Abstract
Introduction
There is no distinct classification system to evaluate the bone defect in previously managed acetabular fractures. We propose a new classification system for bone defect evaluation in a previously managed acetabular fracture that will be helpful for total hip arthroplasty (THA).
Materials and Methods
The preoperative pelvis radiographs of 99 THA patients with previous acetabular fractures with at least 2 years of follow-up were evaluated by 10 experienced surgeons (Paprosky and new classification systems). As per the new classification system, the five types of bone defects are circumferential, posterior wall, posterior column, both column defect, and anterior column. The interobserver and intraobserver reliability was calculated, and a consensus management plan based on the recommendation of the observers was formulated.
Results
There was fair interobserver reliability for Paprosky classification (alpha coefficient 0.39) and substantial interobserver reliability for the new classification (alpha co-efficient 0.71). There was a substantial intraobserver agreement for the new classification (kappa value 0.80) and moderate intraobserver agreement for Paprosky classification (kappa value 0.55). Sixty-nine patients who were treated as per the management plan of the observers reported significant improvement in modified Harris hip score (improved from 25 to 85.88, p < 0.001). 89.7% of patients reported good to excellent outcomes. Overall best health as per EQ-5D VAS was obtained in THA following anterior column fracture (EQ-5D VAS 97.5), and relatively poor health was obtained after THA of posterior column nonunion (EQ-FD VAS 80).
Conclusions
The new classification system for bone defect evaluation in previously treated acetabular fractures is valid and reliable. The proposed surgical plan for the management of bone defects in THA provided good to excellent outcomes.
Keywords: Acetabulum, Paprosky, Total hip replacement, Neglected acetabulum fracture, Bone defect
Introduction
Total hip arthroplasty (THA) after acetabular fractures is challenging, and studies have reported inferior outcomes than non-traumatic osteoarthritis [1–7]. THA in acetabular fractures is indicated in acute fractures, previously operated acetabular fractures, and conservatively managed acetabular fractures. The surgical problems in all three scenarios are diverse. The scar, soft tissue fibrosis, bone defect, prior retained hardware, distorted anatomy, malunion, and nonunion make the surgery complex. There is also an increased risk of infection [1–7].
There is no distinct classification to evaluate the bone defect in postacetabular fractures. Paprosky and American Academy of Orthopaedic Surgeons (AAOS) classifications are widely used even for postacetabular fracture bone defect evaluation [8–12]. However, these two classifications were mainly based on bone defect evaluation for revision arthroplasty. The pattern of bone defect in revision scenarios is different, and it arises because of osteolysis and cup migration [8–12]. The classification proposed by Marmor et al. in acute acetabular fractures of geriatric patients was based on mapping the stable articular surface, and it helps the surgeons specify the pelvic bone corridor for stable cup fixation [13]. However, this classification is not applicable for bone defect evaluation in previously managed acetabular fractures.
A classification system should provide an accurate and adequate description of the problem so that the treatment providers can communicate properly. It should help in preoperative evaluation, allow for appropriate surgical planning, and predict the outcomes after surgery. Although it is difficult to formulate a classification that fulfills all of the above criteria, it should be able to address the major problem. THA after acetabular fracture in developing and underdeveloped countries is more challenging and needs a robust classification system that should guide the surgeon about the surgical plan. Late presentations, neglected fractures, and inadequate treatment are additional problems to the inherent complexities of the THA in acetabular fractures [14]. The purpose of this study is to propose a new classification to evaluate the bone defect in previously managed or neglected acetabular fractures. The radiological interpretation was correlated to intraoperative findings. The interobserver reliability was evaluated, and a treatment plan was proposed.
Materials and Methods
Between June 2006 and December 2019, we operated on 213 patients with THA for their hip problem following the acetabular fracture. The radiographs, intraoperative findings, and clinical outcomes of these patients were retrieved from the clinical case records and our arthroplasty database. The patients with complete radiological and clinical details with a minimum of 2-years follow-up were included in the study. There were 131 patients with complete data; however, 25 patients had associated infection and were hence excluded. In the remaining 106 patients, 84 were males, and 22 were females. Sixty-one patients had acetabular nonunion, malunion, or a combination of nonunion-malunion following previous nonoperative treatment or neglected injury, and 45 patients had undergone prior osteosynthesis. The institutional ethics committee approved the study.
The preoperative radiographs of these 106 patients were arranged in a digital folder, and it was sent to 10 experienced pelvis-acetabular surgeons for evaluation of the acetabular bone defects using Paprosky classification and our new classification. The first seven patients' radiographs were provided as case examples and demonstrated clearly in the folder for clarification and a better understanding of the bone defects. These bone defects were also classified as per the new classification and Paprosky classification (utilized the scoring system of Yu et al.) [10]. The remaining radiographs of 99 patients were arranged sequentially in the digital folder for bone defect classifications and management plans.
The surgeons who participated in this bone defect evaluation had more than 5 years of experience in pelvi-acetabular surgery, and seven out of ten have more than 15 years of experience. All surgeons had more than 5 years of experience in revision arthroplasty, and five had more than 15 years of experience. Seven out of 10 surgeons had operated on more than 50 cases of total hip arthroplasty following acetabular fractures. The radiographs were sent again after 2 weeks to the same observers for re-classification and to look for intraobserver reliability.
The Paprosky classification is based on four radiographic landmarks in the anteroposterior view of the pelvis (5): (1) superior defect, (2) Kohler line, (3) teardrop defect, and (4) ischial defect [10].
Our new classification was based on the acetabular fracture classification of Letournel and Judet. The acetabular defects have resulted from primary traumatic displacements of the acetabular wall or columns that are completely reduced, partially reduced, or not at all reduced at the primary instance. Accordingly, the radiographic landmarks in the anteroposterior view of the pelvis are: (1) posterior wall (2) ilioischial line (3) iliopectineal line (4) position of the femoral head/ direction of migration of femoral head (Fig. 1).
Fig. 1.
The landmarks for the acetabular bone defect evaluation
The directions of migration of the femoral head were of three types:
superior: posterosuperior or superolateral (involving posterior wall).
superomedial (involving posterior column mainly).
medial or anteromedial (involving anterior column with quadrilateral plate).
Based on these radiographic parameters from the anteroposterior view of X-ray, the acetabular bone defects were graded into five types (Table 1, Fig. 2).
Table 1.
New classification based on radiographic landmarks in an X-ray ap view of pelvis with bilateral hips
| New classification type | Posterior wall | Illioischial line | Illiopectineal line | Femoral head position/migration |
|---|---|---|---|---|
| Type 1 (circumferential widening) | Present | Undisplaced | Undisplaced | Minimal |
| Type 2 (posterior wall) | Absent/displaced | Undisplaced | Undisplaced | Posterior superior/supero-lateral/dislocated |
| Type 3 (posterior column) | ||||
| 3A (malunion or fibrous union) | Present | Displaced but not broken | Undisplaced | Supero-medial |
| 3B (frank non-union) | Present | Displaced and broken | Undisplaced | Superomedial |
| Type 4 (transverse) | ||||
| 4A-malunion or fibrous non-union | Present | Displaced but not broken | Displaced but not broken | Supero-medial |
| 4B-frank non-union (pelvic discontinuity) | Present | Displaced and broken | Displaced and broken | Supero-medial |
| Type 5 (anterior column) | Present | Undisplaced | Displaced | Medial |
Fig. 2.

Diagramatic representation of the acetabular bone defect classification (Type 1: cavitary, or circumferential; type 2: posterior wall defect, type 3: A posterior column fibrous union/malunion, B nonunion; type 4: A transeverse fracture fibrous union/malunion, B nonunion; Type 5: anterior column nonunion)
Type 1 (circumferential/cavitary): There is a circumferential widening of the acetabulum because of healed minimally displaced fracture, less than adequate reduction, or secondary arthritis (Fig. 3).
Fig. 3.
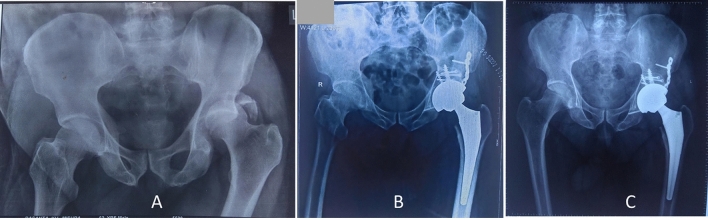
A Post-traumatic arthritis following acetabular fracture fixation with minimal bone defect (Type 1). B Uncemented THA was performed
Type 2 (posterior wall defect): These are the sequel of an unreduced or failed reduction of posterior wall fractures. These are some of the most common acetabular defects found in neglected hip trauma. On an anteroposterior view of the pelvis, one would find (1) a separate posterior wall fragment, (2) an intact ilioischial line (intact posterior column), (3) an intact iliopectineal line (intact anterior column) (4) head migration posterosuperiorly or superolaterally or dislocated posteriorly (Fig. 4).
Fig. 4.
A 3-month-old neglecetd posterior wall acetabular fracture in a 65-year-old male (Type 2). B Uncemented total hip arthroplasty after posterior wall reconstruction using femoral head autograft and buttress plate. C Two-year follow-up X-ray shows completely incorporated graft and stable THA
Type 3 (posterior column): This pattern of defect is primarily associated with posterior column fractures that may be associated with a posterior wall fracture. Radiologically, one may find a separate posterior wall. The ilioischial line is displaced, but the iliopectineal line remains intact. The femur head might have migrated superomedially (more superior than medial). Since the continuity of the posterior column is of utmost importance for a total hip replacement in such a scenario, It was further divided into two types; type 3A (ilioischial line is displaced but still maintains the continuity in malposition) and type 3B (the ilioischial line is displaced significantly) (Fig. 5).
Fig. 5.
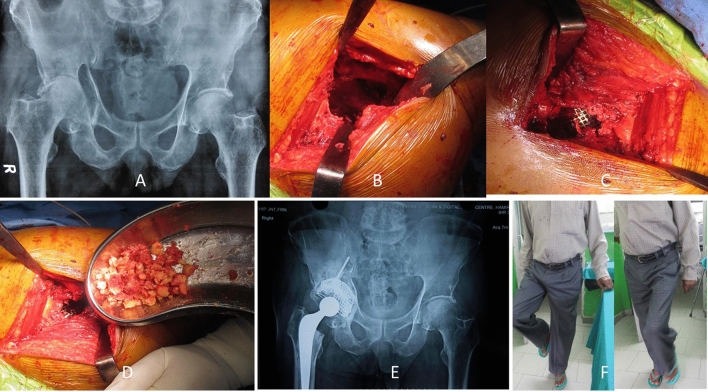
19-year adult with 1-year neglected acetabulum fracture. A The bone defect as per the new classification is Type 3B (posterior column nonunion). B–E Intraoperative pictures shows the posterior column bone defect, reconstructed with femoral head autograft and reconstruction plate, the posterior superomedial defect was filled up with morcellized bone graft and uncemented THA was performed. F Postoperative radiograph shows stable hip and stable components. G–I At 2-year follow up, the radiological and functional outcome is excellent
Type 4 (both column/transverse): This pattern of defects is primarily associated with the transverse pattern of acetabular fractures, which may be seen following transverse fracture, T-type fractures, or anterior column with posterior hemitransverse fracture. Radiological findings are displacement of both the ilioischial line and iliopectineal line. The femur head migration is superomedial (if more superior, the posterior column is involved more, and if more medial-anterior column is involved more). Again, depending on the continuity of the displaced fragments in malposition, these are subdivided into two types. (Fig. 6, 7).
Fig. 6.
48-year-old male with previously operated acetabular fracture. A, Preoperative radiograph shows displaced iliopectineal and ilioischial lines indicating type 4A bone defect. B, Impaction bone grafting and uncemented THA resulted in stable well-functioning hip
Fig. 7.
A One-year neglected anterior column with posterior hemitransverse fracture. B Both columns are displaced indicating pelvis discontinuity (Type 4B). C Posterior column stabilized with bone graft and recon plate. Morcellized bone graft was impacted medially and posteriorly followed by reconstruction with Burch-Schneider Reinforcement cage and cemented cup. D Two years later, the graft is well incorporated and the THA is stable and functional
Type 4A: The ilioischial line or iliopectineal line is displaced but continuous due to malunion.
Type 4B: ilioischial line is significantly displaced, and there is no pelvic continuity with frank nonunion.
Type 5 (anterior column): These bone defects are primarily associated with anterior acetabular fracture, but the posterior column and wall are maintained or not displaced. These could be the result of residual displacement following anterior column fracture, anterior column posterior hemitransverse fracture, or both column fractures. In these defects, the proximal 2/3rd of the ilioischial line is intact, posterior wall fragment is intact, but iliopectineal line is significantly displaced and may not have continuity. The femur head migration will be primarily medial (Fig. 8).
Fig. 8.
Secondary arthritis and anterior column bone defect in a conservatively treated acetabular fracture (Type 5). B Intraoperative photograph shows the bone defect. C, D Mesh and morcellized bone graft impaction was done to fill up the bone defect. E Three years following cemented THA. F, G Functional outcome of the hip is good (mHHS 83)
Data evaluation and statistical analysis
The response of the ten observers regarding the classification systems and management plan was recorded. The observers realized that the Paprosky classification is "not-Applicable (NA)" in a few radiographs (indicating missing values). The interobserver reliability (Alpha coefficient of Krippendorff), percentage level of agreement between the observers, and intraobserver reliability (Kappa coefficient) were calculated [15, 16]. The statistical analysis was performed using SPSS software version 26.0.
The interobserver reliability was calculated by the α (Alpha) coefficient of Krippendorff for the Paprosky classification and the new classification separately. Interpretation of Krippendorff’s alpha values were made according to Landis et al. [15]; poor (< 0), slight (0–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost perfect (0.81–1.00) [9, 10]. The percentage of agreement between the observers for each patient's radiograph was evaluated for both classifications. The interobserver agreement was also labeled using percentage agreement level, and it was divided into three categories: (1) excellent (≥ 0.80), (2) moderate (0.50–0.70), and (3) poor (≤ 0.49). A similar percentage level of agreement for both classifications was compared for statistical significance using Z test.
The hip radiographs showing an excellent level of agreement among the observers for the new classification were further analyzed for intraoperative findings correlation and suggested management plan. The ‘consensus management plan’ was based on the proposal of at least five observers for each type of bone defect in the new classification. The functional outcome (modified Harris hip score, mHHS) and health-related quality of life (EQ-5D VAS) of those patients who received the surgical treatment as per the 'consensus management plan' were analyzed statistically.
Results
The mean age of the patients was 46.3 years (range 19–62 years). Based on the radiographic analysis of 99 patients with acetabular bone defects, there was fair interobserver reliability for Paprosky classification (alpha coefficient 0.39) and substantial interobserver reliability for the new classification (alpha co-efficient 0.71). The percentage of agreement for the Paprosky classification was excellent for three patients, moderate for 33 patients, and poor for 63 patients. However, the percentage of agreement for the new classification was excellent for 69 patients, moderate for 17 patients, and poor for 13 patients. There was a substantial intraobserver agreement for the new classification (kappa value 0.80) and moderate intraobserver agreement for Paprosky classification (kappa value 0.55).
The z test for proportions revealed that there was a significant difference between the Paprosky and the new classification system for excellent, moderate, and poor percentage agreements with a p value < 0.001. (Table 2).
Table 2.
Comparison between Paprosky and new classification systems
| Criteria | Paprosky | New | Interpretation |
|---|---|---|---|
| Krippendorff’s alpha co-efficient | 0.39 | 0.72 |
New classification- significant inter-rater reliability Paprosky classification- moderate inter-rater reliability |
| Excellent percentage agreement (0.8 or more) | 3 | 69 | p value < 0.001 (significant) |
| Moderate percentage agreement (0.5 to 0.7) | 33 | 17 | p value = 0.001 (significant) |
| Poor percentage agreement (0.4 or less) | 63 | 13 | p value < 0.001 (significant) |
The intraoperative findings confirmed the bone defect appreciated by the surgeons in 69 hip radiographs with excellent agreement. The consensus management plan based on the new classification has been mentioned in Tables 3 and 4. Type 1 bone defect with an intact acetabular rim can be managed with conventional total hip arthroplasty. Posterior wall or posterior column defect or nonunion (type 2, 3B) needs structural autograft/allogarft fixation and buttress plate with an uncemented acetabular cup. The posterior column malunion or fibrous union needs impaction bone grafting with cemented or uncemented cup. The suggested treatment plan for transverse fracture nonunion or malunion was impaction bone grafting or structural bone graft fixation for the posterior column defect and uncemented or cemented cup implantation (Fig. 9). The alternative treatment plan for all posterior column or transverse fracture malunion/nonunion is impaction bone grafting with cup-cage construct (Tables 3, 4).
Table 3.
Management proposed as per excellent percentage agreement for cases with acetabular defects in the present study
| Type | Number of cases (total = 69) | Large uncemented cup | Structural graft + plating + uncemented cup | Impaction grafting + cemented cup | Trabecular metal augment | Cup-cage construct |
|---|---|---|---|---|---|---|
| 1 | 4 | 4 | ||||
| 2 | 24 | 20 | 4 | |||
| 3A | 2 | 1 | 1 | |||
| 3B | 2 | 1 | 1 | |||
| 4A | 15 | 6 | 7 | 2 | ||
| 4B | 15 | 9 | 6 | |||
| 5 | 7 | 7 |
Table 4.
Proposed management plan for new classification
| Type | Management |
|---|---|
| 1 | Large uncemented cup |
| 2 | Structural autograft + plate + uncemented cup |
| Trabecular metal augment + cemented/ uncemented cup | |
| 3A | Impaction grafting ± posterior column plating + cemented/ uncemented cup |
| Impaction grafting + cup-cage construct | |
| 3B | Structural graft + plate + uncemented cup |
| Impaction grafting + cup-cage construct | |
| 4A | Impaction grafting + large multihole uncemented cup/ cemented cup |
| Impaction grafting + cup-cage construct | |
| 4B | Structural graft + posterior column plating + multihole uncemented cup |
| Impaction grafting + cup-cage construct | |
| 5 | Impaction grafting ± mesh + uncemented/ cemented cup |
Fig. 9.
Algorithm for management of bone defect in postacetabular fracture as per the new classification (PW posterior wall, PC posterior column, AC anterior column)
There were 39 patients who were managed as per the proposed plan and completed at least 2 years of follow-up. The mean preoperative mHHS of 25 improved to 85.88 in the postoperative period (p < 0.001). There were 89.7% (n = 35) patients with good to excellent outcomes. Overall best health as per EQ-5D VAS was obtained in anterior column fracture (EQ-5D VAS 97.5), and relatively poor health was obtained in posterior column nonunion (EQ-FD VAS 80) (Table 5).
Table 5.
Management of cases according to the proposal of excellent percentage agreement with a minimum 2-year follow-up
| New classification type | Number of cases (n = 39) | Large uncemented cup | Bonegraft + plating | Bursch-schneider cage | Impaction grafting | Trabecular metal augment | Mean mHHS | EQ-5D VAS | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 3 | 3 | 92.3 | 91.67 | 4.7 | ||||
| 2 | 12 | 7 | 4 | 1 | 89.1 | 96.25 | 6 | ||
| 3A | 1 | 1 | 83.5 | 90 | 8 | ||||
| 3B | 1 | 1 | 81.7 | 80 | 5 | ||||
| 4A | 9 | 1 | 8 | 82.4 | 94.4 | 5.8 | |||
| 4B | 9 | 4 | 3 | 2 | 82.6 | 90 | 6 | ||
| 5 | 4 | 4 | 88.3 | 97.5 | 5 |
Discussion
The new acetabular bone defect evaluation classification in posttraumatic conditions showed better interobserver and intraobserver reliability. The radiological interpretation of the new classification matched the intraoperative findings. The treatment plan based on the classification seems appropriate, and 90% of patients reported good to excellent functional scores at a minimum of 2-year follow-up.
Bone defect patterns in postacetabular fracture and revision arthroplasty are different. Bone loss because of aseptic loosening of cemented or uncemented arthroplasty is a gradual process that occurs over a longer period of time [10, 17, 18]. The bone loss in posttraumatic conditions is, however, not orderly and determined mainly by the initial fracture pattern and surgical intervention. Paprosky classification, the most common classification to evaluate bone defect in revision arthroplasty, does not consider the posterior wall defect, which is the most common acetabular defect in neglected or previously treated acetabular fracture [19]. In the revision arthroplasty, ischial bone lysis is considered as a major predictor of the posterior column and posterior wall bone loss, but such defect is usually not seen in posttraumatic conditions. There is a medial shift in the posterior column (seen as the Illioischial line) following acetabular fracture that may be continuous (malunion), noncontinuous (nonunion), or can be seen as a separate posterior wall fragment [19]. There is no “lysis” of the teardrop in postacetabular fracture. In most cases, there may be a medial shift of the teardrop (suggestive of anterior column fracture) along with a break in the iliopectineal line.
The interpretation of the ilioischial line (aka Kohler line) is also different in a posttraumatic scenario. While Paprosky classification suggests that break in Kohler line with medial migration suggests loss of anterior column support, in a posttraumatic scenario, there is a much more proximal break or shift of the ilioischial line medially, causing the head to migrate more superiorly, representing a loss of the native bone in the posterior column.
The validity and reliability of Paprosky classification have been studied previously in revision total hip arthroplasty patients [17, 18, 20, 21]. This classification has been reported to be valid, but the subjective variations in interpretation of the radiological parameters have been acknowledged. Gozzard and associates reported poor to moderate reliability of Paprosky classification in 25 patients of revision arthroplasty [17]. The interobserver reliability ranged between 0.14 and 0.41 for four surgeons. The interobserver agreement for acetabular defect classification using Paprosky was 0.42 (moderate). Campbell et al. also reported poor intraobserver and interobserver reliability in 33 preoperative radiographs as evaluated by 3 observers of different expertise [21]. Yu et al. reported that teaching the observers and using the score for the radiological parameters can improve the reliability [10]. The interobserver reliability improved from a kappa coefficient of 0.56–0.79 after three teaching sessions. The other group who went for one teaching session reported improvement in interobserver reliability from 0.49 to 0.65. In agreement with the literature, we found poor interobserver reliability (alfa = 0.39) for acetabular defect evaluation using Paprosky classification for the posttraumatic scenario. The expertise of the evaluators also cannot be underrated. The observers were experts in pelvis-acetabulum and revision arthroplasty surgeries. We agree with Campbell et al. that this classification can act as a general guide and does not have reliability and consistency [21]. Paprosky classification is not designed for bone defect evaluation in posttraumatic conditions, creates confusion among the surgeons about the radiological interpretation, and leads to poor interobserver reliability even in posttraumatic acetabular defect [22].
Consistency and reliability are essential for any classification system. The available classification systems (Paprosky, AAOS, and Gross) for acetabular defects have not shown good reliability. Nevertheless, these systems were meant for revision arthroplasty scenarios [8, 9, 22]. The bone defect created after acetabular fracture is either a nonunion or malunion at the fracture site [19]. Accordingly, the new classification is based on the understanding of the original Letournel and Judet classification. The posterior wall, posterior column, and anterior column bone defects are seen as a sequela of respective fractures. However, fractures of both the columns as seen in transverse fracture, anterior column posterior hemitransverse, or T-fracture may unite anatomically or malunited in one column and may remain ununited on the other column. All these possible scenarios were taken into consideration for classifying these defects. The new classification showed excellent validity in our study because all 69 radiographs with excellent agreement correlated to the intraoperative findings. The interobserver reliability was substantial, and the intraobserver reliability was also excellent.
The treatment algorithm as proposed by the observers in this study was appropriate as the patients who operated through similar techniques reported good to excellent functional outcomes. It was observed that THA in posterior column nonunion had a relatively poor functional outcome. We agree with the literature that it is essential to have posterior column stability in THA for optimal outcomes. The best outcome was observed in patients with a circumferential widening of the acetabulum where only a bigger acetabular cup was needed, and the stability was not compromised.
There are certain limitations to this study. The observers who evaluated the radiographs were experts in pelvis-acetabular surgeries, and hence, the interpretation of the radiograph among the hip arthroplasty surgeons may differ. It might have effects on the reliability of our new classification system. The implants around the hip joint may obscure the radiological signs. However, the interpretations in nonoperatively treated and operatively treated acetabulum fractures were not separately evaluated. The surgical treatment plan proposed by the observers is based on the current availability of implants and the literature. Accordingly, the treatment options may change with time. Although CT scan may better delineate the fracture nonunion and malunion, the present classification works as a rough guide for treatment plan and cannot substitute the role of CT scan.
To conclude, the new classification system for bone defect evaluation in previously treated acetabular fractures before proceeding for THA is valid and reliable. The proposed surgical plan for different types of bone defects provided good to excellent outcomes; it can be considered as a guideline for surgical management of bone defects in acetabular fracture.
Author contributions
SKT, RKS, RM and SKS designed the study. RM and GS collected the data. RM, and SKS analysed the data. The draft was prepared by SKT and RM. All authors read the manuscript and approved it for publication.
Funding
The authors did not receive support from any organization for the submitted work.
Availability of Data and Material
The data of the study are available to share. The data will be shared on request. This presentation was presented by DR Ramesh Sen in AO trauma masters course and European pelvis expert group.
Materials and/or Code Availability
Available on request.
Declarations
Conflict of Interest
The authors of this manuscript declare that they have no conflicts of interest to disclose.
Ethical Approval
We certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards been approved by the Max Hospital ethics committee, Mohali, Chandigarh.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent to Participate
Consent was obtained from all participants before recruitment into the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ramesh K. Sen, Email: senramesh@rediffmail.com
Reet Mukhopadhyay, Email: reetm.2008@gmail.com.
Veeresh Pattanshetti, Email: veeresh.Shetti7@gmail.com.
Gaurav Saini, Email: gauravsainichd@yahoo.co.in.
Sujit Kumar Tripathy, Email: ortho_sujit@aiimsbhubaneswar.edu.in, Email: sujitortho@aiimsbhubaneswar.edu.in, Email: sujitortho@yahoo.co.in.
Suresh Kumar Sharma, Email: ssharma643@yahoo.co.in.
References
- 1.Gautam D, Gupta S, Malhotra R. Total hip arthroplasty in acetabular fractures. Journal of Clinical Orthopaedics Trauma. 2020;11(6):1090–1098. doi: 10.1016/j.jcot.2020.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stibolt RD, Jr, Patel HA, Huntley SR, Lehtonen EJ, Shah AB, Naranje SM. Total hip arthroplasty for posttraumatic osteoarthritis following acetabular fracture: A systematic review of characteristics, outcomes, and complications. Chinese Journal of Traumatology. 2018;21(3):176–181. doi: 10.1016/j.cjtee.2018.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu M, Phillips D. Total hip arthroplasty for posttraumatic conditions. Journal of American Academy of Orthopaedic Surgeons. 2019;27(8):275–285. doi: 10.5435/JAAOS-D-17-00775. [DOI] [PubMed] [Google Scholar]
- 4.Ranawat A, Zelken J, Helfet D, Buly R. Total hip arthroplasty for posttraumatic arthritis after acetabular fracture. J Arthroplasty [Internet]. 2009;24(5):759–767. doi: 10.1016/j.arth.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Yuan BJ, Lewallen DG, Hanssen AD. Porous metal acetabular components have a low rate of mechanical failure in THA after operatively treated acetabular fracture. Clinical Orthopaedics and Related Research. 2015;473(2):536–542. doi: 10.1007/s11999-014-3852-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.von Roth P, Abdel MP, Harmsen WS, Berry DJ. Total hip arthroplasty after operatively treated acetabular fracture. Journal of Bone Joint Surgery. 2015;97(4):288–291. doi: 10.2106/JBJS.N.00871. [DOI] [PubMed] [Google Scholar]
- 7.Romness DW, Lewallen DG. Total hip arthroplasty after fracture of the acetabulum. Long-term results. Journal of Bone Joint Surgery Series B. 1990;72(5):761–764. doi: 10.1302/0301-620X.72B5.2211750. [DOI] [PubMed] [Google Scholar]
- 8.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. Journal of Arthroplasty. 1994;9(1):33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 9.D'Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH. Classification and management of acetabular abnormalities in total hip arthroplasty. Clinical Orthopaedics and Related Research. 1989;243:126–137. doi: 10.1097/00003086-198906000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Yu R, Hofstaetter JG, Sullivan T, Costi K, Howie DW, Solomon LB. Validity and reliability of the paprosky acetabular defect classification hip. Clinical Orthopaedics and Related Research. 2013;471(7):2259–2265. doi: 10.1007/s11999-013-2844-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Telleria JJ, Gee AO. Classifications in brief: Paprosky classification of acetabular bone loss. Clinical Orthopaedics Related Research. 2013;471(11):3725–3730. doi: 10.1007/s11999-013-3264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paprosky WG, Cross MB. CORR insights ®: Validity and reliability of the Paprosky acetabular defect classification. Clinical Orthopaedics and Related Research. 2013;471(7):2266. doi: 10.1007/s11999-013-2938-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marmor MT, Huang A, Knox R, Herfat S, Firoozabadi R. Mapping of the stable articular surface and available bone corridors for cup fixation in geriatric acetabular fractures. Journal of America Academics Orthopaedics Surgery. 2020;28(13):e573–e579. doi: 10.5435/JAAOS-D-18-00445. [DOI] [PubMed] [Google Scholar]
- 14.Sharma M, Behera P, Sen RK, Aggarwal S, Tripathy SK, Prakash M, Saini G, Saibaba B. Total hip arthroplasty for arthritis following acetabular fractures-evaluation of radiological, functional and quality of life parameters. Journal of Clinical Orthopaedics Trauma. 2019;10(1):131–137. doi: 10.1016/j.jcot.2017.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33(2):363. doi: 10.2307/2529786. [DOI] [PubMed] [Google Scholar]
- 16.Zapf A, Castell S, Morawietz L, Karch A. Measuring inter-rater reliability for nominal data—Which coefficients and confidence intervals are appropriate? BMC Medicine Research Methodology [Internet] 2016;16(1):1–10. doi: 10.1186/s12874-016-0200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gozzard C, Blom A, Taylor A, Smith E, Learmonth I. A comparison of the reliability and validity of bone stock loss classification systems used for revision hip surgery. Journal of Arthroplasty. 2003;18(5):638–642. doi: 10.1016/S0883-5403(03)00107-4. [DOI] [PubMed] [Google Scholar]
- 18.Ghanem M, Zajonz D, Heyde CE, Roth A. Acetabular defect classification and management: Revision arthroplasty of the acetabular cup based on 3-point fixation. Der Orthopäde. 2020;49(5):432–442. doi: 10.1007/s00132-020-03895-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Veerappa LA, Tripathy SK, Sen RK. Management of neglected acetabular fractures. European Journal of Trauma and Emergency Surgery. 2015;41(4):343–348. doi: 10.1007/s00068-014-0462-z. [DOI] [PubMed] [Google Scholar]
- 20.Johanson NA, Driftmier KR, Cerynik DL, Stehman CC. Grading acetabular defects: The need for a universal and valid system. Journal of Arthroplasty. 2010;25(3):425–431. doi: 10.1016/j.arth.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 21.Campbell DG, Garbuz DS, Masri BA, Duncan CP. Reliability of acetabular bone defect classification systems in revision total hip arthroplasty. Journal of Arthroplasty. 2001;16(1):83–86. doi: 10.1054/arth.2001.19157. [DOI] [PubMed] [Google Scholar]
- 22.Käfer W, Fraitzl CR, Kinkel S, Puhl W, Kessler S. Gültigkeit und Reproduzierbarkeit radiologischer Klassifikationskriterien des knöchernen Substanzdefekts vor Revisionshüftendoprothetik [Analysis of validity and reliability of three radiographic classification systems for preoperative assessment of bone stock loss in revision total hip arthroplasty] Zeitschrift fur Orthopadie und Ihre Grenzgebiete. 2004;142(1):33–39. doi: 10.1055/s-2004-818027. [DOI] [PubMed] [Google Scholar]
- 23.Gross AE, Allan DG, Catre M, Garbuz DS, Stockley I. Bone grafts in hip replacement surgery. The pelvic side. Orthopedic Clinics North America. 1993;24(4):679–695. doi: 10.1016/S0030-5898(20)31848-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data of the study are available to share. The data will be shared on request. This presentation was presented by DR Ramesh Sen in AO trauma masters course and European pelvis expert group.
Available on request.