Abstract
Recent value-based payment reforms in the U.S. called for empirical data on how primary care practices of varying characteristics fund their integrated behavioral health services. To describe payment strategies used by U.S. primary care practices to fund behavioral health integration and compare strategies between practices with and without hospital affiliation.Baseline data were used and collected from 44 practices participating in a cluster-randomized, pragmatic trial of behavioral health integration. Data included practice characteristics and payment strategies—fee-for-service payment, pay-for-performance incentives, grants, and graduate medical education funds. Descriptive and comparative analyses using Fisher’s exact tests and independent T-tests were conducted. The sample had 26 (59.1%) hospital-affiliated (hospital/health system-owned, academic medical centers and hospital-affiliated practices) and 18 (40.9%) non-hospital-affiliated practices (community health centers/federally qualified health centers and privately-owned practices). Most practices (88.6%) received payments through fee-for-service; 63.6% received pay-for-performance incentives; 31.8% received grant funds. Collaborative Care Management billing (CPT) codes were used in six (13.6%) practices. Over half (53.8%) of hospital-affiliated practices funded their behavioral health services through fee-for-service and pay-for-performance incentives only, as opposed to two-thirds (66.7%) of non-hospital-affiliated practices required additional support from grants and/or general medical education funds. Primary care practices support behavioral health integration through diverse payment strategies. More hospital-affiliated practices compared to non-hospital-affiliated practices funded integrated behavioral health services through fee-for-service and pay-for-performance incentives. Practices without hospital affiliation relied on multiple funding streams including grants and/or general medical education funds, suggesting their approach to financial sustainment may be more precarious or challenging, compared to hospital-affiliated practices.
Keywords: Payment models, Value-based care, Integrated care, Behavioral health, Primary care
Implications.
Practice: Primary care practices used multiple combinations of payment strategies to support behavioral health integration, and the approaches varied based on hospital affiliation status.
Policy: Policymakers and payers need to consider more reliable funding arrangements for integrated behavioral health, especially among primary care practices without adequate resources to pursue value-based payment strategies.
Research: Future research should be aimed at examining the impact of different payment strategies on the growth and sustainability of behavioral health integration efforts in primary care over time and patient access to behavioral healthcare and outcomes.
Introduction
The stress and devasting impacts of the COVID-19 pandemic have disproportionately affected patients with comorbid behavioral and physical health conditions [1]. Behavioral health (BH) integration in primary care, where BH providers work within primary care teams to offer patients interventions that are effective with specific mental health, substance use, and medical conditions, is much needed now to improve patient access to BH services, positive experiences of care, health outcomes, and cost [2]. Reimbursement is a common barrier for integrating BH services in primary care [3]. The traditional fee-for-service (FFS) payment model incentivizes providers to focus on volume of services without adequately attending to patient-centered outcomes [4] or allowing for protected time outside of direct patient contact and team consultation, thus limiting the scope of services for whole-person, team-based care. Primary care practices have been seeking alternative ways to develop revenue streams to support integrated BH services [5, 6].
New BH reimbursement options have evolved in the last few years through payment reform and value-based care policy changes. The Collaborative Care (CoCM) billing codes, created by the Centers for Medicare, and Medicaid Services (CMS) in 2017, are now one option to potentially increase the access to effective BH integrated services in primary care for practices that employ psychiatric consultants. These FFS codes allow primary care clinicians to bill for services of a qualified BH care manager and psychiatric consultant related to care management support (i.e., registry tracking and follow-up) and psychiatric consultation with the primary care team outside of patient visits [7]. Separate CoCM codes are available for federally qualified health centers and rural health clinics, and the codes have expanded to use outside of Medicare, though adoption varies by state [8].
Value-based contracting has also begun to offer payment strategies that incentivize integration [9]. Incentive programs based on performance levels have been established in many accountable care organizations and with some insurers, to reward providers who meet quality and cost goals measured by a predetermined set of metrics that include BH, such as depression screening [10]. Capitation involves risk-sharing with providers by providing an all-inclusive payment per enrollee for a defined scope of services, regardless of how much care is provided. These monthly payments may or may not have performance-based components but intend to encourage patient-centered care and integration and coordination of services [11]. These alternative payment strategies have been found to improve process outcomes and reduce mental health/substance use-related utilization and spending [9].
Despite recent promising efforts in developing alternative payment strategies to support BH integration, a paucity of data exists on the adoption of these payment strategies in primary care practices, specifically for BH services or on how adoption varies across different organizational structures. Using a national sample of primary care practices in the United States that volunteered to participate in a randomized trial to improve BH integration, this study sought to describe the payment strategies used by these primary care practices to fund BH integration and compare whether there were differences in funding arrangements between practices that affiliate with hospitals versus those that do not. We hypothesized there would be differences in payment strategies for BH integration between these two types of practices, because practice type and organizational characteristics have been associated with differences in quality improvement and change management [12,13]. The findings would elucidate possible implementation gaps in payment strategies that support BH integration in primary care.
Methods
Setting and sample
In this cross-sectional study, baseline data were used that were collected before the COVID-19 pandemic from a pragmatic, cluster-randomized Integrating Behavioral Health and Primary Care (IBH-PC) trial, which tested a practice-centric quality improvement (QI) intervention aimed at improving integrated behavioral health in a convenience sample of primary care practices across the United States. Practices were recruited if they had (1) at least one primary care provider (PCP) and at least one onsite/co-located behavioral health provider (BHP) employed at 0.5 full-time equivalent (FTE); (2) developed and supported electronic health records access, documentation, and communication functions to include medical and behavioral providers; and (3) at least one BHP eligible to provide services for patients with any insurance plan that makes up 10% or more of the practice site’s annual billings. Details of the trial and recruitment are published elsewhere [14].
Data and variables
Clinic champions (i.e., individuals within the organization who led and motivated others to adopt integrated behavioral health in the clinics [15]) and/or practice managers responded to a survey administered in 2019 to early 2020 to indicate whether their practices used the following payment strategies for funding integrated BH services: fee-for-service (FFS), pay-for-performance (P4P), collaborative care (CoCM) codes, capitation, enhanced FFS (practices get a per-member per month payment for coordinating care and are paid FFS for visits [16]), inclusion in health plan preferred networks, grants, and graduate medical education (GME) funds. Data on the following practice characteristics were collected: type of organization, which we categorized as hospital-affiliated practices (hospital/health system-owned clinics, academic medical centers, and hospital-affiliated clinics) or other practices not affiliated with a hospital (community health centers/federally qualified health centers (CHC/FQHC) and privately-owned practices); specialty of practice (family medicine, internal medicine, or both); geographic region of location; non-profit status; residency training status; size of the patient panel; number of visits in the last 12 months; fraction of adult visit revenue from Medicare; BHP and PCP full-time equivalents; years of BH services offered on site; and degree of BH integration (self-assessed by four staff/providers within each practice using the Practice Integration Profile [17]). The study was approved by the University of Vermont and through other local institutional review boards (IRB) who were not able to defer to University of Vermont’s IRB.
Statistical analysis
Descriptive analyses summarized practice characteristics and overall frequencies of payment strategies. Chi-square tests/Fisher’s exact tests and independent T-tests/Mann-Whitney U tests compared practice characteristics and payment strategies by hospital-affiliated and other practices. Since practices reported using more than one payment strategy, we also compared the three common funding combinations in our sample—FFS and P4P only, FFS and any other types of payment strategies (except grants or GME funds), and any combination with grants and GME funds. Due to a small sample size, our comparisons were not adjusted for covariates. No missing data in this dataset.
Results
The analytic sample included 44 primary care practices. The 26 (59.1%) hospital-affiliated practices included 20 (45.5%) hospital/health system-owned clinics, four (9.1%) academic medical center clinics and two hospital-affiliated clinics (4.5%). The 18 (40.9%) non-hospital-affiliated practices included 14 (31.8%) CHCs/FQHCs and four (9.1%) private practices. The practices were recruited from six geographic regions across the U.S.; eight (18%) practices were in rural areas. More hospital-affiliated practices compared to non-hospital-affiliated practices were non-profit organizations (100% vs. 72.2%, p = .008), included internal medicine providers (26.9% vs. 0%, p = .048) and had GME programs (61.5% vs. 11.1%, p = .001). No other differences in practice characteristics were detected between hospital-affiliated and non-hospital-affiliated practices (see Table 1).
Table 1.
Comparison of practice characteristics between hospital-affiliated and non-hospital-affiliated practices
| Characteristics | Overall (n = 44) | Hospital-affiliated (n = 26) | Non-hospital affiliated (n = 18) | p value 1 | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Practice specialty | .048** | ||||||
| Family medicine | 22 | 50 | 12 | 46.2 | 10 | 55.6 | |
| Internal medicine | 7 | 15.9 | 7 | 26.9 | 0 | 0.0 | |
| Both | 15 | 34.1 | 7 | 26.9 | 8 | 44.4 | |
| Residency training status | .001** | ||||||
| No | 26 | 59.1 | 10 | 38.5 | 16 | 88.9 | |
| Yes | 18 | 40.9 | 16 | 61.5 | 2 | 11.1 | |
| Non-profit | .008** | ||||||
| No | 5 | 11.4 | 0 | 0.0 | 5 | 27.8 | |
| Yes | 39 | 88.6 | 26 | 100.0 | 13 | 72.2 | |
| Geographic region | .065 | ||||||
| Mid Atlantic and Great Lakes | 6 | 13.6 | 5 | 19.2 | 1 | 5.6 | |
| Mountain | 8 | 18.2 | 2 | 7.7 | 6 | 33.3 | |
| New England | 10 | 22.7 | 4 | 15.4 | 6 | 33.3 | |
| Pacific Northwest | 3 | 6.8 | 2 | 7.7 | 1 | 5.6 | |
| The South | 8 | 18.2 | 5 | 19.2 | 3 | 16.7 | |
| West Coast and Hawaii | 9 | 20.5 | 8 | 30.8 | 1 | 5.6 | |
| Mean | Range/SD | Mean | Range/SD | Mean | Range/SD | p value | |
| Baseline BHP FTE | 1.50 | 0.50–6.30 | 1.32 | 0.50–2.80 | 1.76 | 0.60–6.30 | .838 |
| Baseline PCP FTE | 6.02 | 2.00–14.30 | 5.89 | 2.70–10.90 | 6.21 | 2.00–14.30 | .288 |
| Baseline BHP FTE: PCP FTE | 5.40 | 0.80–14.80 | 5.61 | 1.10–12.80 | 5.11 | 0.80–14.80 | .641 |
| Years of BHP services | 6.82 | 0–26.16 | 6.45 | 0–25.00 | 7.36 | 0–26.16 | .672 |
| Visits in the last 12 months | 27297.86 | 19177.69 | 28525.00 | 19679.64 | 25525.33 | 18844.23 | .616 |
| Practice total patient panel size | 9318.95 | 4968.96 | 10455.46 | 4173.35 | 7677.33 | 5657.81 | .068 |
| Fraction of adult revenue from Medicare | .21 | .14 | .21 | .15 | .21 | .14 | .994 |
| Baseline total median PIP | 59.28 | 14.16 | 56.32 | 16.56 | 63.56 | 8.42 | .252 |
BHP behavioral health provider; PCP primary care provider; FTE full-time equivalent; PIP Practice Integration Profile—a measure of degree of behavioral health integration in each practice.
p value determined by Fisher-Freeman-Halton Exact test or independent T-test/Mann-Whitney U test; significance at p < .05.
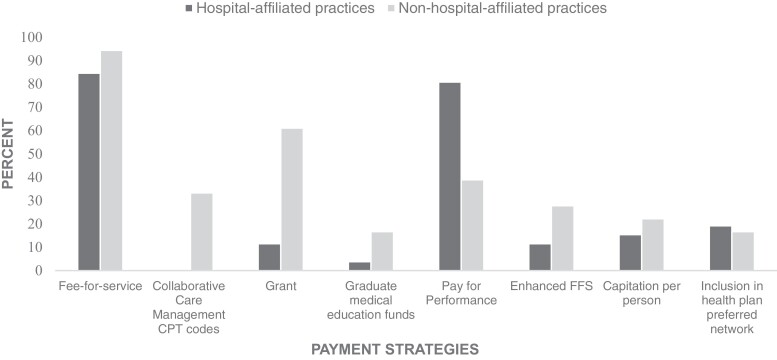
Overall, most (n = 39, 88.6%) practices received FFS payments; nearly two-thirds (n = 28, 63.6%) also received P4P incentives; and about one-third (n = 14, 31.8%) received grants. A fifth (n = 8, 20%) of the practices reported using enhanced FFS, capitation, or were included in a preferred health plan network. Four (9.1%) practices used GME funds. More hospital-affiliated practices funded BH integration via P4P incentives than practices without a hospital affiliation (80.8% vs. 38.9% respectively, p = .01, see Fig. 1). More non-hospital-affiliated practices used grants as compared to hospital-affiliated practices (61.1% vs. 11.5%, p = .001). CoCM codes were used only in six (13.6%) practices, all of which were non-hospital affiliated.
Fig 1.
Comparison of payment strategies between hospital-affiliated (hospital/health system-owned, academic medical, hospital-affiliated) and non-hospital-affiliated (CHC/FQHC and private) practices.
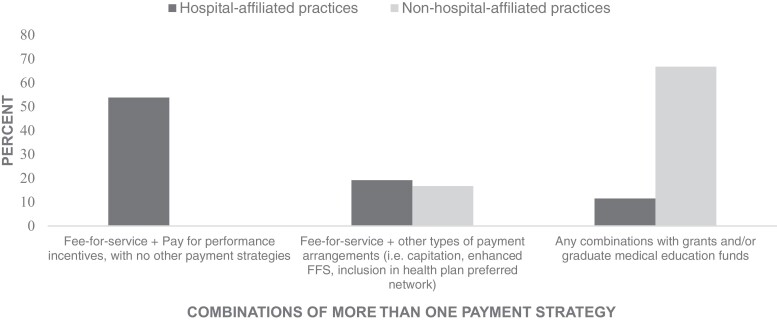
Among practices that used more than one payment strategy (see Fig. 2), over half (53.8%) of the hospital-affiliated practices funded their BH integration through FFS and P4P incentives without other payment strategies, while all the non-hospital-affiliated practices used additional payment strategies outside of FFS and P4P (p < .001). More non-hospital-affiliated practices than hospital-affiliated practices used grants and/or GME funds in addition to other payment strategies (66.7% vs. 11.5%, p < .001). Notably, the CHCs/FQHCs were the dominant practice type in the non-hospital-affiliated group that reported using grants. Among the 10 CHCs/FQHCs that used grants, six also received payments through enhanced FFS, capitation, or inclusion in preferred health plan network, and three practices also used CoCM codes.
Fig 2.
Comparison of three common funding combinations between hospital-affiliated (hospital/health system-owned, academic medical, hospital-affiliated) and non-hospital-affiliated (CHC/FQHC and private) practices in our sample. The second category “Fee-for-service + other types of payment arrangements” does not include pay-for-performance incentives, grants, or graduate medical education funds.
Discussion
The diverse national sample of primary care practices reported multiple combinations of payment strategies to support BH integration, and the approaches varied based on hospital affiliation status. Practices that were affiliated with hospitals or health systems tended to fund their BH integration through the single combination of FFS and performance incentives, which tend to be more stable forms of payment. By contrast, other non-hospital-affiliated practices such as CHCs/FQHCs and private practices relied in part on support from grants and/or GME funds, which are often time-limited and opportunistic forms of payment.
Performance-based incentive programs offer rewards for primary care practices to sustain BH integration. However, the implementation of incentive programs can be challenging, especially for smaller practices that do not have affiliation with a hospital or health system that can provide resources to navigate highly regulated contracting requirements. Previous studies found that the lack of administrative infrastructure and appropriate integration-related performance measures are barriers to implement value-based initiatives [1]. Other studies have found that practices without hospital affiliation reported challenges in contracting negotiations with payers and managed care organizations, because they are not as big as hospitals and do not to have the complex administrative structure required to pursue sophisticated payment strategies like P4P [1]. Also, some performance-based programs have a penalty for practices that do not meet the performance targets, causing potential burden on care providers and practices [18], especially those that have limited resources and are working with disadvantaged and high-risk populations which experience a greater burden of multiple chronic medical and behavioral health conditions [19].
Some U.S. states have taken advantage of the Medicaid 1115 waivers and the State Innovation Models Initiative to implement delivery system reform incentive payment demonstrations that support BH integration [20, 21]. These demonstration programs could allow less resourced practices receive funding for infrastructure investments and services that are foundational to BH integration, project-based incentives for implementing integrated care activities, and performance-based incentives for achieving BH integration objectives and outcomes [22]. Although practices using demonstration programs achieved early success in developing the “building blocks” needed for integrated care, there were persistent challenges due to cumbersome insurance policies and limits on billing practices [22, 23].
CHCs/FQHCs have multiple venues to apply for grants given their status and grants allow these practices to make upfront investment for BH integration. However, the time-limited nature of the funding poses challenges for sustainability and may divert practice resources to grant writing [1]. These results suggest that smaller and potentially less resourced non-hospital affiliated practices could be losing opportunities to transform to value-based initiatives that help BH integration achieve sustainable funding. To help CHCs/FQHCs take advantage of value-based payment systems, states can implement programs that offer health centers flexibility to bill for alternative visits/touches and more provider types, as well as provide upfront funding for infrastructure improvements. Several states such as Oregon, Washington, Illinois, and Minnesota have shown promising results of these programs in improving quality and cost outcomes of integrated care [24]. Other policy changes that could support practices’ ability to participate in value-based payment include providing technical assistance and QI learning collaboratives to support practices through implementation, increasing, and aligning incentives across payment programs to support BH integration, streamlining requirements for billing, and supporting efforts to provide access to specialty behavioral health services [23].
This study has several limitations. Our convenience sample of practices participating in this trial was not large enough to consider covariates, like non-profit status, and availability of GME programs, that may affect how practices choose payment strategies and warrants further studies with larger samples. Although the small sample size may not be generalizable to all practices that have BH integration, the sample included practices from a national sample across diverse organizational structures, serving both rural and urban settings. It is unclear whether the limited use of CoCM codes in this study could be due to few practices using the CoCM model and/or difficulties implementing the CoCM codes. Prior literature has suggested that arduous workflow changes and administrative documentation burden hinder adoption of CoCM codes in clinics that use a CoCM model [6, 25, 26, 8]. The lack of rollout of CoCM codes in hospital- affiliated practices may infer unique barriers to adoption of these codes in larger health systems and this warrants further study.
Implications
Stable financing for BH integration is important to support ongoing sustainability of operations and grow the BH workforce to address the high negative impact of unmet behavioral health needs in primary care. This study found practices used disparate combinations of payment strategies, even among practices that have achieved BH integration as represented in having BH staff onsite and integration of records and workflow. The lack of stable funding for BH integration likely limits other practices from implementing BH integration, particular during times of organizational stress. Future research is needed to understand how payment strategies are associated with the degree of BH integration in practices and patient access to BH integrated care and outcomes [27]. Also, studies are needed to understand both the resources needed to establish funding sources and how potential gaps in funding stifle progression on BH integration in practices. Additionally, QI interventions that target improving BH integration can play a critical role in providing support and coaching to clinics around reimbursement and funding strategies. Our study was part of a pragmatic IBH-PC trial testing a multicomponent QI intervention that in part connected practices with coaches and experts who could address questions related to financing BH integration [14].
Conclusion
Primary care practices in this study used multiple payment strategies to sustain BH integration, which varied based on hospital affiliation status. Namely, non-hospital-affiliated practices tended to use more variable payment strategies that included opportunistic grant funding and organizational based GME funding, both of which may not provide stable funding sources over time as well as FFS and P4P strategies. More studies are needed to explore the impact of using different payment strategies and whether the payment strategies used are adequate to sustain and grow BH integration efforts in practices over time.
Acknowledgements
We would like to extend our gratitude to the 44 practices that participated in the research. We would also like to thank all the researchers, staff and stakeholders for their assistance and support in the IBH-PC trial.
Contributor Information
Kris Pui Kwan Ma, Department of Family Medicine, University of Washington School of Medicine, Seattle, WA, USA.
Brenda L Mollis, Department of Family Medicine, University of Washington School of Medicine, Seattle, WA, USA.
Jennifer Rolfes, Cornerstone Whole Healthcare Organization Inc, Payette, ID, USA.
Margaret Au, Department of Family Medicine, University of Washington School of Medicine, Seattle, WA, USA.
Abigail Crocker, Department of Mathematics and Statistics, University of Vermont, Burlington, VT, USA.
Sarah H Scholle, National Committee for Quality Assurance (NCQA), Washington, DC, USA.
Rodger Kessler, Department of Family Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO, USA.
Laura-Mae Baldwin, Department of Family Medicine, University of Washington School of Medicine, Seattle, WA, USA.
Kari A Stephens, Department of Family Medicine, University of Washington School of Medicine, Seattle, WA, USA.
Funding
This work was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (PCS-1409-24372) and supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under Award Number UL1TR000423. The views, statements, and opinions presented are solely the responsibility of the author(s) and do not necessarily represent the views of PCORI, its Board of Governors or Methodology Committee, or the NIH.
Compliance with Ethical Standards
Conflicts of Interest: Sarah H. Scholle works for the National Committee for Quality Assurance (NCQA), which recognizes practices as patient-centered medical homes and offers a distinction in Behavioral Health integration. Other authors have no competing interest to declare.
Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
Five transparency statements: (1) Study registration: The study was pre-registered at ClinicalTrials.gov NCT02868983 (https://clinicaltrials.gov/ct2/show/NCT02868983). Registered on August 16, 2016. (2) Analytic plan registration: The analysis plan was not formally pre-registered. (3) Availability of data: De-identified data from this study are not available in a public archive. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author. (4) Availability of analytic code: Analytic code used to conduct the analyses presented in this study are not available in a public archive. They may be available by emailing the corresponding author. (5) Availability of materials: Materials used to conduct the study are not publicly available.
References
- 1. Docherty M, Spaeth-Rublee B, Scharf D, et al. How practices can advance the implementation of integrated care in the COVID-19 era.Commonwealth Fund.2020, November. Retrieved January 15, 2022, from https://www.commonwealthfund.org/sites/default/files/2020-11/Pincus_implementing_integrated_care_COVID_era_ib.pdf. [Google Scholar]
- 2. Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;(10). doi: 10.1002/14651858.CD006525.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kathol RG, Butler M, McAlpine DD, Kane RL. Barriers to physical and mental condition integrated service delivery. Psychosom Med. 2010;72(6):511–518. [DOI] [PubMed] [Google Scholar]
- 4. Miller BF, Ross KM, Davis MM, Melek SP, Kathol R, Gordon P. Payment reform in the patient-centered medical home: enabling and sustaining integrated behavioral health care. Am Psychol. 2017;72(1):55–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schwenk TL. Integrated behavioral and primary care: What is the real cost? JAMA 2016;316(8):822. [DOI] [PubMed] [Google Scholar]
- 6. Malâtre-Lansac A, Engel CC, Xenakis L, et al. Factors influencing physician practices’ adoption of behavioral health integration in the United States: a qualitative study. Ann Intern Med. 2020;173(2):92–99. [DOI] [PubMed] [Google Scholar]
- 7. Press MJ, Howe R, Schoenbaum M, Cavanaugh S. Medicare payment for behavioral health integration. N Engl J Med. 2017;376(5):405–407. [DOI] [PubMed] [Google Scholar]
- 8. Raney L. Cracking the codes: State Medicaid approaches to reimbursing psychiatric collaborative care. California Health Care Foundation. 2020, September. Retrieved January 15, 2022, from https://www.chcf.org/wp-content/uploads/2020/09/CrackingCodesMedicaidReimbursingPsychiatricCollaborativeCare.pdf. [Google Scholar]
- 9. Carlo AD, Benson NM, Chu F, Busch AB. Association of alternative payment and delivery models with outcomes for mental health and substance use disorders: a systematic review. JAMA Netw Open. 2020;3(7):Article e207401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bremer RW, Scholle SH, Keyser D, Knox Houtsinger JV, Pincus HA. Pay for performance in behavioral health. Psychiatr Serv. 2008;59(12):1419–1429. [DOI] [PubMed] [Google Scholar]
- 11. Korda H, Eldridge GN. Payment incentives and integrated care delivery: levers for health system reform and cost containment. INQUIRY 2011;48(4):277–287. [DOI] [PubMed] [Google Scholar]
- 12. Lindner S, Solberg LI, Miller WL, et al. Does ownership make a difference in primary care practice? J Am Board Fam Med. 2019;32(3):398–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tirodkar MA, Morton S, Whiting T, et al. There’s more than one way to build a medical home. Am J Manag Care. 2014;20(12):e582–e589. [PubMed] [Google Scholar]
- 14. Crocker, AM, Kessler, R, van Eeghen, C, et al. Integrating behavioral health and primary care (IBH-PC) to improve patient-centered outcomes in adults with multiple chronic medical and behavioral health conditions: Study protocol for a pragmatic cluster-randomized control trial. Trials 2021;22(1):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wood K, Giannopoulos V, Louie E, Baillie A, Uribe G, Lee KS, Haber PSet al. The role of clinical champions in facilitating the use of evidence-based practice in drug and alcohol and mental health settings: a systematic review. Implement Res Pract. 2020;I:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. MACPAC. Provider payment and delivery systems. The Medicaid and CHIP Payment and Access Commission. 2021. Retrieved January 15, 2022, from https://www.macpac.gov/medicaid-101/provider-payment-and-delivery-systems/.
- 17. Kessler RS, Auxier A, Hitt JR, et al. Development and validation of a measure of primary care behavioral health integration. Fam Syst Health. 2016;34(4):342–356. [DOI] [PubMed] [Google Scholar]
- 18. Gavidia, M. Healthcare 2020: a detailed report on the clinical and financial aspects of emerging value-based payment models. American Journal of Managed Care. 2019, October. Retrieved January 15, 2022, from https://www.ajmc.com/view/healthcare-2020-a-detailed-report-on-the-clinical-and-financial-aspects-of-emerging-valuebased-payment-models. [Google Scholar]
- 19. Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389(10077):1475–1490. [DOI] [PubMed] [Google Scholar]
- 20. Medicaid. About Section 1115 demonstrations. U.S. Department of Health and Human Services, Medicaid. n.d.. Retrieved April 15, 2022, from https://www.medicaid.gov/medicaid/section-1115-demonstrations/about-section-1115-demonstrations/index.html. [Google Scholar]
- 21. Centers for Medicare and Medicaid Services. State innovation models initiative: General information. U.S. Department of Health and Human Services, Centers for Medicare and Medicaid Services. 2021, October. Retrieved April 15, 2022, from https://innovation.cms.gov/innovation-models/state-innovations. [PubMed] [Google Scholar]
- 22. Lane K, Baller J, Vogt R, Heeringa J. Promoting physical and behavioral health integration in Medicaid through Section 1115 demonstrations. U.S. Department of Health and Human Services, Medicaid.2020, January. Retrieved April 15, 2022, from https://www.medicaid.gov/medicaid/downloads/promoting-pbhi.pdf. [Google Scholar]
- 23. Goldman ML, Smali E, Richkin T, Pincus HA, Chung H. Implementation of behavioral health integration in small primary care settings: lessons learned and future directions. Community Ment Health J. 2022;58(1):136–144. [DOI] [PubMed] [Google Scholar]
- 24. Howe G, Houston R, McGinnis T. How health centers can improve patient care through value-based payment models. Center for Health Care Strategies. 2020, June. Retrieved April 15, 2022, from https://www.chcs.org/media/HealthCentersImproveCareValueBasedPayment.pdf. [Google Scholar]
- 25. Cross DA, Qin X, Huckfeldt P, Jarosek S, Parsons H, Golberstein E. Use of Medicare’s behavioral health integration service codes in the first two years: an observational study. (2020). J Gen Intern Med. 2020;35(12):3745–3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Carlo AD, Corage Baden A, McCarty RL, Ratzliff ADH. Early health system experiences with collaborative care (CoCM) billing codes: a qualitative study of leadership and support staff. (2019). J Gen Intern Med. 2019;34(10):2150–2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Werner RM, Emanuel E.Pham HH, Navathe AS. The future of value-based payment: Five recommendations to accelerate adoption and transformation. The Leonard Davis Institute of Health Economics and the Healthcare Transformation Institute at the University of Pennsylvania. 2021. Retrieved January 15, 2022 from https://ldi.upenn.edu/sites/default/files/pdf/LDI-HTI-Policy-Brief-Value-Based-Payment-2021.pdf. [Google Scholar]