Graphical abstract
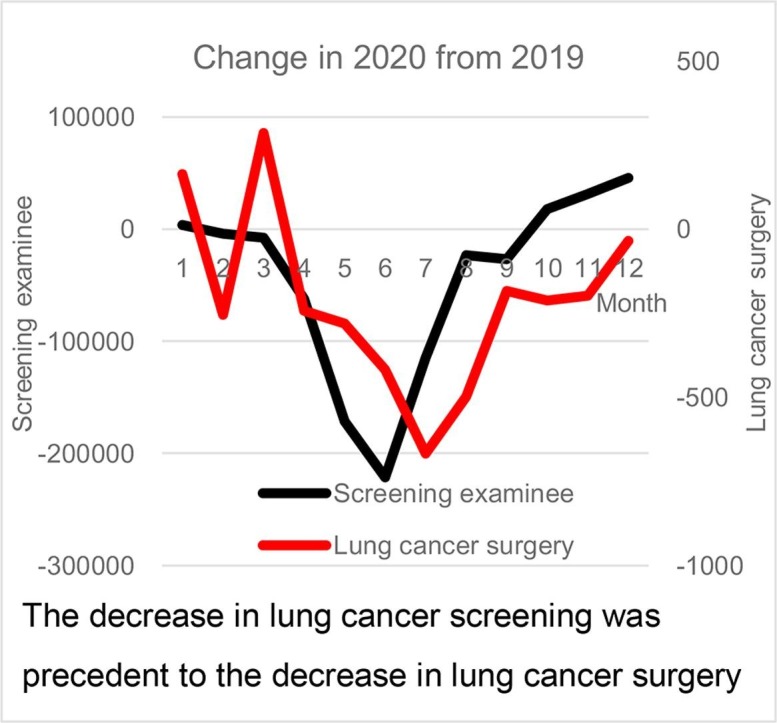
The decrease in lung cancer screening was precedent to the decrease in lung cancer surgery. Key question: Did the COVID-19 pandemic impact the number of surgeries in General Thoracic Surgery? Key findings: Substantial 10 % decrease in primary lung cancer surgeries was due to the decrease of lung cancer screening. Take-home message. Our findings highlight the importance of continuing lung cancer screening with phylaxis even during a pandemic.
Keywords: COVID-19, Lung cancer, Metastatic lung tumor, Lung cancer screening
Abbreviations: NCD, National Clinical Database; MHLW, Ministry of Health, Labor and Welfare
Abstract
Objective
The COVID-19 pandemic has far-reaching collateral health impacts on the ongoing delivery of surgical care worldwide. The current study was designed to analyze the impact of the COVID-19 pandemic on the number of surgeries of general thoracic surgery in Japan.
Methods
Changes in the number of surgeries for total and three representative tumors were analyzed using the National Clinical Database data with reference to the pandemic infection rate and lung cancer screening.
Results
In 2020, the number of surgeries in total and for primary lung cancer and mediastinal lung tumor decreased by 4.9, 5.1, and 5.0 %, respectively. Considering the five-year trend towards a 5 % annual increase, there was a potential 10 % decrease in the number of primary lung cancer surgeries. The number of primary lung cancer surgeries bottomed in July 2020 but recovered towards the end of the year. In contrast, the number of metastatic lung tumor surgeries in 2020 increased by 3.2 %, following a similar trend observed over the previous five years. The number of lung cancer screening examinees decreased markedly with the lowest number in May. Our findings indicate that surgical triage had a limited impact on the decrease in primary lung cancer surgeries during the pandemic; rather, the decrease in lung cancer screening, which was a few months preceding, is most likely responsible.
Conclusions
The decrease in primary lung cancer was mainly caused by the decrease in lung cancer screening, indicating that continuing screening is vital even during a pandemic.
1. Introduction
The novel coronavirus disease 2019 (COVID-19), which first appeared in Wuhan, China, rapidly grew to global pandemic proportions, disrupting all aspects of life for people worldwide [1]. In Japan, the first case of the COVID-19 appeared in January 2020, and despite strong efforts for disease control, the number of infections increased dramatically. By the end of the year, the third wave of the disease had spread across the country [2]. The pandemic necessitated the declaration of the first state of emergency on March 13, 2020, which included restrictions on normal daily activities such as refraining from going outside and working from home.
In preparation for the potential of COVID-19 patients requiring intensive care, including those needing mechanical ventilation and extracorporeal membrane oxygenation, hospitals had to create surge capacity management, which forced restrictions on regular major surgical treatment. Thus, the pandemic caused collateral health damage to the delivery of surgical care to millions of patients [3]. Furthermore, the diagnosis of diseases, especially cancer, stagnated due to the suspension of cancer screening. A backlog of surgical treatment and delays in the new diagnosis of cancer have had profound effects on the healthcare system, the extent of which is just beginning to fathom, and the surgeons can expect increased complexities resulting from treatment delay and disease progression [4]. Delays in resection for primary lung cancer are associated with increased upstaging rates and decreased median survival [5]. Pandemic lockdown measures caused a significant decrease in lung cancer screening participation in the United States, which could have impacted downstream lung cancer disparities [6]. The Japan Cancer Society also reported that, in 2020, cancer examinees for major cancers, i.e. stomach, lung, colon, breast, and uterine cancers, decreased by 30.5 % compared to 2019 [7]; however, the downstream effect of this decrease has not been elucidated.
Using data from the Japanese National Clinical Database (NCD), a nationwide web-based surgical patient registration system, Ikeda et al. reported that the number of pulmonary lobectomies performed in 2020 decreased by 7.8 % compared to 2019 [8], [9]. The decrease in the number of surgeries performed may be ascribed to multiple factors such as surgical triage, the decrease in hospital visits and cancer screening; however, little is known about the specific impact on general thoracic surgery. Furthermore, it is not clear whether thoracic surgeries were postponed or missed due to surgical triage, absence/delay in diagnosis, or whether there were changes in basic and perioperative factors such as mode of surgery, stage of lung cancer, and postoperative course. Thus, the current study aimed to analyze the impact of the COVID-19 pandemic on the number of surgeries of the total and for three representative tumors of general thoracic surgery (primary lung cancer, metastatic lung tumor and mediastinal tumor), with reference to the degree of infection rate per region and lung cancer screening. The results of this observational, retrospective cohort study will be an important resource to help thoracic surgeons appropriately manage their practice in problematic situations such as those brought by the COVID-19 pandemic.
2. Patients and methods
The primary outcome measure of this study was the impact of the COVID-19 pandemic on surgeries for total thoracic (except for esophageal) diseases, and three representative tumors in the general thoracic surgery field (with a focus on primary lung cancer) in reference to the degree of infection by region and lung cancer screening participation. The impact on the basic and perioperative characteristics of the primary lung cancer and metastatic lung tumor were also evaluated. This study was approved by Ethics Committee of University of Tsukuba on July 5, 2021 (R03-100).
This study involved the analysis of data extracted from the NCD. This database, established in 2010, contains data on the surgical procedures performed in Japan in addition to the perioperative factors. As of 2020, approximately 5000 participating hospitals nationwide have registered over 14,340,000 procedures, accounting for more than 90 % of all surgeries performed in Japan [9], [10]. Using the NCD to investigate surgeries performed in 2020 and comparing it with data from previous years is an ideal means to analyze changes in Japanese surgical practices due to the COVID-19 pandemic. The total and respective numbers of procedures in the general thoracic surgery field, except for esophageal surgery, performed in 2020 were analyzed and compared annually with those from 2014 to 2019, and monthly with those of 2019. The basic and perioperative factors of primary lung cancer and metastatic lung tumor were analyzed in 2019 and 2020. To investigate the effect of lung cancer screening on the surgeries, the monthly numbers of lung cancer screening examinees from 2019 and 2020 were obtained in cooperation with the Japan Cancer Society.
2.1. Phases of the COVID-19 pandemic in Japan
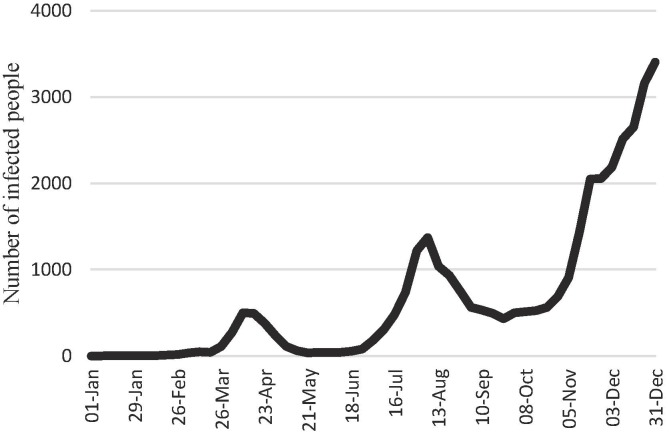
The first, second, and third waves of the COVID-19 pandemic in Japan were recognized as distinct phases of the pandemic in terms of the number of infected people. According to the Japanese Ministry of Health, Labour and Welfare (MHLW), the three pandemic waves peaked in the third week of April, the first week of August, and the fifth week of December, with the highest number of infected people in the third wave (Fig. 1 ).
Fig. 1.
Trend of new −19 infections in 2020.
2.2. Classification of prefectures according to the degree of infection
The cumulative number of infected people per population in each Japanese prefecture by the end of 2020 was used as an index of the degree of infection [2]. Based on this value, the magnitude of infection in each prefecture was classified into three groups: high, medium, and low comprising 12, 22 and 13 prefectures, respectively [8]. The quarterly numbers of surgical procedures for primary lung cancer and metastatic lung tumor performed in 2019 and 2020 were compared and the magnitude and period of influence of the COVID-19 pandemic were evaluated for each group.
2.3. The number of lung cancer screening examinees
The number of lung cancer screening examinees was investigated by the Japan Cancer Society. Questionnaires were sent by Japan Cancer Society to the branch offices of prefectures all over Japan and collected for this study, and the change in the number of examinees in 2020 compared with 2019 was analyzed.
2.4. Statistical analysis
The numerical data are expressed as the median (interquartile range) for non-normal distributions. The categorical data are expressed as percentages. A 95 % confidence interval (CI) for the proportion was calculated under the assumption of binomial distribution.
All statistical analyses were conducted using STATA 17 software (Stata Corp, College Station, TX).
3. Results
3.1. Annual change from 2014 to 2020
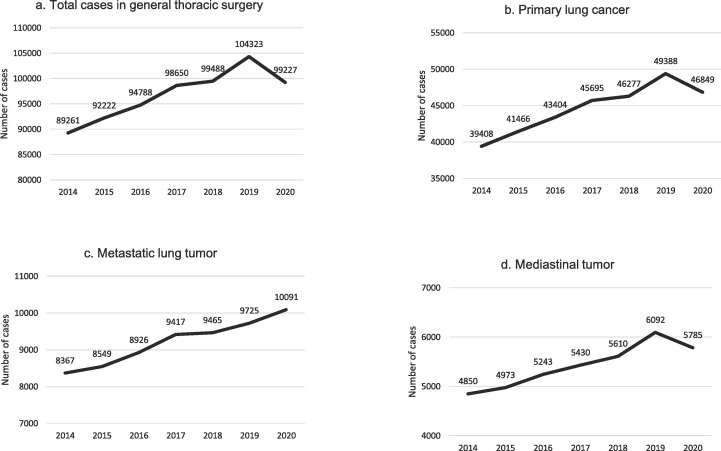
According to the NCD, the number of total surgeries in general thoracic surgery in 2020 (excluding esophageal diseases) decreased by 4.9 % to 99,227 compared to that of 2019 (104323; 95 % confidence interval [CI], 4.8–5.0 % increase), which, considering the steady annual 3.4 % increase from 2014 (89261), to 2019 (104323), indicates a substantial estimated decrease of 8.3 % (Fig. 2 a). Likewise, the number of surgeries for primary lung cancer in 2020 decreased by 5.1 % to 46,849 compared to that of 2019 (49388; 95 % CI, 4.9–5.3 % increase), which, considering the steady annual 5.0 % increase from 2014 (39408), to 2019 (49388), indicates a substantial estimated decrease of 10.1 % (Fig. 2b). On the other hand, the number of surgeries for metastatic lung tumor in 2020 increased by 3.8 % to 10,091 compared to that of 2019 (9725; 95 % CI, 3.4–4.2 % increase), which was similar as the trend of the steady annual 3.2 % increase from 2014 (8367) to 2019 (9725) (Fig. 2c). The number of surgeries for mediastinal tumor in 2020 decreased by 5.0 % to 5785 compared to that of 2019 (6092; 95 % CI, 4.5–5.6 % increase), which, considering the steady annual 5.1 % increase from 2014 (4850), to 2019 (6092), indicates a substantial estimated decrease of 10.1 % (Fig. 2d).
Fig. 2.
Yearly trends in number of thoracic surgical procedures from 2014 to 2020.
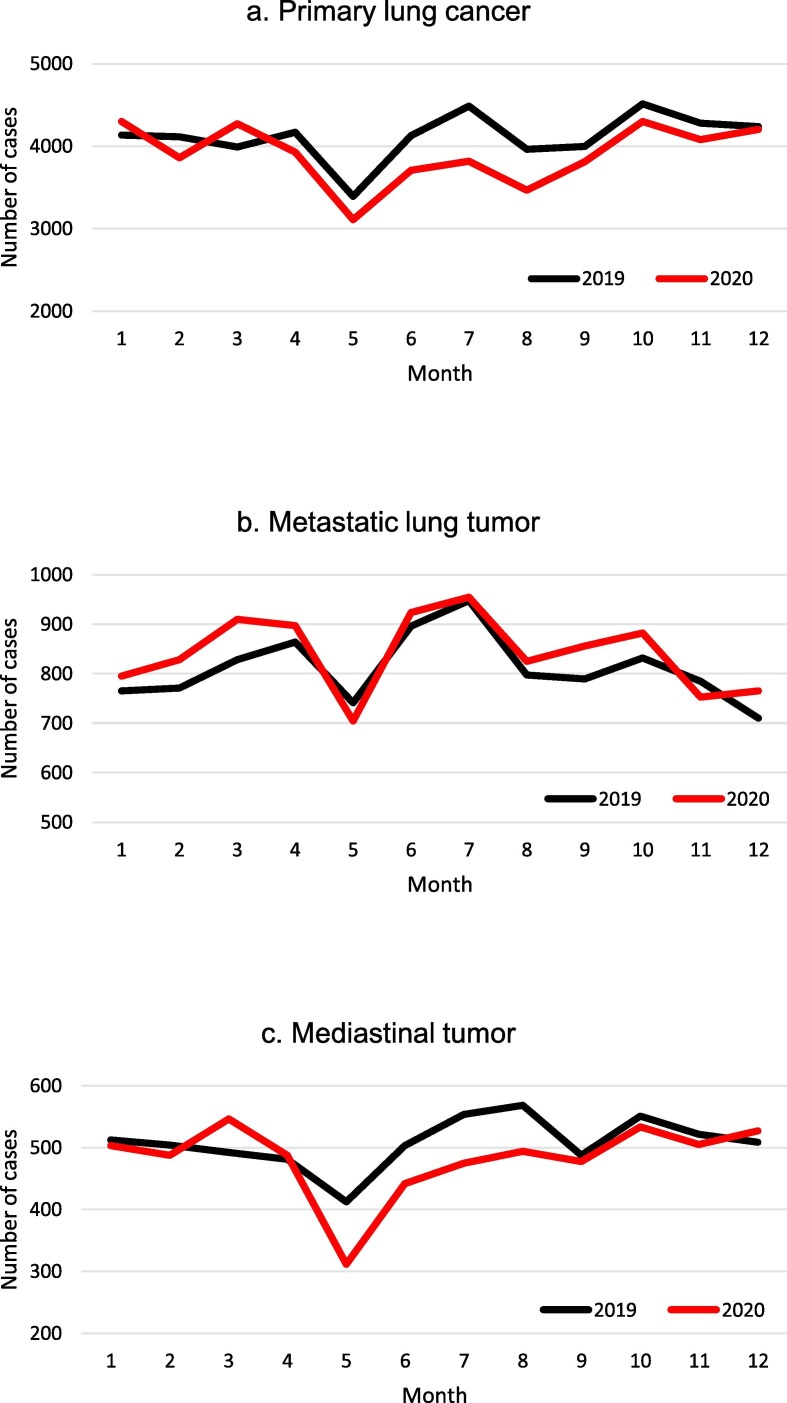
3.2. Monthly change in 2019 and 2020
In 2020, the monthly number of surgeries for primary lung cancer decreased from May to August with the largest decrease in July (−14.8 %) compared with 2019 (Fig. 3 a). In contrast, the monthly number of surgeries for metastatic lung tumor in 2020 increased slightly across most months compared with 2019 (Fig. 3b). The monthly number of surgeries for mediastinal tumor in 2020 decreased from May to August, with the largest decrease in May (−24.5 %) compared to 2019 (Fig. 3c).
Fig. 3.
Monthly trends in number of thoracic surgical procedures in 2020.
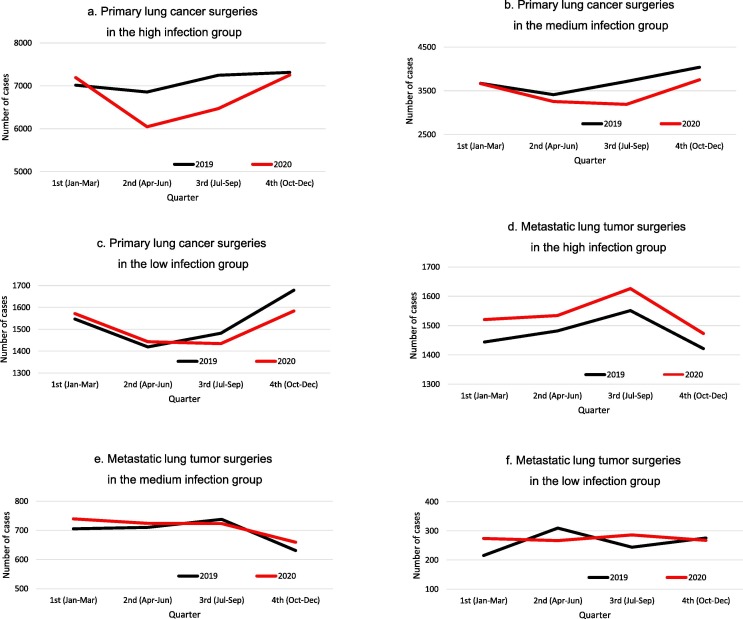
3.3. Quarterly changes in primary lung cancer and metastatic lung tumor dependent on the degree of infection
In the high infection group, the quarterly numbers of surgeries for primary lung cancer in 2020 decreased significantly in the second (−11.8 %) and third quarters (−10.7 %) compared with 2019 (Fig. 4 a). In the middle infection group, the quarterly numbers of surgeries for primary lung cancer in 2020 decreased in the third (−14.1 %) and fourth quarters (−7.2 %) compared to 2019 (Fig. 4b). In the low infection group, the quarterly numbers of surgeries for primary lung cancer in 2020 decreased only in the fourth quarter (−5.7 %) compared to 2019 (Fig. 4c).
Fig. 4.
Quarterly trends in number of primary lung cancer and metastatic lung tumor surgeries by level of infection.
In the high infection group, the quarterly numbers of surgeries for metastatic lung tumor in 2020 increased in all quarters compared to those in 2019 (Fig. 4d). In the middle and low infection groups, the quarterly numbers of surgeries for metastatic lung tumor in 2020 showed no clear trend compared to those in 2019 (Fig. 4e and f).
3.4. The change in basic and perioperative factors of primary lung cancer and metastatic lung tumor
There were no apparent differences in age, sex, and performance status of patients who underwent surgical treatment for primary lung cancer in 2020 compared to 2019. There were no differences in histology, clinical stage, or total and solid tumor size. Regarding the mode of the surgery, lobectomy slightly decreased (−2.4 %), and there was a slight increase in segmentectomy (+1.4 %) and partial resection (+1.0 %). As to approach, video-assisted thoracoscopic surgery decreased by 4.8 %, and there were increases in robotic surgery (+2.4 %) and open chest surgery (+2.4 %). There were no changes in the operation time, bleeding amount, or use of extracorporeal circulation support during the surgery. There were also no changes in postoperative complications, readmission, or 30-day mortality; however, the length of hospital stay was shortened from eight to seven days (Supplemental data: Table 1 ). There were no apparent differences in the basic and perioperative factors of metastatic lung tumor (data not shown).
Table 1.
The change in basic and perioperative factors of primary lung cancer.
| 2019 | 2020 | vs 2019 | ||
|---|---|---|---|---|
| Age | −59 | 5627 (11·6%) | 5058 (11·0%) | −0·6% |
| 60–69 | 12,892 (26·7%) | 11,597 (25·3%) | −1·4% | |
| 70–79 | 22,997 (47·6%) | 22,616 (49·3%) | 1·7% | |
| 80- | 6801 (14·1%) | 6647 (14·5%) | 0·4% | |
| Sex | female | 19,150 (39·6%) | 17,786 (38·7%) | −0·9% |
| male | 29,167 (60·4%) | 28,132 (61·3%) | 0·9% | |
| PS | PS0 | 40,591 (84·0%) | 38,558 (84·0%) | 0·0% |
| PS1 | 5951 (12·3%) | 5630 (12·3%) | 0·0% | |
| PS2-4 | 1775 (3·7%) | 1730 (3·8%) | 0·1% | |
| Neoadjuvant therapy | 953(2·1%) | 911(2·1%) | 0·0% | |
| Mode of surgery | Pneumonectomy | 283 (0·6%) | 255 (0·6%) | 0·0% |
| Segmentectomy | 5501 (11·4%) | 5866 (12·8%) | 1·4% | |
| Lobectomy | 33,809 (70·0%) | 31,061 (67·6%) | −2·4% | |
| Partial resection | 8721 (18·0%) | 8732 (19·0%) | 1·0% | |
| Approach | Robotic | 2073 (4·3%) | 3092 (6·7%) | 2·4% |
| VATS | 41,369 (85·6%) | 37,097 (80·8%) | −4·8% | |
| Open | 4875 (10·1%) | 5729 (12·5%) | 2·4% | |
| Operative time | 175 (125–231) | 174 (123–230) | −0·6% | |
| Blood loss | 21 (10–80) | 20 (10–70) | −4·8% | |
| Clinical Stage | 0 | 2303 (4·8%) | 2077 (4·5%) | −0·3% |
| IA1 | 8823 (18·3%) | 8609 (18·7%) | 0·4% | |
| IA2 | 14,079 (29·1%) | 13,718 (29·9%) | 0·8% | |
| IA3 | 8484 (17·6%) | 7904 (17·2%) | −0·4% | |
| IB | 5290 (10·9%) | 4937 (10·8%) | −0·1% | |
| IIA | 1699 (3·5%) | 1514 (3·3%) | −0·2% | |
| IIB | 3999 (8·3%) | 3736 (8·1%) | −0·2% | |
| IIIA | 2654 (5·5%) | 2425 (5·3%) | −0·2% | |
| IIIB | 442 (0·9%) | 434 (0·9%) | 0·0% | |
| IIIC | 12 (0·0%) | 20 (0·0%) | 0·0% | |
| IVA | 348 (0·7%) | 351 (0·8%) | 0·1% | |
| IVB | 76 (0·2%) | 97 (0·2%) | 0·0% | |
| Total diameter | 2·2 (1·5-3·2) | 2·2 (1·5-3·1) | 0·0% | |
| Consolidation diameter | 1·9 (1·1-2·9) | 1·8 (1·1-2·8) | −5·3% | |
| Historogy | Adenoca. | 34,491 (71·4%) | 32,030 (69·8%) | −1·6% |
| Squamous ca. | 8669 (17·9%) | 8278 (18·0%) | 0·1% | |
| Others | 5157 (10·7%) | 5610 (12·2%) | 1·5% | |
| Complications | Pneumonia | 1070 (2·3%) | 1023 (2·1%) | 0·2% |
| Atelectaissi | 262 (0·5%) | 251 (0·5%) | 0·0% | |
| Pyothorax | 389 (0·8%) | 331 (0·7%) | −0·1% | |
| IP exacerbation | 270 (0·6%) | 250 (0·5%) | −0·1% | |
| Air leakage >7 days | 2461 (5·1%) | 2412 (5·3%) | 0·2% | |
| Respiratory failure | 202 (0·4%) | 209 (0·5%) | 0·1% | |
| Pulmonary embolism | 63 (0·1%) | 63 (0·1%) | 0·0% | |
| Hospital stay | 8 (6–10) | 7 (6–10) | −12·5% | |
| Re-admission <30 days | 852 (1·8%) | 812 (1·8%) | 0·0% | |
| Mortality <30 days | 171 (0·4%) | 168 (0·4%) | 0·0% |
Abbreviations: PS = performance status, VATS = video assisted thoracic surgery, IP = interstitial pneumonia.
3.5. Examinees of lung cancer screening
According to the investigation by the Japan Cancer Society, compared to 2019, the number of examinees of lung cancer screening in 2020 all over Japan decreased drastically from April to August, but gradually recovered towards the end of the year (Fig. 5 a). The numbers of lung cancer screening examinees from January to March in both 2019 and 2020 were low; however, this is to be expected because lung cancer screening is usually administered from April to November with the start of the new fiscal year (which begins in April in Japan). The changes in lung cancer screening examinees and lung cancer surgery between 2019 and 2020 clearly showed that the decrease in lung cancer screening examinees was one to two months precedent to the decrease in lung cancer surgery (Fig. 5b).
Fig. 5.
Monthly trend in the number of lung cancer screening examinees in 2019 and 2020 (a), and the changes in 2020 compared to 2019 in the number of lung cancer screening examinees and lung cancer surgeries (b).
4. Discussion
This study was conducted to evaluate the impact of the COVID-19 pandemic on general thoracic surgeries performed in Japan by analyzing the effects on a total and three representative surgical procedures for tumors in 2020. We also evaluated the effect of the pandemic on the decrease of lung cancer screening and its implications for lung cancer surgery.
The numbers of total surgeries in general thoracic surgery and surgeries for primary lung cancer in 2020 according to the NCD showed estimated 8.3 and 10.1 % decrease respectively, speculated from the steady annual increase from 2014 to 2019. To evaluate the changes in 2020, it is important to consider such recent trends, as a simple comparison with the 2019 numbers could significantly underestimate the impact. This was borne out in the current study, where the decrease in the number of total and primary lung cancer surgeries in 2020 was more evident when the trends from 2014 to 2019 were taken into account. In 2020, the monthly number of surgeries for primary lung cancer decreased markedly from May to August, bottomed in July, and returned to 2019 levels by the end of the year. In the quarterly analysis by degree of regional infection level, the number of primary lung cancer surgeries decreased earlier and to a larger extent in high-infection regions compared to low-infection regions. This infection-level-dependent discrepancy reflects the difference in the magnitude of infection and the delayed spread of COVID-19 from regions of high- to low-level infection.
In contrast to the findings discussed above, the number of surgeries for metastatic lung tumor increased, which was similar to the trend the of annual increase observed from 2014 to 2019 (Fig. 3b). Even in high-infection regions, the number of surgeries for metastatic lung tumor increased in all quarters of 2020. As primary lung cancer and metastatic lung tumor are similar, both being malignant lung tumor, one would expect that the underlying principles guiding decision-making for surgical treatment should have been similar; however, we observed differing trends in 2020.
There are two possible reasons for the decrease in primary lung cancer surgeries during the pandemic: first, the triage of surgical procedures due to the decrease in hospital resources represented by the number of available beds in intensive care units [11]; and second, the decrease in lung cancer diagnosis due to the decrease of lung cancer screening, which might be induced by the temporary closure of screening and the decreased motivation for attending screening due to COVID-19 related concerns [12]. If the main cause was triage of surgical procedures, one would expect a similar, not contrastive, trend for both primary and metastatic lung tumor surgery. The number of people infected with COVID-19 increased most extensively in the third wave at the end of 2020 (Fig. 1), and the peak number of patients hospitalized due to COVID-19 in the third wave was more than double compared to those in the first and second waves [13]; accordingly, the triage of surgical procedures must have been more severe during the third peak. However, the number of surgeries for primary lung cancer recovered towards the end of the year from the lowest point in the summer, even in regions with relatively high levels of infection, which indicates that the impact of surgical triage seems to have been very limited.
Lung cancer screening using chest radiography for all examinees and sputum cytology for smokers was introduced as part of the Japanese annual health check in 1982 under the Health and Medical Services Law and is currently conducted as a national policy based on the Basic Act on Cancer Control law. Now nationally available, a significant number of adults undergo annual lung cancer screening; according to the Japanese MHLW, 53.4 % of men and 45.6 % of women aged 40 to 69 years old, received lung cancer screening in 2019 according to the Comprehensive Survey of Living Conditions [14]. Although chest radiography used for lung cancer screening in Japan, might not be as effective for the reduction of lung cancer death compared to CT screening [15], its wide applicability indicates its potential for reducing the risk of lung cancer mortality [16], [17]. According to the investigation by the Japan Cancer Society, introduced in this study, the number of lung cancer screening examinees decreased markedly in 2020, which must have resulted in the decrease in lung cancer diagnosis and the advancement of lung cancer (Fig. 5a). Similar substantial COVID-19 related reductions in procedures to diagnose cancer have also been reported in a limited number of participants [6], and in estimations of the negative implications of diagnoses with worse long-term outcomes during the pandemic [12], [18]. Our study demonstrated a nation-wide reduction of lung cancer surgery associated with a reduction in lung cancer screening examinees one to two months prior (Fig. 5b). In Japan, the number of examinees decreased drastically from April to August 2020, with the lowest number in May, and gradually recovered towards the end of the year. As there is a delay of a few months from screening to the treatment, the decrease in screening examinees, which bottomed in May, is suspected to account for the decrease in primary lung cancer surgeries, which bottomed in July. The hazard of delayed treatment on patient prognosis is more severe for those with stage I to II cancer who are likely to be asymptomatic and who are usually diagnosed through screening compared to patients with advanced cancer, stage III or IV, who are likely to be symptomatic [19]. Delay in diagnosis and resection are both associated with increased rates of upstaging and decreased median survival even in stage I non-small cell lung cancer [5]. Although the exact impact of the COVID-19 pandemic on lung cancer diagnosis has not yet been elucidated, a model analysis of the impact of COVID-19 related delays in the diagnosis of non-small cell lung cancer suggested deterioration of the 5-year survival [20].
The evidence of COVID-19 countermeasures, such as mRNA vaccine and monoclonal antibody technology, demonstrates the minimal risk of viral exposure that accompanies lung cancer screening [21]; therefore, it is necessary to continue lung cancer screening with proper prophylaxis even during a pandemic to avoid delay in the treatment which will worsen patient outcomes [22].
In contrast, metastatic lung tumors are mostly diagnosed through regular follow-up examinations for the primary tumor rather than lung cancer screening [23]. As the trend regarding the number of annual metastatic lung tumor surgery remained unaltered in 2020, it can be said that essential medical care for cancer patients, including outpatient follow-up, was maintained despite the pandemic. This difference in patient recruitment could explain the contrasting trends between primary lung cancer and metastatic lung tumor surgery.
The number of mediastinal tumor surgeries decreased quite similar to that observed for primary lung cancer, and this similarity can be explained by the fact that mediastinal tumor, like primary lung cancer, is mainly diagnosed with chest radiographic screening.
Most of the basic and perioperative factors did not change in 2020, except for slight changes in the mode and approach of surgery for primary lung cancer and the length of hospital stay. The slight decrease in lobectomy with the increase in segmentectomy and partial resection might have reflected the trend for limited resection for early stage lung cancer or poor-risk patients in recent years [24]. The decrease in video-assisted thoracic surgery and the slight increase in robotic and open chest surgery might have reflected the spread of robotic surgery and the aversion of surgical smoke in endoscopic surgery that has recently gained attention within surgical societies such as the American College of Surgeons [25]. The shortening of the hospital stay from 8 to 7 days might be attributable to measures for securing intensive care resources for patients with COVID-19 [26]. Despite minimal changes in the mode of operation and surgical approach, it can be said that the surgical treatment for primary lung cancer was largely maintained qualitatively. In the first year of the COVID-19 pandemic, the clinical stage and tumor size of the patients who underwent surgery did not change. The observed period might have been too short to analyze the advancement of lung cancer; however, early stage lung cancers that are left unscreened might be detected as advanced cancer in the future. Therefore, further detailed studies on lung cancer could help to verify whether there is a stage shift in surgical cases over the next few years.
4.1. Strengths and limitations
To the best of our knowledge, our analysis is the first to show, not to estimate, a real decrease in lung cancer surgery nationwide using the NCD (which accounts for more than 90 % of all surgeries performed in Japan [9], [10]) in association with the decrease in lung cancer screening. Despite the utilization of a large, reliable, nationwide surgical registry and questionnaires, this study has several limitations. First, only short-term surgical data was registered in the registry; no long-term data was available. Second, we could use only the data obtained from the registry and questionnaires. These limitations might affect the generalizability of the findings of the present study.
5. Conclusion
The total number of general thoracic surgeries, and the number of surgeries for primary lung cancer and mediastinal tumor substantially decreased in 2020. The decrease in primary lung cancer cases seems to be mainly a result of the decrease in primary lung cancer diagnoses due to the decrease in lung cancer screening rather than any pandemic-related triage of surgical procedures. Our findings highlight the importance of continuing lung cancer screening even during a pandemic.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Hiroyuki Yamamoto is affiliated with the Department of Healthcare Quality Assessment of the University of Tokyo. The department is a social collaboration department supported by grants from the National Clinical Database, Johnson & Johnson K.K., and Nipro Co. The other authors declare no conflicts of interest regarding the submitted article.
Acknowledgments
Acknowledgments
We thank Thomas Mayers, Medical English Communications Center, University of Tsukuba for reviewing and editing the manuscript.
Funding
This work was supported by the MHLW Special Research Program (grant Number JPMH20CA2046).
References
- 1.N. Zhu, D. Zhang, W. Wang, X. Li, B. Yang, J. Song, X. Zhao, B. Huang, W. Shi, R. Lu, P. Niu, F. Zhan, X. Ma, D. Wang, W. Xu, G. Wu, G.F. Gao, W. Tan, I. China Novel Coronavirus, T. Research. A Novel Coronavirus from Patients with Pneumonia in China. 2019. New England Journal of Medicine. 382(8). (2020). 727-733. [DOI] [PMC free article] [PubMed]
- 2.About Coronavirus Disease 2019 (COVID-19). 2020. 2022. https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou.html. (Accessed 1 Feb 2022).
- 3.Soreide K., Hallet J., Matthews J.B., Schnitzbauer A.A., Line P.D., Lai P.B.S., Otero J., Callegaro D., Warner S.G., Baxter N.N., Teh C.S.C., Ng-Kamstra J., Meara J.G., Hagander L., Lorenzon L. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. British Journal of Surgery. 2020;107(10):1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carr A., Smith J.A., Camaradou J., Prieto-Alhambra D. Growing backlog of planned surgery due to covid-19. BMJ. 2021;372 doi: 10.1136/bmj.n339. [DOI] [PubMed] [Google Scholar]
- 5.P. Samson, A. Patel, T. Garrett, T. Crabtree, D. Kreisel, A.S. Krupnick, G.A. Patterson, S. Broderick, B.F. Meyers, V. Puri. Effects of Delayed Surgical Resection on Short-Term and Long-Term Outcomes in Clinical Stage I Non-Small Cell Lung Cancer. Annals of Thoracic Surgery. 99(6). (2015). 1906-12. discussion 1913. [DOI] [PMC free article] [PubMed]
- 6.Van Haren R.M., Delman A.M., Turner K.M., Waits B., Hemingway M., Shah S.A., Starnes S.L. Impact of the COVID-19 Pandemic on Lung Cancer Screening Program and Subsequent Lung Cancer. Journal of the American College of Surgeons. 2021;232(4):600–605. doi: 10.1016/j.jamcollsurg.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Japan Anticancer Society Report. Japan Anticancer Society. 2021. 1.
- 8.Ikeda N., Yamamoto H., Taketomi A., Hibi T., Ono M., Niikura N., Sugitani I., Isozumi U., Miyata H., Nagano H., Unno M., Kitagawa Y., Mori M. The impact of COVID-19 on surgical procedures in Japan: analysis of data from the National Clinical Database. Surgery Today. 2022;52(1):22–35. doi: 10.1007/s00595-021-02406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miyata H., Gotoh M., Hashimoto H., Motomura N., Murakami A., Tomotaki A., Hirahara N., Ono M., Ko C., Iwanaka T. Challenges and prospects of a clinical database linked to the board certification system. Surgery Today. 2014;44(11):1991–1999. doi: 10.1007/s00595-013-0802-3. [DOI] [PubMed] [Google Scholar]
- 10.Ikeda N., Endo S., Fukuchi E., Nakajima J., Yokoi K., Chida M., Date H., Iwasaki A., Yokomise H., Sato M., Okumura M., Yamamoto H., Miyata H., Kondo T. Current status of surgery for clinical stage IA lung cancer in Japan: analysis of the national clinical database. Surgery Today. 2020;50(12):1644–1651. doi: 10.1007/s00595-020-02063-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta S., Batt J., Bourbeau J., Chapman K.R., Gershon A., Granton J., Hambly N., Hernandez P., Kolb M., Mehta S., Mielniczuk L., Provencher S., Stephenson A.L., Swiston J., Tullis D.E., Vozoris N.T., Wald J., Weatherald J., Bhutani M. Triaging Access to Critical Care Resources in Patients With Chronic Respiratory Diseases in the Event of a Major COVID-19 Surge: Key Highlights From the Canadian Thoracic Society (CTS) Position Statement. Chest. 2020;158(6):2270–2274. doi: 10.1016/j.chest.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Englum B.R., Prasad N.K., Lake R.E., Mayorga-Carlin M., Turner D.J., Siddiqui T., Sorkin J.D., Lal B.K. Impact of the COVID-19 pandemic on diagnosis of new cancers: A national multicenter study of the Veterans Affairs Healthcare System. Cancer. 2021;06:06. doi: 10.1002/cncr.34011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.About the hospitalized patient due to COVID-19, 2022. https://www.mhlw.go.jp/stf/seisakunitsuite/newpage_00023.html.
- 14.Foundation for Promotion of Cancer Research. Cancer statistics in Japan 2021, https://ganjoho.jp/public/qa_links/report/statistics/2021_en.html., 2021.
- 15.T. National Lung Screening Trial Research, D.R. Aberle, A.M. Adams, C.D. Berg, W.C. Black, J.D. Clapp, R.M. Fagerstrom, I.F. Gareen, C. Gatsonis, P.M. Marcus, J.D. Sicks, Reduced lung-cancer mortality with low-dose computed tomographic screening, New England Journal of Medicine 365(5) (2011) 395-409. [DOI] [PMC free article] [PubMed]
- 16.Horinouchi H., Kusumoto M., Yatabe Y., Aokage K., Watanabe S., Ishikura S. Lung Cancer in Japan, Journal of Thoracic Oncology: Official Publication of the International Association for the Study of. Lung Cancer. 2021;17(3):353–361. doi: 10.1016/j.jtho.2021.11.020. [DOI] [PubMed] [Google Scholar]
- 17.Sagawa M., Nakayama T., Tsukada H., Nishii K., Baba T., Kurita Y., Saito Y., Kaneko M., Sakuma T., Suzuki T., Fujimura S. The efficacy of lung cancer screening conducted in 1990s: four case-control studies in Japan. Lung Cancer. 2003;41(1):29–36. doi: 10.1016/s0169-5002(03)00197-1. [DOI] [PubMed] [Google Scholar]
- 18.Patt D., Gordan L., Diaz M., Okon T., Grady L., Harmison M., Markward N., Sullivan M., Peng J., Zhou A. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clinical Cancer Informatics (4) 2020:1059–1071. doi: 10.1200/CCI.20.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zuniga P.V.S., Ost D.E. Impact of Delays in Lung Cancer Treatment on Survival. Chest. 2021;160(5):1934–1958. doi: 10.1016/j.chest.2021.08.051. [DOI] [PubMed] [Google Scholar]
- 20.M.E. Shipe, D.N. Haddad, S.A. Deppen, B.D. Kozower, E.L. Grogan, Modeling the Impact of Delaying the Diagnosis of Non-Small Cell Lung Cancer During COVID-19, Annals of Thoracic Surgery 112(1) 248-254. [DOI] [PMC free article] [PubMed]
- 21.R.M. Huber, M. Cavic, A. Kerpel-Fronius, L. Viola, J. Field, L. Jiang, E.A. Kazerooni, C.F.N. Koegelenberg, A. Mohan, R. Sales Dos Santos, L. Ventura, M. Wynes, D. Yang, J. Zulueta, C.T. Lee, M.C. Tammemagi, C.I. Henschke, S. Lam, G. members of the Diagnostics Working, D. Early, C. Screening, Lung Cancer Screening Considerations During Respiratory Infection Outbreaks, Epidemics or Pandemics: An International Association for the Study of Lung Cancer Early Detection and Screening Committee Report, Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer 17(2) (2022) 228-238. [DOI] [PMC free article] [PubMed]
- 22.Johnson B.A., Waddimba A.C., Ogola G.O., Fleshman J.W., Jr., Preskitt J.T. A systematic review and meta-analysis of surgery delays and survival in breast, lung and colon cancers: Implication for surgical triage during the COVID-19 pandemic. American Journal of Surgery. 2021;222(2):311–318. doi: 10.1016/j.amjsurg.2020.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Snyder B.J., Pugatch R.D. Imaging characteristics of metastatic disease to the chest. Chest Surgery Clinics of North America. 1998;8(1):29–48. [PubMed] [Google Scholar]
- 24.Okumura M. Trends and current status of general thoracic surgery in Japan revealed by review of nationwide databases. Journal of Thoracic Disease. 2016;8(Suppl 8):S589. doi: 10.21037/jtd.2016.06.44. S595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVID-19: Considerations for Optimum Surgeon Protection Before, During, and After Operation, American College of Surgeons, https://www.facs.org/covid-19/clinical-guidance/surgeon-protection.
- 26.Norisue Y., Deshpande G.A., Kamada M., Nabeshima T., Tokuda Y., Goto T., Ishizuka N., Hara Y., Nakata R., Makino J., Matsumura M., Fujitani S., Hiraoka E. Allocation of Mechanical Ventilators During a Pandemic: A Mixed-Methods Study of Perceptions Among Japanese Health Care Workers and the General Public. Chest. 2021;159(6):2494–2502. doi: 10.1016/j.chest.2021.01.015. [DOI] [PubMed] [Google Scholar]