Summary
Background
The evidence regarding the efficacy of vitamin D supplementation in reducing severity of COVID-19 is still insufficient. This is partially due to the lack of primary robust trial-based data and heterogeneous study designs.
Aim
This evidence summary, aims to study the effect of vitamin D supplementation on morbidity and mortality in hospitalized COVID-19 patients.
Design: Evidence summary of systematic reviews
Methods
For this study, systematic reviews and meta-analysis published from December 2019 to January 2022 presenting the impact of vitamin D supplementation on COVID-19 severity were screened and selected from PubMed and Google scholar. After initial screening, 10 eligible reviews were identified and quality of included reviews were assessed using AMSTAR and GRADE tools and overlapping among the primary studies used were also assessed.
Results
The number of primary studies included in the systematic reviews ranged from 3 to 13. Meta-analysis of seven systematic reviews showed strong evidence that vitamin D supplementation reduces the risk of mortality (Odds ratio: 0.48, 95% CI: 0.346–0.664; P < 0.001) in COVID patients. It was also observed that supplementation reduces the need for intensive care (Odds ratio: 0.35; 95%CI: 0.28–0.44; P < 0.001) and mechanical ventilation (Odds ratio: 0.54; 95% CI: 0.411–0.708; P < 0.001) requirement. The findings were robust and reliable as level of heterogeneity was considerably low. However the included studies were of varied quality. Qualitative analysis showed that supplements (oral and IV) are well tolerated, safe and effective in COVID patients.
Conclusion
The findings of this study show that vitamin D supplementation is effective in reducing the COVID-19 severity. Hence, vitamin D should be recommended as an adjuvant therapy for COVID-19. However, more robust and larger trials are required to substantiate it further.
Introduction
With the new variant OMICRON, the world is again witnessing a huge surge in COVID-19 cases. It is observed that the viral genome has undergone significant changes this time, resulting in a multiple fold increase in infectivity and strengthened immune invasion. Many countries reported a sharp spike in the cases, almost doubling in just over a day.1 With vaccine inequity and hesitancy, experts are already predicting that there might be emergence of new variants. So, it is need of the hour to envisage effective economic treatment strategies, as developing new vaccines for every variant cannot be economically viable or technically feasible solution.
In the midst of the unregulated usage of multiple costlier and mildly effective drug molecules, vitamin D remains an understudied and underused treatment strategy for COVID-19. Vitamin D is an immune modulator known to protect from acute respiratory tract infections.2 The protective effect of vitamin D is exerted through multiple mechanisms such as modulation of ACE-2 receptor activity, triggering of innate and adaptive immune responses and reducing the levels of cytokines. SARS-CoV-2 is known to initiate a cascade of inflammatory reactions where acute phase biomarkers levels are elevated. This leads to COVID-19 acute respiratory distress syndrome (ARDS).3 So similar to other respiratory tract diseases, studies have also explored the potential role of vitamin D supplementation on reducing COVID-19 associated morbidity and mortality. Few randomized controlled trials (RCTs) have shown that, with various doses and forms of vitamin D, risk of hospitalization, need for mechanical ventilation and intensive care unit (ICU) admission can be reduced significantly.4–7 Similarly, the rate of morbidity and mortality was considerably high in COVID positive patients having vitamin D deficiency as compared to patients with normal levels of vitamin D.8–11 However, RCTs showing improvement in the mortality rate with vitamin D supplementation remains non-significant, majorly due to smaller sample size and lower incidence of mortality in the study participants.12 In contrast, there was another study that documented a positive impact on mortality with vitamin D supplementation.13
Despite these promising initial outcomes, integration of vitamin D in preventive or treatment guidelines for COVID-19 has not been recommended by any government agencies or WHO. This could be possibly due to (i) lack of evidence from RCTs with larger sample size, (ii) Heterogeneity with respect to design, drug dosage and population characteristics that have been observed in reported studies, (iii) difference of opinion among clinicians regarding its effectiveness and (iv) lack of clarity about the influence of various confounders such as ethnicity, race, age, gender and comorbidity on vitamin D effectiveness. This points to the fact that a uniform methodology is required in order to reach a final conclusion on vitamin D utility.
Hence, this current evidence summary is designed to generate evidence toward the potential use of vitamin D supplementation in reducing mortality, ICU admissions and the reduction in use of ventilation in hospitalized COVID-19 patients.
Methods
The current review was conducted in accordance with the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).
Inclusion and exclusion criteria
We included systematic reviews that studied the effect of vitamin D supplementation on three outcomes—ventilation, ICU admissions and mortality. Articles published in languages other than English were excluded from the review. Reports that studied the effect vitamin D deficient or replete individuals, on COVID-19 associated mortality and length of hospital stay were excluded.
Search strategy
Articles from December 2020 to January 2022 were screened for the review by two independent reviewers (US and VP) using the following MeSH terms: COVID-19, Coronavirus disease, SARS-CoV2, Coronavirus, Vitamin D supplementation, Vit D, vitamin D supplements, mortality, death, ICU admission, ICU stay, ventilation, mechanical ventilation, COVID-19 outcomes. These search terms were connected using boolean operators (AND, OR, NOT). Additionally, reference tracking of the searched articles was carried out to identify other relevant articles that were missed during the initial search. We excluded duplicate studies from the final search.
Data extraction
The full text of the selected articles was analyzed by three independent reviewers. Qualitative and quantitative data from each study were extracted into an excel sheet. Details of authors, publication dates and country, number of included studies, sample size, vitamin D supplementation and its impact on ICU admissions, ventilation requirement and mortality in COVID patients were extracted from the selected systematic reviews. Quantitative information was used to conduct a meta-analysis and qualitative information regarding key findings, strengths and limitations of the studies were noted from each review. Disagreements regarding any of the information to be extracted were resolved by discussion and mutual agreement.
Quality assessment
All the included systematic reviews were assessed for risk of bias using AMSTAR (A Measurement Tool to Assess Systematic Reviews to assess the methodological quality of review and meta-analysis) tool. Based on the assessed risk of bias the articles were grouped into high, moderate, low and critically low-quality studies. The quality of included reviews was assessed using GRADE (Grading of Recommendations Assessment, Development, and Evaluation) classification.
Data synthesis
Data from each selected systematic review were abstracted into evidence tables and a meta-analysis was performed for seven studies using quantitative data provided by individual studies. Heterogeneity of between-study variance was assessed using Cochrane’s Q test (P < 0.10) and quantified using the I2 statistics. I2 > 50% and a P < 0.05 were considered substantial heterogeneity. Heterogeneity in the results was analyzed using Q statistics (significant at P < 0.10). I2—a quantitative measure of heterogeneity was used to categorize studies into various levels of heterogeneity (high: 75–100%, medium: 50–70%, and low: 0–50%). In case of I2 more than 50%, a random-effect model was considered to measure the impact of an intervention, whereas fixed effect model was applied for the cases having I2 less than 50%. All statistics were performed using Medcalc version 20.026. Publication bias was assessed using Begg’s test and Egger’s test. The presence or absence of a statistically significant bias was concluded from the quantitative results of Egger’s and Begg and Mazumdar rank correlation test, whereas visual inspection of bias was undertaken using a Funnel plot.
Results
Systematic reviews and meta-analysis published from the beginning of pandemic till January 2022 were screened for this study. The reviews comparing effect of vitamin D supplementation on mortality rates, ICU admission and ventilation requirement among COVID positive cases as compared to placebo or routine treatment were studied in detail. An initial search in PubMed and Google scholar using the search strategy yielded 10 221 articles. Finally, 10 articles meeting the inclusion criteria were analyzed for the review (Figure 1).14–23
Figure 1.
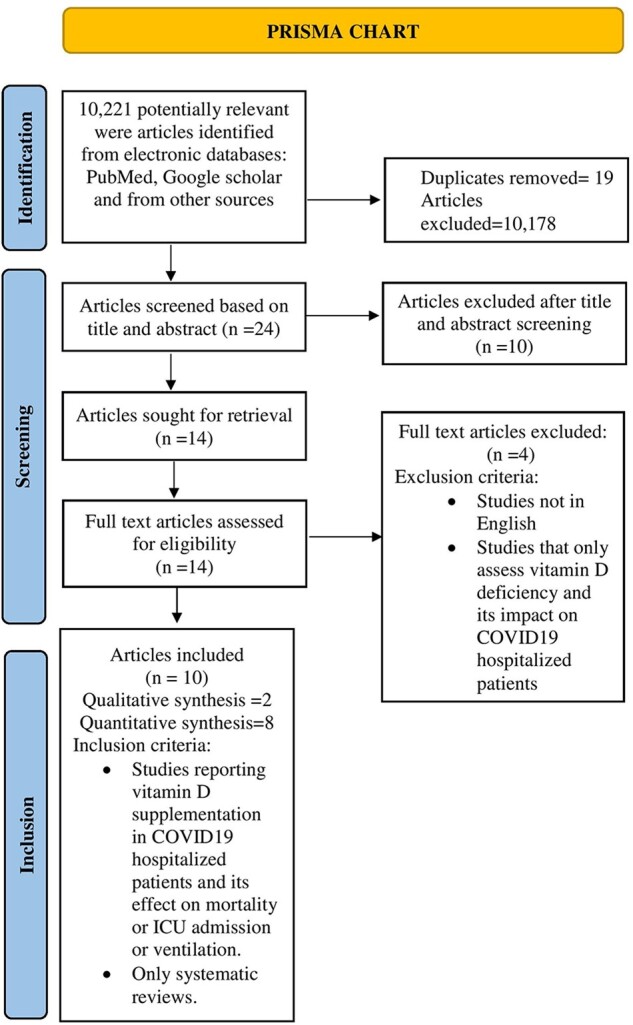
PRISMA chart.
Characteristic details of all the included systematic reviews were extracted and are presented in Table 1. The number of primary studies included in the reviews ranged from 3 to 13, which included all types of study designs including randomized controlled trials. Latest review was published in December 2021. Hence it seems that most studies were done before the appearance of Omicron variant. Three reviews were conducted from India.
Table 1.
Basic characteristics of the included systematic reviews
| Serial number | Authors | Title | Country | No of studies included | Types of studies included | Total population |
|---|---|---|---|---|---|---|
| 1 | Chen et al., Oct 2012114 | Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs | China | 13 | Cohort studies = 11, Randomized control Trials = 2 | 5 36 418 |
| 2 | Grove et al., May 202115 | Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review | UK | 4 | Cross-sectional study = 1, retrospective cohort study = 1, ecological country study = 1, case-control survey = 1 | 2042 |
| 3 | Hariyanto et al., June 202116 | Vitamin D supplementation and Covid-19 outcomes: A systematic review, meta-analysis and meta-regression | Indonesia | 11 | Retrospective cohort studies = 4, Open-label randomized clinical trial = 1, Prospective cohort studies = 2, Cross-sectional studies = 3, double-blind randomized clinical trial = 1 | 2265 |
| 4 | Nikniaz et al., Jan 202117 | The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis | Iran | 4 | Randomized control trials = 2, Quasi Experimental trials = 2 | 259 |
| 5 | Pal et al., June 202118 | Vitamin D supplementation and clinical outcomes in COVID 19: a systematic review and meta-analysis | India | 13 | Randomized control trials = 3, Observational studies = 10 | 2933 |
| 6 | Rawat et al., June 202119 | Vitamin D supplementation and COVID-19 treatment: A systematic review and meta-analysis | India | 5 | Randomized control trials = 3, Quasi experimental studies = 2 | 467 |
| 7 | Shah et al., May 202120 | Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis | India | 3 | Randomized control trials = 2, retrospective case-control study = 1 | 532 |
| 8 | Stroehlein et al., May 202121 | Vitamin D supplementation for the treatment of COVID‐19: a living systematic review | Germany | 3 | Randomized control trials = 3 | 356 |
| 9 | Tentolouris et al., Dec 202122 | The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression | Greece | 10 | Randomized control trials = 2, non-randomized trials = 8 | 2078 |
| 10 | Vaughan et al., Oct 202123 | Changes in 25‐hydroxyvitamin D levels post‐vitamin D supplementation in people of Black and Asian ethnicities and its implications during COVID‐19 pandemic: A systematic review | UK | 8 | Randomized control trials = 8 | 1108 |
Most of the studies considered for this evidence summary have used vitamin D supplementation in oral form either as oral cholecalciferol or oral calcifediol.15,17–19,23 The dosage of the supplementation varied in the studies. Booster therapies given were in the range of 280 000 IU or 400 000 IU.18 Upon careful evaluation, a unique study based on ethnicity found out that vitamin D3 is more efficacious than D2, when supplemented orally. The lowest dose administered was 400 IU while 60 000 IU was the highest.23 Another study by Nikniaz et al.17 supplemented the intervention group with oral vitamin D3 (60 000 IU–80 000IU). The conclusion drawn from the study supported that vitamin D supplementation was more efficacious against mortality when compared to corticosteroids, hydroxychloroquine and other antibiotics.
AMSTAR and GRADE assessment showed that the majority of the systematic reviews were suffering from low quality of evidences (Supplementary tables S1 and S2). Significant heterogeneity was observed among the studies reporting efficacy of vitamin D on morbidity and mortality outcomes in COVID patients. The majority of the studies showed improvement in the outcome, however, due to smaller sample size, some studies could not reach to a statistically significant level. The strength, limitations and key findings of the individual review are summarized in Table 2. Overlapping between the primary studies included in the systematic reviews were also assessed and considerable overlapping was observed. The individual study level analysis is presented as Supplementary table S3.
Table 2.
Findings of the included systematic reviews
| Serial number | Authors | Key findings | Strength | Limitations |
|---|---|---|---|---|
| 1 | Chen et al., Oct 2012114 | No significant association of Vitamin-D deficiency/insufficiency with COVID-19 infections, mortality and ICU admissions. | Study design which includes cohort studies and Randomized control trials. Use of GRADE to evaluate the quality of evidence. | High heterogeneity due to study design and baseline characteristics. Potential risk factors were not completely adjusted. |
| 2 | Grove et al., May 202115 | No robust evidence to assess the association of Vitamin-D supplementation with COVID-19 and its outcomes such as mortality, morbidity. | Study design using PRISMA checklist and information on current situation using multiple living systematic review data bases | Study design which consisted of non-randomized studies. Small amount of evidence that might led to bias and hence the inferences that can be drawn. |
| 3 | Hariyanto et al., June 202116 | Association of Vitamin-D with reduction in ICU admission, mortality and mechanical ventilation. Age is associated with Vitamin-D supplementation and COVID-19 mortality. | The potential of Vitamin-D as a favorable drug to reduce the clinical outcomes of COVID-19. | Significant heterogeneity due to the prescribed doses and co-administered drugs with Vitamin-D. |
| 4 | Nikniaz et al., Jan 202117 | Pooled estimations showed a significant reduction in mortality, severity of disease and serum levels of inflammatory markers upon Vitamin-D supplementation as compared to the control group. | Careful evaluation of the vitamin-D supplementation on mortality rates, ICU admission as well as the secondary outcomes such as reduction in severity of disease using WHO OSCI score. | Ineffective to standardize the optimum dosage and route of administration. |
| 5 | Pal et al., June 202118 | Vitamin-D is significantly associated with COVID-19 in terms of reducing mortality, ICU admissions and other clinical outcomes. | The strength of this study lies in the fact that it reflects the benefits of Vitamin-D supplementation only in COVID-19 positive population. | Appropriate Dose, duration and mode of administration yet could not be answered. |
| 6 | Rawat et al., June 202119 | No significant association is seen between Vitamin-D supplementation in reducing the clinical outcomes such as mortality, ICU admission and ventilation. | Observations drawn on the basis of RCT’S and Quasi Experimental Trials. | The number of studies undertaken were less to arrive to a final conclusion. Time frame was also not considered. Heterogeneity in intervention with respect to Vitamin-D supplementation. Significant non-uniformity with regards to various factors in Vitamin-D supplementation. |
| 7 | Shah et al., May 202120 | Association between Vitamin-D supplementation in reducing ICU requirements, but almost same effects in mortality as placebo. | First meta-analysis that showed the positive association of Vitamin-D supplementation in reducing the clinical outcomes such as ICU requirements. | Heterogeneous baseline populations that were enrolled, Number of trials that took place while the study was being conducted. |
| 8 | Stroehlein et al., May 202121 | Limited safety information to usage of Vitamin-D supplementation for COVID-19 population. | A living approach were based on the current findings and on-going literature data was published. | No pooling of data due to heterogeneity of the studies, leading to uncertainty if Vitamin-D can be potentially used for reducing all-cause mortality in Covid-19 population. |
| 9 | Tentolouris et al., Dec 202122 | No significant linear relationship observed between Vitamin-D supplementation and mortality, although it has a reduced effect on ICU admissions | A meta-regression analysis regarding the relationship between the administered dose of vitamin-D and the outcome of interest. | Inclusion of non-randomized studies. Heterogeneity in the study in forms of dose. |
| 10 | Vaughan et al., Oct 202123 | Vitamin D3 is more efficacious than Vitamin-D, oral supplementation is more effective in black and Asian people. | Form and Route of administration that can be more beneficial in context of ethnicities. | Heterogeneity in studies in terms of dosage, duration and populations. Only English studies were included which could be translated. |
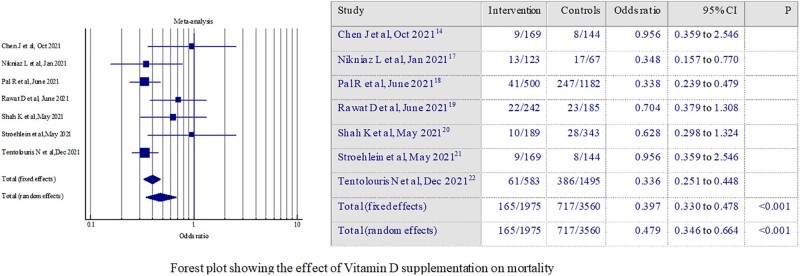
Mortality
A meta-analysis of seven systematic reviews, providing quantitative data regarding the odds of mortality among hospitalized COVID-19 patients with and without vitamin D supplementation was performed. It was found that, in people receiving vitamin D supplements, the odds of mortality were 52% lower as compared to individuals not receiving vitamin D supplements (OR: 0.48, 95% CI: 0.346–0.664; P < 0.001) (Figure 2). This suggests that vitamin D supplementation acts as a protective therapy in reducing overall COVID-19-related mortality. Random effect model was considered due to the presence of heterogeneity (I2-54%; P = 0.04) among the review findings. Significant publication bias was observed through Egger’s test (p=0.015); however, Begg’s test did not show any significant bias (p=0.11).
Figure 2.
Forest plot showing the effect of vitamin D supplementation on mortality.
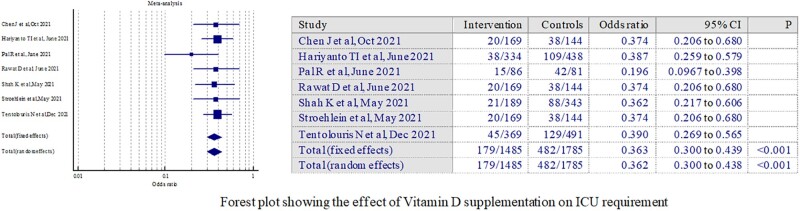
ICU admission
The cumulative effect of vitamin D supplementation on risk of ICU admission in COVID-19 hospitalized patients was assessed using meta-analysis of seven number of systematic reviews. It was observed that there is a statistically significant (P < 0.0001) difference between ICU admission rate in patients receiving vitamin D supplements as compared to patients not receiving vitamin D. The odds of intensive care needs were 0.35 (95% CI: 0.28–0.44) with vitamin D supplementation (Figure 3). The findings were robust and reliable with absence of heterogeneity as indicated by I2 (0%; P = 0.78). No significant bias was observed with Egger’s test and Begg’s test showed some bias (p=0.03).
Figure 3.
Forest plot showing the effect of vitamin D supplementation on ICU admissions.
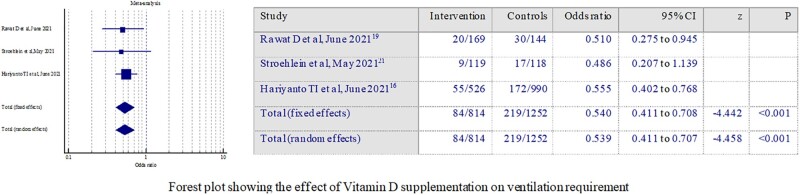
Ventilation
Three studies provided quantitative data regarding the effect of vitamin D supplementation on requirement of mechanical ventilation in COVID patients.16,19,21 Pooled analysis showed that there is a reduction in odds of requiring ventilation support in patients treated with vitamin D supplementation as compared to others without vitamin D treatment (Odds ratio: 0.54; 95% CI: 0.411–0.708; P < 0.001) (Figure 4). Fixed effect model was considered as no heterogeneity was noted as per I2 statistics (0%; P = 0.94). No significant publication bias was observed through Egger’s or Begg’s test.
Figure 4.
Forest plot showing the effect of vitamin D supplementation on ventilation requirement.
Discussion
The current evidence summary presents findings from 10 published systematic reviews studying the effect of vitamin D supplementation on morbidity and mortality in hospitalized COVID-19 patients.14–23 The review attempted to synthesize both qualitative and quantitative evidence from the published articles through a systematic approach and observed that vitamin D supplementation reduces the risk of mortality, need for intensive care and ventilation in COVID-19 patients irrespective of age, gender, race, ethnicity and comorbid conditions. These studies were from India, China, Indonesia, Greece, the United Kingdom and Germany, spanning a large geographical area.
Vitamin D and COVID-19, desirable levels of vitamin D in the serum and the recommended doses of supplementation has been in the spot-light and are still under dialogue among the medical fraternity. However, with the rise of OMICRON and the possibility of future waves of the coronavirus, it is critical to investigate all possible COVID-19 management and treatment options. With the low cost of vitamin D, easy availability in the global pharmaceutical market, good safety at least at a dosage of 4000 IU/day, familiarity of clinicians with the molecule and its mechanism of action and well prevalent deficiency in the population makes it a very suitable drug for COVID management even with controversial efficacy.24 The findings of the present evidence summary overcomes some of the inherent limitations associated with vitamin D supplementation trials and showed that vitamin D can be advocated as a possible adjunctive for the management of at least hospitalized COVID-19 patient.
Use of vitamin-D supplementation to prevent acute respiratory tract infections has already been documented by various clinical trials and systematic reviews.5–7,16,18–20,22 The mode of cellular action of vitamin D3 receptors especially in T cells and dendritic cells make it suitable for the treatment of COVID-19 disease.25 Also, vitamin D cathelicidins are known to promote autophagy and have anti-viral properties. Use of this antimicrobial peptide (human cathelicidin LL-37) can inhibit SARS-Cov-2 infection.26–28 Rationally, all these factors together became the underlying biological foundation for using vitamin D in the present pandemic. However, the impact of supplementation varies from being modest to large as indicated in evidence synthesis report. This might be hugely driven by the baseline levels of vitamin D in patients. It was found that individuals with higher deficiencies will respond better to the supplementation in contrast to participants with normal levels of vitamin D.
The evidence summary consisted of systematic reviews involving as small as three primary trials to 13 trials and have presented entire landscape assessment right from starting of the pandemic. It also presents the impact of vitamin D on patients with entire spectrum of disease severity which showed mixed evidence. From all the systematic reviews identified for this summary synthesis, the review with the largest sample size of 5 36 418 participants concluded that low vitamin D levels do not exacerbate COVID-19 risk and nor does vitamin D supplementation improve outcomes in hospitalized patients with COVID-19.14 In contrast, studies such as those conducted in India using adjunctive pulse D therapy (60 000 IU) in combination with the standard treatments for COVID-19 concluded that vitamin D was a potential immunomodulator that could be added to the COVID-19 treatment protocol. Furthermore, a trial involving 76 participants found that calcifediol at a high dose helped significantly reduce ICU admissions.4
A systematic review involving Asian ethnicities revealed that vitamin D supplementation at a dosage of 400 IU is more effective at raising 25(OH)D levels when sun exposure does not permit sufficient vitamin D synthesis in black and Asian ethnicities.23 The study found that whereas 25(OH)D levels were 25 nmol L1 at baseline, vitamin D supplementation, independent of dosage, mode of delivery or duration, boosted the levels to >25 nmol L1. It was worth mentioning that the mode of vitamin D ingestion played a significant influence in boosting serum 25(OH)D levels.29 Due to climatic conditions, people in the temperate zone are usually less exposed to the sun, whereas Asians and Africans suffer from vitamin D insufficiency due to the constitutive pigment melanin in the skin, which absorbs UV radiation and protects the underlying tissues from damage.30
So far, no guidelines have been established by the Centre for Disease Control or World Health Organization on the supplementation of vitamin D as a treatment for COVID-19 outcomes. The role of vitamin D supplementation on COVID-19-related outcomes has been studied extensively, but it remains controversial whether vitamin D should be included as a curative in the COVID-19 treatment guidelines.
Findings from quantitative analysis presented as meta-analysis in this review addresses one important limitation of the individual systematic reviews—low sample size and presence of heterogeneous data. But the cumulative analysis of the included reviews suggests that vitamin D has the potential to prevent and treat COVID-19-related outcomes, such as mortality, ICU admissions, and ventilation. We also acknowledge that there was a high overlap between the included studies in the reviews. Hence, with this review we aim to advocate the integration of vitamin D supplementation in the treatment protocol for COVID-19. Also due to some inherent bias and varied quality of the included reviews, the recommendations of current review need to be substantiated with large, well designed prospective trials.
Conclusion
The current evidence suggests that vitamin D is a potential immunomodulator that has a major role in lowering COVID-19-related mortality, ICU hospitalizations and ventilation. As a result, we believe that supplementary vitamin D can be safely added to the existing COVID-19 treatment procedures. However, more large-scale trials are recommended to further validate its effect in various heterogenous groups of population.
Supplementary material
Supplementary material is available at QJMED online.
Conflict of interest. None declared.
Supplementary Material
References
- 1. Harvey WT, Carabelli AM, Jackson B, Gupta RK, Thomson EC, Harrison EM, et al. SARS-CoV-2 Variants, Spike Mutations and Immune Escape. www.nature.com/nrmicro. 22 January, 2022. [DOI] [PMC free article] [PubMed]
- 2. Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data Supplementary Material Davaasambuu Ganmaa 7 Adit A Ginde 8 Ilkka Laaksi 13 Semira Manaseki-Holland 14 Iwona Stelmac. 2017. [DOI] [PMC free article] [PubMed]
- 3. Malaguarnera L. Vitamin D3 as potential treatment adjuncts for COVID-19. Nutrients 2020; 12:3512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, Alcalá Díaz JF, López Miranda J, Bouillon R, et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study. J Steroid Biochem Mol Biol 2020; 203:105751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rastogi A, Bhansali A, Khare N, Suri V, Yaddanapudi N, Sachdeva N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study). Postgrad Med J 2020; 98:postgradmedj-2020-139065. [DOI] [PubMed] [Google Scholar]
- 6. Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CSC, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial. J Am Med Assoc 2021; 325:1053–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Han JE, Jones JL, Tangpricha V, Brown MA, Hao L, Hebbar G, et al. High dose vitamin D administration in ventilated intensive care unit patients: a pilot double blind randomized controlled trial. J Clin Transl Endocrinol 2016; 4:59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mercola J, Grant WB, Wagner CL.. Evidence regarding vitamin D and risk of COVID-19 and its severity. Nutrients 2020; 12:3361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Radujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U.. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients 2020; 12: 2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Campi I, Gennari L, Merlotti D, Mingiano C, Frosali A, Giovanelli L, et al. Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy. BMC Infect Dis 2021; 21:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karahan S, Katkat F.. Impact of serum 25(OH) vitamin D level on mortality in patients with COVID-19 in Turkey. J Nutr Heal Aging 2021; 25:189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shen H, Mei Y, Zhang K, Xu X.. The effect of vitamin D supplementation on clinical outcomes for critically ill patients: a systemic review and meta-analysis of randomized clinical trials. Front Nutr 2021; 8:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bouillon R, Manousaki D, Rosen C, Trajanoska K, Rivadeneira F, Richards JB.. The health effects of vitamin D supplementation: evidence from human studies. Nat Rev Endocrinol 2022; 18:96–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen J, Mei K, Xie L, Yuan P, Ma J, Yu P, et al. Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: a meta-analysis and GRADE assessment of cohort studies and RCTs. Nutr J 2021; 20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grove A, Osokogu O, Al-Khudairy L, Mehrabian A, Zanganeh M, Brown A, et al. Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review. BMJ Open 2021; 11:e043737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hariyanto TI, Intan D, Hananto JE, Harapan H, Kurniawan A.. Vitamin D supplementation and Covid‐19 outcomes: a systematic review, meta‐analysis and meta‐regression. Rev Med Virol 2021; e2269. [Google Scholar]
- 17. Nikniaz L, Akbarzadeh MA, Hosseinifard H, Hosseini MS.. The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: a systematic review and meta-analysis. Pharm Sci 2021; 27:S1–12. [Google Scholar]
- 18. Pal R, Banerjee M, Bhadada SK, Shetty AJ, Singh B, Vyas A.. Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis. J Endocrinol Invest 2022; 45:53–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rawat D, Roy A, Maitra S, Shankar V, Khanna P, Baidya DK.. Vitamin D supplementation and COVID-19 treatment: a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev 2021; 15:102189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shah K, Saxena D, Mavalankar D.. Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis. QJM 2021; 114:175–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stroehlein JK, Wallqvist J, Iannizzi C, Mikolajewska A, Metzendorf MI, Benstoem C, et al. Vitamin D supplementation for the treatment of COVID-19: a living systematic review. Cochrane Database Syst Rev 2021; 2021:CD015043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tentolouris N, Samakidou G, Eleftheriadou I, Tentolouris A, Jude EB.. The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID‐19 patients. A systematic review, meta‐analysis and meta‐regression. Diabetes Metab Res Rev 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vaughan M, Trott M, Sapkota R, Premi G, Roberts J, Ubhi J, et al. Changes in 25-hydroxyvitamin D levels post-vitamin D supplementation in people of Black and Asian ethnicities and its implications during COVID-19 pandemic: a systematic review. J Hum Nutr Diet 2021; 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rizzoli R. Vitamin D supplementation: upper limit for safety revisited? Aging Clin Exp Res 2021; 33:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Griffin G, Hewison M, Hopkin J, Kenny R, Quinton R, Rhodes J, et al. Vitamin D and COVID-19: evidence and recommendations for supplementation. R Soc Open Sci 2020; 7:201912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang C, Wang S, Li D, Chen P, Han S, Zhao G, et al. Human cathelicidin inhibits SARS-CoV-2 infection: killing two birds with one stone. ACS Infect Dis 2021; 7:1545–54. [DOI] [PubMed] [Google Scholar]
- 27. Kulie T, Groff A, Redmer J, Hounshell J, Schrager S.. Vitamin D: an evidence-based review. J Am Board Fam Med 2009; 22:698–706. [DOI] [PubMed] [Google Scholar]
- 28. Chung C, Silwal P, Kim I, Modlin RL, Jo EK.. Vitamin D-cathelicidin axis: at the crossroads between protective immunity and pathological inflammation during infection. Immune Netw 2020; 20:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Grønborg IM, Tetens I, Christensen T, Andersen EW, Jakobsen J, Kiely M, et al. Vitamin D-fortified foods improve wintertime vitamin D status in women of Danish and Pakistani origin living in Denmark: a randomized controlled trial. Eur J Nutr 2019; 59:741–53. [DOI] [PubMed] [Google Scholar]
- 30. Webb AR, Kazantzidis A, Kift RC, Farrar MD, Wilkinson J, Rhodes LE.. Colour counts: sunlight and skin type as drivers of vitamin D deficiency at UK latitudes. Nutrients [Internet] 2018; 10:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.