzen B, Germann J, Meuwly N, Bradbury TN, Bodenmann G, Heinrichs M. Intimacy as related to cortisol reactivity and recovery in couples undergoing psychosocial stress. Psychosomatic Medicine. 2019;81:16–25. doi: 10.1097/PSY.0000000000000633. [DOI] [PubMed] [Google Scholar]
- Drews HJ, Wallot S, Weinhold SL, Mitkidis P, Baier PC, Roepstorff A, Göder R. "Are we in sync with each other?" Exploring the effects of cosleeping on heterosexual couples' sleep using simultaneous polysomnography: A pilot study. Sleep Disorders. 2017;2017:8140672. doi: 10.1155/2017/8140672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drews HJ, Wallot S, Brysch P, Berger-Johannsen H, Weinhold SL, Mitkidis P, Baier PC, Lechinger J, Roepstorff A, Goder R. Bed-sharing in couples is associated with increased and stabilized rem sleep and sleep-stage synchronization. Frontiers in Psychiatry. 2020;11:583. doi: 10.3389/fpsyt.2020.00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsey T, Keller PS, El-Sheikh M. The role of couple sleep concordance in sleep quality: Attachment as a moderator of associations. Journal of Sleep Research. 2019;28(5):e12825. doi: 10.1111/jsr.12825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatima Y, Doi SAR, Najman JM, Mamun AA. Exploring gender difference in sleep quality of young adults: Findings from a large population study. Clinical Medicine & Research. 2016;14:138–144. doi: 10.3121/cmr.2016.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Statistical Science. 1992;7:457–472. doi: 10.1214/ss/1177011136. [DOI] [Google Scholar]
- Goldstein-Piekarski AN, Greer SM, Saletin JM, Walker MP. Sleep deprivation impairs the human central and peripheral nervous system discrimination of social threat. Journal of Neuroscience. 2015;35(28):10135–10145. doi: 10.1523/jneurosci.5254-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon AM, Mendes WB, Prather AA. The social side of sleep: Elucidating the links between sleep and social processes. Current Directions in Psychological Science. 2017;26(5):470–475. doi: 10.1177/0963721417712269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon AM, Carrillo B, Barnes CM. Sleep and social relationships in healthy populations: A systematic review. Sleep Medicine Review. 2021;57:101428. doi: 10.1016/j.smrv.2021.101428. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Levenson RW. Marital processes predictive of later dissolution: Behavior, physiology, and health. Journal of Personality and Social Psychology. 1992;63(2):221–233. doi: 10.1037//0022-3514.63.2.221. [DOI] [PubMed] [Google Scholar]
- Gunn, H. E., Buysse, D. J., Matthews, K. A., Kline, C. E., Cribbet, M. R., & Troxel, W. M. (2017). Sleep-wake concordance in couples is inversely associated with cardiovascular disease risk markers. Sleep, 40(1). 10.1093/sleep/zsw028 [DOI] [PMC free article] [PubMed]
- Hasler BP, Troxel WM. Couples' nighttime sleep efficiency and concordance: Evidence for bidirectional associations with daytime relationship functioning. Psychosomatic Medicine. 2010;72(8):794–801. doi: 10.1097/PSY.0b013e3181ecd08a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Birmingham WA, Light KC. Influence of a "warm touch" support enhancement intervention among married couples on ambulatory blood pressure, oxytocin, alpha amylase, and cortisol. Psychosomatic Medicine. 2008;70(9):976–985. doi: 10.1097/PSY.0b013e318187aef7. [DOI] [PubMed] [Google Scholar]
- Izci B, McDonald JP, Coleman EL, Mackay TW, Douglas NJ, Engleman HM. Clinical audit of subjects with snoring & sleep apnoea/hypopnoea syndrome fitted with mandibular repositioning splint. Respiratory Medicine. 2005;99(3):337–346. doi: 10.1016/j.rmed.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Jakubiak, B. K., Fuentes, J. D., & Feeney, B. C. (2021). Individual and relational differences in desire for touch in romantic relationships. Journal of Social and Personal Relationships (online before print).10.1177/02654075211003331
- Jakubiak BK, Feeney BC. Affectionate touch to promote relational, psychological, and physical well-being in adulthood: A theoretical model and review of the research. Personality and Social Psychology Review. 2017;21(3):228–252. doi: 10.1177/1088868316650307. [DOI] [PubMed] [Google Scholar]
- Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, Walker MP. The sleep-deprived human brain. Nature Reviews Neuroscience. 2017;18(7):404–418. doi: 10.1038/nrn.2017.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krizan Z, Hisler G. Sleepy anger: Restricted sleep amplifies angry feelings. Journal of Experimental Psychology: General. 2019;148(7):1239–1250. doi: 10.1037/xge0000522. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Krystal AD. Sleep therapeutics and neuropsychiatric illness. Neuropsychopharmacology. 2020;45(1):166–175. doi: 10.1038/s41386-019-0474-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Chopik WJ, Schiamberg LB. Longitudinal associations between marital quality and sleep quality in older adulthood. Journal of Behavioral Medicine. 2017;40(5):821–831. doi: 10.1007/s10865-017-9850-2. [DOI] [PubMed] [Google Scholar]
- Maranges HM, McNulty JK. The rested relationship: Sleep benefits marital evaluations. Journal of Family Psychology. 2017;31(1):117–122. doi: 10.1037/fam0000225. [DOI] [PubMed] [Google Scholar]
- Mauss IB, Troy AS, LeBourgeois MK. Poorer sleep quality is associated with lower emotion-regulation ability in a laboratory paradigm. Cognition and Emotion. 2013;27(3):567–576. doi: 10.1080/02699931.2012.727783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadyen TA, Espie CA, McArdle N, Douglas NJ, Engleman HM. Controlled, prospective trial of psychosocial function before and after continuous positive airway pressure therapy. European Respiratory Journal. 2001;18(6):996–1002. doi: 10.1183/09031936.01.00209301. [DOI] [PubMed] [Google Scholar]
- Minkel JD, Banks S, Htaik O, Moreta MC, Jones CW, McGlinchey EE, Simpson NS, Dinges DF. Sleep deprivation and stressors: Evidence for elevated negative affect in response to mild stressors when sleep deprived. Emotion. 2012;12(5):1015–1020. doi: 10.1037/a0026871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy MLM, Janicki-Deverts D, Cohen S. Receiving a hug is associated with the attenuation of negative mood that occurs on days with interpersonal conflict. PLoS ONE. 2018;13(10):e0203522. doi: 10.1371/journal.pone.0203522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (1998 –2019). Mplus User’s Guide (8th ed.). Los Angeles, CA: Muthén & Muthén.
- Nicolaides, N. C., Vgontzas, A. N., Kritikou, I., & Chrousos, G. (2000). HPA Axis and Sleep. In K. R. Feingold, B. Anawalt, A. Boyce, G. Chrousos, W. W. de Herder, K. Dungan, A. Grossman, J. M. Hershman, J. Hofland, G. Kaltsas, C. Koch, P. Kopp, M. Korbonits, R. McLachlan, J. E. Morley, M. New, J. Purnell, F. Singer, C. A. Stratakis, D. L. Trence, & D. P. Wilson (Eds.), Endotext. MDText.com, Inc.
- Payne JD, Stickgold R, Swanberg K, Kensinger EA. Sleep preferentially enhances memory for emotional components of scenes. Psychological Science. 2008;19(8):781–788. doi: 10.1111/j.1467-9280.2008.02157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015;38(9):1353–1359. doi: 10.5665/sleep.4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurements. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Richter K, Adam S, Geiss L, Peter L, Niklewski G. Two in a bed: The influence of couple sleeping and chronotypes on relationship and sleep An Overview. Chronobiology International. 2016;33(10):1464–1472. doi: 10.1080/07420528.2016.1220388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt, P. C. (2006). Two in a bed : The social system of couple bed sharing. State University of New York Press. http://www.loc.gov/catdir/toc/ecip0519/2005026824.html
- Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. doi: 10.1093/biomet/63.3.581. [DOI] [Google Scholar]
- Saper CB, Fuller PM, Pedersen NP, Lu J, Scammell TE. Sleep state switching. Neuron. 2010;68(6):1023–1042. doi: 10.1016/j.neuron.2010.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegelhalder K, Regen W, Siemon F, Kyle SD, Baglioni C, Feige B, Nissen C, Riemann D. Your place or mine? Does the sleep location matter in young couples? Behavioral Sleep Medicine. 2017;15(2):87–96. doi: 10.1080/15402002.2015.1083024. [DOI] [PubMed] [Google Scholar]
- Stein PK, Pu Y. Heart rate variability, sleep, and sleep disorders. Sleep Medicine Review. 2012;16(1):47–66. doi: 10.1016/j.smrv.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Stickgold R. Sleep-dependent memory consolidation. Nature. 2005;437(7063):1272–1278. doi: 10.1038/nature04286. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Shema SJ, Roberts RE. Impact of spouses' sleep problems on partners. Sleep. 2004;27(3):527–531. doi: 10.1093/sleep/27.3.527. [DOI] [PubMed] [Google Scholar]
- Triscoli C, Croy I, Steudte-Schmiedgen S, Olausson H, Sailer U. Heart rate variability is enhanced by long-lasting pleasant touch at CT-optimized velocity. Biological Psychology. 2017;128:71–81. doi: 10.1016/j.biopsycho.2017.07.007. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Review. 2007;11(5):389–404. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Buysse DJ, Matthews KA, Kravitz HM, Bromberger JT, Sowers M, Hall MH. Marital/cohabitation status and history in relation to sleep in midlife women. Sleep. 2010;33(7):973–981. doi: 10.1093/sleep/33.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Medicine. 2008;9(Suppl 1):S23–28. doi: 10.1016/s1389-9457(08)70013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Helm E, Walker MP. Sleep and emotional memory processing. Sleep Medicine Clinics. 2011;6(1):31–34. doi: 10.1016/j.jsmc.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner SA, Mattson RE, Davila J, Johnson MD, Cameron NM. Touch me just enough: The intersection of adult attachment, intimate touch, and marital satisfaction. Journal of Social and Personal Relationships. 2020;37(6):1945–1967. doi: 10.1177/0265407520910791. [DOI] [Google Scholar]
- Waldinger RJ, Hauser ST, Schulz MS, Allen JP, Crowell JA. Reading others emotions: The role of intuitive judgments in predicting marital satisfaction, quality, and stability. Journal of Family Psychology. 2004;18(1):58–71. doi: 10.1037/0893-3200.18.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker MP, van der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychological Bulletin. 2009;135(5):731–748. doi: 10.1037/a0016570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Preacher KJ. Moderated mediation analysis using Bayesian methods. Structural Equation Modeling: A Multidisciplinary Journal. 2015;22:249–263. doi: 10.1080/10705511.2014.935256. [DOI] [Google Scholar]
- Wassing R, Schalkwijk F, Lakbila-Kamal O, Ramautar JR, Stoffers D, Mutsaerts H, Talamini LM, Van Someren EJW. Haunted by the past: Old emotions remain salient in insomnia disorder. Brain. 2019;142(6):1783–1796. doi: 10.1093/brain/awz089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters SF, West TV, Mendes WB. Stress contagion: Physiological covariation between mothers and infants. Psychological Science. 2014;25(4):934–942. doi: 10.1177/0956797613518352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep–A prefrontal-amygdala disconnect. Current Biology. 2007;17(20):R877–878. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All materials, syntax and data are available here: https://osf.io/c4sw5/.