Cardiovascular injury has been observed in SARS-CoV-2 infection.1 However, whether endothelial inflammation persists chronically and if this would have any clinical implications is unknown. We aimed to study the potential impact of prior COVID-19 infection on the myocardial flow reserve (MFR) and consequent vascular health using positron emission tomography (PET) myocardial perfusion imaging.
The study population was identified from within an institutional prospective registry of patients who had clinically indicated PET imaging from August 20, 2019, to December 1, 2021, and were followed through April 2, 2022. The registry and its analysis were approved by the Houston Methodist Hospital Institutional Review Board.
Cases consisted of patients with previous COVID-19 infection and were matched on clinical (age and sex) and cardiovascular risk factors (hypertension, diabetes, dyslipidemia, known coronary artery disease and heart failure) with control subjects having no documented prior COVID-19 infection. COVID-19 status was prospectively confirmed by patient report and supplemented by a search of medical records.
Myocardial perfusion imaging was performed according to societal guidelines.2 Myocardial blood flow in mL/g/min was obtained from dynamic images at rest and peak hyperemia. The global MFR was calculated as the ratio of left ventricular stress to rest myocardial blood flow. Patients were followed after PET imaging for occurrence of major adverse cardiovascular events, including all-cause death, myocardial infarction, heart failure admission, and unplanned revascularization—percutaneous coronary intervention or coronary artery bypass grafting occurring >90 days after PET imaging.
Annualized event rates (% per year) were determined stratifying by COVID-19 status and MFR. Logistic regression was used to assess the association of MFR <2 between cases and control subjects. Sensitivity analysis was done in subgroups of patients with diabetes, in those with no prior coronary artery disease with a normal perfusion study (sum difference score <3, sum rest score <3) and stratified by time from COVID-19 to PET imaging (#6 months vs >6 months).
The study population consisted of 101 cases with prior COVID-19 infection matched to 292 control subjects (mean age 65 ± 11 years, 51% men). Cardiovascular risk factors were prevalent (hypertension [61%], diabetes [43%], dyslipidemia [49%], obesity [55%]) and comparable in cases vs control subjects (P > 0.10).
The median number of days between the COVID-19 diagnosis and PET imaging was 190 (IQR: 84-266) days. The most common indication for imaging was chest pain (66% vs 54%; P = 0.032 in cases vs control subjects), followed by dyspnea (41% vs 37%; P = 0.52 in cases vs control subjects). The rates of reversible and fixed perfusion defects were comparable in cases versus control subjects.
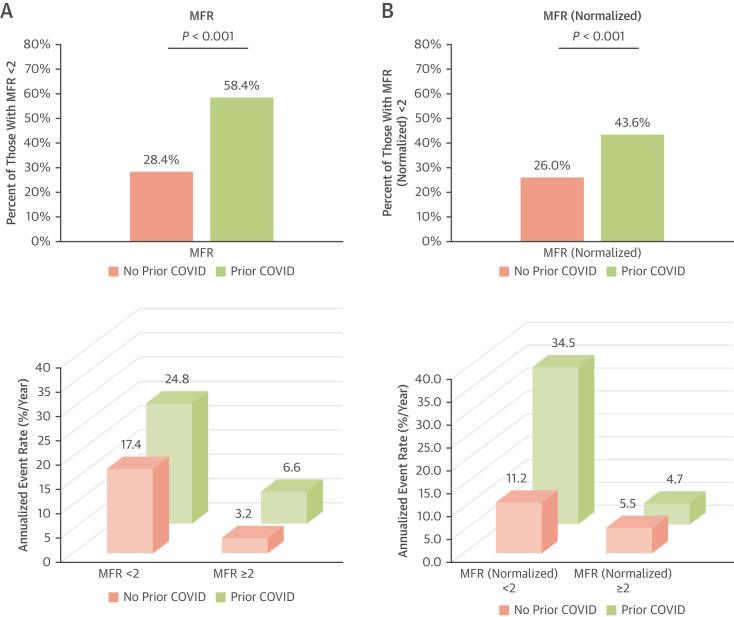
A higher proportion of cases had a reduced global MFR (58% vs 28%; P < 0.001) and global MFR normalized to patients’ rate systolic blood pressure product (44% vs 26%; P < 0.001) when compared with control subjects (Figure 1 ). After adjusting for matching variables, patients with prior COVID-19 had a statistically significant higher odds of having an MFR <2 (OR: 4.0 [95% CI: 2.4-6.6]; P < 0.001) and a normalized MFR <2 (OR: 2.4 [95% CI: 1.4-3.9]; P = 0.001). Results were similar on sensitivity analysis of patients with no prior coronary artery disease with normal perfusion study (OR: 2.9 [95% CI: 1.6-5.6]; P = 0.001), of patients with diabetes, and when stratified by time from COVID-19 to PET imaging. After a median follow-up of 323 (IQR: 199-465) days, 34 patients experienced major adverse cardiovascular events. Annualized event rates were higher in cases versus control subjects and in those with an MFR <2 (Figure 1).
Figure 1.
Comparison of Global MFR and Annualized Event Rates in Cases vs Control Subjects
(A) Global myocardial flow reserve (MFR) <2 and annualized rates of the composite outcome (including all-cause death, myocardial infarction, heart failure admission, and unplanned revascularization—percutaneous coronary intervention or bypass surgery occurring >90 days after positron emission tomography imaging) were higher in cases versus control subjects. (B) Results were similar with global MFR normalized to patients’ rate systolic blood pressure product.
Our analysis suggests that patients with prior COVID-19 infection have higher rates of reduced MFR (likely related to new onset endothelial injury or exacerbation of pre-existing endothelial dysfunction—particularly considering the high prevalence of obesity) and that reduced MFR is a marker of a poor prognosis. Our study is limited by single-center design, use of chart review for follow-up, and high prevalence of cardiovascular risk factors, including obesity. Our findings are particularly relevant to long-haul COVID-19, as persistence of the acute endotheliopathy and inflammation can hypothetically lead to endothelial dysfunction and potentially explain long-haul COVID-19 cardiopulmonary symptoms. Further studies are needed to investigate our findings.
Footnotes
Christopher Kramer, MD, served as the Guest Editor for this paper.
This work was supported in part by grants to John P. Cooke (National Institutes of Health R01 HL133254, R01 HL148338, and R01 HL157790). The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Satterfield B.A., Bhatt D.L., Gersh B.J. Cardiac involvement in the long-term implications of COVID-19. Nat Rev Cardiol. 2022;19:332–341. doi: 10.1038/s41569-021-00631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dilsizian V., Bacharach S.L., Beanlands R.S., et al. ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J Nucl Cardiol. 2016;23:1187–1226. doi: 10.1007/s12350-016-0522-3. [DOI] [PubMed] [Google Scholar]