Abstract
Objectives
uncertainty pervades the complex illness trajectories experienced by older adults with multimorbidity. Uncertainty is experienced by older people, their informal carers and professionals providing care, yet is incompletely understood. We aimed to identify and synthesise systematically the experience of uncertainty in advanced multimorbidity from patient, carer and professional perspectives.
Design
systematic literature review of published and grey qualitative literature from 9 databases (Prospero CRD 42021227480).
Participants
older people with advanced multimorbidity, and informal carers/professionals providing care to this group. Exclusion criteria: early multimorbidity, insufficient focus on uncertainty.
Analysis
weight-of-evidence assessment was used to appraise included articles. We undertook thematic synthesis of multi-perspective experiences and response to uncertainty.
Results
from 4,738 unique search results, we included 44 articles relating to 40 studies. 22 focused on patient experiences of uncertainty (n = 460), 15 on carer experiences (n = 197), and 19 on health professional experiences (n = 490), with 10 exploring multiple perspectives. We identified a shared experience of ‘Total Uncertainty’ across five domains: ‘appraising and managing multiple illnesses’; ‘fragmented care and communication’; ‘feeling overwhelmed’; ‘uncertainty of others’ and ‘continual change’. Participants responded to uncertainty by either active (addressing, avoiding) or passive (accepting) means.
Conclusions
the novel concept of ‘Total Uncertainty’ represents a step change in our understanding of illness experience in advanced multimorbidity. Patients, carers and health professionals experienced uncertainty in similar domains, suggesting a shared understanding is feasible. The domains of total uncertainty form a useful organising framework for health professionals caring for older adults with multimorbidity.
Keywords: uncertainty, multimorbidity, co-morbidity, aged, frail older, attitude to health, carers, health personnel, older people, qualitative
Key Points
Uncertainty pervades patient, carer and health professional experience of multimorbidity among older adults yet is not understood fully.
If addressed poorly, uncertainty can be distressing, with adverse impacts on quality of care and patient experience
In this synthesis, we develop a novel model: total uncertainty, which describes the multi-perspective experience of uncertainty
Importantly, uncertainty is experienced in similar domains by patients, carers and professionals: a shared understanding is possible
The domains of total uncertainty form a useful organising framework for health professionals caring for older adults with multimorbidity, but require further investigation in more diverse populations.
Introduction
Multimorbidity, defined as the presence of multiple chronic illnesses [1], is common and increasing [2], particularly in older people [2, 3], conferring high symptom burden and costs of care [4]. Therefore, it is important to optimise the care of older people with multimorbidity throughout their disease trajectory including at advanced stages [5]. However, the evidence base for management of multimorbidity is lacking, as most studies focus on single diseases [6]. Existing guidelines do not address the complexity of multimorbidity, potentially resulting in poor patient experience, higher healthcare use and overtreatment at the end of life, particularly in high income countries [7–9].
There is a consensus that person-centred, goal-oriented approaches to care are optimal for high quality care in multimorbidity, to ensure that patients and their informal carers are involved in decisions about their care [10–12]. This is particularly important as complexity increases [13], and evidence suggests that the cost saving impact of person-centred approaches such as palliative care increases alongside the number of diagnoses [14]. However, implementation of person-centred care is challenging [15, 16], and trials of such approaches have yet to demonstrate effect on quality of life [17].
This may be because insufficient attention is paid to uncertainty. Multiple uncertainties regarding the illness, care and the future shape experience in advanced illness [18], and can rarely be eliminated in this population [19]. Uncertainty is not always harmful, but if poorly addressed and communicated it can cause considerable distress for all involved [18, 20]. Increasingly, clinical interactions are occurring in the context of extensive uncertainty, and studies exploring the experience of living with multimorbidity identify uncertainty as a key challenge not just for patients, but for informal carers and health professionals as well [21–23]. This is critical because if stakeholders differ in their experience and response to uncertainty, this may contribute to difficulties in negotiating a person-centred plan for care [23, 24], particularly as some struggle to form or express preferences in the context of an uncertain illness trajectory [25].
Person-centred approaches require a shared appraisal of uncertainty, but patients, carers and health professionals do not necessarily experience uncertainty in the same ways or about the same issues. Experiences of uncertainty in the context of multimorbidity have rarely been investigated from different perspectives, nor have patient, carer and health professional experiences been directly compared [26]. We aimed to synthesise evidence regarding the experience of uncertainty in advanced multimorbidity from the perspectives of patients, informal carers and health and social care professionals, specifically focusing on how older people, their informal caregivers, and health and social care professionals experience uncertainty about their care.
Methods
Design
Systematic literature review according to PRISMA guidance with thematic synthesis [27, 28]. The review was prospectively registered on Prospero (CRD 42021227480) where the protocol is available.
Review question
In what ways do older people with advanced multimorbidity, their informal carers, and health and social care professionals experience uncertainty about their illness and care?
Review population and inclusion
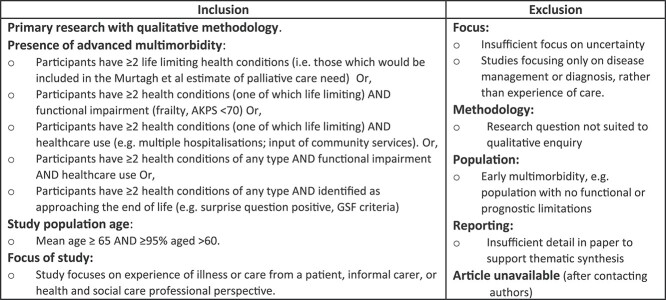
The review population was older people with advanced multimorbidity. We defined advanced multimorbidity as the presence of two or more advanced/life limiting illnesses, in line with previous research [26]. However, this definition is rarely used in practice, so to capture relevant literature, we operationalised the definition as multimorbidity with markers of advanced disease. Because we sought to synthesise insights into the experiences of uncertainty, this review focused on qualitative research, which is more likely to include exploration of experience. We excluded articles with insufficient focus on uncertainty, or where the focus was only on particular aspects of disease or a specific intervention. However we included some articles with a narrower focus (largely on de-prescribing), if they also addressed uncertainty more broadly. See Figure 1 for inclusion and exclusion criteria.
Figure 1.
Inclusion and exclusion criteria [29].
Search
We developed search terms iteratively with the support of a medical librarian (IK) using concepts of (i) older people, their carers and health professionals; (ii) multimorbidity; (iii) experience of illness and uncertainty; (iv) qualitative research (see Supplementary Information for full search strategy). We searched online databases (Medline (Ovid), EMBASE (Ovid), PsycInfo (ProQuest), CINAHL (Ebscohost), SCIE, Web of Science) and grey literature repositories (Opengrey, Dart E-theses, Google Scholar (first 200 results)) [30]. The search was conducted in December 2020, and updated in October 2021. We searched reference and citation lists of relevant review articles and included papers. The search was not limited by language, but we excluded articles if we were unable to procure a translation.
Selection of studies
Search results were de-duplicated, then imported into Rayyan [31]. Screening was by title and abstract (conducted by S.N.E., J.O.L. and J.L.), with 10% double screening. Full text articles were retrieved and each was reviewed by two authors (two of S.E., J.L. and J.O.L.) who independently made inclusion decisions. Disagreements were resolved by discussion. Where there was insufficient information in the paper to make an inclusion decision, the authors of the paper were contacted.
Data extraction
Details of included articles were extracted into a bespoke excel spreadsheet. The full text of the results/findings sections of included papers was imported into NVIVO (version 12 (QSR International (UK) Ltd.) for analysis.
Weight of evidence assessment
Two authors (two of S.E., J.L., J.O.L., S.H.) independently judged what ‘weight’ to give to each piece of included evidence using Gough’s ‘Weight of Evidence’ (WoE) approach. This involves making judgements about A. the methodological quality of the study; B. the review specific quality (appropriateness of methods for the review question), and C. the review relevance (relevance of the findings to the review question). The output of the Gough et al. [32] WoE assessment process is an overall weight (high, medium or low) to be given to that piece of evidence during analysis. Disagreements in weighting were resolved by discussion.
Analysis
We conducted thematic synthesis, coding relevant sections of the results of included articles as qualitative data [28]. We took a mixed deductive/inductive approach, specifying broad areas of analysis deductively based on existing theoretical frameworks, but coding inductively within these areas, and ensuring openness to new areas of analysis not identified in existing theory.
The overarching theoretical framework for analysis was based on the taxonomy of Han et al. [33], and Mishel’s uncertainty in illness theory [34], which we adapted to give a set of high level constructs around which we based our coding (see Supplementary Information for further detail). Early in analysis we identified ‘Response to uncertainty’ as a further area of interest and included this as a separate construct.
We read and re-read the data to familiarise, and then SE coded content relevant to the experience of uncertainty. 8/44 articles were independently double-coded (by J.L. and J.O.L.) and this coding was discussed to ensure consistency of approach. Codes were grouped and themes identified from the groupings. Themes were then named, and checked against the original data to ensure fit. During this process we paid attention to the Weight of Evidence score of each article such that articles with higher scores were given greater weight. A reflexive diary was used during analysis to keep note of progress. We conducted the synthesis in three stages, at each stage revisiting the data to ensure the themes identified fit with the original articles:
Stage 1: Synthesis of patient/carer/professional experience.
Stage 2: Triangulate findings from each perspective to explore similarities and differences.
Stage 3: Build a multi-perspective thematic model of the experience and response to uncertainty.
Ethics
This study did not involve primary data collection; formal ethical approval was not required.
Patient and public involvement
Prior to the main search we consulted a group of people with experience of life limiting illness and of providing care to others with such illnesses. At this initial meeting, patient and public involvement (PPI) representatives highlighted the importance of exploring uncertainty from multiple perspectives, providing the focal point for the review. The PPI group were consulted at intervals throughout the review to provide feedback on the focus and findings. See Supplementary Information for further details and reporting using the GRIPP2 checklist [35].
Results
Of 4,738 unique search results, 260 full texts were retrieved, and we included 44 articles from 40 studies with 1,147 participants (see Figure 2 PRISMA chart). 22 articles explored the patient perspective (n = 460), 15 the carer perspective (n = 197) and 19 were from the perspective of a broad range of healthcare professionals (n = 490). Of these, 10 articles included multiple perspectives.
Figure 2.
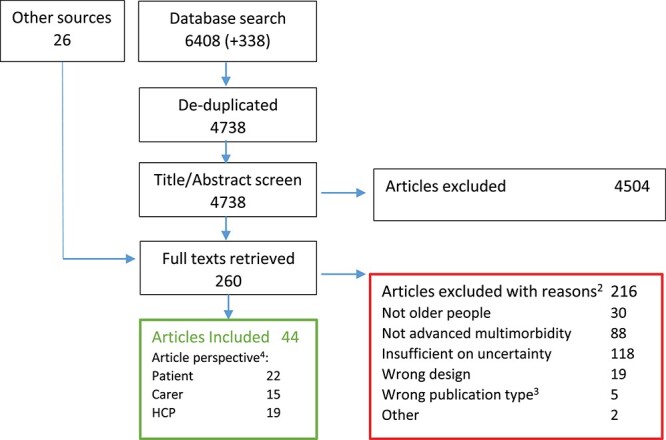
PRISMA chart.
Articles were from Europe (7 countries, n = 23), North America (2 countries, n = 17), Australasia (2, countries n = 4). 27 had an interview design, 7 used focus groups and 10 used other designs including ethnography, observation and mixed-methods. 29 studies were from community or primary care settings: 12 studies involved hospital settings, and 3 were in other settings.
Eleven articles were given high weight of evidence for this review, most of which addressed the patient perspective. Five studies were assigned low weight (four of which concerned healthcare professionals): the remaining 28 were assigned moderate weight. Further details of details of included articles are in the Supplementary Information.
Thematic synthesis
We found that uncertainty exists in relation to five overarching domains that were experienced across all perspectives. Three of these apply within the individual: ‘Appraising and managing multiple illnesses’; ‘Fragmented care and communication’ and ‘Feeling overwhelmed’. ‘Uncertainty of others’ extends beyond the individual to all involved in care. ‘Continual change’ denotes that uncertainty is a construct that changes in focus and intensity over time. Whilst there were differences between patient, carer and healthcare professional focus within these domains, the experience of uncertainty for all perspectives is represented by them. In the subsequent text we illustrate these domains, highlighting experience from each perspective.
Appraising and managing multiple illnesses
Patients, carers and health professionals all experienced uncertainty as they attempted to unpick the complexities of multiple illnesses. They frequently experienced that each additional health condition added an additional layer of complexity to an already complex picture. Patients in particular tended to experience uncertainty regarding the meaning of illness related events or symptoms. They might be uncertain regarding the meaning of a symptom, or what to do about it.
Bearing in mind that all patients had multi- morbidity, it was evident that they were unclear about their different diagnoses and any possible relationship between them. This confusion had a particular impact when participants left the hospital, when they felt they had little guidance about what their symptoms meant, which medicines related to which symptoms/condition, or how to respond to symptoms to avoid a further hospital admission.
Patient perspective [36]
Carers experienced similar uncertainties, but tended to have a more practical focus. A common uncertainty was which of a number of issues was the current main concern or priority for care, with uncertainty about what to do next.
Not only do caregivers make decisions on which of many conditions or symptoms to focus on, but they also consider the fluctuating and often worsening health status of older adults with (Multiple Chronic Conditions) MCC as well as their frequent transitions from home to hospital. The sheer multitude of issues to address as well as the unending changes in care context create a high level of uncertainty for caregivers in setting priorities for care.
Carer perspective [37]
Health professionals’ uncertainties usually coalesced around management decisions or sometimes diagnostic work-up. Professionals were often unsure how best to manage multiple illnesses and came up against situations where there was no ‘right’ answer because what was best for one illness would not help another. Health professionals frequently commented on the absence of an evidence base in multimorbidity, which contributed to uncertainty about treatments and meant they were sometimes making complex treatment decisions with little supporting evidence.
We have frail patients with a lot of co-morbidities to which standard guidelines often do not apply.
Professional Perspective [20]
Fragmented care and communication
Multimorbidity was synonymous with complex care. It was the norm for patients to interact with multiple care providers, and for healthcare professionals to negotiate care plans with colleagues across professional backgrounds. Fragmented care led to uncertainties relating to communication and role function.
The complex older patient is often surrounded with a jumble of professional and informal carers. This can be confusing for the patient and GP.
Professional perspective [38]
Role ambiguity was experienced by all. Patients and carers felt that siloed working, whilst easier for health professionals, did not meet their needs, and were frequently unsure who was responsible for each aspect of their care.
And I’ve always thought of a cardiologist as being a person who doesn’t worry just about your heart pressures but also about the swelling in my feet. … I just found out last fall that he thinks it’s the problem of my family physician. … Anyway, these silos are almost like people are hard-wired into them.
Patient perspective [39]
Professionals themselves, particularly general practitioners (GPs), were ‘stuck in the middle’ of a large number of experts providing single-condition advice and plans. They received conflicting or ambiguous information and were uncertain how to proceed.
In fairness to them, all their letters were bang on ... for COPD: do the sputum, give him the azithromycin, he has the home oxygen — tell him to use that. Everything was according to guidelines. Renal the same, trial this — if this doesn’t work this is what we’re doing — push this as far as we can, nephro-protection and all this, and it’s all bang on target. The same for cardiology. But when you put it in the clinical setting it isn’t working.
Professional perspective [40]
Fragmentation of care systems led to uncertainty because of an inability to access information in a timely fashion, or sometimes at all. This was a particular struggle for carers.
What I have found is accessing information or services or knowing what resources are available is very complex. It is convoluted almost and there are so many people involved that you don’t know where to start.
Carer perspective [41]
Transitions of care were a particular source of uncertainty often due to gaps in communication between services. GPs were frequently left following up patients post-discharge with insufficient information from secondary care. Patients and carers themselves tended to have a poor understanding of the processes surrounding care transitions. As one study of transitions from hospital wards to ‘alternate level of care’ (lower intensity care) services expressed it:
Participants described not knowing about important processes of care. This included not knowing the meaning of “alternate level of care,” the roles of different staff members, processes related to patient isolation, the availability of day passes, or why the patient was being moved.
Patient and carer perspective [42]
Feeling overwhelmed
Uncertainty was experienced at a psychological and existential level. Some patients felt distressed by uncertainty relating to changes in their health, while others experienced an overwhelming whirlwind of illness and care that felt so chaotic that their sense of self was threatened.
For some participants, the impact of uncertainty was overwhelming, resulting in an experience of powerlessness and confusion which did not allow for a presentation during interview, of anything but a patient self.
Patient perspective [43]
Carers watched on and were constantly anxious about whether they were doing the right thing. Some described being unable to ‘turn off’, feeling the need to monitor those they were caring for all the time. They expressed constant worry about the wellbeing of those they were caring for.
Although assuming caring responsibility is a condition of life, it is stressful watching an old parent become ill, frail and dependent and this situation is accompanied by constant concern and uncertainty about the parent's well-being.
Carer perspective [44]
Healthcare professionals were also affected psychologically by uncertainty and some did question their roles or whether they were doing the right thing by patients. Similar to patients, they had a sense of feeling overwhelmed when attempting to manage complex patients, although usually this related to decision making rather than the self as a whole.
Clinicians commented on not knowing where to start and not having an obvious best decision, “There’s a lot of variables to account for. He’s got like 30 things wrong and he’s on a ton of medications.”
Professional perspective [45]
Uncertainty of others
At times participants were aware of uncertainty experienced by others. The uncertainty of others could be experienced in different ways. Some patients noted that professionals and carers were uncertain as to their (the patient’s) ability to function and did not trust their physical abilities. When others were uncertain as to their ability, this tended to affect decisions about care and patients were sometimes side-lined.
Due to health problems, the body is unpredictable and constantly changing. This tends to affect the trust of others in the ability of the persons to live autonomously and prevents participation in decisions that concern themselves.
Patient perspective [46]
Patients and carers also experienced health professional uncertainty. Either due to lack of continuity or perceived lack of expertise, professionals were sometimes seen as uninformed and uncertain about their patient’s needs. Such uncertainty could be perceived as evidence of incompetence, and carers sometimes found themselves in the burdensome role of information providers.
There is no consistency in terms of seeing the same doctor all the time. So many changes, so many different doctors…. Each of them is very considerate but clearly clueless about the uniqueness of the patients. And the whole business of having to re-educate and re-inform each time you go in.
Carer perspective [26]
Professionals noted that patients were sometimes uncertain about their care, the reason for attending appointments, or had a limited grasp of their illnesses. Cognitive impairment was sometimes a factor, but this could also reflect the complexity of their multiple conditions and the healthcare system.
When people have three, four, five different illnesses and particularly where the care is kind of fragmented, under the care of a number of doctors, they’re often not sure what exactly is wrong with them, or what illnesses or diagnoses they have.
Professional perspective [47]
When multiple professionals were involved in care there was also scope for inter-professional uncertainty. This was less usually expressed directly as uncertainty and tended rather to come out in conflicting opinions or advice, sometimes affecting patient experience.
Nurses reported major problems with conflicting advice from different prescribers, leading to patient uncertainty.
Professional perspective [48]
Continual change
The experience of uncertainty was closely intertwined with the course of time and the illness trajectory.
The illness trajectory for patients with advanced illness creates a continuous uncertainty which may predominate or be less acutely experienced depending on circumstances. Other forms of uncertainty are episodic and may relate to symptoms, aspects of care, changes in provision, or decision-making.
Patient perspective [43]
Patients and carers were uncertain what would happen next or how their health would change on a day to day basis. Whilst most patients and carers understood that prognosis was limited, when deterioration occurred this was often unexpected, an uncertainty that could be distressing.
As well as continual uncertainty about prognosis, uncertainty could also occur on a short-term or episodic basis. Some experienced change on a very short timescale and expressed uncertainty as to how they would feel tomorrow or even later that same day. Carers described an experience of constant change, making them uncertain what to focus on at any point
The complexity of living with several simultaneous health problems is that its intensity and impact on daily life can vary from time to time, from day to day but also during the day. “One day I can have more troubles with my legs and one day it is my hands. Other days are different. Sometimes it is better and sometimes it is worse”.
Patient perspective [46]
The unpredictability of some conditions, such as dementia, meant that the caregivers’ focus was constantly changing.
Carer perspective [37]
Health professionals were less buffeted by change but did identify that their clinical practice was affected by the changing nature of chronic conditions. They grappled with the question of when to discuss future care with patients and carers given the unpredictable illness course. More specifically, a treatment plan might be helpful on one day, but might need to change at short notice, for instance in relation to deprescribing.
Even for two seemingly comparable individuals, clinicians might take legitimate actions for, or against, deprescribing depending on subtle differences in patient function, prioritization of inferred or explicit care goals, and likely future trajectory, all of which can change over time between and within individuals.
Professional perspective [49]
Total uncertainty
Taking these domains together, we propose that the multi-perspective experience of uncertainty in advanced multimorbidity can be characterised by a model of ‘Total Uncertainty’ as presented in Figure 3. Total uncertainty represents the experience of uncertainty across all five domains. Each individual may not experience every domain of uncertainty, and the balance and interaction between domains may vary between individuals and over time in ways that require further exploration in subsequent research, but total uncertainty illustrates the sum of experience.
Figure 3.
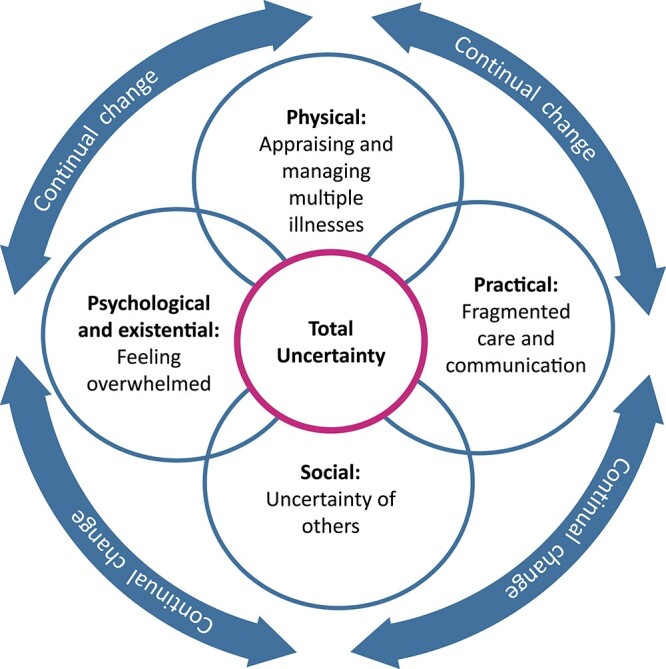
Model of total uncertainty.
Response to uncertainty
Patient, carer and healthcare professional responses to uncertainty were either active, characterised by addressing uncertainty or actively avoiding it, or passive, characterised by accepting uncertainty.
Active responses
Some sought actively to address and manage uncertainty through information seeking, planning ahead or sharing uncertainty. Addressing uncertainty was unusual for patients, to the extent that one study identified a patient doing so as a divergent case. Carers more frequently sought to confront uncertainty by planning ahead for all eventualities. Health professionals often recognised that addressing uncertainty as part of a holistic multidisciplinary approach was helpful. A minority of professionals acted differently, feeling that only they could address uncertainty and therefore taking the burden of decision making on themselves rather than discussing it with patients and carers.
Some GPs felt that patients would be unable to understand the various conflicts and uncertainties faced, and so would ‘just worry about it myself … rather than imparting a huge amount of knowledge’
Professional perspective [40]
Those who felt paralysed or overwhelmed by uncertainty, might seek actively to avoid it. This usually applied to health professionals who avoided areas of uncertainty, focusing only on areas where they were certain, e.g. areas where there was supporting evidence. Alternatively they might defer to other with greater perceived expertise to make decisions where there was uncertainty. This approach was easier to link to evidence, but was not necessarily helpful for patients.
Confidence dealing with uncertainty is required for self-efficacy in deprescribing…. I think, if you are not comfortable in your own skin, in your abilities as a clinician, it is much easier to pay attention or to go along with what the “expert” says. Therefore, you end up building up a list of medicines.
Professional perspective [49].
Passive response
It was common for patients and carers to try to accept or normalise uncertainty as part of their life. This response was most evident in the patient data. A typical response was to focus on the ‘day to day’ and avoid planning ahead for an uncertain future. Some carers expressed acceptance in terms of spiritual coping. Acceptance of uncertainty was unusual for health professionals who usually addressed or avoided it.
“I don’t know, some things you leave to God,” while another said, “I pray.…I was raised that way to ask God—ask Jesus—to help you. You know what’s going to be is going to be but tomorrow may be better.”
Carer perspective [50]
Discussion
This review and synthesis increase our understanding of the experience of uncertainty in advanced multimorbidity, building a bridge between theories of uncertainty, and real life multi-perspective experience. The domains of ‘Total Uncertainty’ provide, for the first time, a clinically applicable model based on empirical data from patient, carer and health professional perspectives, which can be used to approach the construct of uncertainty in this population. We found that uncertainty exists in relation to five domains: ‘appraising and managing multiple illnesses’; ‘fragmented care and communication’; ‘feeling overwhelmed’; ‘uncertainty of others’ and ‘continual change’. By exploring the patient, carer and health professional perspectives together, we were able to demonstrate that uncertainty is experienced in the same domains by these three groups, thus extending theories of uncertainty which have hitherto tended to focus on individual experience [33]. The classification of responses to uncertainty provides a starting point for future clinical interventions.
We undertook an extensive published and grey literature search co-designed with an information specialist. Full text articles were appraised by two reviewers. Meaningful involvement of patients and the public in the review process enabled us to focus on areas deemed important to this population [51]. The analysis used robust qualitative methods underpinned by existing theory to build a novel, clinically relevant model of uncertainty [28, 33, 34]. However, our reliance on an operational definition of advanced multimorbidity led to heterogeneity in terms of the disease stage of participants between studies, meaning that some were more relevant to advanced illnesses than others. This was ameliorated by paying attention to the Weight of Evidence assessment for each article during analysis; less relevant articles were given lower weight. We limited the review to qualitative data and so did not include any insights from quantitative research, as we deemed qualitative research to be best placed to answer the exploratory review question. We did not set out to explore response to uncertainty, rather noted this as an emerging area during analysis, so there may be other relevant data on this topic; however, our findings fit well with what would be expected from relevant theory [34].
We note parallels between the domains of total uncertainty, and the physical, psychological, social, and spiritual domains of Cicely Saunders’ model of total pain [52]. These parallels raise the possibility that total uncertainty may represent a model to underpin the holistic care of those with advanced multimorbidity as total pain has been used in palliative care for advanced cancer [53]. Contrary to expectation, we found that uncertainty is experienced in similar domains by patients, carers and health professionals, though individuals may experience different aspects of uncertainty at different times and we were not able to investigate how the different domains interact. Crucially, this suggests that there is scope for patients, carers and health professionals to develop a shared understanding of the uncertainties in any given situation and apply this understanding to make joint plans for an unpredictable future. Applying the domains of total uncertainty in clinical practice may enable development of this shared understanding and fill a gap in the delivery of person-centred care. A better understanding of uncertainty may also improve tolerance to it, relieving some of the associated distress. However, bringing together the various domains of uncertainty into a single model of total uncertainty should not diminish the importance of addressing each area individually. To address uncertainty fully, clinicians should attend to each of the domains in our model, thinking beyond the uncertainties directly related to illness and care, to the uncertainties that exist beyond the individual and over time.
The question remains as to how to apply this model in practice to improve care. As with complexity, uncertainty can rarely be eliminated and so it is important to address it [54, 55]. Yet promising interventions to address uncertainty directly in advanced illness such as the AMBER care bundle have, to date, been difficult to evaluate [56]. The tendency of some health professionals to avoid uncertainty, reflecting an intolerance to it, may be a target for education interventions [57]. However, despite many decades of research into tolerance of uncertainty [20, 58], it is unclear to what extent education interventions improve patient experience [59]. There are several tools which seek to address specific areas of uncertainty, for example identifying priorities and goals, but optimal communication of uncertainty remains an evidence gap [55, 60]. Our findings indicate that education and training should be a priority because, in agreement with previous studies, we identified that when uncertainty is poorly recognised and addressed by professionals, there is a risk that trusting relationships could break down due to perceived lack of competence [26, 61]. Conversely if uncertainty is shared and considered collaboratively, this may support stronger patient–professional relationships [61, 62]. Understanding more about responses to uncertainty will help to inform targets for future interventions. We were not able to explore relationships between the uncertainties experienced and how they were responded to, but we would hypothesise that there are links between experience of and response to uncertainty. It is also likely that different approaches will be needed for patients or carers who accept uncertainty than for those who actively seek to address it.
There was insufficient evidence to conduct a meaningful synthesis of how uncertainty is addressed during clinical interactions between patients, carers and healthcare. Only one study in our review took this approach, focusing on care planning discussions in primary care [62]. Further investigations of how uncertainty is experienced and responded to within a broad range of clinical interactions could contribute useful information to improve practice and design novel approaches to decision making. For example, if a patient employs an acceptance strategy to uncertainty and a professional is taking an active response what is the outcome? Can and should we try to influence patient strategies to respond to uncertainty including shifting awareness contexts [63], and could patients or carers usefully ask their clinicians to approach uncertainty differently? In addition, we identified a remarkable lack of cultural diversity in the literature. One article investigated the experience of African American caregivers [50], but all articles were from high-income western countries. Since uncertainty is likely to be experienced differently cross-culturally, the evidence gap in relation to multicultural experiences of uncertainty needs addressing urgently.
Conclusions
In advanced multimorbidity, patients, carers and healthcare professionals experience aspects of total uncertainty, responding by either addressing, accepting or avoiding uncertainty. The experience of uncertainty is broadly a shared one across multiple perspectives. The model developed in this study offers a framework to explore and approach uncertainty in research and clinical practice. Future research should explore the effect of uncertainty in clinical interactions, and how addressing uncertainty may contribute to improved communication and person-centred care.
Supplementary Material
Acknowledgements
We would like to thank Sarah Dixon, Irene Moore, Claire Wood, Roberta Lovick and Derek Pinner for their important contributions as members of the patient and public involvement group. Thanks to Dr Tom Weetman, and Professor Jonathan Koffman for their insights and discussion in relation to this work. Data availability: All data for this review are available in the published original articles. See Supplementary Information for reference list of all included articles. Transparency: The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Contributor Information
Simon Noah Etkind, Department of Public Health and Primary Care, University of Cambridge, Cambridge, UK.
Jiaqi Li, School of Clinical Medicine, University of Cambridge, Cambridge, UK.
John Louca, School of Clinical Medicine, University of Cambridge, Cambridge, UK.
Sarah A Hopkins, Department of Public Health and Primary Care, University of Cambridge, Cambridge, UK; Medical Library, School of Clinical Medicine, University of Cambridge, Cambridge, UK.
Isla Kuhn, Medical Library, School of Clinical Medicine, University of Cambridge, Cambridge, UK.
Anna Spathis, Department of Public Health and Primary Care, University of Cambridge, Cambridge, UK.
Stephen I G Barclay, Department of Public Health and Primary Care, University of Cambridge, Cambridge, UK.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
S.E. is funded by a Health Education England Academic Clinical Lectureship. S.B. is part funded by the National Institute for Health Research (NIHR) Applied Research Collaboration East of England (ARC EoE) programme. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. S.H. is jointly funded by The Dunhill Medical Trust and British Geriatrics Society (Grant ref. JBGS20\5).
References
- 1. Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health 2019; 29: 182–9. [DOI] [PubMed] [Google Scholar]
- 2. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380: 37–43. [DOI] [PubMed] [Google Scholar]
- 3. Finucane AM, Bone AE, Etkind S et al. How many people will need palliative care in Scotland by 2040? A mixed-method study of projected palliative care need and recommendations for service delivery. BMJ Open 2021; 11: e041317. 10.1136/bmjopen-2020-041317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Eckerblad J, Theander K, Ekdahl AW, Jaarsma T. Symptom trajectory and symptom burden in older people with multimorbidity, secondary outcome from the RCT AGe-FIT study. J Adv Nurs 2016; 72: 2773–83. [DOI] [PubMed] [Google Scholar]
- 5. Ritchie CS, Zulman DM. Research priorities in geriatric palliative care: multimorbidity. J Palliat Med 2013; 16: 843–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Campbell-Scherer D. Multimorbidity: a challenge for evidence-based medicine. Evid Based Med 2010; 15: 165–6. [DOI] [PubMed] [Google Scholar]
- 7. Calderón-Larrañaga A, Poblador-Plou B, González-Rubio F, Gimeno-Feliu LA, Abad-Díez JM, Prados-Torres A. Multimorbidity, polypharmacy, referrals, and adverse drug events: are we doing things well? Br J Gen Pract 2012; 62: e821–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Condelius A, Edberg A-K, Jakobsson U, Hallberg IR. Hospital admissions among people 65+ related to multimorbidity, municipal and outpatient care. Arch Gerontol Geriatr 2008; 46: 41–55. [DOI] [PubMed] [Google Scholar]
- 9. Sallnow L, Smith R, Ahmedzai SH et al. Report of the lancet commission on the value of death: bringing death back into life. Lancet 2022; 399: 837–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA 2012; 307: 2493–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Boyd C, McNabney M, Brandt N et al. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society expert panel on the Care of Older Adults with multimorbidity. J Am Geriatr Soc 2012; 60: E1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Farmer C, Fenu E, O’Flynn N et al. Clinical assessment and management of multimorbidity: summary of NICE guidance. BMJ (Clin Res Ed) 2016; 354: i4843. [DOI] [PubMed] [Google Scholar]
- 13. Yarnall AJ, Sayer AA, Clegg A, Rockwood K, Parker S, Hindle JV. New horizons in multimorbidity in older adults. Age Ageing 2017; 46: 882–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. May P, Garrido MM, Cassel JB et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff 2016; 35: 44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blaum CS, Rosen J, Naik AD et al. Feasibility of implementing patient priorities Care for Older Adults with multiple chronic conditions. J Am Geriatr Soc 2018; 66: 2009–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koch G, Wakefield BJ, Wakefield DS. Barriers and facilitators to managing multiple chronic conditions: a systematic literature review. West J Nurs Res 2015; 37: 498–516. [DOI] [PubMed] [Google Scholar]
- 17. Salisbury C, Man M-S, Bower P et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet 2018; 392: 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Etkind SN, Bristowe K, Bailey K, Selman LE, Murtagh FEM. How does uncertainty shape patient experience in advanced illness? A secondary analysis of qualitative data. Palliat Med 2016; 31: 171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kimbell B, Murray SA, Macpherson S, Boyd K. Embracing inherent uncertainty in advanced illness. BMJ (Clin Res Ed) 2016; 354: i3802. 10.1136/bmj.i3802. [DOI] [PubMed] [Google Scholar]
- 20. van Iersel MB, Brantjes E, de Visser M et al. Tolerance of clinical uncertainty by geriatric residents: a qualitative study. Eur Geriatr Med 2019; 10: 517–22. [DOI] [PubMed] [Google Scholar]
- 21. Coventry PA, Small N, Panagioti M, Adeyemi I, Bee P. Living with complexity; marshalling resources: a systematic review and qualitative meta-synthesis of lived experience of mental and physical multimorbidity. BMC Fam Pract 2015; 16: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Price ML, Surr CA, Gough B, Ashley L. Experiences and support needs of informal caregivers of people with multimorbidity: a scoping literature review. Psychol Health 2020; 35: 36–69. [DOI] [PubMed] [Google Scholar]
- 23. Sharp T, Malyon A, Barclay S. GPs’ perceptions of advance care planning with frail and older people: a qualitative study. Br J Gen Pract 2018; 68: e44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Im J, Mak S, Upshur R, Steinberg L, Kuluski K. 'The future is probably Now': understanding of illness, uncertainty and end-of-life discussions in older adults with heart failure and family caregivers. Health Expect 2019; 22: 1331–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Etkind SN, Lovell N, Nicholson CJ, Higginson IJ, Murtagh FEM. Finding a ‘new normal’ following acute illness: a qualitative study of influences on frail older people’s care preferences. Palliat Med 2019; 33: 301–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mason B, Nanton V, Epiphaniou E et al. ‘My body's falling apart.’ Understanding the experiences of patients with advanced multimorbidity to improve care: serial interviews with patients and carers. BMJ Support Palliat Care 2016; 6: 60–5. [DOI] [PubMed] [Google Scholar]
- 27. Page MJ, McKenzie JE, Bossuyt PM et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clin Res Ed) 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45. 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Murtagh FE, Bausewein C, Verne J, Groeneveld EI, Kaloki YE, Higginson IJ. How many people need palliative care? A study developing and comparing methods for population-based estimates. Palliat Med 2014; 28: 49–58. [DOI] [PubMed] [Google Scholar]
- 30. Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of Google scholar in evidence reviews and its applicability to Grey literature searching. PLoS One 2015; 10: e0138237–7. 10.1371/journal.pone.0138237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210. 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gough D. Weight of evidence: a framework for the appraisal of the quality and relevance of evidence. Res Pap Edu 2007; 22: 213–28. [Google Scholar]
- 33. Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care a conceptual taxonomy. Med Decis Making 2011; 31: 828–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mishel MH. Uncertainty in illness. Image J Nurs Sch 1988; 20: 225–32. [DOI] [PubMed] [Google Scholar]
- 35. Staniszewska S, Brett J, Simera I et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017; 3: 13. 10.1186/s40900-017-0062-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Doos L, Bradley E, Rushton CA, Satchithananda D, Davies SJ, Kadam UT. Heart failure and chronic obstructive pulmonary disease multimorbidity at hospital discharge transition: a study of patient and carer experience. Health Expect 2015; 18: 2401–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ploeg J, Garnett A, Fraser KD et al. The complexity of caregiving for community-living older adults with multiple chronic conditions: a qualitative study. J Comorb 2020; 10: 2235042X2098119. 10.1177/2235042X20981190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zwijsen SA, Nieuwenhuizen NM, Maarsingh OR, Depla MFIA, Hertogh CMPM. Disentangling the concept of "the complex older patient" in general practice: a qualitative study. BMC Fam Pract 2016; 17: 64. 10.1186/s12875-016-0455-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gill A, Kuluski K, Jaakkimainen L, Naganathan G, Upshur R, Wodchis W. "Where do we go from here?" health system frustrations expressed by patients with multimorbidity, their caregivers and family physicians. Health Policy 2014; 9: 73–89. [PMC free article] [PubMed] [Google Scholar]
- 40. Sinnott C, Hugh SM, Boyce MB, Bradley CP. What to give the patient who has everything? A qualitative study of prescribing for multimorbidity in primary care. Br J Gen Pract 2015; 65: e184–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ploeg J, Matthew-Maich N, Fraser K et al. Managing multiple chronic conditions in the community: a Canadian qualitative study of the experiences of older adults, family caregivers and healthcare providers. BMC Geriatr 2017; 17: 15. 10.1186/s12877-017-0431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cressman G, Ploeg J, Kirkpatrick H, Kaasalainen S, Mcainey C. Uncertainty and alternate level of care: a narrative study of the older patient and family caregiver experience. Can J Nurs Res 2013; 45: 12–29. [DOI] [PubMed] [Google Scholar]
- 43. Nanton V, Munday D, Dale J, Mason B, Kendall M, Murray S. The threatened self: considerations of time, place, and uncertainty in advanced illness. Br J Health Psychol 2016; 21: 351–73. [DOI] [PubMed] [Google Scholar]
- 44. Andersen HE, Hoeck B, Nielsen DS, Ryg J, Delmar C. A phenomenological-hermeneutic study exploring caring responsibility for a chronically ill, older parent with frailty. Nurs Open 2020; 7: 951–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tinetti M, Dindo L, Smith CD et al. Challenges and strategies in patients' health priorities-aligned decision-making for older adults with multiple chronic conditions. PLoS One [Electronic Resource] 2019; 14: e0218249. 10.1371/journal.pone.0218249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Åberg C, Gillsjö C, Hallgren J, Berglund M. 'It is like living in a diminishing world': older persons’ experiences of living with long-term health problems—prior to the STRENGTH intervention. Int J Qual Stud Health Well Being 2020; 15: 1747251. 10.1080/17482631.2020.1747251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Smith SM, O'Kelly S, O'Dowd T. GPs' and pharmacists' experiences of managing multimorbidity: a 'Pandora's box. Br J Gen Pract 2010; 60: e285–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Mc Namara KP, Breken BD, Alzubaidi HT et al. Health professional perspectives on the management of multimorbidity and polypharmacy for older patients in Australia. Age Ageing 2017; 46: 291–9. [DOI] [PubMed] [Google Scholar]
- 49. Anderson K, Foster M, Freeman C, Luetsch K, Scott I. Negotiating "unmeasurable harm and benefit": perspectives of general practitioners and consultant pharmacists on Deprescribing in the primary care setting. Qual Health Res 2017; 27: 1936–47. [DOI] [PubMed] [Google Scholar]
- 50. Unson C, Flynn D, Chukwurah Q, Glendon MA, Testut T. Uncertainty in transition of African American caregivers. Issues Ment Health Nurs 2020; 41: 445–54. [DOI] [PubMed] [Google Scholar]
- 51. Johnson H, Ogden M, Brighton LJ et al. Patient and public involvement in palliative care research: what works, and why? A qualitative evaluation. Palliat Med 2021; 35: 151–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ong C-K, Forbes D. Embracing Cicely Saunders's concept of total pain. BMJ (Clin Res Ed) 2005; 331: 576. 10.1136/bmj.331.7516.576-d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Graham F, Clark D. The changing model of palliative care. Medicine 2008; 36: 64–6. [Google Scholar]
- 54. Pask S, Pinto C, Bristowe K et al. A framework for complexity in palliative care: a qualitative study with patients, family carers and professionals. Palliat Med 2018; 32: 1078–90. [DOI] [PubMed] [Google Scholar]
- 55. Etkind SN, Koffman J. Approaches to managing uncertainty in people with life-limiting conditions: role of communication and palliative care. Postgrad Med J 2016; 92: 412–7. [DOI] [PubMed] [Google Scholar]
- 56. Koffman J, Yorganci E, Yi D et al. Managing uncertain recovery for patients nearing the end of life in hospital: a mixed-methods feasibility cluster randomised controlled trial of the AMBER care bundle. Trials 2019; 20: 1–18. 10.1186/s13063-019-3612-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hillen MA, Gutheil CM, Strout TD, Smets EMA, Han PKJ. Tolerance of uncertainty: conceptual analysis, integrative model, and implications for healthcare. Soc Sci Med 2017; 180: 62–75. [DOI] [PubMed] [Google Scholar]
- 58. Fox RC, Fox RC. The evolution of medical uncertainty. Milbank Mem Fund Q Health Soc 1980; 58: 1–49. 10.2307/3349705. [DOI] [PubMed] [Google Scholar]
- 59. Au DH, Udris EM, Engelberg RA et al. A randomized trial to improve communication about end-of-life care among patients with COPD. Chest 2012; 141: 726–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ellis-Smith C, Dawkins M, Gao W et al. Managing clinical uncertainty in older people towards the end of life: a systematic review of person-centred tools. BMC Palliat Care 2021; 20: 1–41. 10.1186/s12904-021-00845-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Krawczyk M, Gallagher R. Communicating prognostic uncertainty in potential end-of-life contexts: experiences of family members. BMC Palliat Care 2016; 15: 59. 10.1186/s12904-016-0133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Oksavik JD, Solbjør M, Kirchhoff R, Sogstad MKR. Games of uncertainty: the participation of older patients with multimorbidity in care planning meetings—a qualitative study. BMC Geriatr 2021; 21: 242. 10.1186/s12877-021-02184-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Glaser BG, Strauss AL. Awareness of Dying. New Jersey, USA: Transaction Publishers, 1966. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.