Abstract
Background
Enterotoxigenic Escherichia coli (ETEC) is one of the top aetiologic agents of diarrhea in children under the age of 5 in low-middle income countries (LMICs). The lack of point of care diagnostic tools for routine ETEC diagnosis results in limited data regarding the actual burden and epidemiology in the endemic areas. We evaluated performance of the novel Rapid LAMP based Diagnostic Test (RLDT) for detection of ETEC in stool as a point of care diagnostic assay in a resource-limited setting.
Methods
We conducted a cross-sectional study of 324 randomly selected stool samples from children under 5 presenting with moderate to severe diarrhea (MSD). The samples were collected between November 2012 to September 2013 at selected health facilities in Zambia. The RLDT was evaluated by targeting three ETEC toxin genes [heat labile toxin (LT) and heat stable toxins (STh and STp)]. Quantitative PCR was used as the “gold standard” to evaluate the diagnostic sensitivity and specificity of RLDT for detection of ETEC. We additionally described the prevalence and seasonality of ETEC.
Results
The study included 324 participants, 50.6% of which were female. The overall prevalence of ETEC was 19.8% by qPCR and 19.4% by RLDT. The children between 12 to 59 months had the highest prevalence of 22%. The study determined ETEC toxin distribution was LT 28/321(9%), ST 18/321(6%) and LT/ST 16/321(5%). The sensitivity and specificity of the RLDT compared to qPCR using a Ct 35 as the cut-off, were 90.7% and 97.5% for LT, 85.2% and 99.3% for STh and 100% and 99.7% for STp, respectively.
Conclusion
The results of this study suggest that RLDT is sufficiently sensitive and specific and easy to implement in the endemic countries. Being rapid and simple, the RLDT also presents as an attractive tool for point-of-care testing at the health facilities and laboratories in the resource-limited settings.
Author summary
ETEC is one of the top causes of diarrheal diseases in low and middle income countries. The advancement of molecular diagnosis has made it possible to accurately detect ETEC in endemic areas. However, the complexity, infrastructure and cost implication of these tests has made it a challenge to routinely incorporate them in health facilities in endemic settings. The ETEC RLDT is a simple and cost-effective molecular tool that can be used to screen for ETEC in resource limited settings. Here, we described the performance of the RLDT against a qPCR as the gold standard. Our findings showed that the ETEC RLDT performs comparable to the qPCR and would be a suitable screening tool in health facilities in recourse limited settings.
Introduction
Enterotoxigenic Escherichia coli (ETEC) is one of the top ten causes of diarrhea [1] with an estimated 75 million diarrhea episodes annually in children under the age of 5 years. It is also responsible for an estimated 18,700 deaths (9,900–30,659), accounting for ~ 4.2% (2.2–6.8) of total diarrhea-related deaths [2]. Diarrhea is also associated with long-term consequences of poor growth and cognitive development among children [3,4]. The ETEC disease burden estimates are reportedly lower than the actual cases in endemic areas due to limited diagnostic capacity [5]. In low- and middle-income countries (LMICs), diarrhea remains a wet season disease with enteric pathogens like ETEC playing a fundamental role in warmer and wetter summer months [6,7]. It is therefore crucial to understand the seasonality of ETEC in the region to inform policymakers on prevention and control strategies.
To accurately diagnose ETEC, one needs to first culture stool, isolate E. coli colonies and then test if the bacterium produces toxins (LT, STh, and STp) through the use of phenotypic assays such as dot blotting or through the use of conventional PCR. Quantitative PCR (qPCR) is performed with purified DNA from stool; although more sensitive; however its technology dependent and is difficult to perform without well-equipped laboratories [8]. The complex nature of the diagnosis leads to (i) long turnaround time, which in turn promotes presumptive treatment that could lead to Antimicrobial Resistance (AMR) [9,10] (ii) increase in cost and labour needed for the detection of ETEC. These are some of the reasons why ETEC is not routinely tested in resource-limited settings.
The complexity of these diagnostic methods results in the underestimation of the burden of ETEC because countries where the infection is endemic cannot afford the infrastructure and expertise required for this [11]. To develop an effective program for control and prevention, accurate burden data is important [12]. In resource-limited settings, there is a need for a simple, readily available method that can be used to detect ETEC in minimally equipped laboratories and health settings.
Chakraborty et al previously developed a simple diagnostic assay, a Rapid LAMP based Diagnostic Test (RLDT) for detection of ETEC, which is based on Loop mediated Isothermal Amplification (LAMP) [13,14]. The RLDT detects ETEC directly from stool in <1 hour. In this study, we evaluated the RLDT in Zambia compared with qPCR, using previously collected stool samples. We also described the prevalence of ETEC infections among the Zambian children presenting with moderate to severe diarrhea (MSD) as well as asymptomatic cases, at the outpatient clinics.
Materials and methods
Ethics statement
The guardians of the participants in the study gave consent on behalf of the children by filling in consent forms issued in English and Nyanja as these are commonly used languages in Lusaka. An impartial witness was used to interpret for illiterate caregivers and provide a thumbprint signature as evidence of agreement, the impartial witness will attest to the process as being voluntary. For this study, Ethics and regulatory approvals were sought from the University of Zambia Biomedical Research Ethics Committee (UNZABREC) reference number 009–10–18 and the National Health Regulatory Authority (NHRA). Samples were de-identified and given a unique study participant number to maintain confidentiality.
Study design
This was a retrospective study using 324 randomly selected samples from 1500 stored stool samples collected at various health facilities in the Lusaka district of Zambia. These samples were collected between November 2012 to September 2013 from a previous rotavirus vaccine effectiveness study [15]. In which clinical information including diarrhea severity, social demographic data were collected from study participants.
Randomization of stool samples before selection
Statistics were applied to randomly select 324 retrospectively collected samples. This set of samples represented stool samples with equal distribution of sex and under 5 age groups. The statistician also stratified the participant samples with a 2:1 ratio of symptomatic and asymptomatic diarrhea cases.
Laboratory assays
Sample processing, collection and storage
Samples with collected clinical information of moderate to severe diarrhea and asymptomatic representation were sorted, separated and stored at -80°C before testing.
ETEC–RLDT training
A team from the Johns Hopkins University, United States, Baltimore travelled to Zambia to train staff at the Centre for Infectious Diseases Research in Zambia (CIDRZ) on RLDT and quantitative PCR (qPCR) assays in an effort to build laboratory capacity. The RLDT and qPCR training duration lasted 2 weeks and was followed up by evaluation of performance of the staff.
ETEC–RLDT assay
RLDT assays were conducted directly from the frozen stool samples using the RLDT kit as described by Chakraborty et al [13]. In short, samples were added to a sample processing tube with lysis buffer followed by heat lysis. The processed samples were then added to the ETEC RLDT lyophilized reaction tube (LRT) strips. Each strip consisted of 8 tubes, organized as two reaction tubes each for LT, STh and STp genes. One reaction tube was added as the RLDT inhibitor control [14]. The strips were run for 40 minutes in a real time fluorometer reader (Agdia Inc, IN, USA). The results were read as positive/negative by the reader. Although the RLDT is semi-quantitative as described by Chakraborty et al [13] we used the platform qualitatively.
qPCR assay
Nucleic Acid extraction: About 100-150mg of bulk stool were added to SK38 bead tubes (Bertin Technologies, Montigny, France) containing lysis buffer (bioMérieux, Marcy I’Etoile, France). The stool suspension was vortexed for 5 minutes, allowed to stand at room temperature for 10 to 15 minutes, then centrifuged at 14,000 rpm for 2 minutes to pellet stool material. About 200μl of the supernatant were transferred into a nuclease-free 1.5ml microcentrifuge tube for extracting nucleic acid using a QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions.
qPCR Amplification: The 25μl reaction mixtures contained 12.5ul Quantitech SYBR Green Master mix (Qiagen, Hilden, Germany), 1uM primer mix 5ul, PCR grade water 5ul (Invitrogen, USA) and 2.5ul of samples. PCR was carried out for 40 cycles of 95°C for 15s and 60°C for 1 min [16]. qPCR cycling conditions were run on the RotogeneQ platform (Qiagen, Hilden Germany). Cut-off for the determination of ETEC positives was set as Ct35 as was done in previous studies [5, 17]. Each sample was run at a minimum in duplicate, and results were averaged. The ETEC strain H10407 (O78:H11 LT+ STh+ STp+) provided by John Hopkins was used for creation of the standard curve for each run similar to what was described in a previous study [14].
Chakraborty et al previously has established the limit of detection (LOD) of RLDT for ETEC genes LT, STh and STp using stool samples spiked with reference ETEC strain [13, 14]. The LOD was 9x104 CFU/g of stool which corresponds to qPCR Ct of 28.2, 28.6 and 30.07 for LT, STh and STp). Therefore, we also evaluated the performance of the RLDT using this LOD (Ct 28) as the cut-off.
Definitions
Diarrhea (Symptomatic) was defined as the primary caregiver reporting that the child had three or more loose stools within 24 hours.
An asymptomatic case was defined as a child presenting to a health facility with other non-diarrhea complications.
Statistical analysis
A minimum sample size of 324 with an assumed ETEC prevalence of 40.7% [18] produces a two-sided 95% sensitivity confidence interval with a width of 12% when the sample sensitivity is at least 85% and the two-sided 95% specificity confidence interval with a width of 5% when sample specificity is at least 0.95%. Summary statistics for all baseline variables were calculated. Proportions and median (IQR) were used to express categorical and continuous variables where applicable. A Chi-square and fisher exact test were used to determine the association between ETEC positivity and baseline characteristics. Statistical analysis significance was set at p-value <0.05 and data were analysed using Stata version 16.0 (StataCorp LLC, College Station, Texas). The correlation of ETEC monthly positivity frequencies was assessed to determine seasonality (S1 Fig). We also compared the Area Under the Curve (AUC) for the RLDT and qPCR in detecting ETEC using clinical representation (asymptomatic and symptomatic) as a proxy reference. A sample was considered positive for ETEC, when at least one of the ETEC genes, LT, STh or STp was positive. To compare RLDT with qPCR, a Ct value cut-off of 35 was used. Any sample with Ct value of 35 or less by qPCR was considered as true positive. To avoid incorrectly determining some samples to be false positive by RLDT, samples with Ct values greater than 35 detectable by both qPCR and RLDT were also included as true positive. We also compared RLDT with qPCR with the Ct value cut-off of 28.
Results
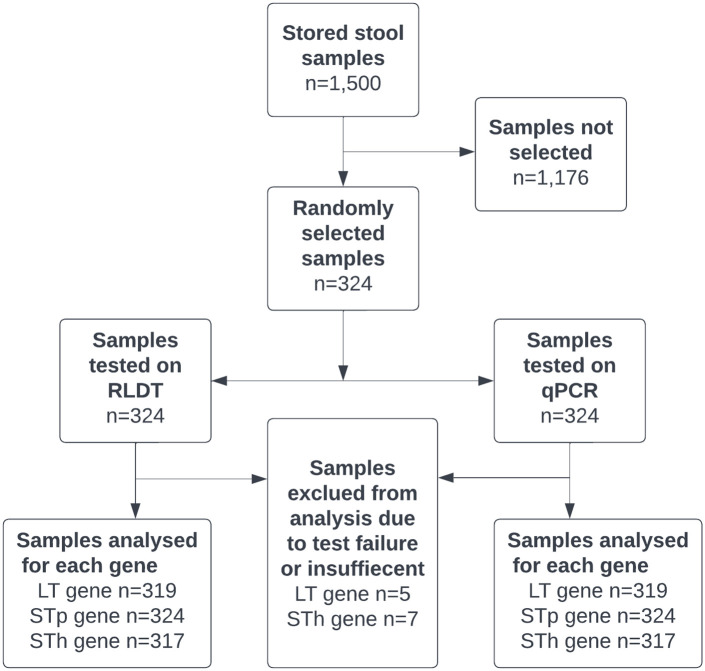
Study design is described in a flow chart
The design of the study is described in the flow chart as shown in Fig 1.
Fig 1. Study participant flow chart.
Note: Samples were excluded from analysis due to either qPCR test failure or the sample was insufficient for repeat DNA extraction.
Social demographics and prevalence
A total of 324 samples with a mean age of about 30months were included in the analysis, 50.9% were female, 28.4% were asymptomatic, with 3.1% of the symptomatic cases presenting with severe disease according to a modified versikari severity score. Overall, ETEC prevalence was about 19% with both the assays, RLDT and qPCR and the highest prevalence was observed in children between 12–59 months of about 22% (Table 1) There was no notable statistically significant difference between baseline characteristics by qPCR and RLDT positivity.
Table 1. Baseline characteristics by qPCR/ RLDT positivity.
| Total samples tested n (%) | Positive by RLDT n (%) | p value | Positive by qPCR n (%) | p value | |
|---|---|---|---|---|---|
| Age | |||||
| <12 months | 159 (49.1) | 26 (16.4) | 0.41 | 26 (16.4) | 0.44 |
| 12–23 months | 37 (11.4) | 9 (24.3) | 8 (21.6) | ||
| 24–59 months | 98 (30.2) | 21 (21.4) | 22 (22.4) | ||
| missing * | 30 (9.3) | 7 (23.3) | 8 (26.7) | ||
| Sex | 63 | 19.75 | |||
| Male | 152 (46.9) | 34 (22.4) | 0.29 | 34 (22.4) | 0.35 |
| Female | 165 (50.9) | 29 (17.6) | 30 (18.2) | ||
| missing * | 7 (2.2) | 0 (0) | 0 (0) | ||
| Symptomatic | |||||
| No | 92(28.4) | 12(13) | 0.07 | 13(14.1) | 0.092 |
| Yes | 227(70.1) | 51(22.5) | 51(22.5) | ||
| missing * | 5(1.5) | 0(0) | 0(0) | ||
| Severity | |||||
| Mild /Moderate | 287 (88.6) | 50 (17.4) | 1.0 1 | 51 (17.8) | 0.70 1 |
| Severe | 10 (3.1) | 1 (10) | 2 (20) | ||
| missing * | 27 (8.3) | 12 (44.4) | 11 (40.7) | ||
| WASH | |||||
| Adequate | 213 (65.7) | 40 (18.8) | 0.15 | 40 (18.8) | 0.70 |
| Inadequate | 62 (19.1) | 11 (17.7) | 13 (21) | ||
| Missing * | 49 (15.1) | 12 (24.5) | 11 (22.4) | ||
| Total | 324 (100) | 63 (19.4) | 64 (19.8) |
NOTE: Chi square test was used to compare the association of baseline characteristics such as age, sex, and Water Sanitation and Hygiene (WASH) data against RLDT and qPCR ETEC positivity.
1 Fishers exact test was used to compare diarrhea severity to the association of the RLDT and qPCR ETEC positivity.
missing* category was not included in the statistical tests; analysis was performed on complete data. P values less than 0.05 show a statistically significant difference.
Performance of the RLDT against qPCR
The performance of the RLDT against qPCR is shown in Table 2. The prevalence of ETEC was 19.8% by qPCR and 19.4% by RLDT. The evaluation of the LT, STh and STp toxin genes sensitivity, specificity, Positive Predictive value (PPV) and Negative Predictive Value (NPV) of the RLDT using a Ct 28 value cut-off with a 95% confidence interval were, 97.3% (85.5–99.9), 96.4% (93.6–98.3), 78.3% (63.6–89.1) and 99.6% (98–100); 95.8% (78.9–99), 99.3% (97.6–99.9), 92% (74–99) and 99.7% (98.1–100); 100% (59.0–100), 99.7% (98.3–100), 87.5% (47.3–99.7) and 100% (98.8–100). Whereas, for evaluation using Ct cut-off 35 sensitivity, specificity, PPV and NPV for the LT, STh and STp toxin genes were, 90.7% (77.9–97.4), 97.5% (94.8–99), 84.8% (71.1–93.7) and 98.5% (96.3–99.6); 85.2% (66.3–95.8), 99.3% (97.5–99.9), 92% (74–99) and 98.6% (96.5–99.6); 100% (59.0–100),99.7% (98.3–100), 87.5% (47.3–99.7) and 100% (98.8–100) respectively.
Table 2. Performance of RLDT against qPCR.
| Ct< = 28** | Number of samples tested | Samples positive by RLDT | Samples positive by qPCR | False positive | False negative | Sensitvity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) |
| LT | 319 | 46 | 37 | 10 | 1 | 97.3(85.5–99.9) | 96.5(93.6–98.3) | 78.3 (63.6–89.1) | 99.6 (98–100) |
| STp | 324 | 8 | 7 | 1 | 0 | 100(59.0–100.0) | 99.7(98.3–100.0) | 87.5 (47.3–99.7) | 100 (98.8–100) |
| STh | 317 | 25 | 24 | 2 | 1 | 95.8(78.9–99.9) | 99.3(97.6–99.9) | 92 (74–99) | 99.7 (98.1–100) |
| Ct< = 35** | Number of samples tested | Samples positive by RLDT | Samples positive by qPCR | False positive | False negative | Sensitivity (95% CI) | Specificity(95%CI) | PPV 95% CI | NPV 95% CI |
| LT | 319 | 46 | 43 | 7 | 4 | 90.7 (77.9–97.4) | 97.5 (94.8–99.0) | 84.8(71.1–93.7) | 98.5(96.3–99.6) |
| STp | 324 | 8 | 7 | 1 | 0 | 100(59.0–100.0) | 99.7 (98.3–100.0) | 87.5(47.3–99.7) | 100(98.8–100) |
| STh | 317 | 25 | 27 | 2 | 4 | 85.2 (66.3–95.8) | 99.3 (97.5–99.9) | 92(74–99) | 98.6(96.5–99.6) |
Note: 28** a Ct value cut-off for both qPCR and the ETEC RLDT, CI = Confidence Interval, 35** a Ct value cut-off for both qPCR and the ETEC RLDT, CI = Confidence Interval
Performance of RLDT against qPCR by the clinical representation and AUC analysis
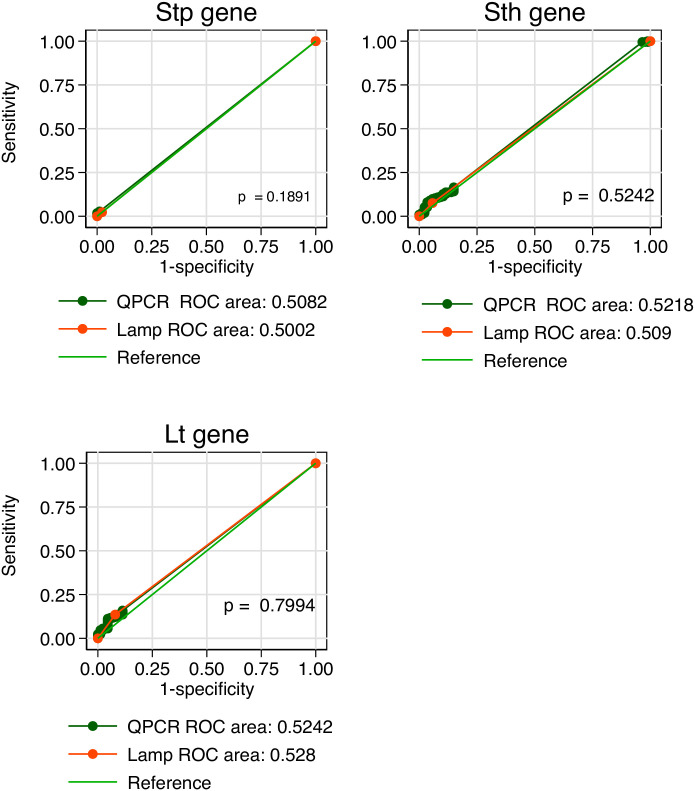
The performance of the RLDT against qPCR by the participants’ clinical representation is shown in Table 3. The evaluation of symptomatic participants of the LT, STh and STp toxin genes sensitivity, specificity, PPV and NPV of the RLDT using the Ct value cut-off of 35 with a 95% confidence interval was 91.4% (76.9–99.7), 96.8% (93.2–98.8),84.2% (68.7–94) and 98.4% (95.4–99.7); 85.7% (63.7–97.0), 99% (96.5–99.9), 90% (68.3–98.8) and 98.5% (95.7–99.7); 100% (54.1–100), 100% (98.3–100), 100% (54.1–100) and 100% (98.3–100) respectively. Similar results observed when asymptomatic cases were evaluated for sensitivity, specificity, PPV and NPV of LT, STh and STp 87.5% (47.4–99.7), 98.8% (93.5–100), 87.5% (47.3–99.7) and 98.8% (93.5–100); 83.3% (35.9–99.6), 100% (95.8–100), 100% (47.8–100) and 98.8% (93.7–100); 100% (2.5–100), 98.9% (94–100), 50% (1.3–98.7) and 100% (96–100) respectively. We compared the Area Under the Curve (AUC) for the RLDT and qPCR in detecting ETEC using clinical representation (asymptomatic and symptomatic) as a proxy reference, we found there was no significant difference between the performance of the RLDT to qPCR (Fig 2).
Table 3. Performance of RLDT against qPCR by the clinical state of participants.
| Ct< = 35** | Clinical Status | Number of samples tested | Samples positive by RLDT | Samples positive by qPCR | False positive | False negative | Sensitivity (95%CI) | Specificity (95%CI) | PPV (95% CI) | NPV (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| LT | ||||||||||
| Asymptomatic | 92 | 8 | 8 | 1 | 1 | 87.5(47.4–99.7) | 98.8(93.5–100) | 87.5(47.3–99.7) | 98.8(93.5–100) | |
| Symptomatic | 224 | 38 | 35 | 6 | 3 | 91.4(76.9–98.2) | 96.8(93.2–98.8) | 84.2(68.7–94) | 98.4(95.4–99.7) | |
| STp | ||||||||||
| Asymptomatic | 92 | 2 | 1 | 1 | 0 | 100.0(2.5–100.0) | 98.9(94.0–100.0) | 50(1.3–98.7) | 100(96–100) | |
| Symptomatic | 227 | 6 | 6 | 0 | 0 | 100 (54.1–100.0) | 100.0(98.3–100.0) | 100(54.1–100) | 100(98.3–100) | |
| STh | ||||||||||
| Asymptomatic | 91 | 5 | 6 | 0 | 1 | 83.3(35.9–99.6) | 100(95.8–100.0) | 100(47.8–100) | 98.8(93.7–100) | |
| Symptomatic | 223 | 20 | 21 | 2 | 3 | 85.7(63.7–97.0) | 99.0 (96.5–99.9) | 90(68.3–98.8) | 98.5(95.7–99.7) |
Note: 35** a Ct value cut-off for both qPCR and the ETEC RLDT, CI = Confidence Interval
Fig 2. Comparison of RLDT to qPCR tests for each gene using AUC analysis.
Note: *Statistical significance (p < 0.05).
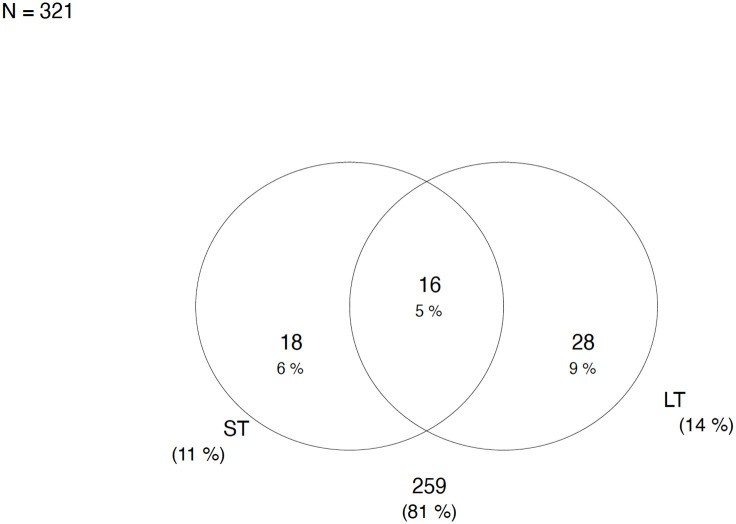
ETEC toxin gene distribution
ETEC with the presence of heat Labile toxin (LT) had a frequency of 44/321 (14%) being the dominant gene. Followed by 34/321 (11%) strains presenting with only the Heat stable toxin (ST) genes. The frequency of ETEC with the combination of both LT/ST toxins was 16/321 (5%) as shown in Fig 3.
Fig 3. Shows the distribution of ETEC toxins.
Seasonality
We observed a seasonal trend of ETEC over 12 months with high positivity rates between December to February (warm, rainy season) and a minor peak between April and May (dry season) (S1 Fig).
Discussion
This study is the first field evaluation of ETEC RLDT and establishes that it performed equally as the qPCR, as demonstrated by the specificity, sensitivity, PPV, NPV and AUC curves for each toxin gene LT, STh and STp. The performance of the RLDT was similar among ETEC positive diarrhea and asymptomatic cases. These findings are important as they support the use of the RLDT for screening for ETEC among children presenting with diarrhea at health facilities. In addition, its turnaround time and simplicity (not requiring skilled laboratory personnel for testing and results interpretation) makes it ideal for resource-limited settings. The RLDT could also be implemented in these countries for ETEC disease surveillance which is crucial to obtain meaningful disease burden data to inform policymakers and healthcare professionals for developing control and prevention programs.
In this study we evaluated the RLDT with the two qPCR Ct cut-offs, Ct35 and Ct28. In the enteric pathogens TaqMan array used in the reanalysis of the GEMS and MALED studies [5, 19], Ct35 was used to analyze the results. The LOD of the ETEC STh gene in the TaqMan array was 105CFU/gm of stool [19] which is same as the LOD of ETEC RLDT assay [13]. It should be noted that the relation of Ct value to CFU/g of stool varies by the qPCR assay chemistry, master mix, assay protocol and the equipment used. Of note, with the TaqMan array in the GEMS study [5], the diarrhea associated quantity for ETEC-STh was found to be Ct value of 26.2 (corresponding to 2.0x107 CFU/g of stool). The LOD of ETEC in the RLDT assay was approximately 2 logs lower than the diarrhea associated quantity defined in the above study. As demonstrated in this study, RLDT is enough sensitive to detect ETEC diarrhea cases and clinically relevant asymptomatic cases.
We determined that across the stratified age groups, the children between 12 to 59 months were at the highest risk of getting ETEC infection with prevalence of ~ 22%. The overall prevalence of ETEC under 5 years old, in this study was ~19%. The isolation rates of ETEC in our study is similar to previous studies that have reported the prevalence of ETEC in developing countries from Bangladesh, Turkey, Peru, Mexico, Egypt, Argentina, India, Nicaragua, and Tunisia which indicated a rate of 18–38% in children [20–24]. However, the ETEC prevalence in our study was lower than what was reported in a previous study (40.7%) conducted in Zambia [18] using Luminex Magpix GPP panel which uses x-TAG technology. This could be attributed to the different in testing platforms, technology and sensitivity of the assays.
The seasonal prevalence observed in our study is similar to what was reported in Kenya [25] which reported the seasonal variation of enteric bacterial pathogens among the hospitalized children with diarrhea. ETEC infections were found all year round with an increase during the warm rainy season and dry seasons. [25]. This information is critical to inform policymakers and healthcare professionals to develop control and prevention programs including when to deploy the ETEC vaccines.
We also found that in Lusaka, Zambia, among the circulating ETEC strains, the LT-ETEC strains was the highest followed by ST-ETEC and LT+ST-ETEC strains. The least detected ETEC strains were STp-ETEC. A similar distribution of toxin genes among ETEC strains was reported from Bolivia (LT 70%, LT+STh 23% and STh 7%) [26]. Michelo et al, also reported similar results, LT+STh being the most common toxin combination and LT+STh+STp being the least common in Zambia [27]. This suggests that vaccines such as ETVAX could be effective for this population and region.
Strengths
This study has several strengths firstly the results of this study were obtained from samples that were collected from several health facilities across the city of Lusaka, which means that our findings can be generalized across Lusaka Province. In addition, this study included symptomatic and asymptomatic cases that were stratified by age. This sampling method accounted for some biases in the computation of the true prevalence. We conducted qPCR assays with samples run in duplicate using average Ct values increasing the accuracy of the study results. This study’s novelty evaluates the ETEC RLDT platform, demonstrating a successful set-up in a resource-limited setting, which is comparable to qPCR.
Limitations
This study has a couple of limitations which include but are not limited to the cross-sectional design only provides prevalence data but does not provide incidence data, which is critical for vaccine trial design and planning control and prevention efforts.
The two assays qPCR and RLDT, compared here, used different sample preparation methods. RLDT was done directly from the stool with minimum sample treatment; qPCR was done from purified DNA; Therefore, the sensitivity of these assays depends not only on the amplification technology but also on the starting material. In addition, while qPCR is quantitative, RLDT is semi-quantitative and was used qualitatively. This study was only carried out in outpatient health facilities but it would be good to evaluate the performance of the RLDT assay in an in-patient facility where there are more severe cases. The RLDT although useful in the diagnostic laboratory is not yet commercially available, however this data will contribute to the commercialization of the assay.
Conclusion
We found that the RLDT performed comparable to the qPCR assay. Additionally, the observed specificity and sensitivity are high enough to suggest that the RLDT could be used in a field setting to rapidly detect ETEC among patients presenting with diarrhea in the health facilities. This study justifies a broader application of the RLDT as a simple and rapid diagnostic test for ETEC in the endemic countries where such simple assays are critically needed. We also determined that LT-ETEC and ST-ETEC strains were highly prevalent and ETEC positivity was highest in the warm rainy season.
Supporting information
(DOCX)
Acknowledgments
We thank all clinical, data, and laboratory staff at the Centre for Infectious Disease Research in Zambia for their contributions to this work. We also acknowledge the training and material contributions from the Johns Hopkins University in Baltimore, USA.
Data Availability
Data cannot be shared publicly because confidentiality of study participants is paramount. Data are available from the Centre for Infectious Disease Research in Zambia (CIDRZ) Institutional Data Access / Ethics Committee (contact via info@cidrz.org) for researchers who meet the criteria for access to confidential data.
Funding Statement
MS,SC, GD were awarded funding from the BactiVac global bacterial vaccinology network grant # BVNCP-11. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Troeger C, Blacker BF, Khalil IA, Rao PC, Cao S, Zimsen SR, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Infectious Diseases. 2018;18: 1211–1228. doi: 10.1016/S1473-3099(18)30362-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khalil IA, Troeger C, Blacker BF, Rao PC, Brown A, Atherly DE, et al. Morbidity and mortality due to shigella and enterotoxigenic Escherichia coli diarrhoea: the Global Burden of Disease Study 1990–2016. The Lancet Infectious Diseases. 2018;18: 1229–1240. doi: 10.1016/S1473-3099(18)30475-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khalil I, Walker R, Porter CK, Muhib F, Chilengi R, Cravioto A, et al. Enterotoxigenic Escherichia coli (ETEC) vaccines: Priority activities to enable product development, licensure, and global access. Vaccine. 2021. doi: 10.1016/j.vaccine.2021.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson JD, Bagamian KH, Muhib F, Amaya MP, Laytner LA, Wierzba T, et al. Burden of enterotoxigenic Escherichia coli and shigella non-fatal diarrhoeal infections in 79 low-income and lower middle-income countries: a modelling analysis. The Lancet Global Health. 2019;7: e321–e330. doi: 10.1016/S2214-109X(18)30483-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu J, Platts-Mills JA, Juma J, Kabir F, Nkeze J, Okoi C, et al. Use of quantitative molecular diagnostic methods to identify causes of diarrhoea in children: a reanalysis of the GEMS case-control study. The Lancet. 2016;388: 1291–1301. doi: 10.1016/S0140-6736(16)31529-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levine MM, Kotloff KL, Nataro JP, Muhsen K. The Global Enteric Multicenter Study (GEMS): Impetus, rationale, and genesis. Clinical Infectious Diseases. 2012;55. doi: 10.1093/cid/cis761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paredes-Paredes M, Okhuysen PC, Flores J, Mohamed JA, Padda RS, Gonzalez-Estrada A, et al. Seasonality of diarrheagenic escherichia coli pathotypes in the US students acquiring diarrhea in Mexico. Journal of Travel Medicine. 2011;18: 121–125. doi: 10.1111/j.1708-8305.2010.00488.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Croxen MA, Law RJ, Scholz R, Keeney KM, Wlodarska M, Finlay BB. Recent advances in understanding enteric pathogenic Escherichia coli. Clinical microbiology reviews. 2013;26: 822–880. doi: 10.1128/CMR.00022-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tribble DR. Resistant pathogens as causes of traveller’s diarrhea globally and impact(s) on treatment failure and recommendations. Journal of travel medicine. 2017;24: S6–S12. doi: 10.1093/jtm/taw090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bokhary H, Pangesti KNA, Rashid H, Abd El Ghany M, Hill-Cawthorne GA. Travel-Related Antimicrobial Resistance: A Systematic Review. Tropical Medicine and Infectious Disease. 2021;6: 11. doi: 10.3390/tropicalmed6010011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lanata CF, Black RE. Estimating the true burden of an enteric pathogen: enterotoxigenic Escherichia coli and Shigella spp. The Lancet Infectious diseases. 2018;18: 1165–1166. doi: 10.1016/S1473-3099(18)30546-2 [DOI] [PubMed] [Google Scholar]
- 12.Fleckenstein JM, Kuhlmann FM. Enterotoxigenic Escherichia coli Infections. Current infectious disease reports. 2019;21: 9. doi: 10.1007/s11908-019-0665-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chakraborty S, Connor S, Velagic M. Development of a simple, rapid, and sensitive diagnostic assay for enterotoxigenic E. coli and Shigella spp applicable to endemic countries. PLOS Neglected Tropical Diseases. 2022;16: e0010180. doi: 10.1371/journal.pntd.0010180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Connor S, Velagic M, Zhang X, Johura F-T, Chowdhury G, Mukhopadhyay AK, et al. Evaluation of a simple, rapid and field-adapted diagnostic assay for enterotoxigenic E. coli and Shigella. PLOS Neglected Tropical Diseases. 2022;16: e0010192. doi: 10.1371/journal.pntd.0010192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beres LK, Tate JE, Njobvu L, Chibwe B, Rudd C, Guffey MB, et al. A Preliminary Assessment of Rotavirus Vaccine Effectiveness in Zambia. Clinical Infectious Diseases. 2016;62: S175–S182. doi: 10.1093/cid/civ1206 [DOI] [PubMed] [Google Scholar]
- 16.Bölin I, Wiklund G, Qadri F, Torres O, Bourgeois AL, Savarino S, et al. Enterotoxigenic Escherichia coli with STh and STp genotypes is associated with diarrhea both in children in areas of endemicity and in travelers. Journal of Clinical Microbiology. 2006;44: 3872–3877. doi: 10.1128/JCM.00790-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu J, Silapong S, Jeanwattanalert P, Lertsehtakarn P, Bodhidatta L, Swierczewski B, et al. Multiplex real time PCR panels to identify fourteen colonization factors of enterotoxigenic Escherichia coli (ETEC). Galdiero M, editor. PLoS ONE. 2017;12: e0176882. doi: 10.1371/journal.pone.0176882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chisenga CC, Bosomprah S, Laban NM, Mwila-Kazimbaya K, Mwaba J. Aetiology of Diarrhoea in Children under Five in Zambia Detected Using Luminex xTAG Gastrointestinal Pathogen Panel. Pediatric Infect Dis. 2018;3: 8. doi: 10.21767/2573-0282.100064 [DOI] [Google Scholar]
- 19.Liu J, Gratz J, Amour C, Kibiki G, Becker S, Janaki L, et al. A Laboratory-Developed TaqMan Array Card for Simultaneous Detection of 19 Enteropathogens. J Clin Microbiol. 2013;51: 472–480. doi: 10.1128/JCM.02658-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qadri F, Svennerholm A-M, Faruque ASG, Sack RB. Enterotoxigenic Escherichia coli in developing countries: epidemiology, microbiology, clinical features, treatment, and prevention. Clinical microbiology reviews. 2005;18: 465–483. doi: 10.1128/CMR.18.3.465-483.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Gallas N, Bahri O, Bouratbeen A, Ben Haasen A, Ben Aissa R. Etiology of acute diarrhea in children and adults in Tunis, Tunisia, with emphasis on diarrheagenic Escherichia coli: prevalence, phenotyping, and molecular epidemiology. The American journal of tropical medicine and hygiene. 2007;77: 571–582. [PubMed] [Google Scholar]
- 22.Hien BTT, Scheutz F, Cam PD, Serichantalergs O, Huong TT, Thu TM, et al. Diarrheagenic Escherichia coli and Shigella strains isolated from children in a hospital case-control study in Hanoi, Vietnam. Journal of clinical microbiology. 2008/01/03 ed. 2008;46: 996–1004. doi: 10.1128/JCM.01219-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bueris V, Sircili MP, Taddei CR, dos Santos MF, Franzolin MR, Martinez MB, et al. Detection of diarrheagenic Escherichia coli from children with and without diarrhea in Salvador, Bahia, Brazil. Memorias do Instituto Oswaldo Cruz. 2007;102: 839–844. doi: 10.1590/s0074-02762007005000116 [DOI] [PubMed] [Google Scholar]
- 24.Işeri L, Zafer Apan T, Aksoy A, Koç F, Sedef Göçmen J, Nuristani D. The prevalence of enterotoxigenic e. Coli isolated from the stools of children aged 0–10 years with diarrhea in mid-anatolia region, Turkey. Brazilian journal of microbiology: [publication of the Brazilian Society for Microbiology]. 2011;42: 243–247. doi: 10.1590/S1517-83822011000100030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah M, Kathiiko C, Wada A, Odoyo E, Bundi M, Miringu G, et al. Prevalence, seasonal variation, and antibiotic resistance pattern of enteric bacterial pathogens among hospitalized diarrheic children in suburban regions of central Kenya. Tropical Medicine and Health. 2016;44: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodas C, Mamani R, Blanco J, Blanco JE, Wiklund G, Svennerholm AM, et al. Enterotoxins, colonization factors, serotypes and antimicrobial resistance of enterotoxigenic Escherichia coli (ETEC) strains isolated from hospitalized children with diarrhea in Bolivia. Brazilian Journal of Infectious Diseases. 2011;15: 132–137. doi: 10.1016/s1413-8670(11)70158-1 [DOI] [PubMed] [Google Scholar]
- 27.Simuyandi M, Chilengi R, Connor S B, Voeglein J B., Laban N M., Mwila-Kazimbaya K, et al. Enterotoxigenic Escherichia Coli Toxins and Colonization Factors Among Zambian Children Presenting with Moderate to Severe Diarrhea to Selected Health Facilities. Arch Microbiol Immunology. 2019;03. doi: 10.26502/ami.93650039 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Data cannot be shared publicly because confidentiality of study participants is paramount. Data are available from the Centre for Infectious Disease Research in Zambia (CIDRZ) Institutional Data Access / Ethics Committee (contact via info@cidrz.org) for researchers who meet the criteria for access to confidential data.