Abstract
Health literacy (HL) is critical to find, understand and use health information for adopting appropriate health behavior, especially during a pandemic crisis in which people can be exposed to an overwhelming amount of information from different media. To this end, we conducted an online study to first validate the measure of COronaVIrus Disease appeared in 2019 (COVID-19) health literacy (CoHL) and then investigated its relationships with locus of control (LoC), news information search and the adoption of protective behaviors (PBs) during the first lockdown in France. We first showed the good structural and psychometric qualities of the CoHL scale on a 3-dimensional structure: the Critical dimension, the Extraction/Communicative and the Application/Communicative dimension. We then found that CoHL was associated with the adoption of PBs suggesting that people with higher CoHL tended to adopt more PBs during the first lockdown, regardless of their LoC. However, people with low CoHL would be more likely to adopt PBs if they believe that they may get COVID-19 due to the behavior and health conditions of others (high external LoC). The study has implications for the design of public health campaigns for people with inadequate HL and with a different LoC.
Introduction
Facing the challenges of the global health crisis caused by the COronaVIrus Disease appeared in 2019 (COVID-19) pandemic, compliance with sanitary rules and the adoption of recommended protective measures are at stake in the fight against the spread of the virus [1]. To reduce this risk, almost all countries were locked down over a period of 6 months more or less in 2020. The prevention campaigns have been launched globally to emphasize the importance of social distancing as an effective approach to prevent the spread of the pandemic, which information has been available on various media (TV news, newspapers, radio, social networks, websites, etc.). In addition to social distancing, a lot of information on COVID-19 varying in relevance and accuracy (such as the information about its origin, infection path, contagiousness, preventive measures, symptoms management, treatment, etc.) has been prevalent on the Internet, TV and radio. Nevertheless, information available on the Internet is not always reliable, and the user engagement of the information (e.g. the number of downloads of the COVID-19-related YouTube videos) is not associated with the reliability of information [2]. Therefore, it is critical for individuals to have the capacity to differentiate high- versus low-quality health information, obtain accurate information, process and understand information to develop behaviors that allow them to protect themselves and others against the virus. Indeed, Thacker et al. [3] showed that people who knew and understood COVID-19-related restrictions were more likely to adhere to them. Consequently, the overarching goal is to promote citizens to modify everyday social interaction behaviors toward forming new daily habits of health prevention behaviors.
To this end, our study plans to identify the psychosocial and cognitive determinants that influence the adoption of these new protective behaviors (PBs). A recent study on the adherence to social distancing and masks-wearing in the United States has shown that the confidence in scientific information and the perception of information overload together influence adherence to these recommendations on PBs [4]. Given the prevalence of misinformation about COVID-19, we argue that health literacy (HL) would play an important role in adherence to recommended protective measures (e.g. social distancing, masks-wearing).
HL is defined as the ability to obtain, process and understand basic health information for making health-related decisions [5]. This is central to promoting public health as underlined by the World Health Organization [6]. Sørensen et al. [7, p. 3] proposed a more comprehensive definition (based on a literature review listing 17 definitions): HL ‘entails people’s knowledge, motivation and competences to access, understand, appraisal and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course’. Specifically, Nutbeam [8, 9], as well as Sørensen et al. [7] identified three dimensions of HL:
(1) Functional dimension refers to the ‘basic’ reading and writing skills required to understand health-related information.
(2) Interactive or communicative dimension refers to a combination of cognitive, literacy and social skills to allow individuals to extract, understand and utilize information from various contexts.
(3) Critical dimension refers to advanced cognitive and social skills that allow individuals to perform a critical analysis on health information, and use it to develop greater control over their lives.
Established evidence has demonstrated the role of HL on health outcomes. For instance, low HL often led to poor health outcomes and self-care [e.g. 10, 11, 12, 7], higher mortality, more hospitalizations and difficulties to adhere to medication [13, 7]. Poor HL is often related to low education, low income and aging [14, 15, 16, 17 for a review]. Therefore, HL is crucial to protect oneself and others to lower the likelihood of infection during the COVID-19 pandemic. Indeed, the COVID-19 pandemic can be considered a unique situation since (i) The concern is universal all around the world, (ii) anyone can be infected by the virus, and some people may develop severe forms of illness and die (generally vulnerable people, i.e. with comorbidities and/or elderly), (iii) information is prevalent and even overwhelmed in our environment from various sources, such as governments, Internet and social networks, which differs in relevance and accuracy. More importantly, [1] has recognized COVID-19 infodemic as an ongoing challenge for the citizens to decide how to obtain, process and understand the COVID-19-related information. Therefore, being able to assess COVID-19-related HL is very important to understand possible difficulties experienced by individuals to adopt protective measures, such as social distancing (to keep themselves and others healthy during the pandemic) which is jointly affected by their age, education and how they gather COVID-19 information.
Besides, the locus of control (LoC) may be another interesting determinant in relation to COVID-19-related HL in the pandemic. The LoC is a construct that originates from the social learning theory [18]. It is defined as the expectation of control that reflects the degree of representation that individuals possess of the relationship between their behaviors and/or their personal characteristics and the positive or negative reinforcements they receive. Originally, this approach proposed two kinds of LoC, including internal and external LoC. Recent studies applying LoC to understand health behavior or well-being have extended the two LoC. The third dimension ‘the powerful others’ has been included to take into account the influence of significant others, as well as the fourth dimension which distinguishes ‘the powerful others’ into people with two different levels of emotional distance such as colleagues and superiors [19]. In the COVID-19 pandemic where the authorities (including government agencies) have been playing a crucial role to implement public health (such as lockdowns), we then proposed to examine four types of LoC, including ‘self’ (i.e. internal LoC), ‘others’, ‘the government’, then ‘chance’ (characterizing the influence of external factors, such as luck or chance).
Prior studies have shown that LoC was related to health outcomes [see in 20]. A low level of internal LoC may limit individuals to apply their HL skills and to modify their behaviors to improve their health. Or, people with high levels of internal LoC may use other resources to overcome poor HL skills [20]. A study on Arabs and Jews living in Israel, [20] showed internal LoC was a mediator between HL and self-report perceived health status. More precisely, individuals with high levels of internal LoC reported better-perceived health than those with low levels of internal LoC (since the former ones perceived more accountability to control their own health). Sigurvinsdottir et al. [21] showed that individuals with high internal LoC were more active on the Internet to search for COVID-19 information. Roncancion et al. [22] showed similar results that people with high internal LoC were more likely to search for health information to assist their self-care.
Previous studies have demonstrated the importance of LoC along with HL on health outcomes. The current study would like to extend the relations between HL and LoC on the adoption of COVID-19-related PBs, such as social distancing and mask-wearing, which were prescribed by government authorities. This research has implications to understand whether the promotion of HL and specific LoC could lead to the adoption of protective measures, which in turn lead to the control of the spread of COVID-19. Hence, this article presents a study whose objective was to validate the reliability of the CoHL scale on a French population during the first mandatory lockdown (from March to May 2020), and examine its relations with the adoption of PBs, news information search (NIS) and LoC. We hypothesized that higher CoHL would be associated with better compliance with protective measures, which could be moderated by LoC.
Method
Participants
1248 people living in France were recruited in the study, with the 1025 participants entered in the final analysis (female 80%). Age ranged between 18 years and 85 years (M = 39.84, SD = 13.73), with the majority of participants from 18 to 40 years old (55%) (41 to 60 years old and 61 to 85 years old: 36.7% and 8.2%, respectively). Regarding the employment situation, 33% reported currently teleworking at home; 19.1% experiencing job loss or decrease of total or partial occupation (artists, craftspeople, shopkeepers and restaurateurs); 9.3% being unemployed prior to the lockdown period; 9.2% being a student and 7.1% being retired. Concerning the education level of the participants, 2% have no diploma; 13.8% have a high school diploma; 16.9% were undergraduates; 14.8% were graduates and 35.3% were postgraduates.
Procedure
The data were collected through a self-administered anonymous online survey from the third to the fifth week of the first lockdown in France (April 2020). Respondents were recruited via virtual snowball sampling instead of random sampling [23, 24]. Specifically, potential participants were recruited through social, professional, university media and announcements in the press journalist without monetary compensation. In compliance with the General Data Protection Regulation (GDPR), participants were given informed consent on the introductory page of the online survey and agreed to participate in the study by checking the checkbox to launch the study. Eligibility criteria included living in France and being 18 years old or older.
Measures
Participants completed an online battery that included five surveys about (i) their demographic information (e.g. gender, age, education and employment situation), (ii) NIS behavior: one question about the frequently participants checking the news on a 5-point Likert scale (all the time continuously, several times a day, once a day, several times a week, once a week, never), (iii) the adoption of PBs to prevent COVID-19: 13 items about the frequencies to perform protective measures, including keeping social distance, use of sanitary mask (and gloves) and washing behaviors, on a 7-point Likert scale from ‘never’ to ‘all the time’, (iv) the LoC about being infected by COVID-19: 4 items about how they would attribute the cause of COVID-19 infection to the following dimensions if they get infected: ‘self’, ‘the others’, ‘the government’, and the chance (implying the influence of external factors, such as luck or chance) on a 7-point Likert scale from ‘strongly disagree’ to ‘strongly agree’, (v) CoHL: eight remaining items from the French version of the Functional, Communicative and Critical Health Literacy scale (FCCHL) which was validated by Ousseine et al. [25].
Statistical analysis
All analyses were performed using SPSS and AMOS Statistics 26.0.
First, statistical analyses were performed to test the construct and internal validity of the COVID-19 Literacy scale based on an iterative approach combining using the internal reliability test, Principal Axis Factoring (PAF) and Confirmatory Factor Analysis (CFA) [26]. In a previous adaptation, the measurement of literacy applied to health has experienced structural differences in the dimensions (see for an adaptation among German citizens [27]). Here, all the indicators were stronger without the Functional HL items that reduce overall psychometric quality given the explained variance, the alpha and the fit indexes altogether. It can be related to the fact that COVID-19-related information was very widely disseminated to a large audience (on all channels in various formats: written, oral and video forms) minimizing the cognitive cost and effort to proactively find information and that in a most intelligible format. Hence, we introduce here the results of analyses on the best-performing form of the CoHL scale.
We first examined the psychometrics of the adapted CoHL scale using PAF and CFA. We then conducted correlations on the relationships among age, education levels, CoHL, adoption of PBs, NIS behavior and four types of LoC. We used regression analysis to examine the relationships between CoHL and the adoption of PBs as well as other correlates. A slope analysis was further used to confirm the moderating effect of LoC on the link between HL and the adoption of PBs.
Results
Structure and properties of the CoHL
We conducted PAF with a Parallel Analysis (PA) utilizing the script developed by O’Connor [28, 29]. This procedure generates eigenvalues from the raw data (including the mean eigenvalues and 95th percentile eigenvalues) based on the Monte Carlo simulation. We adopted Promax rotation and concluded with a three-factor structure (see Table I). Altogether these three factors explain 64.7% of the variance that is regarded as a satisfactory level in the social sciences (see [30], p. 107, on the acceptable minimum explained variance in factor analysis).
Table I.
EFA with Promax rotation on the COVID-19 Health Literacy scale: factors loadings and commonalities
| First factor | Second factor | Third factor | Final commonalities | |
|---|---|---|---|---|
| Extraction/Communicative CoHL (EXCOM) | ||||
| Item 1: I gather information from several sources. (Je rassemble des informations de plusieurs sources.) |
0.22 | 0.78 | 0.29 | 0.61 |
| Item 2: I extract the information I want. (J’extraie les informations que je souhaite.) |
0.11 | 0.78 | 0.20 | 0.60 |
| Item 3: I understand the information obtained. (Je comprends l’information obtenue.) |
0.13 | 0.72 | 0.27 | 0.52 |
| Application/Communicative CoHL (APPCOM) | ||||
| Item 4: I share my opinion on this disease with my entourage (Je partage mon opinion sur cette maladie avec mon entourage.) |
0.120 | 0.30 | 0.80 | 0.64 |
| Item 5: I use the information obtained to change my daily life. (J’utilise les informations obtenues pour changer mon quotidien.) |
0.21 | 0.25 | 0.84 | 0.70 |
| Critical CoHL (CRITIC) | ||||
| Item 6: I wonder if the information applies to my case. (Je me demande si les informations s’appliquent à mon cas.) |
0.79 | 0.11 | 0.30 | 0.65 |
| Item 7: I wonder if the information is credible. (Je me demande si les informations sont crédibles.) |
0.88 | 0.15 | 0.07 | 0.79 |
| Item 8: I check that the information is reliable. (Je vérifie que les informations sont fiables.) |
0.801 | 0.24 | 0.15 | 0.65 |
| Explained variance | 32.36 | 19.64 | 12.67 | |
| Total variance explained (%) | 64.68 | |||
Factor loading values higher than 0.7 are bolded.
These items were translated from French to be presented in Table I but this English version does not constitute the validated version.
As shown in Table I, the three items from Critical COVID-19 Literacy were loaded on the first factor. We then found items in the Communicative literacy dimension loaded on two factors. One factor is related to the ability to obtain health information and derives meaning from different forms of communication, and the other factor is related to the ability to apply the new information to changing circumstances. We rename these two factors as Extraction/Communi-cative HL and Application/Communicative HL, respectively.
These factor loadings were satisfactory as far beyond the accepted threshold of 0.40 [31] and above any debate on it [32]. None of the items loaded highly on more than one factor. The final commonalities were high (>0.60) to moderate (>0.40; item 3 = 0.52) which does not require removing any item. Data factorability were supported by a significant Bartlett’s Sphericity test (χ2 = 1629.15, P < 0.0001) and a high KMO test value of sampling adequacy (0.70; which exceeded the minimum recommended value of 0.60 [33]). CFA under the ULS estimation also demonstrated good model fit of 3-factor model (Fig. 1) through multiple indices (including Goodness of Fit Index (GFI), Adjusted Goodness of Fit (AGFI), Parsimony Goodness of Fit Index (PGFI, see [34], in [35]), Parsimony Ratio (PRATIO, see [36]) and Root-Mean-Square Residual (RMR, see [37]; see Table II).
Fig. 1.
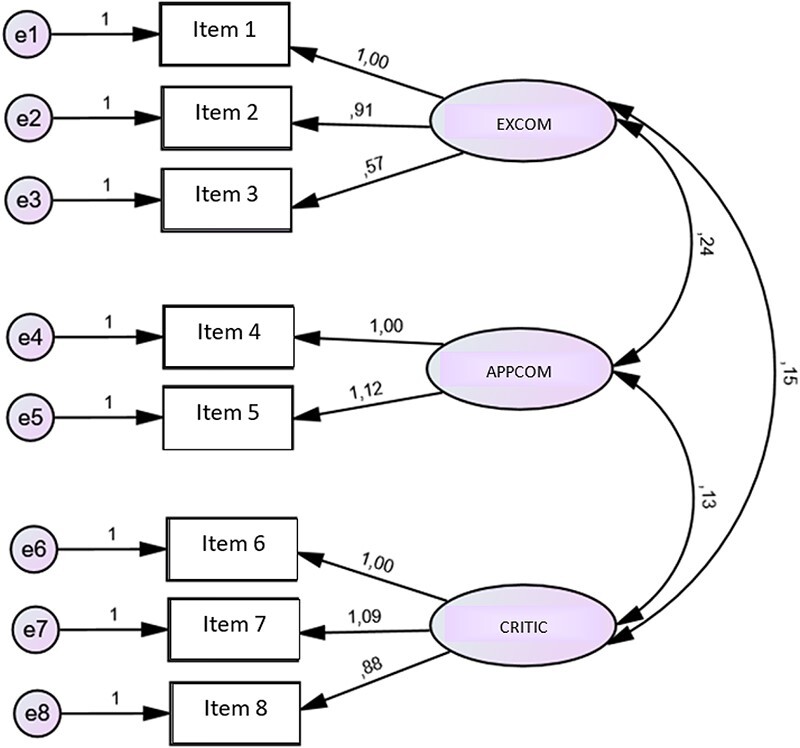
Standardized parameter estimates for the 3-factor model of COVID-19 health literacy scale (CoHL scale).
Table II.
Fit indexes
| Models | Df | GFI | AGFI | PGFI | PRATIO | RMR |
|---|---|---|---|---|---|---|
| Default | 17 | 0.99 | 0.98 | 0.47 | 0.61 | 0.04 |
Finally, reliability was assessed (Cronbach’s α = 0.69) suggesting an acceptable to a good level of internal reliability [38].
Relationship among CoHL, LoC, NIS behavior and the adoption of PBs
We conducted Pearson correlations among age, education (Edu), NIS, CoHL, the adoption of PBs, and four types of LoC (LoC 1: self, LoC2: others, LoC3: government, LoC4: chance). Results suggested that people with higher CoHL tended to have higher education, adopted more recommended PBs, and were more likely to believe that the COVID-19 infection is due to their behavior or health conditions of themselves or the others around them (see Table III).
Table III.
Correlations among age, education (Edu), news information seeking behavior (NIS), health literacy (CoHL), locus of control (LoC), and the adoption of protective behavior (PB)
| Age | Edu | PB | NIS | CoHL | LoC1 | LoC2 | LoC3 | LoC4 | |
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | 39.84 (13.73) | 5.05 (1.99) | 67.56 (11.29) | 2.91 (1.11) | 32.06 (4.53) | 4.53 (1.79) | 5.16 (1.62) | 3.87 (1.80) | 3.65 (1.84) |
| Edu | −0.16* | ||||||||
| PB | 0.18* | −0.11* | |||||||
| NIS | −0.28* | −0.04 | −0.08* | ||||||
| CoHL | 0.10* | 0.10* | 0.11* | −0.15* | |||||
| LoC1 | 0.07* | −0.07* | 0.10* | −0.04 | 0.08* | ||||
| LoC2 | 0.08* | −0.10* | 0.14* | 0.01 | 0.10* | 0.46* | |||
| LoC3 | 0.01 | 0.15* | 0.06 | −0.04 | 0.06 | 0.20* | 0.27* | ||
| LoC4 | 0.03 | −0.09* | −0.02 | −0.04 | 0.02 | −0.12* | −0.07* | −0.14* |
Note.*P < 0.05.
LoC1 refers to the control expectation that one may get the COVID-19 infection because of its self-behaviors. LoC2 refers to the control expectation that one may get COVID-19 infection because of others. LoC3 refers to the control expectation that one may get COVID-19 infection because of the government. LoC4 refers to the control expectation that one may get COVID-19 infection by bad chance.
Correlates of the adoption of PBs
We used multiple linear regressions to investigate the correlates of the PBs, including age, education, CoHL, NIS and two types of LoC (LoC1: self; LoC2: others). We also investigated how LoC (LoC1 and LoC2) moderated the associations between CoHL and PB by adding their interaction terms (CoHL × LoC1, CoHL × LoC2) in the regression models. We computed the Z scores of the correlates and entered these correlates step by step (see Table IV). Model 1 showed that age, education, and CoHL were associated with the adoption of PB (age: t = 4.74, P < 0.001, education: t = −2.97, P < 0.01, CoHL: t = 3.62, P < 0.001). NIS did not explain more variance in the adoption of PBs than age, education, and CoHL; we did not find NIS as a significant correlate in the regression models. Model 2 showed that in addition to the previous correlates, LoC2 (external) also explained more variance in the adoption of PB (age: t = 4.48, P < 0.001, education: t = −2.62, P < 0.01, CoHL: t = 3.20. = , P < 0.001, LoC2: t = 2.79. P < 0.01). After entering the interaction terms, Model 3 showed that the interaction term of CoHL and LoC2 (external) can further explain more variance in the adoption of PB in addition to prior correlates (age: t = 4.50, P < 0.001, education: t = −2.74, P < 0.01, CoHL: t = 3.24. = , P < 0.001, LoC2: t = 2.75. P < 0.01, CoHL × LoC2: t = −2.92, P < 0.01).
Table IV.
Regressions examining the correlates of the adoption of protective behavior
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| F | 13.83* | 11.49* | 9.92* |
| B (SE) | B (SE) | B (SE) | |
| Age | 0.15 (0.03)* | 0.14 (0.03)* | 0.14 (0.03)* |
| Education | −0.09 (0.03)* | −0.08 (0.03)* | −0.09(0.03)* |
| CoHL | 0.11(0.03)* | 0.10 (0.03)* | 0.10 (0.03)* |
| NIS | −0.02 (0.03) | −0.02(0.03) | −0.02(0.03) |
| LoC1 (locus of control: self) | 0.03 (0.03) | 0.03 (0.03) | |
| LoC2 (locus of control: others) | 0.10 (0.03)* | 0.09 (0.03)* | |
| CoHL × LoC1 | 0.02 (0.03) | ||
| CoHL × LoC2 | −0.10 (0.03)* |
Note.*P < 0.05.
We further conducted the slope analysis [39] to better understand the interaction term of CoHL and LoC2 (external LoC) on the adoption of PBs (Fig. 2). Results suggested that people with higher CoHL would adopt the PBs regardless of their belief on the LoC. However, for people with low CoHL, people who tended to believe that they may get infected by COVID-19 due to others were more likely to adopt the PBs than people who tended not to believe so.
Fig. 2.
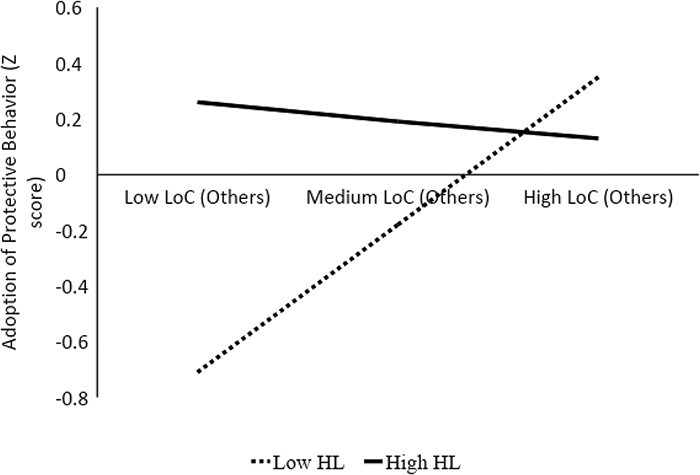
Interaction effect of health literacy and locus of control on the adoption of protective behavior.
Discussion
HL has been found to be associated with health behavior and outcomes. Hence, HL is particularly important during the COVID-19 pandemic given the exponentially increasing amount of information about COVID-19 being disseminated through multiple media or exchanged by family and friends. Having adequate CoHL could enable individuals to access, obtain and process appropriate COVID-19-related information and adopt the recommended PB for oneself and others. To this end, the current article aimed (i) to validate the development of the CoHL scale from a prior general HL scale [25] and (ii) to examine the relationships among CoHL, LoC (internal and external), NIS and the adoption of PBs, such as social and physical distancing.
First, the findings showed CoHL scale has good structural and psychometric qualities. The scale contains three dimensions, including Critical, Extraction/Communicative and Application/Communicative. The CoHL scale could be adopted in the contexts of other pandemics or public health crisis in the future, when the health topic meets the following criteria: (i) being a widespread worldwide pandemic, (ii) affecting the health outcomes of all types of populations, especially for the populations who developed severe symptoms and comorbidities resulting in increased mortality and (iii) containing ubiquitous government communications over various forms of media channels.
Our second aim has confirmed the hypothesis that people with higher CoHL would be more likely to adopt PBs (e.g. social distancing, mask-wearing). This result was consistent with previous literature showing that more adequate HL is associated with better compliance with medical treatments (such as medication adherence) or/and the adoption of health prevention behavior [13, 40, 41].
Another important finding was that the LoC also plays a critical role to moderate the relationship between HL and the adoption of PBs. While the LoC did not influence the adoption of PBs for people with higher CoHL, it matters for people with lower CoHL. People with lower CoHL were more likely to adopt the PBs if they believe that they may get COVID-19 infection due to others. This result has implications on framing the importance of ‘others’ in the control of the COVID-19 pandemic, for individuals with low CoHL. This could be a recommended public health strategy to stress the risk of COVID-19 infection by others as well as the risk of infecting others with COVID-19 to promote the adoption of PBs for people with inadequate levels of HL. During the public health campaign at the beginning of the pandemic, the French authorities mainly framed the importance of wearing a mask as the means to prevent oneself from spreading the virus rather than protecting oneself from getting infected by others. This communication strategy might not be effective for citizens with low COVID-19 literacy leading to unsatisfied rates of mask-wearing during the onset of the pandemic in France.
High CoHL scores were positively associated with the frequency to search for health information (news). Similar to the findings in Chung [42], the study suggested that patients with low HL or who had trouble evaluating online health information were less likely to ask questions or seek guidance during consultations with physicians. In contrast, patients with higher HL were more likely to critically assess online health information and discuss more online information with doctors [43]. This result underlines the importance of empowering the people with low CoHL, by providing access to the easy-to-understand health information, such as the online public health information with high readability, emphasizing the possibility to get infections by others, for them to adopt appropriate PB during the pandemic. Further, to support patient-centered communication, CoHL could be an important measure for physicians or other health care providers to determine the levels of HL of their patients and adopt the appropriate communication strategies. The CoHL measure can also be used in assisting the evaluation of the potential efficacy of public health campaigns in promoting the adoption of health behavior. Szmuda et al. [44] suggested that the readability of articles regarding COVID-19 and other diseases should be improved so that the individuals could understand health information in a better way and respond appropriately to adopt recommended PB and limit the spread of the pandemic.
The other implication is to design interventions to improve CoHL through training programs. Hsu [45] showed that 85% undergraduate students who participated in their study did not take into account the author’s professionalism of Covid-related health information found on the Internet. Therefore, developing training programs at universities and even before to help people to find, evaluate the reliability of the sources and process information on the Internet seems crucial to increase HL in general.
Conclusion and limitations
The present study has substantial implications for promoting public health during the ongoing COVID-19 pandemic. First, the CoHL scale is the first-ever validated instrument available to identify people who may experience difficulties in obtaining, processing and understanding COVID-19-related health information. Other language versions of the scale could be evaluated in other populations and will allow exploring how culture might impact differently on the forming of literacy in this specific health topic. Secondly, the CoHL scale provides a framework that can be used to develop HL measures for other health topics. Given that CoHL is developed based on the French version of the Functional, Communicative and Critical (FCCHL) validated by Ousseine [25], FCCHL is a generic HL scale initially developed in English by Ishikawa et al. [46], validated by various populations and languages (e.g. van der Vaart et al. [47] in German; [48] for young adults and teenagers with cancers), CoHL can also be adapted for other specific health topics following the original constructs (Cholera, Ebola, Yellow fever, Meningitis, Influenza, etc.). Items’ wording can be easily adapted to fit another specific pandemic disease. The interest is that the role of this literacy factor as for other psychosocial and cognitive factors can be described more precisely when it is measured at the same level of specificity as that of a targeted health factor. The present study further suggested one effective strategy to promote the adoption of PBs for people with inadequate CoHL. Communication emphasizing on others’ responsibility to be oneself infected by COVID-19 could help people become more active and willing to adopt social distancing or mask-wearing behaviors. This is the first study demonstrating that external LoC can be associated with adopting preventive behaviors for a specific population. However, two recent studies conducted during the COVID-19 pandemic suggest such an external LoC framing would induce more psychological distress or depression [49, 21]. Taken together, these results call for further research to inform the short- and long-term costs and benefits of such a public communication framework.
This study also had two potential limitations, which reflect the inevitable constraints of conducting research during the lockdown of the pandemic. First, given the restrictions on in-person contact, the study was conducted using an online [54]questionnaire, in which the online participant sample is relatively more educated. Future investigation on a more diverse sample will be conducted. The other potential limitation is the use of online questionnaires via snowball sampling. The choice of sampling and study method is due to the availability of conducting research during the lockdown. There is also established evidence showing that the data collected using online method has no significant difference from those collected by paper and pencil [50,51,52,53,54,55,56,57]. Some studies even suggested more advantages of using an online survey than a paper-and-pen survey in terms of the reduced social desirability of the participants [50], and the increasing willingness of disclosure [58, 59]. Despite the abovementioned limitations, the current study has original contributions to validate the CoHL scale and advance our understanding of its connections with the adoption of PB among individuals with different LoC.
Contributor Information
Carole Rodon, Département Transport Santé Sécurité (TS2), Campus Méditerranée, Laboratoire Mécanismes d’Accidents (LMA), Université Gustave Eiffel (ex-IFSTTAR), 304, Chemin de la croix blanche, Salon-de-Provence 13300, France.
Jessie Chin, School of Information Sciences (MC 387), University of Illinois at Urbana-Champaign, 614 E Daniel St (#5139), Champaign, IL 61820, USA.
Aline Chevalier, UFR de Psychologie, Département de Psychologie Cognitive et Ergonomie, Laboratoire Cognition, Langues, Langage, Ergonomie (CLLE, UT2J & CNRS), Université Toulouse Jean Jaurés (UT2J), Maison de la recherche, 5 allées Antonio Machado, Toulouse, F-31058 Cedex 9, France.
Funding
No funding received.
Conflict of interest statement
None declared.
References
- 1. World Health Organization. An ad hoc WHO technical consultation managing the COVID-19 infodemic: call for action , 7–8 April 2020. Geneva: World Health Organization, 2020. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 2. Bora K, Pagdhune A, Patgiri SJ et al. Does social media provide adequate health education for prevention of COVID-19? A case study of YouTube videos on social distancing and hand-washing. Health Educ Res 2021; 36: 398–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thacker J, Sturman D, Auton J. Predictors of social distancing compliance in an Australian sample. Health Educ Res 2021; 36: 601–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bekalu MA, Dhawan D, McCloud R et al. Adherence to COVID-19 mitigation measures among American adults: the need for consistent and unified messaging. Health Educ Res 2021; 36: 178–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. U.S. Department of Health and Human services . Healthy People 2010: Understanding and Improving Health. 2nd edn. U.S. Government Printing Office, 2000. Available at: http://www.health.gov/healthypeople/. Accessed: 13 September 2020. [Google Scholar]
- 6. Kickbusch I, Jürgen MP, Franklin A et al. Health Literacy: The Solid Facts. 2013. The World Health Organization, the Regional Office for Europe. Available at: http://www.euro.who.int/_data/assets/pdf_file/0008/190655/e96854.pdf. Accessed: January 2022.
- 7. Sørensen K, Van den Broucke S, Fullam J et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012; 12: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nutbeam D. Health literacy as a public goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int 2000; 15: 259–67. [Google Scholar]
- 9. Nutbeam D. The evolving concept of health literacy. Soc Sci Med 2008; 67: 2072–8. [DOI] [PubMed] [Google Scholar]
- 10. Azevedo RFL, Morrow DG. Improving older adults’ comprehension and use of patient portal-based health information. In: Pak R, Collins Mclaughlin A (eds). Aging, Technology and Health. London: Elsevier, 2018, 49–80. [Google Scholar]
- 11. Chin J, Madison A, Gao X et al. Cognition and health literacy in older adults’ recall of self-care information. Gerontologist 2017; 57: 261–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Raine R, Wallace I, Nic A’ Bhaird C et al. Improving the effectiveness of multidisciplinary team meetings for patients with chronic diseases: a prospective observational study. Health Serv Delivery Res 2014; 2.doi: 10.3310/hsdr02370. [DOI] [PubMed] [Google Scholar]
- 13. Chin J, Wang H, Awwad AW et al. Health literacy, processing capacity, illness knowledge, and actionable memory for medication taking in type 2 diabetes: cross-sectional analysis. J Gen Intern Med 2021; 36: 1921–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chin J, Morrow DG, Stine-Morrow EAL et al. The process-knowledge model of health literacy: evidence from a componential analysis of two commonly used measures. J Health Commun 2011; 16: 222–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Heijmans M, Waverijn G, Rademakers J et al. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ Couns 2015; 98: 41–8. [DOI] [PubMed] [Google Scholar]
- 16. Keinwong T, Pathike W, Hunter S et al. An integrative literature review: health literacy and learning ability among older adults with chronic illness. Int J Gerontol 2019; 562–7.doi: 10.6890/IJGE.201910/SP.0010. [DOI] [Google Scholar]
- 17. Sørensen K, Pelikan JM, Röthlin F et al. , HLS-EU Consortium . Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health 2015; 25: 1053–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr 1966; 80: 1–28. [PubMed] [Google Scholar]
- 19. Paquet Y, Lavigne GL, Vallerand RJ. Validation d’une échelle courte et multidimensionnelle de locus de contrôle spécifique au travail (MLCST) [Validation of a short multi-factor locus of control scale specific to work]. Can J Behav Sci 2014; 46: 60–5. [Google Scholar]
- 20. Baron-Epe O, Levin-Zamir D, Cohen V et al. Internal locus of control, health literacy and health, an Israeli cultural perspective. Health Promot Int 2019; 34: 248–57. [DOI] [PubMed] [Google Scholar]
- 21. Sigurvinsdottir R, Thorisdottir IE, Gylfason HF. The impact of COVID-19 on mental health: the role of locus on control and internet use. Int J Environ Res Public Health 2020; 17: 6985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Roncancion AM, Berencon AB, Rahman M. Health locus of control, acculturation, and health-related internet use among latinas. J Health Commun 2012; 17: 631–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Baltar F, Brunet I. Social research 2.0: virtual snowball sampling method using Facebook. Internet Res 2012; 22: 57–74. [Google Scholar]
- 24. Dusek GA, Yurova YV, Ruppel CP. Using social media and targeted snowball sampling to survey a hard-to-reach population: a case study. Int J Dr Stud 2015; 10: 279–99. [Google Scholar]
- 25. Ousseine YM, Rouquette A, Bouhnik AD et al. Validation of the French version of the Functional, Communicative and Critical Health Literacy scale (FCCHL). J Patient-Rep Outcomes 2018; 2: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: a tutorial on parallel analysis. Organ Res Methods 2004; 7: 191–205. [Google Scholar]
- 27. Dwinger S, Kriston L, Härter M et al. Translation and alidation of a multidimensional instrument to assess health literacy. HealthExpect 2015; 18: 2776–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. O’Connor BP. SPSS, SAS, MATLAB, and R programs for determining the number of components and factors using parallel analysis and vehicle’s MAP Test, 2000a. Available at: https://people.ok.ubc.ca/brioconn/nfactors/nfactors.html. Accessed: April 2022. [DOI] [PubMed]
- 29. O’Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behav Res Meth Instrum Comput 2000b; 32: 396–402. [DOI] [PubMed] [Google Scholar]
- 30. Hair JF, Black WC, Babin BJ et al. Multivariate Data Analysis. Seventh New International Edition. Upper Saddle River, NJ: Prentice Hall, 2014. [Google Scholar]
- 31. Henson RK, Roberts JK. Use of exploratory factor analysis in published research: common errors and some comment on improved practice. Educ Psychol Meas 2006; 66: 393–416. [Google Scholar]
- 32. Howard MC. A review of exploratory factor analysis decisions and overview of current practices: what we are doing and how can we improve? Int J Hum Comput Interact 2016; 32: 51–62. [Google Scholar]
- 33. Tabachnick BG, Fidell LS. Using Multivariate Statistics. Boston: Pearson/Allyn & Bacon, 2007. [Google Scholar]
- 34. Mulaik SA, James LR, Van Alstine J et al. Evaluation of goodness-of-fit indices for structural equation models. Psychol Bull 1989; 105: 430–45. [Google Scholar]
- 35. Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods 2008; 6: 53–60. [Google Scholar]
- 36. Heeren A, Douilliez C, Peschard V et al. Cross-cultural validity of the five facets mindfulness questionnaire: adaptation and validation in a French-speaking sample. Rev Eur Psychol Appl 2011; 61: 147–51. [Google Scholar]
- 37. Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 2003; 8: 31–51. [Google Scholar]
- 38. Cronbach LJ. Coefficient alpha and the internal structure of tests. psychometrika 1951; 16: 297–334. [Google Scholar]
- 39. Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat 2006; 31: 437–48. [Google Scholar]
- 40. Heuser C, Diekmann A, Kowalski C et al. Health literacy and patient participation in multidisciplinary tumor conferences in breast cancer care: a multilevel modeling approach. BMC Cancer 2019; 19: 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. von Wagner C, Steptoe A, Wolf MS et al. Health literacy and health actions: a review and a framework from health psychology. Health Educ Behav 2009; 36: 860–77. [DOI] [PubMed] [Google Scholar]
- 42. Chung JE. Patient–provider discussion of online health information: results from the 2007 Health Information National Trends Survey (HINTS). J Health Commun 2013; 18: 627–48. [DOI] [PubMed] [Google Scholar]
- 43. Murray E, Lo B, Pollack L et al. The impact of health information on the internet on the physician-patient relationship: patient perceptions. Arch Intern Med 2003; 163: 1727–34. [DOI] [PubMed] [Google Scholar]
- 44. Szmuda T, Özdemir C, Ali S et al. Readability of online patient education material for the novel coronavirus disease (COVID-19): a cross-sectional health literacy study. Public Health 2020; 185: 21–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hsu WC. Undergraduate students’ online health information-seeking behavior during the COVID-19 Pandemic. Int J Environ Res Public Health 2021; 18: 13250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care 2008; 31: 874–9. [DOI] [PubMed] [Google Scholar]
- 47. van der Vaart R, Drossaert CHC, Taal E et al. Validation of the Dutch functional, communicative and critical health literacy scales. Patient Educ Couns 2012; 89: 82–8. [DOI] [PubMed] [Google Scholar]
- 48. McDonald FE, Patterson P, Costa DS, Shepherd HL. Validation of a Health Literacy measure for adolescents and young adults diagnosed with cancer. J Adolesc Young Adult Oncol 2016; 5: 69–75. [DOI] [PubMed] [Google Scholar]
- 49. Krampe H, Danbolt LJ, Haver A et al. Locus of control moderates the association of COVID-19 stress and general mental distress: results of a Norwegian and a German-speaking cross-sectional survey. BMC Psychiatry 2021; 21: 437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Birnbaum MH. Psychological Experiments on the Internet. New York: Academic Press, 1999. [Google Scholar]
- 51. Buchanan T, Smith JL. Using the internet for psychological research: Personality testing on the world wide web. Br J Psychol 1999; 90: 125–44. [DOI] [PubMed] [Google Scholar]
- 52. Carlbring P, Brunt S, Bohman S et al. Internet vs. paper and pencil administration of questionnaires commonly used in panic/agoraphobia research. Comput Human Behav 2006; 23: 1421–34. [Google Scholar]
- 53. Chuah SC, Drasgow F, Roberts BW. Personality assessment: does the medium matter? No. J Res Pers 2006; 40: 359–76. [Google Scholar]
- 53. Herrero J, Meneses J. Short web-based versions of the perceived stress (PSS) and Center for Epidemiological Studies-Depression (CESD) Scales: a comparison to pencil and paper responses among Internet users. Comput Human Behav 2006; 22: 830–46. [Google Scholar]
- 54. Huang HM. Do print and web surveys provide the same results? Comput Human Behav 2006; 22: 334–50. [Google Scholar]
- 55. Nosek BA, Banaji M, Greenwald AG. Harvesting implicit group attitude and beliefs from a demonstration web site. Group Dyn 2002; 6: 101–15. [Google Scholar]
- 57. Vosylis R, Žukauskienė R, Malinauskienė O. Comparison of Internet based versus paper-and-pencil administered assessment of positive development indicators in adolescent’s sample. Psichologija 2012; 45: 7–21. [Google Scholar]
- 57. Couper MP. Web-based surveys: a review of issues and approaches. Public Opin Q 2000; 64: 464–94. [PubMed] [Google Scholar]
- 59. Witmer DF, Colman RW, Katzman SL. From Paper-and-pencil to Screen-and-keyboard. Thousand Oaks, CA: Sage, 1999. [Google Scholar]


