Abstract
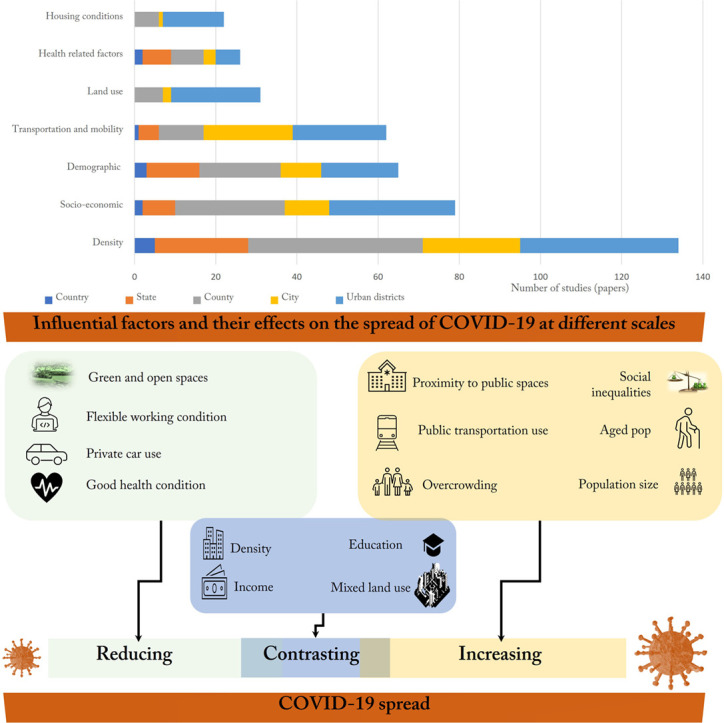
Soon after its emergence, COVID-19 became a global problem. While different types of vaccines and treatments are now available, still non-pharmacological policies play a critical role in managing the pandemic. The literature is enriched enough to provide comprehensive, practical, and scientific insights to better deal with the pandemic. This research aims to find out how the built environment and human factors have affected the transmission of COVID-19 on different scales, including country, state, county, city, and urban district. This is done through a systematic literature review of papers indexed on the Web of Science and Scopus. Initially, these databases returned 4264 papers, and after different stages of screening, we found 166 relevant papers and reviewed them. The empirical papers that had at least one case study and analyzed the effects of at least one built environment factor on the spread of COVID-19 were selected. Results showed that the driving forces can be divided into seven main categories: density, land use, transportation and mobility, housing conditions, demographic factors, socio-economic factors, and health-related factors. We found that among other things, overcrowding, public transport use, proximity to public spaces, the share of health and services workers, levels of poverty, and the share of minorities and vulnerable populations are major predictors of the spread of the pandemic. As the most studied factor, density was associated with mixed results on different scales, but about 58 % of the papers reported that it is linked with a higher number of cases. This study provides insights for policymakers and academics to better understand the dynamic roles of the non-pharmacological driving forces of COVID-19 at different levels.
Keywords: COVID-19, Built environment, Non-pharmacological factors, Density, Socio-economic factors, Urban planning
Graphical abstract
1. Introduction
By June 2022, WHO reported that at least more than half a billion of the world population were infected by COVID-19. Initially, global and large cities around the world with high levels of population and connectivity were the epicenters of the virus. However, in a matter of a few months, the disease reached many cities and even rural areas. Despite this, in most countries, urban areas have higher rates of infection than rural areas. National and local governments around the world are introducing initiatives to mitigate the spread of the virus and its effects on the daily life of residents (Rojas-Rueda and Morales-Zamora, 2021). In parallel to finding pharmacological treatments and vaccines to cure and prevent the spread of the virus, the role of non-pharmacological interventions has been increasingly recognized and prioritized. Identifying human and non-human factors of COVID-19 transmission enables policymakers to develop more efficient solutions (Qiu et al., 2021). The literature is enriched with publications that have investigated the effect of the built environment, environmental, health, socio-economic and individual factors on the spread of COVID-19 (Sharifi and Khavarian-Garmsir, 2020). In general, there is an argument that non-pharmacological interventions play a critical role in mitigating COVID-19 transmission (AbouKorin et al., 2021). This study is trying to shed more light on how non-pharmacological variables have affected the spread of COVID-19 through analyzing empirical papers.
From the early days of this pandemic, many studies have analyzed the effects of different human and non-human factors on the spread of the virus (Jha et al., 2021). These studies are conducted in different countries and focus on different scales ranging from neighborhoods, cities, regions, and countries. To synthesize the existing literature, some literature reviews are conducted that examine the role of non-pharmacological driving factors in the spread of COVID-19 and provide solutions and strategies for its control.
Existing literature reviews have analyzed the interlinkages between COVID-19 and built environment factors at various national, regional, and urban scales. These studies could be categorized into three main themes: first, reviews that have analyzed the effect of COVID-19 on settlements and residents, second, reviews that have investigated the effect of environmental factors, planning and design factors, and resident behavior on the spread of the virus, and third, the reviews that have scrutinized the actions that could be done to control the spread of the virus.
The first group of review papers has analyzed the effect of the COVID-19 pandemic and its associated policies and restrictions on settlements and residents. In general, these papers focus on the environmental, social, and economic consequences of the pandemic and policies developed to battle it. For example, Rojas-Rueda and Morales-Zamora (2021) reviewed the empirical papers that investigated the effect of COIVD-19 on transportation behavior and public spaces. They found that policies designed to control COVID-19 reduced human mobility and contributed to better environmental conditions. Similarly, Shortall et al. (2021) reviewed papers that have analyzed the positive social and economic effects of COVID-19 restriction measures. However, both of these papers focus on specific factors without considering the importance of scale.
The second group of review papers focused on the environmental and urban driving factors of COVID-19. These reviews have analyzed environmental factors that may affect the spread of COVID-19. They have reviewed the effects of factors such as urban greenery, temperature, humidity, wind, air and water quality, and indoor environmental conditions on the spread of COVID-19 (Wu, 2021; Teller, 2021; Valsamatzi-Panagiotou and Penchovsky, 2022; Kumar et al., 2021; Weaver et al., 2022). Some of them also have considered some urban factors such as urban morphology, density, housing, health facilities, urban services, and transportation on the spread of COVID-19 (Hussein, 2022; Azuma et al., 2020; Alam and Sultana, 2021). Also, the effect of social variables such as ethnicity, poverty, health insurance, occupation, and socio-economic factors on the transmission of COVID-19 is reviewed in some studies (Brakefield et al., 2022).
The third group of review papers just focused on the actions and policies that could be implemented to control the spread of COVID-19 and mitigate the adverse effect of this pandemic. For example, Sharifi et al. (2021) and Hassankhani et al. (2021) analyzed the importance of smart technologies and the deployment of technological devices to deal with the adverse effects of COVID-19 in cities. These review papers just focused on smartness and technology deployment without mentioning other factors. In a more holistic review, Harris et al. (2022) investigated other urban planning actions that could be done to control the spread of COVID-19 in urban areas.
Overall, these literature reviews have focused on different aspects such as urban planning factors (Hussein, 2022; Rojas-Rueda and Morales-Zamora, 2021; Harris et al., 2022), urbanization (Wu, 2021), density (Zhang and Schwartz, 2020), transport and travel behavior features (Shortall et al., 2021, Shortall et al., 2022), environmental factors (Azuma et al., 2020; Valsamatzi-Panagiotou and Penchovsky, 2022; Kumar et al., 2021; Weaver et al., 2022), smart city deployment (Sharifi et al., 2021; Hassankhani et al., 2021), and social determinants of health (Brakefield et al., 2022). These papers have discussed the driving factors of COVID-19 spread, how this pandemic has affected nature, settlements, and residents, and how urban planning can mitigate the negative effects of the pandemic. Despite this, there are three main gaps in the literature. First, these review papers tend to focus on specific dimensions such as environmental, social, and transport factors and there is a lack of review articles that explore multiple aspects simultaneously. Second, these reviews have not made a distinction between different scales of analysis. Making such a distinction is needed as patterns and dynamics of the spread of the virus could be different across different scales. Third, while Alam and Sultana (2021), Teller (2021), and Weaver et al. (2022) have addressed different dimensions, their results are based on a few papers. Furthermore, they have not followed systematic approaches in their analyses.
To address these gaps, this study reviews and analyzes the built environment and human driving factors of COVID-19 transmission. The current study has three main novelties in comparison to previous studies. First, we have considered different aspects at the same time to be more comprehensive. Second, we have made a distinction between different scales and categorized the papers based on this criterion. Third, this review is systematic, and the results are based on 166 empirical papers to have more reliable outcomes. We aim to review the literature to provide a better understanding of the role of the built environment and human factors in the spread of COVID-19 on different scales ranging from country, to state, county, city, and urban district. The study is guided by two main review questions: First, what human and non-human factors have affected the spread of COVID-19? Second, how the patterns and dynamics of these factors are differentiated on different scales? As explained in the next section, we have conducted a systematic literature review to answer these questions. This synthesis of the literature can be used to develop more effective solutions to deal with current and future pandemics. As this pandemic still is going on (August 2022), it is obvious that despite the medical findings, non-pharmacological interventions are necessary to manage it. Additionally, many urban and regional planning principles are needed to be reassessed to make more resilient settlements in the future. This study provides recommendations for policy-making to understand the effect of different built environment and human factors on the COVID-19 pandemic and to make more resilient cities to future pandemics.
2. Material and methods
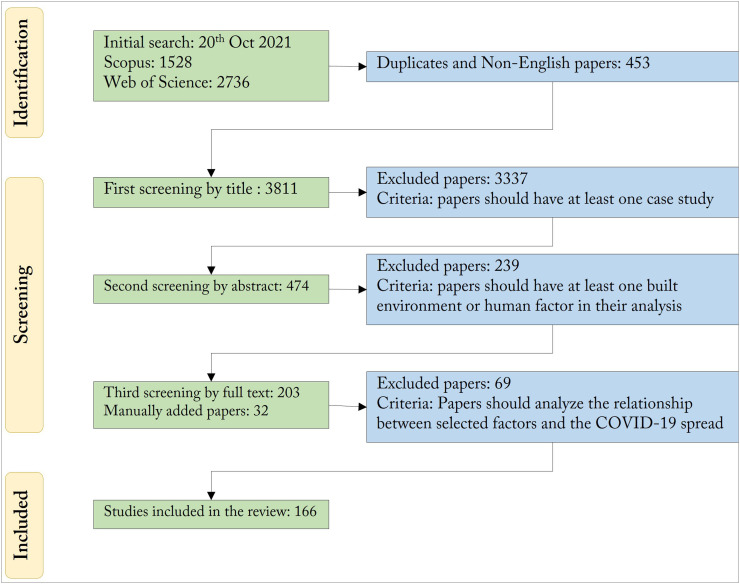
This paper aims to analyze the effects of built environment, socio-economic, and demographic variables on the spread of COVID-19 cases on different scales. To do so, a systematic literature review is conducted to analyze different aspects of the subject. The search string is a combination of different terms related to the topic: “((“built environment” OR “city” OR “cities” OR “neighborhood” OR “county” OR “counties” OR “region” OR “local area” OR “district” OR “urban” OR “town”) AND (“relationship*” OR “association*” OR “effect*” OR “impact*” OR “influence*” OR “connection*” OR “correlation*” OR “co-relation*” OR “link*” OR “inter-linkage*” OR “interlinkage*” OR “inter-connection*” OR “interconnection*”) AND (“COVID-19” OR “COVID” OR “pandemic” OR “epidemic*” OR “coronavirus” OR “SARS-CoV-2”) AND (“attribute*” OR “characteristic*” OR “dimension*” OR “feature*” OR “factor*” OR “variable*” OR “conditions” OR “settings” OR “pattern*” OR “structure*” OR “arrangement”))”. This search was done in two phases on 20 October 2021. Initially, a broad search on the “Web of Science” and “Scopus” databases returned 4264 papers. Through the first screening of the titles, 474 papers were found relevant. The main inclusion criteria in this stage were those papers that have at least one case study and have analyzed the factors affecting the spread of COVID-19. After screening the abstracts of these papers 271 papers were found irrelevant. The papers that did not have at least one built environment factor were excluded at this stage. In the third step, the full texts of 203 papers were reviewed. 134 papers were completely aligned with our review questions (these papers had built environment or human factors, they had case studies and suitable COVID-19 data and analyzed the effects of built environment and human factors on the spread of COVID-19). Also, 32 papers were added manually from other sources such as ResearchGate, the Google Scholar and other databases, and the references cited in the reviewed papers. Finally, 166 papers were relevant to our main review questions and were included in our analysis (see Fig. 1 ). Only empirical papers written in English are included in the final collection All of the screening processes to select the final papers and also the content analysis were done by one of the authors to avoid the bias of selection. For content analysis, we developed a Microsoft Excel sheet and extracted information related to each factor and across different scales. The collected information was later synthesized to report the results presented in the next section. We also conducted a term co-occurrence analysis to understand the thematic focus of the reviewed literature. For this purpose, we used VOSviewer, an open source software tool for bibliometric analysis (https://www.vosviewer.com/).
Fig. 1.
The inclusion criteria and the number of reviewed papers.
3. Results and discussion
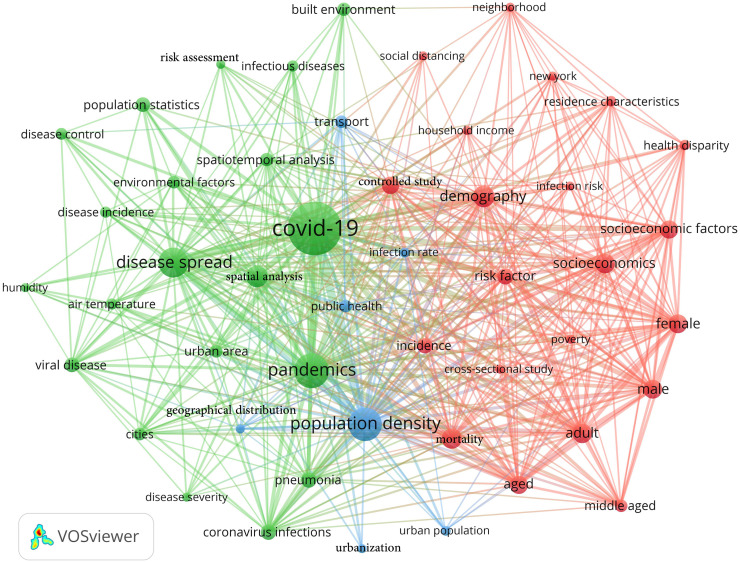
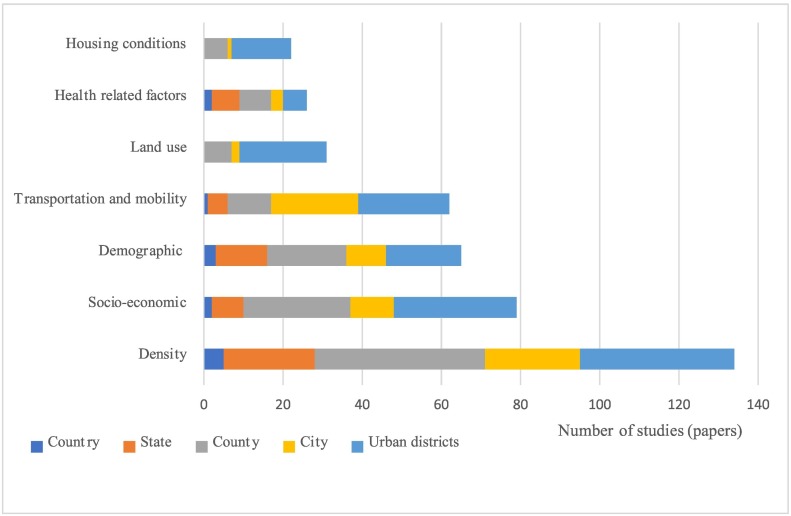
Based on the term co-occurrence map of the reviewed papers (Fig. 2 ) and also the knowledge and judgements of the authors, the results of the reviewed papers are presented in seven main themes. This categorization is also based on the main factors included in the reviewed papers (see Fig. 3 ). Therefore, the current analysis is constructed based on the following factors: density, socio-economic factors, demographic factors, transportation and mobility, housing conditions, land use, and health-related factors. Each factor has several sub-criteria (shown in Table 1, Table 2, Table 3, Table 4, Table 5, Table 6, Table 7, Table 8 ) that explain different aspects of that factor on the country, state, county, city, and urban district scales.
Fig. 2.
The term co-occurrence map of the reviewed papers.
Fig. 3.
The number of papers that examines different factors on different scales.
Table 1.
The number of density criteria included in papers on different scales.
| Criteria | Country | State | County | City | Urban district | Total |
|---|---|---|---|---|---|---|
| Population density | 5 | 23 | 42 | 24 | 36 | 130 |
| Housing density | 0 | 0 | 0 | 0 | 4 | 5 |
| Activity density | 0 | 0 | 1 | 0 | 5 | 6 |
| Transport density | 0 | 0 | 0 | 0 | 5 | 5 |
Table 2.
The effect of density on the spread of COVID-19 on different scales.
| Scale | Positive | Negative | Insignificant | Contrasting | Total number |
|---|---|---|---|---|---|
| Country | 2 | 0 | 2 | 1 | 5 |
| State | 13 | 0 | 9 | 1 | 23 |
| County | 27 | 1 | 11 | 4 | 43 |
| City | 14 | 3 | 5 | 2 | 24 |
| Urban districts | 22 | 5 | 10 | 2 | 39 |
| Total number | 78 | 9 | 37 | 10 | 134 |
| Percentage | 58.20 | 6.71 | 27.61 | 7.46 | 100 |
Table 3.
The number of land use criteria included in papers on different scales.
| Criteria | Country | State | County | City | Urban district | Total |
|---|---|---|---|---|---|---|
| Distance and accessibility | 0 | 0 | 2 | 0 | 3 | 5 |
| Share of land uses | 0 | 0 | 5 | 1 | 7 | 13 |
| POI | 0 | 0 | 0 | 0 | 4 | 4 |
| Density | 0 | 0 | 0 | 1 | 8 | 9 |
| Mixed | 0 | 0 | 0 | 0 | 3 | 3 |
Table 4.
The number of transportation and mobility criteria included in papers on different scales.
| Criteria | Country | State | County | City | Urban district | Total |
|---|---|---|---|---|---|---|
| Infrastructure | 1 | 2 | 3 | 4 | 13 | 23 |
| Internal mobility | 0 | 2 | 4 | 6 | 5 | 16 |
| External mobility | 0 | 2 | 3 | 8 | 1 | 14 |
| Transportation mode | 0 | 0 | 1 | 4 | 7 | 12 |
| Distance to pandemic centers | 0 | 1 | 0 | 7 | 0 | 8 |
Table 5.
The number of housing condition criteria included in papers on different scales.
| Criteria | Country | State | County | City | Urban district | Total |
|---|---|---|---|---|---|---|
| Overcrowding | 0 | 0 | 4 | 1 | 12 | 17 |
| Price | 0 | 0 | 2 | 0 | 3 | 5 |
| Housing type and structure | 0 | 0 | 1 | 0 | 2 | 3 |
Table 6.
The number of demographic criteria included in papers on different scales.
| Criteria | Country | State | County | City | Urban district | Total |
|---|---|---|---|---|---|---|
| Age | 3 | 8 | 16 | 6 | 16 | 49 |
| total pop | 3 | 1 | 4 | 1 | 1 | 10 |
| Urban pop | 0 | 8 | 3 | 3 | 0 | 14 |
| Household size | 1 | 0 | 1 | 0 | 5 | 7 |
Table 7.
The number of demographic criteria included in papers on different scales.
| Criteria | Country | State | County | City | Urban district | Total |
|---|---|---|---|---|---|---|
| Socio-economic status | 2 | 2 | 3 | 7 | 4 | 18 |
| Income and poverty | 1 | 3 | 10 | 3 | 19 | 36 |
| Education | 0 | 2 | 4 | 1 | 10 | 17 |
| Occupation | 0 | 2 | 4 | 2 | 7 | 15 |
| Ethnicity and race | 0 | 0 | 11 | 1 | 15 | 27 |
| Unemployment | 0 | 0 | 3 | 0 | 2 | 5 |
Table 8.
The number of health criteria included in papers on different scales.
| Criteria | Country | State | County | City | Urban district | Total |
|---|---|---|---|---|---|---|
| Health problems | 1 | 3 | 5 | 1 | 3 | 13 |
| Health infrastructures | 1 | 4 | 5 | 3 | 3 | 16 |
3.1. Density
Density is the most critical and problematic issue in urban planning concerning the COVID-19 pandemic. COVID-19 transmits between people through close contact. From the very beginning, density was blamed as it increases the likelihood of transmission. As shown in Table 1 134 out of 166 final reviewed papers have density as a criterion in their analysis. Different types of density such as population, activity, housing, and transport are the most common criteria on all country, state, county, city, and urban district scales.
On the country scale, contrasting evidence has been reported on the effect of density on COVID-19. While some studies found population density as a positive and significant predictor of COVID-19 spread (Gupta et al., 2020; Moosa and Khatatbeh, 2021), Hashim et al. (2020) and Bijari et al. (2021) reported population density as an insignificant factor in explaining the dynamics of COVID-19 cases globally. One of the main reasons could be that population density on the country scale is not a reliable factor. Because two countries with the same population and area might have different types of population distribution.
On the state scale, 23 papers included different types of density in their analysis. As population density is easier to calculate, most of them used this variable instead of other types of density. Based on our review, many studies conducted in countries such as the US (Sarmadi et al., 2021; White and Hébert-Dufresne, 2020), Italy (Ilardi et al., 2020), Iran (Ahmadi et al., 2020), Bangladesh (Sharif et al., 2021; Alam, 2021; Rahman et al., 2021), Oman (Al Kindi et al., 2021), France (Tchicaya et al., 2021), Nigeria (Bayode et al., 2022) and Scotland (Rideout et al., 2021) found population density as a positive and significant predictor of COVID-19 cases on state scale. However, about 40 % of studies reported that population density is not a significant factor to explain the difference in COVID-19 cases in different states (Ramírez-Aldana et al., 2020; Gupta et al., 2020; Perone, 2021; Gargiulo et al., 2020; Basellini and Camarda, 2021; Pilkington et al., 2021; Sen-Crowe et al., 2021).
The highest number of papers that included population density in their analysis is on the county scale (as shown in Table 1). About 63 % of documents on this scale found population density as a driving force of COVID-19 spread (Wong and Li, 2020; Kim et al., 2021; Aw et al., 2021; Jo et al., 2021; Qeadan et al., 2021; Q. Li et al., 2021; Lee et al., 2021). It is worth mentioning that 17 out of 27 of these papers were conducted in the US. More than 25 % of papers reported that population density is not a significant predictor of the spread of the virus on this scale (Barak et al., 2021; Boterman, 2020; Mollalo et al., 2020; Nguyen et al., 2020; Ramírez-Aldana et al., 2020; Barak et al., 2021; Klompmaker et al., 2021). The majority of these studies also were conducted in the US. In general, as COVID-19 data in the US is released on county scale majority of studies are done on this scale. Some studies in the US (Ruck et al., 2021), China (Xiong et al., 2020), Zambia (Phiri et al., 2021) and Germany (Steiger et al., 2021) had reported mixed results regarding the effect of population density on COVID-19 cases on county scale. They showed that this effect is positive in some specific times but not significant in others. Hamidi et al. (2020a) was the only analysis on this scale that found population density as a negative predictor of COVID-19 in the US.
As can be seen in Table 2, about 18 % of the papers considered density as a factor to explain the spread of COVID-19 on the urban scale. The majority of these papers found that cities with higher population densities have a higher rate of COVID-19 cases. Such claims were reported from different countries such as the US, China, Israel, Brazil and other parts of the world. By contrast, three studies conducted in China found that a lower rate of cases was reported in cities with higher population density (Zhang et al., 2021; Qiu et al., 2020; Q. Li et al., 2021). It should be noted that China had imposed stringent mobility restrictions in the early months of COVID-19 and the result of studies in China couldn't be generalized. For example, some studies that included all Chinese cities reported population density as an insignificant variable (Qiu et al., 2021; Lin et al., 2020). Similar results were reported for cities in Iran (Khavarian-Garmsir et al., 2021), US (Almagro and Orane-Hutchinson, 2020; Spotswood et al., 2021; Tieskens et al., 2021; Hamidi and Hamidi, 2021), Italy (Consolazio et al., 2021; De Angelis et al., 2021) and Pakistan (Mehmood et al., 2021).
The finest scale of analysis that included density as an influential factor to explain the spread of COVID-19 is the urban district. From an urban planning perspective, the most reliable definition of density could be grasped on this scale as different types of density such as population, jobs, buildings, and businesses are meaningful on this scale (B. Li et al., 2021). Around 30 % of the reviewed papers are conducted on urban district or neighborhood scales. While about 56 % of these papers found density as a positive and significant predictor of COVID-19 cases, this is the lowest among different scales (Verma et al., 2021; Hao et al., 2020; Nasiri et al., 2021; Han and Jia, 2021; Xu et al., 2022). However, about 13 % of papers found that areas with higher population density have a lower infection rate in cities like New York (Tribby and Hartmann, 2021; Credit, 2020), Hong Kong (Huang et al., 2020), London (Sun et al., 2021) and Fortaleza (Cestari et al., 2021). Also, more than 25 % of papers on this scale found that population density is not a significant factor in explaining the spread of COVID-19 in urban areas (Consolazio et al., 2021; Hamidi and Hamidi, 2021; Khavarian-Garmsir et al., 2021; Spotswood et al., 2021; Almagro and Orane-Hutchinson, 2020). In general, there is no sufficient evidence to prove that neighborhoods with higher population density necessarily have a higher infection rate.
As shown in Table 2, the highest share of papers that included density in their analysis was on the county scale (43 papers). On the other hand, about 71 % of papers on the urban district scale used density as a factor to explain the dynamics of COVID-19 transmission. In general, about 5 % of papers have found density as a significant factor, while in about 27 % of reviewed papers this factor was insignificant. Also, around 7.5 % of papers reported a contrasting impact of density on the spread of COVID-19. The result of our analysis showed that the impact of density on COVID-19 cases and deaths is not straightforward. While it has been discussed in the literature that density is a driving force for the higher rate of COVID-19 cases, about 42 % of papers didn't support this hypothesis. The differences between the impact of density on COVID-19 cases on different scales show that density is highly scaled dependent. Some papers have found density as a positive and significant factor to explain the spread of COVID-19 but this factor had a high level of multi-collinearity and they excluded it in their final model (Rahman et al., 2021; Al Kindi et al., 2021). Therefore, it can be said that density is an easy-to-calculate factor and that is why it has been used in different papers. But as this factor is context and scale-dependent, the results should be interpreted cautiously.
3.2. Land use
Urban land use is one of the most influential factors to manage the dynamics of population and employment in cities. Allocation of land to different functions impacts the mobility, congestion, and distribution of population through space. COVID-19 transmission could be affected by how different land uses are distributed in the city. A variety of land use factors are used in the literature to explain how this dimension has affected the spread of COVID-19 cases in urban areas. Thirty one out of the 166 reviewed papers had land-use factors in their analysis. These are focused on the county (7), city (2), and urban district (22) scales (as shown in Table 3). The result of our review showed that land-use variables include 1. share of different land uses such as roads, open and green spaces (Hassan et al., 2021; Kwok et al., 2021), 2. density of different land uses such as restaurants and clinics (Ma et al., 2021; Huang et al., 2020, Huang et al., 2021), 3. accessibility to different land uses such as commercial and educational (Verma et al., 2021; Sun et al., 2021), 4. the mixture of land uses (Li et al., 2020; Wali and Frank, 2021) and 5. Point of Interest (POI) for different land uses (Xu et al., 2022; B. Li et al., 2021).
Share of different land uses (specifically green and open spaces and roads) in a zone or a city is one of the most common variables employed in reviewed papers. On county scale, urban greenery and green infrastructure were negatively associated with the number of cases in the US, UK and Poland (Ciupa and Suligowski, 2021). There is an argument that there might be some clinical and health-related factors beyond just greenness but exposure to green spaces potentially increase the immunity to any disease by encouraging physical activity (Russette et al., 2021; Lee et al., 2021). While green spaces might increase the mobility of the population and accordingly higher number of cases, Johnson et al. (2021) discussed that using parks and other green spaces might be a good option against for example shopping. In the case of the US, this impact is more significant in counties with higher population density and is differentiated by season (Klompmaker et al., 2021). On city scale, Lata et al. (2021) reported an opposite result about the effect of green spaces on the number of cases in 321 Indian cities. The effect of natural areas on the number of cases was positive and significant. However, this result is just based on a simple correlation analysis and it needs more supplementary pieces of evidence to reach this conclusion.
On the urban district scale, the results were contrasting. In the case of Shenzhen, green space coverage was not a significant factor to explain the variation in COVID-19 cases (C. Liu et al., 2021). Nguyen et al. (2020) and Spotswood et al. (2021) found green spaces as a negative predictor of COVID-19 cases. The same result was reported for the case of King County in Washington (C. Liu et al., 2021). However, You et al. (2020) showed that public green space density is associated with a higher number of cases in the early days of the COVID-19 pandemic in Wuhan. Similarly, Huang et al. (2020) reported a positive association between green space and COVID-19 cases in Hong Kong. The main reason for this result was that green spaces encouraged outdoor activity and accordingly higher contact density.
Accessibility to land uses is another factor that affects the number of cases in urban areas. This factor is just studied on the urban district scale. Accessibility could also be explained by factors such as proximity and distance to facilities. Han et al. (2021) found that Distance to business, parks, shops, and education were positively and significantly associated with the number of cases in Beijing. Distance to the Xinfadi market was the most dominant as this market was known as one of the epicenters of the outbreak. The positive effect of distance to hospitals, public transportation stations, pharmacies, and large supermarkets on COVID-19 cases was also reported for cases in London and Tehran (Razavi-Termeh et al., 2021; Sun et al., 2021). You et al. (2020) discussed that as large retail stores are hot spots of COVID19 cases, the distribution of small retail stores through residential areas could mitigate this effect.
The impact of land use on the spread of COVID-19 is also measured by density and POIs. Higher density of specific land uses such as supermarkets, commercial land uses, clinics, hospitals, administrative, schools, shopping centers, and restaurants are found as the positive and significant predictors of COVID-19 cases in Tehran, Hong Kong, New York, Chicago, Wuhan and Huangzhou (Ma et al., 2021; Nasiri et al., 2021; Li et al., 2020; Lak et al., 2021; Huang et al., 2021, Huang et al., 2020; Yip et al., 2021). The high density of these land uses will contribute to higher POI and accordingly a higher rate of COVID-19 cases (Xu et al., 2022; B. Li et al., 2021). Verma et al. (2021) analyzed the effect of land uses based on trips' destinations. They found that schools and restaurants were the most visited places. Additionally, Niu et al. (2021) found that the effect of land uses on the number of infected people is differentiated by age. For example, shopping centers were a significant factor for zones with a higher number of aged people than zones dominated by younger populations. In general, it can be said that land uses that attract more customers could potentially contribute to a higher rate of COVID-19. The recommendation from the literature is that land uses should be distributed in cities in a more balanced manner and should not be concentrated in specific areas.
Mixed land use is a sustainable planning instrument on the local scale that is analyzed in three reviewed papers. S. Li et al. (2021) and Sun et al. (2021) reported a negative and significant association between mixed land use and the COVID-19 rate in Chinese cities and London, respectively. They discussed that mixed land use reduces the need for long travel and leads to a lower rate of mobility. That is the main reason that these neighborhoods and cities have a lower rate of COVID-19 cases. Similarly, Wali and Frank (2021) found mix land use was a negative predictor of COVID-19 cases in 397 districts of King county. They also discussed that mixed land use neighborhoods are more walkable and bikeable which reduces the spread of the COVID-19 virus.
3.3. Transportation and mobility
Basically, COVID-19 is transmitted through the mobility of the population globally and locally (S. Li et al., 2021). In the literature, population mobility is calculated by different criteria such as internal and external movement of the population, mode of transportation, the share of transportation infrastructures, and distance from major pandemic centers. Based on our review, 62 papers have included at least one of the factors of transportation and population mobility on the country (1), state (5), county (11), city (22), and urban district (23) scales (see Table 4). It shows that transportation and mobility variables have more common on lower scales, irrespective of the factors that are included.
COVID-19 initially appeared in China and was transmitted to other countries through international population mobility. Therefore, one of the main factors used to analyze the mobility of the population is transportation infrastructure and its physical characteristics. Sigler et al. (2021) analyzed the effect of international airports on the spread of COVID-19 cases in 84 countries. The result of their analysis showed that more developed countries that have more globalization features and are more connected to other countries had a higher rate of infection in the first period. Then, hierarchically the virus transmits to lower developed countries. Transportation infrastructures mainly appeared in papers on a lower scale such as urban districts. On the state scale, the number of high-speed railways in China increased the number of cases (Z. Hu et al., 2021), while Bayode et al. (2022) reported no significant relationship between COVID-19 cases and international airports. On the county scale, in Zambia, the number of cases increased due to closeness to airports (Phiri et al., 2021) but in the case of Germany and South Korea, the physical characteristics of transportation infrastructures were not significant factors (Scarpone et al., 2020; Jo et al., 2021). Transportation infrastructures' effect on COVID-19 transmission at the urban district level showed a mixed result. Walkable and physically well-designed sidewalks are associated with a lower number of cases on the neighborhood scale (Kwok et al., 2021; Credit, 2020; Tribby and Hartmann, 2021; Nguyen et al., 2020). However, urban districts with a higher density of transportation facilities such as bus and train stations increased the likelihood of COVID-19 spreading in Tehran (Razavi-Termeh et al., 2021; Khavarian-Garmsir et al., 2021), Hong Kong (Kan et al., 2021; Huang et al., 2020) Wuhan (Xu et al., 2022; Niu et al., 2021) and Huangzhou (B. Li et al., 2021).
Internal and external mobility of population on state, county, and urban scales is another common variable to analyze the spread of COVID-19. The result of studies in Iran, France, and Mexico shows that population mobility, internally and externally, plays a significant role in a higher number of cases on the state scale (Ahmadi et al., 2020; Ramírez-Aldana et al., 2021; Pilkington et al., 2021). As was expected, the higher rate of mobility is a significant predictor of COVID-19 cases on the County scale (Jamshidi et al., 2020; Niu et al., 2020; Tokey, 2021). However, the distinction between different purposes of mobility is necessary for applying restrictions. While population movement in the city for shopping and recreational activities might increase the number of cases (Steiger et al., 2021), visiting green spaces was a negative predictor of COVID-19 cases in 299 UK local authorities (Johnson et al., 2021). Studies on urban scale have made a clear distinction between inter and intra-city mobility of the population and they mainly discussed that the internal movement of the population is not a significant factor but the mobility of the population between cities is a positive predictor (Feng et al., 2020; Ma et al., 2021; J. Liu et al., 2021; Zhu et al., 2020). Studies in Washington (M. Hu et al., 2021), Barcelona (López-Gay et al., 2022) and Beijing (Hao et al., 2020) also emphasized the negative impact of work and recreation commuting on the spread of COVID-19 cases.
The mode of transportation is another factor that affects the spread of COVID-19 cases in urban areas. This factor was used just on city and urban district scales. As places with higher contact density are the hot spot of COVID-19 cases, those who use public transportation such as buses and trains would be more likely to be infected. In the literature, the share of trips by trains and buses was positively associated with the number of cases (De Angelis et al., 2021; Villalobos Dintrans et al., 2021; Thomas et al., 2022). In contrast, the share of private car riders was negatively associated with the number of cases (Lata et al., 2021). A mixed result is reported on the urban district scale regarding the mode of transportation. While some studies have shown that a higher rate of public transport use is associated with a higher number of cases (Cordes and Castro, 2020; Guo et al., 2021; T.-C. Yang et al., 2021), Bryan et al. (2021) found using public transport is an insignificant predictor of COVID-19 cases. Furthermore, commuting to work by bicycle and walking are also correlated with a lower number of cases in those neighborhoods (Tribby and Hartmann, 2021; Guo et al., 2021; Wali and Frank, 2021). Worthy to mention that studies conducted in China showed that distance and connectivity to the pandemic epicenters, specifically Wuhan, are strong, significant and positive predictors of COVID-19 cases (Z. Hu et al., 2021; Qiu et al., 2020, Qiu et al., 2021; Lin et al., 2020; X.-D. Yang et al., 2021).
3.4. Housing conditions
COVID-19 spread is highly influenced by the exposure of the population to infected people. For two main reasons, housing conditions may affect the transmission of the virus. First, isolating infected people is a way of controlling the spread of the virus and households need more spaces to quarantine their infected family members Consolazio et al. (2021). Secondly, governments imposed restrictions to control the spread of the virus and families were forced to stay at their places for some days or weeks. So, having enough space to work, rest and spend time with family members became a necessity. People who were living in small places complained regularly about the lack of enough space and they were forced to go out and it was increasing the possibility of being infected (Whitaker, 2021).
Various studies have considered housing conditions as driving forces that influenced the transmission of the COVID-19 virus. The criteria of this factor were differentiated based on the availability of data but the most common ones were overcrowding index (number of people per house area or per room), price (renting and land and housing price), and housing types and structure (apartments, detached houses, etc.). Out of 166 reviewed papers, 24 considered housing condition factors as an influential driving force that we categorized them, as shown in Table 5, in three main criteria; overcrowding, housing price and housing types and structures.
Housing overcrowding was the most common criterion that emerged in 17 papers mainly on city and urban district scales. The effect of overcrowding on the number of cases was completely consistent throughout the literature. All of them found overcrowding as a positive and significant predictor of COVID-19 cases (Lee et al., 2021; Wang et al., 2021; Gaglioti et al., 2021; Credit, 2020; Ghosh et al., 2021). Even some studies found that overcrowding has significant effects on the death rate in the county (Lee et al., 2021; Nguyen et al., 2021; Ahmad et al., 2020) and urban district scales (Urban and Nakada, 2021; Silva and Ribeiro-Alves, 2021; Z. Hu et al., 2021). The main reason for this result is that in overcrowded households people have limited space to follow the protocols and avoid having contact with other family members (Consolazio et al., 2021; Kashem et al., 2021).
Other housing condition criteria such as housing types, size, amenities, and rent price also are reported as significant driving forces of COVID-19 spread. In general, housing quality is highly associated with the number of deaths, even by controlling other social factors such as race and ethnicity (M. Hu et al., 2021). The same was reported in the case of Rio De Janeiro for different periods of time (Silva and Ribeiro-Alves, 2021). Housing problems such as lack of basic infrastructures during lockdowns increased the number of infected people in counties with lower income groups (Nguyen et al., 2020). Ahmad et al. (2020) also found that a 5 % increase in the share of households with housing problems is associated with 50 % of higher COVID-19 infection and 42 % of mortality risk in US counties. The more important problem is that those vulnerable communities (such as minorities) are more likely to be infected due to various socio-economic factors and housing problem is at its highest level in these social groups (Credit, 2020). Another housing condition factor that affects the spread of COVID-19 cases is housing rent or price (Bryan et al., 2021). Cordes and Castro (2020) revealed households that pay more than 50 % of their income for renting a house have more positive cases in New York City. The last housing condition factor was the size of the place (C. Liu et al., 2021). Nasiri et al. (2021) found that the number of cases in households who live in apartments less than 100 square meters has a higher number of cases.
While introducing restriction measures will practically reduce the transmission of the virus in urban areas, housing conditions become more problematic in these periods. Characteristics of housing could be a critical factor to explain the disparity in COVID-19 morbidity and mortality rate in urban areas (Ghosh et al., 2021). Policymakers need to consider the impacts of overcrowding, unhealthy housing conditions, and housing costs when implementing restriction measures.
3.5. Demographic factors
Demographic criteria such as total population, the age structure of communities or vulnerable populations, urban or rural populations, and household size are among the most common ones studied in relation to COVID-19 spread on different scales. Based on our review 65 papers on the country, state, county, city, and urban district scales have considered these criteria in their analysis (see Table 6).
As the health condition of residents is attributed to their age, older people are more vulnerable to being affected by this virus. So, the age structure of the community is a criterion that is applied in 49 papers to understand the dynamics of COVID-19 spread. There is a confusing point in the literature regarding the effect of the age population. While older age groups are more vulnerable to this virus, young people are more likely to be infected as the exposure of these age groups to the virus is highly more than other age groups. In most of the reviewed papers, in the areas where the share of the population aged 60, 65, or 70 is higher, the number of cases is higher. This issue is not sensitive to the scale, as the results of studies on the country (Sigler et al., 2021; Bijari et al., 2021), state (Basellini and Camarda, 2021; Tchicaya et al., 2021; Ramírez-Aldana et al., 2020), county (Kodera et al., 2020; Hamidi et al., 2020b; Wu and Zhang, 2021), city (Tieskens et al., 2021; Pequeno et al., 2020) and urban district (Chan et al., 2021; López-Gay et al., 2022; Urban and Nakada, 2021) scales show the same outcomes. However, Ilardi et al. (2020); Boterman (2020) and Mondal et al. (2022) found age as an insignificant predictor of COVID-19 and Johnson et al. (2021) showed that the population over 70 is a negative factor and reduces the number of cases in 299 local authorities in the UK. It is worth mentioning that the number of people who live in the household was not a very common criterion (applied in just 9 papers) in the reviewed papers but all of them found the size of the household as a driver of COVID-19 spread (Sigler et al., 2021; Wheaton and Kinsella Thompson, 2020; Almagro and Orane-Hutchinson, 2020; Kashem et al., 2021; Urban and Nakada, 2021).
The majority of infected people are living in urban areas with a high share of the population. Therefore, two main criteria were applied to reflect these issues: total population and urban population. The total population criterion was mainly used in papers on higher scales to compare countries (Sigler et al., 2021), states, and counties (Wheaton and Kinsella Thompson, 2020). The result of their analysis showed that the population size of an area is a significant and positive predictor of COVID-19 (Bijari et al., 2021; Wu and Zhang, 2021; Jamshidi et al., 2020; Niu et al., 2020). Urbanity or rurality or the share of the urban population was also a critical factor to explain the dynamics of COVID-19 spread. 14 out of 164 papers included this criterion in their analysis on state, county, and city scales. The result of our review showed that the urban population in France (Pilkington et al., 2021; Tchicaya et al., 2021), Iran (Ramírez-Aldana et al., 2020), Bangladesh (Alam, 2021), and the US (Qeadan et al., 2021) increased the number of cases. However, reports from Italy (Perone, 2021), the Netherlands (Boterman, 2020), and China (Chu et al., 2021) found an insignificant effect of urbanization on COVID-19 spread. Additionally, in two Brazilian (Ribeiro et al., 2020) and Chinese (X.-D. Yang et al., 2021) studies city size was a positive predictor of cases.
3.6. Socio-economic factors
Socio-economic characteristics of communities, directly and indirectly, affect the spread of COVID-19 cases. Epidemiological studies have also confirmed that the socio-economic status of the population affects the likelihood of being infected with the COVID-19 virus. Out of 166 reviewed papers, 77 unique studies included socio-economic criteria (Table 7). Based on the literature different aspects of the socio-economic characteristics of communities are analyzed including socio-economic status (GDP and HDI), income and poverty, education level and literacy, ethnicity, race and religion, and unemployment rate. Most of these studies are conducted on the county (26) and urban district scales (30) which mainly is due to the availability of data on these scales. Among the socioeconomic criteria, income and poverty and ethnicity and race were the most repeated ones by 35 and 27 papers, respectively.
GDP represents the value added by a country, state, county or even a city. It has been argued that this factor indirectly influences the spread of COVID-19. The majority of the papers found that countries, regions, counties, and cities with a higher GDP, have a higher rates of infection. On the country scale, two papers have investigated GDP and HDI and their influence on COVID-19 spread. Hashim et al. (2020) analysis of 93 countries found that the socio-economic development of countries is not a significant factor in COVID-19 case fatality. Sigler et al. (2021) discussed that HDI is a significant predictor at the beginning but after countries impose restrictions, globalization factors became a significant factor. On the state scale, Gargiulo et al. (2020) and Ramírez-Aldana et al. (2021) both found that GDP is positively and significantly associated with the number of cases in Italy and Mexico, respectively. On the county scale, Xiong et al. (2020) revealed that GDP was positively and significantly associated with the number of COVID-19 cases in China. But, the same analysis in the US counties showed that GDP had different levels of significance during different times of the pandemic. GDP was not a significant factor in counties clustered by high population density (Q. Li et al., 2021). The association between GDP and COVID-19 case rate on the city scale is contrasting. The result of research conducted on Chinese (X.-D. Yang et al., 2021; Qiu et al., 2020, Qiu et al., 2021; Zhang et al., 2021) and Turkish (Baser, 2021) cities all have shown that GDP increases the number of cases. While in the case of Brazil this relationship is insignificant (Nakada and Urban, 2021), Ahmed et al. (2021) reported a negative association between GDP per capita and the rate of COVID-19 cases in 70 cities throughout the world. As GDP is mainly defined on urban, regional or national scales, just one study included this factor on the urban district scale in Shenzhen. GDP was a significant and positive predictor of COVID-19 cases among 10 districts of Shenzhen (Liu et al., 2020).
Income-related criterion represents another aspect of socio-economic characteristics of communities that affect COVID-19 morbidity and mortality rate. 36 papers have included income as a factor to explain the dynamics of COVID-19 cases. As the data for this variable is available for most cities, income is the most common socio-economic factor repeated in reviewed papers (Bayode et al., 2022). The result of our review showed that income is employed on all state, county, city, and urban district scales. On the state scale, poverty and income were not significant factors to explain the variation in COVID-19 rate of infection and death in studies conducted in the US, France, Nigeria, and Bangladesh (White and Hébert-Dufresne, 2020; Bayode et al., 2022; Tchicaya et al., 2021; Rahman et al., 2021). On the county scale, income just appeared in the papers conducted in the US and the results seem to be contrasting. Regarding COVID-19 incidence, income was a strong and significant predictor (Qeadan et al., 2021; Wheaton and Kinsella Thompson, 2020; Wang et al., 2021; Mollalo et al., 2020). Wheaton and Kinsella Thompson (2020) discuss that as socializing and other face-to-face activities of residents are elastic to income, there are higher cases in wealthier households. This conclusion was confirmed by Wang et al. (2021) and Mollalo et al. (2020) but they also included income inequality as a predictor and in both cases, this factor was positively and significantly associated with the number of cases. When it comes to the death rate, Ali et al. (2021) didn't find a clear relationship and they just referred to the results of Mollalo et al. (2020). This Referencing is misleading because Mollalo et al. (2020) didn't find a significant relationship between income and death rate. Iyanda et al. (2021) found a negative association between the number of cases/deaths and income. Interestingly, Sen-Crowe et al. (2021) found a weak, positive and significant correlation between the share of cases of death and income. Poverty was another factor included in three papers conducted in the US. Nguyen et al. (2021) showed that the share of children in poverty is a positive and significant predictor of COVID-19 cases. They discussed that these families have low incomes and they are mainly essential workers. Similarly, Fielding-Miller et al. (2020) showed that poverty is positively associated with the death rate in US counties. However, poverty in New York State was not a significant predictor of COVID-19 cases (Mondal et al., 2022).
Occupation of residents became a very critical issue during the COVID-19 pandemic and 15 studies in our reviewed papers considered this factor in their analysis. On the state scale, in two studies in Bangladesh, the number of health workers was a positive, and the number of industrial workers was a negative predictor of COVID-19 incidence rate (Sarkar et al., 2021; Rahman et al., 2021). On the county scale, in India, marginal workers were associated with a higher number of cases (Tamrakar et al., 2021). In the US, farm workers were contributing to a higher rate of death (Fielding-Miller et al., 2020), while workers in professional, scientific, and technical services had a lower rate of infection (Wang et al., 2021). The unemployment rate on this scale was not the same in all papers. Regarding the death rate, unemployment was a positive predictor Qeadan et al. (2021). When it comes to case rate, Scarpone et al. (2020) and Wang et al. (2021) reported negative and Wu and Zhang (2021) found positive associations between unemployment rate and COVID-19 cases rate.
3.7. Health-related factors
COVID-19 was an infectious virus with a high level of transmission. However, one of the critical factors to deal with the virus was the immune system of the body and how it is supported. So, two main health-related factors in the literature were commonly used (26 out of 164 papers): the health condition of residents and the distribution of health infrastructures and services (as shown in Table 8). The health condition of residents is measured by the share or number of people who suffer from diseases such as chronic disease, diabetes, obesity, depression, and other mental and physical diseases. Most of these studies have analyzed the effect of health conditions on mortality rather than morbidity. The study conducted by Hashim et al. (2020) found that, in different countries, higher rates of lung cancer and Alzheimer is associated with higher rates of death. The same results were reported for France (Moosa and Khatatbeh, 2021) and Mexico (Ramírez-Aldana et al., 2020) states and the US counties (Ali et al., 2021; Nguyen et al., 2021). They found that states and counties with a higher rate of diabetes and obesity have higher rates of COVID-19 infection and death. Chronic diseases also were significant factors in urban districts in Milan (Consolazio et al., 2021), Chicago (Bryan et al., 2021), and Hong Kong (Liao et al., 2021).
As explained, the distribution of healthcare services, facilities, and infrastructures affect the spread of the COVID-19 virus. 16 out of 164 reviewed papers included these factors in their analysis. Moosa and Khatatbeh (2021) found that the healthcare system of countries plays a critical role in mortality rate even in the countries with a low rate of infection. In general states and counties with better health services such as hospital beds, doctors, ICU beds, and primary medical services have a lower rate of mortality (Lee et al., 2021; Basellini and Camarda, 2021; Pilkington et al., 2021). However, this effect is mixed for the number of cases. Health services might be a positive (Gargiulo et al., 2020) or insignificant predictor of COVID-19 cases on a higher scale, but on the city scale, it is a negative predictor (Zhang et al., 2021; Qiu et al., 2020; Lata et al., 2021).
4. Summary and concluding remarks
Since the emergence of the COVID-19 pandemic, researchers have made efforts to better understand its patterns and dynamics and develop solutions to control its spread. In parallel to pharmacological and medical efforts, many studies have focused on non-pharmacological solutions. Through the review of the literature, the current study attempted to find the key built environment and human factors affecting the spread of COVID-19 and its severity on different scales. Based on our review, the seven main factors influencing the spread of COVID-19 include density, land use, transportation and mobility, housing conditions, demographic factors, socio-economic factors, and health-related factors. Each of these factors has several sub-criteria that explain how different factors affect COVID-19 transmission. The main finding of this analysis is that the effects of the built environment and human factors on the transmission of COVID-19 are differentiated spatially and temporally. In other words, while factors might be positively associated in one city or one scale, they could be insignificant or negative in another city or scale. However, we found some significant factors that their effects are consistent throughout the literature. The details of these factors and their effects are presented in Table 9 . It is worth mentioning that contrasting evidence has been reported on the effect of density, as the most commonly studied factor in the literature. The share of papers that have found density as a positive factor is at the highest on the county scale (62 %). But in urban districts, 56 % of papers found density as a positive predictor. It means as the scale changes, the results vary.
Table 9.
Summary of the findings and planning/policy recommendations.
| Factor | Effects on COVID-19 spread | Planning and policy recommendations |
|---|---|---|
| Density | Depending on the scale and context, contrasting evidence has been reported on the effects of density on the spread of COVID-19. However, the congestion of people, facilities and activities in specific areas increase the transmission of the virus. | Compact city is advocated as a sustainable form of development. Based on the fact that it may increase the spread of COVID-19, to maintain interest in compact cities, the densification should be supplemented by other policies such as increasing the walkability and open and green spaces and reducing the distance between work and home. |
| Land use | The mixing of different land uses may not be a significant factor. However, the high density of specific land uses such as restaurants and bars, hospitals and clinics, shopping centers and recreational facilities, and transportation infrastructures positively affect the spread of COVID-19. | Mixing different land uses can reduce the mobility of the population that reduces the transmission of viruses. However, it is of great importance to not concentrate all land uses in specific places such as central areas. The distribution and decentralization of land uses will help residents access their needs at shorter distances and times. Accordingly, it could reduce the spread of COVID-19 in cities and regions. |
| Transportation and mobility | Public transportation and stations were among the most significant and positive contributors to COVID-19 spread on different scales. Higher connectivity to large cities (that are the epicenters of the pandemic) increases the chance of transmission to smaller cities. | It is undeniable that using private car is associated with lower rate of COVID-19. However, it should be considered that post-COVID mobility should feature a balance between sustainability and public health. Therefore, we recommend finding solutions to reduce overcrowding in public transportation, instead of relying on car-dependent mobility in urban regions. |
| Housing conditions | While different factors of housing conditions such as facilities and price may have effect of the spread of COVID-19, overcrowding is the most consistent factor that is associated with higher rates of cases in all scales. | Housing condition is one of the most critical factors that planners and policymakers should pay attention to. New building development policies and regulations should consider provision of appropriate per capita living spaces, albeit based on the context. Also, remote working has now become more common and the need for more flexible housing design layouts should be considered in building permissions and guidelines. |
| Demographic factors | In general, cities or regions with higher share of aged population and household size are more vulnerable to COVID-19 cases. Additionally, more urbanized regions have higher rate of COVID-19 cases based on the current review. | As demographic features of the cities and regions affect COVID-19 spread, we recommend that restrictions and other policies be implemented based on demographic features. For example, a map of population vulnerability be provided, and policies be implemented in cities with higher rates of vulnerable social groups. |
| Socio-economic factors | Contrasting evidence has been reported for the effects of socio-economic factors such as poverty, income, and education in different contexts. However, social inequalities and the share of vulnerable groups and minorities are associated with higher rates of COVID-19 cases. In contrast, employees with higher chance of working remotely reduce the chance of transmission. | Governments need to have more supportive policies for socially vulnerable groups such as minorities as they may not be able to have a decent life if they want to comply with the mobility restrictions. Moreover, remote working is a new working culture that reduces the spread of the virus. We recommend that businesses provide the facilities for flexible working to allow implementing mobility restriction when needed. As mentioned earlier, the needs and requirements of remote working should also be considered in land use planning and housing design. |
| Health-related factors | The regions and cities with better access to health facilities may not have a lower rate of infection but have a lower rate of mortality. Also, health condition of residents, specifically aged population, is a key predictor of infection and mortality rates. | For national government policy makers, we recommend considering accessibility as a key factor and not just emphasize the per capita standard. For planners and designers, we recommend introducing and implementing policies that encourage physical activity in the neighborhoods. |
Our analysis highlights that the scale of analysis is highly important. While, for example, on the county scale population density might be positively associated with the number of cases, contrasting results were observed on the urban scale. Additionally, each factor should be clearly defined before making a conclusion. For example, accessibility to hospitals and medical services might be a negative predictor of COVID-19 cases but it increases face-to-face interactions in the approximate neighborhoods, thereby increasing the possibility of transmission. Population density is another example that should be defined based on a clearer logic. Urban density and population density are not the same, and most of the reviewed papers didn't make a distinction between them.
Current research provides insights for policy-making and research on both public health and built environment planning. The results show that some urban planning concepts such as housing quality play a critical role in promoting public health. Therefore, it is of great importance to revisit housing standards, specifically in large cities, to improve housing conditions such as the area per person. Additionally, public transportation as a critical principle of sustainable development accelerated the spread of COVID-19 cases in many cities. It is necessary to improve the quality of public transport in parallel to its efficiency. Moreover, accessibility to different land uses and services contributes to lower mobility of the population and consequently lower transmission of viruses. Alongside that, minorities and low-income social groups were more vulnerable to the health and economic effects of the pandemic. More social and economic support is needed for vulnerable populations in times of crisis. From a research perspective also the result of our analysis showed that many established planning principles and sustainable development policies are under question. For example, there are some pieces of evidence that areas with lower population density and higher rates of private car use have lower rates of COVID-19 cases. Therefore, sustainable development policies and other planning approaches should be justified based on the new situations.
This research was intended to be comprehensive, including different factors and scales. While this approach provides a better insight into the whole non-pharmacological factors, we were not able to scrutinize the subject on different scales. We suggest that future studies focus on these factors on specific scales and critically analyze each factor concisely. More importantly, the time span of this study was from the beginning of the pandemic till October 2021. As it is discussed in different sections, many papers published in the first year were methodologically and theoretically premature. We suggest follow-up studies with revised and more robust methodological approaches to understand if the results still hold. This enables researchers to provide a more evidence-based framework applicable to planning and policy-making. Moreover, due to the limitations of our study, the results are categorized based on the scale and factors included in the papers. We propose a cross-sectional and temporal literature review to understand how influential factors are differentiated through space and time. Additionally, this review is constructed based on peer-reviewed published papers in English. Future studies can include a broader range of sources and other languages to provide more robust findings. Finally, factors included in most of the reviewed papers are highly correlated. However, a few of them methodologically considered these issues in their analysis. For example, areas with high building and population density have smaller houses in comparison to suburban areas. In this case, population density and overcrowding are both predictors of COVID-19 spread, but they are highly correlated. Simultaneous inclusion of these factors in the study of the COVID-19 transmission pattern needs more deliberate analysis that is rarely found in the reviewed papers and could be done in future studies.
CRediT authorship contribution statement
Mehdi Alidadi: Methodology, Data curation, Visualization, Writing - Original draft preparation, Ayyoob Sharifi: Conceptualization, Methodology, Writing - Original draft preparation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This study was supported by JSPS KAKENHI Grant Number 22K04493 and a grant from Toyota Foundation (Grant No. D21-R-0040).
Editor: Jay Gan
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2022.158056.
Appendix A. Supplementary data
The following is the supplementary data related to this article.
The reviewed articles.
Data availability
No data was used for the research described in the article.
References
- AbouKorin S.A.A., Han H., Mahran M.G.N. Role of urban planning characteristics in forming pandemic resilient cities–case study of covid-19 impacts on European cities within England, Germany and Italy. Cities. 2021;118 doi: 10.1016/j.cities.2021.103324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad K., Erqou S., Shah N., Nazir U., Morrison A.R., Choudhary G., Wu W.C. Association of poor housing conditions with covid-19 incidence and mortality across us counties. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0241327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi M., Sharifi A., Dorosti S., Ghoushchi S.J., Ghanbari N. Investigation of effective climatology parameters on covid-19 outbreak in Iran. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed J., Jaman M.H., Saha G., Ghosh P. Effect of environmental and socioeconomic factors on the spreading of covid-19 at 70 cities/provinces. Heliyon. 2021;7(5) doi: 10.1016/j.heliyon.2021.e06979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Kindi K.M., Al-Mawali A., Akharusi A., Alshukaili D., Alnasiri N., Al-Awadhi T., Charabi Y., El Kenawy A.M. Demographic and socioeconomic determinants of covid-19 across Oman-a geospatial modelling approach. Geospat. Health. 2021;16(1) doi: 10.4081/gh.2021.985. [DOI] [PubMed] [Google Scholar]
- Alam M.S., Sultana R. Influences of climatic and non-climatic factors on covid-19 outbreak: a review of existing literature. Environ. Challenges. 2021;5 doi: 10.1016/j.envc.2021.100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam M.Z. Is population density a risk factor for communicable diseases like covid19? a case of Bangladesh. Asia Pacific Journal of Public Health. 2021;33(8):949–950. doi: 10.1177/1010539521998858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali T., Mortula M., Sadiq R. Gis-based vulnerability analysis of the United States to covid-19 occurrence. J. Risk Res. 2021;24(3–4):416–431. [Google Scholar]
- Almagro M., Orane-Hutchinson A. Jue insight: The determinants of the differential exposure to covid-19 in New York city and their evolution over time. J. Urban Econ. 2020:103293. doi: 10.1016/j.jue.2020.103293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aw S.B., Teh B.T., Ling G.H.T., Leng P.C., Chan W.H., Ahmad M.H. The covid-19 pandemic situation in Malaysia: lessons learned from the perspective of population density. Int. J. Environ. Res. Public Health. 2021;18(12):6566. doi: 10.3390/ijerph18126566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azuma K., Yanagi U., Kagi N., Kim H., Ogata M., Hayashi M. Environmental factors involved in sars-cov-2 transmission: effect and role of indoor environmental quality in the strategy for covid-19 infection control. Environ. Health Prev. Med. 2020;25(1):1–16. doi: 10.1186/s12199-020-00904-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barak N., Sommer U., Mualam N. Sci. Total Environ. 2021. Urban attributes and the spread of covid19: the effects of density, compliance and socio-political factors in Israel; p. 148626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basellini U., Camarda C.G. Explaining regional differences in mortality during the first wave of covid-19 in Italy. Popul. Stud. 2021:1–20. doi: 10.1080/00324728.2021.1984551. [DOI] [PubMed] [Google Scholar]
- Baser O. Population density index and its use for distribution of covid-19: a case study using Turkish data. Health Policy. 2021;125(2):148–154. doi: 10.1016/j.healthpol.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayode T., Popoola A., Akogun O., Siegmund A., Magidimisha-Chipungu H., Ipingbemi O. Spatial variability of covid-19 and its risk factors in Nigeria: a spatial regression method. Appl. Geogr. 2022;138 doi: 10.1016/j.apgeog.2021.102621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bijari N.B., Mahdinia M.H., Daneshvar M.R.M. Investigation of the urbanization contribution to the covid-19 outbreak in Iran and the Meca countries. Environ. Dev. Sustain. 2021:1–22. doi: 10.1007/s10668-021-01423-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boterman W.R. Urban-rural polarisation in times of the corona outbreak? the early demographic and geographic patterns of the sars-cov-2 epidemic in the netherlands. Tijdschr. Econ. Soc. Geogr. 2020;111(3):513–529. doi: 10.1111/tesg.12437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brakefield W.S., Olusanya O.A., White B., Shaban-Nejad A. Disaster Medicine and Public Health Preparedness. 2022. Social determinants and indicators of covid-19 among marginalized communities: A scientific review and call to action for pandemic response and recovery; pp. 1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan M.S., Sun J., Jagai J., Horton D.E., Montgomery A., Sargis R., Argos M. Coronavirus disease 2019 (covid-19) mortality and neighborhood characteristics in Chicago. Ann. Epidemiol. 2021;56:47–54. doi: 10.1016/j.annepidem.2020.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cestari V.R.F., Florˆencio R.S., Sousa G.J.B., Garces T.S., Castro R.R., Cordeiro L.I., Damasceno L.L.V., Pereira M.L.D., et al. Maranha~o T.A., Pessoa V.L.M.d.P. Social vulnerability and covid-19 incidence in a brazilian metropolis. Ciˆencia & Sau´de Coletiva. 2021;26:1023–1033. doi: 10.1590/1413-81232021263.42372020. [DOI] [PubMed] [Google Scholar]
- Chan P.Y., Greene S.K., Woo Lim S., Fine A., Thompson C.N. Persistent disparities in sars-cov-2 test percent positivity by neighborhood in New York City, March 1–July 25, 2020. Annals of Epidemiology. 2021;63:46–51. doi: 10.1016/j.annepidem.2021.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu Z., Cheng M., Song M. What determines urban resilience against covid-19: city size or governance capacity? Sustain. Cities Soc. 2021;75 doi: 10.1016/j.scs.2021.103304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciupa T., Suligowski R. Green-blue spaces and population density versus covid-19 cases and deaths in Poland. Int. J. Environ. Res. Public Health. 2021;18(12):6636. doi: 10.3390/ijerph18126636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consolazio D., Murtas R., Tunesi S., Gervasi F., Benassi D., Russo A.G. Assessing the impact of individual characteristics and neighborhood socioeconomic status during the covid-19 pandemic in the provinces of Milan and Lodi. Int. J. Health Serv. 2021;51(3):311–324. doi: 10.1177/0020731421994842. [DOI] [PubMed] [Google Scholar]
- Cordes J., Castro M.C. Spatial analysis of covid-19 clusters and contextual factors in New York City. Spatial Spatio-temporal Epidemiol. 2020;34 doi: 10.1016/j.sste.2020.100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Credit K. Neighbourhood inequity: exploring the factors underlying racial and ethnic disparities in covid-19 testing and infection rates using zip code data in Chicago and New York. Reg. Sci. Policy Pract. 2020;12(6):1249–1271. [Google Scholar]
- De Angelis E., Renzetti S., Volta M., Donato F., Calza S., Placidi D., Lucchini R.G., Rota M. Covid-19 incidence and mortality in Lombardy, Italy: an ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environ. Res. 2021;195 doi: 10.1016/j.envres.2021.110777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Li Q., Tong X., Wang R., Zhai S., Gao C., Lei Z., Chen S., Zhou Y., Wang J., et al. Spatiotemporal spread pattern of the covid-19 cases in China. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0244351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielding-Miller R.K., Sundaram M.E., Brouwer K. Social determinants of covid-19 mortality at the county level. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0240151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaglioti A.H., Li C., Douglas M.D., Baltrus P.T., Blount M.A., Zahidi R., Caplan L.S., Willock R.J., Fasuyi O.B., Mack D.H. Population-level disparities in covid-19: measuring the independent association of the proportion of black population on covid-19 cases and deaths in us counties. J. Public Health Manag. Pract. 2021;27(3):268–277. doi: 10.1097/PHH.0000000000001354. [DOI] [PubMed] [Google Scholar]
- Gargiulo C., Gaglione F., Guida C., Papa R., Zucaro F., Carpentieri G. The role of the urban settlement system in the spread of covid-19 pandemic. the italian case. TEMA J. Land Use Mobil. Environ. 2020:189–212. [Google Scholar]
- Ghosh A.K., Venkatraman S., Soroka O., Reshnetnyak E., Rajan M., An A., Chae J.K., Gonzalez C., DiMaggio C., Prince J., et al. medRxiv; 2021. Association Between Overcrowded Households, Multigenerational Households, and Covid-19: A Cohort Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y., Yu H., Zhang G., Ma D.T. Exploring the impacts of travel-implied policy factors on covid-19 spread within communities based on multi-source data interpretations. Health Place. 2021;69 doi: 10.1016/j.healthplace.2021.102538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Kumar Patel K., Sivaraman S., Mangal A. Global epidemiology of first 90 days into covid-19 pandemic: disease incidence, prevalence, case fatality rate and their association with population density, urbanisation and elderly population. J. Health Manag. 2020;22(2):117–128. [Google Scholar]
- Hamidi S., Ewing R., Sabouri S. Longitudinal analyses of the relationship between development density and the covid-19 morbidity and mortality rates: early evidence from 1,165 metropolitan counties in the United States. Health Place. 2020;64 doi: 10.1016/j.healthplace.2020.102378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Hamidi I. Subway ridership, crowding, or population density: determinants of covid-19 infection rates in New York City. Am. J. Prev. Med. 2021;60(5):614–620. doi: 10.1016/j.amepre.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Sabouri S., Ewing R. Does density aggravate the covid-19 pandemic? Early findings and lessons for planners. J. Am. Plan. Assoc. 2020;86(4):495–509. [Google Scholar]
- Han L., Jia J. Reductions of migrant population reduces the number of covid-19 epidemic: a case study in China. Environ. Sci. Pollut. Res. 2021:1–11. doi: 10.1007/s11356-021-13195-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Y., Yang L., Jia K., Li J., Feng S., Chen W., Zhao W., Pereira P. Spatial distribution characteristics of the covid-19 pandemic in Beijing and its relationship with environmental factors. Sci. Total Environ. 2021;761 doi: 10.1016/j.scitotenv.2020.144257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao Q., Chen L., Xu F., Li Y. Proceedings of the 26th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining. 2020. Understanding the urban pandemic spreading of covid-19 with real world mobility data; pp. 3485–3492. [Google Scholar]
- Harris P., Harris-Roxas B., Prior J., Morrison N., McIntyre E., Frawley J., Adams J., Bevan W., Haigh F., Freeman E., et al. Respiratory pandemics, urban planning and design: a multidisciplinary rapid review of the literature. Cities. 2022;127 doi: 10.1016/j.cities.2022.103767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashim M.J., Alsuwaidi A.R., Khan G. Population risk factors for covid-19 mortality in 93 countries. J. Epidemiol. Glob. Health. 2020;10(3):204. doi: 10.2991/jegh.k.200721.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan M.S., Bhuiyan M.A.H., Tareq F., Bodrud-Doza M., Tanu S.M., Rabbani K.A. Relationship between covid-19 infection rates and air pollution, geo-meteorological, and social parameters. Environ. Monit. Assess. 2021;193(1):1–20. doi: 10.1007/s10661-020-08810-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassankhani M., Alidadi M., Sharifi A., Azhdari A. Smart city and crisis management: lessons for the covid-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18(15):7736. doi: 10.3390/ijerph18157736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu M., Roberts J.D., Azevedo G.P., Milner D. The role of built and social environmental factors in covid-19 transmission: a look at America's capital city. Sustain. Cities Soc. 2021;65 [Google Scholar]
- Hu Z., Wu Y., Su M., Xie L., Zhang A., Lin X., Nie Y. Population migration, spread of covid-19, and epidemic prevention and control: empirical evidence from China. BMC Public Health. 2021;21(1):1–12. doi: 10.1186/s12889-021-10605-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Kwan M.-P., Kan Z., Wong M.S., Kwok C.Y.T., Yu X. Investigating the relationship between the built environment and relative risk of covid-19 in Hong Kong. ISPRS Int. J. Geo Inf. 2020;9(11):624. [Google Scholar]
- Huang X., Yang Q., Yang J. Importance of community containment measures in combating the covid-19 epidemic: from the perspective of urban planning. Geo-spatial Information Sci. 2021:1–9. [Google Scholar]
- Hussein H.A.A. Investigating the role of the urban environment in controlling pandemics transmission: lessons from history. Ain Shams Eng. J. 2022;13(6) [Google Scholar]
- Ilardi A., Chieffi S., Iavarone A., Ilardi C.R. Sars-cov-2 in italy: population density correlates with morbidity and mortality. Jpn. J. Infect. Dis. 2020;74(1):61–64. doi: 10.7883/yoken.JJID.2020.200. pages JJID–2020. [DOI] [PubMed] [Google Scholar]
- Iyanda A.E., Boakye K.A., Lu Y., Oppong J.R. Racial/ethnic heterogeneity and rural-urban disparity of covid-19 case fatality ratio in the USA: a negative binomial and gis-based analysis. J. Racial Ethn. Health Disparities. 2021:1–14. doi: 10.1007/s40615-021-01006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamshidi S., Baniasad M., Niyogi D. Global to Usa county scale analysis of weather, urban density, mobility, homestay, and mask use on covid-19. Int. J. Environ. Res. Public Health. 2020;17(21):7847. doi: 10.3390/ijerph17217847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha S., Goyal M.K., Gupta B., Gupta A.K. A novel analysis of COVID 19 risk in India incorporating climatic and socioeconomic factors. Technol. Forecast. Soc. Chang. 2021;167 doi: 10.1016/j.techfore.2021.120679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo Y., Hong A., Sung H. Density or connectivity: what are the main causes of the spatial proliferation of covid-19 in Korea? Int. J. Environ. Res. Public Health. 2021;18(10):5084. doi: 10.3390/ijerph18105084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson T.F., Hordley L.A., Greenwell M.P., Evans L.C. medRxiv; 2021. Associations Between Covid-19 Transmission Rates, Park Use, and Landscape Structure. pages 2020–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan Z., Kwan M.-P., Wong M.S., Huang J., Liu D. Identifying the space-time patterns of covid-19 risk and their associations with different built environment features in Hong Kong. Sci. Total Environ. 2021;772 doi: 10.1016/j.scitotenv.2021.145379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashem S.B., Baker D.M., Lee C.A., Gonza´lez S.R. Exploring the nexus between social vulnerability, built environment, and the prevalence of covid-19: A case study of chicago. Sustain. Cities Society. 2021;75:103261. doi: 10.1016/j.scs.2021.103261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khavarian-Garmsir A.R., Sharifi A., Moradpour N. Are high-density districts more vulnerable to the covid-19 pandemic? Sustain. Cities Soc. 2021;70 doi: 10.1016/j.scs.2021.102911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H., Zanobetti A., Bell M.L. Temporal transition of racial/ethnic disparities in covid-19 outcomes in 3108 counties of the united states: three phases from January to December, 2020. Science of The Total Environment. 2021:148167. doi: 10.1016/j.scitotenv.2021.148167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klompmaker J.O., Hart J.E., Holland I., Sabath M.B., Wu X., Laden F., Dominici F., James P. County-level exposures to greenness and associations with covid-19 incidence and mortality in the United States. Environ. Res. 2021;199 doi: 10.1016/j.envres.2021.111331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodera S., Rashed E.A., Hirata A. Correlation between covid-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. Int. J. Environ. Res. Public Health. 2020;17(15):5477. doi: 10.3390/ijerph17155477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S., Singh R., Kumari N., Karmakar S., Behera M., Siddiqui A.J., Rajput V.D., Minkina T., Bauddh K., Kumar N. Current understanding of the influence of environmental factors on sars-cov-2 transmission, persistence, and infectivity. Environ. Sci. Pollut. Res. 2021;28(6):6267–6288. doi: 10.1007/s11356-020-12165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok C.Y.T., Wong M.S., Chan K.L., Kwan M.-P., Nichol J.E., Liu C.H., Wong J.Y.H., Wai A.K.C., Chan L.W.C., Xu Y., et al. Spatial analysis of the impact of urban geometry and socio-demographic characteristics on covid-19, a study in Hong Kong. Sci. Total Environ. 2021;764 doi: 10.1016/j.scitotenv.2020.144455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lak A., Sharifi A., Badr S., Zali A., Maher A., Mostafavi E., Khalili D. Spatio-temporal patterns of the covid-19 pandemic, and place-based influential factors at the neighborhood scale in Tehran. Sustain. Cities Soc. 2021;72 doi: 10.1016/j.scs.2021.103034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lata K., Thapa K., Rajput A.S. Liveability of Indian cities and spread of covid-19–case of tier-1 cities. Indian J. Public Adm. 2021;67(3):365–382. [Google Scholar]
- Lee W., Kim H., Choi H.M., Heo S., Fong K.C., Yang J., Park C., Kim H., Bell M.L. Urban environments and covid-19 in three eastern states of the United States. Sci. Total Environ. 2021;779 doi: 10.1016/j.scitotenv.2021.146334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Peng Y., He H., Wang M., Feng T. Built environment and early infection of covid-19 in urban districts: a case study of Huangzhou. Sustain. Cities Soc. 2021;66 doi: 10.1016/j.scs.2020.102685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Yang Y., Wang W., Lee S., Xiao X., Gao X., Oztekin B., Fan C., Mostafavi A. Unraveling the dynamic importance of county-level features in trajectory of covid-19. Sci. Rep. 2021;11(1):1–11. doi: 10.1038/s41598-021-92634-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Ma S., Zhang J. Association of built environment attributes with the spread of covid-19 at its initial stage in China. Sustain. Cities Soc. 2021;67 doi: 10.1016/j.scs.2021.102752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Zhou L., Jia T., Peng R., Fu X., Zou Y. Associating covid-19 severity with urban factors: a case study of Wuhan. Int. J. Environ. Res. Public Health. 2020;17(18):6712. doi: 10.3390/ijerph17186712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Q., Dong M., Yuan J., Fielding R., Cowling B.J., Wong I.O.L., Lam W.W.T. Assessing community vulnerability over 3 waves of covid-19 pandemic, Hong Kong, China. Emerg. Infect. Dis. 2021;27(7):1935–1939. doi: 10.3201/eid2707.204076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y., Zhong P., Chen T. Association between socioeconomic factors and the covid-19 outbreak in the 39 well-developed cities of China. FrontiersPublic Health. 2020;8 doi: 10.3389/fpubh.2020.546637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Liu Z., Guan C. The impacts of the built environment on the incidence rate of covid-19: a case study of king county, Washington. Sustain. Cities Soc. 2021;74 doi: 10.1016/j.scs.2021.103144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Hao J., Sun Y., Shi Z. Network analysis of population flow among major cities and its influence on covid-19 transmission in China. Cities. 2021;112 doi: 10.1016/j.cities.2021.103138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Qin Y., Xie Z., Zhang J. The spatio-temporal characteristics and influencing factors of covid-19 spread in Shenzhen, china—an analysis based on 417 cases. Int. J. Environ. Res. Public Health. 2020;17(20):7450. doi: 10.3390/ijerph17207450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo´pez-Gay A., Spijker J., Cole H.V., Marques A.G., Triguero-Mas M., Anguelovski I., Alamo-Junquera D., et al. Lo´pez-Gay M., Mo´denes J.A., Lo´pez-Gallego F. Sociodemographic determinants of intraurban variations in covid-19 incidence: the case of barcelona. J. Epidemiol. Community Health. 2022;76(1):1–7. doi: 10.1136/jech-2020-216325. [DOI] [PubMed] [Google Scholar]
- Ma S., Li S., Zhang J. Diverse and nonlinear influences of built environment factors on covid-19 spread across townships in China at its initial stage. Sci. Rep. 2021;11(1):1–13. doi: 10.1038/s41598-021-91849-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehmood K., Bao Y., Abrar M.M., Petropoulos G.P., Soban A., Saud S., Khan Z.A., Khan S.M., Fahad S., et al. Spatiotemporal variability of covid-19 pandemic in relation to air pollution, climate and socioeconomic factors in Pakistan. Chemosphere. 2021;271 doi: 10.1016/j.chemosphere.2021.129584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollalo A., Vahedi B., Rivera K.M. Gis-based spatial modeling of covid-19 incidence rate in the continental United States. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mondal S., Chaipitakporn C., Kumar V., Wangler B., Gurajala S., Dhaniyala S., Sur S. Covid-19 in New York state: effects of demographics and air quality on infection and fatality. Sci. Total Environ. 2022;807 doi: 10.1016/j.scitotenv.2021.150536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moosa I.A., Khatatbeh I.N. The density paradox: are densely-populated regions more vulnerable to covid-19? Int. J. Health Plann. Manag. 2021;36(5):1575–1588. doi: 10.1002/hpm.3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakada L.Y.K., Urban R.C. Covid-19 pandemic: environmental and social factors influencing the spread of sars-cov-2 in s~ao paulo, Brazil. Environ. Sci. Pollut. Res. 2021;28(30):40322–40328. doi: 10.1007/s11356-020-10930-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasiri R., Akbarpour S., Zali A., Khodakarami N., Boochani M., Noory A., Soori H. Spatio-temporal analysis of covid-19 incidence rate using gis: a case study—Tehran Metropolitan, Iran. GeoJournal. 2021:1–15. doi: 10.1007/s10708-021-10438-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen Q.C., Huang Y., Kumar A., Duan H., Keralis J.M., Dwivedi P., Meng H.-W., Brunisholz K.D., Jay J., Javanmardi M., et al. Using 164 million google street view images to derive built environment predictors of covid-19 cases. Int. J. Environ. Res. Public Health. 2020;17(17):6359. doi: 10.3390/ijerph17176359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T.H., Shah G.H., Schwind J.S., Richmond H.L. Community characteristics and covid-19 outcomes: a study of 159 counties in Georgia, United States. J. Public Health Manag. Pract. 2021;27(3):251–257. doi: 10.1097/PHH.0000000000001330. [DOI] [PubMed] [Google Scholar]
- Niu Q., Wu W., Shen J., Huang J., Zhou Q. Relationship between built environment and covid-19 dispersal based on age stratification: a case study of Wuhan. Int. J. Environ. Res. Public Health. 2021;18(14):7563. doi: 10.3390/ijerph18147563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu X., Yue Y., Zhou X., Zhang X. How urban factors affect the spatiotemporal distribution of infectious diseases in addition to intercity population movement in China. ISPRS Int. J. Geo Inf. 2020;9(11):615. [Google Scholar]
- Pequeno P., Mendel B., Rosa C., Bosholn M., Souza J.L., Baccaro F., Barbosa R., Magnusson W. Air transportation, population density and temperature predict the spread of covid-19 in Brazil. PeerJ. 2020;8 doi: 10.7717/peerj.9322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perone G. The determinants of covid-19 case fatality rate (cfr) in the italian regions and provinces: an analysis of environmental, demographic, and healthcare factors. Sci. Total Environ. 2021;755 doi: 10.1016/j.scitotenv.2020.142523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phiri D., Salekin S., Nyirenda V.R., Simwanda M., Ranagalage M., Murayama Y. Spread of covid-19 in Zambia: an assessment of environmental and socioeconomic factors using a classification tree approach. Sci. Afr. 2021;12 doi: 10.1016/j.sciaf.2021.e00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkington H., Feuillet T., Rican S., de Bouill´e J.G., Bouchaud O., Cailhol J., Bihan H., Lombrail P., Julia C. Spatial determinants of excess all-cause mortality during the first wave of the covid-19 epidemic in France. BMC Public Health. 2021;21(1):1–10. doi: 10.1186/s12889-021-12203-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qeadan F., Mensah N.A., Tingey B., Bern R., Rees T., Madden E.F., Porucznik C.A., English K., Honda T. The association between opioids, environmental, demographic, and socioeconomic indicators and covid-19 mortality rates in the United States: an ecological study at the county level. Arch. Public Health. 2021;79(1):1–8. doi: 10.1186/s13690-021-00626-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Li R., Han D., Shao Q., Han Y., Luo X., Wu Y. A multiplicity of environmental, economic and social factor analyses to understand covid-19 diffusion. One Health. 2021;13 doi: 10.1016/j.onehlt.2021.100335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Y., Chen X., Shi W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (covid-19) in China. J. Popul. Econ. 2020;33(4):1127–1172. doi: 10.1007/s00148-020-00778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M.H., Zafri N.M., Ashik F.R., Waliullah M., Khan A. Identification of risk factors contributing to covid-19 incidence rates in Bangladesh: a gis-based spatial modeling approach. Heliyon. 2021;7(2) doi: 10.1016/j.heliyon.2021.e06260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram´ırez-Aldana R., Gomez-Verjan J.C., Bello-Chavolla O.Y. Spatial analysis of covid-19 spread in Iran: Insights into geographical and structural transmission determinants at a province level. PLoS Neglect. Trop. Diseases. 2020;14(11) doi: 10.1371/journal.pntd.0008875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram´ırez-Aldana R., Gomez-Verjan J.C., Bello-Chavolla O.Y., Garc´ıa-Pen~a C. Spatial epidemiological study of the distribution, clustering, and risk factors associated with early covid-19 mortality in Mexico. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0254884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razavi-Termeh S.V., Sadeghi-Niaraki A., Farhangi F., Choi S.-M. Covid-19 risk mapping with considering socio-economic criteria using machine learning algorithms. Int. J. Environ. Res. Public Health. 2021;18(18):9657. doi: 10.3390/ijerph18189657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro H.V., Sunahara A.S., Sutton J., Perc M., Hanley Q.S. City size and the spreading of covid-19 in Brazil. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rideout A., Murray C., Isles C. Regional variation in covid-19 positive hospitalisation across Scotland during the first wave of the pandemic and its relation to population density: a cross-sectional observation study. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0253636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas-Rueda D., Morales-Zamora E. Built environment, transport, and covid19: a review. Curr. Environ. Health Rep. 2021;8(2):138–145. doi: 10.1007/s40572-021-00307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruck D.J., Bentley R.A., Borycz J. Early warning of vulnerable counties in a pandemic using socio-economic variables. Econ. Hum. Biol. 2021;41 doi: 10.1016/j.ehb.2021.100988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russette H., Graham J., Holden Z., Semmens E.O., Williams E., Landguth E.L. Greenspace exposure and covid-19 mortality in the United States: January–July 2020. Environ. Res. 2021;198 doi: 10.1016/j.envres.2021.111195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S.K., Ekram K.M.M., Das P.C. Spatial modeling of covid-19 transmission in Bangladesh. Spat. Inf. Res. 2021:1–12. [Google Scholar]
- Sarmadi M., Moghanddam V.K., Dickerson A.S., Martelletti L. Association of covid-19 distribution with air quality, sociodemographic factors, and comorbidities: an ecological study of us states. Air Qual. Atmos. Health. 2021;14(4):455–465. doi: 10.1007/s11869-020-00949-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarpone C., Brinkmann S.T., Große T., Sonnenwald D., Fuchs M., Walker B.B. A multimethod approach for county-scale geospatial analysis of emerging infectious diseases: a cross-sectional case study of covid-19 incidence in Germany. Int. J. Health Geogr. 2020;19(1):1–17. doi: 10.1186/s12942-020-00225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen-Crowe B., Lin I.-C., Alfaro R., McKenney M., Elkbuli A. Ann. Med. Surg. 2021. Covid-19 fatalities by zip codes and socioeconomic indicators across various us regions; p. 102471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharif O., Islam M.R., Hasan M.Z., Kabir M.A., Hasan M.E., AlQahtani S.A., Xu G. Analyzing the impact of demographic variables on spreading and forecasting covid-19. J. Healthc. Informatics Res. 2021:1–19. doi: 10.1007/s41666-021-00105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi A., Khavarian-Garmsir A.R. The COVID-19 pandemic: impacts on cities and major lessons for urban planning, design, and management. Sci. Total Environ. 2020;749 doi: 10.1016/j.scitotenv.2020.142391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi A., Khavarian-Garmsir A.R., Kummitha R.K.R. Contributions of smart city solutions and technologies to resilience against the covid-19 pandemic: a literature review. Sustainability. 2021;13(14):8018. [Google Scholar]
- Shortall R., Mouter N., Van Wee B. Covid-19 passenger transport measures and their impacts. Transp. Rev. 2021:1–26. [Google Scholar]
- Shortall R., Mouter N., Van Wee B. Covid-19 and transport. A review of factors of relevance to the design of measures and their effects worldwide. Eur. J. Transp. Infrastruct. Res. 2022;22(1):118–130. [Google Scholar]
- Sigler T., Mahmuda S., Kimpton A., Loginova J., Wohland P., Charles-Edwards E., Corcoran J. The socio-spatial determinants of covid-19 diffusion: the impact of globalisation, settlement characteristics and population. Glob. Health. 2021;17(1):1–14. doi: 10.1186/s12992-021-00707-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva J., Ribeiro-Alves M. Social inequalities and the pandemic of covid-19: the case of Rio de Janeiro. J. Epidemiol. Community Health. 2021;75:975–979. doi: 10.1136/jech-2020-214724. [DOI] [PubMed] [Google Scholar]
- Spotswood E.N., Benjamin M., Stoneburner L., Wheeler M.M., Beller E.E., Balk D., McPhearson T., Kuo M., McDonald R.I. Nature inequity and higher covid19 case rates in less-green neighbourhoods in the United States. Nat. Sustain. 2021;4(12):1092–1098. [Google Scholar]
- Steiger E., Mussgnug T., Kroll L.E. Causal graph analysis of covid-19 observational data in german districts reveals effects of determining factors on reported case numbers. PLoS One. 2021;16(5) doi: 10.1371/journal.pone.0237277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Xie J., Hu X. Detecting spatial clusters of coronavirus infection across london during the second wave. Appl. Spat. Anal. Policy. 2021:1–15. doi: 10.1007/s12061-021-09413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamrakar V., Srivastava A., Saikia N., Parmar M.C., Shukla S.K., Shabnam S., Boro B., Saha A., Debbarma B. District level correlates of covid-19 pandemic in India during march-october 2020. PLoS One. 2021;16(9) doi: 10.1371/journal.pone.0257533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teller J. Urban density and COVID-19: towards an adaptive approach. Build. Cities. 2021;2(1) [Google Scholar]
- Tchicaya A., Lorentz N., Leduc K., de Lanchy G. Covid-19 mortality with regard to healthcare services availability, health risks, and socio-spatial factors at department level in France: a spatial cross-sectional analysis. PloS one. 2021;16(9) doi: 10.1371/journal.pone.0256857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas M.M., Mohammadi N., Taylor J.E. Investigating the association between mass transit adoption and covid-19 infections in us metropolitan areas. Sci. Total Environ. 2022;811 doi: 10.1016/j.scitotenv.2021.152284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tieskens K., Patil P., Levy J.I., Brochu P., Lane K.J., Fabian M.P., Carnes F., Haley B.M., Spangler K.R., Leibler J.H. Time-varying associations between covid19 case incidence and community-level sociodemographic, occupational, environmental, and mobility risk factors in massachusetts. Research Square. 2021 doi: 10.1186/s12879-021-06389-w. pages rs–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokey A.I. Spatial association of mobility and covid-19 infection rate in the Usa: a county-level study using mobile phone location data. J. Transp. Health. 2021;22 doi: 10.1016/j.jth.2021.101135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tribby C.P., Hartmann C. Covid-19 cases and the built environment: initial evidence from New York city. Prof. Geogr. 2021:1–12. [Google Scholar]
- Urban R.C., Nakada L.Y.K. Gis-based spatial modelling of covid-19 death incidence in Sa~o Paulo, Brazil. Environ. Urban. 2021;33(1):229–238. doi: 10.1177/0956247820963962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valsamatzi-Panagiotou A., Penchovsky R. Environmental factors influencing the transmission of the coronavirus 2019: a review. Environ. Chem. Lett. 2022:1–8. doi: 10.1007/s10311-022-01418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma R., Yabe T., Ukkusuri S.V. Spatiotemporal contact density explains the disparity of covid-19 spread in urban neighborhoods. Sci. Rep. 2021;11(1):1–11. doi: 10.1038/s41598-021-90483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villalobos Dintrans P., Castillo C., De La Fuente F., Maddaleno M. Covid-19 incidence and mortality in the metropolitan region, Chile: time, space, and structural factors. PLoS One. 2021;16(5) doi: 10.1371/journal.pone.0250707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wali B., Frank L.D. Neighborhood-level covid-19 hospitalizations and mortality relationships with built environment, active and sedentary travel. Health & Place. 2021;71 doi: 10.1016/j.healthplace.2021.102659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Zhang S., Yang Z., Zhao Z., Moudon A.V., Feng H., Liang J., Sun W., Cao B. What county-level factors influence covid-19 incidence in the United states? Findings from the first wave of the pandemic. Cities. 2021;118 doi: 10.1016/j.cities.2021.103396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver A.K., Head J.R., Gould C.F., Carlton E.J., Remais J.V. Environmental factors influencing covid-19 incidence and severity. Annu. Rev. Public Health. 2022;43 doi: 10.1146/annurev-publhealth-052120-101420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton W.C., Kinsella Thompson A. 2020. The Geography of covid-19 Growth in the Us: Counties and Metropolitan Areas. Available at SSRN 3570540. [Google Scholar]
- Whitaker S.D. Cfed District Data Briefs. 2021. Did the covid-19 pandemic cause an urban exodus? (cfddb 20210205) [Google Scholar]
- White E.R., H´ebert-Dufresne L. State-level variation of initial covid-19 dynamics in the united states. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0240648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong D.W., Li Y. Spreading of covid-19: density matters. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0242398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T. The socioeconomic and environmental drivers of the covid-19 pandemic: a review. Ambio. 2021;50(4):822–833. doi: 10.1007/s13280-020-01497-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Zhang J. Exploration of spatial-temporal varying impacts on covid-19 cumulative case in Texas using geographically weighted regression (gwr) Environ. Sci. Pollut. Res. 2021:1–15. doi: 10.1007/s11356-021-13653-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Y., Wang Y., Chen F., Zhu M. Spatial statistics and influencing factors of the covid-19 epidemic at both prefecture and county levels in Hubei province, China. Int. J. Environ. Res. Public Health. 2020;17(11):3903. doi: 10.3390/ijerph17113903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu G., Jiang Y., Wang S., Qin K., Ding J., Liu Y., Lu B. Spatial disparities of self-reported covid-19 cases and influencing factors in Wuhan, China. Sustain. Cities Soc. 2022;76 doi: 10.1016/j.scs.2021.103485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T.-C., Kim S., Zhao Y., Choi S.-W.E. Examining spatial inequality in covid-19 positivity rates across New York City zip codes. Health Place. 2021;69 doi: 10.1016/j.healthplace.2021.102574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X.-D., Su X.-Y., Li H.-L., Ma R.-F., Qi F.-J., Cao Y.-E. Impacts of socio-economic determinants, spatial distance and climate factors on the confirmed cases and deaths of covid-19 in China. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0255229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip T.L., Huang Y., Liang C. Built environment and the metropolitan pandemic: analysis of the covid-19 spread in Hong Kong. Build. Environ. 2021;188 doi: 10.1016/j.buildenv.2020.107471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You H., Wu X., Guo X. Distribution of covid-19 morbidity rate in association with social and economic factors in Wuhan, China: implications for urban development. Int. J. Environ. Res. Public Health. 2020;17(10):3417. doi: 10.3390/ijerph17103417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C.H., Schwartz G.G. Spatial disparities in coronavirus incidence and mortality in the United States: an ecological analysis as of May 2020. J. Rural. Health. 2020;36(3):433–445. doi: 10.1111/jrh.12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Liu Y., Chen F., Mi B., Zeng L., Pei L. The effect of sociodemographic factors on covid-19 incidence of 342 cities in China: a geographically weighted regression model analysis. BMC Infect. Dis. 2021;21(1):1–8. doi: 10.1186/s12879-021-06128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. The mediating effect of air quality on the association between human mobility and covid-19 infection in China. Environ. Res. 2020;189 doi: 10.1016/j.envres.2020.109911. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The reviewed articles.
Data Availability Statement
No data was used for the research described in the article.