Abstract
Introduction
The COVID-19 pandemic has had a considerable impact on mental health. The social distancing and stay-at-home orders have likely also impacted loneliness, social isolation, and social support. Older adults, particularly those with comorbidities such as cancer, have a greater potential to be impacted. Here we assessed loneliness, social isolation, and social support in older adults undergoing active cancer treatment during the pandemic.
Materials and methods
A mixed methods study in which quantitative data and qualitative response items were collected in parallel was conducted in 100 older adults with cancer. Participants completed a survey by telephone with a series of validated questionnaires to assess the domains of loneliness, social isolation, and social support as well as several open-ended questions. Baseline demographics and geriatric assessments were summarized using descriptive statistics. Bivariate associations between social isolation and loneliness and social support and loneliness were described using Spearman correlation coefficients. Conventional content analysis was performed on the open-ended questions.
Results
In a population of older adults with cancer, 3% were noted to be severely lonely, although 27% percent screened positive as having at least one indicator of loneliness by the University of California, Los Angeles (UCLA) Three Item Loneliness Scale. There was a significant positive correlation between loneliness and social isolation (r = +0.52, p < 0.05) as well as significant negative correlation between loneliness and social support (r = −0.49, p < 0.05). There was also a significant negative correlation between loneliness and emotional support (r = −0.43, p < 0.05). There was no significant association between loneliness and markers of geriatric impairments, including comorbidities, G8 score or cognition.
Discussion
Reassuringly, in this cohort we found relatively low rates of loneliness and social isolation and high rates of social support. Consistent with prior studies, loneliness, social isolation, and social support were found to be interrelated domains; however, they were not significantly associated with markers of geriatric impairments. Future studies are needed to study if cancer diagnosis and treatment may mediate changes in loneliness, social isolation, and social support in the context of the pandemic as well as beyond.
Keywords: Geriatrics, COVID-19, Loneliness, Medical oncology
1. Introduction
The COVID-19 pandemic and its attendant mitigation strategies, including stay-at-home orders and social distancing, have made consideration of the health impact of social connection increasingly relevant [1,2]. Loneliness, social isolation, and social support are interrelated but distinct concepts that require consideration in this context. While the term loneliness often refers to the subjective feeling of being alone, social isolation refers to the absence of interpersonal interactions [3,4]. Social support has a variety of definitions, including both quantitative and qualitative dimensions [5]. Qualitative social support refers to the perceived meaning and values people ascribe to their relationships [6]. Quantitative social support focuses on social network, including the length and complexity of relationships [7]. These terms have been shown to overlap, and each has important implications for older adults [8] and individuals with cancer [9].
Models of loneliness have theorized that the perceived sense of social isolation results in feeling unsafe, which leads to a hypervigilance of additional social threats [10]. Consequently, loneliness has important impact on both mental and physical health. Loneliness is a specific risk factor for depressive symptoms, as well as for functional decline, morbidity and mortality [[11], [12], [13]]. Similar to loneliness, social isolation has many overlapping effects on health [14]. Social isolation has clear impact on physical health and is associated with poorer cognitive functioning, coronary heart disease, and all-cause mortality [[15], [16], [17], [18]]. Socially isolated individuals with cancer are more likely to be adversely affected by their cancer diagnosis [19] and have inferior survival [20,21]. Furthermore, amount of social support has important implications for individuals with cancer [22] as higher levels of social support are associated with decreased mortalty [23].
The novel coronavirus (COVID-19) has resulted in over 840,286 deaths in the United States alone as of January 2022 [24]. While social isolation during the COVID-19 pandemic has been particularly emphasized for vulnerable populations such as older adults, the recommendation for physical distancing with resultant social isolation may be especially distressing for people living with cancer who rely on social support [25,26]. Older adults, who traditionally have less familiarity with technology, may be further isolated [27]. The early studies of the effects of the pandemic on social isolation and loneliness are limited, with somewhat mixed results. While upwards of 56% of people over the age of 50 have reported feeling isolated from others, compared to 27% of people in a similar poll in 2018 [28], other studies have found that older adults reported lower rates of loneliness compared to younger adults and no change compared to prior rates [29,30]. Studies of the effects of the pandemic in patients with cancer have shown high levels of stress and symptom burden [31]. A study of patients with cancer found that over half of participants were lonely and reported higher levels of social isolation; however, this was more pronounced in the younger population [32]. Another study in older breast cancer survivors found changes in loneliness during the pandemic similar to those reported by individuals without cancer [33].
Few studies have examined the implications of the COVID-19 pandemic on feelings of loneliness, social isolation, and social support in older adults undergoing active cancer treatment. Here we assessed loneliness, social isolation, and social support in older adults with cancer during the pandemic.
2. Materials and Methods
We performed a mixed methods study in which quantitative data and qualitative response items were collected in parallel [34]. Informed consent was obtained from patients age 65 or older with a biopsy-proven malignancy who were receiving active systemic therapy, such as intravenous chemotherapy or oral medications, and anticipated to continue to receive care at Siteman Cancer Center (SCC). Patients on active surveillance alone or in survivorship clinics were excluded. Potential study candidates were identified from the patients who were seeking initial consultation or continued treatment with a medical oncologist at the SCC. Patients were enrolled onto the study until the recruitment goal of 100 patients was met.
Potential participants were screened from the solid tumor oncology clinic schedule at SCC and contacted by telephone by research team members. Following verbal consent, basic demographic information was collected from the medical record at the time of patient consent, including age/sex, race/ethnicity, cancer diagnosis/staging, description of treatment, and Charlson comorbidity index. Cancer diagnosis was included in the Charlson comorbidity index calculations for all participants. Participants then completed a mixed methods survey by telephone with a series of validated questionnaires to assess the domains of loneliness, social isolation, and social support as well as several open-ended questions. Measures included the G8 geriatric screening tool [35], Patient-Reported Outcomes Measurement Information System (PROMIS) Bank v2.0 Emotional Support Short Form 4a, PROMIS Bank v2.0-Social Isolation Short Form 8a [36], University of California, Los Angeles (UCLA) loneliness scale [37], the Medical Outcomes Study (MOS) social support survey [38], and the Short Blessed Test [39]. These measures were not modified.
Patients were then asked a short series of open-ended questions at the end of the telephone interview to better understand the impact of the COVID-19 pandemic on loneliness. Responses were summarized and recorded by the research coordinator.
To account for the dynamic status of the COVID-19 pandemic, the average seven-day new confirmed cases and average test positivity rate for St. Louis region at the time of the telephone interview and in-person assessment, as publicly reported (https://www.stlouis-mo.gov/covid-19/data/) were recorded for each participant.
The study was approved by the Washington University School of Medicine Human Studies Committee.
2.1. Measures
2.1.1. Loneliness
Loneliness was defined based on the UCLA Loneliness Scale long form [37] as well as UCLA Three Item Loneliness Scale [40]. Using the original UCLA Loneliness Scale, scores >30 were defined as severe loneliness. Using the Three Item UCLA Loneliness Scale, loneliness was categorized in two ways [41]. “Any loneliness” was defined as 1+ points on the scale and “frequently lonely” was defined as 4+ points on the scale.
2.1.1.1. PROMIS Bank Emotional Support Short Form 4a – Version 2
The PROMIS Emotional Support bank evaluates relationships and perceived feelings of being valued. The T-score was calculated, which rescaled the raw score into a standardized score with a mean of 50 in a general US reference population and a standard deviation (SD) of 10 [36]. A higher PROMIS T-score represents more of the concept being measured. Higher scores represent better emotional support.
2.1.1.2. PROMIS Bank Social Isolation Short Form 8a – Version 2
The PROMIS Social Isolation bank evaluates perceived feelings of being excluded or disconnected from other individuals. A T-score was also calculated as above and a higher score indicates higher levels of social isolation [42].
2.1.1.3. MOS Social Support Survey
MOS measures the availability of support in several domains. For this study, emotional/informational (eight questions) and tangible (four questions) support domains were used. The mean item response for each subscale was calculated and then scores were transformed to have a possible range of 0–100, with higher scores indicating more support [38].
2.2. Statistical Analysis
The sample size of this pilot study was determined based on that anticipated recruitment feasible during the study period and was 100 older adults with cancer. It was estimated that a sample size of 100 would allow for an estimation of the true mean score on the UCLA loneliness scale with a margin of error of ±9.8 (95% confidence interval [CI]) [37].
Baseline demographics and geriatric assessments were summarized using descriptive statistics. Bivariate associations between social isolation and loneliness and social support and loneliness were described using Pearson correlation coefficients. Exploratory analysis of the relationship between social isolation, loneliness, social support, and other variables including sex, cancer types, stage, treatment type, education, marital status, living situation, employment, income, and average COVID cases was performed using non-parametric Kruskal-Wallis rank-sum test to compare the average T-scores among the subgroups defined by these variables such as sex, education, etc. Partial correlation coefficients for loneliness versus social isolation or social support were also calculated after adjusting demographic and clinical variables. All analyses were two-sided and significance was set at a p-value of 0.05. Statistical analyses were performed using SAS 9.4 (SAS Institutes, Cary NC).
2.3. Content Analysis
Conventional content analysis was performed on the open-ended questions [43]. The patient responses were reviewed and codes were created based on unique responses which were then sorted into groups. A descriptive analysis of these groups was then performed.
3. Results
From March 2021 to July 2021, 100 patients were enrolled. Baseline demographic values are presented in Table 1 . The mean age of participants was 74.28 years. The majority of participants were White (86%) females (58%) receiving oral therapy (59%). The majority of participants were married (55%) and living with a spouse (54%). Thirty-one percent of participants lived alone, 21% were divorced and 17% were widowed. The majority of patients were retired (75%) and had either an advanced degree (34%) or college degree (21%). The majority of participants reported a yearly household income of $50,000 or greater (57%). The majority of participants had a diagnosis of breast (44%) or prostate cancer (23%) and were stage IV (56%). The average seven-day new confirmed COVID-19 cases in the city of Saint Louis during the time of the study was 23.49. The average test positivity rate in the city of Saint Louis was 5.59%.
Table 1.
Demographics.
| Variable | Number of patients (N = 100) | |
|---|---|---|
| Age | Mean +/− standard deviation | 74.28 ± 5.58 |
| Sex | Male | 42 |
| Female | 58 | |
| Race | White | 86 |
| African American | 14 | |
| Ethnicity | Hispanic | 1 |
| Non-Hispanic | 99 | |
| Other | 0 | |
| Current Treatment ⁎ | IV Chemotherapy | 24 |
| Oral Therapy | 59 | |
| Immunotherapy | 13 | |
| Other, including clinical trial | 29 | |
| Education Level | Grades 1–8 | 0 |
| Grades 9–11 | 3 | |
| High school or GED | 18 | |
| Some college | 15 | |
| Some junior college | 7 | |
| College Degree | 21 | |
| Post-college work | 2 | |
| Advanced Degree | 34 | |
| Marital Status | Married | 55 |
| Divorced | 21 | |
| Widowed | 17 | |
| Single | 7 | |
| Living Situation | Spouse | 54 |
| Parents/Parents-in-law | 1 | |
| Alone | 31 | |
| Children, age ≤ 18 | 1 | |
| Children, age > 18 | 7 | |
| Other | 5 | |
| Employment Status | Employed >32 h/week | 9 |
| Employed <32 h/week | 8 | |
| Homemaker | 1 | |
| Medical leave | 1 | |
| Disabled | 0 | |
| Unemployed | 2 | |
| Retired | 75 | |
| Other | 4 | |
| Yearly Household | Less than $5000 | 3 |
| Income | $5000–$19,999 | 9 |
| $20,000–$49,999 | 24 | |
| $50,000–$99,999 | 25 | |
| $100,000–$149,999 | 14 | |
| Over $150,000 | 18 | |
| Prefer not to answer | 7 | |
| Cancer Types | Breast Cancer | 44 |
| Prostate Cancer | 23 | |
| Others | 33 | |
| Cancer Stage | I | 29 |
| II/III | 14 | |
| IV | 56 |
Sum >100 due to patients being on more than one type of therapy concurrently.
Results of the geriatric assessment, as well as measures of loneliness, social isolation, and social support are presented in Table 2 . The mean BMI for the cohort was 23.49 and the mean Charlson comorbidity index was 7.66. On the G-8 geriatric screening tool, 62% of patients scored ≤14, which is considered abnormal. Only 2% of patients scored >9 (abnormal) on the Short Blessed Test. On the UCLA Loneliness scale, 3% of participants scored >30, which is considered severely lonely. By the UCLA Three Item Loneliness Scale, 27% scored ≥1, indicating any loneliness. The mean T Score for the PROMIS Bank v2.0 Emotional Support Short Form 4a was 56.67 and the mean T score PROMIS Bank v2.0 Social Isolation Short Form 8a was 43.94. The mean MOS Social Support Score was 82.64.
Table 2.
Outcome Variables in cohort of older adults on chemotherapy completing survey of loneliness and social isolation (N = 100).
| BMI (Mean, range) | 23.49 (17.54–55.17) |
|---|---|
| G-8 geriatric screening tool | |
| > 14 | 38 |
| ≤ 14 (abnormal) | 62 |
| Charlson comorbidity index (Mean, range) | 7.66 (4, 13) |
| Short Blessed Test >9 (frequency, percent) | 2/100 (2%) |
| UCLA Loneliness Scale | |
| ≤ 30 | 97 |
| > 30 (severely lonely) | 3 |
| UCLA Three Item Loneliness Scale | |
| 0 | 73 |
| ≥ 1 (any loneliness) | 27 |
| ≥ 4 (frequently lonely) | 3 |
| PROMIS Bank v2.0 Emotional Support Short Form 4a (T score Mean, range) | 56.67 (42.10–62.00) |
| PROMIS Bank v2.0 Social Isolation Short Form 8a (T score Mean, range) | 43.94 (33.90–64.50) |
| MOS Social Support Score (Mean, range) | 82.64 (0−100) |
BMI, body mass index; UCLA, University of California, Los Angeles; PROMIS, Patient-Reported Outcomes Measurement Information System; MOS, Medical Outcomes Study.
All questionnaires showed very good internal consistency, with standardized Cronbach's alpha of 0.78, 0.87, 0.92, 0.95, and 0.72 for PROMIS Emotional Support, PROMIS Social Isolation, MOS Social Support, UCLA Long Form, and UCLA Short Form, respectively.
There was a significant positive correlation between loneliness and social isolation (r = +0.52, p < 0.05) as well as significant negative correlation between loneliness and social support (r = −0.49, p < 0.05). There was also a significant negative correlation between loneliness and emotional support (r = −0.43, p < 0.05). These correlations were significant using both the UCLA long form as well as short form.
There was no significant association between loneliness and markers of geriatric impairments, including comorbidities, G8 score, or cognition. Similarly, there was no significant association between social isolation, social support, or emotional support and markers of geriatric impairments, including comorbidities, G8 score, or cognition.
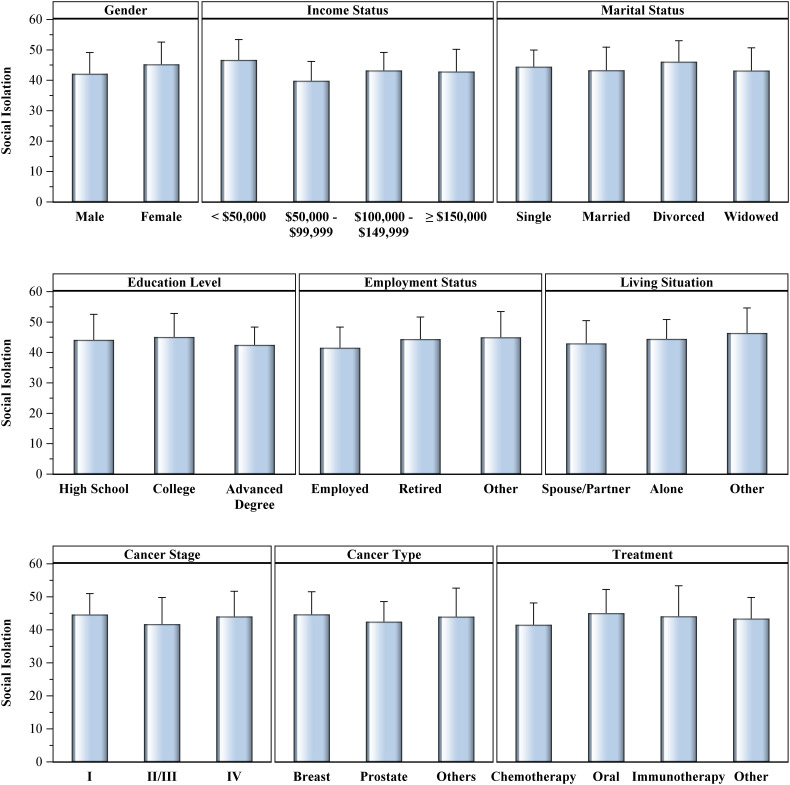
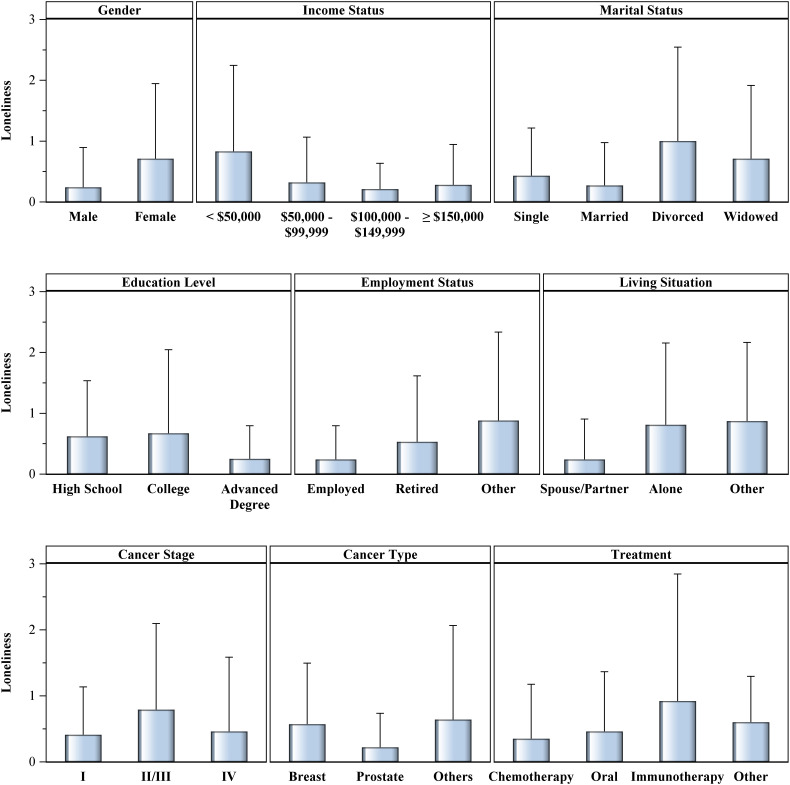
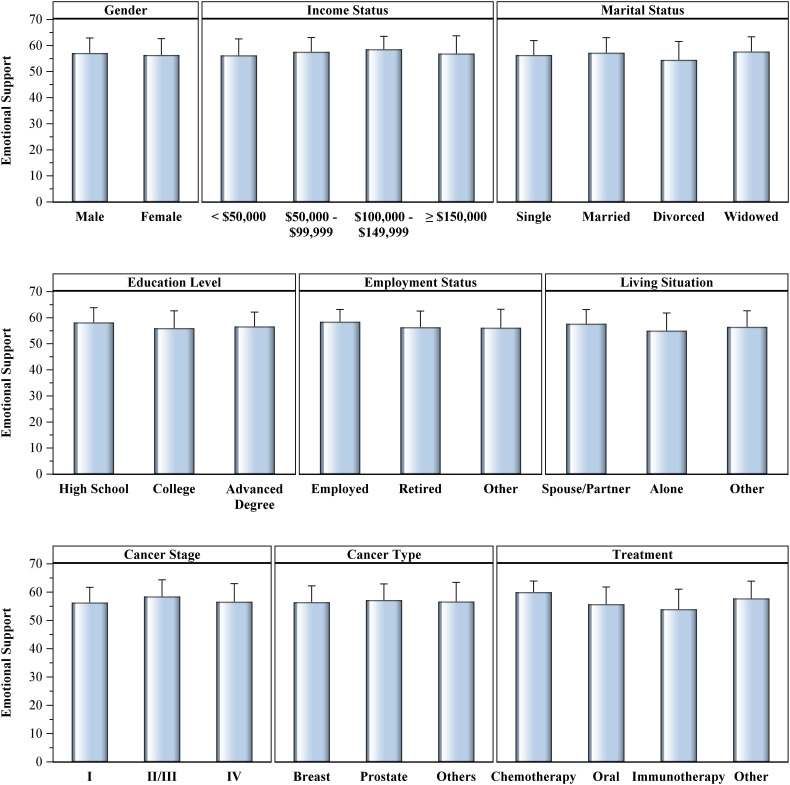
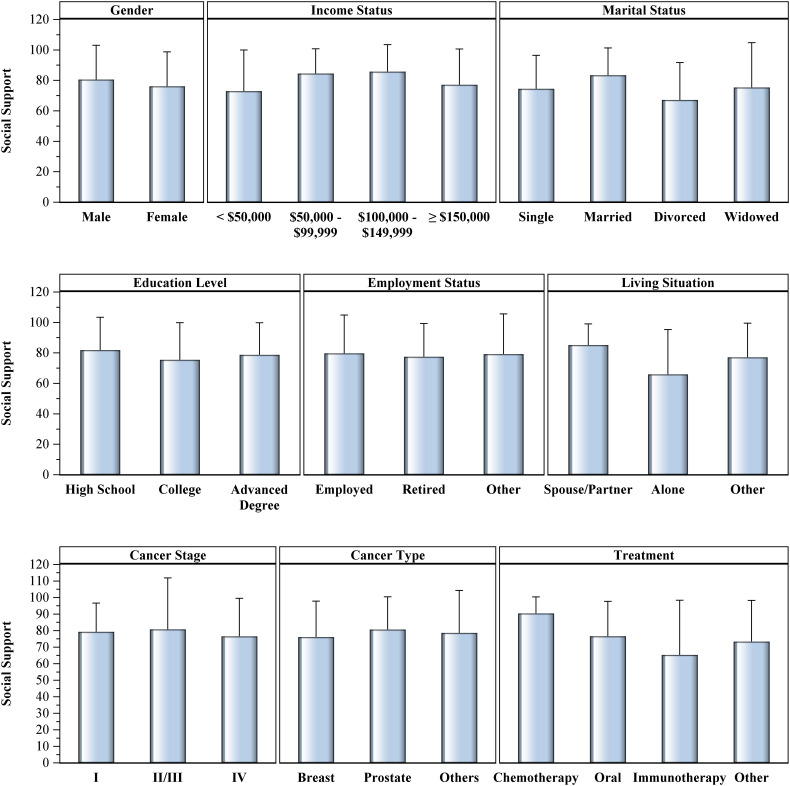
The association between loneliness (Fig. 1 ), social isolation (Fig. 2 ), emotional support (Fig. 3 ) and social support (Fig. 4 ) and multiple demographic variables, including sex, income status, marital status, education level, employment status, living situation, cancer stage, cancer type, and treatment were then analyzed. There was a significant (p < 0.05) association between loneliness and sex, income status, marital status, and living situation. Higher rates of loneliness were associated with being female, annual household income <$50,000 per year, divorced individuals, and individuals living alone or with an individual other than a spouse. There was a significant (p < 0.05) association between social isolation and sex and income status. Higher rates of social isolation were associated with being female with an annual household income <$50,000 per year. There was a significant (p < 0.05) association between emotional support and treatment type. Lower rates of emotional support were associated with patients receiving oral therapy and immunotherapy. There was a significant (p < 0.05) association between social support and living situation and treatment type. Lower rates of social support were associated with living alone and with patients receiving oral therapy and immunotherapy.
Fig. 1.
Association between loneliness and demographic variables in cohort of older adults on chemotherapy completing survey of loneliness and social isolation (N = 100).
Fig. 2.
Association between social isolation and demographic variables in cohort of older adults on chemotherapy completing survey of loneliness and social isolation (N = 100).
Fig. 3.
Association between emotional support and demographic variables in cohort of older adults on chemotherapy completing survey of loneliness and social isolation (N = 100).
Fig. 4.
Association between social support and demographic variables in cohort of older adults on chemotherapy completing survey of loneliness and social isolation (N = 100).
There was no significant association between loneliness, social isolation, emotional support, and social support and daily average number of COVID-19 cases. After adjusting these demographic variables, the conclusion remained unchanged, with a positive correlation between loneliness and social isolation (r = +0.45, p < 0.05), and a negative correlation between loneliness and social support (r = −0.44, p < 0.05), as well as between loneliness and emotional support (r = −0.40, p < 0.05).
3.1. Open Ended Questions
3.1.1. How has COVID-19 pandemic affected you?
On review of responses, three distinct themes were identified: the COVID-19 pandemic did not affect participants, participants found ways to adapt to the pandemic, and/or participants were affected by the pandemic. Representative responses of these themes are presented in Table 3 . The majority of patients (N = 57) discussed how the pandemic has affected them, with the most common ways including physical isolation (N = 32) and change of routines (N = 29). One participant described “It was awful. It was horrible. I have cancer and low blood counts so I was very careful and in isolation for a whole year. I missed two years of my granddaughter's life. I was in remission, but I got diagnosed with cancer right after I got the COVID-19 vaccine, so it has been really hard.”
Table 3.
Representative responses to the open-ended question: How has COVID-19 pandemic affected you?
| No effect (N = 41) | Adapted (N = 19) | Affected (N = 57) |
|---|---|---|
| Continued to have support system of family, friends, etc. (15) | Found solutions (3) | Changed routines (stopped volunteering, traveling) (29) |
| Previously accustomed to being alone (5) | Used technology for interacting with others (7) | Physical isolation (stayed at home) (32) |
| Participated in indoor hobbies (reading, cooking) (5) | Loneliness (1) | |
| Interacted outdoors (5) | Made cancer diagnosis more difficult (3) | |
| Interacted in “pods” (2) | Mental health (depression, anxiety, fear) (6) |
A large number of respondents did state that the pandemic had not affected them (N = 41), most commonly citing that they continued to have support from friends and/or family (N = 15). A subset of patients described ways they adapted to the pandemic (N = 19), including using technology to interact with other (N = 7), interacting outdoors (N = 5) and in “pods” (N = 2), and participating in hobbies (N = 5).
Have you or do you plan to receive a vaccination against the COVID-19 pandemic when available? If yes, how do you perceive this has changed or will change your feelings of loneliness and social isolation?
The overwhelming majority (95%) of patients had received (N = 88) or planned to receive (N = 7) their COVID-19 vaccination. Of those, 26.3% (N = 25) felt that the vaccination would not change their feelings of loneliness or social isolation. Twenty-seven patients (28.4%) responded that the vaccination did change their perceptions by allowing them to socialize, resume previous activities, and travel. One participant responded, “It absolutely changed my feelings. A great weight was lifted.”
Based upon all the things we discussed today, is there anything else you would like to add?
A theme that emerged from the final open-ended question was one of gratitude, with fourteen participants answering that they felt grateful for the support system in their life. One participant noted “The questions make me feel grateful for what I have with my husband and other people in my bubble.” Another eight patients expressed appreciation for being asked about loneliness and social isolation. Other patients offered advice, “Don't sit in it! People need to try to create something positive.”
4. Discussion
We conducted a cross-sectional mixed methods pilot study to assess loneliness, social isolation, and social support in older adults on active treatment for cancer during the COVID-19 pandemic. Reassuringly, in this cohort we found relatively low rates of loneliness and social isolation and high rates of social support. Only a small population in the study, 3%, were noted to be severely lonely although 27% percent screened positive as having at least one indicator loneliness by the UCLA short form. This is in contrast with another study in patients with cancer during the COVID-19 pandemic, which found 53% of patients with cancer were classified as lonely; however, this was in a younger patient population [31]. Multiple studies in a general population also found age to be a risk factor for loneliness, with younger adults exhibiting higher rates of loneliness [29,[44], [45], [46], [47]]. Larger pre-pandemic studies have shown that age is a major risk factor for loneliness and may decline as individuals grow older [48]. Younger individuals may report increased levels of perceived social isolation as the pandemic may have disrupted more social activities such as travel and education. Older adults who are retired and accustomed to staying at home, in contrast, may have had less disruption to their schedules. Additionally, another study revealed older adults exhibited resilience and used technology to protect themselves from loneliness during the pandemic [30].
Females were more likely to be lonely in our patient population. Previous studies regarding sex and loneliness have been mixed, with some studies revealing females are more lonely [[49], [50], [51]] and others that men are more lonely [52,53]. A recent large meta-analysis revealed no significant sex differences [54]. Married individuals were found to be the least lonely, consistent with previous studies [[55], [56], [57]]. Similarly, those living with a partner reported significantly lower rates of loneliness and higher social support, while those living alone or living with another relative or children reported similar rates of loneliness. Those reporting annual incomes <$50,000 had the highest rates of loneliness and social isolation, a finding that has also been shown in recent studies of loneliness during the COVID-19 pandemic [58,59].
Levels of social support were similar to previous studies of patients with cancer prior to the pandemic [60,61]. This study found high levels of emotional support and lower levels of social isolation, which are calibrated to the US general population. While the PROMIS scores were developed in a general population and prior to the COVID-19 pandemic, a study of changes in the PROMIS Global Health during the pandemic in a general population only found modest and non-clinically meaningful decreases in global mental and physical health [62]. It may be hypothesized that the levels of emotional support and lower levels of social isolation may be moderated by patients' cancer diagnoses and treatment. Patients with cancer may receive more emotional and social support from caregivers and have less social isolation as they require frequent interactions with the medical establishment. Similarly, a study of Americans 50 years or older during the COVID-19 pandemic found lower rates of social isolation in participants who had access to a healthcare provider and access to medications [63].
Loneliness, however, was associated with lower rates of emotional support and higher rates of social isolation, as found with a recent study of patients with cancer during the COVID-19 pandemic [32]. Higher rates of loneliness were also associated with less social support, which is similar to a previous meta-analysis in oncology patients [64].
Loneliness, emotional support, social isolation, and social support were not significantly associated with markers of geriatric impairments used in this study, including comorbidities, G8 score, or cognition. This is in contrast with previous studies in which loneliness was associated with increased comorbidities and poorer functional status [32,65]. This may be explained by the relatively low rates of loneliness in this cohort, but underscores the need to consider screening for loneliness rather than relying on the presence of other geriatric impairments as a marker for loneliness.
The open-ended questions in our study added context to the quantitative data. Several important themes were identified in regards to how the pandemic affected patients. The majority of participants (N = 57) felt affected by the pandemic, including increased physical isolation (N = 32) and change of routines (N = 29). However, large numbers of participants felt the pandemic did not affect them (N = 41) and discussed ways they adapted (N = 19). Many participants also discussed gratitude for their support system. The open-ended responses add additional context to the findings of high levels of social and emotional support and lower levels of loneliness and social isolation.
4.1. Strengths
There are several strengths to this study. Unlike many studies which are conducted in patients with cancer on active surveillance, our study was conducted in older adults undergoing active treatment. This population was likely immunocompromised and vulnerable to the social distancing guidelines and restrictions during the COVID- 19 pandemic. Our study was also conducted over the telephone rather than by email, and therefore may have captured additional older adults who have lower proficiency with technology. The telephone nature of the survey also allowed for adherence to the social distancing guidelines and did not put participants at risk for COVID-19. The open-ended questions provided additional context and enriched the participant's responses.
4.2. Limitations
There are several limitations in this study. The study was a cross-sectional study and therefore we are unable to compare rates of loneliness, social isolation, and social support in this cohort during the COVID-19 pandemic to prior to the pandemic or assess for any changes in these domains. Furthermore, the cohort was comprised of largely White, educated individuals with high vaccination rates and therefore may not be generalizable to a larger population. The survey response rate was not recorded, so the representativeness of those who agreed to participate is not known. Furthermore, we did not survey similar individuals without cancer and therefore cannot assess if characteristics from the cohort are unique to patients with cancer or if there are other variables influencing the analysis. Our sample was derived from a population of patients seeking care at a tertiary care facility and thus represents individuals who are either geographically proximate or who have the resources and social support to travel to our institution; thus it is not representative of all older adults with cancer in the United States.
4.3. Implications
The effect of loneliness on mortality has been found to be comparable to other well-known risk factors such as obesity and cigarette smoking [66,67]. Loneliness has been associated with increased risk of coronary heart disease, hypertension, cognitive dysfunction, and poor sleep quality [[68], [69], [70], [71], [72]]. Loneliness among middle-aged men has been associated with an increased likelihood of cancer [73]. It may also have important implications for the treatment of cancer as it may upregulate inflammatory gene expression [74] and has been associated with impaired cellular immunity and decreased NK cell activity [75]. Similarly, socially isolated individuals are at higher risk for negative health behaviors such as heavy drinking, smoking, decreased physical activity, and poor nutrition [16,[76], [77], [78], [79]]. The relationship between social isolation and mental health is not as well understood, with some studies reporting associations between social isolation and depression [80] while others not [81]. It has also been associated with re-hospitalization [18] and falls [82].
A cancer diagnosis and treatment are associated with high levels of stress, so much so that patients may develop cancer-related post-traumatic stress disorder [83]. Following a cancer diagnosis, individuals experience disruptions in their social networks and require greater amounts of social support, particularly older adults [84]. Patients with cancer who have higher levels of social support report improved quality-of-life [[85], [86], [87], [88], [89], [90]]. In breast cancer, lack of social support is an independent risk factor for toxicity from chemotherapy [61] and potentially cancer progression [91].
In this current study, a population of older adults undergoing active treatment for cancer displayed low rates of loneliness and social isolation with higher levels of social support in the setting of the ongoing COVID-19 pandemic. However, females, those who live alone, and individuals with lower incomes were at higher risk of loneliness. Given the important implications of loneliness on both physical and mental health, our study indicates a separate screening for loneliness and social support may be necessary, particularly in these higher risk populations. Limiting screening to patients with significant comorbidities may fail to capture some patients.
4.4. Future Directions
Although the number of participants with severe loneliness in our study was low, almost one third of participants did report some form of loneliness, which may have important implications on mental and physical health. Even prior to the COVID-19 pandemic, the National Academies of Sciences, Engineering, and Medicine Consensus Study Report called on health care professionals to identify, prevent, and mitigate the adverse health impacts of social isolation and loneliness [92]. Numerous interventions have been evaluated to help reduce social isolation and loneliness [93]. Interventions shown to be effective include group activities, animal interventions, befriending interventions, and leisure/skill development (Table 4 ). Unfortunately, many of these interventions involve in-person interactions that are not feasible during the COVID-19 pandemic [94]. Videoconferencing interventions have been previously shown to reduce levels of loneliness, although fewer studies have utilized this technology [95]. Beyond the COVID-19 pandemic, remote interventions may also be helpful for older adults who may have difficulties with mobility or transportation. Furthermore, remote interventions may be more scalable and economic.
Table 4.
Existing Interventions to reduce social isolation.
| Types of interventions | Description | Example | Evidence |
|---|---|---|---|
| Social facilitation | Facilitating interactions with peers | Circle of Friends [96] | Improvement of older adults' well-being, health, and cognition |
| Psychological therapies | Approaches delivered by trained therapists | Mindfulness and stress reduction [97] | Intervention reduced loneliness |
| Health and social care provision | Healthcare professionals supporting older adults | CARELINK program [98] | Those receiving intervention were 12 times less likely to report social isolation compared to control group |
| Animal interventions | Feline and canine companions | Animal-assisted therapy [99] | Effective in improving loneliness as individual animal-assisted therapy |
| Befriending interventions | Formulating new friendships | Call in Time [100] | Participants gained confidence and became socially active again |
| Leisure development | Focus on leisure or skill development | Internet-at-home intervention [101] | Improvements in emotional loneliness and self-confidence |
5. Conclusions
Loneliness, social isolation and social support are overlapping domains which have important implications in the physical and mental health of older adults with cancer. The ongoing social distancing recommendations during the COVID-19 pandemic have potentially impacted these areas. In a cohort of older adults with cancer undergoing active treatment, there were relatively low rates of loneliness and social isolation and high rates of social support. Further studies are needed to investigate if a cancer diagnosis and treatment may mediate changes in loneliness, social isolation, and social support in the context of the pandemic and beyond.
Declarations
Funding Source: Cancer and Aging Research Group Pilot Grant.
Author Contributions
Conceptualization: Katherine Clifton, Tanya Wildes.
Funding acquisition: Katherine Clifton.
Project Administration: JoAnn Jabari, Mary Van Aman, Patricia Dulle.
Data Curation: JoAnn Jabari, Mary Van Aman, Patricia Dulle.
Formal Analysis: Katherine Clifton, Feng Gao, Janice Hanson, Tanya Wildes.
Writing – original draft: All authors.
Writing – review and editing: All authors.
References
- 1.Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Health Res Pol. 2020;5(1):27. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sepúlveda-Loyola W., et al. Impact of social isolation due to COVID-19 on Health in older people: mental and physical effects and recommendations. J Nutr Health Aging. 2020:1–10. doi: 10.1007/s12603-020-1500-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larose S., Guay F., Boivin M. Attachment, social support, and loneliness in young adulthood: a test of two models. Pers Soc Psychol Bull. 2002;28(5):684–693. [Google Scholar]
- 4.Valtorta N., Hanratty B. Loneliness, isolation and the health of older adults: do we need a new research agenda? J R Soc Med. 2012;105(12):518–522. doi: 10.1258/jrsm.2012.120128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pearson J.E. The definition and measurement of Social support. J Couns Dev. 1986;64(6):390–395. [Google Scholar]
- 6.Nguyen A.W., et al. Social support from family and friends and subjective well-being of Older African Americans. J Happiness Stud. 2016;17(3):959–979. doi: 10.1007/s10902-015-9626-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan B.H., Cassel J.C., Gore S. Social support and health. Med Care. 1977;15(5):47–58. doi: 10.1097/00005650-197705001-00006. [DOI] [PubMed] [Google Scholar]
- 8.Donovan N.J., Blazer D. Social isolation and loneliness in older adults: review and commentary of a national academies report. Am J Geriatr Psychiatry. 2020;28(12):1233–1244. doi: 10.1016/j.jagp.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Importance of Social Support in Cancer Patients Asian Pac J Cancer Prev. 2012;13(8):3569–3572. doi: 10.7314/apjcp.2012.13.8.3569. [DOI] [PubMed] [Google Scholar]
- 10.Cacioppo J.T., et al. Loneliness within a nomological net: an evolutionary perspective. J Res Pers. 2006;40(6):1054–1085. [Google Scholar]
- 11.Hawkley L.C., Cacioppo J.T. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med Publ Soc Behav Med. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cacioppo J.T., et al. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- 13.Perissinotto C.M., Stijacic Cenzer I., Covinsky K.E. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172(14):1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nicholson N.R. A review of social isolation: an important but underassessed condition in older adults. J Prim Prev. 2012;33(2–3):137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 15.DiNapoli E.A., Wu B., Scogin F. Social isolation and cognitive function in Appalachian older adults. Res Aging. 2014;36(2):161–179. doi: 10.1177/0164027512470704. [DOI] [PubMed] [Google Scholar]
- 16.Eng P.M., et al. Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Am J Epidemiol. 2002;155(8):700–709. doi: 10.1093/aje/155.8.700. [DOI] [PubMed] [Google Scholar]
- 17.Fratiglioni L., et al. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. 2000;355(9212):1315–1319. doi: 10.1016/S0140-6736(00)02113-9. [DOI] [PubMed] [Google Scholar]
- 18.Mistry R., et al. Social isolation predicts re-hospitalization in a group of older American veterans enrolled in the UPBEAT program. Int J Geriatr Psychiatry. 2001;16(10):950–959. doi: 10.1002/gps.447. [DOI] [PubMed] [Google Scholar]
- 19.Michael Y.L., et al. Social networks and health-related quality of life in breast cancer survivors: a prospective study. J Psychosom Res. 2002;52(5):285–293. doi: 10.1016/s0022-3999(01)00270-7. [DOI] [PubMed] [Google Scholar]
- 20.Moore S., et al. Social isolation: impact on treatment and survival in patients with advanced cancer. J Clin Oncol. 2018;36(34_suppl):156. [Google Scholar]
- 21.Kroenke C.H., et al. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24(7):1105–1111. doi: 10.1200/JCO.2005.04.2846. [DOI] [PubMed] [Google Scholar]
- 22.Usta Y.Y. Importance of social support in cancer patients. Asian Pac J Cancer Prev. 2012;13(8):3569–3572. doi: 10.7314/apjcp.2012.13.8.3569. [DOI] [PubMed] [Google Scholar]
- 23.Pinquart M., Duberstein P.R. Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol. 2010;75(2):122–137. doi: 10.1016/j.critrevonc.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prevention, C.F.D.C.A . 2021. United States COVID-19 Cases, Deaths, and Laboratory Testing (NAATs) by State, Territory, and Jurisdiction. [cited 2021 October 5] [Google Scholar]
- 25.Al-Shamsi H.O., et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25(6):e936–e945. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ford M.B. Social distancing during the COVID-19 pandemic as a predictor of daily psychological, social, and health-related outcomes. J Gen Psychol. 2021;148(3):249–271. doi: 10.1080/00221309.2020.1860890. [DOI] [PubMed] [Google Scholar]
- 27.Vaportzis E., Giatsi Clausen M., Gow A.J. Older adults perceptions of technology and barriers to interacting with tablet computers: a focus group study. Front Psychol. 2017;8(1687) doi: 10.3389/fpsyg.2017.01687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loneliness among older adults before and during the COVID-19 pandemic. University of Michigan; 2020. [Google Scholar]
- 29.Groarke J.M., et al. Loneliness in the UK during the COVID-19 pandemic: cross-sectional results from the COVID-19 psychological wellbeing study. Plos One. 2020;15(9) doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peng S., Roth A.R. Social isolation and loneliness before and during the COVID-19 pandemic: a longitudinal study of U.S. Adults Older than 50. J Gerontol Ser B. 2021;77(7):185–190. doi: 10.1093/geronb/gbab068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miaskowski C., et al. Stress and symptom burden in oncology patients during the COVID-19 pandemic. J Pain Symptom Manage. 2020;60(5):e25–e34. doi: 10.1016/j.jpainsymman.2020.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miaskowski, C., et al., Loneliness and symptom burden in oncology patients during the COVID-19 pandemic. Cancer. [DOI] [PMC free article] [PubMed]
- 33.Rentscher K.E., et al. Loneliness and mental health during the COVID-19 pandemic in older breast cancer survivors and noncancer controls. Cancer. 2021;127(19):3671–3679. doi: 10.1002/cncr.33687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shorten A., Smith J. Mixed methods research: expanding the evidence base. Evid Based Nurs. 2017;20(3):74–75. doi: 10.1136/eb-2017-102699. [DOI] [PubMed] [Google Scholar]
- 35.Bellera C.A., et al. Screening older cancer patients: first evaluation of the G-8 geriatric screening tool. Ann Oncol. 2012;23(8):2166–2172. doi: 10.1093/annonc/mdr587. [DOI] [PubMed] [Google Scholar]
- 36.Ader D.N. Developing the patient-reported outcomes measurement information system (PROMIS) Med Care. 2007;45(5):S1–S2. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Russell D., Peplau L.A., Ferguson M.L. Developing a measure of loneliness. J Pers Assess. 1978;42(3):290–294. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- 38.Sherbourne C.D., Stewart A.L. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 39.Katzman R., et al. Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 40.Hughes M.E., et al. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kotwal, A.A., et al., The epidemiology of social isolation and loneliness among older adults during the last years of life. J Am Geriatr Soc. [DOI] [PMC free article] [PubMed]
- 42.Carlozzi N.E., et al. Understanding health-related quality of life of caregivers of civilians and service members/veterans with traumatic brain injury: establishing the reliability and validity of PROMIS social health measures. Arch Phys Med Rehabil. 2019;100(4S):S110–S118. doi: 10.1016/j.apmr.2018.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 44.Losada-Baltar A., et al. “We are staying at home.” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J Gerontol Ser B. 2020;76(2):e10–e16. doi: 10.1093/geronb/gbaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bu F., Steptoe A., Fancourt D. Loneliness during strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 adults in the UK. medRxiv. 2020;265:1–6. doi: 10.1016/j.socscimed.2020.113521. p. 2020.05.29.20116657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li L.Z., Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291:113267. doi: 10.1016/j.psychres.2020.113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luchetti M., et al. The trajectory of loneliness in response to COVID-19. Am Psychol. 2020;75(7):897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shovestul B., et al. Risk factors for loneliness: the high relative importance of age versus other factors. Plos One. 2020;15(2) doi: 10.1371/journal.pone.0229087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Borys S., Perlman D. Gender Differences in Loneliness. Pers Soc Psychol Bull. 1985;11(1):63–74. [Google Scholar]
- 50.Dahlberg L., Agahi N., Lennartsson C. Lonelier than ever? Loneliness of older people over two decades. Arch Gerontol Geriatr. 2018;75:96–103. doi: 10.1016/j.archger.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 51.Beutel M.E., et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17(1):97. doi: 10.1186/s12888-017-1262-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barreto M., et al. Loneliness around the world: age, gender, and cultural differences in loneliness. Personal Individ Differ. 2021;169 doi: 10.1016/j.paid.2020.110066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hawkley L.C., et al. From social structural factors to perceptions of relationship quality and Loneliness: the Chicago health, aging, and social relations study. J Gerontol Ser B. 2008;63(6):S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maes M., et al. Gender differences in Loneliness across the lifespan: a meta-analysis. Eur J Pers. 2019;33(6):642–654. [Google Scholar]
- 55.Stack S. Marriage, family and loneliness: a cross-national study. Sociol Perspect. 1998;41(2):415–432. [Google Scholar]
- 56.Fokkema T., De Jong Gierveld J., Dykstra P.A. Cross-national differences in older adult loneliness. J Psychol. 2012;146(1–2):201–228. doi: 10.1080/00223980.2011.631612. [DOI] [PubMed] [Google Scholar]
- 57.Umberson D., Williams K. Marital quality, health, and aging: gender equity? J Gerontol B Psychol Sci Soc Sci. 2005;60(Special_Issue_2):S109–S113. doi: 10.1093/geronb/60.special_issue_2.s109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McQuaid R.J., et al. The burden of loneliness: implications of the social determinants of health during COVID-19. Psychiatry Res. 2021;296 doi: 10.1016/j.psychres.2020.113648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bu F., Steptoe A., Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–34. doi: 10.1016/j.puhe.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hurria A., et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol. 2011;29(25):3457–3465. doi: 10.1200/JCO.2011.34.7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Magnuson A., et al. Development and validation of a risk tool for predicting severe toxicity in Older Adults receiving chemotherapy for early-stage breast Cancer. J Clin Oncol. 2021;39(6):608–618. doi: 10.1200/JCO.20.02063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lapin B.R., et al. Evidence of stability in patient-reported Global Health during the COVID-19 pandemic. Value Health J Int Soc Pharmacoecon Outcomes Res. 2021;24(11):1578–1585. doi: 10.1016/j.jval.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peckham A., et al. Aging through the time of COVID-19: a survey of self-reported healthcare access. BMC Health Serv Res. 2021;21(1):1355. doi: 10.1186/s12913-021-07353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Deckx L., van den Akker M., Buntinx F. Risk factors for loneliness in patients with cancer: a systematic literature review and meta-analysis. Eur J Oncol Nurs. 2014;18(5):466–477. doi: 10.1016/j.ejon.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 65.Philip K.E.J., et al. Social isolation, loneliness and physical performance in older-adults: fixed effects analyses of a cohort study. Sci Rep. 2020;10(1):13908. doi: 10.1038/s41598-020-70483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a Meta-analytic review. PLoS Med. 2010;7(7) doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Penninx B.W., et al. Effects of social support and personal coping resources on mortality in older age: the longitudinal aging study Amsterdam. Am J Epidemiol. 1997;146(6):510–519. doi: 10.1093/oxfordjournals.aje.a009305. [DOI] [PubMed] [Google Scholar]
- 68.Cacioppo J.T., Hawkley L.C. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jacobs J.M., et al. Global sleep satisfaction of Older people: the Jerusalem cohort study. J Am Geriatr Soc. 2006;54(2):325–329. doi: 10.1111/j.1532-5415.2005.00579.x. [DOI] [PubMed] [Google Scholar]
- 70.Friedman E.M., et al. Social relationships, sleep quality, and interleukin-6 in aging women. Proc Natl Acad Sci. 2005;102(51):18757–18762. doi: 10.1073/pnas.0509281102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thurston R.C., Kubzansky L.D. Women, loneliness, and incident coronary heart disease. Psychosom Med. 2009;71(8):836. doi: 10.1097/PSY.0b013e3181b40efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hawkley L.C., et al. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21(1):152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- 73.Kraav S.L., et al. Loneliness and social isolation increase cancer incidence in a cohort of Finnish middle-aged men. A longitudinal study. Psychiatry Res. 2021;299 doi: 10.1016/j.psychres.2021.113868. [DOI] [PubMed] [Google Scholar]
- 74.Cole S.W., et al. Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proc Natl Acad Sci. 2015;112(49):15142–15147. doi: 10.1073/pnas.1514249112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kiecolt-Glaser J.K., et al. Psychosocial modifiers of immunocompetence in medical students. Psychosom Med. 1984;46(1):7–14. doi: 10.1097/00006842-198401000-00003. [DOI] [PubMed] [Google Scholar]
- 76.Hanson B.S., et al. Social support and quitting smoking for good. Is there an association? Results from the population study, “men born in 1914,” Malmö, Sweden. Addict Behav. 1990;15(3):221–233. doi: 10.1016/0306-4603(90)90065-6. [DOI] [PubMed] [Google Scholar]
- 77.Locher J.L., et al. Social isolation, support, and capital and nutritional risk in an older sample: ethnic and gender differences. Soc Sci Med. 2005;60(4):747–761. doi: 10.1016/j.socscimed.2004.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Eriksen W., Sandvik L., Bruusgaard D. Social support and the smoking behaviour of parents with preschool children. Scand J Soc Med. 1997;25(2):93–99. doi: 10.1177/140349489702500206. [DOI] [PubMed] [Google Scholar]
- 79.Broman C.L. Social relationships and health-related behavior. J Behav Med. 1993;16(4):335–350. doi: 10.1007/BF00844776. [DOI] [PubMed] [Google Scholar]
- 80.Dorfman R.A., et al. Screening for depression among a well elderly population. Soc Work. 1995;40(3):295–304. [PubMed] [Google Scholar]
- 81.Schoevers R.A., et al. Risk factors for depression in later life; results of a prospective community based study (AMSTEL) J Affect Disord. 2000;59(2):127–137. doi: 10.1016/s0165-0327(99)00124-x. [DOI] [PubMed] [Google Scholar]
- 82.Faulkner K.A., et al. Is social integration associated with the risk of falling in older community-dwelling women? J Gerontol A Biol Sci Med Sci. 2003;58(10):M954–M959. doi: 10.1093/gerona/58.10.m954. [DOI] [PubMed] [Google Scholar]
- 83.Cordova M.J., Riba M.B., Spiegel D. Post-traumatic stress disorder and cancer. Lancet Psychiatry. 2017;4(4):330–338. doi: 10.1016/S2215-0366(17)30014-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kadambi S., et al. Social support for older adults with cancer: young International Society of Geriatric Oncology review paper. J Geriatr Oncol. 2020;11(2):217–224. doi: 10.1016/j.jgo.2019.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Applebaum A.J., et al. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psycho-oncology. 2014;23(3):299–306. doi: 10.1002/pon.3418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lim J.W., Zebrack B. Social networks and quality of life for long-term survivors of leukemia and lymphoma. Support Care Cancer. 2006;14(2):185–192. doi: 10.1007/s00520-005-0856-x. [DOI] [PubMed] [Google Scholar]
- 87.Sammarco A., Konecny L.M. Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncol Nurs Forum. 2008;35(5):844–849. doi: 10.1188/08.ONF.844-849. [DOI] [PubMed] [Google Scholar]
- 88.Filazoglu G., Griva K. Coping and social support and health related quality of life in women with breast cancer in Turkey. Psychol Health Med. 2008;13(5):559–573. doi: 10.1080/13548500701767353. [DOI] [PubMed] [Google Scholar]
- 89.Adam A., Koranteng F. Availability, accessibility, and impact of social support on breast cancer treatment among breast cancer patients in Kumasi, Ghana: a qualitative study. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li M.-Y., et al. Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: a cross-sectional study. Health Qual Life Outcomes. 2016;14(1):73. doi: 10.1186/s12955-016-0481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nausheen B., et al. Social support and cancer progression: a systematic review. J Psychosom Res. 2009;67(5):403–415. doi: 10.1016/j.jpsychores.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 92.National Academies of Sciences, E. and Medicine . The National Academies Press; Washington, DC: 2020. Social isolation and loneliness in older adults: Opportunities for the health care system; p. 316. [PubMed] [Google Scholar]
- 93.Gardiner C., Geldenhuys G., Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community. 2018;26(2):147–157. doi: 10.1111/hsc.12367. [DOI] [PubMed] [Google Scholar]
- 94.Williams C.Y.K., et al. Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: a rapid systematic review. Plos One. 2021;16(2) doi: 10.1371/journal.pone.0247139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tsai H.H., et al. Videoconference program enhances social support, loneliness, and depressive status of elderly nursing home residents. Aging Ment Health. 2010;14(8):947–954. doi: 10.1080/13607863.2010.501057. [DOI] [PubMed] [Google Scholar]
- 96.Jansson A., Pitkälä K.H. Circle of friends, an encouraging intervention for alleviating loneliness. J Nutr Health Aging. 2021;25(6):714–715. doi: 10.1007/s12603-021-1615-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Creswell J.D., et al. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun. 2012;26(7):1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nicholson N.R., Jr., Shellman J. Decreasing social isolation in older adults: effects of an empowerment intervention offered through the CARELINK program. Res Gerontol Nurs. 2013;6(2):89–97. doi: 10.3928/19404921-20130110-01. [DOI] [PubMed] [Google Scholar]
- 99.Banks M.R., Banks W.A. The effects of group and individual animal-assisted therapy on loneliness in residents of long-term care facilities. Anthrozoös. 2005;18(4):396–408. [Google Scholar]
- 100.Cattan M., Kime N., Bagnall A.M. The use of telephone befriending in low level support for socially isolated older people--an evaluation. Health Soc Care Community. 2011;19(2):198–206. doi: 10.1111/j.1365-2524.2010.00967.x. [DOI] [PubMed] [Google Scholar]
- 101.Fokkema T., Knipscheer K. Escape loneliness by going digital: a quantitative and qualitative evaluation of a Dutch experiment in using ECT to overcome loneliness among older adults. Aging Ment Health. 2007;11(5):496–504. doi: 10.1080/13607860701366129. [DOI] [PubMed] [Google Scholar]