Abstract
Purpose
We aimed to compare the outcomes between closed reduction (CR) and open reduction (OR) in children aged 6–24 months with developmental dysplasia of the hip (DDH) who could be reduced safely and stably by the closed reduction operation.
Methods
We retrospectively reviewed the medical records of 77 patients who underwent CR or OR for DDH. Fifty-one patients (56 hips) underwent CR, 26 (29 hips) underwent OR. The demographic data, International Hip Dysplasia Institute classification and acetabular index (AI) before reduction and the centre-edge angle (CEA), AI, Alsberg angle (AA), Reimer’s migration index (RMI), and height-to-width index (HWI) of the epiphysis were compared between two groups at the final follow-up. The percentage of coxa magna > 15% of the normal side and AA > 81° were calculated.
Results
At the final follow-up, the mean AA in the CR and OR groups were 77.66° (60°–89°) and 81.97° (73°–91°) (p = 0.001), respectively, there were 32.14% and 58.62% of the hips with an AA > 81° (p = 0.019). The frequency of coxa magna > 15% of the normal side was higher in the OR group (60.9%) than in the CR group (6.5%) (p < 0.001). There was no difference in the improvement of AI, CEA, HWI, and RMI.
Conclusion
In children aged 6–24 months with DDH, if a stable and safe CR can be obtained but with medial joint space up to 6mm, CR should be attempted first.
Keywords: Developmental dysplasia of the hip, Closed reduction, Open reduction, Outcome comparison
Introduction
The purpose of treatment for developmental dysplasia of the hip (DDH) is to obtain and maintain concentric reduction. For irreducible or unstable DDH, open reduction (OR) is the only option [1]. Closed reduction (CR) is still a common treatment method for DDH in patients aged 6–24 months [2, 3], but not all CRs can immediately obtain complete concentricity between the femoral head and acetabulum. Some studies have confirmed that non-concentric CR occurs for a period of time, but the eventual concentric reduction is achieved by femoral head ‘docking’ [4, 5]. Achievement of an earlier and greater degree of concentric reduction increases the potential of hip restoration and reduces long-term complications and reoperation rate [6–8]. Thus, the indication for CR has become stricter. The majority of physicians believe that a mild widen joint space or widened medial dye pooling (MDP) is acceptable for a stable CR [3, 5]. However, due to the different demographics and severity of DDH in CR studies, disparate results have caused some scholars to only accept an outcome of complete concentric reduction [9, 10]. Therefore, there is still considerable controversy regarding acceptable standards for CR treatment for DDH. This is due to the dearth of reliable evidence-based research that compares CR and OR and the lack of homogeneity among patients in previous cohorts [11, 12].
Within the author’s clinical unit, some physicians accept CR that is safe (hip abduction < 65° that can maintain reduction) and stable (safe zone > 30°) [13], whereas others only accept complete concentric reduction whose MDP is less than 2 mm [9, 10] on the intraoperative radiography for children aged 6–24 months with DDH. Therefore, some patients with DDH who underwent safe and stable CR required subsequent OR due to widening of the joint space. These circumstances presented the opportunity to compare the early outcomes of CR and OR treatment for DDH and increase the current understanding of acceptable CR treatment standards. This study aimed to compare the early outcomes between CR and OR in children aged 6–24 months with DDH who can be initially reduced safely and stably by the closed method.
Patients and Methods
Patient Information
After obtaining the approval of the authors’ Institutional Review Board, the medical records were reviewed for all patients who had treatment for DDH between August 2014 and October 2019. The included patients were those who can be stably and safely reduced by initial manual operation intraoperatively. However, due to the surgeon’s preference, some accepted a certain widening of the joint space, and the patients were then immobilized with a spica cast (CR group), while others accepted a complete reduction. Therefore, a portion of patients underwent subsequent OR (OR group). The other inclusion criteria were as follows: age 6–24 months at the time of a reduction, aforementioned CR or OR treatment alone, no treatment before the reduction, and at least 2 years of follow-up. The exclusion criteria included neuromuscular or syndromic hip dysplasia and irreducible or unstable DDH.
The indication for CR in this group of patients was a stable and safe reduction that could be achieved despite a widening joint space on the intraoperative radiography. Stable meant that the safe zone [13] exceeded 30°. Safe meant that the reduction could be maintained after hip abduction of < 65°. If hip abduction was < 70°, percutaneous adductor tenotomy was performed. After a CR treatment was determined intraoperatively, the patient was placed in a spica cast for 3 months followed by an abduction brace for 3 months. In the OR group, the reduction procedure was completed using an anterior approach for all children [14]. Postoperatively, a spica plaster cast was used for 6–8 weeks followed by an abduction brace for 3 months. All treatments were performed by senior paediatric orthopaedic physicians proficient in CR methods and anterior OR surgery.
Following the aforementioned criteria, 79 children were included in the study, including 53 and 26 patients treated with CR and OR, respectively. Two patients in the CR group continued to have subluxation after brace removal; therefore, OR and pelvic osteotomy were performed at the ages of 3 and 4.5 years, respectively. Then, 77 children with successfully treated DDH were compared in the follow-up analysis, including 51 (56 hips) and 26 patients (29 hips) in the CR and OR groups, respectively.
Measurement Parameters
The severity of dislocation before the reduction was graded according to the International Hip Dysplasia Institute (IHDI) classification, and the preoperative acetabular index (AI) was measured using anteroposterior (AP) pelvic radiographs. The superior joint space (SJS) and medial joint space (MJS) were measured on the MRI within 48 h after reduction. The centre-edge angle (CEA) of Wiberg, AI, Alsberg angle (AA) of the proximal femur (angle between the direction line of the proximal capital physis and the axis of the femoral shaft[15]), Reimer’s migration index (RMI) [16], and height-to-width index (HWI) of the epiphysis were measured on the AP pelvic radiograph at the final follow-up. Avascular necrosis (AVN) of the femoral head was evaluated according to Salter’s criteria.
During the follow-up period, the reoperation rate due to re-dislocation or residual acetabular dysplasia (RAD) was recorded. At the final follow-up, the frequency of RAD, HWI < 0.357, RMI > 33%, and AA > 81° were recorded. Moreover, the incidence of coxa magna was recorded and defined as an increase in the width of the epiphyseal nucleus of > 15% of the normal side [17]. According to the development law for the AI in normal children, RAD was defined as an AI > 26° in children aged > 48 months or an AI > 28° at an age ≦ 48 months [18, 19].
Statistical Analysis
SPSS version 25.0 software (IBM, Armonk, New York, USA) was used for the statistical processing of the measured data. The Kolmogorov–Smirnov method was used to test the normal distribution of the data. The normal distribution data were expressed in the form of means with ranges, and the non-normal data were expressed in the form of medians accompanied by an interquartile range. Student’s t test (for normal distribution data) or the Mann–Whitney U test (for abnormal distribution) was used to compare the age at a reduction, follow-up time, final follow-up age, SJS, MJS, AI, CEA, AA, HWI, and RMI between the CR and OR groups. The χ2 test or Fisher’s exact probability test was used to compare the distributions of gender, side, IHDI classification, AVN, RAD, HWI < 0.357, RMI > 33%, AA > 81°, and difference in the incidence of coxa magna > 15% at the last follow-up. A p value < 0.05 was considered statistically significant.
Results
The demographics of the children in this study are shown in Table 1. There was no significant difference between the CR and OR groups for the distribution of gender, side of the affected hip, age at a reduction, follow-up time, or age at the last follow-up. There was a significant difference in the IHDI classification between the two groups (p = 0.048). Because the dislocation heights for IHDI types II and III were similar to the midpoint of the proximal femoral metaphysis on or below Hilgenreiner’s line, there was no significant difference in the severity of dislocation between the two groups when type II and III hips were combined (χ2 = 1.419, p = 0.234). Before reduction, the AI for the CR and OR groups were average 37.30° (22°–50°) and 36.45° (27°–45°), respectively (t = 0.611, p = 0.543).
Table 1.
Comparison of demographic data between the closed and open reduction groups
| Closed reduction (56 hips) | Open reduction (29 hips) | p value | |
|---|---|---|---|
| Sex | |||
| Male (%) | 7 (13.7) | 1 (3.8) | 0.343a |
| Female (%) | 44 (86.3) | 25 (96.2) | |
| Side | |||
| Left (%) | 30 (58.8) | 15 (57.7) | 0.973a |
| Right (%) | 16 (31.4) | 8 (30.8) | |
| Bilateral (%) | 5 (9.8) | 3 (11.5) | |
| IHDI grade | |||
| Type II (%) | 9 (16.1) | 0 (0) | 0.048b |
| Type III (%) | 31 (55.4) | 17 (58.6) | |
| Type IV (%) | 16 (28.6) | 12 (41.4) | |
| Age at reduction (months) (range; SD) | 13.16 (6–23; 4.85) | 14.73 (6–24; 5.30) | 0.196c |
| Duration of follow up (months) (range; SD/median) | 39.63 (24–74; 14.27) | 25 (24–74; 25)e | 0.109d |
| Age at final follow up (months) (range; SD) | 52.78 (30–90; 14.41) | 49.85 (30–83; 14.74) | 0.404c |
For calculation of each p value in the table
IHDI International Hip Dysplasia Institute
aChi-square test is used
bFisher's exact probability test is used
cTwo independent sample t test is used
dMann–Whitney U test is used; e is the median of reorganization data
42 (46 hips) and 26 patients’ (29 hips) complete MRI images within 48 h after operation in the CR and OR groups were measured, respectively. The average SJS (Student’s t test, t = 2.126; p = 0.037) and MJS (Student’s t test, t = 2.086; p = 0.040) in OR group were obviously less than that in the CR group (Table 2).
Table 2.
Comparison of superior joint space and medial joint space between the closed and open reduction groups on MRI within 48 h after operation
| Closed reduction (46 hips) | Open reduction (29 hips) | p value | |
|---|---|---|---|
| Superior joint space (mm) | 5.39 (2.25–8.28; 1.24) | 4.83 (3.09–6.59; 0.87) | 0.037 |
| Medial joint space (mm) | 3.44 (1.25–6.75; 1.35) | 2.83 (1.02–5.27; 1.05) | 0.040 |
Data are presented as the mean (range; standard deviation), each p value in the table is calculated by two independent-samples t test
During the final follow-up, two hips in two children with a persistent subluxation in the CR group underwent a second reduction surgery. Therefore, the re-dislocation rate was 3.45% (2/58) in the CR group. No re-dislocation occurred in the OR group. At the final follow-up, the AI in the OR group was slightly higher than that in the CR group (Table 3). The AI in the CR and OR groups was significantly improved compared with the AI before reduction (paired sample t test, t = 12.69 and 6.40, respectively; p = 0.001). The average AI improvements were 11.96° (− 8°–31°) and 8.76° (0°–28°) in the CR and OR groups (Student’s t test, t = 1.956, p = 0.054), respectively.
Table 3.
Comparison of the measurements between the closed and open reduction groups at the final follow-up
| Closed reduction (56 hips) | Open reduction (29 hips) | p value | |
|---|---|---|---|
| Acetabular index (°) | 25.34 (15–28; 3.14) | 27.69 (21–36; 4.19) | 0.027 |
| Centre-edge angle (°) | 12.61 (− 9–26; 8.30) | 10.45 (0–23; 5.58) | 0.212 |
| Alsberg angle (°) | 77.66 (60–89; 6.84) | 81.97 (73–91; 4.33) | 0.001 |
| Height-to-width index | 0.46 (0.24–0.59; 0.07) | 0.46 (0.37–0.57; 0.05) | 0.746 |
| Reimer’s migration index (%) | 26.09 (5–54; 11.11) | 30.23 (17–44; 8.27) | 0.081 |
Data are presented as the mean (range; standard deviation), each p value in the table is calculated by two independent-samples t test
At the last follow-up, there was no significant difference between the two groups for CEA, HWI, and RMI; however, the AA in the OR group was significantly higher than that in the CR group (Table 3, Figs. 1, 2). The incidence of AA > 81° was higher in the OR group than in the CR group (χ2 = 5.530, p = 0.019, Table 4).
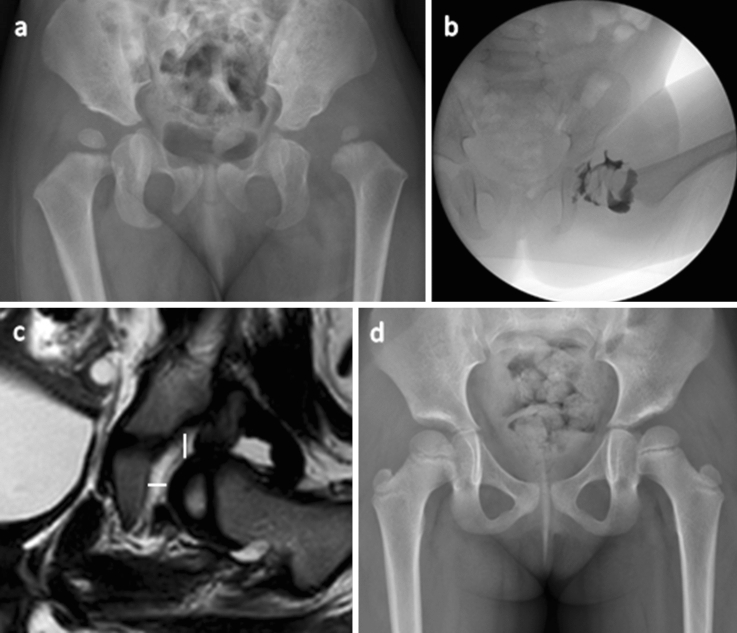
Fig. 1.
A girl of 15-month old with developmental dysplasia of the hip in the left hip underwent closed reduction. a: Preoperative anteroposterior pelvic radiograph; b: Intraoperative arthrogram after closed reduction; c: Postoperative MRI during 48 h, the superior and medial joint space were 5.31 mm and 3.75 mm, respectively; d: Anteroposterior pelvic radiograph 45 months after surgery; Shenton’s line was intact; the shape and size of the femoral head were similar to that of the contralateral side; acetabular index is 23°; alsberg angle is79°
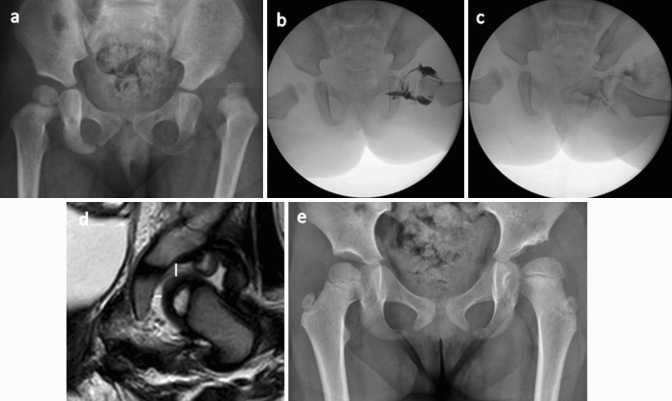
Fig. 2.
Female, 14 months old, open reduction for DDH in the left hip a Preoperative anteroposterior pelvic radiograph; b Intraoperative arthrogram after closed reduction with widened medial joint space; c Intraoperative arthrogram after open reduction; d Postoperative MRI during 48 h, the superior and medial joint space were 3.98 mm and 2.05 mm, respectively. e Anteroposterior pelvic radiograph 41 months after surgery; the shape and size of the femoral head were larger than that of the contralateral side; left acetabular index is 29°; right acetabular index is 19°; left alsberg angle is 88°; right alsberg angle is 79°
Table 4.
Morphological comparison of the hip joints between the closed and open reduction groups at the final follow-up
| Closed reduction number (%) | Open reduction number (%) | p value | |
|---|---|---|---|
| Residual acetabular dysplasia | |||
| Positive | 18 (32.14) | 14 (48.28) | 0.146 |
| Negative | 38 (67.86) | 15 (51.72) | |
| Height-to-width index | |||
| ≥ 0.357 | 52 (92.86) | 29 (100) | 0.294* |
| < 0.357 | 4 (7.14) | 0 (0) | |
| Alsberg angle | |||
| ≤ 81º | 38 (67.86) | 12 (41.38) | 0.019 |
| > 81º | 18 (32.14) | 17 (58.62) | |
| Reimer’s migration index | |||
| ≤ 33% | 40 (71.43) | 15 (51.72) | 0.071 |
| > 33% | 16 (28.57) | 14 (48.28) | |
*The calculation of p value adopts Fisher's exact probability test; the rest adopts chi-square test
According to Salter’s criteria, AVN was found in 15 (26.79%) and 10 (34.48%) hips in the CR and OR groups, respectively (χ2 = 0.545, p = 0.460). In patients with unilateral DDH, the frequencies of the coxa magna (> 15% of the normal side) were 6.5% (3/46) and 60.9% (14/23) in the CR and OR groups (continuous correction χ2 test, χ2 = 21.553, p < 0.001), respectively (Figs. 1, 2).
Discussion
Complete concentric reduction of the femoral head and acetabulum is a necessary condition for the normal development of the hip joint. Stable CR with an MDP of < 4 mm can obtain good long-term results [20]. However, the average MJS on postoperative MRI in the OR group is close to 2 mm which is apparently less than that in the CR group. The factors that affect the quality of CR include abnormal bony, cartilaginous, and soft tissue structure. The CR standard for safety and stability in our study combined the effects of these pathological factors. For the first time, this study compared the results of OR and CR under a similar degree of DDH reducibility and excluded the influence of different baseline factors before reduction.
The remodeling ability of the acetabulum is an important internal factor for the normal development of the hip joint after CR or OR. The AI is an important index for the morphological development of the acetabulum and an important reference for the prognosis of reoperation intervention and long-term osteoarthritis. Generally, the AI of normal infants decreases continuously before the age of 4, which is the peak of development. After the age of 4, development enters the platform stage [18, 19]. The key period of acetabulum shaping is 2 years after DDH reduction [21], and the remodeling ability is obviously weakened by the age of 4 years [22]. Therefore, CR should be performed in patients aged < 2 years to make full use of the self-shaping ability of the acetabulum.[2, 3, 23]. The average age at the final follow-up in our study was > 48 months, allowing us to fully compare acetabulum shaping between the groups. It is traditionally believed that a better acetabular remodelling would be achieved if an earlier fully concentric reduction was maintained through OR. However, the current results indicated that the improvement of AI, incidence of RAD, CEA, and RMI were not different between CR and OR when the reducibility was similar; therefore, our results demonstrate that a safe and stable CR is acceptable in children aged 6–24 months [5].
Re-dislocation is a common complication of CR or OR. The reported re-dislocation rates vary between 0 and 18% [3, 24]. In a multicentre, prospective study, a re-dislocation rate of 9% after CR was reported [25]. In the CR group of our study, the subluxation rate was 3.45%. This may be related to our emphasis on the stability of reduction (safe zone > 30°) and shows that stability was important for the maintenance of reduction. There was no re-dislocation in the OR group, which may be related to the small sample size and biased sample selection.
Previous studies have suggested that OR increases the risk of osteonecrosis, but other studies do not support this conclusion. [24, 26, 27] Here, there was no significant difference in the presence of AVN between the two groups. Because of the lack of follow-up to bone maturity, the Kalamchi–MacEwen method could not be used for accurate typing of AVN.
An increase of coxa magna after DDH reduction is a common developmental disorders. If the increase in the width of the epiphyseal nucleus of the femoral head is > 15% of the normal side, it may eventually lead to adverse consequences [17, 28]. Our study indicated that overgrowth of the femoral head was related to OR. In unilateral DDH patients, the frequency of the coxa magna was 6.5% (3/46) in the CR group but is 60.9% (14/23) in the OR group. Imatani et al. [28] observed that even if children receiving OR had concentric and matched reduction, excessive growth of the femoral head cartilage occurred several months postoperatively and resulted in a poorer prognosis. Excessive growth after OR may be related to the abnormal mechanical stress caused by acetabular dysplasia or subluxation[17] and/or induction of synovitis in the hip joint that may increase the vascularization of the femoral head, activate chondrocytes, and lead to overgrowth of the femoral head [29]. Furthermore, overgrowth of the femoral head may be related to changes in microcirculation within the proximal femur after OR; however, more studies are needed to confirm this.
The orientation of the proximal femur epiphysis (OPFE) is an important reference for the morphological development of the proximal femur and serves as the basis for the diagnosis and early surgical intervention of Kalamchi–MacEwen type II developmental disturbance [30]. The AA can be used as an index to measure OPFE. In children with successful CR, the AA reached the level found in normal children (approximately 73°) by the age of 5 [15]. Here, the increased AA in the OR group (Fig. 2) indicated that OR interfered with the development of the OPFE, which has not been reported previously. Special attention should be paid to long-term follow-up for patients with DDH who undergo OR to determine the incidence of type II development disorder during the bone maturation period.
Our study has the following limitations. First, a retrospective study inevitably presents a selective bias. Second, we only compared the AI and IHDI classification of the two groups before reduction; thus, other pathological factors may have hindered reduction. Third, with short-term follow-up, the hip joint did not reach the mature developmental state, making it impossible to accurately compare AVN and the reoperation rate of the two groups. Fourth, bilateral DDH is an important factor for poor prognosis; however, here, there were few bilateral cases, and stratified analysis was not possible. Therefore, it was not clear whether there were differences in the outcomes of CR or OR in bilateral DDH. Fifth, OR can increase stability after reduction and maintain the reduction with a relatively small abduction angle, but this effect was not specifically evaluated.
In summary, although OR can achieve maximum concentric reduction, it had a potential risk of leading to development disturbance of the proximal femur, due to the invasiveness of OR and the vulnerability of the femoral head in infants and young children. In children aged 6–24 months with DDH, if a stable and safe CR can be obtained but with a medial joint space up to 6 mm, an OR may not benefit acetabular remodelling more than a CR procedure. Therefore, CR should be attempted for these patients first, although further research is warranted to determine the long-term outcomes of CR and OR.
Acknowledgements
This work was supported by National Nature Science Foundation of China (Grant number: 81772296).
Author contributions
SM: data collection and analysis, manuscript preparation. WZ: data collection and analysis, manuscript preparation. LL: project administration, manuscript revision, fund acquisition. EW: data collection and analysis. LZ: data analysis, manuscript revision. QL: data analysis, manuscript revision.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Medical Ethics Committee of the authors' institution (Approval No. 2020PS113K).
Informed consent
Informed consent was waived due to the retrospective design of this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. Journal of American Academy of Orthopaedic Surgeons. 2001;9(6):401–411. doi: 10.5435/00124635-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Li Y, Zhou Q, Liu Y, Chen W, Li J, Canavese F, Xu H. Closed reduction and dynamic cast immobilization in patients with developmental dysplasia of the hip between 6 and 24 months of age. European Journal of Orthopaedic Surgery & Traumatology. 2019;29(1):51–57. doi: 10.1007/s00590-018-2289-5. [DOI] [PubMed] [Google Scholar]
- 3.Tennant SJ, Eastwood DM, Calder P, Hashemi-Nejad A, Catterall A. A protocol for the use of closed reduction in children with developmental dysplasia of the hip incorporating open psoas and adductor releases and a short-leg cast: Mid-term outcomes in 113 hips. The Bone & Joint Journal. 2016;98-B(11):1548–1553. doi: 10.1302/0301-620X.98B11.36606. [DOI] [PubMed] [Google Scholar]
- 4.Talathi NS, Chauvin NA, Sankar WN. Docking of the femoral head following closed reduction for DDH: Does it really occur. Journal of Pediatric Orthopedics. 2018;38(8):e440–e445. doi: 10.1097/BPO.0000000000001199. [DOI] [PubMed] [Google Scholar]
- 5.Zhou W, Sankar WN, Zhang F, Li L, Zhang L, Zhao Q. Evolution of concentricity after closed reduction in developmental dysplasia of the hip. The Bone & Joint Journal. 2020;102-B(5):618–626. doi: 10.1302/0301-620X.102B5.BJJ-2019-1496.R1. [DOI] [PubMed] [Google Scholar]
- 6.Cooper AP, Doddabasappa SN, Mulpuri K. Evidence-based management of developmental dysplasia of the hip. Orthopedic Clinics of North America. 2014;45(3):341–354. doi: 10.1016/j.ocl.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Li Y, Xu H, Li J, Yu L, Liu Y, Southern E, Liu H. Early predictors of acetabular growth after closed reduction in late detected developmental dysplasia of the hip. Journal of Pediatric Orthopedics Part B. 2015;24(1):35–39. doi: 10.1097/BPB.0000000000000111. [DOI] [PubMed] [Google Scholar]
- 8.Vaquero-Picado A, González-Morán G, Garay EG, Moraleda L. Developmental dysplasia of the hip: Update of management. EFORT Open Reviews. 2019;4(9):548–556. doi: 10.1302/2058-5241.4.180019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alsiddiky AM, Bakarman KA, Alzain KO, Aljassir FF, Al-Ahaideb AS, Kremli MK, Zamzam MM, Mervyn Letts R. The early detection and management of unstable concentric closed reduction of DDH with percutaneous K-wire fixation in infants 6 to 12 months of age. Journal of Pediatric Orthopedics. 2012;32(1):64–69. doi: 10.1097/BPO.0b013e318236b1fc. [DOI] [PubMed] [Google Scholar]
- 10.Tarassoli P, Gargan MF, Atherton WG, Thomas SR. The medial approach for the treatment of children with developmental dysplasia of the hip. The Bone & Joint Journal. 2014;96-B(3):406–413. doi: 10.1302/0301-620X.96B3.32616. [DOI] [PubMed] [Google Scholar]
- 11.Abousamra O, Deliberato D, Singh S, Klingele KE. Closed vs open reduction in developmental dysplasia of the hip: The short-term effect on acetabular remodeling. Journal of Clinical Orthopaedics and Trauma. 2020;11(2):213–216. doi: 10.1016/j.jcot.2019.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tennant SJ, Hashemi-Nejad A, Calder P, Eastwood DM. Bilateral developmental dysplasia of the hip: Does closed reduction have a role in management? Outcome of closed and open reduction in 92 hips. Journal of Pediatric Orthopedics. 2019;39(4):e264–e271. doi: 10.1097/BPO.0000000000001297. [DOI] [PubMed] [Google Scholar]
- 13.Ramsey PL, Lasser S, MacEwen GD. Congenital dislocation of the hip. Use of the Pavlik harness in the child during the first six months of life. Journal of Bone and Joint Surgery. 1976;58(7):1000-4. doi: 10.2106/00004623-197658070-00017. [DOI] [PubMed] [Google Scholar]
- 14.Dhar S, Taylor JF, Jones WA, Owen R. Early open reduction for congenital dislocation of the hip. Journal of Bone and Joint Surgery. British Volume. 1990;72(2):175–180. doi: 10.1302/0301-620X.72B2.2312552. [DOI] [PubMed] [Google Scholar]
- 15.Gui R, Canavese F, Liu S, Li L, Zhang L, Li Q. The potential role of the Alsberg angle as a predictor of lateral growth disturbance of the capital femoral epiphysis in children with developmental dysplasia of the hip treated by closed reduction. Journal of Children's Orthopaedics. 2020;14(2):106–111. doi: 10.1302/1863-2548.14.190158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthopaedica Scandinavica. 1980;184:1–100. doi: 10.3109/ort.1980.51.suppl-184.01. [DOI] [PubMed] [Google Scholar]
- 17.Gamble JG, Mochizuki C, Bleck EE, Rinsky LA. Coxa magna following surgical treatment of congenital hip dislocation. Journal of Pediatric Orthopedics. 1985;5(5):528–533. doi: 10.1097/01241398-198509000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Li LY, Zhang LJ, Li QW, Zhao Q, Jia JY, Huang T. Development of the osseous and cartilaginous acetabular index in normal children and those with developmental dysplasia of the hip: A cross-sectional study using MRI. Journal of Bone and Joint Surgery. British Volume. 2012;94(12):1625–1631. doi: 10.1302/0301-620X.94B12.29958. [DOI] [PubMed] [Google Scholar]
- 19.Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clinical Orthopaedics and Related Research. 1976;119:39–47. [PubMed] [Google Scholar]
- 20.Drummond DS, O’Donnell J, Breed A, Albert MJ, Robertson WW. Arthrography in the evaluation of congenital dislocation of the hip. Clinical Orthopaedics and Related Research. 1989;243:148–156. doi: 10.1097/00003086-198906000-00022. [DOI] [PubMed] [Google Scholar]
- 21.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. The Journal of Bone and Joint Surgery. British Volume. 2004;86(6):876–886. doi: 10.1302/0301-620X.86B6.14441. [DOI] [PubMed] [Google Scholar]
- 22.Shin CH, Yoo WJ, Park MS, Kim JH, Choi IH, Cho TJ. Acetabular remodeling and role of osteotomy after closed reduction of developmental dysplasia of the hip. Journal of Bone and Joint Surgery. American Volume. 2016;98(11):952–957. doi: 10.2106/JBJS.15.00992. [DOI] [PubMed] [Google Scholar]
- 23.Alassaf N. Treatment of developmental dysplasia of the hip (DDH) between the age of 18 and 24 months. European Journal of Orthopaedic Surgery & Traumatology. 2020;30(4):637–641. doi: 10.1007/s00590-019-02601-5. [DOI] [PubMed] [Google Scholar]
- 24.Pospischill R, Weninger J, Ganger R, Altenhuber J, Grill F. Does open reduction of the developmental dislocated hip increase the risk of osteonecrosis. Clinical Orthopaedics and Related Research. 2012;470(1):250–260. doi: 10.1007/s11999-011-1929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sankar WN, Gornitzky AL, Clarke N, Herrera-Soto JA, Kelley SP, Matheney T, Mulpuri K, Schaeffer EK, Upasani VV, Williams N, Price CT, International Hip Dysplasia Institute Closed reduction for developmental dysplasia of the hip: Early-term results from a prospective, multicenter cohort. Journal of Pediatric Orthopedics. 2019;39(3):111–118. doi: 10.1097/BPO.0000000000000895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Firth GB, Robertson AJ, Schepers A, Fatti L. Developmental dysplasia of the hip: Open reduction as a risk factor for substantial osteonecrosis. Clinical Orthopaedics and Related Research. 2010;468(9):2485–2494. doi: 10.1007/s11999-010-1400-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Novais EN, Hill MK, Carry PM, Heyn PC. Is age or surgical approach associated with osteonecrosis in patients with developmental dysplasia of the hip? A meta-analysis. Clinical Orthopaedics and Related Research. 2016;474(5):1166–1177. doi: 10.1007/s11999-015-4590-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imatani J, Miyake Y, Nakatsuka Y, Akazawa H, Mitani S. Coxa magna after open reduction for developmental dislocation of the hip. Journal of Pediatric Orthopedics. 1995;15(3):337–341. doi: 10.1097/01241398-199505000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Gershuni-Gordon DH, Axer A. Synovitis of the hip joint—An experimental model in rabbits. The Journal of Bone and Joint Surgery. British Volume. 1974;56(1):69–77. [PubMed] [Google Scholar]
- 30.Shin CH, Hong WK, Lee DJ, Yoo WJ, Choi IH, Cho TJ. Percutaneous medial hemi-epiphysiodesis using a transphyseal screw for caput valgum associated with developmental dysplasia of the hip. BMC Musculoskeletal Disorders. 2017;18(1):451. doi: 10.1186/s12891-017-1833-5. [DOI] [PMC free article] [PubMed] [Google Scholar]