Abstract
Objective
We study the association between payment parity policies and telehealth utilization at community health centers (CHCs) before, during, and after the onset of the pandemic.
Materials and Methods
We use aggregated, de-identified data from FAIR Health for privately insured patients at CHC sites. Descriptive statistics and time trends are calculated. Logistic regression models were used to quantify the factors associated with telehealth utilization for each of our time periods: 1) pre-pandemic (March-June 2019), 2) immediate pandemic response (March-June 2020), and 3) sustained pandemic response (March-June 2021).
Results
Telehealth usage rates at CHC sites surged to approximately 61% in April 2020. By April 2021, only 29% of CHC sites in states without payment parity policies used telehealth versus 42% in states with payment parity policies. Controlling for other characteristics, we find that CHC sites in states with payment parity were more likely to utilize telehealth one year after the onset of the pandemic (OR:1.740, p<0.001) than states without, but did not find this association in 2019 or 2020.
Discussion
The public health emergency drove widespread use of telehealth, making the virtual care environment inherently different in 2021 than in 2019. Due to the unique fiscal constraints facing CHCs, the financial sustainability of telehealth may be highly relevant to the relationship between telehealth utilization and payment parity we find in this paper.
Conclusion
Supportive payment policy and continued investments in broadband availability in rural and undeserved communities should enable CHCs to offer telehealth services to populations in these areas.
Keywords: telehealth, payment parity, community health centers, COVID-19
INTRODUCTION
During the initial weeks of the pandemic, community health centers (CHCs) quickly pivoted to offer telehealth despite relatively low telehealth visit volume prior to March 2020.1 The federal government enacted new policies enabling CHCs to expand telehealth availability,2 and states quickly altered coverage and payment parity policies in response to the pandemic to encourage telehealth adoption and limit physical contact.3 CHCs are a major part of the safety net health care system providing primary care and behavioral health services to nearly 30 million patients in 2019. Payment parity, which requires insurers to reimburse providers at the same rate as in-person services, is viewed by many stakeholders, including small clinics and CHCs, as an incentive to telehealth utilization.4–6
However, critics of payment parity cite concerns about these policies. These concerns include impeding the development of innovative care delivery models based on new technologies, and limiting the ability of telehealth to address the high costs of care that is a hallmark of the US healthcare system.7
Prior to the pandemic, coverage for telehealth services was widespread, but only 15 states had requirements for parity in reimbursement.8 Analysis has shown that broad state-level telehealth coverage requirements had no significant association with telehealth adoption prior to the pandemic.9 Lack of payment parity, specifically among Medicaid, has been described as a barrier to utilization at CHCs.10,11 While implementing telehealth in response to COVID-19 was more seamless than many primary care providers anticipated, questions remain regarding utilizing telehealth services without payment parity.12
In 2020, 10 additional states moved to require payment parity for private insurers in response to the pandemic.8 Primary care providers became dependent on scaling up virtual visits to help with their financial bottom line as in-person visits plummeted due to the pandemic.13 This raised concern that safety net providers may be at a disadvantage in terms of standing up telehealth sites, particularly since many are located in rural communities or other areas with limited broadband.14 A survey of CHCs conducted by Health Resources & Services Administration (HRSA) during the pandemic found that several grantees were forced to scale back operations or close sites.1 One study of telehealth usage in CHCs in California found a modest decline in visit volume due to telehealth.15 CHCs are estimated to have lost $3 billion in revenue during the first 6 months of the pandemic due to reduced visits.16
Changes in telehealth policies and visit levels in response to the pandemic have been well documented,17 but the extent that state-level policies are associated with telehealth utilization is not well studied. Understanding these associations could help inform policy makers and CHC administrators in how to proceed in the future in utilizing telehealth services to serve their patients and communities. This study aims to contribute to that understanding by focusing on the association of state-level policy changes and internet infrastructure with telehealth utilization while controlling for other factors. These 2 areas of analysis can be greatly influenced by policy action.
DATA AND METHODS
We use aggregated and deidentified medical, mental health and dental care data from the FAIR Health National Private Insurance Claims (FH NPIC®) multi-payer dataset which includes claims data submitted by more than 70 national and regional payors and third-party administrators who insure or process claims for private insurance plans (both fully insured and self-insured plans) and is statistically significant in all 50 states and Washington, DC. Data on Medicare Advantage enrollees are included in this dataset.18 FAIR Health provided CHC site level monthly counts of in-person and telehealth visits for privately insured medical, mental health, and dental care for the period March 2019 through June 2021.
In aggregating our CHC sites to the grantee level using the Health Center Program Uniform Data System (UDS) data (explained further in the Supplementary Appendix), we find substantial variation in telehealth usage, particularly in 2019, within grantees. We interpret this as further evidence to support site-level analysis. Among CHC grantees that report any telehealth usage in 2019, we find on average only 2.35% of the individual sites within those CHC grantees report any telehealth usage in the FAIR Health data, meaning telehealth usage at the grantee level in 2019 appears to be driven by an extremely small number of associated sites.
We start by understanding the trends in telehealth utilization from a descriptive standpoint. We aggregate the volume of monthly visits over time for the CHC sites in our sample, as well as calculate the percent of CHC sites that utilized telehealth by month and stratified by whether they were located in a state with payment parity or not. This allows us to understand the time trends across the period we study. Further descriptive statistics were computed for key variables in our analysis.
Logistic regression models were used to quantify and statistically test the factors associated with telehealth utilization for each of our time periods. To account for seasonal variation, we examine visit rates during the same 4-month window of March–June of the years 2019, 2020, and 2021 which we categorize as: (1) pre-pandemic (March–June 2019), (2) immediate pandemic response (March–June 2020), and (3) sustained pandemic response (March–June 2021). Across these time periods, we have 6,637 total CHC practice sites distributed across all 50 states and the District of Columbia that serve as the unit of analysis. A binary telehealth utilization variable for each time period is used as the dependent variable and the independent variables include an indicator for if the CHC site was located in a state with payment parity requirements, visit volume size categories, percent of mental health visits, percent of dental visits, percent of households with a broadband connection, and rural categorization.
The remaining portion of this section describes additional data sources, we use in our analysis.
State policies
To incorporate state-level telehealth policies, we use data compiled by Volk et al8 that documented state-level changes for telehealth in private insurance requirements in response to the pandemic.
For the purpose of our analysis, states that were reported in Volk et al that enacted payment parity laws in response to the pandemic were assumed to have this law starting in March 2020 (when state legislatures quickly adopted emergency legislation to combat the pandemic). With the exception of Texas, we retain the payment parity classification in 2020 per Volk et al for our 2021 period. Emergency payment parity policies expired in Texas at the end of 2020, and to our knowledge, the state legislature did not take any action in legislating payment parity in any permanent regulations. Supplementary Appendix Table A4 shows which states are included in each time period as having payment parity.
Site characteristics
To control for characteristics of the CHC sites, we group the CHC sites into 2 categories (low-medium or high) based on total visit volume for each site and visit type during a time period. The distributions were split into 3 equal parts with the lowest tercile representing low visit volume CHC sites, the second tercile representing medium visit volume CHC sites, and the last tercile representing high visit volume CHC sites.
The percentage of visits that were mental health and dental care were calculated to control for variation in telehealth utilization that is due to visit types.
Demographic characteristics
We use CHC site level zip codes to match demographic data to each site to control for potential correlations with telehealth utilization specific to the area. The zip codes were assigned to a zip code tabulation area (ZCTA) using the zip code to ZCTA crosswalk from the Census Bureau. From the American Community Survey (ACS) 2019 5-year estimates, we use the percent of households with a broadband connection within each ZCTA to control for the connectivity capabilities of households. Because telehealth utilization is dependent on utilizing internet connections for virtual visits for both the provider and the patient, this is an important capability variable to study.
We controlled for rurality of the zip code using the Rural-Urban Commuting Area (RUCA) Codes from the US Department of Agriculture. Zip codes of the CHC sites were assigned RUCA codes and classified as rural if the zip code is in a rural or small-town area. While correlation exists between broadband connectivity and rurality, using these 2 variables allows us to separately identify the correlations due only to connectivity.
RESULTS
Visits over time
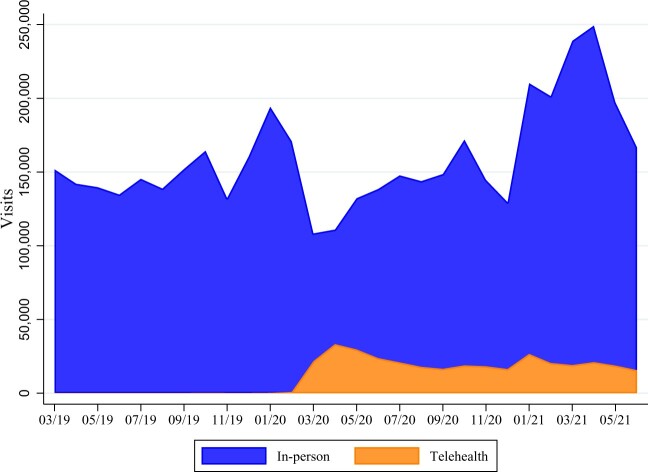
Figure 1 shows the total monthly visits across our CHC sites segmented by in-person or telehealth visits. Between January 2019 and February 2020, we find telehealth usage represented an extremely small portion of all visits at CHC sites. The graph of these visit volumes depicts how total visit volume sharply declined at the onset of the pandemic, but telehealth played a newly important role in supplementing visit levels.
Figure 1.
CHC site visit volume for privately insured patients. Notes: Total number of visits across all CHC sites in our sample are aggregated at each month and segmented by modality (in-person or telehealth).
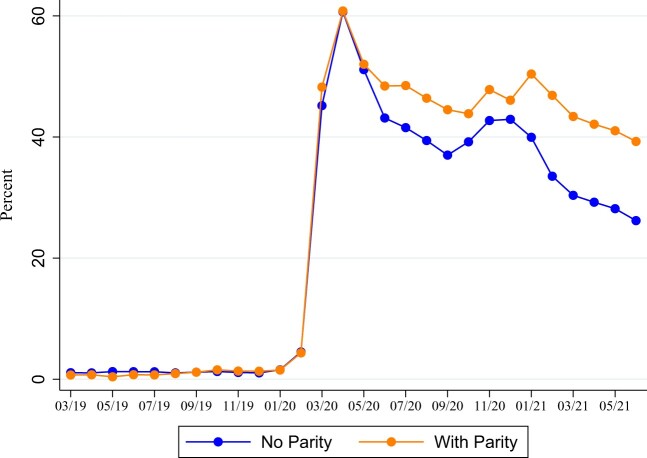
Figure 2 shows the percentage of CHC sites that used telehealth by month and state payment parity status. Prior to the pandemic, we see very low rates of telehealth utilization and insignificant differences in utilization by payment parity status. During the initial pandemic response, telehealth usage reached a high of 61% in April 2020. The differences between CHC sites in states that had payment parity versus without were minimal. Telehealth usage began to taper off after the onset of the pandemic; however, it is apparent there are stark differences in these trajectories by payment parity status. Telehealth usage rates in states without payment parity laws declined at a faster rate than sites in states with payment parity laws. By April 2021, only 29% of CHC sites in states without payment parity used telehealth versus 42% in states with payment parity requirements.
Figure 2.
Percent of CHC sites that used telehealth for privately insured visits by state reimbursement parity requirement. Notes: CHC sites that utilized telehealth at each month are identified, as well as CHC sites in states with or without payment parity requirements in the corresponding month. The percent of CHC sites within each month that utilized telehealth is calculated and plotted by state payment parity status for private insurance.
Descriptive statistics
Table 1 reports descriptive statistics for all our CHC sites (N = 6,598), those that never used telehealth during our analysis period (N = 938), those that used telehealth in 2019 (N = 89), 2020 (N = 2,819), and/or 2021 (N = 2,477).
Table 1.
Descriptive statistics
| Overall sample | Never used telehealth, 2019–2021 | Used telehealth in 2019 | Used telehealth in 2020 | Used telehealth in 2021 | |
|---|---|---|---|---|---|
| Number of CHC sites | 6,598 | 938 | 89 | 2,819 | 2,477 |
| Percent of sites that are rural | 18.14 | 25.37 | 25.84 | 17.91 | 14.21 |
| Mean percent mental health visits | 12.03 | 8.78 | 18.33 | 14.67 | 15.33 |
| Mean percent medical visits | 79.79 | 77.23 | 75.72 | 80.20 | 80.28 |
| Mean percent dental visits | 8.18 | 13.99 | 5.96 | 5.13 | 4.39 |
| Percent of sites in states with payment parity | 55.93 | 54.05 | 49.44 | 56.33 | 62.77 |
| Total number of states represented | 51 | 49 | 35 | 51 | 51 |
Notes: Descriptive statistics for overall sample and by telehealth usage status by year. CHC sites and site characteristics are based on an aggregated, de-identified sample of commercial insurance claims from FAIR Health. Rurality is based on Rural-Urban Commuting Area (RUCA) Codes from the U.S. Department of Agriculture. State payment parity status is based on classification by Volk et al and the authors’ further investigation.
Overall, 18.14% of our CHC sites are located in rural areas, with a much higher share (25.37%) of rural sites in the group that never used telehealth than those that used telehealth in 2020 and 2021.
The mean mental health visit share at the CHC site level is 12.03% for the overall sample and is much lower at 8.78% for those that never used telehealth compared to the groups of sites that used telehealth in 2020 and 2021. Dental visits make up a lesser share, with a mean of 8.18% of all visits for the overall sample. Medical visits compromise the largest share of visits at 79.79% of overall visits.
For the overall sample, 55.93% of CHC sites are located in states with payment parity at some point in time during our analysis. This percentage increases for those that use telehealth from 49.44% in 2019 to 62.77% in 2021.
State reimbursement parity
Table 2 reports the odds ratios (ORs) with standard errors from the logistic regression results. We find that the difference in telehealth utilization rates by payment parity status is statistically significant and higher for CHCs in states with payment parity than states without in 2021, even while controlling for other factors. CHC sites in states with payment parity in 2021 were 1.740 (P < .001) times more likely to utilize telehealth than CHC sites in states without payment parity.
Table 2.
Probability that a CHC site used telehealth for privately insured visits during March–June of each year
| (1) | (2) | (3) | |
|---|---|---|---|
| 2019 | 2020 | 2021 | |
| State has reimbursement parity | 0.745 | 1.026 | 1.740*** |
| (ref: no reimbursement parity) | (0.184) | (0.0702) | (0.109) |
| % of households with | 0.985 | 1.008* | 1.019*** |
| Broadband | (0.0105) | (0.00342) | (0.00331) |
| Rural area | 1.428 | 0.828* | 0.608*** |
| (0.369) | (0.0726) | (0.0516) | |
| Mental health visit share (%) | 1.033*** | 1.028*** | 1.033*** |
| (0.00703) | (0.00226) | (0.00215) | |
| Dental visit share (%) | 0.994 | 0.987*** | 0.987*** |
| (0.00636) | (0.00164) | (0.00155) | |
| High visit volume | 4.786*** | 6.580*** | 6.492*** |
| (ref: low-medium visit volume) | (1.121) | (0.554) | (0.435) |
| Number of CHC sites | 4,941 | 4,657 | 5,603 |
| Pseudo-R2 | 0.089 | 0.161 | 0.191 |
| Fraction with telehealth | 0.018 | 0.605 | 0.442 |
Notes: Linear probability regression results for CHC site level telehealth utilization. Exponentiated coefficients (odds ratios); standard errors in parentheses.
P < .05, **P < .01, ***P < .001.
We find no statistically significant relationship between payment parity requirements and telehealth utilization during 2019 or 2020.
Site characteristics
Among our controls, the visit volume level of the CHC sites had the largest magnitude of correlation with telehealth. These differences are statistically significant across all time periods. In 2019, high volume sites were more likely to utilize telehealth than low-medium volume sites (OR: 4.786, P < .001). These estimations increased in magnitude for 2020 (OR: 6.580, P < .001) and 2021 (OR: 6.492, P < .001).
Mental health visit share was associated with higher telehealth utilization across all years (2019 OR: 1.033, P < .001; 2020 OR: 1.028, P < .001; 2021 OR: 1.033, P < .001). Dental care visit share was associated with a lower likelihood of telehealth utilization in 2020 (OR: 0.987, P < .001) and in 2021 (OR: 0.987, P < .001).
Demographic characteristics
CHC sites in rural areas were significantly less likely to use telehealth in 2020 (OR: 0.828, P < .001) and 2021 (OR: 0.608, P < .001). The association between rurality and telehealth utilization for 2019 is not statistically significant in our regressions.
Household connectivity in the CHC site area was also associated with telehealth utilization. The percent of households with a broadband connection is positively associated with higher telehealth utilization in both 2020 (OR: 1.008, P < .001) and 2021 (OR: 1.019, P < .001).
DISCUSSION
We find state payment parity policies were associated with telehealth utilization by CHC sites 1 year after the onset of the COVID-19 pandemic. These findings hold even when controlling for CHC site-level factors such as rurality, access to broadband, visit composition, and visit volume. However, payment parity was not associated with telehealth utilization before the pandemic or during the immediate response.
The lack of a substantial difference in telehealth utilization between states with or without payment parity in 2020, during the immediate pandemic response, is intuitive to us. During this time, states quickly altered policies for reimbursement and public health directives strongly encouraged the use of telehealth to minimize or eliminate in-person contact to control the spread of COVID-19. There was a rapid rise in telehealth visits in response, and when social distancing requirements were later relaxed, in-person interactions and a return to pre-pandemic care approaches became feasible again.
The lack of substantial differences in telehealth utilization by payment parity status in 2019 versus substantial and statistically significant differences in 2021 is an interesting finding. Prior to the pandemic, barriers to the provision of telehealth are well documented including concerns about reimbursement, liability, licensure, training, equipment, technology, and broadband availability.7,19,20 Providers had few incentives to adopt telehealth even if visits were reimbursed at parity, resulting in relatively low telehealth usage across the board.21 Less than 2% of providers offered outpatient visits via telehealth before the pandemic with the exception of mental health providers, of which 4%–5% provided care via telehealth.17 While a growing number of CHCs were offering telehealth prior to the pandemic, telehealth visit volume was relatively low across all CHCs.
As the public health emergency drove widespread use of telehealth, leading to large amounts of visits being conducted via telehealth, the environment became inherently different in 2021 than in 2019, when few used telehealth regardless of state policies.9 When masking and later vaccines made in-person encounters a relatively safe option again in 2021, CHCs in states without payment parity would now be at risk for losing money with telehealth encounters versus in-person visits. Furthermore, the temporary waivers around Health Insurance Portability and Accountability Act of 1996 (HIPAA) compliant technologies could add to the cost of offering telehealth for organizations relying on Zoom or other temporarily approved platforms at the end of the public health emergency. Due to the unique fiscal constraints facing CHCs, the financial sustainability of telehealth may be highly relevant to the relationship between telehealth utilization and payment parity we find in this article.
We also find that broadband access is positively associated with CHCs offering telehealth services. Conversely, we find rural CHCs are less likely to offer telehealth, consistent with earlier studies showing urban CHCs were more likely to offer higher volumes of telehealth visits than rural CHCs.22
Limitations
Privately insured patients at CHCs represented only 19% of patients in 2019.23 The FAIR Health data used in this study only covers privately insured patients (and Medicare Advantage), but does not represent the entire universe of privately insured claims, nor all CHC sites. Our data are therefore a sample of these visits. Our results are consistent with telehealth usage rates in UDS when looking at the percent of grantees where telehealth usage represented greater than 1% of total CHC visits (see Supplementary Appendix for further details on this comparison).
Further, we cannot control for whether individual commercial insurers are reimbursing at parity in states without payment parity laws. While insurers may indeed be reimbursing at parity in states without such requirements by law, they could revert to paying less. This fiscal uncertainty may influence an organization’s decision to invest in telehealth care delivery, making state policies that reduce uncertainty important in driving telehealth use.
Lastly, due to the limitations of our analysis, we do not claim that payment parity policies are causal in telehealth utilization. We are limited in our ability to estimate this direct, causal effect in our statistical model. Other policies around telehealth utilization (i.e. cost-sharing, audio only versus video requirements, etc.) could certainly have an effect on utilization and, more importantly to our limitation on causality, be correlated with payment parity policies. Additional research could help clarify the relative importance of different policy approaches on telehealth utilization.
POLICY IMPLICATIONS
To date, the availability and benefits of telehealth have not been evenly distributed among the population. Before and during the pandemic, numerous studies have documented lower telehealth utilization among the patient populations that have the greatest burden of disease and access to care challenges, including low-income, Medicaid, and rural patients.9,24
In order to realize telehealth’s potential to improve care for underserved populations, payment policies cannot financially penalize safety net providers, including CHCs, for offering telehealth services to patients. Payment parity may be an important strategy to ensure the ongoing use of telehealth at CHCs as they continue to operate in a predominantly fee for service environment. In the long-term, payment policies that offer greater support and flexibility to adopt telehealth as part of rewarding high-quality care at lower cost (value-based payment) would be preferred.7,20 Additional support is critical, as CHC providers and their patients face unique challenges.
At the practice level, although it is often perceived as a low-cost care modality, practices that provide both in-person care and telehealth must invest in secure and reliable technology. Patient privacy and information security are vital considerations and additional personnel training is required to coordinate and facilitate secure, high-quality care via telehealth.6 This is a heavy burden carried by CHCs, as they may lack the same types of technologies, equipment, and training resources as other medical practices.20
Patient preferences and needs are central to any health policy discussion. With respect to patient preferences, reports that low-income and underserved patient populations prefer in-person care should be interpreted with caution. In one health system evaluation, practices and clinicians appeared to drive variation in visit type more than patients.24 Others have noted that prior experience with telehealth is linked to patient preferences for telehealth versus in-person care.25 Limited telehealth resourcing and availability for low-income individuals may well influence patient preferences for in-person care, offering a convenient rationale to perpetuate the inequitable provision of telehealth services. When examined, patient satisfaction with telehealth in underserved populations has been high (with lack of stable internet as a notable exception).26,27
The use of telehealth in this sample was positively correlated with mental health visits, a need that increased during the pandemic.28 For CHC patients, the need for these services may already have been more acute, as living in a low-income household has been associated with an increased risk for mental health problems.29 Nonetheless, access to mental health services remains limited and telehealth could provide an important linkage to care for many underserved patients.30
Investments in broadband infrastructure could also help increase telehealth utilization. There is significant variation in access to broadband and digital services, which impacts rural and socioeconomically disadvantaged areas.31 The Infrastructure Investment and Jobs act was signed into law at the end of 2021, which contained significant provisions to increase access to digital services, with a specific focus on digital equity.32 Continued investments in digital equity will be important factors in expanding the ability for disadvantaged communities to access and utilize telehealth services. Not surprisingly, patients are dissatisfied with their visits when they do not have a stable internet connection, which interferes with virtual communication.33
CONCLUSION
The COVID-19 pandemic drastically elevated the role of telehealth in medical care and elevated the importance of related policies. We find CHC sites in states with payment parity policies were more likely to utilize telehealth 1 year after the onset of the pandemic than CHC sites in states without such requirements. Broadband access is also positively associated with CHCs offering telehealth services. Supportive payment policy and continued investments in broadband availability in rural and undeserved communities should enable CHCs to offer telehealth services to populations in these areas.
FUNDING
This project is supported by the Bureau of Health Workforce (BHW), National Center for Health Workforce Analysis (NCHWA), Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $450,000, with zero percent financed with non-governmental sources. The contents are those of the author[s] and do not necessarily represent the official views of, nor an endorsement by HRSA, HHS, or the U.S. Government.
AUTHOR CONTRIBUTIONS
All authors contributed equally to this work.
Supplementary material
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
Contributor Information
Clese Erikson, Fitzhugh Mullan Institute for Health Workforce Equity, Department of Health Policy and Management, Milken Institute School of Public Health, George Washington University, Washington, District of Columbia, USA.
Jordan Herring, Fitzhugh Mullan Institute for Health Workforce Equity, Department of Health Policy and Management, Milken Institute School of Public Health, George Washington University, Washington, District of Columbia, USA.
Yoon Hong Park, Fitzhugh Mullan Institute for Health Workforce Equity, Department of Health Policy and Management, Milken Institute School of Public Health, George Washington University, Washington, District of Columbia, USA.
Qian Luo, Fitzhugh Mullan Institute for Health Workforce Equity, Department of Health Policy and Management, Milken Institute School of Public Health, George Washington University, Washington, District of Columbia, USA.
Guenevere Burke, Fitzhugh Mullan Institute for Health Workforce Equity, Department of Health Policy and Management, Milken Institute School of Public Health, George Washington University, Washington, District of Columbia, USA.
DATA AVAILABILITY STATEMENT
The data for this article were obtained through contractual arrangements with FAIR Health, a third-party provider. The data cannot be shared publicly per the research license agreement between FAIR Health and George Washington University.
REFERENCES
- 1. Impact of Coronavirus on Community Health Centers | KFF [Internet]. https://www.kff.org/coronavirus-covid-19/issue-brief/impact-of-coronavirus-on-community-health-centers/ Accessed August 30, 2021.
- 2. Early Impact of CMS Expansion of Medicare Telehealth During COVID-19 | Health Affairs [Internet]. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/ Accessed August 30, 2021.
- 3. States’ Actions to Expand Telemedicine Access During COVID-19 | Commonwealth Fund [Internet]. https://www.commonwealthfund.org/publications/issue-briefs/2021/jun/states-actions-expand-telemedicine-access-covid-19 Accessed August 17, 2021.
- 4. Smith S, Raskin S.. Achieving health equity: examining telehealth in response to a pandemic. J Nurse Pract 2021; 17 (2): 214–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shachar C, Engel J, Elwyn G.. Implications for telehealth in a postpandemic future. JAMA 2020; 323 (23): 2375–6. [DOI] [PubMed] [Google Scholar]
- 6. Ellimoottil C. Understanding the case for telehealth payment parity. Health Affairs Blog 2021. https://www.healthaffairs.org/do/10.1377/forefront.20210503.625394/full/ [Google Scholar]
- 7. Lee NT, Karsten J, Roberts J. Removing Regulatory Barriers to Telehealth Before and After COVID-19 [Internet]. 2020. https://www.brookings.edu/research/removing-regulatory-barriers-to-telehealth-before-and-after-covid-19/#footnote-45 Accessed June 1, 2022.
- 8. Volk J, Palanker D, O’Brien M, Goe CL. States’ Actions to Expand Telemedicine Access During COVID-19 and Future Policy Considerations [Internet]. The Commonwealth Fund, 2021. https://www.commonwealthfund.org/publications/issue-briefs/2021/jun/states-actions-expand-telemedicine-access-covid-19 Accessed February 8, 2022.
- 9. Park J, Erikson C, Han X, Iyer P.. Are state telehealth policies associated with the use of telehealth services among underserved populations? Health Aff (Millwood) 2018; 37 (12): 2060–8. [DOI] [PubMed] [Google Scholar]
- 10. Lin CCC, Dievler A, Robbins C, Sripipatana A, Quinn M, Nair S.. Telehealth in health centers: key adoption factors, barriers, and opportunities. Health Aff (Millwood) 2018; 37 (12): 1967–74. [DOI] [PubMed] [Google Scholar]
- 11. Lori UP, Bouskill KE, Jessica S, Mimi S, Shira HF.. Experiences of medicaid programs and health centers in implementing telehealth. Rand Health Q 2020; 8(4):RR-2564-ASPE. [PMC free article] [PubMed] [Google Scholar]
- 12. Impact of the COVID-19 Pandemic on Primary Care Practices—RWJF [Internet]. https://www.rwjf.org/en/library/research/2021/02/impact-of-the-covid-19-pandemic-on-primary-care-practices.html Accessed August 30, 2021.
- 13. Basu S, Phillips RS, Phillips R, Peterson LE, Landon BE.. Primary care practice finances in the United States amid the COVID-19 pandemic. Health Aff (Millwood) 2020;39(9):1605–14. [DOI] [PubMed] [Google Scholar]
- 14. How the Rapid Shift to Telehealth Leaves Many Community Health Centers Behind During The COVID-19 Pandemic | Health Affairs [Internet]. https://www.healthaffairs.org/do/10.1377/hblog20200529.449762/full/?utm_campaign=HASU+6-7-20&utm_medium=email&utm_content=Health+Affairs++June+Issue%3A++Rural+Health%2C+Behavioral+Health+++More%3B+Editor-In-Chief+Alan+Weil+On+Institutional+Racism+And+Health+Care%3B+COVID-19%3A+Lessons+From+Chicago+s+Cook+County+Jail&utm_source=Newsletter& Accessed August 30, 2021.
- 15. Uscher-Pines L, Sousa J, Jones M, et al. Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA 2021; 325 (11): 1106–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gibson G, Rchn/Health C, Sharac J, et al. Months into the COVID-19 Pandemic, Community Health Centers Months into the COVID-19 Pandemic, Community Health Centers Report Signs of Improvement, But Face Financial Uncertainty Report Signs of Improvement, But Face Financial Uncertainty. 2020.
- 17. Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML.. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood) 2021; 40 (2): 349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. FAIR Health. Data Repository [Internet]. https://www.fairhealth.org/data Accessed February 8, 2022.
- 19. Moore MA, Coffman M, Jetty A, Petterson S, Basemore A. Only 15% of FPs Report Using Telehealth; Training and Lack of Reimbursement are Top Barriers [Internet]. 2016. https://www.aafp.org/pubs/afp/issues/2016/0115/p101.html Accessed June 4, 2022. [PubMed]
- 20. Kim JH, Desai E, Cole MB. How the Rapid Shift to Telehealth Leaves Many Community Health Centers Behind During the COVID-19 Pandemic [Internet]. 2020. https://www.healthaffairs.org/do/10.1377/forefront.20200529.449762/full/ Accessed February 8, 2022.
- 21. Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood) 2020; 39 (7): 1253–62. [DOI] [PubMed] [Google Scholar]
- 22. Demeke HB, Pao LZ, Clark H, et al. Telehealth practice among health centers during the COVID-19 pandemic—United States, July 11–17, 2020. MMWR Morb Mortal Wkly Rep 2020; 69 (50): 1902–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Health Resources & Services Administration (HRSA). National Health Center Program Uniform Data System (UDS) Awardee Data [Internet]. 2020. https://data.hrsa.gov/tools/data-reporting/program-data/national Accessed February 13, 2022.
- 24. Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I.. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021; 27 (1): 21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L.. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw Open 2021; 4 (12): e2136405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Burke G v, Osman KA, Lew SQ, et al. Improving specialty care access via telemedicine. Telemed J E Health 2022. [DOI] [PubMed] [Google Scholar]
- 27. Kyle MA, Blendon RJ, Findling MG, Benson JM.. Telehealth use and satisfaction among U.S. households: results of a national survey. J Patient Exp 2021; 8: 237437352110527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Panchal N, Kamal R, Cox C, Garfield R. The Implications of COVID-19 for Mental Health and Substance Use [Internet]. 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ Accessed February 10, 2022.
- 29. Hodgkinson S, Godoy L, Beers LS, Lewin A.. Improving mental health access for low-income children and families in the primary care setting. Pediatrics 2017; 139 (1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Warren JC, Smalley KB. Using Telehealth to Meet Mental Health Needs During the COVID-19 Crisis [Internet]. 2020. https://www.commonwealthfund.org/blog/2020/using-telehealth-meet-mental-health-needs-during-covid-19-crisis Accessed February 8, 2022.
- 31. Fisbane L, Tomer A. Neighborhood Broadband Data Makes It Clear: We Need an Agenda to Fight Digital Poverty [Internet]. 2020. https://www.brookings.edu/blog/the-avenue/2020/02/05/neighborhood-broadband-data-makes-it-clear-we-need-an-agenda-to-fight-digital-poverty/#:~:text=We%20have%20defined%20a%20tract,not%20have%20a%20wireless%20subscription.&text=Moreover%2C%20in%20a%20quarter%20of,tracts%20are%20experiencing%20digital%20poverty Accessed February 8, 2022.
- 32. U.S. Department of Commerce. Fact Sheet: Department of Commerce’s Use of Bipartisan Infrastructure Deal Funding to Help Close the Digital Divide [Internet]. 2021. https://www.commerce.gov/news/fact-sheets/2021/11/fact-sheet-department-commerces-use-bipartisan-infrastructure-deal-funding Accessed February 8, 2022.
- 33. Abdulwahab S, Zedan H.. Factors affecting patient perceptions and satisfaction with telemedicine in outpatient clinics. J Patient Exp 2021; 8: 237437352110637. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data for this article were obtained through contractual arrangements with FAIR Health, a third-party provider. The data cannot be shared publicly per the research license agreement between FAIR Health and George Washington University.