Heart failure is a clinical syndrome with symptoms and/or signs caused by a structural and/or functional cardiac abnormality and corroborated by elevated natriuretic peptide levels and/or objective evidence of pulmonary or systemic congestion.1),2) In South Korea, the prevalence rate of heart failure was 2.24% in 2018, and the number of older adult patients is increasing significantly (Heart Failure Statistics in Korea, 2020).3) In addition, older adult patients have various comorbidities such as diabetes mellitus, hypertension, dyslipidemia, arrhythmia, chronic kidney disease, cancer, stroke, dementia, and arthritis. The use of multiple medications increases the risk of side effects. Therefore, the treatment of chronic heart failure in older adult patients is complicated.
Heart failure is characterized by repeated worsening of symptoms and heart function, leading to frequent hospitalization and poor quality of life.4) Heart failure has a worse prognosis than cancer (excluding lung cancer), with 40–50% of the patients dying within 5 years after diagnosis. However, the prognosis may vary depending on the cause of heart failure. Most patients are often hospitalized because their heart functions continue to deteriorate, causing dyspnea, edema, arrhythmia, syncope, and sudden cardiac death. Therefore, it is essential to prevent the worsening of heart failure. The reduction in the number of hospitalizations or visits to the emergency department due to worsening of heart failure improves the quality of life and reduces the burden of medical expenses. According to Korean data,5) the mean 1-year heart failure-related cost per patient was KRW 2,607,173, which included both outpatient care (KRW 952,864) and inpatient care (KRW 1,654,309) expenses. Among hospitalized patients, the 1-year costs were 1.7-fold greater for patients who were admitted to the hospital via the emergency department than for those who were not (KRW 11,040,453 vs. KRW 6,317,942). Therefore, appropriate treatment strategies, including modification of risk factors to decrease hospitalization, are needed to reduce the economic burden of heart failure patients in South Korea.
In particular, older adult patients with heart failure require meticulous treatment as they receive a comprehensive evaluation of the condition as well as specialized treatment for various comorbidities. These patients should receive disease education from heart failure specialists and nurses as well as lifestyle and dietary changes and exercise education from nutritionists and physical therapists. It is necessary to control risk factors for heart failure, such as high blood pressure, dyslipidemia, and diabetes mellitus and ensure smoking cessation, reduced alcohol consumption, a low-salt diet, and reduced stress. Thus, multidisciplinary treatment is necessary, and the focus should be on cardiac rehabilitation of heart failure patients.
In South Korea, the patient classification system includes the specialized medical disease group (group A), general medical disease group (group B), and simple treatment disease group (group C). This classification is one of the most important criteria for selecting a tertiary hospital, which is reviewed every 4 years. Heart failure currently belongs to group B; however, considering the clinical course and prognosis, it needs to be upgraded to group A. This is because older adult patients with heart failure are repeatedly hospitalized or have various comorbidities or worsening symptoms, which is a burden to the health insurance sector.
According to the Health Insurance Review and Assessment Service, the burden of medical expenses of patients with heart failure has increased by 3.1 times over the past 10 years. In the United States, the multidisciplinary treatment system is well-established, and the government provides financial support to hospitals with good treatment outcomes in patients with severe heart failure.6) In South Korea, which has a super-aged society, it is essential to prepare long-term and systematic measures at the government level to treat the increasing number of patients with heart failure. These measures will simultaneously reduce patients’ medical expenses and health insurance finances. With the current health insurance system, a few minutes of outpatient treatment is insufficient to comprehensively determine the condition of patients with heart failure and many comorbidities and establish a treatment plan.
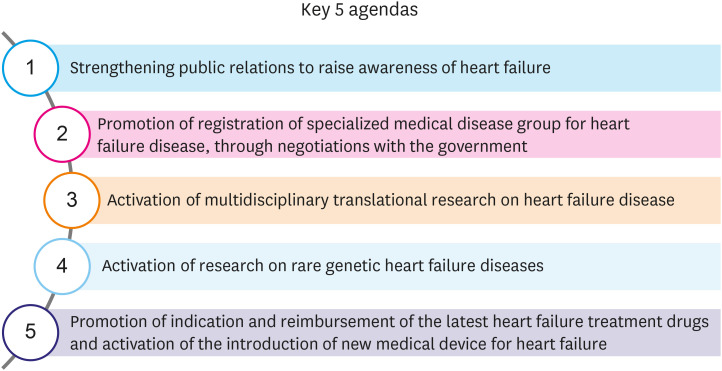
Therefore, the Korean Heart Failure Society presents five key agendas for the treatment of heart failure (Figure 1). First, public relations should be strengthened to raise awareness regarding heart failure. The general public, patients with heart failure, the government, media, and even medical personnel do not fully understand heart failure. Over the past few years, we have been able to improve awareness to some extent through the campaign hosted by the Korean Heart Failure Society. We should continue to promote “knowing heart failure right away” through various media channels and other activities. According to a previous study,7) Korean patients with heart failure did not have adequate knowledge about the disease, and they did not recognize the importance of being informed regarding heart failure. Therefore, we need to improve disease education and self-care program for Korean patients with heart failure. Second, registration of the specialized medical disease group for heart failure should be promoted through negotiations with the government. Heart failure is a disease that, if left untreated, follows a severe clinical course and has a high treatment cost and a very high risk of sudden death. In line with this evidence, we should urge the government to upgrade heart failure to the specialized medical disease group (group A). Third, multidisciplinary translational research on heart failure should be actively conducted. Heart failure is associated with various comorbidities, which can be investigated in cooperation with various sectors. We should strive to promote multidisciplinary research. Fourth, research on rare genetic causes of heart failure should be actively conducted. An interest in various hereditary causes of heart failure, such as familial dilated cardiomyopathy, cardiac amyloidosis, Fabry disease, etc., should be raised, and various clinical studies should be supported and initiated. Fifth, indication and reimbursement of the latest drugs for the treatment of heart failure should be promoted, and the introduction of new medical devices for the treatment of heart failure should be encouraged.
Figure 1. Key 5 agendas of Korean Society of Heart Failure.
Previously, doctors treated patients within their individual capacities. Currently, it is necessary to create a medical environment that can satisfy patients and ultimately reduce mortality rates through a systematic and individualized cooperative care system. Thus, it is essential to prepare a global policy for patients with heart failure, a representative chronic disease, in the near future.
Footnotes
Conflict of Interest: The author has no financial conflicts of interest.
References
- 1.Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:895–1032. doi: 10.1161/CIR.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 2.McDonagh TA, Metra M, Adamo M, et al. Corrigendum to: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42:4901. doi: 10.1093/eurheartj/ehab670. [DOI] [PubMed] [Google Scholar]
- 3.Park JJ, Lee CJ, Park SJ, et al. Heart failure statistics in Korea, 2020; a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021;3:224–236. doi: 10.36628/ijhf.2021.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shahar E, Lee S, Kim J, Duval S, Barber C, Luepker RV. Hospitalized heart failure: rates and long-term mortality. J Card Fail. 2004;10:374–379. doi: 10.1016/j.cardfail.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Ku H, Chung WJ, Lee HY, et al. Healthcare costs for acute hospitalized and chronic heart failure in South Korea: a multi-center retrospective cohort study. Yonsei Med J. 2017;58:944–953. doi: 10.3349/ymj.2017.58.5.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Psotka MA, Fonarow GC, Allen LA, et al. The hospital readmissions reduction program: nationwide perspectives and recommendations: a JACC: heart failure position paper. JACC Heart Fail. 2020;8:1–11. doi: 10.1016/j.jchf.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 7.Kim SS, Ahn JA, Kang SM, Kim G, Lee S. Learning needs of patients with heart failure a descriptive, exploratory study. J Clin Nurs. 2013;22:661–668. doi: 10.1111/j.1365-2702.2012.04075.x. [DOI] [PubMed] [Google Scholar]