Abstract
The primary objective of this study was to examine whether psychological distress mediates the relationship between income and increases in body mass index in adolescent girls. To answer this question, we analyzed data from 2379 participants in the longitudinal NHLBI Growth and Health Study using regularized regression and path analysis. The exposure was household income at age 9–10 and the outcome was body mass index at age 18–19. Income negatively predicted psychological distress, which in turn predicted psychological and behavioral factors that were associated with increases in body mass index. Overall, psychological distress and related variables accounted for around 20% of the relationship between income and increases in body mass index in adolescent girls. The impacts of income on a complex constellation of psychological risks for obesity support the evaluation of income support policies for reducing economic inequalities in obesity. Obesity reduction programs focused on changing psychological distress should be developed with consideration of the household economic environment.
Electronic supplementary material
The online version of this article (10.1007/s42761-020-00010-0) contains supplementary material, which is available to authorized users.
Keywords: Obesity, Weight, Health inequalities, Socioeconomic status, Emotion, Affect
Income disparities in obesity are well documented (Drewnowski & Specter, 2004). These disparities emerge during adolescence (Frederick, Snellman, & Putnam, 2014) and tend to be larger among women than men (Ogden et al., 2017). The factors that lead to the emergence of these gender-based income inequalities in obesity during adolescence are not well understood, in part due to the fact that a complex constellation of factors is likely to have an impact (Rehkopf, Laraia, Segal, Braithwaite, & Epel, 2011), and that studies that measure a wide range of these factors over time are rare. Understanding the factors linking household income and increases in body mass index (BMI) among adolescent girls is a critical first step to developing policies and interventions to decrease income-related disparities in obesity among women.
One potential factor is psychological distress. Low-income individuals tend to experience higher levels of psychological distress than high-income individuals (Cohen, Doyle, & Baum, 2006; Gallo & Matthews, 2003). This is true for both stress (Cohen & Janicki-Deverts, 2012; Cohen et al., 2006) and anxiety (Sareen, Afifi, McMillan, & Asmundson, 2011). Several mechanisms are thought to account for these effects. Three prominent candidates are material deprivation (Whelan & Maître, 2013), the sense of occupying a low rung on the social ladder (Singh-Manoux, Adler, & Marmot, 2003), and stigma associated with having low income (Reutter et al., 2009).
Higher levels of psychological distress are associated both with increased levels of unhealthy eating and with higher BMI (Dallman, 2010; Torres & Nowson, 2007). Although much of the research on this topic has focused on the relationships among stress, unhealthy eating, and increases in BMI (Torres & Nowson, 2007), longitudinal studies have indicated that anxiety may also lead to increases in BMI (Brumpton, Langhammer, Romundstad, Chen, & Mai, 2013). There are several mechanisms by which anxiety, stress, and other forms of psychological distress are thought to have these effects. First, psychological distress has been shown to impair executive function and self-control (Arnsten, 2009; Maier, Makwana, & Hare, 2015) which are often required for engaging in healthy behaviors, such as healthy eating (Hare, Camerer, & Rangel, 2009). Second, studies have shown that people engage in unhealthy eating behavior to make themselves feel better when they feel bad (Arnow, Kenardy, & Agras, 1995). Elevated stress in particular has also been shown to lead to increases in levels of glucocorticoids and insulin which, in turn, lead to increased food consumption and increases in BMI (Dallman, 2010).
Drawing on these two bodies of literature—one showing increased psychological distress among low-income individuals and one showing that psychological distress leads to unhealthy eating and increases in BMI—prior studies have examined whether psychological distress mediates the relationship between income and increases in BMI, but with inconsistent results. First, while some of this work indicates that psychological distress does mediate this relationship, some findings rely on the use of cross-sectional data (Spinosa, Christiansen, Dickson, Lorenzetti, & Hardman, 2019) which makes it difficult to draw causal inferences, especially given prior work showing that obesity can lead to increased psychological distress (Puhl & Heuer, 2009). Furthermore, existing studies using longitudinal data have not yielded consistent findings (see Claassen, Klein, Bratanova, Claes, & Corneille, 2019 for a recent review) or have used indicators of socioeconomic status (SES) other than income, such as education (Ball, Schoenaker, & Mishra, 2017). Finally, few studies have examined these relationships in children and adolescents, arguably the most important populations in which to examine these links given the rising prevalence of childhood obesity (CDC, 2019). The current state of the literature suggests that additional research should be done to examine the possibility that psychological distress mediates the relationship between income and increases in BMI.
In the present research, we analyzed longitudinal data from the National Heart Lung and Blood Institute (NHLBI) Growth and Health Study (NGHS) to examine whether household income was associated with psychological distress in adolescent girls, and, if so, whether psychological distress was associated with increases in BMI over a 10-year period. To conduct these analyses, we employed a combination of techniques from machine learning—variable selection, cross-validation, and validation—and path analysis methods to build models of the relationships among income, psychological distress, and increases in BMI. In addition, we drew upon the rich set of psychosocial variables available in the NGHS dataset and assessed whether any of these measures contributed to this relationship but made no a priori predictions about which variables might play a role. Although prior work has examined these relationships in the context of race (Tomiyama, Puterman, Epel, Rehkopf, & Laraia, 2013), no prior studies using this dataset have examined these relationships in the context of income.
Method
Participants
For the current paper, we used data from the National Heart Lung and Blood Institute (NHLBI) Growth and Health Study (NGHS). The NGHS was a cohort study launched in 1987 in which a sample of 2379 of girls (1213 Black and 1166 White) between the ages of 9 and 10 were recruited and followed for 10 years. Researchers recruited participants from three sites: Richmond, California, Cincinnati, Ohio, and the Washington D.C. area. The Institutional Review Board at Stanford University approved the present analysis. The public release dataset used in this analysis was acquired from NHLBI. This dataset is available from the NHLBI.
Materials
Prior to using automated variable selection methods (described below), variables were grouped into conceptual categories which were then used in the variable selection process outlined in the statistical analyses section below. Our primary outcome measure was year 10 BMI and our primary exposure was year 1 household income (see SOM for sensitivity analyses including other outcomes related to weight and body size).
Psychological distress was measured using two scales: the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) and the Children’s Manifest Anxiety Scale (CMAS; Reynolds & Richmond, 1978). We identified these two scales as the ones that most cleanly measured our construct of interest out of all scales in the dataset. The PSS measures the extent to which a person experiences events in his or her life as stressful (Cohen et al., 1983) and was collected in years 2, 4, 6, 8, and 10 of the study. The CMAS (an adaptation of Taylor’s Manifest Anxiety Scale; Taylor, 1953) was designed to assess the magnitude of anxiety that a child experiences and was collected in years 3 and 5. We used the years 2 and 4 of the PSS and years 3 and 5 of the CMAS in our variable selection step so that variables selected in later steps (see below) could follow these variables in time.
The eating-related psychological variables category included all subscales (interoceptive awareness, bulimia, ineffectiveness, maturity fears, perfectionism, and interpersonal distrust) of the Eating Disorders Inventory (EDI) except for the body dissatisfaction and drive for thinness subscales (Garner, Olmstead, & Polivy, 1983). We elected not to use these subscales in our analysis as they seemed more likely to be symptomatic of increases in BMI than the other EDI subscales. The EDI was designed to assess a host of psychological and behavioral patterns related to unhealthy eating (Garner et al., 1983). Although not all of the remaining subscales are directly related to eating, we categorized these variables together under the eating-related psychological variables heading as they all came from a validated scale that was designed to assess disordered eating (Garner et al., 1983). This category also included the Emotional Eating Index (EEI) which is a measure developed specifically for the NGHS. The EDI was collected in years 3, 5, 7, and 9. We used year 5 of the EDI in our variable selection step as this was the only year following year 3 CMAS for which we had data on all subscales. The EEI was collected in years 1–7 and 9. We used years 4–7 and 9 of the EEI in our variable selection step.
The other psychological variables category included variables from the Perceived Competence Scale for Children (PCSC; Harter, 1982) and the Coping Strategies Inventory (CSI; Tobin, Holroyd, Reynolds, & Wigal, 1989). The PCSC assesses a child’s competence across a variety of important life domains (Harter, 1982). The CSI assesses a variety of adaptive and maladaptive strategies that an individual can use to regulate psychological distress (Tobin et al., 1989). In keeping with prior work by the last author, for the PCSC, we analyzed data from the social acceptance, behavioral conduct, and global self-worth subscales (Rehkopf et al., 2011). We opted not to analyze data from the athletic competence and physical appearance subscales as we reasoned that responses to these questions were more likely to be symptomatic of increases in BMI than the other subscales. Also in keeping with prior work by the last author, for the CSI, we analyzed data from the cognitive restructuring, expressed emotions, and self-criticism subscales (Rehkopf et al., 2011). The PCSC was collected in years 1, 3, 5, 7, and 9, although only certain subscales were used in years 7 and 9. We used year 5 of the PCSC in our variable selection step as this was the only year following the year 3 CMAS for which we had data on all subscales. The CSI was collected in years 2, 4, 6, 8, and 10. We used years 4, 6, and 8 of the CSI as these were the only years between year 3 CMAS and year 10 BMI.
The eating behavior variables (collected in years 1, 2, 3, 4, 5, 7, 8, and 10) included any eating behavior variable that could reasonably be assumed to have been influenced by the affective state of the participant. We used years 4–9 of these variables as these were the years between year 3 CMAS and year 10 BMI. Please see SOM for a full list of these variables.
Our control variables included participant BMI at year 1, parent BMI at year 1, and race.
Statistical Analyses
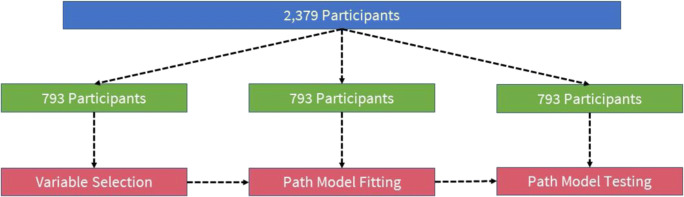
Before conducting statistical analyses, we imputed missing data for any variable which had fewer than 30% of observations missing using the R package “missForest” (see SOM for additional detail; sStekhoven & Buhlmann, 2012). For our statistical analyses, we used a validation-set approach and began by partitioning the data into three equal parts (each n = 793) using random sampling (see Fig. 1). Part 1 data was used for variable selection, part 2 data was used for path analysis model building and pruning, and part 3 data was used for path analysis model testing. This procedure was implemented to avoid overfitting and inflation of type I error.
Fig. 1.
Data partitioning procedure
Variable Selection
In the variable selection step, using part 1 data, we first split the variables into the four conceptual categories outlined above: (1) psychological distress, (2) eating-related psychological variables, (3) other psychological variables, and (4) eating behavior variables. Because our dataset only included two measures of psychological distress, we began by using variable selection methods to determine (a) whether each of these two measures were predicted by household income at the start of the study, (b) whether each measure predicted year 10 BMI at the end of the study, and (c) the time point at which these relationships were strongest. Household income predicted both year 2 stress and year 3 anxiety and each of these measures predicted BMI. We created separate models for each type of psychological distress to examine whether one provided more explanatory power than the other.
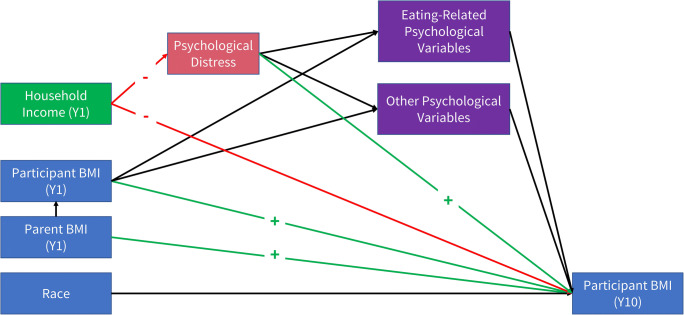
After identifying that both stress and anxiety predicted our outcome of interest, we constructed two sets of hypothesized path models focused on psychological variables (see Fig. 2) and behavioral variables. The decision to separate these two sets of variables was made to avoid oversaturating the regressions in the models with a high number of potentially collinear variables. We then used the R package “glmnet” to fit a series of regularized regression models (least absolute shrinkage and selection operator or LASSO and Elastic-Net) and select important variables for our path models (Friedman, Hastie, & Tibshirani, 2010). LASSO and Elastic-Net fitting procedures each have different strengths and weaknesses that might lead one or the other method to provide a better fit for a given set of variables (Tibshirani, 1996; Zou & Hastie, 2005). One benefit of using these methods for variable selection is that they do not select variables based on p values and so these analyses do not call for a multiple comparisons correction to adjust the cutoff for statistical significance (Tibshirani, 1996; Zou & Hastie, 2005). Tuning parameters for each model were selected using 5-fold repeated (10 repeats) cross-validation implemented with the R package “caret” (Kuhn, 2008). More specifically, for each regression in our hypothesized path models, we fit both the LASSO and Elastic-Net models to select among all of the variables in a particular conceptual category that might predict a particular outcome within the model. We then selected whichever model (LASSO or Elastic-Net) provided better fit to the data for the set of paths pertaining to a specific conceptual category. Next, we checked for overlapping variables with the other regressions for a set of paths in each model. For example, if we found that year 2 stress predicted one set of eating-related psychological variables and another set of eating-related psychological variables predicted year 10 BMI, we then selected variables that were identified as important in both of those sets of regressions. In this specific example, this procedure ensured that we avoided selecting any eating-related psychological variables that were not predicted by year 2 stress or any eating-related psychological variables that did not predict year 10 BMI.
Fig. 2.
Hypothesized path model. Note that this hypothesized model includes both eating-related psychology variables and other psychological variables which were examined in separate actual models
Many of the variables in the NGHS dataset were measured at multiple time points. We made no a priori predictions regarding why a given variable measured at a particular year would have a greater effect than that same variable measured during an alternate year. Thus, in many cases, we selected among multiple measures of the same variable during the variable selection step, allowing the model to select the time points with measurements that were most predictive of a given outcome. However, we preserved the temporal structure of the data in that we only put variables into the regression paths where the arrows in our path model would go forward in time.
Path Analysis Model Building and Pruning
Using the results from our variable selection step with part 1 data, we next used part 2 data to create four initial path analysis models (stress and psychological variables, anxiety and psychological variables, stress and eating behavior variables, anxiety and eating behavior variables). For each initial model, we noted the regressions that had small or non-significant parameter values and created four pruned path analysis models with the non-significant paths removed.
Path Analysis Model Testing
Finally, using part 3 data (our test set), we fit each pruned model and examined model fit statistics as well as parameter values for these final models. In addition, we fit each pruned model to the entire dataset to assess examined model fit for our entire sample. There are several rules of thumb for sample size in fitting path models. Many of these specify a ratio of participants to parameters (n:q). One very common rule of thumb is 10:1 (Nunally, 1967). In our model with the greatest number of parameters (q = 49), we have a ratio of greater than 16 to 1.
Results
Pairwise correlations and descriptive statistics for all variables included in the various path analyses are listed in the supplement. For results of the variable selection process and specification of initial path analysis models, please see the supplement. Model fit and parameter values are reported for part 3 data unless otherwise noted.
Model fit indices indicated excellent fit for the model which included stress and eating-related psychological variables (see Table 1) both for our test set (χ2(5, N = 793) = 5.68, p = 0.339, TLI = 0.99, CFI = 1.00, RMSEA = 0.01, SRMR = 0.01) and for the entire dataset (χ2(5, N = 2379) = 3.30, p = 0.654, TLI = 1.00, CFI = 1.00, RMSEA = 0.00, SRMR = 0.01). Model fit indices also indicated excellent fit for the model which included anxiety and eating-related psychological variables (see Table 2) both for our test set (χ2(6, N = 793) = 9.45, p = 0.150, TLI = 0.99, CFI = 0.99, RMSEA = 0.03, SRMR = 0.02) and for the entire dataset (χ2(6, N = 2379) = 7.92, p = 0.244, TLI = 1.00, CFI = 1.00, RMSEA = 0.01, SRMR = 0.01). These two models were identical in their specification except for (1) the presence of stress in the former and anxiety in the latter and (2) race did not predict anxiety.
Table 1.
Parameter values for path model with stress and psychological variables
| Predictor | b | 95% CI | SE | z | p |
|---|---|---|---|---|---|
| Predictors of year 10 BMI | |||||
| Year 1 income | − 0.05 | [− 0.1, − 0.01] | 0.02 | − 2.37 | 0.018 |
| Year 5 interoceptive awareness | 0.03 | [− 0.02, 0.08] | 0.03 | 1.27 | 0.204 |
| Year 5 interpersonal distrust | 0.07 | [0.02, 0.12] | 0.02 | 2.92 | 0.004 |
| Year 5 ineffectiveness | − 0.03 | [− 0.09, 0.03] | 0.03 | − 0.9 | 0.368 |
| Year 5 self-worth | − 0.04 | [− 0.09, 0.01] | 0.03 | − 1.65 | 0.099 |
| Year 1 BMI | 0.76 | [0.72, 0.79] | 0.02 | 47.51 | < 0.001 |
| Year 1 parent BMI | 0.1 | [0.05, 0.14] | 0.02 | 4.37 | < 0.001 |
| Race | 0.02 | [− 0.03, 0.06] | 0.02 | 0.72 | 0.47 |
| Predictors of year 5 interoceptive awareness | |||||
| Year 2 perceived stress | 0.16 | [0.09, 0.23] | 0.03 | 4.71 | < 0.001 |
| Year 1 income | − 0.13 | [− 0.2, − 0.06] | 0.04 | − 3.6 | < 0.001 |
| Year 1 BMI | 0.11 | [0.04, 0.18] | 0.04 | 3.1 | 0.002 |
| Year 1 parent BMI | 0.02 | [− 0.05, 0.1] | 0.04 | 0.64 | 0.519 |
| Race | 0.1 | [0.03, 0.17] | 0.04 | 2.69 | 0.007 |
| Predictors of year 5 interpersonal distrust | |||||
| Year 2 perceived stress | 0.12 | [0.06, 0.19] | 0.03 | 3.62 | < 0.001 |
| Year 1 income | − 0.1 | [− 0.17, − 0.03] | 0.04 | − 2.87 | 0.004 |
| Year 1 parent BMI | 0.08 | [0.01, 0.15] | 0.03 | 2.25 | 0.025 |
| Race | 0.22 | [0.15, 0.29] | 0.04 | 6.24 | < 0.001 |
| Predictors of year 5 ineffectiveness | |||||
| Year 2 perceived stress | 0.24 | [0.17, 0.3] | 0.03 | 7.18 | < 0.001 |
| Year 1 income | − 0.11 | [− 0.18, − 0.04] | 0.04 | − 3.2 | 0.001 |
| Year 1 BMI | 0.09 | [0.03, 0.15] | 0.03 | 2.86 | 0.004 |
| Year 1 parent BMI | 0.09 | [0.02, 0.16] | 0.04 | 2.46 | 0.014 |
| Race | − 0.02 | [− 0.09, 0.05] | 0.04 | − 0.57 | 0.566 |
| Predictors of year 5 self-worth | |||||
| Year 2 perceived stress | − 0.25 | [− 0.31, − 0.18] | 0.03 | − 7.44 | < 0.001 |
| Year 1 income | 0.04 | [− 0.03, 0.11] | 0.04 | 1.19 | 0.234 |
| Year 1 BMI | − 0.1 | [− 0.16, − 0.03] | 0.03 | − 2.85 | 0.004 |
| Year 1 parent BMI | − 0.08 | [− 0.15, − 0.01] | 0.04 | − 2.13 | 0.033 |
| Race | 0.13 | [0.06, 0.2] | 0.04 | 3.65 | < 0.001 |
| Predictors of year 2 perceived stress | |||||
| Year 1 income | − 0.14 | [− 0.21, − 0.07] | 0.04 | − 3.79 | < 0.001 |
| Year 1 parent BMI | − 0.07 | [− 0.15, 0] | 0.04 | − 1.97 | 0.049 |
| Race | 0.1 | [0.03, 0.17] | 0.04 | 2.79 | 0.005 |
| Predictors of year 1 BMI | |||||
| Year 1 parent BMI | 0.29 | [0.22, 0.35] | 0.03 | 8.73 | < 0.001 |
| Race | 0.09 | [0.02, 0.15] | 0.03 | 2.52 | 0.012 |
| Predictors of year 1 parent BMI | |||||
| Race | 0.21 | [0.15, 0.28] | 0.03 | 6.37 | < 0.001 |
| Predictors of year 1 income | |||||
| Race | − 0.29 | [− 0.35, − 0.23] | 0.03 | − 9.11 | < 0.001 |
Table 2.
Parameter values for path model with anxiety and psychological variables
| Predictor | b | 95% CI | SE | z | p |
|---|---|---|---|---|---|
| Predictors of year 10 BMI | |||||
| Year 1 income | − 0.05 | [− 0.1, − 0.01] | 0.02 | − 2.27 | 0.023 |
| Year 5 interoceptive awareness | 0.03 | [− 0.02, 0.08] | 0.03 | 1.26 | 0.207 |
| Year 5 interpersonal distrust | 0.07 | [0.01, 0.13] | 0.03 | 2.36 | 0.018 |
| Year 5 ineffectiveness | − 0.03 | [− 0.1, 0.04] | 0.04 | − 0.75 | 0.455 |
| Year 5 self-worth | − 0.04 | [− 0.09, 0.01] | 0.03 | − 1.63 | 0.103 |
| Year 1 BMI | 0.76 | [0.72, 0.79] | 0.02 | 40.52 | < 0.001 |
| Year 1 parent BMI | 0.1 | [0.05, 0.14] | 0.02 | 4.14 | < 0.001 |
| Race | 0.02 | [− 0.03, 0.06] | 0.02 | 0.72 | 0.472 |
| Predictors of year 5 interoceptive awareness | |||||
| Year 3 anxiety | 0.35 | [0.29, 0.41] | 0.03 | 11.3 | < 0.001 |
| Year 1 income | − 0.11 | [− 0.18, − 0.04] | 0.04 | − 3.11 | 0.002 |
| Year 1 BMI | 0.09 | [0.02, 0.16] | 0.04 | 2.6 | 0.009 |
| Year 1 parent BMI | 0 | [− 0.07, 0.07] | 0.04 | − 0.05 | 0.963 |
| Race | 0.11 | [0.04, 0.17] | 0.03 | 3.2 | 0.001 |
| Predictors of year 5 interpersonal distrust | |||||
| Year 3 anxiety | 0.23 | [0.16, 0.29] | 0.03 | 6.97 | < 0.001 |
| Year 1 income | − 0.09 | [− 0.16, − 0.02] | 0.03 | − 2.67 | 0.008 |
| Year 1 parent BMI | 0.06 | [0, 0.12] | 0.03 | 1.96 | 0.05 |
| Race | 0.22 | [0.15, 0.29] | 0.04 | 6.25 | < 0.001 |
| Predictors of year 5 ineffectiveness | |||||
| Year 3 anxiety | 0.35 | [0.29, 0.41] | 0.03 | 11.23 | < 0.001 |
| Year 1 income | − 0.11 | [− 0.17, − 0.04] | 0.04 | − 2.97 | 0.003 |
| Year 1 BMI | 0.08 | [0, 0.16] | 0.04 | 2.07 | 0.039 |
| Year 1 parent BMI | 0.07 | [0, 0.14] | 0.04 | 1.85 | 0.064 |
| Race | − 0.02 | [− 0.09, 0.05] | 0.04 | − 0.53 | 0.594 |
| Predictors of year 5 self-worth | |||||
| Year 3 anxiety | − 0.4 | [− 0.46, − 0.34] | 0.03 | − 13.31 | < 0.001 |
| Year 1 income | − 0.08 | [− 0.16, − 0.01] | 0.04 | − 2.26 | 0.024 |
| Year 1 BMI | − 0.05 | [− 0.13, 0.02] | 0.04 | − 1.49 | 0.135 |
| Year 1 parent BMI | 0.03 | [− 0.04, 0.09] | 0.03 | 0.88 | 0.378 |
| Race | 0.13 | [0.06, 0.19] | 0.03 | 3.73 | < 0.001 |
| Predictors of year 3 anxiety | |||||
| Year 1 income | − 0.11 | [− 0.17, − 0.04] | 0.03 | − 3.06 | 0.002 |
| Year 1 parent BMI | 0.12 | [0.06, 0.18] | 0.03 | 3.79 | < 0.001 |
| Predictors of year 1 BMI | |||||
| Year 1 parent BMI | 0.29 | [0.21, 0.37] | 0.04 | 6.79 | < 0.001 |
| Race | 0.09 | [0.02, 0.15] | 0.03 | 2.57 | 0.01 |
| Predictors of year 1 parent BMI | |||||
| Race | 0.21 | [0.15, 0.28] | 0.03 | 6.59 | < 0.001 |
| Predictors of year 1 income | |||||
| Race | − 0.29 | [− 0.35, − 0.23] | 0.03 | − 8.91 | < 0.001 |
In each of these two models, the pathways that were of primary interest were from household income to stress or anxiety, from stress or anxiety to more fine-grained psychological variables, and from these psychological variables to BMI at year 10. We found that household income predicted both stress and anxiety, such that lower levels of income led to higher levels of each of these two types of psychological distress. Stress and anxiety both negatively predicted global self-worth and positively predicted poor interoceptive awareness, interpersonal distrust, and ineffectiveness. In each model, higher levels of interpersonal distrust predicted higher year 10 BMI, whereas global self-worth only marginally predicted lower year 10 BMI. Both the relationship between poor interoceptive awareness and year 10 BMI and the relationship between ineffectiveness and year 10 BMI were non-significant. In addition, household income negatively predicted interpersonal distrust, poor interoceptive awareness, and ineffectiveness. Additionally, year 1 BMI positively predicted poor interoceptive awareness and ineffectiveness and negatively predicted global self-worth. Year 1 parent BMI positively predicted interpersonal distrust, ineffectiveness, and both forms of psychological distress and negatively predicted self-worth. Year 1 parent BMI also strongly positively predicted year 1 participant BMI, and year 1 parent BMI as well as year 1 participant BMI positively predicted year 10 participant BMI. Race predicted poor interoceptive awareness (greater levels of poor interoceptive awareness for African-Americans), interpersonal distrust (higher for African-Americans), stress (lower for African-Americans), and self-worth (higher for African-Americans), but not anxiety. After accounting for all these relationships, household income still negatively predicted year 10 participant BMI and the relationship between race and year 10 BMI was non-significant. Race predicted income and parent BMI such that African-American participants had lower income and parents with higher BMI.
Model fit indices indicated good fit for the model which included stress and eating behavior variables both for our test set (χ2(12, N = 793) = 15.08, p = 0.237, TLI = 0.99, CFI = 0.99, RMSEA = 0.02, SRMR = 0.03; see Table S1 in SOM) and for the entire dataset (χ2(12, N = 2379) = 23.72, p = 0.022, TLI = 0.99, CFI = 0.99, RMSEA = 0.02, SRMR = 0.02). Model fit indices indicated good fit for the model which included anxiety and eating behavior variables both for our test set (χ2(14, N = 793) = 32.86, p = 0.003, TLI = 0.96, CFI = 0.98, RMSEA = 0.04, SRMR = 0.04; see Table S2 in SOM) and for the entire dataset (χ2(14, N = 2379) = 25.91, p = 0.027, TLI = 0.99, CFI = 0.99, RMSEA = 0.02, SRMR = 0.02).
In each of these two models, we again found that household income predicted both stress and anxiety such that lower levels of income led to higher levels of each of these two types of psychological distress. In the model which included stress, stress positively predicted year 7 eating secretly, year 6 purchases snack food whenever, and marginally predicted year 5 stopped eating (question asked whether participant stopped eating for more than a day due to reasons other than sickness). In the model which included anxiety, anxiety positively predicted year 7 eating secretly, and year 5 stopped eating, but not year 6 purchases snack food. Importantly, these three eating behavior variables did not predict year 10 BMI after controlling for year 1 BMI, parent BMI, and race. Year 1 parent BMI positively predicted both forms of psychological distress. In each of these two models, year 1 parent BMI strongly positively predicted year 1 participant BMI. Year 1 participant BMI positively predicted year 10 participant BMI. Race predicted stress (lower for African-Americans) and year 6 purchases snack food (higher for African-Americans). After accounting for all of these relationships, household income only marginally negatively predicted year 10 participant BMI. Race also predicted income and parent BMI such that African-American participants had lower income and parents with higher BMI.
Discussion
Our results provide evidence that psychological distress mediates the relationship between income and increases in BMI in adolescent girls. In particular, lower levels of household income predicted higher levels of both stress and anxiety, each of which predicted a host of more fine-grained psychological and behavioral outcomes, some of which predicted increases in BMI over the 10-year study period. Importantly, these additional psychological and behavioral measures accounted for all of the variance in what were statistically significant direct paths of similar magnitude from stress and anxiety to BMI at year 10 (see SOM).
From Income to Outcomes
In models focused on psychological variables, psychological distress strongly predicted interpersonal distrust, interoceptive awareness, ineffectiveness, and self-worth. However, only interpersonal distrust predicted BMI at year 10 after controlling for year 1 BMI, parent BMI, and race. In a separate regression model, interpersonal distrust, interoceptive awareness, and self-worth were all statistically significant predictors of year 10 BMI (see SOM). We believe it is important to control for demographic variables that have been shown to predict increases in BMI. However, because some of these control variables (e.g., year 1 BMI) are themselves predictors of interpersonal distrust, interoceptive awareness, and self-worth, our models may control for some of the variance associated with these psychological constructs. Nonetheless, these results corroborate prior work indicating that low SES individuals tend to experience higher levels of distrust than high SES individuals (Jachimowicz, Chafik, Munrat, Prabhu, & Weber, 2017) and also that this facet of the EDI is associated with disordered eating and higher BMI (Clausen, Rosenvinge, Friborg, & Rokkedal, 2011). Interestingly, the items in the interpersonal distrust subscale (e.g., “I am open about my feelings,” reverse scored) assess problems communicating emotion and are similar to items that measure expressive suppression (Gross & John, 2003), which has recently been linked to emotional eating (Görlach, Kohlmann, Shedden-Mora, Rief, & Westermann, 2016). Apart from disordered eating and body dissatisfaction, the constructs assessed by the EDI appear to measure impairments in affect regulation (Sainsbury et al., 2019) and self-efficacy (Linde, Rothman, Baldwin, & Jeffery, 2006), both of which have been linked to unhealthy eating behavior.
In models focused on eating behavior variables, although stress and anxiety both predicted eating behaviors, these behaviors did not predict increases in BMI. Measuring eating behavior is notoriously difficult and generally yields noisy estimates of true eating behavior (Johnson, 2002). This greater level of noise manifested in our data in that the eating behavior variables predicted increases in BMI when our models were fit on the entire dataset, but not when fit on the test set alone. Additionally, we interpret the variables in our models as representative of what we speculate are broader trends in maladaptive eating behavior that result from psychological distress, such as unhealthy eating, overeating, and restrictive eating.
Across all models, we found no evidence of a relationship between income and participant BMI at year 1. The fact that the relationships between income, psychological distress, increases in BMI, and other variables developed over the course of the 10-year study supports the causal argument made in this paper and suggests that this relationship may begin to develop during adolescence. Indeed, we found evidence in support of baseline relationships between parental BMI and psychological distress, but not between own BMI and psychological distress, suggesting that a parent’s excess weight might have been related to this construct when the participant’s own weight was not yet a source of distress.
Implications
A growing body of literature indicates that external features of the low-income environment (Allcott et al., 2019; Hastings, Kessler, & Shapiro, 2019; Pechey & Monsivais, 2016) do not account for the entire relationship between SES and unhealthy eating, which is strongly linked to increases in BMI. The results of the present research are consistent with the hypothesis that psychological factors may play a role in driving unhealthy eating behavior and increases in BMI. The purpose of this work was to examine whether psychological distress mediates the relationship between income and increases in BMI in adolescents. This research sets the stage for future research to examine precisely why psychological distress leads to increases in BMI. There are likely to be several reasons why psychological distress has this effect. Psychological distress may impair self-control needed to engage in healthy eating behavior (Arnsten, 2009; Maier et al., 2015), and it may lead to people to engage in eating behaviors aimed at reducing psychological distress (Arnow et al., 1995).
The present findings suggest that interventions that decrease psychological distress may be one effective method for reducing socioeconomic health disparities. Psychological interventions designed to reduce food-related or integral affect (i.e., affect directly related to the behavior at hand, craving for food) have recently been deployed with success (Boswell, Sun, Suzuki, & Kober, 2018). While these interventions show promise, most psychological distress that people experience is in fact incidental (i.e., unrelated) to food (Trampe, Quoidbach, & Taquet, 2015). Interventions designed to teach people how to downregulate psychological distress in general may therefore be even more effective than ones designed to downregulate food-related affect.
Strengths and Limitations
There are notable strengths of the present research including the relatively large sample size and the 10-year prospective design. In addition, the rich array of psychological measures is rare in a study of this size and duration. However, the primary strength of the current research is that it used methods from machine learning and path analysis to analyze longitudinal data and to build models of the relationships between income, psychological distress, and increases in BMI. Using validation set and variable selection methods allowed for a more principled approach to model building and testing than is feasible with smaller datasets that do not allow for such partitioning. Using path analysis with longitudinal data licenses stronger causal inferences than those that can be made with cross-sectional data.
Several limitations of the present research should be acknowledged. First, the sample was composed exclusively of adolescent female participants, limiting generalizability. In addition, all participants were either White or Black. Other research has shown that weight-related diseases are highly prevalent among other ethnic populations, such as Hispanics (Cossrow & Falkner, 2004), and it remains unknown whether the models presented in the current paper apply to these populations as well. Finally, because all participants in the current study were age 9 or 10 when the study began and age 18 or 19 when the study completed, most participants went through puberty during the study. Prior research has shown that complex relationships exist among psychological distress, increases in BMI, and puberty (Jasik & Lustig, 2008). Due to the complexity of the models presented in the current research, we opted not to include measures related to puberty, but interactions among income, psychological distress, and pubertal timing likely played a role in the outcomes examined. Future research should investigate these relationships further.
Conclusion
The present research indicates that psychological factors are partly responsible for disparities in behavior and health observed in societies plagued by the obesity epidemic. In addition, it suggests that psychological distress may be one factor causing these health disparities. Future work should examine what features of the experience of low-income individuals are most likely to lead to heightened psychological distress and should develop interventions aimed at alleviating associated psychological distress.
Electronic Supplementary Material
(DOCX 62 kb)
Additional Information
Data Availability
All data is publicly available from the NHLBI. All analysis code is available online at: https://github.com/djolear/nghs1_pub_repo.
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethical Approval
This study was approved by the Institutional Review Board at Stanford University.
Informed Consent
Informed consent was obtained by the researchers who originally collected the data used in this study (see https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.82.12.1613).
References
- Allcott H, Diamond R, Dubé JP, Handbury J, Rahkovsky I, Schnell M. Food deserts and the causes of nutritional inequality. Quarterly Journal of Economics. 2019;134:1793–1844. doi: 10.1093/qje/qjz015. [DOI] [Google Scholar]
- Arnow B, Kenardy J, Agras WS. The Emotional Eating Scale: The development of a measure to assess coping with negative affect by eating. The International Journal of Eating Disorders. 1995;18:79–90. doi: 10.1002/1098-108X(199507)18:1<79::AID-EAT2260180109>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Arnsten AFT. Stress signalling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience. 2009;10:410–422. doi: 10.1038/nrn2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K, Schoenaker DAJM, Mishra GD. Does psychosocial stress explain socioeconomic inequities in 9-year weight gain among young women? Obesity. 2017;25:1109–1114. doi: 10.1002/oby.21830. [DOI] [PubMed] [Google Scholar]
- Boswell RG, Sun W, Suzuki S, Kober H. Training in cognitive strategies reduces eating and improves food choice. Proceedings of the National Academy of Sciences of the United States of America. 2018;115:E11238–E11247. doi: 10.1073/pnas.1717092115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumpton B, Langhammer A, Romundstad P, Chen Y, Mai X-M. The associations of anxiety and depression symptoms with weight change and incident obesity: The HUNT Study. International Journal of Obesity. 2013;37:1268–1274. doi: 10.1038/ijo.2012.204. [DOI] [PubMed] [Google Scholar]
- Childhood Overweight and Obesity. (2019). Retrieved from https://www.cdc.gov/obesity/childhood/index.html
- Claassen MA, Klein O, Bratanova B, Claes N, Corneille O. A systematic review of psychosocial explanations for the relationship between socioeconomic status and body mass index. Appetite. 2019;132:208–221. doi: 10.1016/j.appet.2018.07.017. [DOI] [PubMed] [Google Scholar]
- Clausen L, Rosenvinge JH, Friborg O, Rokkedal K. Validating the eating disorder inventory-3 (EDI-3): A comparison between 561 female eating disorders patients and 878 females from the general population. Journal of Psychopathology and Behavioral Assessment. 2011;33:101–110. doi: 10.1007/s10862-010-9207-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of Applied Social Psychology. 2012;42(6):1320–1334. doi: 10.1111/j.1559-1816.2012.00900.x. [DOI] [Google Scholar]
- Cohen S, Doyle WJ, Baum A. Socioeconomic status is associated with stress hormones. Psychosomatic Medicine. 2006;68:414–420. doi: 10.1097/01.psy.0000221236.37158.b9. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. The Journal of Clinical Endocrinology & Metabolism. 2004;89:2590–2594. doi: 10.1210/jc.2004-0339. [DOI] [PubMed] [Google Scholar]
- Dallman MF. Stress-induced obesity and the emotional nervous system. Trends in Endocrinology and Metabolism. 2010;21:159–165. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Specter S. Poverty and obesity: The role of energy density and energy costs. The American Journal of Clinical Nutrition. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- Friedman, J., Hastie, T., & Tibshirani, R. (2010). Regularization Paths for Generalized Linear Models via Coordinate Descent. Journal of Statistical Software,33(1), 1-22. [PMC free article] [PubMed]
- Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:1338–1342. doi: 10.1073/pnas.1321355110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–34. doi: 10.1002/1098-108X(198321)2:2<15::AID-EAT2260020203>3.0.CO;2-6. [DOI] [Google Scholar]
- Görlach MG, Kohlmann S, Shedden-Mora M, Rief W, Westermann S. Expressive suppression of emotions and overeating in individuals with overweight and obesity. European Eating Disorders Review. 2016;24:377–382. doi: 10.1002/erv.2452. [DOI] [PubMed] [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hare T, Camerer C, Rangel A. Self-control in decision-making involves modulation of the vmpfc valuation system. Science. 2009;324:646–648. doi: 10.1126/science.1168450. [DOI] [PubMed] [Google Scholar]
- Harter S. The perceived competence scale for children. Child Development. 1982;53:87–97. doi: 10.2307/1129640. [DOI] [PubMed] [Google Scholar]
- Hastings, J., Kessler, R. E., & Shapiro, J. M. (2020). The effect of SNAP on the composition of purchased foods: Evidence and implications. Manuscript in preparation.
- Jachimowicz JM, Chafik S, Munrat S, Prabhu JC, Weber EU. Community trust reduces myopic decisions of low-income individuals. Proceedings of the National Academy of Sciences of the United States of America. 2017;114:5401–5406. doi: 10.1073/pnas.1617395114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasik CB, Lustig RH. Adolescent obesity and puberty: The “perfect storm”. Annals of the New York Academy of Sciences. 2008;1135:265–279. doi: 10.1196/annals.1429.009. [DOI] [PubMed] [Google Scholar]
- Johnson RK. Dietary intake-how do we measure what people are really eating? Obesity Research. 2002;10:63S–68S. doi: 10.1038/oby.2002.192. [DOI] [PubMed] [Google Scholar]
- Kuhn, M. (2008). Building predictive models in R using the caret package. Journal of Statistical Software, 28.
- Linde JA, Rothman AJ, Baldwin AS, Jeffery RW. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychology. 2006;25:282–291. doi: 10.1037/0278-6133.25.3.282. [DOI] [PubMed] [Google Scholar]
- Maier S, Makwana A, Hare T. Acute stress impairs self-control in goal-directed choice by altering multiple functional connections within the brain’s decision circuits. Neuron. 2015;87:621–631. doi: 10.1016/j.neuron.2015.07.005. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Fakhouri TH, Carroll MD, Hales CM, Fryar CD, Li X, Freedman DS. Prevalence of obesity among adults, by household income and education — United States, 2011–2014. Morbidity and Mortality Weekly Report. 2017;66:1369–1373. doi: 10.15585/mmwr.mm6650a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechey R, Monsivais P. Socioeconomic inequalities in the healthiness of food choices: Exploring the contributions of food expenditures. Preventive Medicine. 2016;88:203–209. doi: 10.1016/j.ypmed.2016.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Rehkopf DH, Laraia BA, Segal M, Braithwaite D, Epel E. The relative importance of predictors of body mass index change, overweight and obesity in adolescent girls. International Journal of Pediatric Obesity. 2011;6:e233–e242. doi: 10.3109/17477166.2010.545410. [DOI] [PubMed] [Google Scholar]
- Reutter LI, Stewart MJ, Veenstra G, Love R, Raphael D, Makwarimba E. “Who do they think we are, anyway?”: Perceptions of and responses to poverty stigma. Qualitative Health Research. 2009;19:297–311. doi: 10.1177/1049732308330246. [DOI] [PubMed] [Google Scholar]
- Reynolds, C. R., & Richmond, B. O. (1978). What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology, 25, 15–20. [DOI] [PubMed]
- Sainsbury K, Evans EH, Pedersen S, Marques MM, Teixeira PJ, Lähteenmäki L, Stubbs RJ, Heitmann BL, Sniehotta FF. Attribution of weight regain to emotional reasons amongst European adults with overweight and obesity who regained weight following a weight loss attempt. Eating and Weight Disorders. 2019;24:351–361. doi: 10.1007/s40519-018-0487-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Afifi TO, McMillan KA, Asmundson GJG. Relationship between household income and mental disorders. Archives of General Psychiatry. 2011;68:419–427. doi: 10.1001/archgenpsychiatry.2011.15. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Social Science & Medicine. 2003;56:1321–1333. doi: 10.1016/S0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Spinosa, J., Christiansen, P., Dickson, J. M., Lorenzetti, V., & Hardman, C. A. (2019). From socioeconomic disadvantage to obesity: The mediating role of psychological distress and emotional eating. Obesity., 27, 559–564. [DOI] [PMC free article] [PubMed]
- Stekhoven DJ, Buhlmann P. MissForest--non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28:112–118. doi: 10.1093/bioinformatics/btr597. [DOI] [PubMed] [Google Scholar]
- Taylor JA. A personality scale of manifest anxiety. Journal of Abnormal and Social Psychology. 1953;48:285–290. doi: 10.1037/h0056264. [DOI] [PubMed] [Google Scholar]
- Tibshirani, R. (1996). Regression Shrinkage and Selection Via the Lasso. Journal of the Royal Statistical Society: Series B (Methodological) 58(1), 267-288.
- Tobin DL, Holroyd KA, Reynolds RV, Wigal JK. The hierarchical factor structure of the coping strategies inventory. Cognitive Therapy and Research. 1989;13:343–361. doi: 10.1007/BF01173478. [DOI] [Google Scholar]
- Tomiyama AJ, Puterman E, Epel ES, Rehkopf DH, Laraia BA. Chronic psychological stress and racial disparities in body mass index change between black and white girls aged 10–19. Annals of Behavioral Medicine. 2013;45:3–12. doi: 10.1007/s12160-012-9398-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23:887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- Trampe D, Quoidbach J, Taquet M. Emotions in everyday life. PLoS One. 2015;10:1–15. doi: 10.1371/journal.pone.0145450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whelan CT, Maître B. Material deprivation, economic stress, and reference groups in Europe: An analysis of EU-SILC 2009. European Sociological Review. 2013;29(6):1162–1174. doi: 10.1093/esr/jct006. [DOI] [Google Scholar]
- Zou, H., Hastie, T. (2005). Regularization and variable selection via the elastic net. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 67(2), 301-320.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 62 kb)
Data Availability Statement
All data is publicly available from the NHLBI. All analysis code is available online at: https://github.com/djolear/nghs1_pub_repo.