Abstract
Tackling mental health has become a priority for governments around the world because it influences not only individuals but also the whole society. As people spend a majority of their time (i.e., around 90%) in buildings, it is pivotal to understand the relationship between built environment and mental health, particularly during COVID-19 when people have experienced recurrent local and national lockdowns. Despite the demonstration by previous research that the design of the built environment can affect mental health, it is not clear if the same influence pattern remains when a ‘black swan’ event (e.g., COVID-19) occurs. To this end, we performed logistic regression and hierarchical regression analyses to examine the relationship between built environment and mental health utilising a data sample from the United Kingdom (UK) residents during the COVID-19 lockdown while considering their social demographics. Our results show that compared with depression and anxiety, people were more likely to feel stressed during the lockdown period. Furthermore, general house type, home workspace, and neighbourhood environment and amenity were identified to have significantly contributed to their mental health status. With the ensuing implications, this study represents one of the first to inform policymakers and built environment design professionals of how built environment should be designed to accommodate features that could mitigate mental health problems in any future crisis. As such, it contributes to the body of knowledge of built environment planning by considering mental health during the COVID-19 lockdown.
Keywords: Built environment design, COVID-19 lockdowns, Mental health, Regression analysis, The UK
1. Introduction
As maintained by the World Health Organisation (2020), mental health is one of the three basic components of health, along with physical and social well-being. People with good mental health can be defined as individuals who can: (1) realise their own abilities; (2) cope with the normal stresses of life; (3) work productively; and (4) make a contribution to their community (World Health Organisation, 2018). However, a large number of people fail to meet this standard. In England, for example, National Health Service (2021) disclosed that one in four adults experience mental illness. Data from China (Huang and Zhao, 2020a, Huang and Zhao, 2020b; Liu et al., 2020; Zhang and Ma, 2020), Europe (Banna et al., 2020; Gualano et al., 2020), Australia (Fisher et al., 2020), and the United States (Fitzpatrick et al., 2020) have reported that mental health illness often appears in the form of depression, anxiety and stress. Such mental health disorders, as reported by Bloom et al. (2011), incurred around $2.5 trillion loss globally in 2010, and this figure will rise to $6.0 trillion by 2030. According to Rosenberg et al. (2020), this situation has been exacerbated by the unprecedented COVID-19 pandemic where people experienced persistent mental health problems due to the considerably long lockdown/quarantine, and the health system's failure to contain it. These staggering statistics highlight that mental health has become an issue that cannot be ignored.
Studies have been conducted to investigate the causes of mental health (e.g., environment, social relationships and employment) and subsequent countermeasures (Weich et al., 2002; Nurse et al., 2003; Hudson, 2010; Sullivan and Chang, 2011; Appelqvist-Schmidlechner et al., 2020). Among them, increasing attention has been paid to explore its relationship with the built environment, given that people spend 90% of their time in buildings and frequently interact with their surrounding built environment in their daily lives (Klepeis et al., 2001; Evans, 2003; Wright and Kloos, 2007; Reichert et al., 2020). For example, Sullivan and Chang (2011) found that the lack of green space, and crowded and noisy places are usually associated with psychological distress and even depression. In terms of housing tenure, Berglund et al. (2017) reported that poor psychological well-being was found to be lowest in people living in private houses. It has also been shown that good indoor environmental quality (e.g., thermal comfort, lighting, and natural view) can be conducive to decreased stress, reduced anxiety and improved mood (Santamouris et al., 2014; Akbari et al., 2021). Hence, built environment design should aim to sustain mental health of the residents in addition to its physical and cognitive functions.
During COVID-19 pandemic lockdowns, people spent much more time (i.e., 24/7) at home than before, rendering mental health an ever-increasing concern (Dawson and Golijani-Moghaddam, 2020; Singh et al., 2020). This is well illustrated in the doubled prevalence of moderate-to-severe depressive and generalized anxiety symptoms following the restrictions put in place to halt the spread of COVID-19 (Fisher et al., 2021). Markedly, the pandemic has imposed greater challenges on the pre-COVID situation where disability was mainly caused by mental health disorders in the UK (Mental Health Taskforce, 2016), and that the overall mental health condition is still deteriorating (Office for National Statistics - ONS, 2017). Although existing studies have identified built environment design as a contributing factor to mental health, its specific influence during the COVID-19 lockdowns, when people spent almost 24 h at home, remains unclear. In addition, previous studies often focused on a single set of characteristics of the built environment, such as the construction of new roads around the neighbourhood (Egan et al., 2003), neighbourhood social and physical characteristics (Cerda et al., 2013), and indoor environment quality (Burns et al., 2019), without considering the agglomeration effect (i.e., how the addition of multiple built environment factors impacts their effect). More importantly, ‘black swan’ events similar to COVID-19 are likely to intrude in the future as had been estimated by Cabinet Office (2017), indicating an additional degree of uncertainty that surrounds the relationship between the built environment and mental health (Hoisington et al., 2019).
To fill this knowledge void, this work aims to examine how built environment impacts the mental health of residents during COVID-19 lockdowns in the UK, and identify design approaches that may have been previously overlooked. Notably, the built environment is defined as ‘‘the physical form of communities’’ (Brownson et al., 2009), which can include land-use patterns, large- and small-scale built and natural features, and the transport system. For the purpose of economy and considering the context of the UK, this study deliberately delimits itself to three categories in the environment of residential buildings, namely, general house type, indoor environment quality, and neighbourhood amenity quality. It also considers the residents' social demographics. To do so, this present study employs the widely-recognised Patient Health Questionnaire (PHQ-2) (Scoppetta et al., 2020), General Anxiety Disorder (GAD-7) (Spitzer et al., 2006), and Perceived Stress Scale (PSS-4) (Cohen et al., 1983) as proxies for mental health (i.e., the terms ‘depression’, ‘anxiety’ and ‘stress’ are used interchangeably with ‘poor mental health’ in this article), and collects information regarding the built environment design during the COVID-19 lockdowns in the UK through an online questionnaire survey. When analysing the collected data, the logistic regression model and hierarchical regression model are adopted to demonstrate the incremental changes where different combinations of independent variables exist. By addressing the question ‘how does built environment, and in particular, social demographics, general house type, indoor environmental quality, and neighbourhood amenity quality, affect mental health during the COVID-19 lockdown in the UK?’, this research contributes to providing policymakers and built environment design professionals with knowledge on how built environment can be designed to mitigate mental health problems in any future crisis.
2. Literature review
2.1. Measures of mental health
Mental health of the general population has been a long-standing topic in the agenda of the society and research. Depression, anxiety and stress are distinct but interrelated measures of mental health. People experiencing depression often struggle with anxiety, i.e., shouldering intensifying feelings of anxiety, fear, worry, and/or panic, which adversely interferes with everyday activities (Centers for Disease Control and Prevention, 2021). Stress, on the other hand, can trigger physical and mental symptoms and changes in behaviour, although sometimes it can be helpful or even motivating (National Health Service, 2019). Bakioğlu et al. (2021) state that COVID-19 has increased people's stress levels and further activated anxiety and depression. Over time, PHQ-9, GAD-7 and PSS have become the well-known measures of depression, anxiety and stress, respectively. According to Kroenke et al. (2001), the validity and brevity of PHQ-9 make it a useful clinical and research tool in diagnosing depression and measuring its severity. PHQ-2, in comparison, has been confirmed by Scoppetta et al. (2020) to be another useful method to preliminarily screen depression before PHQ-9 intervenes. Hence, studies (e.g., González-Sanguino et al., 2020; Shapiro et al., 2020, and Twenge and Joiner, 2020) have shown that PHQ-2 is convenient and effective to detect the early-stage mental health of residents during the pandemic. According to Spitzer et al. (2006), GAD-7 is one of the common approaches to diagnosing anxiety and assessing its severity, and its good reliability, validity and effectiveness have made great contributions to the clinical research. During the pandemic, scholars (e.g., Dawel et al., 2020, Fisher et al., 2020, and Huang and Zhao, 2020a, Huang and Zhao, 2020b) have widely adopted GAD-7 in the study of residents' anxiety and their anxiety level. For stress, Cohen et al. (1983) emphasise that PSS-4 is characterised with briefness and management-friendly possesses, which makes assessing the individual's stress over the phone possible. As a short version of PSS, Warttig et al. (2013) argue that PSS-4 continues to remain good reliability and validity. A germane case is that Li and Leung (2020) successfully apply PSS-4 to study the stress of Filipino workers in Hong Kong in view of the COVID-19.
In the research of relative importance of physical and social neighbourhood characteristics to depression, Helbich et al. (2019) find that personal attributes seem to be more important than neighbourhood characteristics. That means young adults and persons with low income, low education, unemployment and divorce are more likely to be depressed. Similarly, depression and anxiety seem to be negatively correlated with age (Jorm, 2000), which indicates that as people get older, the risk of feeling depressed and anxious reduces. In terms of gender, the psychological effects of housing are found by McLean et al. (2011) to be different on men and women. In addition, the residents' income (Evans et al., 2003), education (Jensen et al., 2018), and ethnicity (Proto and Quintana-Domeque, 2021), to a large extent, impact the housing quality and/or mental health. Nevertheless, how the social demographics interacts with mental health within residents’ living built environment during the COVID-19 lockdowns has not been fully unpacked.
2.2. Built environment and mental health
There is an array of built environment factors that can influence mental health. It is common observation that people who reside in houses or low-rise buildings have better mental health (see, for example, Evans et al., 2003). This contrasts with the relatively worse mental health reflected in residents of high-rise buildings due to the poorer quality of semi-public areas (e.g., shared entrances, communal space, and corridors) (Barros et al. 2019), which can instigate a lower sense of control and greater awareness of anti-social behaviour (Gibson et al., 2011). For indoor environmental quality, Al horr et al. (2016) consider thermal comfort to be the most important variable. It is also complicated, as a warmer temperature can cause fatigue and lower productivity (Tanabe et al., 2007) while a lower temperature has been associated with depression and anxiety (Thomson and Snell, 2013). Annoyance, as the most common result of aural discomfort is associated with high levels of perceived stress (Jensen et al., 2018), indicating the importance of a suitable acoustic environment in which to live and/or work (Mui and Wong, 2006). Similarly, Codinhoto et al. (2009) and Elsadek et al. (2020) argue that well-designed lighting and high-quality window views (e.g., of urban and green spaces) can contribute to positive physical, physiological, and psychological health. For indoor air quality, exposure to PM2.5, toxins and malodorous pollutants often directly or indirectly lead to negative mental states (e.g., anxiety) (Oiamo et al., 2015; Power et al., 2015; Beemer et al., 2019). However, this effect can be alleviated through ventilation by opening windows, installing mechanical facilities (Beemer et al., 2019), and emerging technologies such as sensors (Awada et al., 2021). Notwithstanding this, Allen et al. (2015) noted their potential shortfalls, such as increased concentrations of pollutants indoors and energy consumption. Furthermore, the neighbourhood environment - which includes surrounding green spaces (Nutsford et al., 2013), traffic nuisance (Putrik et al., 2015), shops, working and education amenities (Barnett et al., 2018) - is another element of built environment that is attested to be significantly correlated with mental health performance, in which the neighbourhood's social characteristics also have a role to play (Saarloos et al., 2011; Helbich et al., 2019).
Existing knowledge of the impacts of built environment design on mental health from the perspectives of social demographics, general house attribute, indoor environmental quality and neighbourhood amenity quality has been critically reviewed. It is identified that good built environment design can contribute to positive mental health. However, with the stringent restrictions in place, the probability of residents suffering from mental health problems among residents is more than incremental. Staying at home during the lockdowns has turned built environment into a major factor affecting mental health. Although the impact of built environment on mental health has been explored in prior studies, it is not clear whether and how built environment design can impact mental health in extreme events, such as the COVID-19 lockdowns. It is against such a backdrop that this study becomes novel and thus contributes to the body of knowledge of built environment by examining how built environment under uncertainties (e.g., COVID-19 lockdowns) impacts people's mental health.
3. Method
3.1. Research strategy and design
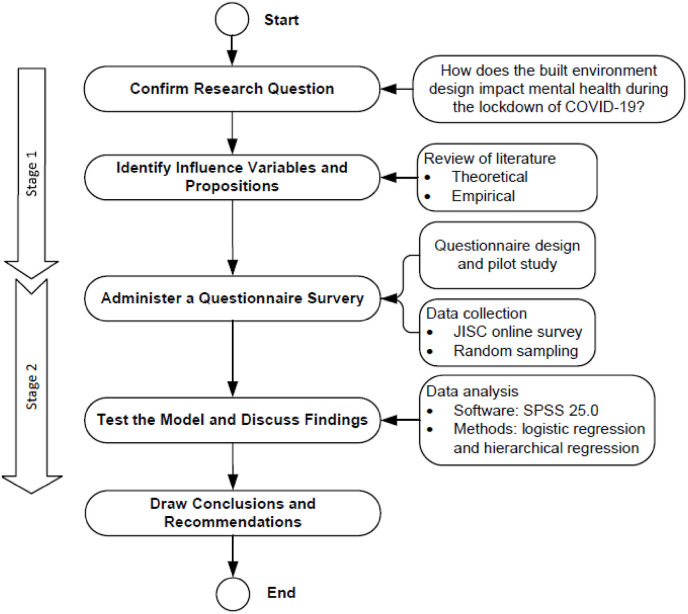
The epistemological design of empiricism was employed to acquire knowledge on the impact of built environment design on mental health during the COVID-19 lockdown (Amaratunga et al., 2002). Accordingly, we adopted a two-stage research design (Fig. 1 ) to navigate the research process. In stage one, a comprehensive literature review was conducted to identify the built environment variables that may impact mental health during the COVID-19 lockdown. To ensure validity of the data collection, a pilot study was undertaken where five experts who assume more than 10-year experience of built environment and psychology in the UK were consulted as part of the questionnaire design. In stage two, using the random sampling described in Arsham (2005), the fine-tuned questionnaire survey was administered through JISC online survey, a popular online survey platform supported by the authors’ institutions, to residents in the UK. After that, the logistic regression model (Berglund et al., 2017) and hierarchical regression model (Radmacher and Martin, 2001) were performed using SPSS 25.0 to analyse the data. Reliability analyses were also undertaken to examine if the independent variable can statistically explain the dependent variable. Based on these analyses, the relationship between various parameters of built environment and mental health during the COVID-19 lockdown is revealed in Section 4 , and the implications are discussed in Section 5.
Fig. 1.
Research design.
3.2. Data collection
Due to the lockdown restrictions, an online questionnaire survey was deployed as it is capable of generating reliable and effective results if designed carefully (Taherdoost, 2016). Approved by the ethics committee of the University of Reading, UK, the survey was carried out from May to July 2020 when the UK was in its first lockdown. Respondents were invited to answer questions in the first part about their personal and family information, such as age, gender, ethnicity, employment status, etc., followed by the second to the fourth part regarding the conditions of the built environment they lived in at that time and their satisfaction with the built environment design. For example, questions about the house size, the house type, satisfaction level (i.e., measured by a seven-point Likert scale) with indoor environmental quality, thermal comfort, acoustic environment, natural light and window view, and the surrounding open space and food and convenience shops were asked. In the fifth part, PHQ-2, GAD-7 and PSS-4 were used to test the mental health outcomes during the lockdown, given their validated clinical and research use (González-Sanguino et al., 2020; Fisher et al., 2020; Li and Leung, 2020). PHQ-2, consisting of two questions with four possible responses (i.e., 0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day), is a measurement of depression (Kroenke et al., 2001; Scoppetta et al., 2020). According to Spitzer et al. (2006), anxiety can be usefully evaluated using the seven-item subscales in GAD-7. The scores of the four possible responses in GAD-7 are the same as in PHQ-2. PSS-4 consists of four questions with each having five possible responses to measure stress (Cohen et al., 1983). In questions 1 and 4, the scores of the five possible responses are never = 0, almost never = 1, sometimes = 2, fairly often = 3 and very often = 4, while in questions 2 and 3, the scores are opposite from those in questions 1 and 4. In short, a higher score indicates a poorer mental health status. A comment box was provided in the last section to solicit information about what changes the respondents would like to make to their living environment.
3.3. Data analysis and method justification
A total of 285 participants started and completed the survey, among whom 237 were based in the UK, 46 overseas, and two preferred not to disclose their location. Given that this research targets UK residents, only the 237 entries from the UK were retained for data analysis. As 1000 questionnaires were distributed and expected, the response rate is 23.70%, which is acceptable for research of this nature (De Vaus, 2001). In addition, a study of a similar ilk by Tan et al. (2020) investigated the relationship between workspace design and employees’ well-being using a sample of 195 participants. While we acknowledge that there are studies (e.g., Amerio et al., 2020) that have employed a much bigger sample size, it is widely considered that sample sizes equal to or greater than 30 are sufficient for the central limit theorem to hold (Chang et al., 2006). In addition, a statistical power analysis using G*Power (Faul et al., 2007) was conducted, indicating that 214 participants (this study involved 237 participants) would make the regression model with 40 independent variables sensitive enough to detect an effect size of f 2 = 0.15 (α = 0.05; power = 0.80). Therefore, data collected here were considered to be adequate for addressing the research question.
In order to analyse the data, regression analysis, including logistic regression and hierarchical regression, was adopted because it is robust in identifying the most appropriate fit to describe the relationship between the dependent variables and a set of independent variables (Pohar et al., 2004). Logistic regression analysis has been widely applied in built environment and psychology-related studies. For example, Lai et al. (2009) used logistic regression analysis to find the relationship between occupants' acceptance and the indoor environmental quality in residential buildings. In addition, logistic regression analysis has been applied to explore the impacts of neighbourhood characteristics on mental health among African Americans and Whites who live in a racially integrated urban community (Gary et al., 2007). Another example is that the relationships between the neighbourhood environment characteristics and self-related health and depression symptoms are explored in multilevel logistic regression models (Putrik et al., 2015). Similar to Radmacher and Martin (2001) and Berglund et al. (2017), in this study, each set of variables (i.e., social demographics, general house, indoor environmental quality and neighbourhood amenity) were added into the logistic regression and hierarchical regression models step by step. For example, the first step was to study depression and social demographic information. The second step was to study depression, social demographic information and general house attribute and compare the variables’ significance differences between step two and step one. It is iterative until all four sets of variables were integrated into the model and the reference category in each step was listed under the tables shown below. This process can provide a deep understanding on how each set of variables impacts mental health individually and collectively, and can reflect the changes in their significance.
In addition, when interpretating the mental health outcome, if the score is less than or equal to three in PHQ-2, the participant shows ‘absence of significant (or major) depression’, while the participant has ‘major depression’ if the score is 4, 5, or 6 (Lowe et al., 2005). Although there are four categories in GAD-7, it is usually agreed that a degree of 0–9 means ‘no major anxiety’ and ‘10 to 21’ indicates ‘major anxiety’ (Spitzer et al., 2006). The discrete nature of depression and anxiety also suits the logistic regression as it is appropriate to deal with this dichotomous problem (Tung, 1985). Furthermore, to perform the logistic regression analysis, the recommended number of cases per variable (n/P) should be greater than 3:1 and lower than 20:1 (Cattell, 1978; Hair et al., 1979). In this study, the number of samples and the variables were 237 and 40, respectively, which yields the value of n/P as 5.93:1 and thus meets the threshold. By contrast, according to Lee (2012), the interpretation of the outcome of stress in PSS-4 is continuous (i.e., the higher the score is, the more stressed the respondent is likely to be). In this instance, following the approach of Lee (2012), the hierarchical regression model was applied to cope with this situation. Given that there were four sets of variables, hierarchical regression was capable of showing if each set of variables is statistically significant in explaining the dependent variable (i.e., mental health during the COVID-19 lockdown) and measuring the significance differences by adding a set of variables (Rutter and Gatsonis, 2001). Owing to these attributes, logistic regression was selected to examine depression and anxiety whilst hierarchical regression was used to study stress.
4. Results
4.1. Overall descriptive analysis
4.1.1. Social demographics outcome
Among the received responses, 71.73% of the participants were female and the majority of the participants (i.e., 92.83%) lived in England during the COVID-19 lockdown. For ethnicity distribution, ‘White-British, Irish and other’ took up 59.92%, followed by ‘Chinese/Chinese British’ at 18.57%. In addition, 48.52% of the participants were between 18 and 29 years old, whereas the percentage of participants over 60 years old was only 5.49%. Participants were mainly students and full-time employees, accounting for 34.18% and 32.49%, respectively. The total household net income of most participants was no more than £90,000 per year. A minority of participants lived in houses with more than five people and 64.56% participants had no children in their houses during the lockdown. Moreover, the proportion of tenants and houseowners were almost evenly divided. In terms of COVID-19 issues, 87.34% participants reported that nobody was infected with COVID-19 in their houses during the lockdown. This is consistent with the data provided by the UK's Office for National Statistics (2020) where around 6.2% of people tested positive for COVID-19 between April 26 and July 26, 2020 (Data in this study were collected from May to July 2020 as mentioned earlier). Although ‘infections’ seem to be slightly higher, there could be time lapse when cases were reported. In addition, among the 12.66% who reported ‘positive’ in this study, 10% chose the option ‘suspected and recovered’. This again validates the reliability of the data collected. A visualised demographic analysis of participants can be found in the Appendix.
4.1.2. Mental health outcome
Based on the interpretation of the scores as mentioned above, Fig. 2 presents the mental health conditions of the participants. Of the 237 participants, the percentage that showed 'absence of major depression' was 80.17%, which implies that only a minority of respondents (i.e., 19.83%) felt depressed during the COVID-19 lockdown (Fig. 2a). For anxiety (Fig. 2b), 102 participants had 'no-minimal anxiety' and 81 had 'mild anxiety'. The numbers of the participants with 'moderate anxiety' and 'severe anxiety' were similar, at 29 and 25, respectively. The proportion of the participants with 'no-minimal anxiety' and 'mild anxiety' (i.e., no major anxiety) was 77.22%, which suggests that most participants did not feel anxious or had slight sense of anxiety during the COVID-19 lockdown. Stress was evaluated using continuous numeric variables as PSS-4 has no formal cut-off points. As can be seen in Fig. 2c, the stress score of most participants (i.e., 71.73%) is between 4 and 9. Notably, the number of participants with a stress score of 8 (i.e., 55) is the highest. Compared with anxiety and depression, stress was revealed to be the most obvious mental health problem of residents during the COVID-19 lockdown.
Fig. 2.
Distribution analysis of the mental health outcomes of residents.
4.2. Reliability analysis
Cronbach's alpha was selected as an indicator of scale reliability to measure the internal consistency. Among the 20 items tested, the Cronbach's alpha index was calculated to be 0.730, which exceeds the minimum acceptable level (Nunnally and Bernstein, 1994). Furthermore, in order to investigate whether the independent variables (i.e., social demographics, general house, indoor environmental quality, and neighbourhood amenity quality) can statistically explain the dependent variable (i.e., depression, anxiety, or stress), three separate reliability analyses were conducted as shown in Table 1 and Table 2 .
Table 1.
Model reliability for depression and anxiety.
| Observed | Predicted |
||||
|---|---|---|---|---|---|
| Depression (Anxiety) |
Percentage Correct (%) | ||||
| No Depression (No) | Major depression (Yes) | ||||
| Step 1 | Depression (Anxiety) | No Depression (No) | 123 (119) | 7 (8) | 94.6 (93.7) |
| Major depression (Yes) | 27 (28) | 11 (13) | 28.9 (31.7) | ||
| Overall Percentage | 79.8 (78.6) | ||||
Note: data in brackets are that of anxiety.
Table 2.
Model reliability for stress.
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate | Durbin-Watson |
|---|---|---|---|---|---|
| 1 | .435 | .189 | .066 | 2.94421 | |
| 2 | .489 | .239 | .086 | 2.91182 | |
| 3 | .534 | .286 | .096 | 2.89604 | |
| 4 | .557 | .310 | .093 | 2.90072 | 1.915 |
Table 1 shows that the logistic regression analysis model can significantly explain the relationship between built environment and depression as well as anxiety with the correct prediction rate being 79.8% and 78.6%, respectively. In other words, the possibility of failing to simulate the interrelation (i.e., whether a variable is statistically significant in explaining the dependent variable - mental health) was only 20.2% or 21.4%. Similarly, the hierarchical regression analysis model demonstrated a satisfactory performance in showing the relationship between built environment and stress (Table 2). The Durbin-Watson value was calculated to be 1.915, suggesting that the model is statistically significant (i.e., no autocorrelation in the sample). This is becasue, acoording to Liberopoulos and Tsarouhas (2005), if the Durbin-Watson value is closer to 2, the model is more effective.
4.3. Relationship between built environment design and mental health
4.3.1. Depression during the COVID-19 lockdown
Table 3 shows the outcome of the logistic regression analysis model for depression and the differences between each model. For the sake of brevity, only the regression coefficient and significance of each variable are presented as they are sufficient to identify if a certain variable is statistically significant in explaining depression. The same principle applies to the rest of the models. In addition, all models were performed at the 95% confidence intervals.
Table 3.
Results of regression models on built environment design and depression.
| Variables | Step 1 |
Step 2 |
Step 3 |
Step 4 |
||||
|---|---|---|---|---|---|---|---|---|
| B | Sig. | B | Sig. | B | Sig. | B | Sig. | |
| Social demographics | ||||||||
| Ethnicity a | ||||||||
| Black/Black British-Caribbean, African, other | −20.370 | 1.000 | −20.017 | 1.000 | −20.615 | 1.000 | −21.657 | 1.000 |
| Mixed race – other | .940 | .589 | 1.880 | .304 | 2.023 | .274 | 2.490 | .199 |
| White – British, Irish, other | −.237 | .762 | .064 | .940 | −.028 | .975 | −.331 | .728 |
| Chinese/Chinese British | −1.082 | .238 | −1.269 | .193 | −1.382 | .173 | −1.435 | .177 |
| Middle Eastern/Middle Eastern British – Arab, Turkish, other | .334 | .757 | .781 | .510 | .893 | .465 | 1.021 | .421 |
| Other | −20.560 | .999 | −20.162 | .999 | −20.191 | .999 | −21.518 | .999 |
| Gender b | .115 | .809 | .214 | .679 | .146 | .790 | .263 | .653 |
| Age | −.525 | .037* | −.483 | .073 | −.506 | .078 | −.432 | .174 |
| Employment status c | ||||||||
| Self-employed | 1.217 | .206 | 1.002 | .303 | 1.292 | .209 | 1.066 | .356 |
| In part-time employment | .143 | .862 | .120 | .886 | .144 | .869 | −.238 | .799 |
| In full-time employment | .399 | .502 | .197 | .755 | .167 | .801 | .239 | .742 |
| Unable due to disability | 21.910 | 1.000 | 22.510 | 1.000 | 22.782 | 1.000 | 22.090 | 1.000 |
| Homemaker/full-time parent | −19.485 | .999 | −19.844 | .999 | −20.142 | .999 | −20.650 | .999 |
| Unemployed and seeking work | .314 | .693 | .384 | .636 | .502 | .559 | .573 | .522 |
| Furlough | −.972 | .408 | −.177 | .885 | −.184 | .885 | −.328 | .799 |
| Retired | 2.981 | .090 | 2.798 | .122 | 3.003 | .117 | 2.277 | .277 |
| Household income | −.108 | .068 | −.088 | .673 | −.044 | .847 | .076 | .747 |
| The number of people in the house | −.007 | .962 | .097 | .599 | .102 | .605 | .120 | .560 |
| Rent or own the house d | −.305 | .542 | .015 | .978 | .072 | .906 | .062 | .923 |
| Has anyone in your household had COVID-19 | ||||||||
| Suspected and recovered e | −41.445 | .999 | −60.676 | .999 | −60.399 | .999 | −62.768 | .999 |
| Suspected and still ill | −61.588 | .999 | −81.291 | .999 | −81.533 | .999 | −84.520 | .999 |
| No | −41.976 | .999 | −61.230 | .999 | −61.001 | .999 | −63.366 | .999 |
| General housef | ||||||||
| House size | −.242 | .260 | −.272 | .238 | −.255 | .287 | ||
| House type | ||||||||
| A house without a garden | 1.475 | .233 | 1.655 | .188 | 2.370 | .080 | ||
| An apartment with a balcony | .368 | .778 | .452 | .741 | .899 | .520 | ||
| An apartment with no balcony | .689 | .284 | .487 | .474 | .400 | .597 | ||
| A home with access to an outdoor communal area | −.543 | .691 | −.547 | .707 | −.147 | .924 | ||
| Other | −19.681 | .999 | −19.359 | .999 | −19.600 | .999 | ||
| Indoor environmental quality | ||||||||
| Natural light | −.077 | .655 | −.026 | .889 | ||||
| Thermal comfort | −.059 | .735 | −.110 | .560 | ||||
| Indoor air quality | .029 | .892 | .053 | .811 | ||||
| Acoustic environment | −.031 | .853 | .004 | .980 | ||||
| Window view | .061 | .717 | .021 | .905 | ||||
| Indoor physical activity space | −.095 | .606 | −.111 | .565 | ||||
| Home workspace | −.061 | .694 | −.090 | .588 | ||||
| Neighbourhood amenity quality | ||||||||
| Neighbourhood type g | ||||||||
| Town | 1.774 | .015* | ||||||
| Suburb | .351 | .681 | ||||||
| Rural | 1.341 | .198 | ||||||
| Proximity to the nearest open space | −.008 | .978 | ||||||
| Proximity to the nearest shops | .087 | .772 | ||||||
Note: a ‘Asian/British-Indian, Pakistani, Bangladeshi, other’ is used as the reference category; b ‘Male’ is used as the reference category; c ‘Still at school’ is used as the reference category; d ‘Rent’ is used as the reference category; e ‘Yes, diagnosed and recover’ is used as the reference category; f ‘A house with a garden’ is used as the reference category; and g ‘City’ is used as the reference category.
The first step is to explore the relationship between social demographics and depression. Results suggest that age (B = −0.525, p = 0.037) is significantly associated with depression, with younger people reporting being more depressed than older people. Although all other variables are not significant, household income is marginally significant (B = −0.108, p = 0.068), with people having higher annual income reporting less depression symptoms. In the second step and third step, after adding variables of general house attribute and indoor environmental quality, there is no significant variable shown to be associated with depression. Interestingly, even age becomes insignificant with the p values rising to 0.073 and 0.078. However, in the final step the neighbourhood type is significantly related to depression after adding the neighbourhood amenity quality variables. Living in a town (B = 1.774, p = 0.015) is associated with greater depression compared with living in a city. This could be because it is easier and faster for residents in the city to access neighbourhood amenities. Supporting evidence can also be found in Medlock et al. (2021), where concerns for COVID-19 transmission have considerably reduced the use of public transport. In the current study, residents of towns may need to spend more time outside and using public transport to buy food during the lockdown, which may lead to worries about contracting the disease.
4.3.2. Anxiety during the COVID-19 lockdown
Table 4 shows the outcome of the logistic regression analysis model for anxiety and the differences between each model. Similarly, the first step is to explore the relationship between social demographics and anxiety. Age (B = −0.543, p = 0.039) is significantly associated with anxiety, indicating that older people are less anxious than younger people. Differing from depression, age (B = −0.623, p = 0.024) remains to be significant after adding the general house variables in the second step. This is perhaps because older people are less sensitive to the house type and house size when it comes to anxiety. It is possible that older people who live in a bigger house suffer less from anxiety than younger people during the lockdown. In the third model, both age and house type are significantly related to anxiety after adding indoor environmental quality variables. Such a phenomenon reveals that those who are younger (B = −0.741, p = 0.014) or living a house without a garden (B = 2.562, p = 0.037) manifest greater anxiety compared with those older or living in a house with a garden. In the fourth step, however, after adding neighbourhood amenity quality variables, age is no longer significant, whereas house type and neighbourhood type become significantly associated with anxiety. Here, despite the social background, people living in a house without a garden (B = 3.240, p = 0.018) are more likely to feel anxious compared with those living in a house with a garden. In addition, living in the town (B = 2.277, p = 0.002) is associated with greater anxiety compared with living in the city.
Table 4.
Results of regression models on built environment design and anxiety.
| Variables | Step 1 |
Step 2 |
Step 3 |
Step 4 |
||||
|---|---|---|---|---|---|---|---|---|
| B | Sig. | B | Sig. | B | Sig. | B | Sig. | |
| Social demographics | ||||||||
| Ethnicity | ||||||||
| Black/Black British-Caribbean, African, other | −20.373 | 1.000 | −19.494 | 1.000 | −19.744 | 1.000 | −22.151 | 1.000 |
| Mixed race – other | 1.297 | .451 | 2.101 | .246 | 2.385 | .198 | 2.269 | .253 |
| White – British, Irish, other | −.417 | .580 | .058 | .943 | .127 | .884 | −.143 | .884 |
| Chinese/Chinese British | −1.714 | .068 | −1.565 | .116 | −1.718 | .095 | −1.979 | .084 |
| Middle Eastern/Middle Eastern British – Arab, Turkish, other | .383 | .719 | .943 | .406 | 1.152 | .329 | 1.029 | .434 |
| Other | .036 | .975 | .049 | .971 | −.024 | .987 | −.662 | .682 |
| Gender | .292 | .542 | .467 | .364 | .477 | .380 | .645 | .271 |
| Age | −.543 | .039* | −.623 | .024* | −.741 | .014* | −.682 | .050 |
| Employment status | ||||||||
| Self-employed | 1.194 | .223 | 1.162 | .237 | 1.492 | .154 | .865 | .478 |
| In part-time employment | −.387 | .674 | −.303 | .745 | −.392 | .690 | −1.197 | .283 |
| In full-time employment | −.023 | .969 | −.104 | .864 | −.059 | .925 | −.233 | .746 |
| Unable due to disability | 21.423 | 1.000 | 20.397 | 1.000 | 20.264 | 1.000 | 19.130 | 1.000 |
| Homemaker/full-time parent | −19.642 | .999 | −19.472 | .999 | −18.931 | .999 | −19.306 | .999 |
| Unemployed and seeking work | .141 | .861 | .140 | .866 | .156 | .857 | .218 | .816 |
| Furlough | 1.259 | .170 | 1.575 | .110 | 1.792 | .096 | 1.132 | .309 |
| Retired | −17.442 | .999 | −17.232 | .999 | −16.950 | .999 | −18.236 | .999 |
| Household income | .035 | .851 | .095 | .644 | .136 | .539 | .301 | .201 |
| The number of people in the house | −.079 | .596 | −.177 | .340 | −.247 | .227 | −.218 | .326 |
| Rent or Own the house | −.637 | .213 | −.521 | .355 | −.332 | .590 | −.464 | .490 |
| Has anyone in your household had COVID-19 | ||||||||
| Suspected and recovered | −41.267 | .999 | −42.134 | .999 | −42.313 | .999 | −45.527 | .999 |
| Suspected and still ill | −63.607 | .999 | −65.598 | .999 | −65.931 | .999 | −69.888 | .999 |
| No | −41.935 | .999 | −42.846 | .999 | −42.963 | .999 | −46.224 | .999 |
| General house | ||||||||
| House size | −.029 | .883 | −.035 | .866 | .017 | .941 | ||
| House type | ||||||||
| A house without a garden | 2.196 | .060 | 2.562 | .037* | 3.240 | .018* | ||
| An apartment with a balcony | .425 | .747 | .584 | .662 | 1.307 | .366 | ||
| An apartment with no balcony | −.079 | .907 | −.103 | .886 | −.355 | .666 | ||
| A home with access to an outdoor communal area | .953 | 384 | 1.350 | .239 | 2.418 | .070 | ||
| Other | −.874 | .660 | −.941 | .653 | −.076 | .977 | ||
| Indoor environmental quality | ||||||||
| Natural light | −.055 | .769 | −.117 | .574 | ||||
| Thermal comfort | .115 | .527 | .118 | .554 | ||||
| Indoor air quality | −.109 | .614 | −.041 | .858 | ||||
| Acoustic environment | .041 | .815 | .069 | .709 | ||||
| Window view | −.121 | .480 | −.091 | .624 | ||||
| Indoor physical activity space | .045 | .812 | .037 | .855 | ||||
| Home workspace | −.120 | .456 | −.146 | .399 | ||||
| Neighbourhood amenity quality | ||||||||
| Neighbourhood type | ||||||||
| Town | 2.277 | .002* | ||||||
| Suburb | .561 | .506 | ||||||
| Rural | .537 | .614 | ||||||
| Proximity to the nearest open space | .263 | .370 | ||||||
| Proximity to the nearest shops | .451 | .151 | ||||||
Note: The same reference categories as Table 3 are used.
4.3.3. Stress during the COVID-19 lockdown
Table 5 shows the outcome of the hierarchical regression analysis model for stress and the differences between each model. In the first model, the relationship between social demographics and stress is studied. Compared with the models for depression (Table 3) and anxiety (Table 4), it is not age but the household income (B = −0.479, p = 0.029) that is significantly associated with stress. Specifically, households with higher annual income report less stress. In addition, as household income is marginally significant in Table 3, it can be inferred that income is more of a stressor rather than a cause for depression during the lockdown. Put simply, people with lower income are more likely to be stressed instead of being depressed and a lower income is usually associated with a worse living environment in reality.
Table 5.
Results of regression models on between built environment design and stress.
| Variables | Model 1 |
Model 2 |
Model 3 |
Model 4 |
||||
|---|---|---|---|---|---|---|---|---|
| B | Sig. | B | Sig. | B | Sig. | B | Sig. | |
| Social demographics | ||||||||
| Ethnicity | ||||||||
| Black/Black British-Caribbean, African, other | −5.037 | .111 | −6.145 | .055 | −6.776 | .038* | −8.098 | .017* |
| Mixed race – other | .777 | .748 | 1.077 | .659 | .978 | .688 | −.002 | .999 |
| White – British, Irish, other | −.678 | .502 | −.560 | .587 | −.817 | .438 | −1.068 | .319 |
| Chinese/Chinese British | −1.791 | .108 | −2.299 | .043* | −2.575 | .024* | −2.656 | .021* |
| Middle Eastern/Middle Eastern British – Arab, Turkish, other | −1.855 | .204 | −2.238 | .134 | −2.342 | .119 | −2.411 | .113 |
| Other | −1.659 | .314 | −1.789 | .289 | −2.180 | .200 | −2.474 | .153 |
| Gender | −.647 | .247 | −.692 | .224 | −.857 | .145 | −.756 | .202 |
| Age | −.261 | .311 | −.138 | .601 | −.168 | .531 | −.147 | .610 |
| Employment status | ||||||||
| Self-employed | −.111 | .921 | −.297 | .791 | .055 | .961 | −.183 | .880 |
| In part-time employment | −1.787 | .058 | −1.983 | .035* | −2.072 | .030* | −2.348 | .016* |
| In full-time employment | −.010 | .988 | −.266 | .712 | −.184 | .799 | −.334 | .663 |
| Unable due to disability | .834 | .788 | 2.040 | .536 | 1.994 | .550 | 2.475 | .471 |
| Homemaker/full-time parent | .283 | .900 | .190 | .934 | .273 | .907 | −.258 | .914 |
| Unemployed and seeking work | −.146 | .885 | −.024 | .981 | .129 | .899 | .077 | .940 |
| Furlough | −.706 | .555 | −.759 | .538 | −.512 | .686 | −1.126 | .396 |
| Retired | −1.799 | .398 | −2.055 | .335 | −1.777 | .409 | −2.704 | .240 |
| Household income | −.479 | .029* | −.602 | .010* | −.530 | .031* | −.485 | .043* |
| The number of people in the house | .072 | .667 | .279 | .171 | .173 | .408 | .228 | .286 |
| Rent or Own the house | −.813 | .173 | −.557 | .379 | −.201 | .768 | −.151 | .828 |
| Has anyone in your household had COVID-19 | ||||||||
| Suspected and recovered | −4.092 | .347 | −2.663 | .580 | −3.397 | .492 | −4.747 | .348 |
| Suspected and still ill | −1.978 | .682 | .256 | .962 | −.011 | .998 | −1.756 | .757 |
| No | −4.128 | .336 | −2.591 | .589 | −3.152 | .520 | −4.421 | .378 |
| General house | ||||||||
| House size | −.022 | .926 | −.010 | .968 | .044 | .858 | ||
| House type | ||||||||
| A house without a garden | .111 | .938 | .487 | .733 | .153 | .916 | ||
| An apartment with a balcony | 2.463 | .060 | 1.983 | .136 | 2.131 | .119 | ||
| An apartment with no balcony | 1.819 | .022* | 1.768 | .028* | 1.525 | .044* | ||
| A home with access to an outdoor communal area | −.674 | .612 | −.323 | .810 | .112 | .936 | ||
| Other | 2.152 | .276 | 1.538 | .443 | 1.801 | .380 | ||
| Indoor environmental quality | ||||||||
| Natural light | .091 | .638 | .097 | .625 | ||||
| Thermal comfort | −.025 | .890 | −.059 | .756 | ||||
| Indoor air quality | −.063 | .782 | −.034 | .881 | ||||
| Acoustic environment | −.071 | .708 | −.078 | .683 | ||||
| Window view | −.271 | .151 | −.221 | .247 | ||||
| Indoor physical activity space | .233 | .272 | .236 | .271 | ||||
| Home workspace | −.296 | .115 | −.299 | .015* | ||||
| Neighbourhood amenity quality | ||||||||
| Neighbourhood type | ||||||||
| Town | .368 | .591 | ||||||
| Suburb | −.114 | .886 | ||||||
| Rural | −.285 | .785 | ||||||
| Proximity to the nearest open space | .578 | .043* | ||||||
| Proximity to the nearest shops | −.056 | .857 | ||||||
In the second model, the household income remains significant after adding the extra general house attribute. Surprisingly, ethnicity and employment status have for the first time become significant. Based on the statistics, ‘Chinese/Chinese British’ (B = −2.299, p = 0.043) are less likely to feel stressed than ‘Asian/British-Indian, Pakistani, Bangladeshi, other’. People who are in part-time employment (B = −1.983, p = 0.035) have less stress compared with students. In addition, house type is also significantly associated with stress in this model. Living in an apartment with no balcony (B = 1.819, p = 0.022) is associated with greater stress than living in a house with a garden. As people have to stay at home every day during the lockdown, those with a garden can sometimes go out in the garden for some fresh air and natural views. However, if there is no access to a garden or a balcony, it is understandable that people may feel more stressed.
In the third model, household income, ethnicity, employment status and house type remain significant as in the second model. Moreover, ‘black/black British’ (B = −6.776, p = 0.038) is also shown to have less stress than ‘Asian/British-Indian, Pakistani, Bangladeshi, other’. In the fourth model, after adding the neighbourhood amenity variables, the relationship between social demographic variables (i.e., household income, ethnicity and employment status) and stress is consistent with the results in the third model. In addition, both house type and home workspace are significantly correlated with stress. Residents who live in an apartment with no balcony (B = 1.525, p = 0.044) have higher levels of stress than those who live in a house with a garden. Moreover, the home workspace (B = −2.99, p = 0.015) has a significant impact on stress. As residents' satisfaction with the home workspace increases, their stress decreases. This can be because people are required to work from home during the lockdown and a satisfying home workspace can provide residents with proper facilities without having to worry about having no place to work. Furthermore, the proximity to the nearest open space (B = 0.578, Sig. p = 0.043) is associated with stress, which suggests that residents who live near the green and open space are less likely to feel stressed.
5. Discussion and implications
While there is a wealth of reasons that can cause mental health problems (e.g., stress, anexity, and depression), current literature has established their relationship with built environment (see, for example, Evans et al., 2003; Power et al., 2015; Wang et al., 2021). Importantly, there are both similarities and differences between this research and the extant studies on built environment and mental health that may advance the existing understanding and knowledge. Specific to the context of COVID-19, age is negatively correlated with depression and anxiety, which is consistent with Khan et al. (2021). The impact on the daily routine of young people and adults during the COVID-19 lockdown may be more drastic because young people and adults are forced to stay at home when they should be studying and working, which may be one of the reasons for their depression and anxiety. In comparison, the elderly has become accustomed to staying at home for long periods before the COVID-19 lockdown. Contrasting with Evans et al. (2003) who found older people are less sensitive to housing quality than young adolescents, the association between age and mental health becomes insignificant after adding the factors of built environment design in this study. This suggests that age is not an important factor influencing the relationship between the built environment and mental health during the COVID-19 lockdown.
Employment status and household income can significantly affect the levels of stress. For instance, people who work part-time are more stressed, which may be because their jobs become more unstable during the lockdown. Individuals who lost their jobs during the pandemic are associated with worse mental health and feel pessimistic about life (Fisher et al., 2021). In addition, we find that income is an important factor mediating the relationship between built environment design and mental health, i.e., low-income families tend to live in poor-quality houses and feel more stressed during the COVID-19 lockdown. Evans et al. (2003) report a similar case where the quality of the built environment design, to a large extent, can affect the mental health of the general population. However, our study provides empirical evidence on the direct and indirect relationship between social demographics and mental health when it is mandatory to stay at home during extreme events (e.g., COVID-19), and thus addresses this gap in the literature.
Gardens and balconies are important design elements of the built environment, which have a positive effect on mental health during the COVID-19 lockdown. In this study, residents who live in a house without a garden show a greater anxiety level than those who also live in a house but with a garden. Additionally, apartments with no balcony can make occupants feel more stressed. These results concur with Akbari et al. (2021) and Zarrabi et al. (2021), indicating that open and semi-open spaces can boost individuals’ wellbeing due to better access to fresh air, sunshine and natural views. This further explains our findings that residents who live a house with a garden are less likely to feel anxious and stressed. Compared with Corley et al. (2021) in which it is the time spent in the garden that is more important, we suggest that private gardens themselves offer an opportunity for the residents to deviate, relax and cultivate and maintain plants, which results in better mental health during the COVID-19 lockdown. This way, we ascertain that private gardens have a great impact on mental health. In light of the frequent occurrence of uncertain events, this advocates for the idea of gardens and/or more open space in built environment design because they act as outlets for psychological catharsis and alleviate the feelings of isolation and loneliness.
In terms of indoor environmental quality, home workspace has a significant impact on stress but not on anxiety or depression. The level of stress of residents decreases when their satisfaction with the home workspace improves. Interestingly, four other basic components of indoor environmental quality (i.e., thermal comfort, indoor air quality, acoustic and visual comfort) are not significantly correlated with mental health in this study. This somewhat counter-intuitive finding contradicts existing studies (see, for example, Evans, 2003; Lai et al., 2009; Tanabe et al., 2007; Thomson and Snell, 2013; Beemer et al., 2019) where these components were found to have effects on mental health. For example, Amerio et al. (2020) report students in Italy who live in apartments with poor indoor quality experienced increased depression during the lockdown. However, as people reconfigure their rooms to create home workspace, its corresponding thermal comfort, light, ventilation, visual comfort, etc. may have been adjusted to their comfortable level as well, thus decreasing their significance to mental health during the lockdown period. In fact, Lovec et al. (2021) report that indoor air quality becomes better during the pandemic because of the ventilation guidelines put in place. The lack of a proper home workspace with comfortable indoor environmental quality also explains the worsened working performance and depression reported by participants in Amerio et al. (2020). In addition, the genial weather in the UK during the first lockdown when data were collected (i.e., May to July 2020) may have contributed to the satisfactory indoor environmental quality.
Neighbourhood type and the proximity to the nearest open space are significantly associated with mental health in this research. In particular, residents who live in cities are less likely to feel depressed and anxious than those who live in towns. Moreover, residents who live near green spaces show lower levels of stress. This is COVID-19-specific, as Hartig et al. (2003) and Peen et al. (2010) propose that urban populations are more likely to have negative emotions. However, in the case of COVID-19 lockdown, the medical and health facilities and amenities are better in the city, which provides a sense of security that can mitigate anxiety and depression of residents (Sharifi and Khavarian-Garmsir, 2020). In terms of the distance to open space, these results are similar to Sturm and Cohen (2014) and Völkern and Kistemann (2015) who argue that green environment settings in the cities can help release negative emotions. However, Helbich et al. (2019) propose that the effects of open space on depression should not be exaggerated and are minor. This is corroborated by our study: open space is identified to have no significant impact on residents' depression and anxiety during the COVID-19 lockdown. Nevertheless, given its significant role in relieving residents’ stress, planners need to accommodate open space close to the residents. Finally, the significant correlation between shopping facilities, social demographics and mental health is not detected.
Our study could provide some design implications for policymakers and built environment design professionals in the case of a future crisis. First, it is imperative that the awareness of built environment design's impact on mental health should be fostered (Galea et al., 2005). Although to what degree the built environment design affects mental health can be further quantitatively explored, we have provided an aggregate view on their interaction. Second, we do not support the consideration of all variables as there is always a balance to be made between built environment design and its cost (Guo and Gandavarapu, 2010). Also, better design quality usually means a higher property transaction price, which some people cannot afford. As a result, potential mental health problems can be engendered by this tension between the two. However, paying attention to the factors identified as more important in this study could offset this tension. Third, engaging public opinion would be a sustainable solution to public demands (Kua and Lee, 2002). Typically, there is a discrepancy between what the policymakers and architects think is best for residents' mental health and what residents think for themselves. Therefore, an ideal way is to cover parts of the general public's concerns. Reflecting on this research, a comment box regarding the question “if you want to make a change to your current physical environment, what would the change be?” was provided at the end of the questionnaire. A majority of participants preferred to have a better home workspace and a larger indoor physical activity place, and some expressed the desire to live away from any main road. Therefore, architects and engineers need to consider the rationality and practicality of the house type and the location. Although individual differences will not disappear, such 'public engagement trailblazer' can make overall progress.
6. Conclusions
By performing two step-by-step regression models (i.e., logistic and hierarchical) with survey data collected in the UK, this research illustrates the influence of individual and collective built environment features on the depression, anxiety and stress of residents, respectively. While studies on this are not scarce, our timely research is conducted within the context of COVID-19 lockdown to address the consideration of uncertainties in future built environment design. Compared with depression and anxiety, residents are more likely to show symptoms of stress during the COVID-19 lockdown. To mitigate this, our empirical evidence suggests that the consideration of open space detached to the property (e.g., gardens and balconies), home workspace, neighbourhood type, and houses' distance to green space is important to people's mental health during the COVID-19 lockdown period. However, residents' social demographics should be considered simultaneously as they can exert a fluctuating effect on the relationship between mental health and built environment. As such, policymakers and architects can be better equipped with an enhanced awareness of mental health, significant built environment factors, and sense of public engagement in their long-term practice.
Despite our following of a rigorous research design (Fig. 1), there are limitations that form the basis for future works. Firstly, we employed PHQ-2, GAD-7 and PSS-4 to assess residents' early-stage mental health during the COVID-19 lockdown. While this fits the unprecedented nature of the crisis and ensures initial actions, we acknowledge the importance of a longitudinal study of this phenomenon, particularly as some restrictions are recurrent. The comparison with a post-COVID-19 mental health and built environment study will together underpin more solid design decisions. Such a comparison can also include ‘social demographics’ so that a deeper understanding of its interaction with built environment and mental health can be garnered. Despite the fact that existing studies have adopted a similar sample size as ours, this future longitudinal research could consider a larger sample to extrapolate the results on a larger population. Secondly, our study focused on the housing type in which people spend most of their time during COVID-19. However, future studies can configure the setting to other building types (e.g., offices and classrooms) as people begin to live with the ‘new normal’ but with some restriction rules. Finally, although we managed to consider social demographics, the indoor built environment (internal) and the surrounding environment people reside within (external), and identified the new home workspace feature in combating stress, this is not a ‘panacea’ to de-mystify the complex mental health working mechanism. Therefore, we call for multi-disciplinary studies (e.g., economics, architecture, engineering, urban planning, and psychology) to acquire a better understanding of the relationship between built environment and mental health.
Acknowledgement
The authors would like to thank the Editor and the anonymous reviewers for the constructive and insightful comments that have helped improve the quality of this article. The contribution of the participants of this research must also be acknowledged. The authors would like to bring the issue of mental health to people’s attention, and hope that everyone can live happily in our built environment, especially during this unusual time. The fourth author – Fang Liu was supported by a European Research Council (ERC) Starting Grant (CAASD, 678733).
Appendix.
Demographic analysis of participants.
References
- Akbari P., Yazdanfar S.-A., Hosseini S.-B., Norouzian-Maleki S. Housing and mental health during outbreak of COVID-19. J. Build. Eng. 2021;43 [Google Scholar]
- Al horr Y., Arif M., Katafygiotou M., Mazroei A., Kaushik A., Elsarrag E. Impact of indoor environmental quality on occupant well-being and comfort: a review of the literature. International Journal of Sustainable Built Environment. 2016;5:1–11. [Google Scholar]
- Allen J.G., MacNaughton P., Laurent J.G.C., Flanigan S.S., Eitland E.S., Spengler J.D. Green buildings and health. Current Environmental Health Reports. 2015;2:250–258. doi: 10.1007/s40572-015-0063-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaratunga D., Baldry D., Sarshar M., Newton R. Quantitative and qualitative research in the built environment: application of “mixed” research approach. Work. Stud. 2002;51(1):17–31. [Google Scholar]
- Amerio A., Brambilla A., Morganti A., Aguglia A., Bianchi D., Santi F., Costantini L., Odone A., Costanza A., Signorelli C., Serafini G. COVID-19 lockdown: housing built environment's effects on mental health. Int. J. Environ. Res. Publ. Health. 2020;17(16):5973. doi: 10.3390/ijerph17165973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appelqvist-Schmidlechner K., Lamsa R., Tuulio-Henriksson A. Factors associated with positive mental health in young adults with a neurodevelopmental disorder. Res. Dev. Disabil. 2020;106 doi: 10.1016/j.ridd.2020.103780. [DOI] [PubMed] [Google Scholar]
- Arsham H. Questionnaire design and surveys sampling. 2005. https://www.researchgate.net/profile/Dr-Hossein-Arsham/publication/344638672_Questionnaire_Design_and_Surveys_Sampling/links/5f866791458515b7cf7f657e/Questionnaire-Design-and-Surveys-Sampling.pdf Available at:
- Awada M., Becerik-Gerber B., Hoque S., O'neill Z., Pedrielli G., Wen J., Wu T. Ten questions concerning occupant health in buildings during normal operations and extreme events including the COVID-19 pandemic. Build. Environ. 2021;188 doi: 10.1016/j.buildenv.2020.107480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakioğlu Fuad, Korkmaz Ozan, Ercan & Hülya. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. International Journal of Mental Health and Addiction. 2021;19:2369–2382. doi: 10.1007/s11469-020-00331-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banna M.H.A., Sayeed A., Kundu S., Christopher E., Hasan M.T., Begum M.R., Kormoker T., Dola S.T.I., Hassan M.M., Chowdhury S., Khan M.S.I. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. Int. J. Environ. Health Res. 2020:1–12. doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- Barnett A., Zhang C.J.P., Johnston J.M., Cerin E. Relationships between the neighborhood environment and depression in older adults: a systematic review and meta-analysis. Int. Psychogeriatr. 2018;30(8):1153–1176. doi: 10.1017/S104161021700271X. [DOI] [PubMed] [Google Scholar]
- Barros P., Fat L.N., Garcia L.M.T., Slovic A.D., Thomopoulos N., de Sá T.H., Morais P., Mindell J.S. Social consequences and mental health outcomes of living in high-rise residential buildings and the influence of planning, urban design and architectural decisions: a systematic review. Cities. 2019;93:263–272. [Google Scholar]
- Beemer C.J., Stearns-Yoder K.A., Schuldt S.J., Kinney K.A., Lowry C.A., Postolache T.T., Brenner L.A., Hoisington A.J. A brief review on the mental health for select elements of the built environment. Indoor Built Environ. 2019:1–14. 0(0. [Google Scholar]
- Berglund E., Westerling R., Lytsy P. Housing type and neighbourhood safety behaviour predicts self-rated health, psychological well-being and frequency of recent unhealthy days: a comparative cross-sectional study of the general population in Sweden. Plann. Pract. Res. 2017;32(4):444–465. [Google Scholar]
- Bloom D., Cafiero E., Jane-Llopis E., Abrahams-Gessel S., Bloom L., Fathima S., Feigl A., Gaziano T., Mowafi M., Pandya A. WHO; Geneva, Switzerland: 2011. The Global Economic Burden of Noncommunicable Diseases. [Google Scholar]
- Brownson R.C., Hoehner C.M., Day K., Forsyth A., Sallis J.F. Measuring the built environment for physical activity: state of the science. Am. J. Prev. Med. 2009;36(4):S99–S123. doi: 10.1016/j.amepre.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns J., Boogaard H., Polus S., Pfadenhauer L.M., Rohwer A.C., Van Erp A.M., Turley R., Rehfuess E. Interventions to reduce ambient particulate matter air pollution and their effect on health. Cochrane Database Syst. Rev. 2019;5:CD010919. doi: 10.1002/14651858.CD010919.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabinet Office National risk register of civil emergencies. 2017. https://www.gov.uk/government/publications/national-risk-register-of-civil-emergencies-2017-edition Available at:
- Cattell R.B. Plenum Press; New York: 1978. The Scientific Use of Factor Analysis in Behavioral and Life Sciences. [Google Scholar]
- Centers for Disease Control and Prevention Mental health conditions: depression and anxiety. 2021. https://www.cdc.gov/tobacco/campaign/tips/diseases/depression-anxiety.html Available at:
- Cerda M., Ransome Y., Keyes K.M., Koenen K.C., Tardiff K., Vlahov D., Galea S. Revisiting the role of the urban environment in substance use: the case of analgesic overdose fatalities. Am. J. Publ. Health. 2013;103(12):2252–2260. doi: 10.2105/AJPH.2013.301347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang H.J., Huang K., Wu C. Determination of sample size in using central limit theorem for weibull distribution. Int. J. Inf. Manag. Sci. 2006;17(3):31–46. [Google Scholar]
- Codinhoto R., Tzortzopoulos P., Kagioglou M., Aouad G., Cooper R. The impacts of the built environment on health outcomes. Facilities. 2009;27(3/4):138–151. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Corley J., Okely J.A., Taylor A.M., Page D., Welstead M., Skarabela B., Redmond P., Cox S.R., Russ T.C. Home garden use during COVID-19: associations with physical and mental wellbeing in older adults. J. Environ. Psychol. 2021;73 doi: 10.1016/j.jenvp.2020.101545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawel A., Shou Y., Smithson M., Cherbuin N., Banfield M., Calear A.L., Farrer L.M. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D., Golijani-Moghaddam N. COVID-19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vaus D. SAGE; London: 2001. Research Design in Social Research. [Google Scholar]
- Egan M., Petticrew M., David Ogilvie D., Hamilton V. New roads and human health: a systematic review. Am. J. Publ. Health. 2003;93(9):1463–1471. doi: 10.2105/ajph.93.9.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsadek M., Liu B., Xie J. Window view and relaxation: viewing green space from a high-rise estate improves urban dwellers' wellbeing. Urban For. Urban Green. 2020;55 [Google Scholar]
- Evans G.W. The built environment and mental health. J. Urban Health: Bull. N. Y. Acad. Med. 2003;80(4):536–555. doi: 10.1093/jurban/jtg063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans G.W., Wells N.M., Moch A. Housing and mental health: a review of the evidence and a methodological and conceptual critique. J. Soc. Issues. 2003;59(3):475–500. [Google Scholar]
- Faul F., Erdfelder E., Lang A.G., Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Fisher J.R., Tran T.D., Hammarberg K., Sastry J., Nguyen H., Rowe H., Popplestone S., Stocker R., Stubber C., Kirkman M. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med. J. Aust. 2020;213(10):458–464. doi: 10.5694/mja2.50831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J., Tran T., Hammarberg K., Nguyen H., Stocker R., Rowe H., Sastri J., Popplestone S., Kirkman M. Quantifying the mental health burden of the most severe COVID-19 restrictions: a natural experiment. J. Affect. Disord. 2021;293:406–414. doi: 10.1016/j.jad.2021.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Drawve G., Harris C. Facing new fears during the COVID-19 pandemic: the state of America's mental health. J. Anxiety Disord. 2020;75 doi: 10.1016/j.janxdis.2020.102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Ahern J., Rudenstine S., Wallace Z., Vlahov D. Urban built environment and depression: a multilevel analysis. J. Epidemiol. Community. 2005;59:822–827. doi: 10.1136/jech.2005.033084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gary T.L., Stark S.A., Laveist T.A. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health Place. 2007;13:569–575. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Gibson M., Thomson H., Ade Kearns A., Petticrew M. Understanding the psychosocial impacts of housing type: qualitative evidence from a housing and regeneration intervention. Hous. Stud. 2011;26(4):555–573. [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of COVID-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Publ. Health. 2020;17:4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J.Y., Gandavarapu S. An economic evaluation of health-promotive built environment changes. Preventative Medicine. 2010;50:44–49. doi: 10.1016/j.ypmed.2009.08.019. [DOI] [PubMed] [Google Scholar]
- Hair J.F., Anderson R.E., Tatham R.L., Grablowsky B.J. Pipe Books; Tulsa, Oklahoma: 1979. Multivariate Data Analysis. [Google Scholar]
- Hartig T., Evans G.W., Jamner L.D., Davis D.S., Garling T. Tracking restoration in natural and urban field settings. J. Environ. Psychol. 2003;23(2):109–123. [Google Scholar]
- Helbich M., Hagenauer J., Roberts H. Relative importance of perceived physical and social neighborhood characteristics for depression: a machine learning approach. Soc. Psychiatr. Psychiatr. Epidemiol. 2019;55:599–610. doi: 10.1007/s00127-019-01808-5. [DOI] [PubMed] [Google Scholar]
- Hoisington A.J., Stearns-yoder K.A., Schuldt S.J., Beemer C.J., Maestre J.P., Kinney K.A., Postolache T.T., Lowry C.A., Brenner L.A. Ten questions concerning the built environment and mental health. Build. Environ. 2019;155:58–69. [Google Scholar]
- Huang Y., Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian journal of psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102052. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Huang Y., Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group? Psychol. Health Med. 2020:1–12. doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- Hudson C.G. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am. J. Orthopsychiatry. 2010;75(1):3–18. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- Jensen H.A.R., Rasmussen B., Ekholm O. Neighbour and traffic noise annoyance: a nationwide study of associated mental health and perceived stress. Eur. J. Publ. Health. 2018;28:1050–1055. doi: 10.1093/eurpub/cky091. [DOI] [PubMed] [Google Scholar]
- Jorm A.F. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol. Med. 2000;30(1):11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- Khan M.A.S., Debnath S., Islam M.S., Zaman S., Ambia N.E., Barshan A.D., Hossain M.S., Tabassum T., Rahman M., Hasan M.J. Mental health of young people amidst COVID-19 pandemic in Bangladesh. Heliyon. 2021;7 doi: 10.1016/j.heliyon.2021.e07173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klepeis N.E., Nelson W.C., Ott W.R., Robinson J.P., Tsang A.M., Switzer P., Behar J.V., Hern S.C., Engelmann W.H. The national human activity pattern survey (NHAPS): a resource for asses- sing exposure to environmental pollutants. J. Expo. Anal. Environ. Epidemiol. 2001;11:231–252. doi: 10.1038/sj.jea.7500165. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kua H.W., Lee S.E. Demonstration intelligent building—a methodology for the promotion of total sustainability in the built environment. Build. Environ. 2002;37(3):231–240. [Google Scholar]
- Lai A.C.K., Mui K.W., Wong L.T., Law L.Y. An evaluation model for indoor environmental quality (IEQ) acceptance in residential buildings. Energy Build. 2009;41:930–936. [Google Scholar]
- Lee E.H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs. Res. 2012;6(4):121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Li D.C.Y., Leung L. Psychometric data on knowledge and fear of coronavirus disease 2019 and perceived stress among workers of Filipino origin in Hong Kong. Data Brief. 2020;(33) doi: 10.1016/j.dib.2020.106395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberopoulos G., Tsarouhas P. Reliability analysis of an automated pizza production line. J. Food Eng. 2005;69(1):79–96. [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatr. Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovec V., Premrov M., Leskovar V.Ž. Practical impact of the COVID-19 pandemic on indoor air quality and thermal comfort in kindergartens. A case study of Slovenia. Int. J. Environ. Res. Publ. Health. 2021;18:9712. doi: 10.3390/ijerph18189712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe B., Korennke K., Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) J. Psychosom. Res. 2005;58(2):163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- McLean C.P., Asnaani A., Litz B.T., Hofmann S.G. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011;45:1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medlock K.B., Temzelides T., Hung S. COVID-19 and the value of safe transport in the United States. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-01202-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mental Health Taskforce The five year forward view for mental health. 2016. https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf Available at:
- Mui K.W., Wong L.T. A method of assessing the acceptability of noise levels in air-conditioned offices. Build. Serv. Eng. Technol. 2006;27(3):249–254. [Google Scholar]
- National Health Service Mental health. 2021. https://www.england.nhs.uk/mental-health/ Available at:
- NHS Stress. 2019. https://www.nhs.uk/mental-health/feelings-symptoms-behaviours/feelings-and-symptoms/stress/ Available at:
- Nunnally J.C., Bernstein I.H. The assessment of reliability. Psychometric Theory. 1994;3:248–292. [Google Scholar]
- Nurse J., Woodcock P., Ormsby J. Influence of environmental factors on mental health within prisons: focus group study. The BMJ. 2003;327:480–484. doi: 10.1136/bmj.327.7413.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutsford D., Pearson A.L., Kingham S. An ecological study investigating the association between access to urban green space and mental health. Publ. Health. 2013;127(11):1005–1011. doi: 10.1016/j.puhe.2013.08.016. [DOI] [PubMed] [Google Scholar]
- Office for National Statistics . 2017. Measuring National Well-Being: Life in the UK.https://www.gov.uk/government/statistics/measuring-national-well-being-life-in-the-uk-apr-2017 Apr 2017, Available at: [Google Scholar]
- Office for National Statistics . 2020. Coronavirus (COVID-19) Infection Survey Pilot: England.https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/31july2020 31 July 2020, Available at: [Google Scholar]
- Oiamo T.H., Luginaah I.N., Baxter J. Cumulative effects of noise and odour annoyances on environmental and health related quality of life. Soc. Sci. Med. 2015;146:191–203. doi: 10.1016/j.socscimed.2015.10.043. [DOI] [PubMed] [Google Scholar]
- Peen J., Schoevers R.A., Beekman A.T., Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- Pohar M., Blas M., Turk S. Comparison of logistic regression and linear discriminant analysis: a simulation study. Metodoloski Zvezki. 2004;1(1):143–161. [Google Scholar]
- Power M.C., Kioumourtzoglou M.A., Hart J.E., Okereke O.I., Laden F., Weisskopf M.G. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. The BMJ. 2015;350:1–9. doi: 10.1136/bmj.h1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proto E., Quintana-Domeque C. COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0244419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putrik P., de Vries N.K., Mujakovic S., van Amelsvoort L., Kant I., Kunst A.E., van Oers H., Jansen M. Living environment matters: relationships between neighborhood characteristics and health of the residents in a Dutch municipality. J. Community Health. 2015;40:47–56. doi: 10.1007/s10900-014-9894-y. [DOI] [PubMed] [Google Scholar]
- Radmacher S.A., Martin D.J. Identifying significant predictors of student evaluations of faculty through hierarchical regression analysis. J. Psychol. 2001;135(3):259–268. doi: 10.1080/00223980109603696. [DOI] [PubMed] [Google Scholar]
- Reichert M., Braun U., Lautenbach S., Zipf A., Ebner-Priemer U., Tost H., Meyer-Lindenberg A. Studying the impact of built environments on human mental health in everyday life: methodological developments, state-of-the-art and technological frontiers. Current Opinion in Psychology. 2020;32:158–164. doi: 10.1016/j.copsyc.2019.08.026. [DOI] [PubMed] [Google Scholar]
- Rosenberg S., Mendoza J., Tabatabaei-Jafari H., Pan-Mhin, Salvador-Carulla L. 2020. International Experiences of the Active Period of COVID-19 - Mental Health Care, Health Policy and Technology. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter C.M., Gatsonis C.A. A hierarchical regression approach to meta‐analysis of diagnostic test accuracy evaluations. Stat. Med. 2001;20:2865–2884. doi: 10.1002/sim.942. [DOI] [PubMed] [Google Scholar]
- Saarloos D., Alfonso H., Giles-Corti B., Middleton N., Almeida O.P. The built environment and depression in later life: the health in men study. Am. J. Geriatr. Psychiatr. 2011;19(5):461–470. doi: 10.1097/JGP.0b013e3181e9b9bf. [DOI] [PubMed] [Google Scholar]
- Santamouris M., Alevizos S.M., Aslanoglou L., Mantzios D., Milonas P., Sarelli I., Karatasou S., Cartalis K., Paravantis J.A. Freezing the poor—indoor environmental quality in low and very low income households during the winter period in Athens. Energy Build. 2014;70:61–70. [Google Scholar]
- Scoppetta O., Cassiani-Miranda C.A., Arocha-DÃaz K.N., Cabanzo-Arenas D.F., Campo-Arias A. Validity of the patient health questionnaire-2 (PHQ-2) for the detection of depression in primary care in Colombia. J. Affect. Disord. 2020;278:576–582. doi: 10.1016/j.jad.2020.09.096. [DOI] [PubMed] [Google Scholar]
- Shapiro E., Levine L., Kay A. Mental health stressors in Israel during the coronavirus pandemic. Psychological Trauma: Theory, Research, Practice and Policy. 2020;12:499–501. doi: 10.1037/tra0000864. [DOI] [PubMed] [Google Scholar]
- Sharifi A., Khavarian-Garmsir A.R. The COVID-19 pandemic: impacts on cities and major lessons for urban planning, design, and management. Sci. Total Environ. 2020;749 doi: 10.1016/j.scitotenv.2020.142391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatr. Res. 2020;293 doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sturm R., Cohen D. Proximity to urban parks and mental health. J. Ment. Health Pol. Econ. 2014;17(1):19–24. [PMC free article] [PubMed] [Google Scholar]
- Sullivan W.C., Chang C. In: Making Healthy Places. Dannenberg A.L., Frumkin H., Jackson R.J., editors. Island Press; Washington, DC: 2011. Mental health and the built environment. [Google Scholar]
- Taherdoost H. Validity and reliability of the research instrument; how to test the validation of a questionnaire/survey in a research. Int. J. Acad. Res. Manag. 2016;5(3):28–36. [Google Scholar]
- Tan Z., Roberts A.C., Lee E.H., Kwok K.W., Car Josip, Soh C.K., Christopoulos G. Transitional areas affect perception of workspaces and employee well-being: a study of underground and above-ground workspaces. Build. Environ. 2020;179 [Google Scholar]
- Tanabe S.I., Nishihara N., Haneda M. Indoor temperature, productivity, and fatigue in office tasks. HVAC R Res. 2007;13:623–633. [Google Scholar]
- Thomson H., Snell C. Quantifying the prevalence of fuel poverty across the European Union. Energy Pol. 2013;52:563–572. [Google Scholar]
- Tung Y.K. Channel scouring potential using logistic analysis. J. Hydraul. Eng. 1985;111(2):194–205. [Google Scholar]
- Twenge J.M., Joiner T.E. U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. Anxiety. 2020;37:954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Völkern S., Kistemann T. Developing the urban blue: comparative health responses to blue and green urban open spaces in Germany. Health Place. 2015;35:196–205. doi: 10.1016/j.healthplace.2014.10.015. [DOI] [PubMed] [Google Scholar]
- Wang L., Zhou Y., Wang F., Ding L., Love P.E., Li S. The influence of the built environment on people's mental health: an empirical classification of causal factors. Sustain. Cities Soc. 2021;74 [Google Scholar]
- Warttig S.L., Forshaw M.J., South J., White A.K. New, normative, English-sample data for the short form perceived stress scale (PSS-4) J. Health Psychol. 2013;18(12):1617–1628. doi: 10.1177/1359105313508346. [DOI] [PubMed] [Google Scholar]
- Weich S., Blanchard M., Prince M., Burton E., Erens B., Sproston K. Mental health and the built environment: cross-sectional survey of individual and contextual. Br. J. Psychiatry. 2002;180:428–433. doi: 10.1192/bjp.180.5.428. [DOI] [PubMed] [Google Scholar]
- World Health Organisation Mental health: strengthening our response. 2018. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response Available at:
- World Health Organisation Basic documents: forty-ninth edition. 2020. https://apps.who.int/gb/bd/pdf_files/BD_49th-en.pdf Available at:
- Wright P.A., Kloos B. Housing environment and mental health outcomes: a levels of analysis perspective. J. Environ. Psychol. 2007;27(1):79–89. doi: 10.1016/j.jenvp.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarrabi M., Yazdanfar S.-A., Hosseini S.-B. COVID-19 and healthy home preferences: the case of apartment residents in Tehran. J. Build. Eng. 2021;35 [Google Scholar]
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in liaoning province, China: a cross-sectional study. Int. J. Environ. Res. Publ. Health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]