Abstract
Introduction
This study assessed changes in e-cigarette use since the COVID-19 pandemic began and reasons for these changes among US youth and young adults.
Aims and Methods
We combined data from two cross-sectional samples of youth and young adult (15–24 years) participants of a monthly surveillance study (data collected in April and June 2021). Analyses were restricted to past-year e-cigarette users who reported using e-cigarettes before the pandemic (n = 1762). Participants reported changes in e-cigarette use since the pandemic began, reasons for changing their behavior, and their perceptions around COVID-19 risk related to e-cigarette use. Multinomial logistic regression models assessed associations between demographics and COVID vaping risk perceptions and changes in e-cigarette use.
Results
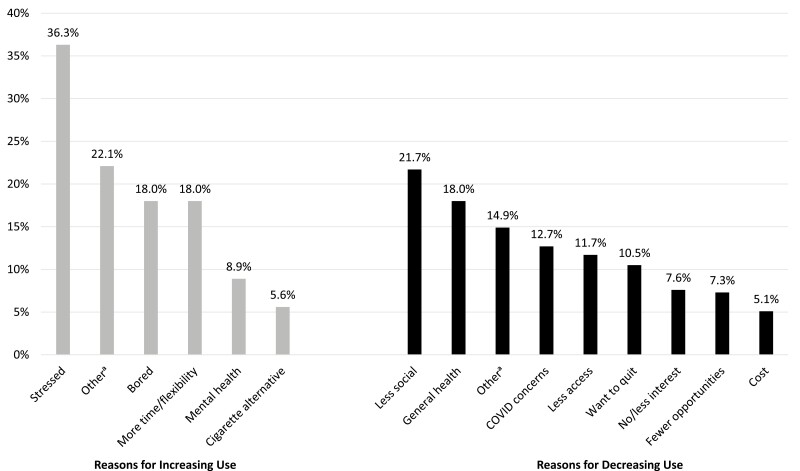
Over a third of the sample (37.9%) reported increasing e-cigarette use, while 28.9% reported decreasing use, and 33.1% reported no change. Analyses revealed associations between change in e-cigarette use and age, race and ethnicity, e-cigarette use status, and COVID vaping risk perceptions. The most common reason for increasing use was managing stress (36%); the most common reasons for decreasing use included fewer social interactions (22%) and concerns over general health (18%). Results also indicated differences in reasons for decreasing use by race and ethnicity, and differences in reasons for both increasing and decreasing use by age.
Conclusions
This study provides recent data on how the ongoing and evolving COVID-19 pandemic has impacted youth and young adults’ e-cigarette use. Findings identify subpopulations that may benefit from e-cigarette prevention interventions, as well as insights that may inform the content and delivery of such interventions.
Implications
This study provides recent insights into if and why the ongoing COVID-19 pandemic has impacted e-cigarette use behavior among youth and young adults. Findings contribute to the understanding of the role e-cigarettes play in young people’s lives—insights that can inform youth and young adult prevention efforts.
Introduction
E-cigarette use among young people continues to be a public health concern. In 2021, approximately 11% of US high school students reported current e-cigarette use,1 and 9% of young adults (18–24 years) were current users in 2019.2 Extant research has identified reasons that these products appeal to youth and young adults, including use by friends, beliefs that e-cigarettes are less harmful than cigarettes, reduce stress, and use where cigarettes are prohibited.3–5 Because the legal age of sale of tobacco in the United States is 21 years, underage youth commonly report acquiring e-cigarettes from friends, with multiple studies reporting over half of the youth acquired the device from a social source.6–8 Despite being under the minimum age for sale of tobacco, a notable proportion of youth also report buying e-cigarettes from retailers, with an estimated 22% buying a device at a gas station and convenience store and 18% at a vape shop in 2020.9
There is limited evidence of how the current coronavirus disease 2019 (COVID-19) pandemic has impacted youth and young adults’ e-cigarette use. In response to the pandemic, many US states implemented stay-at-home orders and closed non-essential businesses beginning in March 2020.10 Federal, state, and local leaders promoted social distancing and many schools migrated from in-person to online learning to control the spread of the virus.11 These responses may impact youth and young adults’ e-cigarette use by reducing access to devices and opportunities for use.
Researchers have begun to examine the impact of the COVID-19 pandemic on e-cigarette use. Among a sample of US youth and young adults, Gaiha et al.12 found over half (56%) changed their use behavior since the beginning of the pandemic, with the majority reporting quitting or reducing use. Concerns over the impact of e-cigarettes on the lungs were the primary reason participants decreased use, and managing boredom and stress were the most common reasons for increasing use.12 Kreslake et al.13 assessed changes in e-cigarette use since the start of the pandemic among a national sample of youth and young adults, finding the largest proportion decreased use. Results revealed that limited access to retailers was associated with decreased use.13 These data were collected at the start of the pandemic, and little is known about how the pandemic continues to impact e-cigarette use. As the pandemic continues to evolve with the availability of vaccines for adults and youth as young as 12 years as of May 2021,14 the actions of both state and local leaders, as well as individuals, in response to the pandemic have likely shifted, resulting in a context that differs from the early days of the pandemic, during which data were collected for previously reported studies.
This report shares results from a cross-sectional, convenience sample of US youth and young adult e-cigarette users, collected in the spring and summer of 2021. Analyses assess changes in participants’ e-cigarette use since the COVID-19 pandemic, reasons why participants changed their behavior, and their perceptions around the risk of COVID-19 related to e-cigarette use.
Methods
Sample
Two cross-sectional samples of youth and young adults were recruited as part of a monthly surveillance study. Data were collected from these two samples in April (wave 1) and June (wave 2) 2021. Participants from these two cross-sectional samples were combined into a single sample for the purposes of the current study. Recruitment advertisements on Facebook and Instagram directed participants to an eligibility screener. Participants were eligible if they lived in the United States, were aged 15–24 years, and reported ever use or susceptibility to use e-cigarettes (among never users; based on the four-item Pierce Susceptibility Scale15,16). Sampling quotas were used to recruit approximately equal numbers of males and females and equal numbers of those aged 15–20 years and 21–24 years. Eligible participants provided consent or assent, completed the survey on Qualtrics, and received a $5 gift card upon completion. To ensure data quality, age, and date of birth were asked separately and required to match for a respondent to qualify for the survey, and email addresses were used to prevent respondents from completing the survey multiple times. Once data were collected, they were checked for duplicate completes, and quality checks were conducted throughout data collection to ensure the survey was performing as programmed. At wave 1, 1825 individuals were determined to be eligible and started the survey; at wave 2, 1747 were eligible and started the survey. After limiting to completed surveys, the sample sizes at waves 1 and 2 were 1502 and 1500, respectively. This study was approved by the Office of Research Protection at RTI International (study number: STUDY00021435).
Measures
E-cigarette Use
Participants reported the last time they used an e-cigarette. Response options included earlier today, not today but sometime during the past 7 days, not during the past 7 days but sometime during the past 30 days, not during the past 30 days but sometime during the past 6 months, not during the past 6 months but sometime in the past-year, 1–4 years ago, 5 or more years ago and I have never vaped. Participants who responded with anything besides I have never vaped were classified as “ever users”. Participants who reported use in the past 30 days (earlier today, not today but sometime in the past 7 days, or not during the past 7 days but sometime during the past 30 days) were classified as “current users”.
Change in E-cigarette Use
E-cigarette users were asked: Are you vaping more, less, or about the same as you did before the COVID-19 pandemic, with response options: more, less, about the same, and I was not vaping before the pandemic. Those reporting more or less were asked why they changed their behavior and responses were open-ended and coded by two analysts: the first 25 responses were coded together, then the next 25 responses separately and tested for inter-rater reliability using Cohen’s kappa coefficient. Inter-rater reliability was high (k > 0.80). The remaining qualitative responses were coded separately. Reasons for using e-cigarettes more were coded into the categories: more time and flexibility (eg, having more free time, being home more often), boredom, stress, mental health (eg, using e-cigarettes to reduce anxiety), and cigarette alternatives. Reasons for using e-cigarettes less were coded into the categories: fewer opportunities (eg, less privacy at home to use e-cigarettes), less access (eg, e-cigarettes are harder to get), less social (eg, hanging out with friends less often), cost, COVID concerns, general health concerns, desire to quit, and no and less interest. As our goal was to identify the most salient reasons for changing use behavior,17 we only report categories with at least 20 responses; categories with fewer than 20 responses, or responses that lacked specificity, were coded into an “other” category. Responses were coded into as many categories as were applicable.
COVID Vaping Risk Perceptions
A risk perception scale related to COVID-19 and e-cigarette use included the mean of three items: (1) in my opinion, vaping may increase the risk for getting sick from COVID-19; (2) in my opinion, vaping may weaken the immune system, making people more at risk for getting sick from COVID-19; and (3) in my opinion, vaping may make COVID-19 symptoms worse. Response options ranged from 1 = strongly disagree to 4 = strongly agree. Internal consistency of the scale was high (α = .85 at each wave individually and combined) and factor analysis revealed all items loaded onto a single factor at both waves.
Demographics
Demographic variables included gender (male, female, genderqueer and non-conforming), race and ethnicity (non-Hispanic White, Black, Asian, and other, and Hispanic), and age (15–20 years, 21–24 years). Age category cutoffs were established based on US Tobacco 21 laws which prohibit the sale of tobacco products to anyone under the age of 21 years.
Analysis
Analyses were restricted to those who had ever used an e-cigarette, reported use within the past-year, and did not respond I was not vaping before the pandemic (n = 1762). Participants who indicated that they did not use e-cigarettes before the pandemic (n = 508) were not included in the analysis and are not reported in the results as e-cigarette initiation was outside the scope of the current study. Multinomial logistic regression was used to estimate the relative risk ratio (RRR) of reporting decreasing use (“less often”) relative to increasing use (“more often”) or no change in use since the pandemic among demographic subgroups, e-cigarette use subgroups, and as a function of COVID vaping risk perception. The reference categories are youth (ages 15–20 years), male, and non-Hispanic White for age, gender, and race and ethnicity, respectively. A wave indicator variable was included as a control in the model to account for unmeasured differences in the 2 months of data collection. Listwise deletion was used for missing data (5.6%, n = 99). Descriptive analysis of open-ended responses assessed differences in reasons for behavior change by age group (15–20 years vs. 21–24 years) and race and ethnicity, collapsed into the following groups due to limited sample sizes: non-Hispanic White, Hispanic, and non-Hispanic other (comprised of Black, Asian, and “other” participants). Analyses were conducted in Stata v16.
Results
After removing those with missing data, the analytic sample included n = 1663 past-year e-cigarette users. Demographic characteristics are presented in Table 1. Slightly more than half of the sample was aged 15–20 years (54.5%) and identified as female (56.7%). Approximately half the sample (50.6%) identified as non-Hispanic White. In terms of e-cigarette use, 88.6% of the sample were classified as current users, with the remainder (11.4%) classified as ever, noncurrent users.
Table 1.
Sample Description and Results of Multinomial Logistic Regression Predicting Change in E-cigarette Use Since the COVID-19 Pandemic
| Change in E-cigarette Use Since COVID-19 Pandemic | |||||
|---|---|---|---|---|---|
| Total sample (N = 1663) | Less often vs. no change | Less often vs. more often | |||
| n (%) | RRR | P-value | RRR | P-value | |
| COVID vaping risk perception scale (range = 1–4) | Mean score: 2.8 | 1.97 | .000 | 1.53 | .000 |
| E-cigarette usea | |||||
| Current | 1473 (88.6) | Ref. | Ref. | Ref. | Ref. |
| Ever, noncurrent | 190 (11.4) | 2.90 | .000 | 8.38 | .000 |
| Age | |||||
| 15–20 years | 907 (54.5) | Ref. | Ref. | Ref. | Ref. |
| 21–24 years | 756 (45.5) | 1.06 | .678 | 1.42 | .007 |
| Gender | |||||
| Male | 578 (34.8) | Ref. | Ref. | Ref. | Ref. |
| Female | 943 (56.) | 1.17 | .262 | 1.09 | .550 |
| Genderqueer and non-conforming | 142 (8.5) | 1.36 | .238 | 0.97 | .898 |
| Race and ethnicity | |||||
| NH, White | 842 (50.6) | Ref. | Ref. | Ref. | Ref. |
| NH, Black | 103 (6.2) | 1.87 | .030 | 1.18 | .526 |
| Hispanic | 370 (22.2) | 1.54 | .009 | 1.52 | .009 |
| NH, Asian | 212 (12.7) | 1.49 | .040 | 1.95 | .001 |
| NH, otherb | 136 (8.2) | 0.79 | .377 | 0.68 | .142 |
E-cigarette use was assessed with the item: The next questions are about vaping products or vapes. You may also know them as e-cigarettes. They can contain nicotine and/or flavors. Some common brands are JUUL, Suorin, and Puff Bar. Please do NOT include vaping marijuana, THC and CBD when answering these questions. When did you last vape, even one time?
Non-Hispanic other includes those who identified as Native Hawaiian or other Pacific Islander, those who identified as biracial and multiracial, and those who selected the “other” response option to the race survey question.
Bold indicates significant relative risk ratios (RRR) and p-values (α = .05). Model also controlled for wave of data collection.
NH = Non-Hispanic.
Change in E-cigarette Use
Among the analytic sample, 37.9% reported increasing use since the COVID-19 pandemic, while 28.9% reported decreasing use, and 33.1% reported no change.
Multinomial logistic regression indicated significant associations between change in e-cigarette use and COVID vaping risk perceptions, age, and race and ethnicity (Table 1). Participants with stronger agreement on the COVID vaping risk perception scale were more likely to report using e-cigarettes “less often” compared with “more often” (RRR = 1.53, p < .001) and “no change” (RRR = 1.97, p < .001). Compared with current e-cigarette users, ever non-current users were more likely to report using e-cigarettes “less often” relative to “more often” (RRR = 8.38, p < .001) or “no change” (RRR = 2.90, p < .001). Young adult participants (21–24 years) were more likely than youth participants (15–20 years) to report using e-cigarettes “less often” compared to “more often” (RRR = 1.42, p < .01). Compared with participants who identified as non-Hispanic White, those who identified as non-Hispanic Black, non-Hispanic Asian, and Hispanic were more likely to report using e-cigarettes “less often” compared to “no change” (RRR = 1.87, RRR = 1.49, RRR = 1.54, respectively; p < .05). Hispanic and non-Hispanic Asian participants were also more likely than non-Hispanic White participants to report using “less often” compared with “more often” (RRR = 1.52, RRR = 1.95; p < .01).
Reasons for Change in E-cigarette Use
Figure 1 shows the percent of total responses to open-ended reasons for changing e-cigarette use behavior that fit into each category. The most common reason for increasing e-cigarette use was stress management (36.3%). Managing boredom (18.0%) and having more time and flexibility (18.0%) were also common reasons for increasing use. The most common reason for decreasing use was having fewer social interactions (21.7%). General health concerns (18.0%) and concerns related to COVID-19 (12.7%) were also reasons for decreasing use.
Figure 1.
Reasons for change in e-cigarette use among those reporting increasing their use (n = 551, gray bars) or decreasing their use (n = 410, black bars) since the start of the COVID-19 pandemic. Percentages represent the percent of responses that fell into each category. a “Other” is comprised of additional open-ended responses that did not fit criteria for a defined category due to small sample size (<20) or lack of specificity. For increases in use, examples include fun and entertainment, convenience, and changes in environment where vaping is more common (new friends and coworkers). For decreases in use, examples include self-improvement and switching to other products.
Descriptive analysis of open-ended responses suggests that differences in reasons for changes in e-cigarette use by age group and race and ethnicity. The proportion of participants reporting less access to e-cigarettes as a reason for decreasing use was over 3.6× higher for youth (ages 15–20 years) compared with young adults (ages 21+ years; 18% vs. 5%). Conversely, the proportion who reported decreasing use due to general health concerns was 1.8× higher for young adults compared with youth (23% vs. 13%). Among participants who increased use, the proportion who reported using e-cigarettes as an alternative to cigarettes was 2× higher for young adults compared with youth (8% vs. 4%). In terms of racial and ethnic differences, the proportion of Hispanic respondents that reported decreasing their use due to fewer opportunities was 3× higher compared with non-Hispanic White participants (13% vs. 4%). Additionally, the proportion of non-Hispanic White participants that reported decreasing use due to fewer social interactions was 2.1× higher compared with Hispanic respondents (28% vs. 13%). We did not observe racial and ethnic differences in reasons for using e-cigarettes more.
Discussion
This report presents findings from a sample of youth and young adult e-cigarette users on changes in their use since the COVID-19 pandemic began and the reasons for this change. Similar to other recent research of youth and young adults, findings indicate that the majority of e-cigarette users changed their behavior, with approximately one-third reporting no change. However, while prior research found more participants decreased use,12,13 the current study found slightly more participants increased use. These divergent findings may be related to when the data were collected. While previous studies were conducted in the early months of the pandemic,12,13 the current study used data collected approximately a year into the pandemic. Limited social opportunities, lack of access to retailers, supply chain disruptions, increased parental monitoring due to at-home schooling, and fear over lung health were likely heightened during the early months of the pandemic. However, the reopening of schools and retailers, and the fatigue of the ongoing pandemic may explain why fewer participants in the current study reported decreasing their e-cigarette use. Differences across studies may also be the result of differing sampling strategies, given the purposeful sampling techniques used in the current study. Additional studies are needed to validate the findings.
Findings reveal differences in changes in e-cigarette behavior by age and race and ethnicity. Results indicate that youth and non-Hispanic Whites may be less likely to reduce their use in response to the COVID-19 pandemic, suggesting that these populations may benefit from targeted interventions. Given that stronger agreement with the COVID vaping risk perception scale was associated with decreasing use, interventions that highlight the risk of COVID-19 as related to e-cigarette use may be a promising strategy. Among a sample of US adults, Grummon et al.18 found evidence of the effectiveness of anti-smoking messages that linked smoking to increased COVID susceptibility and severity. However, messages linking e-cigarette use to COVID harm were found to be no more effective than messages of traditional, non-COVID health consequences.18 While early evidence suggests that possible associations between e-cigarette use and COVID-19 susceptibility and severity,19–21 available evidence is mixed and more research on this topic is needed.22–24
This study also provides insights into the reasons youth and young adult e-cigarette users changed their behavior during the pandemic. Managing stress was the most common reason for increasing use. This finding was unsurprising given prior research identifying stress as a reason for e-cigarette use among youth and young adults,4,5 and the increased stress young people likely feel due to the pandemic.25 Youth and young adults’ reduced ability to socialize as a reason for decreasing e-cigarette use reinforces the social nature of the behavior and the important role social networks have in influencing behavior, both in terms of setting norms and modeling behavior and with respect to access to the product. Approximately 12% of participants reported reduced access to e-cigarettes as a reason for decreasing use. This finding is consistent with findings from Kreslake et al.13 and may speak to not only reduced access to the product through social means but also the impact of closing non-essential businesses—which vape shops were considered to be in numerous states26—in response to the pandemic. This reason for decreasing e-cigarette use was reported more often by youth participants. While youth under the age of 21 years cannot legally be sold e-cigarettes, prior research has indicated that youth are able to purchase devices from retailers9 and the retail environment may present opportunities for interventions to reduce youth access and use.
Strengths of this study include the recency of the data being reported, collected over one year into the COVID-19 pandemic when shut-downs and social isolation mandates were being relaxed due to the availability of the vaccine to an increasing number of Americans. Additionally, our measure of changes in e-cigarette use behavior since the pandemic was cognitively tested with members of the target population and found to be easily understood. Furthermore, the use of an open-ended question to measure reasons for the change in e-cigarette use allowed the authors to explore a broader range of responses than would have been captured with fixed response options.
This study also has a few limitations to note. First, the sample was recruited based on e-cigarette use and through social media advertisements on a limited number of platforms. Therefore, findings should not be generalized to the broader youth and young adult population. Additionally, these data only capture a limited point in time within the context of an ongoing and evolving pandemic and additional research should continue to monitor how the pandemic impacts tobacco use behavior. We were also unable to assess differences by geographic location, which is an important area for future research given variations in responses to the COVID-19 pandemic by location. Furthermore, the two waves of cross-sectional data were collected approximately one month apart, and unmeasured external factors that may impact the relationship between the variables of interest and e-cigarette use behavior may differ between the 2 months of data collection. In addition, we were required to collapse some of the racial and ethnic groups when comparing reasons for changing e-cigarette use behavior due to limited sample sizes, so future research is needed with more robust sample sizes. Finally, ongoing regulatory changes and prioritizations around e-cigarettes from the US Food and Drug Administration may have also impacted youth and young adults’ e-cigarette use behavior, but were not captured in the present study.
The current COVID-19 pandemic has impacted many aspects of youth and young adults’ lives. This report provides insights into if and why e-cigarette use behavior may change in response to the pandemic. Findings identify subpopulations that may be particularly in need of e-cigarette prevention interventions, as well as insights that may inform the content and delivery of such interventions.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Acknowledgment
This publication represents the views of the author(s) and does not represent FDA and CTP position or policy.
Contributor Information
Morgane Bennett, Department of Research and Evaluation, Office of Health Communication and Education, Center for Tobacco Products, U.S. Food and Drug Administration, Silver Spring, MD, USA.
Jessica Speer, Center for Health Analytics, Media, and Policy, RTI International, Research Triangle Park, NC, USA.
Nathaniel Taylor, Center for Health Analytics, Media, and Policy, RTI International, Research Triangle Park, NC, USA.
Tesfa Alexander, Department of Research and Evaluation, Office of Health Communication and Education, Center for Tobacco Products, U.S. Food and Drug Administration, Silver Spring, MD, USA.
Funding
This study was funded by the US Food and Drug Administration.
Declaration of Interests
None declared.
Data Availability
Data sharing are not possible because it was not part of the study consent and assent process and we do not have a process for ensuring participants are not individually identifiable.
References
- 1. Park-Lee E, Ren C, Sawdey MD, et al. Notes from the field: e-Cigarette use among middle and high school students—National Youth Tobacco Survey, United States, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(39):1387–1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ.. Tobacco product use among adults—United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(46):1736–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tsai J, Walton K, Coleman BN, et al. Reasons for electronic cigarette use among middle and high school students—National Youth Tobacco Survey, United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(6):196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fadus MC, Smith TT, Squeglia LM.. The rise of e-cigarettes, pod mod devices, and JUUL among youth: factors influencing use, health implications, and downstream effects. Drug Alcohol Depend. 2019;201:85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pokhrel P, Herzog TA, Muranaka N, Fagan P.. Young adult e-cigarette users’ reasons for liking and not liking e-cigarettes: a qualitative study. Psychol Health. 2015;30(12):1450–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liu ST, Snyder K, Tynan MA, Wang TW.. Youth access to tobacco products in the United States, 2016-2018. Tob Regul Sci. 2019;5(6):491–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baker HM, Kowitt SD, Meernik C, et al. Youth source of acquisition for e-cigarettes. Prev Med Rep. 2019;16:101011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Truth Initiative. Where are kids getting JUUL? May 29, 2018; https://truthinitiative.org/research-resources/emerging-tobacco-products/where-are-kids-getting-juul. Accessed September 22, 2021.
- 9. Wang TW, Gentzke AS, Neff LJ, et al. Characteristics of e-cigarette use behaviors among US youth, 2020. JAMA Netw Open. 2021;4(6):e21113361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moreland A, Herlihy C, Tynan MA, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement — United States, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1198–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. EducationWeek. The Coronavirus Spring: The Historic Closing of U.S. Schools (A Timeline). July 1, 2020; https://www.edweek.org/leadership/the-coronavirus-spring-the-historic-closing-of-u-s-schools-a-timeline/2020/07. Accessed September 22, 2021.
- 12. Gaiha SM, Lempert LK, Halpern-Felsher B.. Underage youth and young adult e-cigarette use and access before and during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(12):e2027572–e2027572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kreslake JM, Simard BJ, O’Connor KM, et al. E-cigarette use among youths and young adults during the COVID-19 pandemic: United States, 2020. Am J Public Health. 2021;111(6):1132–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Coronavirus (COVID-19) Update. FDA Authorizes Pfizer-BioNTech COVID-19 Vaccine for Emergency Use in Adolescents in Another Important Action in Fight Against Pandemic [press release]. May 10, 2021.
- 15. Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK.. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15(5):355–361. 10.1037/0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- 16. Pierce JP, Distefan JM, Kaplan RM, Gilpin EA.. The role of curiosity in smoking initiation. Addict Behav. 2005;30(4):685–696. [DOI] [PubMed] [Google Scholar]
- 17. Weller SC, Vickers B, Bernard HR, et al. Open-ended interview questions and saturation. PLoS One. 2018;13(6):e0198606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grummon AH, Hall MG, Mitchell CG, et al. Reactions to messages about smoking, vaping and COVID-19: two national experiments. Tob Control. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Adams SH, Park MJ, Schaub JP, Brindis CD, IrwinCE, Jr. Medical vulnerability of young adults to severe COVID-19 illness—data from the national health interview survey. J Adolesc Health. 2020;67(3):362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gaiha SM, Cheng J, Halpern-Felsher B.. Association between youth smoking, electronic cigarette use, and COVID-19. J Adolesc Health. 2020;67(4):519–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McFadden DD, Bornstein SL, Vassallo R, et al. Symptoms COVID 19 positive vapers compared to COVID 19 positive non-vapers. J Prim Care Community Health. 2022;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Majmundar A, Allem J-P, Cruz TB, Unger JB. . Public health concerns and unsubstantiated claims at the intersection of vaping and COVID-19. Nicotine Tob Res. 2020;22(9):1667–1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kale D, Herbec A, Perski O, et al. Associations between vaping and COVID-19: cross-sectional findings from the HEBECO study. Drug Alcohol Depend. 2021;221:108590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jose T, Croghan IT, Hays JT, Schroeder DR, Warner DO.. Electronic cigarette use is not associated with COVID-19 diagnosis. J Prim Care Community Health. 2021;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Varma P, Junge M, Meaklim H, Jackson ML.. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Berg CJ, Callanan R, Johnson TO, et al. Vape shop and consumer activity during COVID-19 non-essential business closures in the USA. Tob Control. 2020;30(e1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing are not possible because it was not part of the study consent and assent process and we do not have a process for ensuring participants are not individually identifiable.