Abstract
In the wake of Coronavirus disease 2019 (COVID-19), several nations have sought to implement digital vaccine passports (DVPs) to enable the resumption of international travel. Comprising a minimum dataset for each unique individual, DVPs have the makings of a global electronic health record, broaching key issues involved in building a global digital health ecosystem. Debate simulations offer a safe, interactive space to foster participatory policy discussions for advancing digital health diplomacy. This study used an online simulation of a Model World Health Assembly to critically analyze the sociotechnical issues associated with the global implementation of DVPs, and to generate useful insights and questions about the role of diplomacy in global digital health. The debate arguments addressed and provided insights into the technological, scientific, ethical, legal, policy, and societal aspects of DVPs. Reflecting on the simulation, we discuss its opportunities and challenges for the digitalization, decolonization, decentralization, and democratization of participatory policymaking.
Keywords: global health informatics, global health diplomacy, Model World Health Organization, WHO simulation
INTRODUCTION
Digital vaccine passports (DVPs) are electronically documented verifications that someone has tested negative for, or has been protected against, certain infections.1 They provide a means for immigration authorities to determine who qualifies for entry into their borders based on disease or vaccination status. The curtailment of international travel to slow the spread of Coronavirus disease 2019 (COVID-19) hindered freedom of movement and stifled travel-dependant economic sectors. As COVID-19 vaccines became available, countries sought to certify vaccinated individuals for international travel, turning the discourse toward DVPs. Several nations are already implementing DVPs.2 However, with limited legal/technical standardization between the various technological approaches in use, they may not be interoperable, resulting in the fragmentation of certification systems.
To address this fragmentation, the World Health Organization (WHO) convened a Smart Vaccination Certificate Working Group to provide technical guidance on “key standards” for DVPs.3 Enacting this global DVP requires international governments to cooperate and agree on (1) universal standards, (2) a minimum dataset (eg, of vaccination details and basic health status), and (3) a unique personal ID system for DVPs, eventually associated with a unique ID for each person.4 This could build upon the International Patient Summary developed by the Joint Council for Global Health Informatics,5 and serve as an initial step toward a Global Electronic Health Record (G-EHR).
DVPs as a stepping-stone to a Global Electronic Health Record?
Achieving international consensus on DVPs could set a diplomatic precedent and lay the foundation for the future establishment of a G-EHR system, and guide the development of a governance mechanism for an interoperable global digital health ecosystem.6 Advancing this “sociotechnical” agenda would involve a multi-sectoral stakeholder discussion with relevant UN bodies, Standards Development Organizations, the WHO, and other interested parties. Diplomatic simulations offer a safe means to better prepare for this.
Diplomatic simulations for global digital health
Diplomacy is an increasingly essential aspect of global digital health.7 The WHO Global Strategy for Digital Health (2020–25) calls for “mechanisms for more effective public participation and transparency in national and international digital health decision-making processes, such as through international consultation processes or a stakeholder forum”. In a previous paper, we recognized the concept of Digital Health Diplomacy (DHD) as a type of Science diplomacy,7 we can relate to the Madrid Declaration for Science diplomacy which recommends (1) creating interactive spaces, (2) promoting bi-directional science and diplomacy fluency; (3) engaging the full spectrum of science; (4) ensuring open and interpretable science for diplomacy; and (5) exerting bold values-based leadership.8 These recommendations mirror those made by the WHO Global Strategy for Digital Health (2020–25), highlighting the need for interactive spaces to advance DHD. Parliamentary policy debates might offer such an “interactive space” for public participation, bi-directional fluency in digital health and diplomacy, where digital health can find application in diplomacy, and “bold values-based leadership” can be fostered.
Simulations are “a tool that reproduces the real-life characteristics of an event or situation”,9 and diplomatic simulations are well recognized to enable participants “to experience and more fully understand theories, issues and concepts within international relations”.10 As a type of diplomatic simulation, Model WHO (MWHO) simulations reenact the procedures of the WHO’s policymaking committee, the World Health Assembly.11 Following the “The Mercury Game”, which simulated policymaking to address an environmental health crisis, policymaking simulations in health science education have gained credence.12 Our prior simulations debated the health relevance of climate change,13 the built environment, and medicolegal issues of international relevance.13–18 Through active and experiential learning,10 policymaking simulations offer the participants an opportunity to gain substantive (ie, content-based) knowledge regarding the debate topic itself (2) process-based knowledge (ie, on debate procedure, and the science-policy interactions) and (3) communication knowledge (ie, knowledge translation).19,20 They also develop social learning and collaborative capacity, essential for negotiation, teamwork, and leadership.17 Online environments are increasingly being used to facilitate such policymaking simulations.21
Building on our previous work regarding debate simulations for cultivating digital health policymaking,22 this article reports on a pilot study of a simulated online debate on DVPs. This study sought to use a participatory policy simulation to critically analyze the sociotechnical issues associated with the global implementation of DVPs, and to generate useful insights and questions about the role of diplomacy in global digital health.
METHODS
Debate preparation
The Asia-Pacific Model United Nations Conference (AMUNC) is a traveling conference held annually in different countries within the Asia-Pacific region. It attracts participation from university students based within the region and beyond. AMUNC 2021 was held as an online conference owing to COVID-19-related restrictions on international travel. Through a competitive process, MAG was selected as director and chairperson of the MWHO simulation at AMUNC 2021. He proposed the debate topic and developed a policy brief to prepare participants for the debate (Table 1).23 This document outlined key considerations regarding DVPs for participating delegates to research with respect to their assigned nation’s policy stance, including technological, ethical, legal, scientific, and societal considerations. It referred to salient technical reports, policy documents, and peer-reviewed research. It outlined the current status of international health policy on travel, including the International Health Regulations and recent WHO publications.24 Delegates were given the policy brief 1 week before the debate to research the country they were assigned to represent in the MWHO council.
Table 1.
Thematic summary of key considerations regarding DVPs presented in the Policy brief
| Themes | Issues |
|---|---|
| Technological considerations |
|
| Ethical considerations |
|
| Legal considerations |
|
| Scientific considerations |
|
| Public Policy & Societal Concerns |
|
Debate process and context
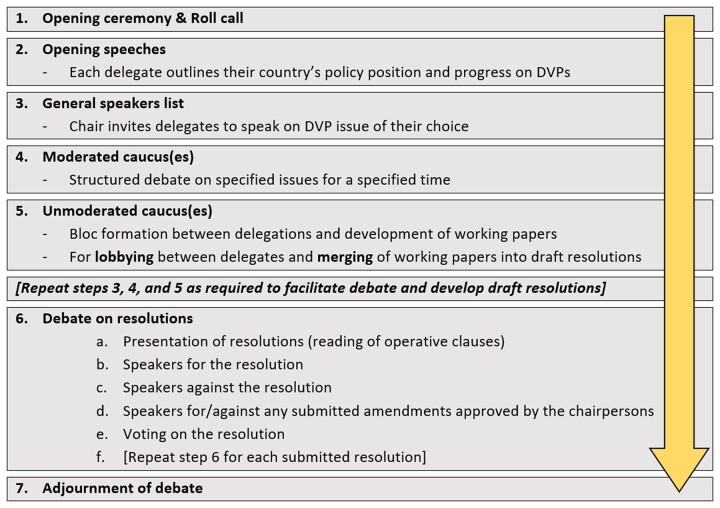
Debate on the issue lasted 3 days (October 1–4, 2021), beginning with opening statements to present nation’s policy positions, followed by a general speakers list. Delegates them motioned for moderated caucuses on specific topics where delegates each presented and rebutted arguments for up to 2 min each. Unmoderated caucuses (upto 1 h each) were permitted to enable lobbying and merging between delegates for negotiation, bloc formation and drafting working papers. An outline of the parliamentary procedure used is presented in Figure 1, and procedural details may be found elsewhere.38
Figure 1.
Outline of debate council procedure.
The conference timing coincided with media discourse on the Australian vaccine passport, and with a diplomatic issue on vaccine recognition for inclusion in a DVP between the United Kingdom and India, which illustrated the debate topic’s timeliness.39
Participants
The 6 participants were self-selected respondents to public advertising about the debate via social media platforms. They included law, development studies, medicine, and dentistry students from Australia, Indonesia, the Philippines, and the United States.
FINDINGS AND DISCUSSION
The findings reaffirmed the capacity of simulated debates to facilitate a critical discursive analysis of arguments in a safe, collegial setting. The debate provided insights into the practical, technical, and social challenges that countries may have when implementing DVPs and offered practical suggestions on the role of DHD in this process. Most arguments reflected the themes presented in the policy brief (Table 1).
Technological considerations
Delegates emphasized the importance of knowledge sharing between countries, especially to benefit those lacking the technology for implementing DVPs (aka “knowledge diplomacy”).40 Recognizing that DVPs can only be as reliable as the data maintained by governments’ record-keeping, delegates emphasized the need to establish minimum standards and hardware for data quality and security to ensure that once standardized, all nations accept the validity of DVPs, to avoid the risk of future challenges to their credibility.
Scientific considerations
For those unable to receive the COVID vaccine, delegations noted that DVPs should also record the traveler’s most recent negative test (and test type). Additionally, delegations recognized that not all vaccines are equally efficacious and that DVPs should include details of the vaccination received by the traveler. It was also noted that some countries might tend to recognize (and derecognize) vaccines based on their country of origin rather than their scientific properties (eg, efficacy, safety). Vaccines are also used as a form of humanitarian aid, giving rise to the phenomenon of vaccine diplomacy.41 Prejudice toward or against a vaccine can introduce political biases into what should be an objective, transparent, scientific process.39
Ethical considerations
While diplomacy has historically been the domain of international policymakers, this is rapidly changing as we become increasingly dependent on privately-owned, multi-national technology companies to provide the innovation required. The importance of non-state actors in providing the technology for implementing DVPs highlights the potential role of innovation diplomacy.42 This represents a changing configuration of actors in diplomacy and a shifting of the balance of power between these actors. It also highlights the importance of ensuring that essential digital public goods remain freely available for public use to avoid being beholden to private actors and their profit motives.
Legal considerations
The legal considerations included issues around collecting, storing, sharing, using and accessing personal health information. The participants recommended that DVP data not be held by the WHO but by the individuals’ home country. Instead, the WHO could be the accreditor of the certification system, ensuring its’ legitimacy. The decision suggested that countries lack trust in a centralized DVP system and have ongoing concerns about security breaches. This highlights the concerns of data diplomacy and related issues of international data security, privacy, and ownership.43 Data decentralization through blockchain technology was discussed as a potential solution to foster the trust required to help transition health systems toward virtual models of integrated care.44–47
Public policy and societal concerns
While certifiable medical exemptions were broadly considered legitimate, some nations raised concerns about the validity of religious exemptions. The discussion centered around the risk that they might offer an unquestionable label behind which anti-vaccination communities could disguise a misinformed agenda.
OPPORTUNITIES AND CHALLENGES FOR ONLINE DEBATE SIMULATIONS
As health diplomacy simulations continue to increase in popularity, conducting them in the online environment is likely to offer both opportunities and challenges.48
Opportunities for online debate simulations
Digitalization: The online nature of the conference underscored the potential for digital media to scale and sustain this innovation despite travel barriers, augmented by online tools (eg, MUNCoordinated) for MUN sessions over videoconferencing platforms (eg, Zoom). Delegates could participate without the added costs of travel, enabling participation from beyond the Western Pacific Region and democratizing participation overall.
Decolonization: While literature’s emphasis on health policy debate simulations in developed nations portrays them as a phenomenon of the global north,11 our experience with several health policy simulations in the global south suggest otherwise.13–18 Online debate platforms remove travel and cost barriers to participation, potentially improving opportunities for South-South sharing of culture and knowledge for health, accelerating the decolonization of global health through knowledge diplomacy.40,49 In the context of DHD, such knowledge sharing may help avoid reliance on donor nations in the global north who may skew policy agendas to their interests.7
Decentralization and Democratization: Online policymaking simulations and roleplays open to all irrespective of location can gain economies of scale, building local capacity through global conferences. Online simulations could be more rapidly adapted than in-person meetings to reflect changing geopolitics. This can potentially improve the local capacity for community advocacy and health policy change in developing nations,18 enabling more significant citizen input into local health governance,50 and care services.47
Challenges of online debate simulations
Most limitations can be attributed to the online mode of participation and the global distribution of participants. As delegates were based in very different time zones, some had to participate at unusual hours, likely affecting performance. Moreover, the shift to Australian Eastern Daylight Time during the conference caused some confusion about the timing of committee sessions.
Online conferences are a less enticing proposition for potential MUN participants when compared to in-person conferences, resulting in fewer registered participants and limiting the diversity of countries and perspectives in each debate council. With online meetings there is also a loss of interpersonal in-person communication, which can help build trust and help open more dialog among participants. There were also technical challenges related to internet bandwidth issues that hindered audio transmission and prevented video and screen sharing making it difficult to ensure that participants were attentively engaged or distracted. However, these issues are not unlike those faced by real-world diplomatic processes.51 Despite challenges to participation, the validity of debate arguments can still be considered on their merit.
CONCLUSION
Co-creating international consensus around DVPs that are globally interoperable is not just a public health, technical, or health systems challenge but also a trust-building effort, for which diplomatic experience and learning can be essential. While challenging to organize, online debate simulations can offer safe, collegial environments to train “digital health diplomats” and foster balanced conversations about digital health issues while ensuring equitable participation. This can create the necessary conditions to begin the journey toward a global EHR and digital health ecosystem.
AUTHOR CONTRIBUTIONS
MAG conceptualized and designed the work, interpreted the data, drafted the work critically for important intellectual content, approved the final version, and is accountable for all aspects of the work. S-TL made substantial contributions to the conception and design of the work, interpreted the data, revised the work critically for important intellectual content, approved the final version and is accountable for all aspects of the work. CK made substantial contributions to the interpretation of the data, revised the work critically for important intellectual content, approved the final version and is accountable for all aspects of the work. HFM made substantial contributions to the interpretation of the data, revised the work critically for important intellectual content, approved the final version, and is accountable for all aspects of the work. HM made substantial contributions to the interpretation of the data, revised the work critically for important intellectual content, approved the final version, and is accountable for all aspects of the work. YQ made substantial contributions to the interpretation of the data, revised the work critically for important intellectual content, approved the final version, and is accountable for all aspects of the work.
ACKNOWLEDGMENTS
We acknowledge and thank the participants, secretariat, and organizers of the Asia-Pacific Model United Nations Conference 2021 for their contributions. We also acknowledge Dr. Najeeb Al-Shorbaji for their contributions to the simulation preparation and policy brief.
CONFLICT OF INTEREST STATEMENT
None declared.
Contributor Information
Myron Anthony Godinho, WHO Collaborating Centre for eHealth, School of Population Health, UNSW Sydney, Sydney, Australia.
Siaw-Teng Liaw, WHO Collaborating Centre for eHealth, School of Population Health, UNSW Sydney, Sydney, Australia.
Chipo Kanjo, Department of Computer Science, University of Malawi, Zomba, Malawi.
Heimar F Marin, Federal University of São Paulo, São Paulo, Brazil.
Henrique Martins, ISCTE Business School, ISCTE-IUL, Lisbon, Portugal; Faculty of Health Sciences, Universidade da Beira Interior, Covilhã, Portugal.
Yuri Quintana, Division of Clinical Informatics, Beth Israel Deaconess Medical Center, Boston, Massachusetts, USA; Harvard Medical School, Boston, MA, USA.
DATA AVAILABILITY STATEMENT
All data are contained within the manuscript and associated materials.
REFERENCES
- 1. Satria FB, Khalifa M, Rabrenovic M, Iqbal U.. Can digital vaccine passports potentially bring life back to “true-normal”? Comput Methods Programs Biomed 2021; 1: 100011. [Google Scholar]
- 2. Mithani SS, Bota AB, Zhu DT, Wilson K. A scoping review of global vaccine certificate solutions for COVID-19. Hum Vaccin Immunother 2022; 18 (1): 1–12. [DOI] [PMC free article] [PubMed]
- 3. World Health Organisation. Digital documentation of COVID-19 certificates: vaccination status: technical specifications and implementation guidance Geneva: World Health Organisation; 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Digital_certificates-vaccination-2021.1. Accessed May 31, 2022.
- 4. Pavli A, Maltezou HC.. COVID-19 vaccine passport for a safe resumption of travel. J Travel Med 2021; 28 (4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Joint Initiative Council for Global Health Informatics Standardization. The International Patient Summary. 2022. https://international-patient-summary.net/. Accessed May 31, 2022.
- 6. Martins HM. Digital health diplomacy in chained globalised health context. Health Management 2020; 20 (10): 712–5. [Google Scholar]
- 7. Godinho MA, Martins H, Al-Shorbaji N, Quintana Y, Liaw S-T.. Digital Health Diplomacy” in Global Digital Health? A call for critique and discourse. J Am Med Inform Assoc 2022; 29 (5): 1019–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. S4D4C. The Madrid Declaration on Science Diplomacy. Madrid: S4D4C; 2019.
- 9. Chernikova O, Heitzmann N, Stadler M, Holzberger D, Seidel T, Fischer F.. Simulation-based learning in higher education: a meta-analysis. Rev Educ Res 2020; 90 (4): 499–541. [Google Scholar]
- 10. Obendorf S, Randerson C.. Evaluating the Model United Nations: diplomatic simulation as assessed undergraduate coursework. Eur Polit Sci 2013; 12 (3): 350–64. [Google Scholar]
- 11. Wong BL, Khurana MP, Acharya N, Drejza M, Martins D.. World Health Organization simulations: an increasingly popular learning tool for the development of future global health practitioners. J Glob Health 2020; 10 (1): 010305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stokes LC, Selin NE.. The mercury game: evaluating a negotiation simulation that teaches students about science-policy interactions. J Environ Stud Sci 2016; 6 (3): 597–605. [Google Scholar]
- 13. Godinho MA, Murthy S, Mohammed CA.. Academic health policy debates for local climate change leadership. Lancet Planet Health 2019; 3 (10): e407. [DOI] [PubMed] [Google Scholar]
- 14. Godinho MA, Murthy S, Mohammed CA.. Fostering global health policy leadership through World Health Assembly simulations: debating Climate Change and Health. Health Promot Int 2021; 36 (3): 731–40. [DOI] [PubMed] [Google Scholar]
- 15. Am C, Godinho MA, Murthy S, et al. The built environment and health: fostering interprofessional collaboration for better policy recommendations. J Interprof Care 2020; 34 (3): 414–7. [DOI] [PubMed] [Google Scholar]
- 16. Godinho MA, Murthy SA, Mohammed C. Medical Model United Nations (MedMUN): a platform for evidence-based policy debates in the health professions classroom [version 1; not peer reviewed] 2017 [1713]. 10.7490/f1000research.1114889.1. [DOI]
- 17. Godinho MA, Murthy S, Ali Mohammed C.. Debating evidence-based health policy in an interprofessional classroom: an exploratory study. J Interprof Care 2019; 33 (5): 576–8. [DOI] [PubMed] [Google Scholar]
- 18. Godinho MA, Murthy S, Ciraj AM.. Health policy for health professions students: building capacity for community advocacy in developing nations. Educ Health (Abingdon) 2017; 30 (3): 254–5. [DOI] [PubMed] [Google Scholar]
- 19. Selin NE, Stokes LC, Susskind LE.. The need to build policy literacy into climate science education. Wiley Interdiscip Rev Clim Change 2017; 8 (3): e455. [Google Scholar]
- 20. Rumore D, Schenk T, Susskind L.. Role-play simulations for climate change adaptation education and engagement. Nat Clim Change 2016; 6 (8): 745–50. [Google Scholar]
- 21. Doumanis I, Economou D, Sim GR, Porter S.. The impact of multimodal collaborative virtual environments on learning: a gamified online debate. Comput Educ 2019; 130: 121–38. [Google Scholar]
- 22. Godinho MA, Borda A, Kostkova P, Molnar A, Liaw S-T.. Serious Games’ for unboxing Global Digital Health policymaking. BMJ Stel 2020; 6 (5): 255–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asia-Pacific Model United Nations Conference 2021. AMUNC 2021 World Health Organisation Background Guide: AMUNC 2021; 2021. https://amunc.org/s/AMUNC-2021-WHO-Background-Guide.pdf. Accessed May 31, 2022.
- 24. World Health Organisation. Interim position paper: considerations regarding proof of COVID-19 vaccination for international travellers. World Health Organisation; 2021. https://www.who.int/news-room/articles-detail/interim-position-paper-considerations-regarding-proof-of-covid-19-vaccination-for-international-travellers. Accessed May 31, 2022.
- 25. Corici AA, Hühnlein T, Hühnlein D, Rode O, ed. Towards Interoperable Vaccination Certificate Services. In: The 16th International Conference on Availability, Reliability and Security; Association for Computing Machinery; August 17, 2021: 1–9. https://doi.org/10.1145/3465481.3470035. Accessed May 31, 2022.
- 26. Wilford SH, McBride N, Brooks L, et al. The digital network of networks: regulatory risk and policy challenges of vaccine passports. Eur J Risk Regul 2021; 12 (2): 393–11. [Google Scholar]
- 27. Angelopoulos CM, Damianou A, Katos V. DHP Framework: Digital Health Passports Using Blockchain—use case on international tourism during the COVID-19 pandemic. arXiv 2020. doi: 10.48550/arXiv.2005.08922. [DOI]
- 28. Ouellette M, Shaw ML. For a Decentralized Vaccine Passport. Health Policy. Montreal Economic Institute (MEI); 2021. https://www.iedm.org/wp-content/uploads/2021/04/lepoint042021_en.pdf. Accessed May 31, 2022.
- 29. Ricci L, Maesa DDF, Favenza A, Ferro E.. Blockchains for covid-19 contact tracing and vaccine support: a systematic review. IEEE Access 2021; 9: 37936–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Osama T, Razai MS, Majeed A. Covid-19 vaccine passports: access, equity, and ethics. BMJ2021; 373: n861. doi: 10.1136/bmj.n861. [DOI] [PubMed] [Google Scholar]
- 31. Ljungholm DP, Olah ML.. Implementing digital vaccine passports to control the spread of COVID-19: law, rights, and ethics. Linguist Philos Investig 2021; 20: 35–44. [Google Scholar]
- 32. Milan S, Veale M, Taylor L, Gurses S.. Promises made to be broken: performance and performativity in digital vaccine and immunity certification. Eur J Risk Regul 2021; 12 (2): 382–92. [Google Scholar]
- 33. Voo TC, Reis AA, Thomé B, et al. Immunity certification for COVID-19: ethical considerations. Bull World Health Organ 2021; 99 (2): 155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. World Health Organisation. Statement on the sixth meeting of the International Health Regulations (2005) Emergency Committee regarding the coronavirus disease (COVID-19) pandemic. 2021. https://www.who.int/news/item/15-01-2021-statement-on-the-sixth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic. Accessed May 31, 2022.
- 35. Thomas B, Flood CM, Krishnamurthy V, Tanner R, Wilson K. Vaccine Ins and Outs: An Exploration of the Legal Issues Raised by Vaccine Passports. Vaccine. C.D.HOWE INSTITUTE; 2021. https://www.cdhowe.org/sites/default/files/attachments/research_papers/mixed/Working%20Paper%202021-07-13.pdf. Accessed May 31, 2022.
- 36. Blinken AJ, Becerra X.. Strengthening global health security and reforming the international health regulations: making the world safer from future pandemics. JAMA 2021; 326 (13): 1255. [DOI] [PubMed] [Google Scholar]
- 37. World Health Organization. Digital Technology and COVID-19 in the Western Pacific Region. WHO Regional Office for the Western Pacific; 2021. https://apps.who.int/iris/handle/10665/343609. Accessed May 31, 2022.
- 38. Chen GM. United Nations Handbook. 2011. https://www.scribd.com/doc/9717149/Model-United-Nations-Handbook Accessed September 21, 2016.
- 39. Krishnan M. India: How disputes over digital vaccine certificates are limiting travel options: Deutsche Welle. 2021. https://p.dw.com/p/40yqg. Accessed May 31, 2022.
- 40. Knight J. Knowledge Diplomacy. International Higher Education 2020; (100): 38–9. [Google Scholar]
- 41. Hotez PJ, Narayan KV.. Restoring vaccine diplomacy. JAMA 2021; 325 (23): 2337–8. [DOI] [PubMed] [Google Scholar]
- 42. Leijten J. Exploring the future of innovation diplomacy. Eur J Futures Res 2017; 5 (1): 20. [Google Scholar]
- 43. Boyd A, Gatewood J, Thorson S, Dye TD.. Data diplomacy. Sci Diplomacy 2019; 8 (1). https://www.sciencediplomacy.org/article/2019/data-diplomacy. [PMC free article] [PubMed] [Google Scholar]
- 44. Jonnagaddala J, Godinho MA, Liaw ST.. From telehealth to virtual primary care in Australia? A rapid scoping review. Int J Med Inform 2021; 151: 104470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Godinho MA, Jonnagaddala J, Gudi N, Islam R, Narasimhan P, Liaw S-T.. mHealth for integrated people-centred health services in the Western Pacific: a systematic review. Int J Med Inform 2020; 142: 104259. [DOI] [PubMed] [Google Scholar]
- 46. Godinho MA, Ashraf MM, Narasimhan P, Liaw S-T.. Community health alliances as social enterprises that digitally engage citizens and integrate services: a case study in Southwestern Sydney (protocol). Digit Health 2020; 6: 2055207620930118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Godinho MA, Ashraf MM, Narasimhan P, Liaw S-T.. Digital health, social enterprise & citizen engagement in integrated people-centred health services: a hermeneutic systematic review and preliminary framework synthesis. Int J Integr Care 2021; 20 (3): 196. [Google Scholar]
- 48. Li J, John A, Tasos E, et al. WHO simulations for youth engagement in global governance in a post-COVID world: Opportunities and challenges of moving conferences online. J Glob Health 2021; 11:03070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Khan M, Abimbola S, Aloudat T, Capobianco E, Hawkes S, Rahman-Shepherd A.. Decolonising global health in 2021: a roadmap to move from rhetoric to reform. BMJ Glob Health 2021; 6 (3): e005604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Godinho MA, Borda A, Kariotis T, Molnar A, Kostkova P, Liaw S-T.. Knowledge co-creation in participatory policy and practice: building community through data-driven direct democracy. Big Data & Society 2021; 8 (1): 205395172110194. [Google Scholar]
- 51. Lynch CU. Agencies Struggle to Carry On Remotely Foreign Policy: THE SLATE GROUP; 2020. https://foreignpolicy.com/2020/04/03/united-nations-coronavirus-pandemic-human-rights-council-work-remotely/. Accessed May 31, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are contained within the manuscript and associated materials.