Abstract
Choosing the appropriate site of care for patients is a vital clinical skill when caring for older adults. For better patient safety and smoother transitions of care, we need improved curricula to train clinicians about the system of sites and services where older adults receive care. Here we present an innovative introduction for medical trainees to the complexities of long-term and post-acute care for geriatric patients. Students participated in a team-based ‘jigsaw’ learning activity, in which each team researched a particular site of care and then taught a larger group of their peers about that site. It was subsequently converted to a virtual format due to COVID-19. The activity was assessed using students’ written feedback and satisfaction scores. Students enjoyed the interactivity and hands-on approach, giving the activity an average score of 3.9 out of 5 (1 = ‘poor’; 5 = ‘excellent’). The jigsaw provided an engaging, case-based foundation for learning about sites of care and was well-received by students.
Keywords: medical education, long-term care, post-acute care, care transitions, active learning
Key Points
Clinician proficiency in transitions of care for older adults is essential and complex.
Increasing demand on long-term and post-acute care calls for urgent need to improve medical education of geriatric sites of care.
We used an engaging team-based ‘jigsaw’ activity to teach students about sites and services where older patients receive care.
Introduction
The COVID-19 pandemic has caused a staggering number of cases and deaths (over 640,000 and 130,000 respectively, at the time of writing) in long-term care (LTC) facilities throughout the USA, representing over one-third of the country’s total COVID-19-related deaths [1, 2]. As such, geriatric sites of care have received new public attention and healthcare professionals must better understand these sites and services to improve their patients’ care. Millions of older Americans receive LTC services, including over 280,000 participants at adult day centers, 800,000 residents of assisted living facilities (ALFs) or similar residences, and 1.3 million skilled nursing facility (SNF) residents [3]. In addition to LTC, increasing numbers of patients are discharged from hospitals to post-acute care (PAC) settings for increasingly longer rehabilitation stays, averaging over 25 days in 2015 [4]. Over 45% of Medicare beneficiaries are discharged from hospitals to these various PAC sites, including SNFs, inpatient rehabilitation facilities, long-term acute care hospitals and home health agencies [5].
Medical education must address the call to improve geriatric care. However, few trainees receive formal instruction or structured experiences about best practices in hospital discharges and transitions of care, let alone an opportunity to practice clinically at sites beyond the hospital or clinic [6]. These training gaps lead to misconceptions about the post-discharge process and inadequate transitional care plans, resulting in inefficiency, miscommunication, medical errors and high-risk complications, including rehospitalizations and adverse drug events [5, 6]. We propose a redesigned curriculum that prepares new clinicians to properly determine the best level of care for every patient and to educate patients and families on their options [7].
To close this knowledge gap at an early stage, we used an innovative teaching method, a team-based jigsaw learning activity, to teach first-year medical and dental students about sites of care. ‘Jigsaw’ is a cooperative learning strategy in which students gather information in groups and then teach one another, piece by piece, like solving a jigsaw puzzle. It has been shown to improve students’ engagement and knowledge retention [8]. This method has been successful in introducing medical students to the roles of various professionals on a PAC healthcare team [9], but to our knowledge, has never been used to teach the complexities involved in evaluating a geriatric patient’s ideal setting for care. The session learning objectives included:
compare and contrast various types of geriatric care settings,
identify the services and interprofessional team members at these sites, and
describe the costs and eligibility requirements for each site.
In response to COVID-19, we also aimed for students to apply new knowledge to current events, particularly applied to older adults. We hypothesized that students would find the jigsaw approach more engaging than a traditional lecture or reading assignment.
Methods
The activity took place in 2019 and 2020. In the second year amid the COVID-19 pandemic, we adapted to virtual learning via videoconference. In 2019, the activity was piloted as part of a larger geriatric education session consisting of the jigsaw and a home visit to an older adult at an independent living facility. The jigsaw was evaluated as part of new longitudinal curricular theme, Aging Population & End of Life Care, at Harvard Medical School (HMS), which was approved by the HMS Educational Scholarship Review Team as educational quality improvement not requiring IRB review.
Medical student participants were divided into seven groups of six to eight students each, corresponding to the seven different PAC and LTC sites/services under examination (Table 1). Each group was given 10 minutes to answer questions on their assigned site(s) of care, using preselected articles from the geriatrics literature [5, 10] and resources they found online. To guide their research, each group completed a worksheet on topics of patient eligibility, services provided, interprofessional team players, payment structure and local examples of this site of care (Appendix 1).
Table 1.
Geriatrics sites of care and services in a jigsaw learning activity for medical students
| Site/service | Patient description (‘One-Liner’) |
|---|---|
| 1. Independent Living | Eight six-year-old woman with diabetes and hypertension who lives independently and would like to continue doing so, while having access to social groups and activities in her community. |
| 2. Assisted Living Facility | Ninety-two-year-old woman who is looking to live somewhere where meals are provided, and assistance is available for bathing and dressing. She manages her own finances. |
| 3. Home with services (Visiting Nurse Agencies, Area Agencies on Aging/Elder Services) | Seventy-five-year-old previously functionally independent community-dwelling man with diverticulitis status post end colostomy wanting assistance with colostomy care as he returns home. |
| 4. Post-acute care (Skilled Nursing Facility/Sub-Acute Rehab) | Eighty-four-year-old previously functionally independent community-dwelling woman status post hip fracture repair who needs strengthening before she is ready to return home. |
| 5. Programs of All-Inclusive Care for the Elderly (PACE) | Sixty-year-old woman with diabetes, hypertension, CHF, aortic stenosis, stage 4 CKD and osteoporosis who continues to live safely in her community and is dually eligible for Medicare and Medicaid. |
| 6. Long-term care (Skilled Nursing Facility/Nursing Home) | Eighty-five-year-old man with advanced Alzheimer’s dementia and diabetes who needs assistance with iADLs and several ADLs, 24 hour supervision and medication management. |
| 7. Hospice | Seventy-two-year-old man with metastatic colorectal cancer and expected prognosis less than 6 months. |
Legend: ADL = activity of daily living; CHF = congestive heart failure; CKD = chronic kidney disease, iADL = instrumental activity of daily living.
The seven teams then joined in a large group discussion facilitated by geriatrics faculty. For each site of care, the facilitator presented a ‘one-liner’ (Table 1) about a typical older adult who might live in or benefit from that particular setting. Students identified the best site or service, then the assigned group presented their research for 3–5 minutes. The facilitator provided additional detail and clarified questions from the larger group. In 2020, an experienced geriatrics faculty member joined the video conference from their site of care, providing their perspective on how COVID-19 had impacted the patients, staff and practice of medicine at that site.
Overall, the jigsaw activity requires about 1 hour, including a brief introduction, the 10-minute breakout groups, and the class-wide faculty-led summaries and discussion (Figure 1). At a minimum, one to two faculty members are required to coordinate the activity and facilitate the final discussion. However, during our virtual activity, an additional three faculty joined, each representing a different site of care. The activity can be held on-site at any geriatric site of care which has the capacity to accommodate the learners and faculty (in our case, a local independent senior living facility) or online, where the capacity for attendees is unlimited.
Figure 1.
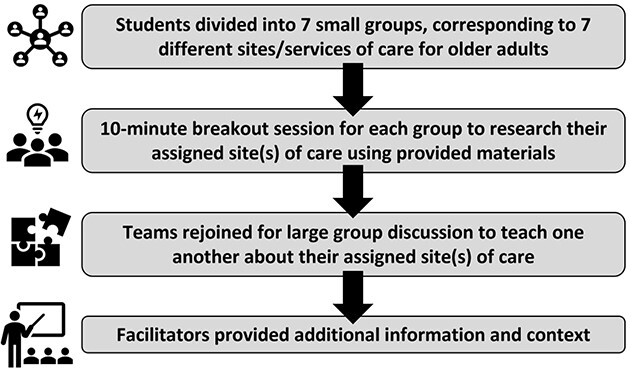
Geriatric sites of care jigsaw activity framework.
Results
The jigsaw activity was evaluated by students using both quantitative and qualitative feedback, on an optional and anonymous basis. They rated the jigsaw activity using a Likert scale (poor, fair, good, very good or excellent), and provided narrative feedback on the overall session. They were also asked to comment on one or two new things they had learned from the session. In 2020, a pre- and post-activity quiz asked students to identify three different sites of care through multiple choice questions (Appendix 2) to assess students’ knowledge of the material and to rate their confidence in determining the appropriate site of care for a geriatric patient.
Over our two years tracking the jigsaw activity, 242 of 341 total participants (71%) completed the evaluations. The average rating across multiple sessions held during these two academic years was 3.9 out of 5 on a Likert scale (1 = ‘poor’; 5 = ‘excellent’). The 2019 in-person activity had received an average rating of 4.2 out of 5 by 132 out of 171 students, whereas the 2020 virtual activity received an average rating of 3.5 out of 5 by 110 out of 170 students. In 2020, students’ average pre- and post-activity confidence scores were 2.4 and 3.8 out of 5, respectively (P < 0.05; 1= ‘not at all confident’, 5 = ‘very confident’). Despite reporting increased confidence after the activity, student scores on the knowledge assessment failed to improve from before to after the jigsaw (40.8% [pre] to 40.3% [post], P = 0.9).
In written responses across both years, students reported a new appreciation of the nuances in selecting various sites of care, such as one student who ‘learned about many “SNF-like” places [they] didn’t know existed before’. Others praised the interactivity and group work of the session. Constructive feedback that we received in our first year suggested providing a summary handout and making the session more case-based, changes incorporated into the following year’s activity. In the second year, several students suggested discussing strategies to guide patients and families through shared decisions on sites of care.
Discussion
The Sites of Care jigsaw is an innovative approach to introducing students to the complexities of post-acute and LTC for geriatric patients. We aimed to teach students using an engaging active learning strategy and found that many students enjoyed learning from one another using this method. However, although the 1-hour session did increase learners’ confidence, it did not result in an increase in knowledge in this student group.
Kirkpatrick’s pyramid offers a model for evaluating these types of educational interventions: the four levels include (i) learner reaction or satisfaction, (ii) knowledge gained, (iii) impact of learning on behaviour and (iv) results (on patient care) [11]. The evaluation of this educational program was limited: we assessed learner satisfaction and general reaction to the 2019 program and added a brief pre- and post-activity knowledge assessment in 2020. Though learner self-efficacy improved, learner knowledge did not, pointing to the need to learn from this essentially negative study to improve the teaching session going forward. This outcome may reflect a combination of factors, including a need for further validation of questions, the session being too short or fast-paced, or too much information presented at once. In addition, though student feedback was generally positive, we did not assess their behaviours or attitudes towards caring for older adults and carrying out challenging discharge plans and discussions. Further iterations of the jigsaw activity could incorporate more structured, validated evaluations regarding student knowledge, skills and attitudes that would identify key aspects of the activity that need to be adjusted to better meet the learning needs of our students. For instance, in order to evaluate learner behaviour, an activity such as role play or OSCE (Objective Structured Clinical Exam [12]) where students discuss discharge planning with a patient could be implemented, and ultimately, we would hope that with increased provider education in this area, patient care would improve in the long run.
Future iterations of the jigsaw learning activity will continue to build upon students’ written feedback, such as creating more case-based, patient-centered content and providing students with summarized information they can use, such as a pocketcard summarizing the sites of care [13]. Their evaluations help us understand that first-year students lack basic knowledge of the healthcare system and reflect successes and areas for improvement in our teaching of this material.
The COVID-19 pandemic has created a new era of virtual medical school education, which presents its own unique set of challenges [14]. Our student satisfaction ratings were lower for the virtual format than the in-person format, pointing to the challenge of keeping virtual learners engaged. Although videoconferencing ‘breakout rooms’ were organized for small groups to meet during the virtual jigsaw activity, student interest may have dipped from our in-person sessions. Capturing a patient-centered approach will be more important now than ever before. We sought to do this by inviting geriatrics faculty to reflect on their COVID experience at various site of care. Future iterations can invite patients to share their own perspectives on transitioning from one level of care to another. Further instruction and role-playing could also be incorporated to explore the difficult emotions surrounding discharge planning and placement discussions with patients and families. Finally, a more experiential program, in which each group visits a site (when social distancing guidelines permit such visitation) and then shares what they learned, might be more enriching.
The concepts introduced in this jigsaw learning activity need to be continually reinforced during the clinical years and in health policy classes. Faculty also need more professional development in teaching about sites of care. Ideally, experiential clinical learning at sites other than the hospital and clinic should be incorporated into medical education for doctors to feel well-prepared to advise patients and their families about choosing the appropriate site of care.
We invite educators to use the Geriatric Sites of Care jigsaw activity as an engaging way to share knowledge with the next generation of clinicians caring for our world’s growing ageing population. We have shown that the activity can be adapted to a variety of settings, including in-person or virtual. It could likewise be adapted to meet the curricular needs of students at different levels of training or even different healthcare systems worldwide. This could be accomplished by providing students with different reading materials or adjusting the groups to appropriately reflect the various sites of care that are locally available to patients. This is a very complex landscape even for practicing physicians, so further research is needed to determine the best way to teach medical trainees about this topic. Ultimately, although this Sites of Care jigsaw activity did not improve student knowledge, the interactivity was well-received and offers a promising model to close a real skills gap for physicians in training: the knowledge to guide their patients to the right level of care to support them as they age.
Supplementary Material
Acknowledgements
We thank Melissa Greeley, the team at Hebrew Senior Life, and the leadership of the HMS Practice of Medicine course for supporting this learning activity and the HMS Geriatrics Clinical Immersion. We also thank the many faculty and students who have participated in this session.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
Some of this material is the result of work supported with resources and the use of facilities at the Veterans Affairs Boston Healthcare System and the New England Geriatric Research Education and Clinical Center. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. The learning activity was hosted at Hebrew Senior Life, A Harvard Teaching Affiliate, and was supported by the Harvard Medical School Practice of Medicine Course and the Dean’s Innovation Award.
References
- 1. Centers for Medicare & Medicaid Services . COVID-19 Nursing Home Data. DataCMS.gov, 2021. [Google Scholar]
- 2. The New York Times . Nearly One-Third of U.S. Coronavirus Deaths Are Linked to Nursing Homes. The New York Times. 2021. https://www.nytimes.com/interactive/2020/us/coronavirus-nursing-homes.html. (accessed 5 October 2021). [Google Scholar]
- 3. National Center for Health Statistics (U.S.) ed . Long-Term Care Providers and Services Users in the United States, 2015–2016. Washington, DC: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, 2019. [Google Scholar]
- 4. Werner RM, Konetzka RT. Trends in post–acute care use among Medicare beneficiaries: 2000 to 2015. JAMA 2018; 319: 1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kane RL. Finding the right level of Posthospital care: “We Didn’t Realize There Was Any Other Option for Him”. JAMA 2011; 305: 284. [DOI] [PubMed] [Google Scholar]
- 6. Ward KT, Eslami MS, Garcia MBet al. Do internal medicine residents know enough about skilled nursing facilities to orchestrate a good care transition? J Am Med Dir Assoc 2014; 15: 841–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ouslander JG, Sehgal M. The conundrum of choosing post-acute care: a challenge for patients, families, and clinicians: editorial. J Am Geriatr Soc 2019; 67: 638–40. [DOI] [PubMed] [Google Scholar]
- 8. Walker S, Olvet DM, Chandran L. The jigsaw technique of peer teaching and learning: an efficient and enjoyable teaching strategy in medicine. MedEd 2015. 10.15694/mep.2015.006.0014. [DOI] [Google Scholar]
- 9. Buhr GT, Heflin MT, White HKet al. Using the jigsaw cooperative learning method to teach medical students about long-term and postacute care. J Am Med Dir Assoc 2014; 15: 429–34. [DOI] [PubMed] [Google Scholar]
- 10. Goldberg TH. The long-term and post-acute care continuum. W V Med J 2014; 110: 24–30. [PMC free article] [PubMed] [Google Scholar]
- 11. Yardley S, Dornan T. Kirkpatrick’s levels and education “evidence”. Med Educ 2012; 46: 97–106. [DOI] [PubMed] [Google Scholar]
- 12. Lyons MD, Miles DB, Davis AMet al. Preventing breakdowns in communication: teaching patient-centered posthospital care transitions to medical students. MedEdPORTAL 12: 10435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Holliday AM, Hawley CE, Schwartz AW. Geriatrics 5Ms pocket card for medical and dental students. J Am Geriatr Soc 2019; 67: E7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rose S. Medical student education in the time of COVID-19. JAMA 2020; 323: 2131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


