Abstract
Introduction:
Consumption of ultra-processed foods (UPFs) has been linked with higher intakes of added sugars, sodium, and unhealthful fats, but the associations of UPFs with overall diet quality and major food groups are not well known.
Methods:
Data were derived from the National Health and Nutrition Examination Survey (2015–2018) including 9,758 adults (aged ≥20 years) and 5,280 children (aged 2–19 years) with 24-hour dietary recalls (≥1), with analysis performed in 2020. UPFs were identified using the NOVA classification, with intake (% energy) assessed in quintiles. Diet quality was assessed using the validated American Heart Association (AHA) 2020 continuous primary and secondary diet score and Healthy Eating Index 2015. Poor diet was defined as <40% adherence to the AHA secondary score. Generalized linear regressions estimated relationships between UPF intake and diet quality.
Results:
Compared with the lowest quintile of UPF consumption (<39.1% energy), the AHA primary score in adults was progressively lower in Quintile 2 (−1.99, 95% CI= −2.73, −1.25), 3 (−3.60, 95% CI= −4.47, –2.72), 4 (−5.29, 95% CI= −6.28, −4.30), and 5 (−7.24, 95% CI= −8.13, −6.36; >70.7% energy). Corresponding values in children were −2.05 (95% CI= −3.01, −1.09), −2.97 (95% CI= −4.16, −1.79), −3.82 (95% CI= −5.20, −2.44), and −6.22 (95% CI= –7.20, −5.25; >79.0% energy). The estimated proportions of children having poor diet progressively increased from 31.3% (95% CI=26.2%, 36.5%) in Quintile 1 and up to 71.6% (95% CI=68.1%, 75.1%) in Quintile 5. Corresponding proportions of adults having poor diet increased from 18.1% (95% CI=14.3%, 22.0%) in Quintile 1 and up to 59.7% (95% CI=55.3%, 64.1%) in Quintile 5. Findings were similar using the AHA secondary score and Healthy Eating Index 2015 score.
Conclusions:
Higher UPF consumption is associated with substantially lower diet quality among children and adults.
INTRODUCTION
Ultra-processed foods (UPFs) are defined as industrial formulations manufactured from substances derived from foods with little, if any, whole food and typically with added flavors, colors, and other additives.1 Food supplies have dramatically changed over the past 50 years, with UPF products becoming the major source of energy, especially in Western countries, perhaps owing to their higher profit margin and increased shelf life, availability, and convenience.2,3 In the U.S., UPFs contribute to more than half of total calories consumed.4 The association between UPF consumption and adverse health outcomes increasingly has been studied.1 Findings support positive associations of UPF consumption with mortality,5–8 overweight and obesity,9 type 2 diabetes,10 cardiovascular disease,11 cancer,12 and depression.13,14 In addition, one short-term metabolic RCT15 showed that eating a diet made up of UPFs led to higher calorie consumption and weight gain compared with a diet of whole or minimally processed foods. Studies modeling mediation analysis concluded that differences in nutrient intake (such as sodium, fats, carbohydrates) and dietary food patterns were at least partial drivers of the association between UPF consumption and health outcomes.8,11,12
Though studies have suggested inverse associations of UPF consumption with specific nutrients like protein, vitamins, dietary fiber, minerals, and overall nutrient-balanced patterns,16–19 no prior studies have focused comprehensively on the associations of UPF consumption with dietary quality and major food groups among both children and adults. Understanding these relationships is important for policymakers to set effective strategies to improve diet quality and related health outcomes. To address this gap in knowledge, this study investigates how UPF consumption relates to overall diet quality and major food group consumption among nationally representative samples of U.S. adults and children.
METHODS
Study Population
The National Health and Nutrition Examination Survey (NHANES) is a series of cross-sectional surveys designed to assess health and nutritional status of Americans in a nationally representative sample using a complex, stratified, and multistage probability sampling method. Details on design, study protocol, and data collection have been reported.20 The study protocol was approved by the National Center for Health Statistics Research Ethics Review Board, and all participants provided written informed consent. This analysis combined the 2 most recent cycles of NHANES (2015–2016 and 2017–2018). Investigators separately evaluated children (aged 2–19 years) and adults (aged ≥20 years). Dietary habits were assessed through 1–2 standardized 24-hour dietary recalls per person (Appendix Text 1).21 Individuals with potentially unreliable dietary intake and young children who were breastfed were excluded (Appendix Figure 1).
Measures
All recorded food items were classified according to NOVA, a food classification system characterizing the extent and purpose of industrial food processing.1 This classification includes 4 groups: unprocessed or minimally processed foods; processed culinary ingredients; processed foods; and UPFs, products characterized by several stages and various processing techniques and ingredients. Details regarding each food group and examples are provided (Appendix Text 2, Appendix Table 1). If a food item (food code) was deemed to be a homemade recipe, the NOVA classification was applied to the underlying ingredients (U.S. Department of Agriculture National Nutrient Database for Standard Reference Code-SR code) obtained from the U.S. Department of Agriculture Food and Nutrient Database for Dietary Studies. Details have been described previously4,22 and are provided in Appendix Figure 2.
Diet quality was assessed using American Heart Association (AHA) diet score23 and Healthy Eating Index (HEI)-2015 score24 (Appendix Text 3). The AHA score was chosen because it was developed as a measure of cardiovascular health, has been widely validated against diverse clinical outcomes in a range of studies,23 and is a largely food-based score that is readily translated to the public and policymakers. The AHA diet score was constructed based on the AHA 2020 Strategic Impact Goals for diet, which have been associated with cardiometabolic and other disease outcomes in multiple populations.23 The 5 primary dietary components of the AHA diet score are total fruits/vegetables, whole grains, fish/shellfish, sugar-sweetened beverages (SSBs), and sodium. The AHA secondary dietary components add nuts/seeds/legumes, processed meat, and saturated fat. The HEI-2015 was chosen because it reflects adherence to key recommendations in the U.S. Dietary Guidelines for Americans.24 The 9 adequacy components include total fruit, whole fruit, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant protein, and fatty acids. The 4 moderation components include refined grains, sodium, percentage of energy from added sugars, and percentage of energy from saturated fatty acids. The diet scores range from 0 to 50 for AHA primary score, 0 to 80 for AHA secondary score, and 0 to 100 for the HEI-2015 score (Appendix Tables 2–3). Poor diet was defined as being <40% adherent to AHA secondary score (<32 points).25 In addition, this study evaluated intake of individual foods/beverages and nutrients linked to major health outcomes as well as those of current policy or general public interest across the distribution of UPFs.26 Intake of all dietary components were energy adjusted using the residual method to minimize measurement error in dietary estimates and help account for differences in age, sex, muscle mass, physical activity, and metabolic expenditure.
Covariates included age, sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and other), educational level (less than high school, high school graduate or equivalent, some college, and college graduate), family income (ratio to the federal poverty level: <1.30, 1.30– 1.84, 1.85–2.99, and ≥3.00), and BMI levels. Educational level among children refers to their parental education attainment. The ratio to the federal poverty level was calculated by dividing family income by the poverty guidelines, specific to family size, as well as the appropriate year and state, set by HHS.27
Statistical Analysis
All statistical analyses were performed using Stata, version 14. All analyses used the NHANES dietary weights, which account for differential probabilities of selection and the complex survey design to create nationally representative estimates. The 1-day value was used for individuals with single recalls and 2-day means for those with 2 recalls. The significance level was 0.05, and all tests were 2-sided.
This study presents quintiles of UPF contribution to total energy intake (% energy). Proportions were calculated to describe the characteristics of participants overall and by quintiles of UPF (% energy). Linear regression models were used to assess the associations between UPF in quintiles and diet quality scores with adjustments of the aforementioned covariates. Logistic regression models were used to assess the associations of UPF with poor diet quality with the same covariate adjustments as in linear models. Predicted margins were calculated and showed the standardized prevalence of poor diet quality by quintiles of the contribution of UPF (% energy; based on the model coefficients and standardized to the distribution of the model covariates within the analytic sample).
RESULTS
This study included 5,919 children and 10,064 adults from NHANES cycles 2015–2016 and 2017–2018. Characteristics of these participants across quintiles of UPF (% energy) are shown (Table 1). Among both children and adults, participants who were male, non-Hispanic White or Black, and had lower education were among the highest UPF consumers; Hispanic and other race/ethnicity and college graduates were among the lowest consumers. Whereas in children UPF consumption increased with age, an opposite trend was observed in adults. In adults, the highest income stratum consumed less UPF, compared with lower incomes.
Table 1.
Sociodemographic Characteristics of Study Participants by Quintiles of the Contribution of Ultra-Processed Foods to Total Energy Intake, NHANES 2015–2018a
| Variable | Overall | Q1 | Q2 | Q3 | Q4 | Q5 |
|---|---|---|---|---|---|---|
|
| ||||||
| Children | N=5,280 | n=1,157 | n=1,063 | n=998 | n=985 | n=1,077 |
| Age, years | ||||||
| 2 to 5 | 21.4 (20.1, 22.8) | 31.5 (27.7, 35.7) | 27.7 (24.6, 31.1) | 19.6 (16.4, 23.2) | 15.9 (13.0, 19.2) | 12.4 (9.73, 15.6) |
| 6 to 11 | 33.4 (31.7, 35.3) | 25.3 (22.0, 29.0) | 28.5 (25.2, 32.2) | 39.2 (35.1, 43.4) | 38.3 (34.5, 42.1) | 35.8 (31.7, 40.2) |
| 12 to 19 | 45.1 (42.4, 47.9) | 43.1 (37.6, 48.8) | 43.7 (38.8, 48.9) | 41.2 (36.3, 46.4) | 45.8 (41.8, 49.9) | 51.8 (47.9, 55.7) |
| Sex | ||||||
| Male | 50.9 (48.7, 53.0) | 45.7 (42.3, 49.1) | 49.4 (44.2, 54.5) | 49.5 (44.9, 54.1) | 56.0 (51.6, 60.3) | 53.8 (50.4, 57.3) |
| Female | 49.1 (47.0, 51.3) | 54.3 (50.9, 57.7) | 50.6 (45.5, 55.8) | 50.5 (45.9, 55.1) | 44.0 (39.7, 48.4) | 46.2 (42.7, 49.6) |
| Race/Ethnicity | ||||||
| Non-Hispanic | 50.7 (43.8, 57.6) | 39.4 (31.4, 48.1) | 48.6 (42.1, 55.1) | 54.7 (47.1, 62.2) | 55.6 (47.9, 63.0) | 55.2 (45.9, 64.3) |
| White | ||||||
| Non-Hispanic | 13.3 (9.87, 17.8) | 10.7 (7.6, 14.7) | 10.8 (‘.77, 14.8) | 13.7 (9.86, 18.8) | 13.5 (9.77, 18.5) | 18.0 (12.5, 25.1) |
| Black | ||||||
| Hispanic | 24.7 (19.5, 30.7) | 32.8 (25.5, 41.1’ | *’9.6 (23.1, 37.1) | 20.8 (15.8, 27.0) | 21.7 (16.8, 27.5) | 18.5 (13.8, 24.4) |
| Other | 11.3 (9.3, 13.6) | 17.1 (13.3, 21.8) | 11.0 (8.27, 14.5) | 10.7 (7.96, 14.2) | 9.20 (6.92, 12.1) | 8.25 (5.96, 11.3) |
| Education levelb | ||||||
| Less than high | 17.6 (14.1, 21.7) | 21.6 (16.2, 28.2) | 20.5 (15.3, 26.9) | 18.6 (14.7, 23.3) | 13.1 (10.2, 16.6) | 14.1 (11.0, 18.0) |
| school graduate | ||||||
| High school | 54.3 (50.8, 57.8) | 47.1 (41.4, 52.9) | 53.0 (47.7, 58.2) | 50.3 (45.0, 55.5) | 55.8 (50.2, 61.3) | 65.1 (60.0, 69.9) |
| graduate or GED or some college | ||||||
| College graduate or above | 28.2 (23.9, 32.8) | 31.3 (24.0, 39.7) | 26.6 (21.2, 32.7) | 31.1 (25.3, 37.6) | 31.1 (25.7, 37.0) | 20.8 (15.8, 26.8) |
| Ratio of family income to poverty level | ||||||
| <1.30 | 32.0 (28.2, 36.1) | 31.9 (26.5, 37.9) | 33.7 (28.4, 39.5) | 29.9 (24.6, 35.8) | 28.9 (24.6, 33.5) | 35.7 (29.9, 41.9) |
| 1.30 to 1.849 | 12.9 (11.0, 15.2) | 13.3 (6.82, 17.6) | 13.7 (10.3, 17.9) | 13.2 (10.6, 16.3) | 10.4 (8.73, 12.4) | 14.1 (10.4, 18.9) |
| 1.85 to 2.99 | 19.1 (16.6, 21.9) | 22.1 (18.2, 26.6) | 18.4 (14.7, 22.6) | 16.0 (12.2, 20.7) | 20.0 (16.8, 23.7) | 19.0 (15.1, 23.6) |
| ≥3.0 | 36.0 (30.9, 41.4) | 32.7 (26.5, 39.6) | 34.2 (28.4, 40.6) | 40.9 (34.1, 48.0) | 40.7 (34.4, 47.2) | 31.2 (24.5, 38.9) |
| BMI categories | ||||||
| Underweight | 3.61 (2.73, 4.75) | 3.55 (2.35, 5.31) | 3.84 (2.27, 6.44) | 4.33 (2.51, 7.38) | 3.07 (1.64, 5.68) | 3.25 (2.14, 4.93) |
| Normal weight | 59.1 (56.7, 61.3) | 63.2 (58.8, 67.4) | 59.3 (55.9, 62.7) | 56.4 (51.1, 61.5) | 57.3 (53.6, 60.9) | 59.1 (54.1, 63.8) |
| Overweight | 16.0 (14.7, 17.4) | 15.1 (11.6, 19.3) | 15.2 (12.2, 18.7) | 18.5 (14.8, 23.0) | 17.2 (13.8, 21.2) | 14.0 (11.7, 16.6) |
| Obese | 21.3 (19.3, 23.6) | 18.2 (15.3, 21.5) | 21.6 (18.2, 25.5) | 20.8 (17.3, 24.7) | 22.5 (18.9, 26.5) | 23.7 (20.0, 27.8) |
| Adults | N=9,758 | n=2,277 | n=1,945 | n=1,877 | n=1,780 | n=1,879 |
| Age, years | ||||||
| 20 to 44 | 43.8 (41.2, 46.4) | 39.9 (35.6, 44.3) | 44.6 (40.1, 49.2) | 39.4 (35.1, 43.8) | 45.4 (40.5, 50.4) | 49.6 (46.1, 53.0) |
| 45 to 64 | 35.4 (33.6, 37.2) | 40.1 (36.0, 44.5) | 33.3 (29.7, 37.1) | 36.8 (32.2, 41.6) | 31.5 (28.6, 34.6) | 35.1 (31.7, 38.6) |
| ≥65 | 20.9 (18.9, 22.9) | 19.9 (17.1, 23.2) | 22.0 (18.7, 25.8) | 23.8 (20.3, 27.8) | 23.1 (20.3, 27.8) | 15.4 (13.1, 17.9) |
| Sex | ||||||
| Male | 48.0 (46.8, 49.4) | 46.4 (43.6, 49.2) | 47.5 (43.8, 51.3) | 48.8 (44.9, 52.6) | 48.9 (44.9, 52.9) | 48.8 (46.1, 51.5) |
| Female | 51.9 (50.6, 53.2) | 53.6 (50.8, 56.4) | 52.5 (48.7, 56.2) | 51.2 (47.4, 55.1) | 51.1 (47.1, 55.1) | 51.2 (48.5, 53.9) |
| Race/Ethnicity | ||||||
| Non-Hispanic | 63.2 (58.3, 67.8) | 51.9 (45.3, 58.4) | 62.9 (56.6, 68.8) | 65.6 (59.5, 71.2) | 68.5 (63.9, 72.8) | 67.2 (61.8, 72.2) |
| White | ||||||
| Non-Hispanic | 11.3 (8.87, 14.2) | 9.41 (7.29, 12.1) | 9.21 (7.05, 11.9) | 11.0 (8.64, 14.0) | 11.5 (8.71, 15.1) | 15.2 (11.4, 20.1) |
| Black | ||||||
| Hispanic | 15.4 (12.4, 19.0) | 19.0 (14.8, 24.0) | 17.9 (14.2, 22.4) | 16.6 (12.6, 21.5) | 12.5 (9.59, 16.2) | 11.1 (8.96, 13.7) |
| Other | 10.1 (8.32, 12.2) | 19.8 (16.1, 24.0) | 9.91 (6.39, 11.4) | 6.84 (5.21, 8.94) | 7.42 (5.83, 7.02) | 6.45 (4.98, 8.31) |
| Educational level | ||||||
| Less than high school graduate | 12.2 (10.6, 14.1) | 14.0 (11.6, 16.8) | 12.2 (10.1, 14.6) | 11.6 (9.08, 14.8) | 10.6 (8.65, 12.9) | 12.8 (10.3, 15.9) |
| High school graduate or GED | 24.6 (22.7, 26.5) | 20.5 (17.1, 24.4) | 20.4 (17.8, 23.1) | 23.7 (20.9, 26.8) | 26.2 (22.6, 30.3) | 32.1 (28.3, 36.1) |
| Some college | 32.1 (31.2, 34.1) | 26.5 (23.8, 29.4) | 31.1 (26.9, 35.6) | 31.9 (27.7, 36.3) | 36.8 (33.9, 40.9) | 34.2 (30.8, 37.8) |
| College graduate or above | 31.1 (27.4, 35.0) | 39.0 (32.9, 45.5) | 36.4 (31.6, 41.5) | 32.7 (28.1, 37.7) | 26.4 (21.9, 31.4) | 20.9 (17.3, 24.9) |
| Ratio of family income to poverty level | ||||||
| <1.30 | 20.8 (19.0, 22.8) | 23.4 (19.6, 27.8) | 19.0 (16.2, 22.1) | 18.3 (16.2, 20.6) | 19.8 (16.3, 23.9) | 23.7 (20.7, 27.0) |
| 1.30 to 1.849 | 10.8 (9.47, 12.3) | 10.4 (8.28, 13.1) | 9.56 (7.43, 12.2) | 10.9 (8.57, 13.7) | 10.6 (8.63,12.9) | 12.7 (10.0, 15.9) |
| 1.85 to 2.99 | 18.6 (16.5, 20.8) | 15.2 (12.3, 18.7) | 19.1 (15.6, 23.2) | 19.5 (16.9, 22.4) | 19.6 (16.7, 22.9) | 19.3 (16.5, 22.6) |
| ≥3.0 | 49.8 (46.4, 53.1) | 50.9 (45.5, 56.3) | 52.3 (47.4, 57.2) | 51.4 (46.5, 56.2) | 50.0 (44.6, 55.4) | 44.3 (39.9, 48.7) |
| BMI categories | ||||||
| Underweight | 1.49 (1.18, 1.88) | 1.29 (0.82, 2.03) | 1.25 (0.64, 2.42) | 1.47 (0.81, 2.65) | 1.30 (0.64, 2.60) | 2.13 (1.59, 2.84) |
| Normal weight | 25.0 (23.1, 27.0) | 29.4 (26.6, 32.3) | 28.9 (25.6, 32.5) | 23.4 (20.1, 27.1) | 22.4 (19.6, 25.6) | 21.0 (18.5, 23.7) |
| Overweight | 31.6 (30.0, 33.1) | 35.9 (33.2, 38.7) | 31.9 (28.5, 35.5) | 32.1 (28.2, 36.2) | 29.3 (26.7, 32.1) | 28.6 (24.7, 32.7) |
| Obese | 41.9 (39.4, 44.5) | 33.4 (30.3, 36.8) | 37.9 (33.8, 42.1) | 43.0 (38.7, 47.4) | 47.0 (43.7, 50.2) | 48.3 (44.3, 52.3) |
Notes: Children Q1=≤50.2%; Q2=50.2%–61.2%; Q3=61.2%–70.0%; Q4=70.0%–79.0%; Q5=≥79.0%. Adults Q1=<39.1%; Q2=39.1%–50.2%; Q3=50.6%–60.1%; Q4=60.1%–70.7%; Q5=>70.7%.
Data were weighted to be nationally representative.
For children, education refers to parental/household educational levels. Due to the existing categorization in NHANES 2017–2018 (less than high school, high school graduate or GED or some college, and college graduate and above), authors combined the high school graduate or GED and some college together for previous NHANES cycle 2015–2016.
NHANES, National Health and Nutrition Examination Survey.
The contribution of UPF across quintiles of consumption (% energy) and their relationships with predicted means of AHA and HEI-2015 total and component scores are shown in Table 2 and Appendix Table 4. Among both children and adults, the multivariable-adjusted dietary scores decreased significantly across increasing quintiles of UPF intake. For example, compared with the lowest quintile of UPF consumption in children (<50.2% energy), the multivariable-adjusted score for the highest quintile (>79.0% energy) was −6.22 (95% CI= −7.20, −5.25) lower for the AHA primary score and −9.96 (95% CI= −11.4, −8.50) lower for the AHA secondary score. Among adults, compared with the lowest quintile of UPF consumption (<39.1% energy), the diet score for the highest quintile (>70.7% energy) was −7.24 (95% CI= −8.13, −6.36) lower for the primary AHA and −12.6 (95% CI= −13.8, −11.4) lower for the secondary AHA score. Similar results were found for HEI-2015 scores among both children and adults.
Table 2.
Associations of Quintiles of the Contribution of Ultra-Processed Foods to Total Energy Intake with American Heart Association Dietary Scores Among U.S. Children and Adults, NHANES 2015–2016 and 2017–2018a
| Variable | Regression coefficients (95% CI) | Predicted margins (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q1 | Q2 | Q3 | Q4 | Q5 | |
| Children | ||||||||||
| AHA primary component goals | ||||||||||
| Primary total diet score | 0.0 (ref) | −2.05 (− 3.01, −1.09) | −2 2.97 (− 4.16, −1.79) | −3.82 (− 5.20, −2.44) | −6.22 (− 7.20, −5.25) | 21.6 (20.6, 22.6) | 19.5 (18.7, 20.4) | 18.6(17.8, 19.5) | 17.8 (16.7, 18.8) | 15.4 (14.8, 15.9) |
| Fruits and vegetables | 0.0 (ref) | −0.88 (−1.23, −0.54) | −1.47 (−1.77, −1.16) | −1.67 (−2.11, −1.23) | −2.64 (−3.02, −2.26) | 5.14 (4.78, 5.50) | 4.26 (4.01, 4.51) | 3.68 (3.36, 3.89) | 3.47 (3.19, 3.76) | 2.50 (2.37, 2.63) |
| Whole grain | 0.0 (ref) | −0.01 (−0.42, 0.41) | 0.16 (−0.32, 0.63) | −0.04 (−0.58, 0.50) | −0.58 (−0.96, −0.20) | 2.92 (2.60, 3.24) | 2.91 (2.51, 3.31) | 3.08 (2.75, 3.40) | 2.88 (2.47, 3.29) | 2.34 (2.09, 2.58) |
| Fish and shellfish | 0.0 (ref) | −0.54 (− 0.89, −0.20) | −0.68 (− 1.06, −0.30) | −0.67 (− 1.07, −0.26) | −0.93 (− 1.29, −0.57) | 1.35 (1.04, 1.67) | 0.81 (0.63, 0.99) | 0.67 (0.46, 0.88) | 0.69 (0.44, 0.93) | 0.43 (0.26, 0.59) |
| Sugar-sweetened beverages | 0.0 (ref) | −0.65 (−1.13, −0.18) | −1.18 (−1.71, −0.65) | −1.84 (−2.37, −1.30) | −2.34 (−2.78, −1.90) | 7.99 (7.61, 8.37) | 7.33 (6.97, 7.70) | 6.81 (6.39, 7.22) | 6.15 (5.70, 6.60) | 5.65 (5.17, 6.13) |
| Sodium | 0.0 (ref) | 0.04 (−0.25, 0.32) | 0.20 (−0.13, 0.53) | 0.39 (−0.02, 0.79) | 0.27 (−0.08, 0.62) | 4.20 (3.92, 4.47) | 4.23 (3.97, 4.49) | 4.40 (4.17, 4.62) | 4.58 (4.33, 4.84) | 4.46 (4.28, 4.64) |
| AHA secondary component goals | ||||||||||
| Secondary total diet score | 0.0 (ref) | −3.79 (−5.46, −2.12) | −5.13 (−6.90, −3.36) | −6.52 (−8.39, −4.65) | −9.96 (−11.4, −8.50) | 37.9 (36.5, 39.2) | 34.1 (32.5, 35.7) | 32.8 (31.4, 34.1) | 31.4 (29.9, 32.8) | 27.9 (27.3, 28.6) |
| Nuts, seeds, and legumes | 0.0 (ref) | −0.31 (−0.87, 0.25) | −0.75 (− 1.28, −0.22) | −1.17 (− 1.83, −0.51) | −1.85 (− 2.30, −1.41) | 3.95 (3.56, 4.33) | 3.63 (3.13, 4.14) | 3.19 (2.72, 3.67) | 2.78 (2.27, 3.28) | 2.09 (1.77, 2.42) |
| Processed meat | 0.0 (ref) | −0.87 (− 1.50, −0.23) | −0.95 (− 1.50, −0.39) | −0.81 (− 1.33, −0.29) | −1.22 (− 1.68, −0.76) | 7.88 (7.47, 8.28) | 7.01 (6.50, 7.51) | 6.93 (6.53, 7.33) | 7.06 (6.66, 7.46) | 6.65 (6.25, 7.05) |
| Saturated fat, % energy | 0.0 (ref) | −0.56 (−1.19, 0.07) | −0.46 (−1.07, 0.15) | −0.72 (− 1.28, −0.16) | −0.67 (− 1.21, −0.12) | 4.47 (3.95, 4.99) | 3.91 (3.53, 4.29) | 4.01 (3.65, 4.38) | 3.75 (3.47, 4.03) | 3.81 (3.58, 4.03) |
| Adults | ||||||||||
| AHA primary component goals | ||||||||||
| Primary total diet score | 0.0 (ref) | −1.99 (−2.73, −1.25) | −3.60 (−4.47, −2.72) | −5.29 (−6.28, −4.30) | −7.24 (−8.13, −6.36) | 23.6 (22.9, 24.3) | 21.6 (21.0, 22.2) | 20.0 (19.2, 20.8) | 18.3 (17.4, 19.2) | 16.3 (15.6, 17.1) |
| Fruits and vegetables | 0.0 (ref) | −0.91 (− 1.17, −0.64) | −1.37 (− 1.71, −1.02) | −1.86 (−2.18, −1.53) | −2.61 (−2.90, −2.31) | 5.89 (5.62, 6.16) | 4.99 (4.77, 5.21) | 4.53 (4.27, 4.78) | 4.04 (3.74, 4.33) | 3.29 (3.08, 3.49) |
| Whole grain | 0.0 (ref) | −0.08 (−0.46, 0.30) | −0.10 (−0.50, 0.30) | −0.36 (−0.69, −0.02) | −0.49 (−0.80, −0.18) | 2.81 (2.51, 3.11) | 2.73 (2.50, 2.96) | 2.71 (2.42, 2.99) | 2.45 (2.17, 2.74) | 2.32 (2.01, 2.63) |
| Fish and shellfish | 0.0 (ref) | −0.29 (−0.63, 0.05) | −0.78 (− 1.16, −0.40) | −0.70 (− 1.22, −0.18) | −1.39 (− 1.94, −0.84) | 2.47 (2.11, 2.83) | 2.18 (1.85, 2.51) | 1.69 (1.38, 2.0) | 1.77 (1.35, 2.19) | 1.08 (0.80, 1.36) |
| Sugar-sweetened beverages | 0.0 (ref) | −0.78 (− 1.14, −0.43) | −1.38 (− 1.77, −0.98) | −2.47 (− 2.95, −1.99) | −2.93 (− 3.35, −2.51) | 8.52 (8.23, 8.81) | 7.74 (7.46, 8.02) | 7.15 (6.78, 7.51) | 6.05 (5.57, 6.53) | 5.60 (5.23, 5.97) |
| Sodium | 0.0 (ref) | 0.06 (−0.17, 0.29) | 0.03 (−0.22, 0.28) | 0.09 (−0.21, 0.39) | 0.17 (−0.07, 0.41) | 3.88 (3.73, 4.04) | 3.95 (3.72, 4.17) | 3.92 (3.73, 4.10) | 3.98 (3.73, 4.22) | 4.06 (3.85, 4.26) |
| AHA secondary component goals | ||||||||||
| Secondary total diet score | 0.0 (ref) | −4.09 (− 5.12, −3.08) | −6.91 (− 8.13, −5.69) | −9.92 (− 11.3, −8.55) | −12.6 (− 13.8, −11.4) | 42.6 (41.7, 43.6) | 38.5 (37.6, 39.5) | 35.7 (34.6, 36.9) | 32.7 (31.5, 33.9) | 30.0 (29.1, 31.0) |
| Nuts, seeds, and legumes | 0.0 (ref) | −0.30 (−0.73, 12.9) | −1.01 (−1.45, −0.58) | −1.42 (−1.89, −0.96) | −2.12 (−2.62, −1.62) | 5.40 (5.02, 5.78) | 5.10 (4.74, 5.46) | 4.39 (4.01, 4.77) | 3.98 (3.58, 4.37) | 3.27 (3.02, 3.54) |
| Processed meat | 0.0 (ref) | −0.65 (− 1.03, −0.27) | −1.09 (− 1.55, −0.63) | −1.70 (− 2.18, −1.22) | −1.66 (− 2.11, −1.21) | 8.06 (7.78, 8.34) | 7.41 (7.12, 7.69) | 6.97 (6.62, 7.32) | 6.36 (5.92, 6.79) | 6.40 (6.04, 6.76) |
| Saturated fat, % energy | 0.0 (ref) | −1.15 (− 1.56, −0.74) | −1.21 (− 1.59, −0.83) | −1.50 (−1.92, −1.08) | −1.57 (− 1.93, −1.20) | 5.60 (5.29, 5.92) | 4.45 (4.16, 4.75) | 4.39 (4.16, 4.62) | 4.10 (3.86, 4.35) | 4.04 (3.80, 4.27) |
Data were weighted to be nationally representative, and adjusted for age, sex (male, female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and others), education (less than high school, high school graduate or GED, some college, or college graduate or above), ratio of family income to poverty (<1.30, 1.30–1.849, 1.85–2.99, and ≥3.0), and BMI categories (underweight, normal weight, overweight, and obese). Individuals with missing data on education (n=242 for children, n=10 for adults) and income (n=461 for children, n=1,038 for adults) were excluded.
NHANES, National Health and Nutrition Examination Survey.
Relatively large differences by quintiles of the contribution of UPF (% energy) were observed among diet scores for fruits and vegetables, SSBs, nuts/seeds/legumes, refined grains, and added sugars (Tables 2, Appendix Table 4). For example, among children, compared with the lowest quintile of UPF consumption, the multivariable-adjusted added sugar score for progressively higher quintiles was −1.02 (95% CI= −1.24, −0.79), −2.06 (95% CI= −2.36, −1.76), −2.64 (95% CI= −2.99, −2.30), and −3.20 (95% CI= −3.48, −2.91).
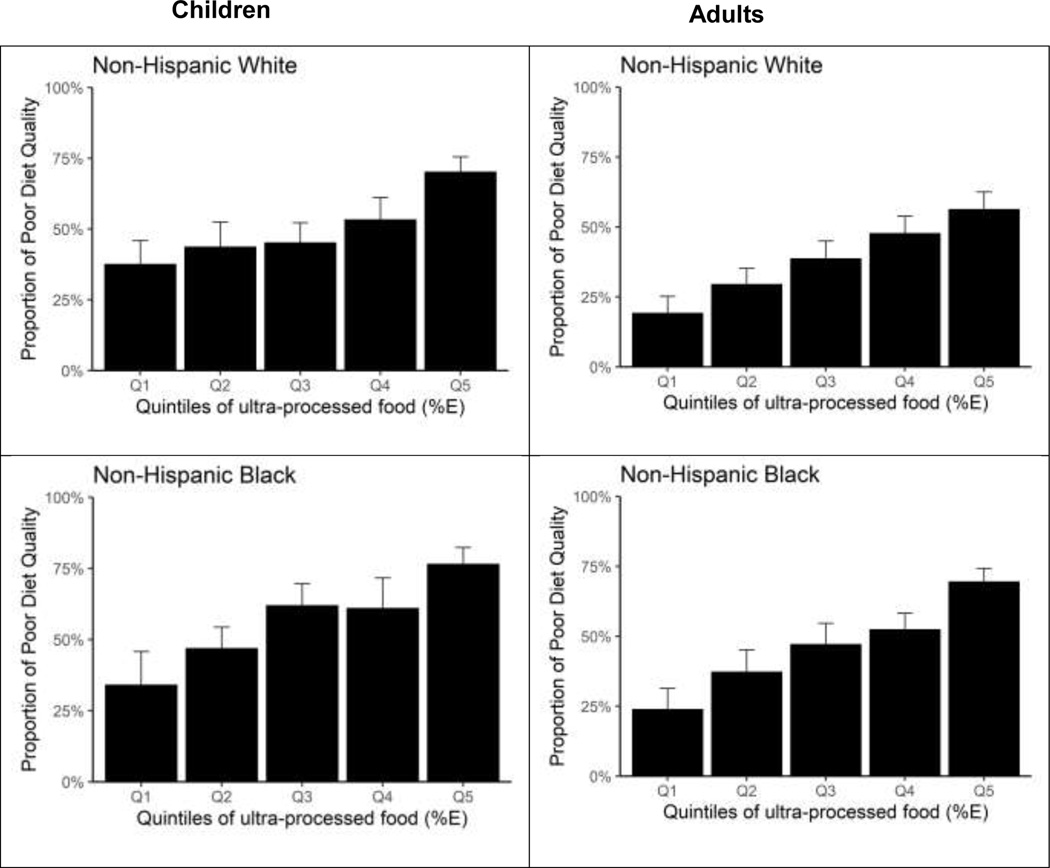
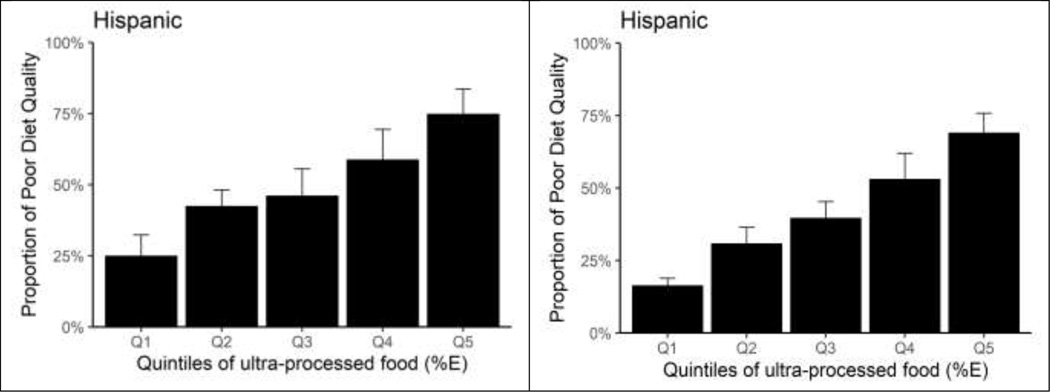
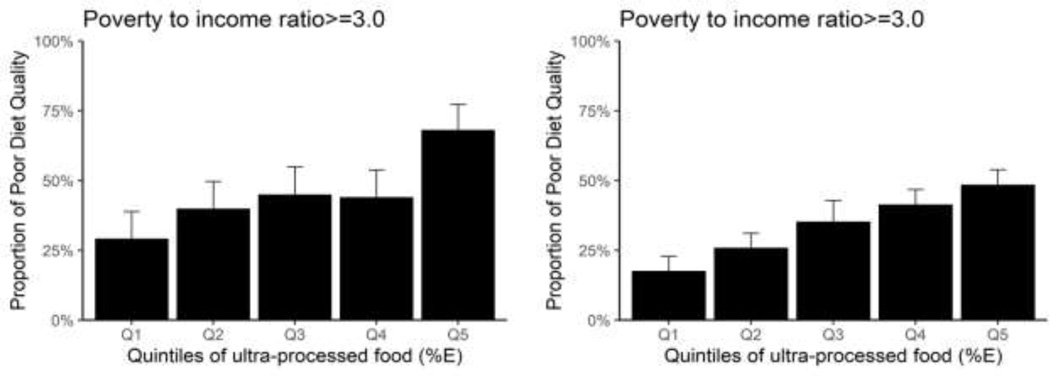
This study also examined the association of UPF with poor diet quality, characterized by <40% adherence to the AHA secondary diet score. The ORs and predicted margins (standardized prevalence) across quintiles of the contribution of UPF (% energy) are shown in Appendix Table 5. After adjustment for covariates, both children and adults consuming higher UPFs had significantly higher odds of having poor diet quality. The estimated proportions of children having poor diet quality almost doubled across quintiles, increasing from 31.3% of children (95% CI=26.2%, 36.5%) in the lowest, 43.9% (95%CI= 38.2%, 49.5%) in the second, 47.8% (95%CI=42.2%, 53.3%) in the third, 55.9% (95%CI=50.2%, 61.7%) and up to 71.6% (95% CI=68.1%, 75.1%) in the highest quintile (Appendix Figure 3). The predicted proportions of adults having poor diet quality were 18.1% (95% CI=14.3%, 22.0%) for the lowest, 29.4% (95% CI=25.7%, 33.0%) for the second, 38.9% (95% CI=34.0%, 43.8%) for the third, 47.8% (95% CI=43.1%, 52.4%) for the fourth, and 59.7% (95% CI=55.3%, 64.1%) for the highest quintile (Appendix Figure 3).
The progressive magnitudes of associations were similar across quintiles of UPF intake by sociodemographic subgroups but were more pronounced among minorities, lower education and household income levels, and higher BMI levels (Figures 1–2, Appendix Table 5). For example, the predicted proportions of adults in low-income household (ratio to the federal poverty level <1.30) having poor diet quality were 22.9% (95% CI=15.4%, 30.4%) for the lowest, 35.4% (95% CI=29.4%, 41.5%) for the second, 45.6% (95% CI=37.7%, 53.5%) for the third, 57.1% (95% CI=49.9%, 64.4%) for the fourth, and 72.6% (95% CI=67.0%, 78.3%) for the highest quintile. The corresponding values among adults in high-income household (ratio to the federal poverty level ≥3.0) were 17.6% (95% CI=12.4%, 22.9%) for the lowest, 25.9% (95% CI=20.7%, 31.1%) for the second, 35.3% (95% CI=27.7%, 42.9%) for the third, 41.4% (95% CI=35.9%, 46.8%) for the fourth, and 48.5% (95% CI=43.1%, 53.9%) for the highest quintile.
Figure 1.
Predicted marginal proportions of poor diet quality across quintiles of ultra-processed food consumption (%E) among U.S. children (aged 2–19 years) and adults (aged ≥20 years) by race/ethnicity, NHANES 2015–2018.
Notes: Data were adjusted for NHANES survey weights to be nationally representative. Error bars indicate 95% CIs.
NHANES, National Health and Nutrition Examination Survey.
Figure 2.
Predicted marginal proportions of poor diet quality across quintiles of ultra-processed food consumption (%E) among U.S. children (aged 2–19 years) and adults (aged ≥20 years) by household income, NHANES 2015–2018.
Notes: Data were adjusted for NHANES survey weights to be nationally representative. Error bars indicate 95% CIs.
NHANES, National Health and Nutrition Examination Survey.
The multivariable-adjusted associations of the contribution of UPFs (% energy) with major food groups and nutrients were additionally shown for children and adults (Appendix Figure 4 and Appendix Tables 6–7). The consumption of healthy foods such as fruits, vegetables, nuts/seeds, and fish significantly decreased with increasing consumption of UPFs. For example, among adults, the predicted marginal mean intake for total fruits were 1.28 (95% CI=1.17, 1.40), 1.02 (95% CI=0.91, 1.12), 0.88 (95% CI=0.79, 0.97), 0.76 (95% CI=0.67, 0.85), and 0.55 (95% CI=0.50, 0.60) servings/day corresponding to the quintiles. Similar differences were observed among children. On the other hand, consumption patterns for unhealthy foods such as refined grains, SSBs, and added sugar were reversed. For example, among adults, the predicted marginal mean intake for SSBs was 0.58 (95% CI=0.44, 0.72), 0.76 (95% CI=0.66, 0.85), 0.97 (95% CI=0.86, 1.08), 1.30 (95% CI=1.13, 1.47), and 1.73 (95% CI=1.54, 1.93) servings/day corresponding to the quintiles.
DISCUSSION
Using nationally representative data, this study assessed the relationships of UPF consumption with overall dietary quality and major food groups/nutrients among both U.S. children and adults. The findings provide strong evidence that higher UPF consumption is associated with poor diet quality. Across quintiles of UPF consumption, the percentage of children with a poor-quality diet rose from 31.3% to 71.6%, and from 18.1% to 59.7% among adults. Among dietary components relatively large differences were found across quintiles of UPF consumption for added sugars, SSBs, refined grains, fruits and vegetables, and nuts/seeds/legumes. To the authors’ knowledge, this is the first study to examine the relationship of UPF consumption with overall diet quality scores, component scores, and major food groups/nutrients among children and adults, separately.
This study suggests that as consumed calories from UPFs increases, consumption of healthy foods progressively decreased while that of unhealthy food progressively increased. The percentage of children and adults having poor diet quality doubled from the lowest quintile to the highest quintile of UPF consumption. Similar differences were observed in food groups and nutrients. These findings not only reflect the differences associated with percentage calories contributed by UPFs but also provide opportunities and strategic targets on reducing UPF intake and improving diet quality.
The findings also provide insightful knowledge on disparities in diet quality associated with UPF intake by population subgroups. For example, by race/ethnicity, the proportions of adults having poor diet quality tripled among non-Hispanic Whites and Blacks while the corresponding proportion quadrupled among Hispanics from the lowest to the highest quintile of UPF consumption. Similar differences were observed by household income levels, education levels, and BMI levels. These results may provide additional information about efficient and cost-effective interventional strategies on subgroups to reduce poor diet and promote healthy diet equity.
Juul et al.19 analyzed U.S. grocery purchasing data from the National Household Food Acquisition and Purchase Survey 2012–2013 and observed that households purchasing the most UPFs (>67.9% energy) scored 10.7 points lower on the HEI-2015 than those purchasing the least (<48.4% energy) (p<0.001) and were furthest from meeting the 2015–2020 Dietary Guidelines for Americans for total fruits, whole fruits, total vegetables, greens and beans total protein food, seafood and plant protein, refined grains, sodium, and added sugars except whole grains. The present investigation builds upon and extends these prior results by assessing individual dietary consumption (rather than household-level food purchases) and foods from all sources (rather than only grocery stores). Though largely consistent with these results, in this study, whole grain scores decreased with UPF consumption in both children and adults, dairy scores decreased with UPF consumption among children, and fatty acid ratio and saturated fats scores decreased among adults. Using data from the 2000–2012 Nielsen Homescan Panel, Poti and colleagues33 observed that >90% of highly processed household-level food purchases exceeded saturated fat, sugar, and sodium 2010 Dietary Guidelines for Americans recommendations.
The findings are consistent with prior studies from Brazil, Chile, Mexico, Colombia, France, the United Kingdom, Australia, and Canada showing that increases in the dietary share of UPFs are associated with lower nutritional quality.17,28–33 Furthermore, the nutritional quality in those studies was evaluated based on either individual nutrient such as free sugars; total, saturated, and trans fats; sodium; fiber; potassium; and protein or nutrient-derived profiles such as a nutrient-balanced-pattern Principal Component Analysis factor score. In addition, prior studies included both children and adults as a whole sample. This study provides important information about differences in the association of contribution of UPFs (% energy) with poor diet quality, separately for children and adults. Concerns regarding the increased share of UPFs in diets have led to various policy actions to discourage consumption of UPFs and promote freshly prepared meals. For example, avoidance of UPFs is a central component of recent national dietary guidelines issued in Brazil, Uruguay, Israel, and Peru.34,35 France has set the goal of reducing UPF consumption by 20% between 2018 and 2021 in their public health nutritional policy.36 Policy actions to reduce the consumption of unhealthy processed foods include a junk food tax implemented in Mexico and Hungry,37 and “black box” warning labels on packaged foods that contain high levels of added sugars, added salt, and added saturated fat in Chile and Mexico.38,39
Several studies have investigated and supported the positive association of UPFs with adverse health outcomes. For example, large prospective cohort studies carried out in France, Spain, Brazil, and U.S. suggested that an increased proportion of UPFs in the diet is associated with a higher risk of total mortality, obesity, hypertension, cardiovascular disease, diabetes, and cancer.5–8,10–12,40,41 A randomized trial conducted by NIH researchers showed that, over 2 weeks, higher UPF consumption led to increased intake of calories and weight gain, compared with unprocessed or minimally processed foods, even when the overall meals were designed to be well matched for energy density, fat, protein, carbohydrate, sugar, sodium, and fiber.15 This study suggested that limiting consumption of UPFs may be an effective strategy for obesity prevention and treatment.
Strengths of this study include use of a nationally representative sample, assessment of different validated dietary quality scores, and use of NOVA classification, the most widely studied system to characterize food processing. The largely food-based AHA scores are also more easily incorporated into public messages and therefore have utility for public health.
Limitations
First, self-reported dietary information is subject to error, owing to memory and reporting bias leading to inaccurate individual food, nutrient, and energy (especially absolute) estimates.42 Yet, interview-administered 24-hour recalls using a computer-assisted personal interview system were used, and results were further adjusted for total energy, each of which reduce measurement error. Also, diet recalls account and weight for days of the week to provide unbiased population average estimates. Second, no single gold standard is established to assess overall diet quality. However, this study assessed both AHA and HEI-2015 diet scores, both of which have been validated against clinical outcomes, and the general patterns for each were similar across quintiles of UPF. Third, reporting bias where people may under-report consumption of less-healthy processed foods may lead to an underestimation of UPF consumption. Fourth, although NHANES collects considerable information on different foods, these data are not consistently determined for all food items and may also not incorporate all brand names or updated, market-representative nutrient information, which could lead to overestimation or underestimation of UPF. Inaccuracies can also arise for mixed dishes, for which Food and Nutrient Database for Dietary Studies uses standard recipes based on assumptions about the types and quantities of ingredients consumed when respondents are unable to provide this information, or does not disaggregate some homemade recipes.43 In this analysis, all food items were classified independently by 2 researchers, reducing the chances of classification errors; and in cases of doubt, most food items were classified conservatively (as non-ultra-processed), which could lead to UPF underestimation.4
CONCLUSIONS
Higher consumption of UPFs is associated with substantially lower diet quality in the U.S. among both adults and children.
Supplementary Material
ACKNOWLEDGMENTS
This research was supported by a postdoctoral fellowship award (17POST33670808) from the American Heart Association (Dr. Liu), NIH (NHLBI R01 HL 130735, Principal Investigator [PI] Micha; R01HL141427, PI Li; R01HL115189-02, PI Mozaffarian), the São Paulo Research Foundation (Processo 2018/17972-9- Dr. Martinez Steele; Processo 2015/14900-9- Prof. Monteiro), and 2R01HL115189 PI Mozaffarian. The funding agencies did not contribute to design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
All authors report support from NIH grants during the conduct of the study. In addition, Dr. Micha reports research funding from Unilever and personal fees from the World Bank and Bunge; Dr. Mozaffarian reports research funding from NIH, the Gates Foundation, and the Rockefeller Foundation; personal fees from Acasti Pharma, America’s Test Kitchen, Barilla, Cleveland Clinic Foundation, Danone, GOED, and Motif FoodWorks; scientific advisory board, Beren Therapeutics, Brightseed, Calibrate, DayTwo (ended 6/20), Elysium Health, Filtricine, Foodome, HumanCo, January Inc., Perfect Day, Season, and Tiny Organics; and chapter royalties from UpToDate; all outside the submitted work.
Footnotes
DM and JXL contributed to study planning. JXL conducted data analyses and drafted the manuscript. EM contributed to analysis and manuscript development. All authors read, revised, and approved the final manuscript.
Data described in the manuscript, code book, and analytic code will be made available pending e-mail request to the corresponding author.
REFERENCES
- 1.Monteiro CA, Cannon G, Levy RB, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019;22(5):936–941. 10.1017/s1368980018003762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayton A, Ibrahim A. The dramatic rise of ultra-processed foods. BMJ. 2019;366:l4970. 10.1136/bmj.l4970. [DOI] [PubMed] [Google Scholar]
- 3.Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14(suppl 2):21–28. 10.1111/obr.12107. [DOI] [PubMed] [Google Scholar]
- 4.Martinez Steele E, Baraldi LG, Louzada ML, Moubarac JC, Mozaffarian D, Monteiro CA. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. BMJ Open. 2016;6(3):e009892. 10.1136/bmjopen-2015-009892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blanco-Rojo R, Sandoval-Insausti H, Lopez-Garcia E, et al. Consumption of ultra-processed foods and mortality: a national prospective cohort in Spain. Mayo Clin Proc. 2019;94(11):2178–2188. 10.1016/j.mayocp.2019.03.035. [DOI] [PubMed] [Google Scholar]
- 6.Rico-Campa A, Martinez-Gonzalez MA, Alvarez-Alvarez I, et al. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ. 2019;365:l1949. 10.1136/bmj.l1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schnabel L, Kesse-Guyot E, Alles B, et al. Association between ultraprocessed food consumption and risk of mortality among middle-aged adults in France. JAMA Intern Med. 2019;179(4):490–498. 10.1001/jamainternmed.2018.7289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim H, Hu EA, Rebholz CM. Ultra-processed food intake and mortality in the USA: results from the Third National Health and Nutrition Examination Survey (NHANES III, 1988–1994). Public Health Nutr. 2019;22(10):1777–1785. 10.1017/s1368980018003890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Askari M, Heshmati J, Shahinfar H, Tripathi N, Daneshzad E. Ultra-processed food and the risk of overweight and obesity: a systematic review and meta-analysis of observational studies. Int J Obes (Lond). 2020;44(10):2080–2091. 10.1038/s41366-020-00650-z. [DOI] [PubMed] [Google Scholar]
- 10.Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultraprocessed food consumption and risk of type 2 diabetes among participants of the NutriNet-Sante Prospective Cohort. JAMA Intern Med. 2020;180(2):283–291. 10.1001/jamainternmed.2019.5942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Sante). BMJ. 2019;365:l1451. 10.1136/bmj.l1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiolet T, Srour B, Sellem L, et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Sante prospective cohort. BMJ. 2018;360:k322. 10.1136/bmj.k322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen X, Zhang Z, Yang H, et al. Consumption of ultra-processed foods and health outcomes: a systematic review of epidemiological studies. Nutr J. 2020;19(1):86. 10.1186/s12937-020-00604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021;125(3):308–318. 10.1017/s0007114520002688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall KD, Ayuketah A, Brychta R, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 2019;30(1):67–77.e3. 10.1016/j.cmet.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martinez Steele E, Popkin BM, Swinburn B, Monteiro CA. The share of ultra-processed foods and the overall nutritional quality of diets in the US: evidence from a nationally representative cross-sectional study. Popul Health Metr. 2017;15(1):6. 10.1186/s12963-017-0119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moubarac JC, Batal M, Louzada ML, Martinez Steele E, Monteiro CA. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite. 2017;108:512–520. 10.1016/j.appet.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Vandevijvere S, De Ridder K, Fiolet T, Bel S, Tafforeau J. Consumption of ultra-processed food products and diet quality among children, adolescents and adults in Belgium. Eur J Nutr. 2019;58(8):3267–3278. 10.1007/s00394-018-1870-3. [DOI] [PubMed] [Google Scholar]
- 19.Juul F, Simoes BDS, Litvak J, et al. Processing level and diet quality of the US grocery cart: is there an association? Public Health Nutr. 2019;22(13):2357–2366. 10.1017/s1368980019001344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics. NHANES survey methods and analytic guidelines. Published 2018. [Google Scholar]
- 21.Centers for Disease Control and Prevention. Information about dietary variables in National Health and Nutrition Examination Survey. https://wwwn.cdc.gov/nchs/nhanes/tutorials/default.aspx. Accessed March 17, 2020.
- 22.Juul F, Martinez-Steele E, Parekh N, Monteiro CA, Chang VW. Ultra-processed food consumption and excess weight among US adults. Br J Nutr. 2018;120(1):90–100. 10.1017/s0007114518001046. [DOI] [PubMed] [Google Scholar]
- 23.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics−−2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. 10.1161/cir.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 24.Reedy J, Lerman JL, Krebs-Smith SM, et al. Evaluation of the Healthy Eating Index-2015. J Acad Nutr Diet. 2018;118(9):1622–1633. 10.1016/j.jand.2018.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. 10.1161/circulationaha.109.192703. [DOI] [PubMed] [Google Scholar]
- 26.Micha R, Penalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912–924. 10.1001/jama.2017.0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Center for Health Statistics. National Health and Nutrition Examination Survey. 2015–2016 Data Documentation, Codebook, and Frequencies. https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/DEMO_I.htm#INDFMPIR. Accessed August 8, 2020.
- 28.Rauber F, da Costa Louzada ML, Steele EM, Millett C, Monteiro CA, Levy RB. Ultra-processed food consumption and chronic non-communicable diseases-related dietary nutrient profile in the UK (2008–2014). Nutrients. 2018;10(5):587. 10.3390/nu10050587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Louzada M, Ricardo CZ, Steele EM, Levy RB, Cannon G, Monteiro CA. The share of ultra-processed foods determines the overall nutritional quality of diets in Brazil. Public Health Nutr. 2018;21(1):94–102. 10.1017/s1368980017001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cediel G, Reyes M, da Costa Louzada ML, et al. Ultra-processed foods and added sugars in the Chilean diet (2010). Public Health Nutr. 2018;21(1):125–133. 10.1017/s1368980017001161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Machado PP, Steele EM, Levy RB, et al. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: evidence from a nationally representative cross-sectional study. BMJ Open. 2019;9(8):e029544. 10.1136/bmjopen-2019-029544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marron-Ponce JA, Flores M, Cediel G, Monteiro CA, Batis C. Associations between consumption of ultra-processed foods and intake of nutrients related to chronic non-communicable diseases in Mexico. J Acad Nutr Diet. 2019;119(11):1852–1865. 10.1016/j.jand.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 33.Parra DC, da Costa-Louzada ML, Moubarac JC, et al. Association between ultra-processed food consumption and the nutrient profile of the Colombian diet in 2005. Salud Publica Mex. 2019;61(2):147–154. 10.21149/9038. [DOI] [PubMed] [Google Scholar]
- 34.Monteiro CA, Cannon G, Moubarac JC, et al. Dietary guidelines to nourish humanity and the planet in the twenty-first century. A blueprint from Brazil. Public Health Nutr. 2015;18(13):2311–2322. 10.1017/s1368980015002165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The Israeli Ministry of Health, 2019. Nutritional Recommendations. https://health.gov.il/PublicationsFiles/dietary%20guidelines%20EN.pdf. Accessed November 19, 2020.
- 36.Haut Conseil de la Santé Publique. Avis relatifaux objectifs quantifiés pour la politique nutritionnelle de santé publique (PNNS) 2018–2022. https://www.hcsp.fr/Explore.cgi/avisrapportsdomaine?clefr=648. Accessed August 28, 2020.
- 37.Pomeranz JL, Wilde P, Huang Y, Micha R, Mozaffarian D. Legal and administrative feasibility of a federal junk food and sugar-sweetened beverage tax to improve diet. Am J Public Health. 2018;108(2):203–209. 10.2105/ajph.2017.304159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corvalan C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: update on the Chilean law of food labelling and advertising. Obes Rev. 2019;20(3):367–374. 10.1111/obr.12802. [DOI] [PubMed] [Google Scholar]
- 39.Gómez FR, Velasco AT. Norma oficial Mexicana nom-051-scfi/ssa1–2010, especificaciones generales de etiquetado para alimentos y bebidas no alcoholicas preenvasados-informacion comercial y sanitaria. [Google Scholar]
- 40.Mendonca RD, Pimenta AM, Gea A, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr. 2016;104(5):1433–1440. 10.3945/ajcn.116.135004. [DOI] [PubMed] [Google Scholar]
- 41.Mendonca RD, Lopes AC, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad de Navarra Project. Am J Hypertens. 2017;30(4):358–366. 10.1093/ajh/hpw137. [DOI] [PubMed] [Google Scholar]
- 42.Thompson FE, Subar AF. Dietary assessment methodology. In: Coulston AM, Boushey CJ, Ferruzzi MG, Delahanty LM, eds. Nutrition in the Prevention and Treatment of Disease. 4th edition. Academic Press; 2017:5–48. 10.1016/b978-0-12802928-2.00001-1. [DOI] [Google Scholar]
- 43.U.S. Department of Agriculture, Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies 2017–2018. Food Surveys Research Group. https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/. Published 2018. Accessed September 20, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.