Abstract
Introduction
Prior studies on the association between the intensity of and motives for vaping e-cigarettes have highlighted the psychological dynamics of motivational changes, but less about how vaping motives may shift as a function of risk perceptions exacerbated by unanticipated events. This study frames the COVID-19 pandemic as an exacerbating threat to pulmonary health, and tests how e-cigarette users’ risk perceptions of COVID-19 are related to different motives for vaping and ultimately the intensity of e-cigarette use.
Aims and Methods
An online survey of e-cigarette users in the United States (n = 562) was conducted during April 2020 when much of the United States was under “lockdown” conditions. We distinguished three types of vaping motives (health, socialization, and dependence) and established the classification with confirmatory factor analysis. Structural equation modeling was conducted for path analyses and mediation tests.
Results
All three vaping motives were significantly associated with greater use intensity. A heightened risk perception of e-cigarette users’ vulnerability to COVID-19 was inversely associated with use intensity (−.18, p < .01) and health motives for vaping (−.27, p < .001), but not associated with socialization and dependence motivations. Health motives for vaping mediated 35% of the association between COVID-19 risk perceptions and use intensity.
Conclusions
Our findings indicate that risk perceptions of exacerbated threats may reduce e-cigarette use directly, and also indirectly through shifting certain types of motivations for vaping. Beyond elucidating the relational dynamics between vaping psychology and health risks, these results also indicate health professionals may leverage the pandemic to promote nicotine cessation or reduced use.
Implication
Little is known about how vaping motives shift after unanticipated events such as pandemics. This study contributes to knowledge of how the use of e-cigarettes is motivated by different dimensions of rationales and exogenous risks. Exploiting the emergence of the COVID-19 pandemic, we found risk perceptions are associated with the intensity of e-cigarette use indirectly specifically through health motivations. Risk perceptions are not associated with socialization and dependence motives for vaping.
Introduction
Electronic nicotine delivery systems (hereafter e-cigarettes) are non-combustible nicotine delivery devices that transmit aerosol mixed with vaporized nicotine and sometimes flavored chemicals. Globally, the number of people using e-cigarettes grew from 7 million to over 40 million between 2011 and 2018.1 E-cigarettes have been advertised broadly to adults as a harm reduction alternative to combustible tobacco. Further, while smoking tobacco is prohibited in many public spaces in many countries, public vaping’s current status involves a great deal of ambiguity.2,3 In part due to the lack of inconsistency in regulations between combustible tobacco and e-cigarettes, e-cigarette users may hold beliefs that vaping is safer, noninvasive, and a fashionable alternative that helps them socialize or quit smoking conventional tobacco products.4,5
Yet, the popular beliefs about e-cigarettes were destabilized by a host of informational uncertainty following the onset of the COVID-19 pandemic; some favorable beliefs about e-cigarettes may have been curtailed. On one hand, early evidence suggests that e-cigarette users may be less vulnerable to COVID-19 pathogen,6–8 largely due to nicotine’s occupation of the angiotensin-converting enzyme responsible for binding coronavirus.9,10 However, during late 2019, the US CDC warned about lung injuries brought by e-cigarette additives.11 With the emergence of the COVID-19 pandemic, threats to pulmonary health rose given that the disease primarily impairs the respiratory system in patients with severe symptoms. Beyond concerns related to the known pulmonary vulnerabilities of tobacco use, the pandemic instigated concerns that e-cigarette users may be at a greater danger.9,12 Little is known about how e-cigarette users’ risk perceptions responded to the pandemic under such uncertainty. Thus, the COVID-19 pandemic as a natural event offers an opportunity to explore how health motives and behavior can align with risk perceptions potentially exacerbated by an external environmental stressor.
While motives for smoking and vaping have been examined within models that build upon the contemporaneous constituents of health beliefs, less is known about how an externally imposed event such as the introduction of a virus,13–15 may affect such motivations for consumption and, ultimately, health behaviors. While such events writ large may affect motivations, environmental threats directly linked to respiratory health, such as COVID-19, may alter motivations and subsequent behaviors.
Motivations for Using E-cigarettes
Motivations are multidimensional; individuals often possess a constellation of motives related to different aspects of life. The motives for vaping may vary across several domains of key concerns. Studies have shown that the most common motives for using e-cigarettes include perceived health benefits, smoking cessation, aesthetic preferences, social acceptability, and circumventing legal regulations such as smoking bans.4,5,16,17 For the use of an addictive substance such as nicotine, motivation also may arise outright from physiological dependence, adding a dependence motive for users.17,18 Absent the combustion of tars and other compounds in combustible tobacco, e-cigarettes are often perceived as less harmful, which stimulates motivations for e-cigarettes as a cessation tool or healthier alternative for smokers.13,19 In addition, the social learning perspective suggests that a major motivation for using substances, including nicotine products, relates to the substance’s facilitative role in occasions of recreation and socializing. Thus, some e-cigarette users have developed stronger social motives and formed communal solidarity with other e-cigarette users.5,16,20
Risk Perception and Motivations for Vaping
Several theories may elucidate how externally imposed threats (eg, COVID-19) may change motivations for using e-cigarettes, particularly motivations related to health promotion. Scientists have long recognized that external stimuli can potentially alter health motives as a part of ongoing interaction between actors and the environment. For instance, studies show that heavier air pollution elevates awareness for stricter tobacco control policy.21 Additionally, exposure to anti-smoking media promotes anti-smoking attitudes.22 Since motives for a health behavior come in multifaceted dimensions, the impact of risk factors in the environment on specific motives may also be heterogeneous, depending on the operative mechanism between the motive and the behavioral outcome. Several theories have elaborated on how risk perception may alter the motivations for health behaviors. As examples, we briefly consider aspects of the health belief model, protective motivation theory, and theories of health communication; all point to the susceptibility of motivations for e-cigarette use to change given perceived COVID-19 risk.
Health Belief Model
Motivations for vaping may be accommodated within the Health Belief Model, which suggests that people become motivated to change their behavior when they perceive an increased risk relative to its benefits.23 For tobacco control, the health belief model has stressed the critical role of raising people’s risk awareness when conducting behavioral interventions such as smoking cessation programs.
Studies have shown that existing beliefs about risks and benefits to substances may shift in response to the influences of peers, health education, implicit association, and role models, among a variety of signaled information or symbolic representations.24–27 Although many e-cigarette users believe e-cigarettes are less harmful than combustible tobacco, the emergence of severe lung injuries due to illicit vaping additives during late 2019 as well as e-cigarettes’ purported role in shaping severe cases of COVID-19 may impact certain motives for vaping in response to changes in these beliefs.
Protection Motivation Theory
Roger’s Protection Motivation Theory,28 revised from the earlier fear appraisal theory, aims to explain how externally imposed threats change health behaviors. The theory also proposes that the cognitive assessment of danger should affect health behavior via mediation by changing motivations for engaging in risk activities.
Protection Motivation Theory’s proposition may help explain how perceived COVID-19 risk may reduce motivations for using e-cigarettes. There is a strong association between risk perception and considerations to quit vaping29; the experience of smoking-related health problems directly affects smoking motivations with increases in the perceived threat of smoking.30,31 Longitudinal research also identified that protection motivation accounted for 35% of the variance in subsequent motivations for health behaviors.32 In this way, e-cigarette users may incorporate new negative information related to the pandemic as threats that exacerbate e-cigarette risks and accordingly shift their motivations for vaping.
Health Communication and Education
The rich literature in health communication elaborates on processes of communication about the severity of risk behaviors and the role of communication in educating people about risks, which in turn may reduce motivations.33 Carefully designed health communication can vastly heighten anti-smoking beliefs and in doing so suppress smoking motivations.22,34 Health information diffused via social media platforms, even infused with uncertainty, may considerably impact health beliefs and behavioral motivations.35 Regarding tobacco use, globally-coordinated health communication is responsible for increased awareness of tobacco harms, which reduced smokers’ motivations to smoke and encouraged cessation.34,36 However, countervailing efforts also occur as corporations utilize social media to instill favorable beliefs and positive motives for e-cigarette use.37,38
Current Study
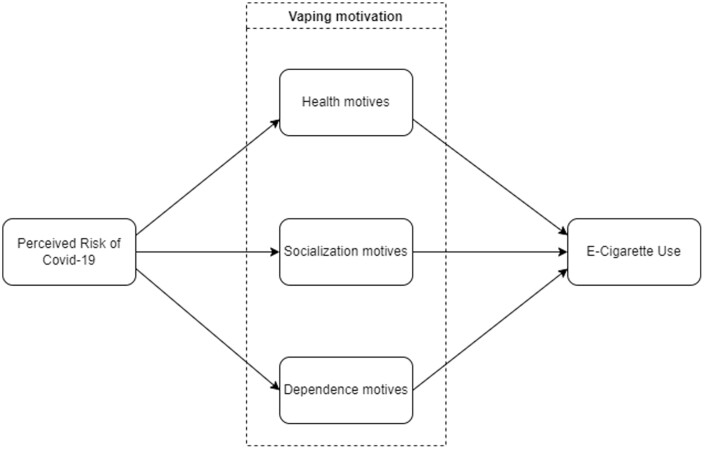
As shown in Figure 1, this study explores how e-cigarette users’ perceived vulnerability to an external threat (COVID-19) is associated with three different types of vaping motivations, which ultimately indirectly shape the intensity of e-cigarette use. Although we do not make a direct test of any of the theories described above, we draw upon components of them to consider how the changing risk environment may lead to shifts in motivations to consume e-cigarettes. We note that these considerations also cohere with Rhodes’ conceptualization of risk environments, wherein risk perception originates from and intersects with social and natural spaces.39 More specifically, we examine the mediating role of multiple motivations in the links between COVID-19 risk perceptions with e-cigarette users and the intensity of vaping. As depicted in Figure 1, motivations for vaping may become susceptible to new events that compel e-cigarette users to update their belief systems. While smoking and vaping were suspected of potentially worsening the pulmonary damages of COVID-19, we note that scientific evidence is ambiguous regarding e-cigarettes’ impact on COVID-19 prognosis.6,7,9
Figure 1.
Conceptual pathways of perceived risk of COVID-19, e-cigarette use, and motivation.
At this point, although some have examined how disruptions of the COVID-19 pandemic are associated with motivations for smoking and vaping, these studies have focused on the motivation to quit vaping,40,41 or general perceived risk,42,43 irrespective of the different types of motives that may not be equally present in each person. However, as people draw from different domains to produce information, motivation for a behavior is a complex psychological process that can rarely be reduced to a single dimension. We know little about how divergent motives for vaping—a sociopsychological construct—may shift as a function of COVID-19 risk perception and in turn how these motivations subsequently how e-cigarette users adapt their vaping behaviors. Building on components of theories of health beliefs, we examine the mediating role of motivations for e-cigarette use in the relationship between COVID risk perceptions and e-cigarette use intensity. Using structural equation modeling (SEM), we identified three types of vaping motivations (socialization, health, and dependence), then tested whether risk perceptions of COVID-19 were directly and indirectly (via motives for vaping) associated with intensity of vaping among e-cigarette users.
Methodology
Sample
The research team distributed a rapid assessment survey during April 2020 to a panel of US adults via the panel platform of Prolific Academic, yielding a final analytic sample of 562 e-cigarette users. Web-based panels are especially useful for rapid assessment of population groups and Prolific offers advantages over alternative online sources such as Amazon’s mTurk.44 Researchers can specify a battery of background characteristics to narrow down the target population. Research on causal inference has explicated why non-representative samples are merituous45 and we have summarized in the Supplementary Appendix why our study’s inference is not invalidated by the main issues of non-representativeness. The sampling frame initially targeted individuals indicating to Prolific they used e-cigarettes at least 20 times during their lifetime; inclusion criteria for the study is that subjects have used e-cigarettes during the past 30 days. This criterion allowed us to sample a broad spectrum of current users beyond daily users. Within the survey, e-cigarettes were defined for subjects as “any electronic nicotine delivery system that creates vaporized nicotine to inhale.” The Institutional Review Board approved the project prior to data collection. Table 1 displays detailed information about the sample; characteristics approximate those found for current e-cigarette users in nationally representative samples such as the Population Assessment of Tobacco & Health (PATH) study.
Table 1.
Demographic Descriptive Statistics (n = 562)
| Mean/% | SD/n | |
|---|---|---|
| Age | 35.43 | 13.44 |
| Education attainment | ||
| <HS Degree | 0.9% | 5 |
| HS Diploma | 14.8% | 83 |
| GED Recipient | 2.1% | 12 |
| Some College | 29.0% | 163 |
| Associates/2 year degree | 12.5% | 70 |
| Bachelors/4 year degree | 31.7% | 178 |
| Masters degree | 8.2% | 46 |
| Doctorate | 0.9% | 5 |
| Male gender | 57.7% | 324 |
| White race | 67.8% | 381 |
| Smoking tobacco | ||
| Current smoker | 38.3% | 215 |
| Former smoker | 41.8% | 235 |
| Never smoker | 19.9% | 112 |
| Income group | ||
| <$25k | 34.9% | 196 |
| $25k–$50k | 24.2% | 136 |
| $50k–$75k | 23.5% | 132 |
| $75k–$100k | 8.9% | 50 |
| Over $100k | 8.4% | 47 |
| Per day e-cigarette use | 20.54 | 32.52 |
| Past 30-day e-cigarette use | 19.20 | 11.29 |
| Risk for COVID-19 | 5.98 | 3.20 |
| Risk for severe COVID-19 problems | 5.42 | 3.22 |
HS = higher secondary.
Measurement
E-cigarette Use
We asked respondents to report vaping intensity in two forms46: the number of vaping days during the past 30 days, and average number of vaping instances per day of use.
COVID-19 Risk Perceptions
Participants responded to questions assessing their attitudes that e-cigarette use increases the risk and progression of COVID-19, which were rated on scales ranging from 0 (not at all) to 10 (Q1 definitely/Q2 extremely concerned). The two questions are: “Do you believe e-cigarette users are at greater risk from the coronavirus?” and “How much are you concerned you are at increased risk for serious problems if you caught the coronavirus.”
Motives to Use E-cigarettes
There are a variety of motivations for using e-cigarettes. E-cigarette users sometimes adopt e-cigarette use to avoid stigma from tobacco emitting second-hand smoke, the aesthetic values of e-cigarettes, or as a healthier alternative to tobacco.4,5,16 The variety of motives may be further categorized into different epistemological pursuits, with some emphasizing the functional values of vaping whereas others have more of a social identification with vaping.5,20 The survey deployed 15 items based upon issues identified within a literature review,16,19,20 covering a range of common motives for vaping. We conducted exploratory factor analysis and retained 13 items based on uniqueness and explained proportion of variance. Based on the results from exploratory factor analysis and prima facie conceptual validation, we categorized these items into three motivational types: health concerns, dependence on nicotine, and socialization purposes. Confirmatory factor analysis then validated the fitness of the three-factor configuration. The manifest indicators to measure these latent constructs are all listed in Table 2 along with their estimates.
Table 2.
Exploratory Factor Analysis for Motives of E-cigarette Use Under Three Latent Factors
| Manifest items | Mean (SD) | Latent factor loadings | ||
|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | ||
| 1. I would find it really hard to stop using e-cigarettes | 5.94 (3.31) | .71 | .21 | .15 |
| 2. After not using e-cigarettes for a while, I need to vape to be less irritable | 5.74 (3.33) | .93 | .16 | .16 |
| 3. After not using e-cigarettes for a while, I need to vape to be comfortable | 5.57 (3.36) | .90 | .12 | .18 |
| 4. E-cigarettes help me feel better if I’m feeling down | 6.27 (3.15) | .54 | <.10 | .47 |
| 5. Vaping helps me think better | 5.78 (3.22) | .54 | <.10 | .42 |
| 6. E-cigarettes might be less harmful to me than cigarettes | 8.41 (2.61) | .12 | .72 | <.10 |
| 7. E-cigarettes might be less harmful to others around me than cigarettes | 8.59 (2.51) | <.10 | .80 | .18 |
| 8. Using e-cigarettes helps people quit smoking cigarettes | 8.23 (3.03) | .12 | .53 | <.10 |
| 9. I can use e-cigarettes when smoking cigarettes is prohibited | 7.29 (3.27) | .14 | .18 | .28 |
| 10. E-cigarettes come in flavors I like | 8.26 (2.77) | <.10 | .27 | .47 |
| 11. E-cigarettes are more acceptable to non-smokers | 7.98 (2.66) | <.10 | .42 | .44 |
| 12. I like socializing when using an e-cigarette | 6.79 (3.18) | .12 | <.10 | .64 |
| 13. Advertising for e-cigarettes appeals to me | 4.23 (2.98) | .12 | <.10 | .61 |
| Proportional variance | .190 | .142 | .142 |
Bold font for the highest comparative loading of each manifest item.
Demographic characteristics, including gender, income, years of attained education, and race (coded as ”white” or “non-white”), were utilized as controls for background information. We also included covariates for tobacco use divided into three types: current smoker, former smoker, and never-smoker.
Statistical Analyses
This study focused upon identifying associations between COVID-19 perceived risk, motives for vaping, and intensity of e-cigarette use. Prior to these analyses, we employed factor analyses to establish the validity and reliability of measuring these constructs by a series of manifest items. Motives for vaping were categorized into three distinct types. Mediation analyses were employed to test which type(s) of motivation mediates the effect of risk concerns on intensity of e-cigarette use.
We employed SEM using R’s lavaan package47 for exploratory factor analysis, confirmatory factor analysis, and path analysis. For psychometric measurement involving both manifest items and latent constructs such as attitudes and beliefs, SEM offers the advantages of conducting both measurement reliability tests and regression techniques simultaneously and tests the data’s fitness to the configured conceptual model. Thus, SEM improves over single-equation regressions when a construct is measured by multidimensional items.48 For meditation analysis, SEM also tests multiple dependent variables and provides a comprehensive comparison of direct effects, indirect effects, and total effects. The model obtains estimates of indirect, direct, total effects, and their ratios by using bootstrap resampling. We allow covariance between the residuals of latent constructs of motivation based on the study design, which theoretically had assumed that different subtypes of motivation belong in the same spectrum.49 We adopted four commonly used goodness-of-fit indices to evaluate the model’s fit50,51: The Tucker-Lewis Index (TLI) above 0.9 suggests a good fit; the goodness of fit index close to 1 indicates very good fit; the root mean square error of approximation (RMSEA) below 0.05 indicates good fit, and 0.08 acceptable fit.52
Results
Table 1 provides descriptive statistics of key sample characteristics. As displayed, average age was 35.4 years (SD = 13.4), and the sample was comprised of 57.7% males, 67.8% whites, 40.8% having earned at least a Bachelor’s degree, and 40.8% earning over $50 000 US dollars. The sample includes a number of current (38.3%) and former (41.8%) smokers of tobacco cigarettes, only 19.9% have never smoked. The population inferred from this sample has a higher educational level than the US average, but other differences are not pronounced. Mean daily vaping occasions is 20.5 (SD = 32.5), and the average days of vaping in the last month are 19.2 days (SD = 11.3). Out of 10 points, perceived risk for e-cigarette users to contract COVID-19 is 5.98 (SD = 3.2) and perceived risk for e-cigarette users to develop severe COVID-19 problems is 5.42 (SD = 3.2).
Exploratory factor analysis with a tri-factors configuration shows the correlational magnitude between manifest items and latent factors in Table 2. We determined the proper allocation of each manifest item to a latent factor by the magnitude of the correlation between the manifest item and all three latent factors. We also considered the semantic face validity of whether the manifest items grouped together share a common understandable theme. Here the exploratory factor analysis grouped the first five items together, which we later labeled “dependence motives”. These five items registered relatively low means in comparison to other items. The items for dependence motives have means from 5.57 to 6.27, whereas items in the other two latent constructs typically range around 0.7 or 0.8. Items 6, 7, and 8 were grouped together under Factor 2, indicating need to improve health by using e-cigarettes, named “health motives”. The last five items were grouped for commonality in non-physical benefits of using e-cigarettes, named “socialization motives”. Factor 3 highlights the motivation of e-cigarette users’ social and aesthetic reasons.
Table 3 shows two types of information related to confirmatory factor analysis of the latent constructs. The right side of the table indicates to what degree the manifest items significantly load onto their respective latent constructs. For the purposes of identification, we have set to 1 the item with the strongest loading for each latent construct as a reference. The squared factor loadings in the right show the explained proportion of the variance of a manifested item by the latent construct. All manifested measures significantly loaded on the latent construct with a coefficient of at least.50. Combined with the goodness of fit indices presented at the bottom of Table 2 (comparative fit index [CFI] > .90, TLI > .90, RMSEA < .08, standardized root mean square residual [SRMR] < .08), we conclude that our theoretical constructs, including identifying all motives into the three subtypes, are also reliable and internally valid.
Table 3.
Confirmatory Factor Analysis Results by Correlation Matrix and Measurement Estimates
| Correlation between latent factors | Loadings of manifest indicators | |||||||
|---|---|---|---|---|---|---|---|---|
| Socialization | Health | Dependence | Use | COVID Risk | Latent constructs | Manifest indicators | Estimates (SE) | Squared loading |
| 1 | COVID risk | Do you believe e-cigarette users are at greater risk from the coronavirus? | .98(.30)*** | .69 | ||||
| How much are you concerned you are at increased risk for serious problems if you caught the coronavirus | 1 | .72 | ||||||
| 1 | −.27** | E-cigarette use | Average number of vaping per day | 1 | .21 | |||
| Days of past month e-cigarette use | .56(.08)*** | .55 | ||||||
| 1 | .53*** | .12* | Dependence motives | I would find it really hard to stop using e-cigarettes #1 | .79(.03)*** | .57 | ||
| After not using e-cigarettes for a while, I need to vape to be less irritable #2 | 1 | .91 | ||||||
| After not using e-cigarettes for a while, I need to vape to be comfortable #3 | .99(.02)*** | .85 | ||||||
| E-cigarettes help me feel better if I’m feeling down #4 | .56(.04)*** | .31 | ||||||
| Vaping helps me think better #5 | .55(.05)*** | .26 | ||||||
| 1 | .33*** | .55*** | −.26*** | Health motives | E-cigarettes might be less harmful to me than cigarettes #1 | 1 | .62 | |
| E-cigarettes might be less harmful to others around me than cigarettes #2 | .96(.07)*** | .54 | ||||||
| Using e-cigarettes helps people quit smoking cigarettes #3 | .85(.09)*** | .33 | ||||||
| 1 | .36*** | .38*** | −.05 | .04 | Socialization motives | I can use e-cigarettes when smoking cigarettes is prohibited #1 | .59(.08)*** | .16 |
| E-cigarettes come in flavors I like #2 | .62(.07)*** | .25 | ||||||
| E-cigarettes are more acceptable to non-smokers #3 | .66(.09)*** | .25 | ||||||
| I like socializing when using an e-cigarette #4 | 1 | .52 | ||||||
| Advertising for e-cigarettes appeals to me #5 | .80(.07)*** | .39 | ||||||
N = 560, degree of freedom = 136. = 3927.1, CFI = .93, TLI = .91, RMSEA = .07, SRMR = .07. Constraints (~~: covariance): feel_better~~think_better, harm_others~~acceptable.
CFI = comparative fit index; RMSEA = root mean square error of approximation; TLI = Tucker-Lewis Index.
*p < .05.
** p < .01.
*** p < .001.
The left panel of Table 3 displays a correlation matrix for all latent constructs. The shaded diagonal line contains full correlations of 1, when a latent construct in the row corresponds to itself in the column. The construct of socialization motives significantly correlates with health motives (.36, p < .001) and dependence motives (.38, p < .001), but its correlations with perceived COVID-19 risk and e-cigarette use are not significant.
In Table 4, we present the stepwise strategies resulting in our final SEM configuration. The first model is a raw path analysis without modification or control variables. This first model (M1) represents the basic conceptual pathways in Figure 1. However, goodness of fit of the first model is not entirely satisfactory, with indices below conventional thresholds for model fit (CFI < .90, TLI < .90, RMSEA > .08, SRMR > .08). As explained in the methods section, there is likely an unmeasured source of correlation between the three types of vaping motives since these subtypes, theoretically, form a common underlying spectrum. Therefore, M2 allowed the residuals of the latent constructs of motivation to freely co-vary. M2 improves goodness of fit. As suggested by modification indices, we freed two pairs of manifest items within the same latent construct to retain substantive meaning. The modeled structure of M3 is considered a good fit with the data by all four indices (CFI > .09, TLI > .09, RMSEA < .08, SRMR < .07). Finally, M4 incorporated all covariates: smoking status, gender, race, age, income, and educational level. The fit remain on par with M2, which is normal when the model starts to include background variables of heterogenous information. Two of the fitness indices remained satisfactory in M4 (RMSEA < .08, SRMR < .08). Nevertheless, M3 indicates that our model’s main constructs are a reasonable fit to the actual data, whereas M4 shows that controlling a host of background information does not invalidate the preceding model.
Table 4.
Hierarchically Nested Model Comparison
| N | Degree of Freedom | CFI | TLI | RMSEA | SRMR | BIC | ||
|---|---|---|---|---|---|---|---|---|
| M1 | 560 | 112 | 796.2 | .82 | .78 | .10 | .14 | 49431 |
| M2 | 560 | 109 | 651.2 | .86 | .82 | .09 | .08 | 49305 |
| Covariance in latent resid. | ||||||||
| M3 | 560 | 107 | 387.3 | .93 | .91 | .07 | .07 | 49054 |
| Covariance in latent resid. Covariance in manifested resid. | ||||||||
| M4 | 559 | 212 | 844.6 | .85 | .82 | .07 | .08 | 48962 |
| Covariance in latent resid. Covariance in manifested resid. Control variables (gender, race, age, income, education, smoking status) |
Constraints on the residuals of latent measures (~~: covariance): social~~health, social~~dependence, health~~dependence. Covariance between residuals of manifested items: feel_better~~ think_better, harm_others~~acceptable.
BIC = Bayesian information criteria; CFI = comparative fit index; RMSEA = root mean square error of approximation; TLI = Tucker-Lewis Index.
*p < .05.
** p < .01.
*** p < .001.
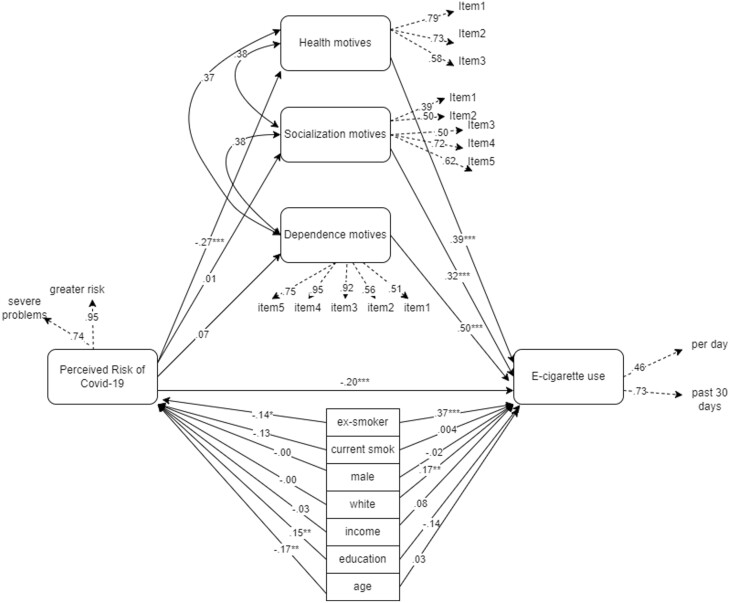
The SEM configuration of M4 and its standardized coefficients were presented in Figure 2. Correlations between the residuals of three motivation types were approximately equal in strength (.38, p < .001; .37, p < .001; .38, p < .001). All three motivation types were associated with more intensive use of e-cigarettes. By order of coefficient magnitude, dependence motives are most strongly associated with e-cigarette use intensity (.50, p < .001), followed by health motives (.39, p < .001) and socialization motives (.32, p < .001). Substantively these estimates indicate that for every SD increase in motivation, the intensity of e-cigarette use would change by 0.50, 0.39, and 0.32 SDs, respectively. Perceived risk of COVID-19 is significantly associated with health motives (−.27, p < .001), but not socialization motives or dependence motives. Perceived COVID-19 risk itself is negatively associated with e-cigarette use (−.20, p < .01), meaning that e-cigarette users with greater concerns for personally contracting COVID-19 use e-cigarettes at reduced intensity. Among covariates, education is positively associated with greater perceived risk of COVID-19 (.15, p < .01), older age is negatively associated with the perceived risk of COVID-19 (−.17, p < .001), and identifying as White is positively associated with more intensive use (.17, p < .01). For a SD increment in education and age, the perceived risk of COVID-19 would change by 0.15 and −0.17 SDs. The intensity of e-cigarette use would increase by 0.17 SD if the e-cigarette user is white, compared to other races. Compared to never-smokers, ex-smokers show reduced risk perception of COVID-19 (−.14, p < .05) and increased intensity of e-cigarette use (.37, p < .001), but current smokers show no difference in these outcomes.
Figure 2.
Structural equation modeling results.
Informed by the results in Figure 2, we used bootstrap resampling for tests of indirect effects. Table 5 confirms the preliminary findings from Figure 2 that health motives constitute a mediator between perceived COVID-19 risk and e-cigarette use intensity. There is a significant direct effect between perceived COVID-19 risk and e-cigarette use (−.94, p < .05), as well as a significant indirect effect via the mediating role of health motives (−.50, p < .01). The indirect to total effect ratio is .35 (p < .01), indicating that 35% of the association between perceived COVID-19 risk and e-cigarette use was mediated by health motives. This finding implies that a portion of the effect of risk beliefs about COVID-19 threats to e-cigarette users on vaping behaviors is due to how such risk beliefs alter health motivations. However, we find no evidence the other two types of motives have a mediating role.
Table 5.
Direct and Indirect Effects (Unstandardized Coefficients)
| Pathways | Effect estimates | Indirect/direct effect ratio | Indirect/total effect ratio |
|---|---|---|---|
| Covid risk → e-cigarette use | −.94 (.42)* | ||
| Covid risk → health motives →e-cigarette use | −.50 (.18)** | .53 (.62) | .35 (.13)** |
| Covid risk → dependence motives →e-cigarette use | .28 (.24) | -.30 (.91) | -.43 (.47) |
| Covid risk → socialization motives →e-cigarette use | -.07 (.17) | .07 (1.29) | .07 (.24) |
*p < .05.
** p < .01.
*** p < .001.
Discussion
To date, prevailing health psychology models of health beliefs have focused more on endogenous psychological attributes than environmental factors’ involvement in the production and maintenance of such motivations. This study investigated how health motives are related to a disruptive event—the COVID-19 pandemic. More specifically, we explored whether motivations for vaping e-cigarettes were associated with perceived risk of COVID-19, and whether such motivations mediate the relationship between COVID-19 risk beliefs and the intensity of e-cigarette use.
Motivation is a significant psychological predictor of actual vaping behavior. Motivation for specific conduct involves gathering supportive evidence from multiple domains, thus constituting a multidimensional psychological process that requires typological analysis. We classified vaping motivation into three types: health, socialization, and dependence. This study found that all three types of motivations for using e-cigarettes are significantly associated with the intensity of e-cigarette use. The standardized coefficients of all three dimensions of vaping motives were in similar magnitude ranging from .40 to .54 (p < .001). When the perceived risk increases, motivation to engage in a risk behavior declines and people adapt to the new belief system by cessation (eg, quit vaping) or, as in the case of self-exempting beliefs, they may innovate their knowledge and replace beliefs.26,27 As viral epidemics and negative information about lung injuries emerge, e-cigarette users may incorporate these external threats into their beliefs and accordingly shift their motivations for vaping.
We argued the perceived risk has a different impact on each of the vaping motivation. While some prior studies have divided and categorized vaping motivation into subtypes, few have studied how specific dimensions of vaping motivations differentially vary with other risk factors. We found that COVID-19 risk perception is only associated with health motives (−.27, p < .001), after accounting for the correlation between different motive subtypes. This result suggests diversity in the composition of vaping motivations. As a strategy of stigma management and social resistance, some have adopted e-cigarettes as a performative tool and to foster community without inviting the suspicion of non-smokers.20 In this way, a viral pandemic with disease implications does not render much opportunity for health intervention work on socialization motivations. Instead, by working on health motives, health education and communication efforts promoting risk awareness may prove effective. For example, a study found that, given their relatively younger age, e-cigarette users preferred health communication messages relying on scientific evidence and individual agency.53 Thus, spreading evidence-based medical research on the harms of vaping not only avoids marginalizing e-cigarette users, it may more effectively reduce health motives for some e-cigarette users.
Further, the findings also indicate ex-smokers, compared to never-smokers, vaped e-cigarettes more intensely and held less risk perceptions of COVID-19. Classifying e-cigarette users into three categories in terms of their tobacco use, we may consider ex-smokers those who completely transitioned from tobacco cigarettes to e-cigarettes. Compared to both current smokers and never-smokers, these e-cigarette users show greater preference for e-cigarettes. Thus, while e-cigarettes may be important smoking cessation tools for these individuals, ex-smokers should receive greater attention from health intervention experts. Health policies may leverage this study’s finding to conduct more targeted intervention. Because the health motives of vaping were most often cited as a reason to quit smoking,54,55 perceived environmental risks that weaken the utility of health motives of e-cigarettes may unintentionally prompt a reverse back to smoking tobacco. Tobacco control efforts must consider the COVID-19 pandemic as an environmental trigger and carefully tailor health communication to demonstrate the harms of tobacco cigarettes, while encouraging reduced use of e-cigarettes. For former smokers who switched to e-cigarettes, further harm reduction can be achieved by demystifying the health motives they rely on to continue vaping.
Limitations
Although these results provide early information on e-cigarette use and motivations in light of COVID-19, we note some limitations. First, although this rapid assessment survey reached a national sample of e-cigarette users, it is not a probability-based sample. While the data cannot be fully generalized, such data collection techniques provide opportunities to assess relationships between variables among substance-using populations.56 Further, the data cohere well with demographic characteristics of e-cigarette users in probability-based samples such as the PATH dataset. Second, as the data are cross-sectional, we cannot fully infer causality. While this study provides important information related to this sudden event, the cross-sectional nature of the study design cautions against interpretations that insinuate a causal mechanism behind perceived risk and e-cigarette use. Lastly, common with surveys, subjects self-reported their experiences and social desirability or recall biases may shape these reports. However, computer-assisted surveys reduce such biases in the self-report of sensitive topics.57
Conclusions
Perceptions of risk related to the pandemic have had a direct and indirect effect on vaping behaviors among e-cigarette users. E-cigarette users who have high risk perceptions related to the pandemic reported lower intensity of vaping within the past month. Health motivations for vaping appear to be a key mediating pathway by which motivations shape the relationship between risk perceptions and e-cigarette use. Opportunities to intervene on e-cigarette use during the pandemic may be particularly persuasive for e-cigarette users who have chosen vaping as a healthier alternative to smoking.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Contributor Information
Xiaozhao Yousef Yang, School of Sociology and Anthropology, Sun Yat-sen University, Guangzhou, Guangdong, China.
Brian C Kelly, Department of Sociology, Purdue University, West Lafayette, IN, USA.
Mark Pawson, Department of Sociology, Purdue University, West Lafayette, IN, USA.
Michael Vuolo, Department of Sociology, The Ohio State University, Columbus, OH, USA.
Funding
No funds received for the study.
Declaration of Interests
The authors are not aware of any conflict of interests with any affiliations, membership, or financial holdings that may affect the objectivity of this study. This study is in no part associated with any entities engaged in the production, cultivation, and sale of tobacco and tobacco-derived products. The study is conducted in full compliance with the 1964 Declaration of Helsinki and its amendments as the criteria of ethical conduct.
Data Availability
The collection of the data has not been funded by tax revenue, the data are proprietary and are not available for public use.
References
- 1. WHO. WHO Global Report on Trends in Prevalence of Tobacco Smoking 2000-2025. (9241514175). Geneva, Switzerland: World Health Organization; 2021. https://www.who.int/publications/i/item/9789240039322. Accessed February 25, 2022. [Google Scholar]
- 2. Kadowaki J, Vuolo M, Kelly BC. A review of the current geographic distribution of and debate surrounding electronic cigarette clean air regulations in the United States. Health Place. 2015;31:75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mons U, Nagelhout GE, Allwright S, et al. Impact of national smoke-free legislation on home smoking bans: findings from the International Tobacco Control Policy Evaluation Project Europe Surveys. Tob Control. 2013;22(e1):e2–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Thirlway F. Nicotine addiction as a moral problem: barriers to e-cigarette use for smoking cessation in two working-class areas in Northern England. Soc Sci Med. 2019;238:112498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pokhrel P, Herzog TA, Muranaka N, Fagan P. Young adult e-cigarette users’ reasons for liking and not liking e-cigarettes: a qualitative study. Psychol Health. 2015;30(12):1450–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cai H. Sex difference and smoking predisposition in patients with COVID-19. . The Lancet Res Med. 2020;8(4):e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meini S, Fortini A, Andreini R, Sechi LA, Tascini C. The paradox of the low prevalence of current smokers among COVID-19 patients hospitalized in non-intensive care wards: results from an Italian Multicenter Case-Control Study. Nicotine Tob Res. 2021;23(8):1436.– 1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Miyara M, Tubach F, Pourcher V, et al. Low rate of daily active tobacco smoking in patients with symptomatic COVID-19. Qeios. 2020;9. https://www.qeios.com/read/WPP19W.4. [Google Scholar]
- 9. Cattaruzza MS, Zagà V, Gallus S, D’Argenio P, Gorini G. Tobacco smoking and COVID-19 pandemic: old and new issues. A summary of the evidence from the scientific literature. Acta Biomed. 2020;91(2):106–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tindle HA, Newhouse PA, Freiberg MS. Beyond smoking cessation: investigating medicinal nicotine to prevent and treat COVID-19. Nicotine Tob Res. 2020;22(9):1669–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Krishnasamy VP, Hallowell BD, Ko JY, et al. Update: characteristics of a nationwide outbreak of e-cigarette, or vaping, product use–associated lung injury — United States, August 2019–January 2020. MMWR Morb Mortal Wkly Rep. 2020;69:90–94. doi:10.15585/mmwr.mm6903e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. The Lancet Editorial. The EVALI outbreak and vaping in the COVID-19 era. The Lancet Res Med. 2020;8(9):831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pepper JK, Emery SL, Ribisl KM, Rini CM, Brewer NT. How risky is it to use e-cigarettes? Smokers’ beliefs about their health risks from using novel and traditional tobacco products. J Behav Med. 2015;38(2):318–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mohammadi S, Ghajari H, Valizade R, et al. Predictors of smoking among the secondary high school boy students based on the health belief model. Int J Prev Med. 2017;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mantler T. A systematic review of smoking Youths’ perceptions of addiction and health risks associated with smoking: utilizing the framework of the health belief model. Addiction Res Theory. 2013;21(4):306–317. [Google Scholar]
- 16. Cooper M, Harrell MB, Perry CL. Comparing young adults to older adults in e-cigarette perceptions and motivations for use: implications for health communication. Health Educ Res. 2016;31(4):429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Morean ME, Wedel AV. Vaping to lose weight: predictors of adult e-cigarette use for weight loss or control. Addict behav. 2017;66:55–59. [DOI] [PubMed] [Google Scholar]
- 18. Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70(6):1224–1239. [DOI] [PubMed] [Google Scholar]
- 19. Farrimond H. A typology of vaping: identifying differing beliefs, motivations for use, identity and political interest amongst e-cigarette users. Int J of Drug Policy. 2017;48:81–90. [DOI] [PubMed] [Google Scholar]
- 20. Tokle R, Pedersen W. “Cloud chasers” and “substitutes”: e-cigarettes, vaping subcultures and vaper identities. Sociol Health Illn. 2019;41(5):917–932. [DOI] [PubMed] [Google Scholar]
- 21. Yang XY, Yang T, Nie F. Air pollution as a catalyst for supporting tobacco control policies? Evidence from a nationwide study on Chinese medical students. Tob Control. 2018;27(5):505–512. [DOI] [PubMed] [Google Scholar]
- 22. Niederdeppe J, Kellogg M, Skurka C, Avery RJ. Market-level exposure to state antismoking media campaigns and public support for tobacco control policy in the United States, 2001–2002. Tob Control. 2018;27:177–184. [DOI] [PubMed] [Google Scholar]
- 23. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–335. [DOI] [PubMed] [Google Scholar]
- 24. Gottlieb NH, Baker JA. The relative influence of health beliefs, parental and peer behaviors and exercise program participation on smoking, alcohol use and physical activity. Soc Sci Med. 1986;22(9):915–927. [DOI] [PubMed] [Google Scholar]
- 25. Kelly BC, Liu T, Zhang G, Hao W, Wang J. Perceptions of HIV risk among methamphetamine users in China. Am J Drug Alcohol Abuse. 2013;39(2):99–102. [DOI] [PubMed] [Google Scholar]
- 26. Radtke T, Scholz U, Keller R, Hornung R. Smoking is ok as long as I eat healthily: compensatory health beliefs and their role for intentions and smoking within the Health Action Process Approach. Psychol Health 2011;27(sup2):91–107. [DOI] [PubMed] [Google Scholar]
- 27. Yang XY, Kelly BC, Yang T. The influence of self-exempting beliefs and social networks on daily smoking: a mediation relationship explored. Psychol Addict Behav. 2014;28(3):921–927. [DOI] [PubMed] [Google Scholar]
- 28. Rogers RW. A protection motivation theory of fear appeals and attitude change1. J Psychology. 1975;91(1):93–114. [DOI] [PubMed] [Google Scholar]
- 29. Kelly BC, Pawson M, Vuolo M. Beliefs on COVID-19 among electronic cigarette users: behavioral responses and implications for COVID prevention and e-cigarette interventions. J Drug Issues. 2021;0(0):0022042620977828. [Google Scholar]
- 30. McBride CM, Pollak KI, Garst J, et al. Distress and motivation for smoking cessation among lung cancer patients’ relatives who smoke. J Cancer Educ. 2003;18(3):150–156. [DOI] [PubMed] [Google Scholar]
- 31. Ostroff JS, Buckshee N, Mancuso CA, Yankelevitz DF, Henschke CI. Smoking cessation following CT screening for early detection of lung cancer. Prev Med. 2001;33(6):613–621. [DOI] [PubMed] [Google Scholar]
- 32. Plotnikoff RC, Rhodes RE, Trinh L. Protection motivation theory and physical activity: a longitudinal test among a representative population sample of Canadian adults. J Health Psychol. 2009;14(8):1119–1134. [DOI] [PubMed] [Google Scholar]
- 33. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259–267. [Google Scholar]
- 34. Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20(5):327–337. [DOI] [PubMed] [Google Scholar]
- 35. Abroms LC, Maibach EW. The effectiveness of mass communication to change public behavior. Annu Rev Public Health. 2008;29(1):219–234. [DOI] [PubMed] [Google Scholar]
- 36. Willemsen MC, de Zwart WM. The effectiveness of policy and health education strategies for reducing adolescent smoking: a review of the evidence. J Adolesc. 1999;22(5):587–599. [DOI] [PubMed] [Google Scholar]
- 37. Collins L, Glasser AM, Abudayyeh H, Pearson JL, Villanti AC. E-Cigarette marketing and communication: how e-cigarette companies market e-cigarettes and the public engages with e-cigarette information. Nicotine Tob Res. 2018;21(1):14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Emery SL, Vera L, Huang J, Szczypka G. Wanna know about vaping? Patterns of message exposure, seeking and sharing information about e-cigarettes across media platforms. Tob Control. 2014;23(suppl 3):iii17–iii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rhodes T. The “risk environment”: a framework for understanding and reducing drug-related harm. Int J Drug Policy. 2002;13(2):85–94. [Google Scholar]
- 40. Brown CRH. The relationship between COVID-19-specific health risk beliefs and the motivation to quit smoking: a UK-based survey. Drug Alcohol Depend. 2021;227:108981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Klemperer EM, West JC, Peasley-Miklus C, Villanti AC. Change in tobacco and electronic cigarette use and motivation to quit in response to COVID-19. Nicotine Tob Res. 2020;22(9):1662–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. White AM, Li D, Snell LM, et al. Perceptions of tobacco product-specific COVID-19 risk and changes in tobacco use behaviors among smokers, e-cigarette users, and dual users. Nicotine Tob Res. 2021;23(9):1617–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gravely S, Craig LV, Cummings KM, et al. Smokers’ cognitive and behavioural reactions during the early phase of the COVID-19 pandemic: findings from the 2020 ITC Four Country Smoking and Vaping Survey. PLoS One. 2021;16(6):e0252427e0252427-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Palan S, Schitter C. Prolific.ac—A subject pool for online experiments. J Behav Experimental Finance. 2018;17:22–27. [Google Scholar]
- 45. Richiardi L, Pizzi C, Pearce N. Commentary: Representativeness is usually not necessary and often should be avoided. Int J Epidemiol. 2013;42(4):1018–1022. [DOI] [PubMed] [Google Scholar]
- 46. Yingst J, Foulds J, Veldheer S, et al. Measurement of electronic cigarette frequency of use among smokers participating in a randomized controlled trial. Nicotine Tob Res. 2020;22(5):699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Software. 2012;48(2):1–36. [Google Scholar]
- 48. Bollen KA, Pearl J. Eight myths about causality and structural equation models. In: S.L. Morgan, ed. Handbook of Causal Analysis for Social Research. Dordrecht: Springer Netherlands; 2013: 301–328. [Google Scholar]
- 49. Cole DA, Ciesla JA, Steiger JH. The insidious effects of failing to include design-driven correlated residuals in latent-variable covariance structure analysis. Psychol Methods. 2007;12(4):381–398. [DOI] [PubMed] [Google Scholar]
- 50. Arbuckle JL. IBM SPSS® Amos™ 20 User’s Guide. Chicago, IL: IBM SPSS Inc; 2011. [Google Scholar]
- 51. Kline RB. Principles and Practice of Structural Equation Modeling. New York, NY: Guilford; 2005. [Google Scholar]
- 52. Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods Res. 1992;21(2):230–258. [Google Scholar]
- 53. Escoto A, Watkins SL, Welter T, Beecher S. Developing a targeted e-cigarette health communication campaign for college students. Addict Behav. 2021;117:106841. [DOI] [PubMed] [Google Scholar]
- 54. Hartmann-Boyce J, McRobbie H, Lindson N, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2020(10). Art. no.: CD010216. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8094228/pdf/CD010216.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wang RJ, Bhadriraju S, Glantz SA. E-Cigarette use and adult cigarette smoking cessation: a meta-analysis. Am J Public Health. 2021;111(2):230–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Barratt MJ, Ferris JA, Zahnow R, et al. Moving on from representativeness: testing the utility of the Global Drug Survey. Subst Abuse: Res Treat. 2017;11:1178221817716391178221817716391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Williams ML, Freeman RC, Bowen AM, et al. A comparison of the reliability of self-reported drug use and sexual behaviors using computer-assisted versus face-to-face interviewing. AIDS Educ Prevention. 2000;12(3):199–213. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The collection of the data has not been funded by tax revenue, the data are proprietary and are not available for public use.