Background
Lapses in quality of care for patients with chronic pain who have been prescribed long-term opioid therapy can lead to worsened function, addiction, and death [1]. For this vulnerable group, guidelines recommend a patient-centered, team-based approach that includes 1) individualized assessment of the benefits and harms of long-term opioid therapy, 2) reduction or discontinuation of long-term opioid therapy when the benefits no longer outweigh the harms, 3) a switch to buprenorphine if difficulty tapering or opioid use disorder emerges, and 4) optimization of nonpharmacological and non-opioid pain treatment [2, 3]. Because of the coronavirus disease 2019 (COVID-19) pandemic, in March 2020, our interdisciplinary pain team pivoted quickly to deliver these essential services virtually. Here, we describe and report an evaluation of those adaptations.
Program Description
The Opioid Reassessment Clinic (ORC) of Veterans Administration (VA) Connecticut Healthcare System provides interdisciplinary assessment and longitudinal, team-based care to veterans with chronic pain exhibiting problems related to the safety, efficacy, or misuse of prescribed opioids [4]. The ORC works with patients to enhance the multimodal treatment plan (e.g., by promoting engagement in new nonpharmacological pain management approaches) and implement changes in pain medication (e.g., by offering an opioid taper or transition to buprenorphine). ORC staff include an addiction psychiatrist, an internist, a psychologist, a pharmacist, and a nurse, as well as trainees from several disciplines. The clinic typically receives referrals from primary care providers at their own discretion and schedules up to two new patient evaluations per week. Clinicians in the ORC incorporate motivational interviewing [5] techniques, such as evoking patients’ perspectives and the elicit–provide–elicit technique, to enhance collaboration. Typically, the clinic runs one half day per week in a primary care clinic space at VA Connecticut. In March 2020, to adapt to the COVID-19 pandemic, the ORC became entirely virtual—clinicians interacted with each other and patients via videoconferencing platforms and telephone only.
Program Modifications
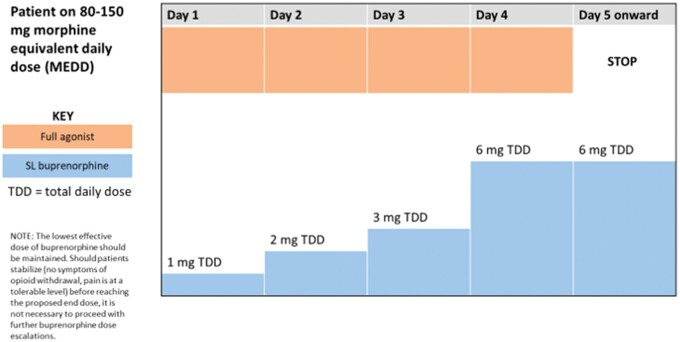
To facilitate the success of a virtual clinic, we implemented changes in patient assessment, buprenorphine initiation, patient experience, and team functioning. We streamlined the intake process by combining the medical and psychology intake assessments (previously done separately) to minimize redundancy without changing appointment length. We implemented several standardized templates and interview guides to facilitate coordination between disciplines and consistency across intake assessments. Second, we evaluated buprenorphine appropriateness and provided counseling and education about buprenorphine via telephone or video. When indicated, we used an overlap dosing protocol [6] developed in our clinic (see Figure 1) to start buprenorphine. With the use of this protocol, risk of opioid withdrawal is minimized; buprenorphine is mailed to patients’ homes with written instructions on how to gradually escalate the buprenorphine dose while continuing full agonist opioids. After 4–6 days, full agonist opioids are discontinued, and we provide frequent follow-up via telephone or video to titrate buprenorphine doses to maximize function and analgesia. Third, we enhanced the patient experience by adding a welcome letter and pre-appointment phone call to orient patients to the clinic, expanded the use of patient handouts to facilitate communication, offered patients a choice between video and telephone visits, and added standardized language to clinic templates to ensure a patient-centered approach (e.g., use of motivational interviewing [5] and trauma-informed care [7]). Finally, to enhance team functioning, we added dedicated team time with a structured agenda before clinic started each week (including time for brief “learning bursts,” such as refreshers on motivational interviewing [5]), added weekly team meetings outside of clinic to debrief and review follow-up plans, used multiple video/chat platforms to enhance team communication during clinic (to simulate a “team workroom”), and more explicitly defined team members’ roles.
Figure 1.
Example of buprenorphine overlap dosing protocol.
Program Evaluation
To evaluate clinic changes, we began conducting satisfaction surveys with patients who had been evaluated in our clinic; this quality improvement project did not require institutional review board approval. Satisfaction surveys were offered to all new patients evaluated by our clinic between May 2020 and October 2020. Surveys included seven close-ended Likert-scale questions and three open-ended questions: “What was something you liked about your intake appointment?”, “What was something that you think could have been even better?”, and “Do you have any additional comments or concerns?”. Answers were notated by interviewers. Survey data were summarized with descriptive statistics (Table 1). Rapid qualitative analysis [8] identified themes. Opioid changes at 30 days after intake were assessed by chart review.
Table 1.
Descriptive statistics of survey results
| Question | n | Mean (SD) | Median |
|---|---|---|---|
| 1. How easy was it for you to access your appointment? (5 = very easy, 1 = not easy at all) | 20 | 4.5 (1.00) | 5 |
| 2. How clearly could you hear the ORC members over the phone/video during your appointment? (5 = very clearly, 1 = not clearly at all) | 20 | 4.53 (0.82) | 5 |
| 3. How comfortable did you feel sharing your experiences with the ORC team? (5 = very comfortable, 1 = not comfortable at all) | 20 | 4.25 (1.16) | 5 |
| 4. How comfortable did you feel asking questions during your appointment? (5 = very comfortable, 1 = not comfortable at all) | 20 | 4.26 (1.07) | 5 |
| 5. How well do you feel that the ORC team members listened to you during your appointment? (5 = very well, 1 = not well at all) | 20 | 4.18 (1.04) | 4 |
| 6. How well did you understand your treatment options communicated by the ORC team? (5 = very well, 1 = not well at all). | 18 | 4.22 (1.11) | 5 |
| 7. Have you had any follow-up calls or contact with anyone from the clinic since your intake appointment? If yes, how satisfied were you with the follow-up? (5 = very satisfied, 1 = not satisfied at all) | 5* | 4.40 (0.89) | 5 |
SD = standard deviation.
Smaller n is due to several patients not having follow-up contact at the time of the survey.
Over the 6-month study period, the ORC evaluated 29 new patients; 20 completed the survey (five declined, and four were not reachable); sample characteristics are given in Table 2. With regard to survey results, patients felt it was easy to access their appointments and were satisfied (see Table 1), noting that providers were empathetic, patient centered, and nonjudgmental. One patient said, “The main priority was me … I felt very comfortable.” Another patient noted, “I felt comfortable to say what I needed to say, I knew they would listen to me, and they gave me good advice moving forward.” A patient remarked, “Everybody was very open-minded and nonjudgmental. They want to help me, and I don’t feel like I am being treated like a number. It was a great experience.” Other themes included clarity of the plan, appreciation of the interdisciplinary approach, and ease of accessing appointments virtually. One patient commented, “I liked that there were multiple providers on the call, it was a team approach.”
Table 2.
Sample characteristics
| Characteristic | M (SD) or % (n) |
|---|---|
| Age, years | 62.9 (11.2) |
| Gender, male | 86.2% (25) |
| Race | |
| White | 82.8% (24) |
| Black | 13.8% (4) |
| Other | 3.4% (1) |
| Referral source | |
| Primary care provider | 79.3% (23) |
| Palliative care | 10.3% (3) |
| Other | 10.3% (3) |
| Opioid use disorder diagnosis, % yes | 3.4% (1) |
| Urine drug toxicology in past 12 months, % yes | 65.5% (19) |
| Health psychology, % with at least one appointment | 34.4% (10) |
| Opioid medication recommendation at intake | |
| Buprenorphine | 58.6% (17) |
| Continued full agonist opioid | 31.0% (9) |
| Other | 10.3% (3) |
| Opioid medication at 30 days after intake | |
| Buprenorphine | 48.3% (14) |
| Continued full agonist opioid | 3.8% (11) |
| Not on buprenorphine or full agonist opioid | 13.8% (4) |
M = mean; SD = standard deviation.
With regard to needed improvements, the most common theme was confusion about the treatment plan. One patient asked, “What happens if the medication doesn’t work? Where do we go from here?” Other themes included technology challenges, dissatisfaction with the visit structure (e.g., too long), and a preference for in-person appointments, particularly when patients had technological challenges and were unable to use video: “I wished I could have seen the faces of the people I was talking with” (in reference to a phone appointment due to problems with video connectivity).
With regard to opioids, at intake we recommended buprenorphine to slightly more than half of our patients (58.6%), and at 30 days after intake, 48.3% of patients were taking buprenorphine (see Table 2). No patients reported adverse events related to tapering or transitioning to buprenorphine.
Lessons Learned
The opioids crisis has complicated care for patients with chronic pain, particularly patients who have been prescribed long-term opioid therapy who demonstrate problems related to the safety, efficacy, or misuse of opioids. Interdisciplinary team-based care of pain and opioid use disorder, including access to multimodal evidence-based pain management approaches, is important. During the COVID-19 pandemic, access to care has been reduced: Interdisciplinary care is more difficult to coordinate, and some pain treatments are temporarily unavailable. Furthermore, stress related to the pandemic and reduced access to care may be contributing to worsened pain-related functioning and increased risk of adverse opioid-related events [9]. Novel ways to continue to care for these patients during the pandemic are urgently needed.
To adapt to restrictions on in-person care due to the COVID-19 pandemic, the ORC made changes in patient assessment, buprenorphine initiation, patient and trainee experience, and team functioning. On the basis of high patient satisfaction scores (i.e., higher than previous scores reported from this clinic [4]) and uncomplicated transitions to buprenorphine from full agonist opioids, we demonstrated successful adaptation of an interdisciplinary in-person pain clinic to all-virtual delivery. Patients felt listened to, a critical piece of rapport-building that was not lost in virtual care delivery, likely because of providers’ use of motivational interviewing and our clinic’s efforts to frequently review motivational interviewing skills during team meetings. Some patients commented on the ease of participating from their homes. As patients with chronic pain often have mobility and transportation problems, offering video visits routinely irrespective of pandemic status could improve access to care. Some patients were dissatisfied with aspects of their visit to clinic, highlighting the need for technology support and developing additional written materials tailored to individual patients. Our buprenorphine initiation approach—telehealth assessment and counseling with a standardized overlap dosing protocol—was well tolerated by patients. This approach could be key in addressing many long-standing patient and provider barriers to buprenorphine initiation. We anticipate that several of the changes that were implemented to adapt to an all-virtual clinic model will be maintained as we return to offering in-person clinic: we plan to continue following a structured template for streamlined interdisciplinary intakes, providing patients with more information about our clinic before their intake, and protecting time for team meetings while we offer a mixture of virtual and in-person visits. Continuing to conduct some clinic visits and team meetings virtually also allows us more opportunities to disseminate the ORC model by inviting colleagues to join us virtually to observe patient evaluations or team meetings. Additionally, using virtual modalities for team communication allowed opportunities for real-time input from team members, either via chat functions or co-visiting, which can improve trainees’ experiences and care delivered to patients. We are engaged in ongoing work to disseminate the ORC model throughout the VA; implementation efforts in non-VA settings are needed. Offering flexible formats for patient appointments expands access to clinical care. Interprofessional, team-based assessments decreases duplicative assessments while enhancing interdisciplinary learning. Overall, increased structure (e.g., intake templates), multiple communication platforms (chat/video), and an emphasis on interdisciplinary team function (e.g., interdisciplinary intakes, time for team meetings, learning bursts) contributed to our success. More work is also needed to evaluate clinical outcomes of patients who participate in the ORC, including post-pandemic comparisons of patients who participate fully virtually vs patients who attend in-person appointments.
Contributor Information
Sara N Edmond, VA Connecticut Healthcare System, West Haven, Connecticut; Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut.
Sophia Currie, Yale University, New Haven, Connecticut.
Amanda Gehrke, Bay Pines VA Healthcare System, Lee County VA Health Care Center, Cape Coral, Florida.
Caroline G Falker, VA Connecticut Healthcare System, West Haven, Connecticut; Department of Internal Medicine, Yale School of Medicine, New Haven, Connecticut, USA.
Minhee Sung, VA Connecticut Healthcare System, West Haven, Connecticut; Department of Internal Medicine, Yale School of Medicine, New Haven, Connecticut, USA.
Audrey Abelleira, VA Connecticut Healthcare System, West Haven, Connecticut.
Ellen L Edens, VA Connecticut Healthcare System, West Haven, Connecticut; Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut.
William C Becker, VA Connecticut Healthcare System, West Haven, Connecticut; Department of Internal Medicine, Yale School of Medicine, New Haven, Connecticut, USA.
Funding sources: Dr. Edmond’s time on this project was supported by the Veterans Health Administration Health Services Research and Development Service Center of Innovation (CIN 13-407).
Disclosures: The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs or the United States Government.
Conflicts of interest: There are no conflicts of interest to disclose.
References
- 1. Lin L, Peltzman T, McCarthy JF, et al. Changing trends in opioid overdose deaths and prescription opioid receipt among veterans. Am J Prev Med 2019;57(1):106–10. [DOI] [PubMed] [Google Scholar]
- 2.VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives; National Mental Health Office—Substance Use Disorders; National Pain Management Strategy Coordinating Committee. Buprenorphine formulations for chronic pain management in patients with opioid use disorder or on long term opioid therapy with physiologic tolerance. 2020. Available at: www.pbm.va.gov.
- 3.VA/DoD. Clinical practice guideline for opioid therapy for chronic pain. 2017. Available at: https://www.va.gov/HOMELESS/nchav/resources/docs/mental-health/substance-abuse/VA_DoD-CLINICAL-PRACTICE-GUIDELINE-FOR-OPIOID-THERAPY-FOR-CHRONIC-PAIN-508.pdf
- 4. Becker WC, Edmond SN, Cervone DJ, et al. Evaluation of an integrated, multidisciplinary program to address unsafe use of opioids prescribed for pain. Pain Med 2018;19(7):1419–24. [DOI] [PubMed] [Google Scholar]
- 5. Miller WR, Rollnick S. Motivational Interviewing: Helping People Change, 3rd edition. New York, NY: The Guilford Press; 2013. [Google Scholar]
- 6. Becker WC, Frank JW, Edens EL. Switching from high-dose, long-term opioids to buprenorphine: A case series. Ann Intern Med 2020;173(1):70–1. [DOI] [PubMed] [Google Scholar]
- 7. Shamaskin-Garroway AM, Burg MM, Vasquez L, Brandt C, Haskell S. An interprofessional pilot program training medical residents in trauma-sensitive communication. J Interprof Educ Pract 2017;8:14–9. [Google Scholar]
- 8. Hamilton AB, Finley EP. Qualitative methods in implementation research: An introduction. Psychiatry Res 2019;280:112516 (doi: 10.1016/j.psychres.2019.112516). [DOI] [PMC free article] [PubMed]
- 9. Becker WC, Fiellin DA. When epidemics collide: Coronavirus disease 2019 (COVID-19) and the opioid crisis. Ann Intern Med 2020;173(1):59–60. [DOI] [PMC free article] [PubMed] [Google Scholar]