Abstract
Using computed tomography scans, we were able to treat symptomatic osteoid osteoma of the distal radius with the help of 3D printing technology that involves designing bone models and fabricating surgical guides to locate the tumour precisely and resect it successfully with limited exposure without the use of any intraoperative imaging. This is a new technology that can be applied to treat bony lesions and can be an alternative solution to currently available techniques.
Keywords: Osteoid osteoma, 3D printing in osteoid osteoma, Additive manufacturing, 3D designs and guides, Bone tumour surgery
Introduction
Osteoid osteoma (OO) is the commonest benign bone tumour, presenting in the second decade of life with pain and diagnosed with radiographs and computed tomography (CT) scans. These tumours are known to self-regress over time and have improved with the use of aspirin and analgesics. The current trend of tumour removal is CT-guided percutaneous techniques, such as radiofrequency ablation, trephine excision, cryoablation, and laser thermo-coagulation [1]. However, these procedures require technical expertise, hospital facilities, and can lead to hazardous radiation exposure to the patient. In this report, we present a case of distal radius osteoid osteoma treated with the help of additive manufacturing (or three-dimensional (3D) printing) technology that was used to locate and remove the tumour with the help of a personalised fabricated device.
Statement of Informed Consent
The patient was informed that data concerning the case would be submitted for publication, and the patient agreed.
Case Report
An 18-year-old man, a mechanic by profession, presented to us with left forearm pain for more than 3 years despite analgesics, and it was affecting his daily activities. On examination, he had tenderness over the distal radius without restricting the range of motion. His radiograph revealed a thickened cortex of the radius at the metaphyseal–diaphyseal junction with negative ulnar variance, and a CT scan revealed a nidus surrounded by a sclerotic bone (10 mm × 5 mm in size) over the volar and ulnar sides of the radius, suggestive of an OO (Fig. 1). After a discussion with the patient about various options, we proceeded with tumour removal using the help of 3D printing technology.
Fig. 1.
A, B Radiograph of the left forearm showing thickened cortex at metaphysis–diaphysis junction with ulnar negative variance, C–E computed tomography of the forearm in sagittal, coronal and axial sections showing osteoid osteoma, a nidus surrounded by thick sclerotic bone
For 3D planning, the representative bone models were constructed based on the raw radiological data of the patient obtained in DICOM format from his CT scan. The DICOM files were processed in medical image processing software (Mimics, Materialise, Leuven, Belgium) to generate a 3D model of the bone. Following this, a 3D virtual model created in Mimics was exported to 3-Matic (Materialise, Leuven, Belgium) for further processing. The patient-specific guide was planned virtually after visualising the tumour using transparency over bone in such a way that the guide was contoured on the thickened bone with additional supports exactly on the tumour. The bone model and guide were exported as an STL file and transferred to the 3D printer. Bone models and guides were printed with PLA in the Ultimaker S5 Bundle. The guide had an oval opening (14 mm × 8 mm) replicating the tumour shape with 2 mm holes on either end for anchorage to the bone and flanges in the sides for better contouring (Fig. 2).
Fig. 2.
Schematic demonstrating the virtual planning for the surgery a bone model, b transparent bone to visualise the tumour, c tumour as highlighted in (b), d cross-sectional view of the tumour, e designer guide to extract the tumour, and f the bone post operation
After the printing, the patient was taken for a surgical procedure under regional anaesthesia. The limb was prepped on a side table, and the bone model was placed on the forearm, matching the radius. The location of the tumour was marked on the skin using the bone model, and a small incision was made over the distal radius using a Flexor carpi radialis approach, just enough to insert the guide. On reaching the bone, the guide was placed on the tumour and held with two pins on either side. Another 1.5 mm pin was taken and drilled unicortically on the inner borders of the oval hole in the guide to create a cortical window around the tumour, and a fine osteotome was used to remove the tumour with 2 mm margins of normal bone (Fig. 3). The wound was closed in layers, and the patient was sent for a CT scan to confirm tumour excision (Fig. 4). The patient had a drastic improvement in symptoms, and there were no signs of recurrence on a follow-up for 1 year duration. The sample was confirmed to be an OO on histopathology.
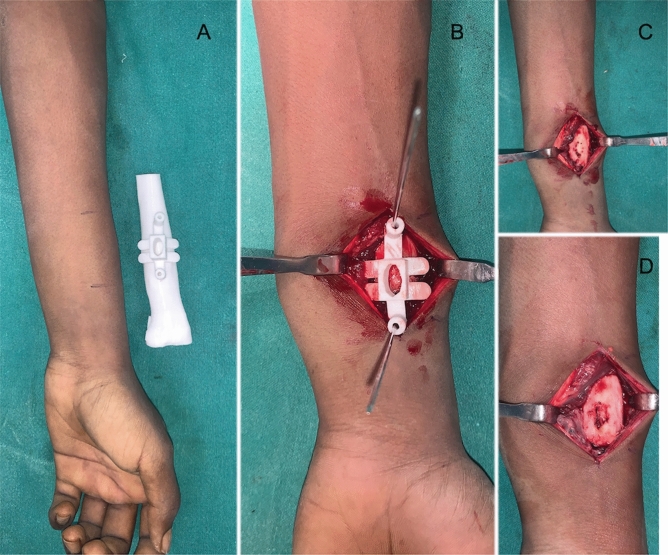
Fig. 3.
A 3D printed bone model placed against the forearm to locate the tumour postion, B the 3D printed guide placed over the radius and held with pins on either side, C cortical window created with the help of the guide after drilling and D radius after tumour resection
Fig. 4.
A–C Postoperative computed tomography of forearm in sagittal, coronal and axial sections to confirm tumour resection
Discussion
The current management options for OO are CT-guided, minimally invasive procedures. This procedure is routinely done by an interventional radiologist in a CT scan room under anaesthesia and is known to have a faster recovery. They have the added advantage of reaching inaccessible areas, such as the neck of the femur and pelvic bones [2]. Some of the complications of these minimally invasive techniques are persistent symptoms, iatrogenic fractures, revision procedures, injury to nearby tendons, and the need for a second open procedure to remove the tumour [2, 3]. We believe that CT-guided procedures involve hazardous radiation exposure to the patient. These are contraindicated in areas closer to neurovascular structures, the spine, and small bones, although there are few successful case reports. Another drawback is the inability to obtain a sample for histopathological confirmation most of the time. To perform this technique, hospital facilities, expertise, and higher costs are involved.
On the other hand, an open procedure can be of two types: (a) wide en bloc resection with the surrounding bone and (b) unroofing of nidus and excision of tumour with curette and burr [3]. For open procedures, identifying the tumour is based on gross pathological changes, which requires experience and often needs a wider surgical exposure as most of these tumours are unrecognisable on radiographs [4]. Some centres use intraoperative CT, Scintigraphy, or teracycle labelling to locate the tumour [5, 6]..Wide en bloc resection may require a larger area of bone to be removed, often requiring the use of internal fixation, bone graft, or post-operative immobilisation [7].
OO due to chronic inflammation causes a periosteal reaction, sclerosis, overgrowth, and deformity of the bone [8].. The bony irregularities were used as an advantage to locate the tumour intraoperatively. In our case, we used 3D technology to locate the position of the tumour in relation to the bony irregularities, and a specific jig/guide was fabricated in such a way that it contoured over the tumour mass, and the tumour was excised completely with 2 mm margins of normal bone that did not require any supplementation with bone graft for internal fixation. The advantage of this technology is that it allows one to precisely locate the tumour intraoperatively with the help of the model. The margins required to be removed can be planned beforehand, and the guide can be fabricated accordingly. This does not require the use of any intraoperative radiographs or other imaging. Though it requires surgical exposure, it is limited just enough to place the guide. Without the use of any kind of intraoperative imaging, we were able to successfully retrieve the entire nidus for histopathological confirmation. This technology can also be used to reach various bone tumours and lesions using a fabricated guide, avoiding extensive surgical exposure and reducing operative time.
Ren et al. [9] used 3D printing guides to reach the OO of calcaneus for resection, and there are many studies where this technology is used for the resection of malignant tumours [10]. In our study, we used a guide to identify the tumour and resect is precisely, and we believe this technique has not been described in the literature in the use of osteoid osteoma where intraoperative imaging can be avoided.
Limitations with the technology are that press-fit guides may be difficult to design on bones with a normal cortical surface, and instead, we may have to use a fixed bony landmark closer to the lesion.
In conclusion, we believe that additive manufacturing (or 3D printing) is a new age technology that can be used to resect various bony lesions, including osteoid osteoma, by fabricating personalised guides that can lead us to the tumour with minimal surgical exposure, aid resection, reduce operative time, and limit radiation exposure to the patient and the surgeon.
Acknowledgements
The authors thank the Common Engineering Facility Centre (CEFC) at IISc for access to the 3D printer. We appreciate the support rendered by Dr Chandrashekar H S, Director of Sanjay Gandhi Institute of Trauma and Orthopaedics and Dr Frederik Verstrekan for inspiring us.
Funding
The author(s) received NO financial support for the preparation, research, authorship, and/or publication of this manuscript.
Declarations
Conflict of interest
The author(s) do NOT have any potential conflicts of interest with respect to this manuscript.
Ethical approval
This study is exempted from ethical approval.
Statement of consent
The patient and the guardians were informed about the publication and consent was obtained regarding the same.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Boscainos PJ, Cousins GR, Kulshreshtha R, Oliver TB, Papagelopoulos PJ. Osteoid osteoma. Orthopedics. 2013;36(10):792–800. doi: 10.3928/01477447-20130920-10. [DOI] [PubMed] [Google Scholar]
- 2.Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. Journal of Bone and Joint Surgery. American Volume. 1998;80(6):815–821. doi: 10.2106/00004623-199806000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Campanacci M, Ruggieri P, Gasbarrini A, Ferraro A, Campanacci L. Osteoid osteoma. The Journal of Bone and Joint Surgery. British Volume. 1999;81(5):814–820. doi: 10.1302/0301-620X.81B5.0810814. [DOI] [PubMed] [Google Scholar]
- 4.Klein MH, Shankman S. Osteoid osteoma: Radiologic and pathologic correlation. Skeletal Radiology. 1992;21(1):23–31. doi: 10.1007/BF00243089. [DOI] [PubMed] [Google Scholar]
- 5.Lee DH, Malawer MM. Staging and treatment of primary and persistent (recurrent) osteoid osteoma Evaluation of intraoperative nuclear scanning, tetracycline fluorescence, and tomography. Clinical Orthopaedics. 1992;281:229–238. [PubMed] [Google Scholar]
- 6.Healey JH, Ghelman B. Osteoid osteoma and osteoblastoma. Current concepts and recent advances. Clinical Orthopaedics. 1986;204:76–85. [PubMed] [Google Scholar]
- 7.Gitelis S, Schajowicz F. Osteoid osteoma and osteoblastoma. Orthopaedics Clinical North America. 1989;20(3):313–325. [PubMed] [Google Scholar]
- 8.Norman A, Dorfman HD. Osteoid-osteoma inducing pronounced overgrowth and deformity of bone. Clinical Orthopaedics. 1975;110:233–238. doi: 10.1097/00003086-197507000-00033. [DOI] [PubMed] [Google Scholar]
- 9.Ren, X., Yang, L., & Duan, X.J. (2017). Three-dimensional printing in the surgical treatment of osteoid osteoma of the calcaneus: A case report. J Int Med Res, 45(1):372–380.10.1177/0300060516686514. PMID: 28222618. [DOI] [PMC free article] [PubMed]
- 10.Park JW, Kang HG, Lim KM, Park DW, Kim JH, Kim HS. Bone tumor resection guide using three-dimensional printing for limb salvage surgery. Journal of Surgical Oncology. 2018;118(6):898–905. doi: 10.1002/jso.25236. [DOI] [PubMed] [Google Scholar]