Abstract
Background
During the COVID-19 pandemic, the incidence of chronic disease had drastically been reduced due to health care interruptions. The aim of this study is to analyse cancer diagnosis during the last 2 years of the COVID-19 pandemic.
Methods
Time-series study of cancer diagnoses recorded in primary care settings, using data from the primary care electronic health records from January 2014 to December 2021. We obtained the expected monthly rate per 100,000 inhabitants using a time regression adjusted by trend and seasonality. We additionally compared rates of cancer diagnoses in 2019 with those of 2020 and 2021 using the t-test. We performed the analysis globally, by sex and by type of cancer.
Results
In 2020, the rate of cancer diagnoses had reduced by −21% compared to 2019 (P < 0.05). Greater reductions were observed during the lockdown in early 2020 (>40%) and with some types of cancers, especially prostate and skin cancers (−29.6% and −26.9%, respectively, P < 0.05). Lung cancers presented statistically non-significant reductions in both years. Cancer diagnosis returned to expected around March 2021, and the rate in 2021 was similar to that of 2019 (overall difference of 0.21%, P = 0.967). However, an 11% reduction was still found when comparing the pandemic months of 2020–2021 with pre-pandemic months.
Conclusions
Although primary care cancer diagnoses in 2021 have returned to pre-pandemic levels, missing diagnoses during the last 2 years have not been fully recovered.
Keywords: COVID-19, electronic health records, epidemiology, neoplasms, primary care
Key messages.
Cancer diagnoses have dramatically dropped worldwide in 2020.
We observe a 21% decline in 2020, but a return to pre-pandemic rates in 2021.
An 11% drop was still found comparing pre-pandemic to pandemic months.
Reductions were greater during the lockdown (>40%).
Lung and breast cancers presented fewer reductions.
Prostate and skin cancers had greater drops.
Background
The coronavirus disease 2019 (COVID-19) pandemic has put healthcare systems around the world under unprecedented pressure, leading to a disruption in health care which included suspension of screening programmes, reduction of chronic disease control, and reduction of non-COVID diagnosis, among others.1,2
Cancer diagnoses decreased in 2020 in several countries.3–6 In a previous study in Catalonia (Spain), we observed a 34% reduction in cancer diagnosis from March to September 2020, but this reduction was even higher during the lockdown (>40%).7 These disruptions were likely to lead to significant delays in cancer diagnosis and treatment, which would translate into more cancers diagnosed in later stages and decreased long-term survival.4,8–10
Although this situation is well described in several articles, these studies are focused on cancer trends in 2020, and little is known about cancer diagnosis evolution during the second year of the COVID-19 pandemic. After the first wave of COVID-19, some restrictions were lifted in several countries and screening programmes were recovered, thus contributing to a change in cancer diagnostic trends. For instance, in a study in Canada, researchers observed that after a huge drop in cancer screening during the first months of COVID-19 pandemic, within a few months, programmes and cancer management had been adapted to the new situation and 1 year later, the number of procedures had reached pre-pandemic levels, suggesting that the level of cancer diagnosis level had returned to normal.11
The aim of our study is to analyse cancer diagnosis through the analysis of primary care electronic health records (EHR) data in Catalonia almost 2 years after the beginning of the COVID-19 pandemic, by updating the previous figures7 and with the hypothesis that after a reduction in cancer diagnosis in 2020, cancer diagnoses in 2021 have reached pre-pandemic levels.
Methods
We performed a time-series study of cancer case reported diagnoses in primary care settings. Data were extracted from the primary care EHR of the Institut Català de la Salut (Catalan Institute of Health; or ICS, its Catalan initials). ICS is the main primary care provider in Catalonia. It manages around 75% of all primary care practices (PCPs) in the Catalan public health system and covers about 5.8 million people. We included all patients aged over 14 years with a clinical diagnosis of cancer according to the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10 CM) (Supplementary material S1). The study period was from January 2014 to December 2021. We divided this period into two sets for the time-series analysis: training (2014–2019) and analysis (2020–2021). Validation and details of the model used in this research were described elsewhere.7
Monthly cancer rates per 100,000 inhabitants were calculated. Time-series were performed globally, and by sex and type of cancer. To contextualize, some related cancer diagnostic procedures, such as mammograms and colonoscopies were also analysed.
Statistical analysis
We obtained the point forecast and 95% confidence interval (95% CI) of expected monthly cancer diagnoses rate for the analysis period by projecting the time-series regression model from the rate per 100,000 inhabitants fitted in the training period. The adjustment variables were the trend and seasonality of the time series. We also calculated the percentage of reduction as follows: (observed rate − expected rate)/expected rate. More details are provided in a previous publication.7 The same analysis was performed for some diagnostic procedures with data available, such as mammograms and colonoscopies.
Additionally, we compared the monthly average rate of cancer diagnoses registered in primary care settings in 2019 with those of 2020 and 2021 using the independent-samples t-test, and we calculated the percentage of reduction compared to 2019.
Finally, we calculated the Pearson’s correlation coefficient (R) between monthly colorectal cancer (CRC) and colonoscopies and between mammograms and breast cancer during the pandemic months of 2020 and 2021.
All analyses were conducted using R v.3.5.1.
Results
From January 2014 to December 2021, 327,452 new malignant neoplasms were registered in the Catalan primary care EHR. This represents a monthly average rate per 100,000 inhabitants of 72.5 during the 2014–2018 period, 73.0 in 2019, only 57.4 in 2020, and 73.2 in 2021.
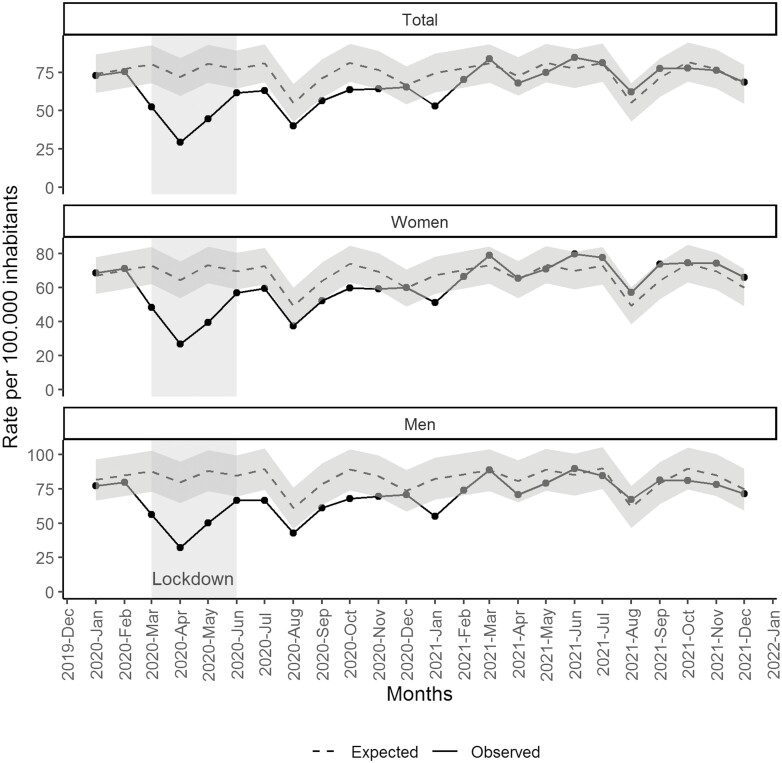
Figure 1 shows the observed and estimated monthly rates of cancer diagnoses (with 95% CI) since January 2020. We observed great reductions in 2020, especially during March (−35%), April (−59%), and May (−45%), coinciding with the first wave of COVID-19 and the lockdown in Spain. After that period, cancer diagnoses were below the expected but with lesser reductions (i.e. statistically significant reductions between 10% and 20%) until March 2021 where rates remained closer to the estimated; and slightly above the expected for women (Supplementary material S2).
Fig. 1.
Monthly observed and expected (with 95% CI) rate of cancer diagnoses per 100,000 inhabitants registered in Catalan primary care settings since January 2020, total and by sex.
During the pre-pandemic year 2019, 42,799 new malignant neoplasms were registered in the Catalan primary care EHR. This number decreased to 34,024 in 2020 and slightly increased in 2021 (43,719 new cancers registered). By comparing the monthly average of new cancer diagnoses rates in 2019, 2020, and 2021, we observed a 21.4% reduction in 2020 (P < 0.05) and a statistically non-significant increase of 0.21% in 2021 (P = 0.967). However, if we compared the pandemic months of 2020 and 2021 (from March 2020 to December 2021) to the pre-pandemic period (from January 2019 to February 2020) an overall 11.8% decline was still found (P < 0.05). We estimated that the overall reduction during the nearly 2 years of the COVID-19 pandemic accounted for 10,262 (95% CI: 4,737 to 15,787) fewer cancer diagnoses.
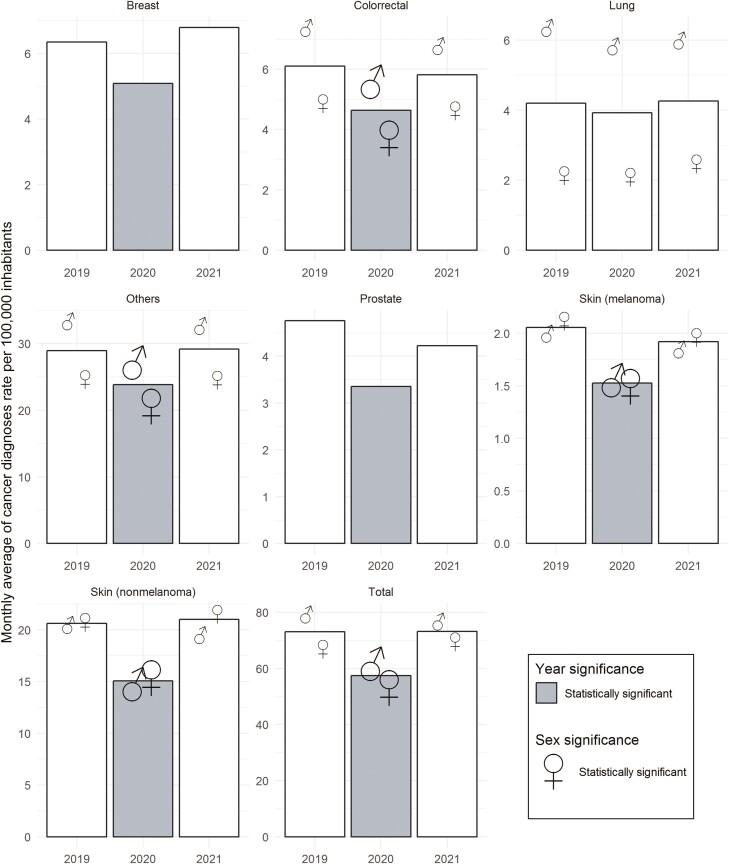
All types of cancer presented reductions in 2020, although they differ depending on the type of cancer and were similar for both sexes (Fig. 2). Reductions in 2020 compared to 2019 accounted for −29.6%, −26.9%, −25.7%, − 23.9%, −19.8%, and −17.6% in prostate cancer, non-melanoma skin cancer, melanoma, CRC, breast cancer and other cancers, respectively (P < 0.05). Contrarily, lung cancer had a non-significant reduction of −6.6% (P = 0.266). In 2021, all cancers reached similar rates to those of 2019, although prostate and melanoma had 11.2% (P = 0.12) and 6.7% (P = 0.34) drops, respectively; while breast cancer had a 7% increase (P = 0.19).
Fig. 2.
Mean monthly rate of cancer diagnoses registered in Catalan primary care settings by type of cancer and year (2019–2021). Reference value is the monthly average rate of cancer diagnoses in 2019 by type of cancer. Bars represent the total monthly average rate and the sex symbols represent the stratified values. Bars coloured in grey represent statistically significant differences compared to 2019 for the overall population. Larger sex symbols represent statistically significant differences by sex compared to 2019.
Finally, we observed that since mid-2021, the rates of diagnostic procedures were similar to the expected (Supplementary material S3). In addition, we observed a high correlation during the pandemic months between CRC and colonoscopies with R = 0.78, and between mammograms and breast cancer with R = 0.73. The number of diagnostic procedures by year is provided in Supplementary material S4.
Discussion
We hereby describe a reduction in cancer diagnoses in 2020 and a return to the expected in 2021. The reduction was greater during the early stages of the pandemic, coinciding with the lockdown in Spain. However, after the first months, cancer diagnosis rates were also consistently under the expected until March 2021, just after the third COVID-19 wave in Spain, where diagnosis returned to baseline levels (i.e. comparable to 2019) and remained relatively stable thereafter. Other studies worldwide described similar reductions in 2020 as in our research,3–6,12 highlighting the impact of the pandemic on non-COVID diseases. Several reasons have been described to explain this decrease, such as disruption of health care due to the pandemic, drop of face-to-face visits, halt of screening and diagnostic procedures and non-essential services, some COVID-19 control measures, and changes in patients’ healthcare-seeking behaviour, among others.7,13,14
Nevertheless, primary care adapted quickly to the COVID-19 pandemic within a few months, and cancer diagnosis rates in 2021 returned to similar values to those of 2019 in Catalonia. Despite this, the return to pre-pandemic diagnosis level in 2021 did not compensate for the drops in 2020, and more than 10,000 diagnoses were still missed. Although a part of this reduction could be related to the harvesting effect due to the high impact of the first COVID-19 wave in Spain in terms of mortality, a study performed in Catalonia in 2020 estimated that only 4% of diagnoses may have been lost to COVID-19 deaths.2 This means that there has yet to be a complete recovery with a reduction of diagnosis still outstanding. This could still have consequences described elsewhere such as diagnoses in more advanced stages and delays in treatments that could affect patients’ survival.9,15–17 This return to the 2019 diagnosis level is not yet described in many articles, although some studies observed that screening programmes and cancer diagnosis returned to close to pre-pandemic levels in late 2020.11,12
Regarding the type of cancer, we found a similar trend in all of them, with a reduction in 2020 and a return to pre-pandemic level in 2021 (although with different percentages), except for lung cancer. This different pattern for lung cancer was observed in other articles2,7 and could be related to an increase of chest radiographs due to COVID-19 pulmonary infections that led to more incidental findings, as suggested in previous research.7
Limitations of this analysis include the ecological analysis, alterations in patients’ healthcare-seeking behaviour during the COVID-19 pandemic, and the use of primary care EHR data and thus a potential lack of hospital diagnoses, although Catalan primary care EHR have been previously validated for cancer research.18
In conclusion, although the level of primary care cancer diagnosis in 2021 has returned to pre-pandemic levels, lost diagnoses during the last 2 years have not been fully recovered. Additional strategies may be needed, such as public awareness campaigns, promoting participation in screening programmes, and improving coordination between primary care and hospitals, to address remaining backlogs and potential consequences in terms of long-term cancer survival.
Supplementary Material
Acknowledgments
We would like to acknowledge the efforts of all members of the SISAP team during the last months. We would also like to thank all the primary care healthcare professionals in Catalonia during these challenging times and thank the Spider’s Web translator company for their English-style review of the manuscript.
Contributor Information
Núria Mora, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Carolina Guiriguet, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain; Equip d’Atenció Primària de Gòtic, Institut Català de la Salut, Barcelona, Spain.
Roser Cantenys, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Leonardo Méndez-Boo, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Mercè Marzo-Castillejo, Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol), Barcelona, Spain; Unitat de Suport a la Recerca Metropolitana Sud, Direcció d’Atenció Primària Costa de Ponent, Institut Català de la Salut, Barcelona, Spain.
Mència Benítez, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain; Equip d’Atenció Primària de Gòtic, Institut Català de la Salut, Barcelona, Spain.
Francesc Fina, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Mireia Fàbregas, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Eduardo Hermosilla, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain; Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol), Barcelona, Spain.
Albert Mercadé, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Manuel Medina, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Ermengol Coma, Sistemes d’Informació dels Serveis d’Atenció Primària (SISAP), Institut Català de la Salut (ICS), Barcelona, Spain.
Funding
None.
Conflict of interest
None.
Ethical approval
This study was done in accordance with existing statutory and ethical approvals from the Clinical Research Ethics Committee of the IDIAPJGol (project code: 20/172-PCV).
Data availability
EHR data and analytical code are provided at https://github.com/ErmengolComa/cancer2021/.
References
- 1. Dinmohamed AG, Cellamare M, Visser O, de Munck L, Elferink MAG, Westenend PJ, Wesseling J, Broeders MJM, Kuipers EJ, Merkx MAW, et al. The impact of the temporary suspension of national cancer screening programmes due to the COVID-19 epidemic on the diagnosis of breast and colorectal cancer in the Netherlands. J Hematol Oncol. 2020;13(1):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pifarré I Arolas H, Vidal-Alaball J, Gil J, López F, Nicodemo C, Saez M.. Missing diagnoses during the COVID-19 pandemic: a year in review. Int J Environ Res Public Health. 2021;18(10):5335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zadnik V, Mihor A, Tomsic S, Zagar T, Bric N, Lokar K, Oblak I. Impact of COVID-19 on cancer diagnosis and management in Slovenia—preliminary results. Radiol Oncol. 2020;54(3):329–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dinmohamed AG, Visser O, Verhoeven RHA, Louwman MWJ, van Nederveen FH, Willems SM, Merkx MAW, Lemmens VEPP, Nagtegaal ID, Siesling S. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020;21(6):750–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Vincentiis L, Carr RA, Mariani MP, Ferrara G.. Cancer diagnostic rates during the 2020 ‘lockdown’, due to COVID-19 pandemic, compared with the 2018-2019: an audit study from cellular pathology. J Clin Pathol. 2021;74(3):187–189. [DOI] [PubMed] [Google Scholar]
- 6. London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform. 2020;4:657–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coma E, Guiriguet C, Mora N, Marzo-Castillejo M, Benítez M, Méndez-Boo L, Fina F, Fàbregas M, Mercadé A, Medina M.. Impact of the COVID-19 pandemic and related control measures on cancer diagnosis in Catalonia: a time-series analysis of primary care electronic health records covering about five million people. BMJ Open. 2021;11(5):e047567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sud A, Jones ME, Broggio J, Loveday C, Torr B, Garrett A, Nicol DL, Jhanji S, Boyce SA, Gronthoud F, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020;31(8):1065–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nossiter J, Morris M, Parry MG, Sujenthiran A, Cathcart P, van der Meulen J, Aggarwal A, Payne H, Clarke NW. Impact of the COVID-19 pandemic on the diagnosis and treatment of men with prostate cancer. BJU Int. 2022. doi:10.1111/bju.15699. [DOI] [PubMed] [Google Scholar]
- 10. Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, Rachet B, Aggarwal A. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Decker KM, Feely A, Bucher O, Singh H, Turner D, Lambert P.. Evaluating the impact of the COVID-19 pandemic on cancer screening in a central Canadian province. Prev Med. 2022;155:106961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Peacock HM, Tambuyzer T, Verdoodt F, Calay F, Poirel HA, De Schutter H, Francart J, Van Damme N, Van Eycken L. Decline and incomplete recovery in cancer diagnoses during the COVID-19 pandemic in Belgium: a year-long, population-level analysis. ESMO Open. 2021;6(4):100197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2021;19(5):1875–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vanni G, Materazzo M, Pellicciaro M, Ingallinella S, Rho M, Santori F, Cotesta M, Caspi J, Makarova A, Pistolese CA, et al. Breast cancer and COVID-19: the effect of fear on patients’ decision-making process. In Vivo. 2020;34(3 Suppl):1651–1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cano-Valderrama O, Sánchez-Santos R, Vigorita V, Paniagua M, Flores E, Garrido L, Facal C, Ruano A, San-Ildefonso A, Moncada E. ¿Ha cambiado la pandemia de COVID-19 la presentación clínica y el estadio tumoral en el momento del diagnóstico en los pacientes con cáncer colorrectal? Estudio retrospectivo de cohortes [Has the COVID-19 pandemic changed the clinical picture and tumour stage at the time of presentation of patients with colorectal cancer? A retrospective cohort study.] [published online ahead of print, 2022 Feb 11]. Cir Esp. 2022. [Google Scholar]
- 16. Petrova D, Pollán M, Rodriguez-Barranco M, Garrido D, Borrás JM, Sánchez MJ.. Anticipated help-seeking for cancer symptoms before and after the coronavirus pandemic: results from the Onco-barometer population survey in Spain. Br J Cancer. 2021;124(12):2017–2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sud A, Torr B, Jones ME, Broggio J, Scott S, Loveday C, Garrett A, Gronthoud F, Nicol DL, Jhanji S, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21(8):1035–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Recalde M, Manzano-Salgado CB, Díaz Y, Puente D, Garcia-Gil MDM, Marcos-Gragera R, Ribes-Puig J, Galceran J, Posso M, Macià F, et al. Validation of cancer diagnoses in electronic health records: results from the information system for research in primary care (SIDIAP) in northeast Spain. Clin Epidemiol. 2019;11:1015–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
EHR data and analytical code are provided at https://github.com/ErmengolComa/cancer2021/.