Abstract
Background:
Adolescent electronic cigarette use (e-cigarette) is a public health concern and factors associated with vaping remain to be understood. Childhood emotional abuse/neglect is a risk factor for e-cigarettes. Yet, pathways by which trauma impacts use remain unclear. Alexithymia (i.e., difficulties identifying and describing feelings) is one possible link. Indeed, emotional abuse/neglect leads to difficulties identifying and verbalizing emotions. This impairment may lead to distress and promote e-cigarette use as a coping strategy.
Methods:
Using parallel mediation, this study examined the degree to which alexithymia, assessed using the Toronto Alexithymia Scale, mediates the link between emotional abuse/neglect, assessed using the Child and Adolescent Trauma Screen, and e-cigarette use. The sample (n=166) consisted of adolescents from a larger multi-wave study.
Results:
Emotional abuse/neglect predicted difficulty describing feelings (effect = 0.23, p = 0.001), which in turn predicted e-cigarette use (effect = 0.30, p = 0.004). Moreover, difficulty describing feelings mediated the link between emotional abuse/neglect and e-cigarette use (sum of indirect 95% CI [1.68, 16.48]). Difficulty identifying feelings was not a significant mediator and the externally-oriented thinking subscale was excluded due to low reliability.
Conclusions:
As e-cigarettes are often used in social contexts, teens who experience difficulty describing feelings may vape as a means of connecting emotionally with others. Moreover, nicotine, found in most e-cigarettes, releases dopamine and noradrenaline in the brain modulating action, learning, and memory processes; plausibly, improving verbalization of emotions. Programming which identifies nuances in alexithymia among adolescents with emotional abuse/neglect could mitigate e-cigarette use or delay initiation.
Keywords: adolescence, alexithymia, emotional abuse, emotional neglect, e-cigarette use, childhood trauma
1. Introduction
Adolescent electronic cigarette (e-cigarette) use remains a public health concern. Indeed, in 2020, 37% of US high school students reported lifetime e-cigarette use and 21% reported past month use (Johnston et al., 2021). Given the growing popularity of e-cigarettes among adolescents, youth vaping has been declared an epidemic (U.S. Food and Drug Administration, 2018). Yet, factors influencing its use remain unclear. Although little is understood regarding the long-term negative health consequences of youth vaping, e-cigarette use has been associated with respiratory problems and heart attacks (Shin et al., 2019). Moreover, Leventhal et al. (2015) found that 30% of adolescent e-cigarette users are likely to transition to combustible cigarettes within 6 months of e-cigarette use, compared to 8% of non-users. This is particularly alarming as nicotine, which is found in most e-cigarette products, is addictive and can harm the developing brain’s structure and function (Shin et al., 2019; Sutherland et al., 2016). As such, examining risk factors that lead to youth e-cigarette use is critical to help address this epidemic by reducing rates of use and informing prevention programming. Prior work has linked substance use (SU), such as nicotine, to childhood trauma and alexithymia (Cruise and Becerra, 2018; De Rick et al., 2009; Evren et al., 2009; Kristman-Valente et al., 2013a; Lewis et al., 2011); these factors may also be associated with the use of e-cigarettes.
A link between childhood trauma and nicotine has been demonstrated in the literature. Prior studies have demonstrated that childhood trauma, such as maltreatment and neglect, can predict cigarette smoking later in adolescence (Kristman-Valente et al., 2013b; Lewis et al., 2011; Yoon et al., 2020). A recent study conducted by Yoon and colleagues (2020) found that adolescents who experienced childhood neglect were more likely to initiate cigarette use and were more prone to gradually increase use over time, compared to those who had not experienced childhood neglect. Though the relation between childhood trauma and e-cigarette use has not been extensively examined, some studies have found a link among young adults (Melka, A. et al., 2019; Shin et al., 2019). For example, in a sample of adults 18–21 years old, childhood emotional abuse/neglect was significantly associated with lifetime e-cigarette use (Shin et al., 2019). Indeed, emotional abuse/neglect can significantly harm a child’s behavioral, psychological, and emotional development which could increase risk of behavioral difficulties in adolescence (Glaser, 2002).
Individuals who have experienced childhood trauma, such as emotional abuse/neglect, may use e-cigarettes, to alleviate negative affect associated with their experienced trauma (Ayres, 2020). Some preliminary research indicates that one of the common reasons teens start using e-cigarettes is to cope with negative affect such as stress and anxiety (Kong et al., 2019). The self-medication hypothesis posits that some individuals may turn to substances as a way to cope with their symptomatology (Khantzian, 1985). More specifically, e-cigarette users and non-users alike perceive that e-cigarette use can help “calm someone down” (Fadus et al., 2019; Gibson et al., 2018; Heinz et al., 2010). In fact, prior work has suggested that adolescents may be more susceptible to the anxiolytic effects of nicotine compared to adults (Kupferschmidt et al., 2010). Even though childhood trauma has been linked to nicotine, past research has indicated that trauma does not predict SU per se. That is, Ayres (2020) demonstrated that subsequent deficits (such as in emotional coping) due to childhood trauma predicted whether drug use would escalate to problematic use. Hence, it is important to elucidate the possible mechanisms that link childhood trauma to e-cigarette use among adolescents in order to prevent its use. One factor that might explain this association could be alexithymia given its associations with emotional abuse/neglect and SU (Evren et al., 2009; Zdankiewicz-Ścigała and Ścigała, 2020).
Alexithymia, a term originally proposed by Sifneos (1973) to describe the impairment of finding appropriate words for emotions, is characterized by difficulties describing and identifying one’s feelings (de Bruin et al., 2019; Kopera et al., 2015). Prior work has found an association between childhood emotional abuse/neglect and alexithymia among adults with a SU disorder (Evren et al., 2009; Zdankiewicz-Ścigała and Ścigała, 2020). Indeed, individuals who experience trauma are more likely to exhibit difficulty identifying emotions (Zdankiewicz-Ścigała and Ścigała, 2020). Moreover, childhood adversity, such as neglect, has been associated with emotional self-regulation problems later in life (Pollak, 2008). This affects the ability of individuals to understand their emotional states. Conversely, awareness of emotional states may serve as a precondition for efficient self-regulation of behavior (Jakubczyk et al., 2020). When individuals are unable to differentiate emotional states, it can cause distress since they cannot employ strategies to regulate their emotions. This may ultimately lead to smoking cigarettes as a way to cope with stressors (Kopera et al., 2020). Prior work has demonstrated a link between difficulty recognizing and describing emotions, two dimensions of alexithymia, and cigarette smoking among adults (Ünübol and Hızlı Sayar, 2019). More specifically, a link between alexithymia and nicotine has been found among pregnant smokers, such that smoking cigarettes may serve as a coping strategy to manage the negative effects associated with alexithymia (Linn et al., 2020). Despite the available data linking alexithymia and combustible cigarettes, to our knowledge, the role of alexithymia as a mediator between emotional abuse/neglect and e-cigarettes remains understudied.
Data regarding alexithymia’s role in adolescent SU is scarce. Likewise, the association between childhood trauma, alexithymia, and e-cigarette use remains to be empirically tested. Given the alarmingly high rate of e-cigarette use among adolescents (Johnston et al., 2021), it is important to identify whether adolescents who have experienced emotional abuse/neglect are at heightened risk of using e-cigarettes compared to those who have not experienced emotional abuse/neglect. Furthermore, it is critical to understand factors that contribute to the association between emotional abuse/neglect and e-cigarette use. Therefore, this study examined whether the link between emotional abuse/neglect and e-cigarette use can be explained in part by various facets of alexithymia. We focused on emotional abuse/neglect because this type of maltreatment has been shown to be the most detrimental long-term (Strathearn et al., 2020) and highly associated with alexithymia (Brown et al., 2018). The current study hypothesized that two facets of alexithymia (i.e., difficulty identifying feelings and difficulty describing feelings) would mediate the association between emotional abuse/neglect and e-cigarette use among adolescents. To our knowledge, prior work has not examined such associations. Identifying factors that contribute to the use of e-cigarettes among adolescents may help inform prevention programming by targeting teens at greater risk for e-cigarette use.
2. Methods
2.1. Participants
We assessed data from a subsample of adolescents (n=166; 48.80% female, 88.55% White, Mage=14.90) who completed the first wave (W1) of a larger ongoing multi-wave longitudinal study examining risk and protective factors impacting e-cigarette use. A subsample was used in the present study because not all adolescents participated in the magnetic resonance imaging scan at Wave 1-Visit 2 and the Toronto Alexithymia Scale was only collected during Wave 1-Visit 2. The sample was predominantly from a Hispanic/Latinx ethnic background (84.94%) due to the region of the country where the study was conducted and the aims of the larger study. The current subsample did not differ from the larger study sample (N = 264) on demographic characteristics, emotional abuse/neglect, or e-cigarette use. Freshmen and sophomores enrolled in South Florida high schools, as well as their caregivers completed W1 and wave 2 (W2; ~15 months apart). Data were collected from March 2018 through December 2019 for W1, and from June 2019 to June 2021 for W2. Exclusion criteria consisted of adolescents with intellectual or physical disabilities, neurological diseases, a learning disorder, severe mental illness, and not being fluent in English. In addition, in order to be able to differentiate risk and protective factors related to e-cigarette use onset, the larger multi-wave study required a considerable number of participants to initiate some type of SU. Hence, adolescents needed to meet criteria for either endorsement of a sibling or friend having tried a substance or high levels of personality factors linked with SU (i.e., impulsivity, sensation seeking). It is worth noting that only 2.6% (11) of adolescents that were screened did not meet the high-risk criterion (i.e., most high school students in this region screen at high risk). Accordingly, the study sample is likely representative of typical high school students in the region.
2.2. Procedures
Public schools in South Florida were contacted regarding their willingness to participate in recruitment events. Interested adolescents and their caregivers completed an eligibility screen, and those meeting criteria were scheduled for W1 data collection. W1 data collection involved two in-person visits for this subsample of participants. During the first visit, adolescents and caregivers each completed a set of questionnaires for approximately 1.5 hours and 45 minutes, respectively. After completing the informed consent and assent process, adolescents and caregivers completed questionnaires in separate rooms to ensure confidentiality. During the second visit (scheduled within a month after the first visit), adolescents completed a second set of questionnaires (~15 minutes) and completed a magnetic resonance imaging (MRI) scan given the scope of the larger study (MRI data not discussed further herein). W2 assessments were conducted approximately 15 months after W1 with similar procedures; however, due to COVID-19 safety restrictions, a portion of the participants completed their questionnaires remotely. All questionnaires were administrated via REDCap (Research Electronic Data Capture; (Harris et al., 2019; Harris et al., 2009) on an iPad during in-person visits and on personal tablets or computers during remote visits. Participants were compensated for their participation. The Institutional Review Board at the university approved study procedures.
2.3. Measures
Child and Adolescent Trauma Screen (CATS).
The sum of four items (e.g., “Having a parent or other adult swear at you, insult you, put you down, or humiliate you often or very often?”) from the CATS (Sachser et al., 2017) administered at W1 was used to assess emotional abuse/neglect. Items were rated as 0 = not endorsing emotional abuse/neglect, 1 = endorsing yes to 1 or more items.
Toronto Alexithymia Scale (TAS).
During the second visit of W1, participants completed the TAS (Bagby et al., 1994) to assess levels of alexithymia. The TAS is comprised of three subscales. However, given the stronger association between Difficulty Describing Feelings (e.g. “It is difficult for me to find the right words for my feelings”; Cronbach’s α = 0.79) and Difficulty Identifying Feelings (e.g. “When I am upset, I don’t know if I am sad, frightened, or angry”; Cronbach’s α = 0.81) with trauma and SU (Cruise and Becerra, 2018; Ünübol and Hızlı Sayar, 2019) compared to the TAS’ third subscale (Externally-Oriented Thinking) and the poor reliability of the measure (Cronbach’s α = 0.32), only the first two subscales were examined. This is consistent with prior studies demonstrating low reliability of the Externally-Oriented Thinking subscale (Loas et al., 2017). According to Loas et al. (2017), it appears that the reliability of this subscale decreases with age. Moreover prior work indicated that Externally-Oriented Thinking is not strongly associated with trauma (Guzzo et al., 2014). Items on the TAS were rated on a 5-point Likert scale (1= Strongly disagree, 5= Strongly agree) and responses were summed to produce a subscale score, with higher scores reflecting greater difficulties.
Adolescent e-cigarette use.
E-cigarette use was assessed at W2 using one item adapted from the Population Assessment of Tobacco and Health Survey (PATH; (Hyland et al., 2016). Participants were asked “Since your last visit, on how many days did you use an Electronic Nicotine Delivery System (ENDS) product?” and were provided with detailed instructions and pictures of ENDS products in order to capture the wide variety of available ENDS products. Number of days were entered in a textbox.
Covariates.
The following demographic variables were included as covariates: adolescent’s biological sex, age, and ethnicity. Moreover, as poly-victimization is commonly found in childhood trauma (Finkelhor et al., 2007), we controlled for physical and sexual abuse at W1. Prior lifetime e-cigarette use at W1 was also included as a control variable. Participants answered a dichotomous question asking, “Have you ever used an ENDS product, such as NJOY, Blu, Smoking Everywhere, a vape pen, or a vape mod, even one or two times?”
2.4. Data Analytic Plan
Structural equation modeling was used to estimate parallel mediation in Mplus 7.2 (Muthén and Muthén, 1998–2012). Specifically, a parallel mediator path model was estimated to examine how difficulty identifying and describing feelings mediated the impact of emotional abuse/neglect on e-cigarette use.1 Indirect effects were assessed using 95% bias-corrected bootstrap confidence intervals (CIs) based on 10,000 bootstrapped samples. Bias-corrected bootstrapping is considered a rigorous method for estimating mediated effects (Preacher and Hayes, 2008; Valente et al., 2016).
3. Results
Table 1 provides descriptive statistics and correlations for study variables. All study variables were normally distributed (skewness range = 0.18, 0.79, kurtosis range = −1.51,−0.12) apart from e-cigarette use at W2 (skewness = 5.37, kurtosis = 31.95). Given that the outcome was not normally distributed, the test of joint significance using a maximum likelihood estimator with robust standard errors (MLR) was also calculated as a comparison to the bias-corrected bootstrapping results. Of note, 33.3% of adolescents reported lifetime ENDS use at W1, 24.0% reported subsequent ENDS use between their W1 and W2 assessments, and 36.8% reported having experienced emotional abuse/neglect. Emotional abuse/neglect was positively correlated with physical and sexual abuse, difficulty identifying and describing feelings. Emotional abuse/neglect was not correlated with lifetime or subsequent e-cigarette use. Moreover, W2 e-cigarette use was positively correlated with lifetime e-cigarette use, difficulty describing feelings, and marginally correlated with difficulty identifying feelings and sexual abuse. Lastly, females reported greater difficulty describing feelings.
Table 1.
Means, Standard Deviations, and Correlations for Study Variables
| M | SD | Correlations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| 1. Ethnicitya (W1) | 0.85 | 0.36 | – | |||||||||
| 2. Age (W1) | 14.90 | 0.68 | 0.11 | – | ||||||||
| 3. Sexb (W1) | 0.51 | 0.50 | −0.11 | 0.02 | – | |||||||
| 4. Physical abuse (W1) | 0.22 | 0.41 | −0.06 | −0.01 | 0.08 | – | ||||||
| 5. Sexual abuse (W1) | 0.05 | 0.21 | 0.02 | −0.05 | −0.01 | 0.22** | – | |||||
| 6. Lifetime E-Cigarette Use (W1-V1) | 0.38 | 0.49 | 0.16* | 0.09 | −0.01 | 0.10 | 0.17* | – | ||||
| 7. Emotional Abuse/Neglect (W1-V1) | 0.37 | 0.48 | −0.06 | −0.02 | 0.04 | 0.45*** | 0.24** | 0.12 | – | |||
| 8. Difficulty Identifying Feelings (W1-V2) | 13.22 | 5.24 | 0.04 | −0.02 | −0.04 | 0.12 | 0.13 | 0.11 | 0.21** | – | ||
| 9. Difficulty Describing Feelings (W1-V2) | 12.60 | 4.83 | 0.14† | 0.07 | −0.22** | 0.03 | 0.01 | 0.02 | 0.22** | 0.61*** | – | |
| 10. E-Cigarette Use since last visit (~15 months apart; W2) | 9.36 | 37.55 | −0.09 | 0.04 | 0.09 | −0.05 | 0.16† | 0.18* | 0.03 | 0.15† | 0.23** | – |
Note:
marginal p = 0.07;
p < 0.05;
p < 0.01;
p < 0.001;
W1-V1 = Wave 1-Visit 1, W1-V2 = Wave 1-Visit 2; W2 = Wave 2;
Hispanic No = 0, Yes = 1;
Female = 0, Male = 1;
3.1. Model Results
Figure 1 illustrates the results of the parallel mediator model regressed on emotional abuse/neglect. Results for the MLR indirect effects and the bias-corrected bootstrapping CIs were largely the same across procedures.
Figure 1.
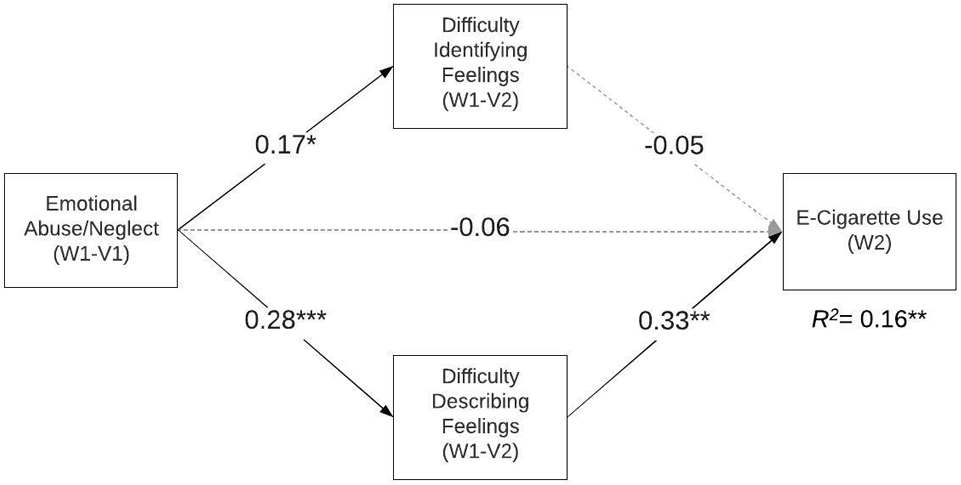
Youth’s self-report of emotional abuse/neglect on e-cigarette use through difficulty identifying and describing feelings via parallel mediation; *p < 0.05, ** p < 0.01, *** p < 0.001; W1-V1 = Wave 1-Visit 1, W1-V2 = Wave 1-Visit 2; W2 = Wave 2.
The model accounted for approximately 6% of the variance in difficulty identifying feelings. Emotional abuse/neglect was a significant predictor of difficulty identifying feelings (effect = 0.17, p = 0.03), such that higher levels of emotional abuse/neglect were associated with greater difficulty identifying feelings. Further, the model accounted for approximately 13% of the variance in difficulty describing feelings. Emotional abuse/neglect was a significant predictor of difficulty describing feelings, such that higher levels of emotional abuse/neglect were associated with greater difficulty describing feelings (effect = 0.28, p = 0.001).
The model accounted for approximately 16% of the variance in e-cigarette use. There was no support for a direct effect of emotional abuse/neglect on e-cigarette use (effect = −0.06, p = 0.48). Furthermore, the effect of difficulty identifying feelings on e-cigarette use was not significant (effect = −0.05, p = 0.70). However, the effect of difficulty describing feelings on e-cigarette use was significant (effect = 0.33, p = 0.003), such that higher levels of difficulty describing feelings were associated with greater e-cigarette use.
Overall, results supported a significant indirect effect of emotional abuse/neglect through difficulty describing feelings (sum of indirect 95% CI [1.68, 16.48]; specific indirect 95% CI [1.74, 18.58). Mediation through difficulty identifying feelings was not supported in the model (specific indirect 95% CI [−5.91, 2.94]).2
4. Discussion
Adolescent e-cigarette use in the US has skyrocketed in recent years and has been declared a public health epidemic (U.S. Food and Drug Administration, 2018). Given the public health concerns surrounding adolescent e-cigarette use, the purpose of this study was to provide a better understanding of factors leading to e-cigarette use. The association between childhood emotional abuse/neglect and alexithymia (difficulty identifying and describing feelings) on e-cigarette use was examined as both factors have been associated with smoking cigarettes (Lewis et al., 2011; Linn et al., 2020; Melka, Alemu et al., 2019; Ünübol and Hızlı Sayar, 2019; Yoon et al., 2020). We hypothesized that difficulties identifying and describing feelings would mediate the association between emotional abuse/neglect and e-cigarettes among adolescents. Results of our parallel mediation model offered partial support for our hypotheses. Consistent with prior work (Ayres, 2020), findings indicated that emotional abuse/neglect did not directly predict e-cigarette use. However, findings supported emotional abuse/neglect as a pathway to adolescent e-cigarette use via difficulty describing feelings. Specifically, more emotional abuse/neglect predicted greater difficulty describing feelings, which in turn predicted future e-cigarette use even when controlling for lifetime e-cigarette use. By contrast, there was no support for difficulty identifying feelings as a potential mediator along this pathway.
The findings of this study are novel in a number of ways. Past research has identified other pathways linking childhood trauma with SU, suggesting that it is not trauma per se directly predicting SU, but rather subsequent cognitive/emotional alterations linked with trauma (e.g., limited problem solving, negative emotionality) that may explain the association (Ayres, 2020). The current study expands on the aforementioned findings by examining difficulties describing and identifying feelings as additional specific factors characterizing impaired emotion regulation to further explain the link between childhood emotional abuse/neglect and e-cigarette use. Moreover, this study expands on the adult literature given a focus on a younger sample of female and male adolescents. Namely, we demonstrated that among adolescents, childhood trauma was not directly associated with e-cigarettes, but may be explained by other factors such as alexithymia.
Further, we demonstrated that emotional abuse/neglect predicted both aspects of alexithymia (i.e., difficulty identifying and describing feelings). Brown et al. (2018) examined the link between emotional abuse and emotional neglect with alexithymia. Those authors found that self-reported emotional abuse or neglect was significantly associated with difficulty describing and identifying feelings. Indeed, childhood trauma appears to have detrimental effects on a child’s development including emotion regulation and identification (Pollak, 2008; Zdankiewicz-Ścigała and Ścigała, 2020). Moreover, trauma can harm awareness of emotions impacting how an individual is able to distinguish different emotions and communicate them to others (Brown et al., 2018).
Yet, an important finding of this study was that just one of the two tested aspects of alexithymia predicted adolescent e-cigarette use. That is, only difficulty describing feelings (not difficulty identifying feelings) predicted e-cigarette use among adolescents, mediating the association between emotional abuse/neglect and e-cigarette use. Noteworthy, most studies investigating the overall impact of alexithymia on SU as a whole compared to a more nuanced understanding of differences across difficulty identifying and describing feelings. Nevertheless, prior studies have demonstrated associations between difficulties in emotion identification and regulation and SU, such as alcohol use (Axelrod et al., 2011; Betka et al., 2018; Di Pierro et al., 2015; Kopera et al., 2020). For example, Betka et al. (2018) found that difficuly identifying feelings (and not difficulties describing feelings) explained the association between sensitivity to bodily sensations and alcohol use. Prior work has suggested that individuals with higher levels of alexitymia may use alcohol to reduce tension and for affective change. Indeed, it has been demonstrated that difficulties in emotion regulation and psychological distress could explain the link between alexithymia and alcohol (Linn et al., 2021). Drinking behavior is linked to outcome expectancies, such as affect regulation expectancies and tension reduction expectancies (Thorberg et al., 2011). Although not tested directly, our findings suggest that nuances might exist across different substances and aspects of alexithymia. Notably, our results indicate that adolescents may recur to e-cigarettes to mitigate alterations in describing their feelings instead of as a coping mechanism for identifying emotions. Prior work has suggested that those who have experienced some type of recurrent affective burden may use substances, such as alcohol, to handle uncontrolled feelings and communicate emotions (Zdankiewicz-Ścigała & Ścigała, 2020). E-cigarettes are often used in social contexts (Kong et al., 2019; Park et al., 2019). Nicotine, which is often found in e-cigarettes, releases dopamine and noradrenaline in the brain (Quattrocki, Braid & Yurgelun-Todd, 2000), modulating action, learning, and memory processes (Ranjbar-Slamloo & Fazlali; 2020); plausibly, improving verbalization of emotions. For example, prior work suggests that dopamine modulates the motivational properties of social play, whereas noradrenaline is implicated in attention and arousal processes (Achterberg et al., 2016). Possibly, noradrenaline that is released by nicotine improves attention to emotional states and emotion regulation, while dopamine promotes social interaction. Thus, adolescents who are limited in describing their feelings as a result of prior adverse experiences may vape as a way to connect emotionally with others and emotions within themselves. In addition, consistent with Akers and Lee (1996) work on social learning theory and smoking, it is possible that adolescents’ vaping behavior is reinforced through social interaction and feelings of belonginess. Yet, more research is needed to understand links between e-cigarettes, or nicotine specifically, on different facets of alexithymia, as research in this area is limited.
4.1. Limitations
Potential limitations of this research include generalizability across adolescent populations. Namely, the sample was comprised mainly of Hispanic/Latinx (84.94%) adolescents. Prior work has shown that Hispanic/Latinx adolescents present an increased risk for initiating e-cigarette use at an early age compared to adolescents from other ethnicities suggesting that Hispanic/Latinx adolescents are at higher risk for future nicotine dependence (Lanza et al., 2017). Moreover, people of Hispanic/Latinx origin are more likely to experience childhood emotional neglect compared to those of non-Hispanic white origin (Hunt et al., 2017; Taillieu et al., 2016). This suggests that our sample may reflect high rates of childhood emotional abuse/neglect and e-cigarette use (i.e., 36.8% and 24.0; respectively). Hence, our findings may not generalize to other ethnicities. Furthermore, the inclusion criteria of the larger longitudinal study required a sample of adolescents at greater risk of SU initiation (e.g., reporting having a friend or sibling ever try a substance). Even though our sample is likely representative of typical high school students in the region (i.e., most high school students screened at high-risk with only 2.6% not meeting a high-risk criterion), results may not generalize to adolescents from other regions. The current study relies on self-report measures to assess childhood trauma, e-cigarette use, and alexithymia. This could pose a problem of shared method variance (Orth, 2013). Moreover, cognitive factors (e.g., comprehension of the question) or situational factors (e.g., stigma about substance use) may have impacted adolescent’s honest responding of e-cigarette use (Brener et al., 2003). Furthermore, individuals with alexithymia can demonstrate biased perceptions of their emotional states when using subjective measures (Betka et al., 2018). Future studies should consider including multiple reporters on trauma experiences or more objective measures of alexithymia and e-cigarette use, and examine such associations within a larger sample. Lastly, only 16% of the variance in e-cigarette use is explained by our model; thus, other potential pathways to adolescent e-cigarette use may exist.
4.2. Clinical implications
A closer examination of negative sequelae of childhood trauma, such as difficulty describing feelings, may have utility in informing which adolescents who have experienced emotional abuse/neglect could be at increased risk for e-cigarette use and benefit from prevention programming. Promoting emotion regulation skills may be beneficial for those adolescents who have experienced childhood trauma (Sloan et al., 2018). However, one challenge of enhancing emotion regulation skills among individuals with alexithymia is the mere task of accurately identifying and describing emotions. Thus, instructing individuals how to interpret affective signals, also known as “somatic markers,” which consist of assessing bodily signals and feelings as “good” or “bad” is a critical first step (Damasio, 1994; Storch et al., 2011). For example, the Zurich Resource Model (ZRM) is a psychoeducational training that has shown positive effects on individuals with alexithymia as it focuses on affect regulation skills, which includes addressing somatic markers (Storch et al., 2011). Psychoeducational trainings combined with expressive writing practices may have potential benefits to offset the negative sequelae of childhood trauma, such as difficulty describing feelings. Fostering expressive writing about traumatic, stressful, or emotional events could also have benefits for adolescents with difficulties communicating their emotions(Baikie and Wilhelm, 2005). Expressive writing has shown positive effects on individuals with high alexithymia, specifically for those with difficulties describing their feelings (Baikie, 2008).
Moreover, we speculate that, promoting transdiagnostic treatment targets, such as Emotion Regulation Treatment (ERT), could have positive effects on adolescents’ deficits in not only identifying but also describing feelings. ERT is a combination of promoting emotion regulation skills with cognitive-behavioral treatment, and includes awareness and understanding of emotions (Sloan et al., 2018; Stasiewicz et al., 2018). This type of intervention has shown to be effective among young adults seeking treatment for alcohol and other SU disorders as emotion regulation has been implicated as a potential mechanism linking childhood maltreatment and subsequent SU (Sloan et al., 2018).
5. Conclusion
As rates of adolescent e-cigarette use remain high, the current study provides enhanced insight into factors linked with adolescent e-cigarette use. Specifically, the present study demonstrated an association between childhood emotional abuse/neglect and e-cigarette use through difficulties describing feelings. Adolescents who have experienced emotional abuse/neglect were more likely to exhibit difficulties describing feelings and, in turn, may experience an increased risk of e-cigarette use. Fostering targeted treatment associated with emotion regulation and verbalization may offer utility in reducing risk for e-cigarette use among adolescents with experience of emotional trauma during childhood.
Footnotes
Due to non-significant associations between emotional abuse/neglect with Externally-Oriented Thinking subscale (r = −0.02, p = 0.84), the Externally-Oriented Thinking subscale was not included in the estimated model.
Results demonstrated that the joint significant test also supported mediation through difficulty describing feelings.
References
- Akers RL, Lee G, 1996. A longitudinal test of social learning theory: Adolescent smoking. Journal of Drug Issues 26(2), 317–343. [Google Scholar]
- Axelrod SR, Perepletchikova F, Holtzman K, Sinha R, 2011. Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. The American Journal of Drug and Alcohol Abuse 37(1), 37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayres TC, 2020. Childhood trauma, problematic drug use and coping. Deviant Behavior. [Google Scholar]
- Bagby RM, Parker JDA, Taylor GJ, 1994. The twenty-item Toronto Alexithymia Scale: I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research 38(1), 23–32. [DOI] [PubMed] [Google Scholar]
- Baikie KA, 2008. Who does expressive writing work for? Examination of alexithymia, splitting, and repressive coping style as moderators of the expressive writing paradigm. British Journal of Health Psychology 13(1), 61–66. [DOI] [PubMed] [Google Scholar]
- Baikie KA, Wilhelm K, 2005. Emotional and physical health benefits of expressive writing. Advances in Psychiatric Treatment 11(5), 338–346. [Google Scholar]
- Betka S, Pfeifer G, Garfinkel S, Prins H, Bond R, Sequeira H, Duka T, Critchley H, 2018. How Do Self-Assessment of Alexithymia and Sensitivity to Bodily Sensations Relate to Alcohol Consumption? Alcoholism: Clinical and Experimental Research 42(1), 81–88. [DOI] [PubMed] [Google Scholar]
- Brener ND, Billy JOG, Grady WR, 2003. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health 33(6), 436–457. [DOI] [PubMed] [Google Scholar]
- Brown S, Fite PJ, Stone K, Richey AL, Bortolato M, 2018. Associations between emotional abuse and neglect and dimensions of alexithymia: The moderating role of sex. Psychol Trauma 10(3), 300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruise KE, Becerra R, 2018. Alexithymia and problematic alcohol use: A critical update. Addictive Behaviors 77, 232–246. [DOI] [PubMed] [Google Scholar]
- Damasio A, 1994. Descartes’ error. Emotion, reason, and the human brain. New York: Putnam. [Google Scholar]
- de Bruin PMJ, de Haan HA, Kok T, 2019. The prediction of alexithymia as a state or trait characteristic in patients with substance use disorders and PTSD. Psychiatry Res. 282, 112634. [DOI] [PubMed] [Google Scholar]
- De Rick A, Vanheule S, Verhaeghe P, 2009. Alcohol Addiction and the Attachment System: An Empirical Study of Attachment Style, Alexithymia, and Psychiatric Disorders in Alcoholic Inpatients. Substance Use & Misuse 44(1), 99–114. [DOI] [PubMed] [Google Scholar]
- Di Pierro R, Benzi IMA, Madeddu F, 2015. Difficulties in emotion regulation among inpatients with substance use disorders: The mediating effect of mature defenses mechanisms. Clinical Neuropsychiatry: Journal of Treatment Evaluation 12(4), 83–89. [Google Scholar]
- Evren C, Evren B, Dalbudak E, Ozcelik B, Oncu F, 2009. Childhood abuse and neglect as a risk factor for alexithymia in adult male substance dependent inpatients. J Psychoactive Drugs 41(1), 85–92. [DOI] [PubMed] [Google Scholar]
- Fadus MC, Smith TT, Squeglia LM, 2019. The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects. Drug and Alcohol Dependence 201, 85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA, 2007. Poly-victimization: A neglected component in child victimization. Child Abuse & Neglect 31(1), 7–26. [DOI] [PubMed] [Google Scholar]
- Gibson LA, Creamer MR, Breland AB, Giachello AL, Kaufman A, Kong G, Pechacek TF, Pepper JK, Soule EK, Halpern-Felsher B, 2018. Measuring perceptions related to e-cigarettes: Important principles and next steps to enhance study validity. Addictive Behaviors 79, 219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser D, 2002. Emotional abuse and neglect (psychological maltreatment): a conceptual framework. Child Abuse Negl 26(6–7), 607–714. [DOI] [PubMed] [Google Scholar]
- Guzzo G, Pace U, Lo Cascio V, Craparo G, Schimmenti A, 2014. Bullying Victimization, Post-Traumatic Symptoms, and the Mediating Role of Alexithymia. Child Indicators Research 7(1), 141–153. [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delasqua F, Kirby J, Duda SN, consortium R., 2019. The REDCap consortium: Building an international community of software partners. J Biomed Inform. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne L, Gonzalez N, Conde JG, 2009. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinz AJ, Kassel JD, Berbaum M, Mermelstein RJ, 2010. Adolescents’ expectancies for smoking to regulate affect predict smoking behavior and nicotine dependence over time. Drug and Alcohol Dependence 111, 128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt TKA, Slack KS, Berger LM, 2017. Adverse childhood experiences and behavioral problems in middle childhood. Child Abuse & Neglect 67, 391–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, Taylor K, Crosse S, Fong GT, Cummings KM, Abrams D, Pierce JP, Sargent J, Messer K, Bansal-Travers M, Niaura R, Vallone D, Hammond D, Hilmi N, Kwan J, Piesse A, Kalton G, Lohr S, Pharris-Ciurej N, Castleman V, Green VR, Tessman G, Kaufman A, Lawrence C, van Bemmel DM, Heather L Kimmel HL, Blount B, Yang L, O’Brien B, Tworek C, Alberding D, Hull LC, Cheng Y, Maklan D, Backinger CL, Compton WM, 2016. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tobacco Control 26, 371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubczyk A, Trucco EM, Klimkiewicz A, Skrzeszewski J, Suszek H, Zaorska J, Nowakowska M, Michalska A, Wojnar M, Kopera M, 2020. Association Between Interoception and Emotion Regulation in Individuals With Alcohol Use Disorder. Frontiers in Psychiatry 10(1028). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME, 2021. Monitoring the Future national survey results on drug use 1975–2020: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, University of Michigan. [Google Scholar]
- Khantzian EJ, 1985. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. The American journal of psychiatry 142(11), 1259–1264. [DOI] [PubMed] [Google Scholar]
- Kong G, Bold KW, Morean ME, Bhatti H, Camenga DR, Jackson A, Krishnan-Sarin S, 2019. Appeal of JUUL among adolescents. Drug and Alcohol Dependence 205, 107691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopera M, Jakubczyk A, Suszek H, Glass JM, Klimkiewicz A, Wnorowska A, Brower KJ, Wojnar M, 2015. Relationship Between Emotional Processing, Drinking Severity and Relapse in Adults Treated for Alcohol Dependence in Poland. Alcohol and Alcoholism 50(2), 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopera M, Trucco EM, Jakubczyk A, Suszek H, Kobylinski P, Wojnar M, Zucker RA, 2020. Relationship Between Alcohol-related Family Adversity, Alcohol Use Across Adolescence, and Mental States Recognition in Young Adulthood. Journal of Addiction Medicine 14(5), e247–e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristman-Valente AN, Brown EC, Herrenkohl TI, 2013a. Child Physical and Sexual Abuse and Cigarette Smoking in Adolescence and Adulthood. Journal of Adolescent Health 53(4), 533–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristman-Valente AN, Brown EC, Herrenkohl TI, 2013b. Child physical and sexual abuse and cigarette smoking in adolescence and adulthood. J Adolescent Health 53(4), 533–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kupferschmidt DA, Funk D, Erb S, Le AD, 2010. Age-related effects of acute nicotine on behavioural and neuronal measures of anxiety. Behavioural Brain Research 213, 288–292. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Russell MA, Braymiller JL, 2017. Emergence of electronic cigarette use in US adolescents and the link to traditional cigarette use. Addictive behaviors 67, 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, Stone MD, Khoddam R, Samet JM, Audrain-McGovern J, 2015. Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence. JAMA 314(7), 700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TL, Kotch J, Wiley TRA, Litrownik AJ, English DJ, Thompson R, Zolotor AJ, Block SD, Dubowitz H, 2011. Internalizing Problems: A Potential Pathway From Childhood Maltreatment to Adolescent Smoking. Journal of Adolescent Health 48(3), 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linn BK, Stasiewicz PR, Fillo J, Bradizza CM, 2020. The Great Disrupter: Relationship of Alexithymia to Emotion Regulation Processes and Smoking among Pregnant Women. Substance Use & Misuse 55(7), 1113–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linn BK, Zhao J, Bradizza CM, Lucke JF, Ruszczyk MU, Stasiewicz PR, 2021. Alexithymia disrupts emotion regulation processes and is associated with greater negative affect and alcohol problems. Journal of Clinical Psychology 77(12), 2915–2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loas G, Braun S, Delhaye M, Linkowski P, 2017. The measurement of alexithymia in children and adolescents: Psychometric properties of the Alexithymia Questionnaire for Children and the twenty-item Toronto Alexithymia Scale in different non-clinical and clinical samples of children and adolescents. PLOS ONE 12(5), e0177982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melka A, Chojenta C, Holliday E, Loxton D, 2019. Adverse childhood experiences and electronic cigarette use among young Australian women. Preventive Medicine 126, 105759. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 1998–2012. Mplus User’s Guide: Statistical Analysis with Latent Variables (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Orth U, 2013. How Large Are Actor and Partner Effects of Personality on Relationship Satisfaction? The Importance of Controlling for Shared Method Variance. Personality and Social Psychology Bulletin 39(10), 1359–1372. [DOI] [PubMed] [Google Scholar]
- Pollak SD, 2008. Mechanisms Linking Early Experience and the Emergence of Emotions. Current Directions in Psychological Science 17(6), 370–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF, 2008. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Sachser C, Berliner L, Holt T, Jensen TK, Jungbluth N, Rish E, Rosner R, Goldbeck L, 2017. International development and psychometric properties of the Child and Adolescent Trauma Screen (CATS). J Affect Disord 1(210), 189–195. [DOI] [PubMed] [Google Scholar]
- Shin SH, Conley D, Ksinan Jiskrova G, Wills TA, 2019. Adverse Childhood Experiences and E‐Cigarette Use During Young Adulthood. The American Journal on Addictions 28(4), 303–310. [DOI] [PubMed] [Google Scholar]
- Sifneos PE, 1973. The prevalence of ‘Alexithymic’ characteristics in psychosomatic patients. Psychotherapy and Psychosomatics 22(2/6), 255–262. [DOI] [PubMed] [Google Scholar]
- Sloan E, Hall K, Simpson A, Youssef GJ, Moulding R, Mildred H, Staiger PK, 2018. An emotion regulation treatment for young people with complex substance use and mental health issues: A case-series analysis. Cognitive and Behavioral Practice 25, 427–411. [Google Scholar]
- Stasiewicz PR, Bradizza CM, Slosman KS, 2018. Emotion Regulation Treatment of Alcohol Use Disorders.
- Storch M, Keller F, Weber J, Spindler A, Milos G, 2011. Psychoeducation in Affect Regulation for Patients with Eating Disorders: A Randomized Controlled Feasibility Study. American Journal of Psychotherapy 65(1), 81–93. [DOI] [PubMed] [Google Scholar]
- Strathearn L, Giannotti M, Mills R, Kisely S, Najman J, Abajobir A, 2020. Long-term Cognitive, Psychological, and Health Outcomes Associated With Child Abuse and Neglect. Pediatrics 146(4), e20200438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland MT, Riedel MC, Flannery JS, Yanes JA, Fox PT, Stein EA, Laird AR, 2016. Chronic cigarette smoking is linked with structural alterations in brain regions showing acute nicotinic drug-induced functional modulations. Behavioral and Brain Functions 12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taillieu TL, Brownridge DA, Sareen J, Afifi TO, 2016. Childhood emotional maltreatment and mental disorders: Results from a nationally representative adult sample from the United States. Child Abuse & Neglect 59, 1–12. [DOI] [PubMed] [Google Scholar]
- Thorberg FA, Young RM, Sullivan KA, Lyvers M, Hurst CP, Connor JP, Feeney GFX, 2011. Alexithymia in alcohol dependent patients is partially mediated by alcohol expectancy. Drug and Alcohol Dependence 116(1–3), 238–241. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration, 2018. Statement from FDA Commissioner Scott Gottlieb, M.D., on proposed new steps to protect youth by preventing access to flavored tobacco products and banning menthol in cigarettes. https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-proposed-new-steps-protect-youth-preventing-access. (Accessed 11/15 2018).
- Ünübol H, Hızlı Sayar G, 2019. Psychological factors associated with smoking and quitting: addiction map of Turkey study. Neuropsychiatric Disease and Treatment Volume 15, 1971–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente MJ, Gonzalez O, Miočević M, Mackinnon DP, 2016. A Note on Testing Mediated Effects in Structural Equation Models. Educational and Psychological Measurement 76(6), 889–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon S, Dillard R, Kobulsky J, Nemeth J, Shi Y, Schoppe-Sullivan S, 2020. The Type and Timing of Child Maltreatment as Predictors of Adolescent Cigarette Smoking Trajectories. Substance Use & Misuse 55(6), 937–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zdankiewicz-Ścigała E, Ścigała DK, 2020. Attachment Style, Early Childhood Trauma, Alexithymia, and Dissociation Among Persons Addicted to Alcohol: Structural Equation Model of Dependencies. Frontiers in Psychology 10(2957). [DOI] [PMC free article] [PubMed] [Google Scholar]


