Abstract
Background
There is significant concern that cancer care is adversely impacted due to the coronavirus disease pandemic. Using the national database, we document the impact of the pandemic on cancer diagnosis in Japan.
Methods
Data from 735 hospital-based cancer registries, covering >70% of newly diagnosed cases, were analysed. We compared trends during 2016–2019 and those in 2020 by the type of cancer, diagnostic process, stage and 13 prefectures as requiring special precautions to prevent the spread of infection.
Results
Overall, the number of patients who began treatment decreased by 1.9% in 2020 as compared with the average number during 2016–2019. A sharp decline of 13.8% was observed for stomach cases. The decline in cases (22.0% decrease for all cancers) was more pronounced in May. Cancer screening and resulting detection decreased significantly in 2020 (8.1–24.3%). Case registrations of stage I and II gastric cancer, stage II intrahepatic cholangiocarcinoma, stage II oesophageal cancer, stage 0 and I laryngeal cancer and stage II gallbladder cancer decreased by >10% compared with those in 2018 and 2019. The trends in cancer cases by area of residence indicated a decline in 13 prefectures in May 2020 compared with other areas.
Conclusions
The number of cancer diagnoses decreased during the year 2020 under coronavirus pandemic, especially right after the Japanese government declared the first state of emergency in April. We need to carefully observe the consequences of these decrease in diagnosis, or perhaps the delay in care, on patient survival or population mortality.
Keywords: treatment, real-world data, neoplasms, hospital-based cancer registries, COVID-19
The number of patients diagnosed with cancer who initiated treatment reduced since the Japanese government first declared the state of emergency in April during the COVID-19 pandemic.
Introduction
The World Health Organization declared the coronavirus disease 2019 (COVID-19) a ‘Public Health Emergency of International Concern’ in January 2020. Since then, there has been a significant concern that COVID-19 has had a negative impact on cancer care (1). The primary concern was that people may refrain from consulting with a specialist even if they had symptoms, as they were concerned about getting infected with severe acute respiratory syndrome coronavirus 2 in clinical settings. Early simulation studies warned that the delay in care will have led to the substantial increase in the number of avoidable cancer deaths (2–6). Long-term effects of the COVID-19 pandemic can have a significant impact on cancer patient survival (2,6). Furthermore, recent reports on cancer care in several countries, including those from England and New Zealand, have reported that COVID-19 has led to a sustained reduction (40–63%) in the number of people referred, diagnosed and treated in the first half of 2020 (7–9). Although there is oscillation in the number of infected people, COVID-19 continues to be a major public health issue as of January 2022.
In Japan, the number of infected people increased since the first case was reported on 15 January 2020. The government declared the first state of emergency on 7 April 2020 and extended it until 25 May 2020 (10). The government also issued a notice to temporarily suspend or to postpone screening and health check-up services, including cancer screening, conducted in municipalities (11). A single-facility study reported that the number of inpatients and outpatients decreased during this first state of emergency (12). Kuzuu et al. reported that significantly fewer patients with stage I gastric and colorectal cancers were diagnosed in two hospitals in Kanagawa, during this period (13). In addition, the analysis of surgeries using the National Clinical Database reported that the number of most oncological (e.g. gastrectomy) and cardiovascular procedures (e.g. valve replacement + valve plasty) decreased in 2020 (14). These studies indicated that the effects of the COVID-19 pandemic might differ depending on cancer type.
In 2020, the number of people with COVID-19 in Japan varied monthly and between areas (10). As such, the number of people with COVID-19 was relatively high in large cities, such as Tokyo and Osaka, and tended to be low in rural areas. To address the needs of patients with cancer, especially when considering cancer treatment during future epidemics of emerging infectious diseases, we need to learn from the experience of COVID-19 in detail.
The purpose of this study was to clarify the impact of the COVID-19 pandemic on the diagnosis and detection of cancer in Japan by the type of cancer and prefecture, using the hospital-based cancer registries (HBCR), which register >70% of all new cancer cases in Japan.
Patients and methods
Data source
We used the national HBCR data from 735 hospitals, including all cancer care hospitals designated by the Ministry of Health, Labour and Welfare in Japan and other participating hospitals, which provided all data for cancer cases during 2016–2020. The HBCR database covers  72% of patients newly diagnosed with cancer in Japan (15). Trained cancer registrars in a hospital registered each cancer case in the HBCR based on standardized rules and criteria (16). The HBCR includes information on demographic characteristics (sex and date of birth) and tumour characteristics [topography, morphology and the eighth Union for International Cancer Control (UICC) tumour node metastasis (TNM) Classification of Malignant Tumours stage). The National Cancer Center has published an annual cancer registry report since 2007. In addition to the routine statistical report, the 2020 report provided a comparison of the monthly trend of cancer cases during the COVID-19 pandemic. This study is based on this specific section of the 2020 report (17).
72% of patients newly diagnosed with cancer in Japan (15). Trained cancer registrars in a hospital registered each cancer case in the HBCR based on standardized rules and criteria (16). The HBCR includes information on demographic characteristics (sex and date of birth) and tumour characteristics [topography, morphology and the eighth Union for International Cancer Control (UICC) tumour node metastasis (TNM) Classification of Malignant Tumours stage). The National Cancer Center has published an annual cancer registry report since 2007. In addition to the routine statistical report, the 2020 report provided a comparison of the monthly trend of cancer cases during the COVID-19 pandemic. This study is based on this specific section of the 2020 report (17).
Identification of cancer cases
In Japan, patients can choose and have free access to hospitals where they want to receive cancer treatment. In the HBCR database, the class of case (COC) shows how the hospital was involved in the cancer treatment of the patients. For example, if a patient is diagnosed with cancer at ‘Hospital A’ and starts the first course treatment at ‘Hospital B’, the COC at ‘Hospital A’ is registered as a ‘diagnosis only’. The HBCR does not collect identifiable information, such as names or unique numbers, of these patients. Thus, to avoid duplication, cases that started their first course of treatment in the registered hospitals were extracted from the HBCR database and the number of cases was compared by the month of diagnosis. To compare the number of cases by stage, epithelial cancers were selected because the UICC TNM classification does not apply to non-epithelial cancers, depending on the cancer site (17). From the cases diagnosed in 2018, the stage information was registered based on the eighth edition of the UICC TNM classification (18). Therefore, we used the data of cases diagnosed between 2018 and 2020 for the comparison of enrolment numbers by stage. Both the clinical and pathological UICC TNM classifications are registered in the HBCR. However, the pathological stage is not recorded for patients who receive chemotherapy or radiation therapy before undergoing surgical resection. In this analysis, we used a summary stage combining clinical and pathological stages; the pathological stage was used for patients who had this information available, whereas the clinical stage was used for those who lacked pathological stage information (19).
Data analysis
We defined the years 2016–2019 as the pre-COVID period, the most recent years before the COVID-19 pandemic, which would best predict the linear and seasonal patterns of cancer registries in 2020 in the absence of a pandemic. We compared the number of cases and monthly trends in 2020 with the average in the last 4 years by cancer site and route of detection (screening cases and non-screening cases). The non-screening cases included subjective symptoms and case which was detected by some tests during consultation with other disease. Data from cases diagnosed in 2018–2020 were used to compare the number of registered cases by summary stage. Using the detection process, we analysed five (stomach, lung, breast, colon/rectum and cervix uteri) cancers for which cancer screening is recommended by the Japanese government guidance. The number of registrations by stage was analysed for 18 common cancers (stomach cancer, colon cancer, hepatocellular carcinoma, intrahepatic cholangiocarcinoma, small cell lung cancer, non-small cell lung cancer, breast cancer, oesophageal cancer, pancreatic cancer, prostate cancer, cervical cancer, endometrial cancer, bladder cancer, laryngeal cancer, gallbladder cancer, kidney cancer, renal pelvis and ureter cancer and ovarian cancer) in Japan. In April 2020, the Ministry of Health, Labour and Welfare designated 13 prefectures (Tokyo, Osaka, Hokkaido, Ibaraki, Saitama, Chiba, Kanagawa, Ishikawa, Gifu, Aiti, Kyoto, Hyogo and Fukuoka) as requiring special precautions to prevent the spread of infection (area under special precautions) among 47 prefectures. In this study, we compared the case registrations and cancer trends for each of these 13 prefectures (special precaution area) and other prefectures. We also compared the number of registrations for all cancer between 2019 and 2020 by hospital type. All statistical analyses were performed using Stata software (ver. 16.0; Stata Corporation, Texas, USA).
Ethical considerations
This work was conducted as part of the official operation of the Center for Cancer Registries, National Cancer Center, according to the Operational Guidelines of HBCRs issued by the Ministry of Health, Labour and Welfare, based on the Cancer Registry Act. All data included in this study are publicly available on the Cancer Information Service website of the National Cancer Center (17) According to the research ethics guidelines in Japan, studies operated by the law are exempted from ethical reviews. Thus, the need for informed consent was waived.
Results
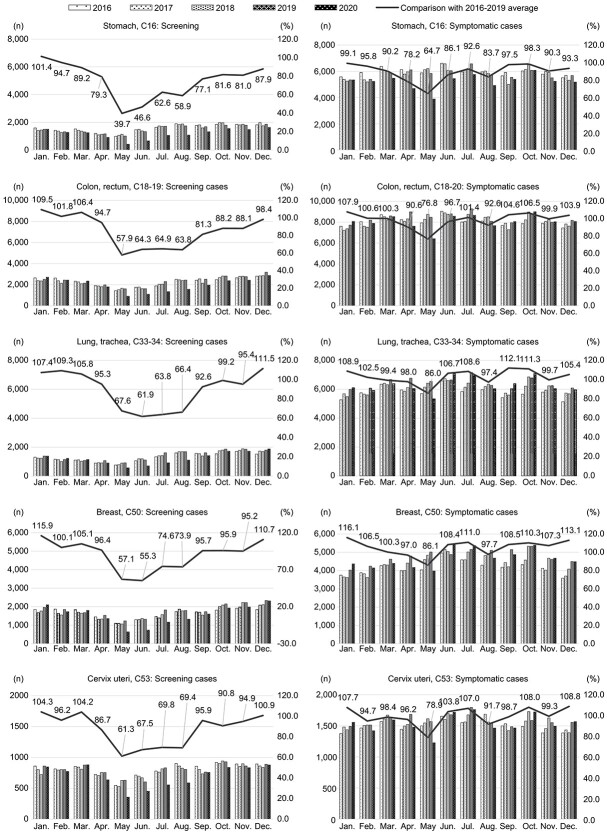
In total, 3 885 417 cases diagnosed between 2016 and 2020 were included in the analysis. Overall, 765 201 cancer patients initiated treatment in 735 hospitals in 2020, indicating a 5.8% decrease from 2019 and a 1.9% decrease compared with the average number during 2016–2019 (Table 1). The number of cases reported in 12 of 23 cancer sites (namely; cancers of the stomach, larynx, thyroid, liver, cervix uteri, colon/rectum, prostate, oesophagus, skin, multiple myeloma, gallbladder, and bone, joint and articular cartilage) declined in 2020, compared with the average in the last 4 years. At the same time, the number of leukaemia and pancreatic cancer cases increased in 2020. The sharp decline was observed in cancers of the stomach (13.8%), followed by cancers of the larynx (9.9%). Looking at the monthly trends, there was a sharp decline in case registrations in May 2020 (22.0% for all cancers) (Fig. 1). Upon analysing case registration by area of residence, the rate of decline was slightly high in 13 prefectures (specific caution area) in May 2020 compared with other areas; however, this difference was not observed in the subsequent months (Fig. 2). The expected decrease in the number of cancer cases was 8.2% if the situation in May would continue, although the observed decline for the entire year of 2020 was 2.2%.
Table 1.
The number of cases by cancer site
| The number of cases in 2020 | The number of cases during 2016–2019 (average) | Difference in cases in 2020 and in 2016–2019 | Proportionate difference | |
|---|---|---|---|---|
| All cancers | 765 201 | 780 054 | –14 853 | -1.9 |
| Stomach, C16 | 76 756 | 89 063 | −12 307 | -13.8 |
| Larynx, C32 | 4291 | 4762 | −471 | -9.9 |
| Thyroid, C73 | 10 050 | 10 654 | −604 | -5.7 |
| Liver, C22 | 22 208 | 23 428 | −1220 | -5.2 |
| Cervix uteri, C53 | 26 890 | 28 157 | −1267 | -4.5 |
| Colon, rectum, C18–20 | 120 453 | 125 807 | −5354 | -4.3 |
| Prostate, C61 | 55 178 | 57 230 | −2052 | -3.6 |
| Oesophagus, C15 | 22 556 | 23 280 | −724 | -3.1 |
| Skin, C43–44 | 23 798 | 24 451 | −653 | -2.7 |
| Multiple myeloma, C88–90 | 5221 | 5333 | −112 | -2.1 |
| Gallbladder, bible duct, C23–24 | 13 961 | 14 248 | −287 | -2.0 |
| Bones, joint and articular cartilage, C40–41 | 3073 | 3083 | −10 | -0.3 |
| Kidney and other urinary organs, C64–66, 68 | 22 855 | 22 847 | 8 | 0.0 |
| Ovary, C56 | 10 122 | 10 102 | 20 | 0.2 |
| Brain, nervous system, C70–72 | 17 789 | 17 701 | 88 | 0.5 |
| Lung, trachea, C33–34 | 90 096 | 89 538 | 558 | 0.6 |
| Bladder, C67 | 29 310 | 28 922 | 388 | 1.3 |
| Breast, C50 | 74 679 | 73 658 | 1021 | 1.4 |
| Oral cavity and pharynx, C00–14 | 20 406 | 19 760 | 646 | 3.3 |
| Malignant lymphoma, C81–85, C96 | 27 763 | 26 245 | 1518 | 5.8 |
| Corpus uteri, C54 | 15 109 | 14 174 | 935 | 6.6 |
| Pancreas, C25 | 29 312 | 27 143 | 2169 | 8.0 |
| Leukaemia, C91–95 | 11 411 | 9765 | 1646 | 16.9 |
Figure 1.
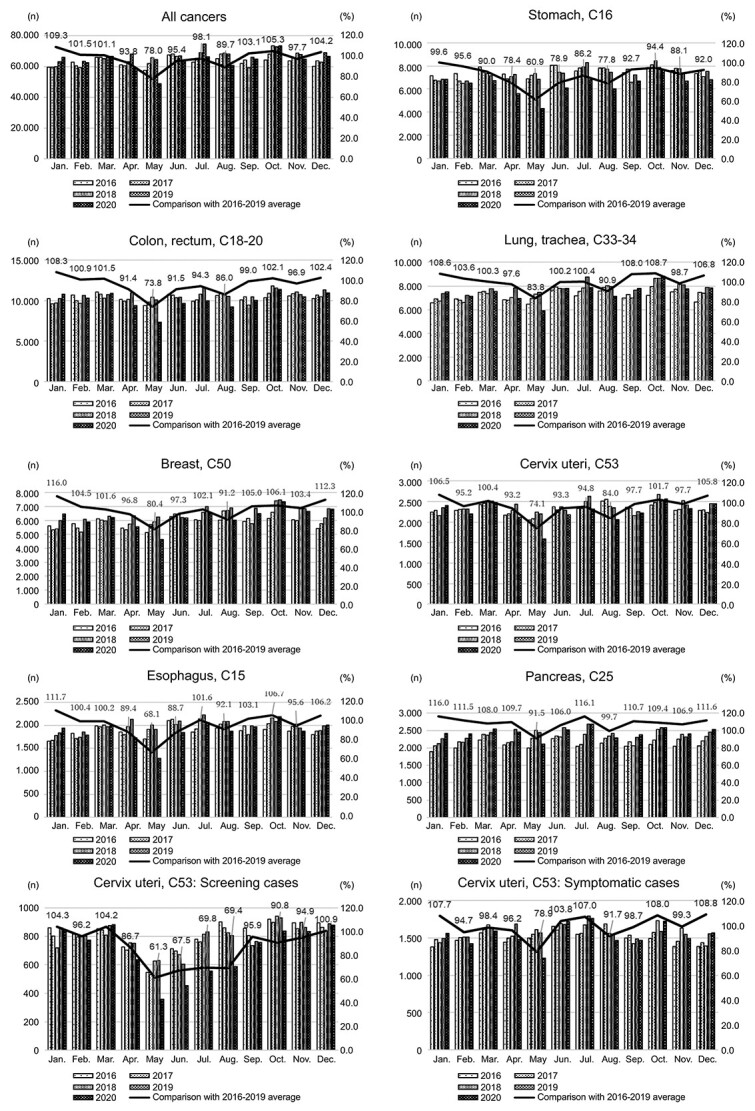
The number of cases diagnosed by the month of diagnosis (all cancer and major 7 cancer site)
Figure 2.
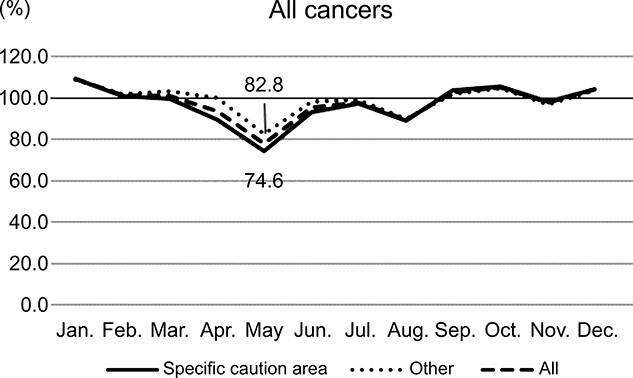
The number of cases diagnosed by the month of diagnosis (specific caution area). Specific caution area: 13 prefectures (Tokyo, Osaka, Hokkaido, Ibaraki, Saitama, Chiba, Kanagawa, Ishikawa, Gifu, Aiti, Kyoto, Hyogo and Fukuoka)
The number of cases detected by screening for the five cancer sites which the Japanese government recommended in 2020 ranged from 8.1 to 24.3%, lower than the average number in the past 4 years (Table 2). Analysis by cancer site indicated that the decrease was by 24.3% for cancers of the stomach in 2020, compared with the average value in the past 4 years. Compared with the monthly average during 2016–2019, the number of cases detected by screening decreased significantly between May and August, during which the first and second wave of COVID-19 pandemic occurred in Japan, and then gradually recovered towards December (Fig. 3). The number of cancer cases detected via non-screening cases including subjective symptoms and case which was detected by some tests during consultation with other disease also declined in May and August. The number of case registrations for the entire year (2020) was almost the same as the average number in the last 4 years, with an exception only in the case of stomach cancers (a decrease of 11.0%). Among the five cancer sites, the highest percentage of cases with unknown route of detection was cervix cancer (1.3% in 2020); the percentage of an unknown case in all other sites was < 1.0%.
Table 2.
The number of cases by the process of detection
| The number of cases in 2020 | The number of cases during 2016–2019 (average) | Difference in cases in 2020 and 2016–2019 | Proportionate difference | |
|---|---|---|---|---|
| All cancers | ||||
| Screening cases | 113 442 | 129 010 | −15 568 | -12.1 |
| Symptomatic cases | 651 759 | 651 044 | 715 | 0.1 |
| Stomach, C16 | ||||
| Screening cases | 14 152 | 18 690 | −4538 | -24.3 |
| Symptomatic cases | 62 604 | 70 373 | −7769 | -11.0 |
| Colon, rectum, C18–20 | ||||
| Screening cases | 23 839 | 27 536 | −3697 | -13.4 |
| Symptomatic cases | 96 614 | 98 271 | −1657 | -1.7 |
| Lung, trachea, C33–34 | ||||
| Screening cases | 14 704 | 16 291 | −1587 | -9.7 |
| Symptomatic cases | 75 392 | 73 247 | 2145 | 2.9 |
| Breast, C50 | ||||
| Screening cases | 18 715 | 20 359 | −1644 | -8.1 |
| Symptomatic cases | 55 964 | 53 300 | 2664 | 5.0 |
| Cervix uteri, C53 | ||||
| Screening cases | 8401 | 9558 | −1157 | -12.1 |
| Symptomatic cases | 18 489 | 18 599 | −110 | -0.6 |
Figure 3.
The number of cases registered monthly owing to cancer screening or others
For the five (gastric, colorectal, non-small cell lung cancer, oesophageal and laryngeal) cancer types, the number of registrations in 2020 was lower than the average number during 2018–2019 in all stages, I–IV (Table 3). The number of case registrations for stage I and II gastric cancer, stage II intrahepatic cholangiocarcinoma, stage II oesophageal cancer, stage 0 and I laryngeal cancer and stage II gallbladder cancer decreased by >10%, compared with that in the past 2 years (2018 and 2019). The number of case registrations for stage I pancreatic cancer (26.5%), stage 0 gallbladder cancer (15.1%) and stage IV bladder cancer (13.7%) increased by >10%, compared with that in the previous 2 years. Among the 18 cancers, the highest percentage of cases with unknown stage was renal pelvis and ureter cancer (5.0% in 2020); the percentage cases with unknown stage in all other cancers were <4.0%.
Table 3.
The number of cases by summary stage
| The number of cases in 2020 | The number of cases during 2018–2019 (average) | Difference in the cases | Proportionate difference | |
|---|---|---|---|---|
| Stomach cancer | ||||
| Stage I | 45 356 | 53 570 | −8214 | -15.3 |
| Stage II | 6061 | 7040 | −979 | -13.9 |
| Stage III | 7176 | 7907 | −731 | -9.2 |
| Stage IV | 13 753 | 14 606 | −853 | -5.8 |
| Colon cancer | ||||
| Stage 0 | 31 105 | 34 108 | −3003 | -8.8 |
| Stage I | 22 611 | 24 037 | −1426 | -5.9 |
| Stage II | 22 251 | 23 328 | −1077 | -4.6 |
| Stage III | 22 009 | 22 972 | −963 | -4.2 |
| Stage IV | 17 753 | 17 826 | −73 | -0.4 |
| Hepatocellular carcinoma | ||||
| Stage I | 8813 | 9263 | −450 | -4.9 |
| Stage II | 4511 | 4965 | −454 | -9.1 |
| Stage III | 2814 | 3028 | −214 | -7.1 |
| Stage IV | 1680 | 1657 | 23 | 1.4 |
| Intrahepatic cholangiocarcinoma | ||||
| Stage I | 562 | 594 | −32 | -5.4 |
| Stage II | 699 | 786 | −87 | -11.1 |
| Stage III | 735 | 707 | 28 | 4.0 |
| Stage IV | 1453 | 1380 | 73 | 5.3 |
| Small cell lung cancer | ||||
| Stage I | 600 | 582 | 18 | 3.1 |
| Stage II | 521 | 553 | −32 | -5.8 |
| Stage III | 2012 | 2124 | −112 | -5.3 |
| Stage IV | 4445 | 4633 | −188 | -4.1 |
| Non-small cell lung cancer | ||||
| Stage 0 | 3087 | 3357 | −270 | -8.0 |
| Stage I | 32 488 | 32 929 | −441 | -1.3 |
| Stage II | 6668 | 7122 | −454 | -6.4 |
| Stage III | 12 914 | 13 297 | −383 | -2.9 |
| Stage IV | 24 497 | 24 679 | −182 | -0.7 |
| Breast cancer | ||||
| Stage 0 | 9834 | 10 222 | −388 | -3.8 |
| Stage I | 30 332 | 31 532 | −1200 | -3.8 |
| Stage II | 22 165 | 22 737 | −572 | -2.5 |
| Stage III | 7516 | 7519 | −3 | 0.0 |
| Stage IV | 4295 | 4065 | 230 | 5.7 |
| Oesophageal cancer | ||||
| Stage 0 | 2615 | 2860 | −245 | -8.6 |
| Stage I | 8460 | 9105 | −645 | -7.1 |
| Stage II | 2334 | 2597 | −263 | -10.1 |
| Stage III | 3196 | 3226 | −30 | -0.9 |
| Stage IV | 4897 | 4999 | −102 | -2.0 |
| Pancreatic cancer | ||||
| Stage 0 | 742 | 722 | 20 | 2.8 |
| Stage I | 6044 | 4777 | 1267 | 26.5 |
| Stage II | 4093 | 4361 | −268 | -6.1 |
| Stage III | 1822 | 1704 | 118 | 6.9 |
| Stage IV | 12 350 | 12 314 | 36 | 0.3 |
| Prostate cancer | ||||
| Stage I | 19 031 | 21 128 | −2097 | -9.9 |
| Stage II | 15 991 | 16 982 | −991 | -5.8 |
| Stage III | 9233 | 9804 | −571 | -5.8 |
| Stage IV | 10 162 | 10 111 | 51 | 0.5 |
| Cervical cancer | ||||
| Stage 0 | 18 175 | 19 414 | −1239 | -6.4 |
| Stage I | 3552 | 3867 | −315 | -8.1 |
| Stage II | 1397 | 1466 | −69 | -4.7 |
| Stage III | 2338 | 2379 | −41 | -1.7 |
| Stage IV | 1289 | 1266 | 23 | 1.8 |
| Endometrial cancer | ||||
| Stage I | 10 312 | 9999 | 313 | 3.1 |
| Stage II | 827 | 777 | 50 | 6.4 |
| Stage III | 1863 | 1864 | −1 | -0.1 |
| Stage IV | 1333 | 1295 | 38 | 2.9 |
| Bladder cancer | ||||
| Stage 0 | 14 464 | 14 760 | −296 | -2.0 |
| Stage I | 7378 | 7399 | −21 | -0.3 |
| Stage II | 3350 | 3148 | 202 | 6.4 |
| Stage III | 2353 | 2249 | 104 | 4.6 |
| Stage IV | 1044 | 918 | 126 | 13.7 |
| Laryngeal cancer | ||||
| Stage 0 | 285 | 346 | −61 | -17.6 |
| Stage I | 1620 | 1908 | −288 | -15.1 |
| Stage II | 906 | 971 | −65 | -6.7 |
| Stage III | 645 | 674 | −29 | -4.3 |
| Stage IV | 810 | 839 | −29 | -3.5 |
| Gallbladder cancer | ||||
| Stage 0 | 298 | 259 | 39 | 15.1 |
| Stage I | 481 | 537 | −56 | -10.4 |
| Stage II | 754 | 835 | −81 | -9.7 |
| Stage III | 968 | 1034 | −66 | -6.4 |
| Stage IV | 2201 | 2311 | −110 | -4.8 |
| Kidney cancer | ||||
| Stage I | 10 465 | 10 813 | −348 | -3.2 |
| Stage II | 660 | 638 | 22 | 3.4 |
| Stage III | 1770 | 1814 | −44 | -2.4 |
| Stage IV | 1872 | 1739 | 133 | 7.6 |
| Renal pelvis and ureter cancer | ||||
| Stage 0 | 1507 | 1395 | 112 | 8.0 |
| Stage I | 1153 | 1099 | 54 | 4.9 |
| Stage II | 892 | 884 | 8 | 0.9 |
| Stage III | 1682 | 1662 | 20 | 1.2 |
| Stage IV | 2056 | 2066 | −10 | -0.5 |
| Ovarian cancer | ||||
| Stage I | 5597 | 5653 | −56 | -1.0 |
| Stage II | 789 | 837 | −48 | -5.7 |
| Stage III | 2986 | 2960 | 26 | 0.9 |
| Stage IV | 1849 | 1781 | 68 | 3.8 |
The percentage change in registrations in 2020 compared with 2019 varied by hospital type. The number of registrations in the designated cancer care hospitals by the Ministry of Health, Labour and Welfare decreased by an average of 5.3% in 2020 compared with 2019. In contrast, other cancer hospitals showed an average decrease of 4.0% in the hospitals designated by the prefectures and 4.7% in other hospitals.
Discussion
This analysis of nationwide registry-based data was conducted to compare previous cancer registrations to assess the impact of the COVID-19 epidemic on cancer care in Japan in the year 2020. Consistent with the findings of previous reports from other countries, including the United Kingdom and New Zealand (7–9,20–22), this study illustrated that the number of cancer cases decreased significantly during the first wave of COVID-19, and this decrease was observed regardless of prefectures (specific caution area). Screening for cancer cases along with the number of non-screening cases including consultations due to subjective symptoms decreased during the first wave of the pandemic. It is likely that some patients refrained from availing health services. In the early stages of the COVID-19 pandemic, many aspects such as effective prevention and risk factors and treatment methods were unclear. We did not know whether to postpone health services. Now that effective vaccines and treatment are available, we should encourage people to seek care when necessary, such as cancer screening and treatment at the right time.
In the first wave of the COVID-19 pandemic, early detection was substantially affected. When many countries worldwide implemented a lock-down policy, Japan declared the first state of emergency in April and May and asked people to stay home. Furthermore, the Ministry of Health, Labour and Welfare issued a statement to temporarily suspend or to postpone cancer screening (11). The Japan Gastroenterological Endoscopy Society recommended that non-urgent gastrointestinal endoscopy, such as those for screening purposes and for mild symptoms, should be postponed (23). Compliance to these recommendations may explain the sharp drop that we observed in the number of stomach cancer cases diagnosed in May, and the number of cases for the year 2020 was lower than usual. As the majority of gastric cancer cases in Japan are diagnosed in early stages (62% are stage I in 2019) (24), the influence of these national movements was large. A similar effect was observed for other cancer types, for which screening is recommended. In contrast, the number of some cancer cases including leukaemia, pancreas, corpus uteri increased. This can be influenced by changes in the cancer registration system in Japan. Since the Cancer Registration Act came into effect in 2016, the registration targets of the HBCR were more clarified and the registration rules were reviewed. From 2016 to 2019, the number of registrations to the HBCR trended slightly upward. This will be considered to be due to more accurate registration rather than a true increase in the number of cancer patients. In addition, the number of pancreatic cases did not decrease, as suggested in a previous study (14). Pancreatic cancer is asymptomatic in the early stages. Therefore, in many cases, cancer progresses before it is detected. According to the Japanese HBCR cancer statistics in 2019,  40% of pancreatic cancer cases were detected at stage IV (24).
40% of pancreatic cancer cases were detected at stage IV (24).
A previous study conducted in Kanagawa in 2020 reported the possibility of fewer cases detected for gastrointestinal cancer and that colorectal cancer may be diagnosed only at a more advanced stage (13). The results of our study showed that the number of cases was lower than usual at all stages, although the proportion of decrease in stage 0 to I cancer cases was large. Using a nationwide database, colorectal cancer was not found to be diagnosed at a more advanced stage. Future studies need to investigate the effects of delayed cancer detection at a relatively early stage.
Our study has some limitations. First, the HBCR data mainly covered relatively large hospitals, such as designated cancer care hospitals. Although the data cover >70% of new cases in Japan, we could not determine whether patients visited other hospitals that treat the remaining 30% of the cases. In 2020, > 90% of the designated cancer care hospitals were treating patients with COVID-19 infections. (25) There is a possibility that the decrease in the number of cases we observed in our data may be due to the patients moving to other hospitals. Future studies using population-based cancer registry may shed light on the comprehensive dynamics during the pandemic. Second, although the number of cases has decreased, especially for relatively early-stage cancers, the effect on survival or mortality due to decreased screening remains unknown. Simulation studies have also indicated that advanced cancer and cancer-related deaths would increase after the COVID-19 pandemic (2,4,6), although these results need confirmation by real data in later years. Third, this study is based on the published report of the nationwide HBCRs. Therefore, additional analysis such as standardization of age distribution and statistical test was not included. These analyses should be performed after official permission for the secondary data analysis. Fourth, some people have some symptoms but still receive a cancer screening. Therefore, it is possible that some of the cases detected during screening may include those with symptoms. Finally, this report only covers the first year of the pandemic in Japan. Although the government declared a state of emergency and social activities were substantially reduced from April to May, the reduction was mainly voluntary. Our findings have limited generalizability to the different future situations in Japan with respect to the pandemic and cancer burden. The trends in cancer diagnosis may differ greatly in 2021 and beyond. We need to continuously monitor trends in cancer screening, diagnosis and treatment as well as outcomes, and to perhaps prepare guidelines for unforeseen conditions that can affect cancer management.
Conclusion
This study showed that the number of reported cancer cases decreased significantly during the first COVID-19 pandemic, regardless of cancer type, detection process, stage and prefecture. In the early stages of the pandemic, the epidemiology of COVID-19 was unclear. In addition to changes in the level of cancer screening, it is likely that patients did not seek health care at hospitals even if they had subjective symptoms and that hospitals were unable to handle the patient load. It is important that hospitals implement appropriate measures to control infections. Policies are required to increase awareness about infection prevention and the significance of early screening and addressing symptoms for better management and survival.
Funding
This study was supported by the Cancer Research and Development Fund of the National Cancer Centre, Japan (2020–A–20).
Conflict of interest
All authors were employed by the National Cancer Center, Japan and in charge of operating hospital-based cancer registry.
Acknowledgements
We thank the tumour registrars in the hospitals for their great work in registering data that enabled our analysis. We also thank Kondo S for his work in collecting HBCR data from the hospitals.
Contributor Information
Ayako Okuyama, Center for Cancer Registries, National Cancer Center Institute for Cancer Control, Tokyo, Japan.
Mari Watabe, Center for Cancer Registries, National Cancer Center Institute for Cancer Control, Tokyo, Japan.
Riko Makoshi, Center for Cancer Registries, National Cancer Center Institute for Cancer Control, Tokyo, Japan.
Hirokazu Takahashi, Division of Screening Assessment and Management, National Cancer Center Institute for Cancer Control, Tokyo, Japan.
Yoichiro Tsukada, Center for Cancer Registries, National Cancer Center Institute for Cancer Control, Tokyo, Japan.
Takahiro Higashi, Center for Cancer Registries, National Cancer Center Institute for Cancer Control, Tokyo, Japan.
References
- 1. World Health Organization . COVID-19 public health emergency of international concern (PHEIC). Global research and innovation forum: towards a research map. 2020. https://covid19-evidence.paho.org/handle/20.500.12663/714. 17 February 2022, date last accessed.
- 2. Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population–based, modelling study. Lancet Oncol 2020;21:1023–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lai AG, Pasea L, Banerjee A, et al. Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: near real-time data on cancer care, cancer deaths and a population–based cohort study. BMJ Open 2020;10:e043828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol 2020;21:1035–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sud A, Jones ME, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol 2020;31:1065–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Jonge L, Worthington J, van Wifferen F, et al. Impact of the COVID-19 pandemic on faecal immunochemical test-based colorectal cancer screening programmes in Australia, Canada, and the Netherlands: a comparative modelling study. Lancet Gastroenterol Hepatol 2021;6:304–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Morris EJA, Goldacre R, Spata E, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population–based study. Lancet Gastroenterol Hepatol 2021;6:199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gurney JK, Millar E, Dunn A, et al. The impact of the COVID-19 pandemic on cancer diagnosis and service access in New Zealand-a country pursuing COVID-19 elimination. Lancet Reg Health West Pac 2021;10:100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ranganathan P, Sengar M, Chinnaswamy G, et al. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol 2021;22:970–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ministry of Health, Labour, and Welfare, Japan . The COVID-19. (in Japanese). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000164708_00001.html 17 February 2022, date last accessed.
- 11. Ministry of Health, Labour, and Welfare, Japan . About measures related to implementation of health promotion business based on the stage of emergency related to COVID-19. 2020. (in Japanese). https://www.mhlw.go.jp/content/000621941.pdf. 17 February 2022, date last accessed.
- 12. Sato Y, Fujiwara Y, Fukuda N, et al. Changes in treatment behavior during the COVID-19 pandemic among patients at a cancer hospital. Cancer Cell 2021;39:130–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kuzuu K, Misawa N, Ashikari K, et al. Gastrointestinal cancer stage at diagnosis before and during the COVID-19 pandemic in Japan. JAMA Netw Open 2021;4:e2126334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ikeda N, Yamamoto H, Taketomi A, et al. The impact of COVID-19 on surgical procedures in Japan: analysis of data from the National Clinical Database. Surg Today 2022;52:22–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Okuyama A, Tsukada Y, Higashi T. Coverage of the hospital–based cancer registries and the designated cancer care hospitals in Japan. Jpn J Clin Oncol 2021;51:992–8. [DOI] [PubMed] [Google Scholar]
- 16. National Cancer Center, Japan . The standardised roles for hospital–based cancer registries. (in Japanese). https://ganjoho.jp/med_pro/cancer_control/can_reg/hospital/regulation.html 17 February 2022, date last accessed.
- 17. Higashi T, Okuyama A ed. Report of the Hospital-Based Cancer Registries, 2020. 2021. (in Japanese). https://ganjoho.jp/public/qa_links/report/hosp_c/hosp_c_registry.html 17 February 2022, date last accessed.
- 18. Brierley JD, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours Stage, 8th edn. United States: Wiley-Blackwell, 2016. [Google Scholar]
- 19. Okuyama A, Higashi T. Patterns of cancer treatment in different age groups in Japan: an analysis of hospital–based cancer registry data, 2012-2015. Jpn J Clin Oncol 2018;48:417–25. [DOI] [PubMed] [Google Scholar]
- 20. Xiao H, Dai X, Wagenaar BH, et al. The impact of the COVID-19 pandemic on health services utilization in China: time-series analyses for 2016-2020. Lancet Reg Health West Pac 2021;9:100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dinmohamed AG, Cellamare M, Visser O, et al. The impact of the temporary suspension of national cancer screening programmes due to the COVID-19 epidemic on the diagnosis of breast and colorectal cancer in the Netherlands. J Hematol Oncol 2020;13:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol 2020;21:750–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Irisawa A, Furuta T, Matsumoto T, et al. Gastrointestinal endoscopy in the era of the acute pandemic of coronavirus disease 2019: recommendations by Japan gastroenterological endoscopy society (issued on April 9th, 2020). Dig Endosc 2020;32:648–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Higashi T, Okuyama A ed. Report of the hospital-based cancer registries, 2019. 2021. (in Japanese). https://ganjoho.jp/public/qa_links/report/hosp_c/pdf/2019_report.pdf 17 February 2022, date last accessed. [DOI] [PubMed]
- 25. Okuyama A, Toyama Y ed. Report of the hospital-based Cancer registries fact-finding survey. (in Japanese). https://www.ncc.go.jp/jp/icc/ccr/project/010/jittai_report.pdf 6 May 2022, date last accessed.