To the editor:
Hypnosis is an induced physiological and dynamic mental state characterized by dissociation and dissipation of attention. Thanks to the physician-patient relationship it is possible to induce a state of relaxation and focused attention on a particular idea or image. In this way it is achievable to induce psychic, somatic and visceral modifications in the patient [1]. We used hypnosis in association with general anesthesia for major hepatic surgery. The patient was a 56-years-old male (height of 185 cm and weight of 95 kg) candidate for orthotopic liver transplantation (OLT) because of persistent liver metastasis secondary to a previous colorectal cancer. The anesthesiological risk of the patient was ASA 3 [2]. Before the orthotopic liver transplantation, the patient performed a preliminary interview and two preparation sessions to assess his responsiveness to relaxation stimuli and his susceptibility to hypnotic analgesia. The protocol we used to perform hypnosis during the preparatory sessions and the day of the liver transplantation was characterized by the following phases as shown in Fig. 1.
Fig. 1.
Clinical operative sequence for hypnosis implementation to general anesthesia.
First phase – mental relaxation and induction of a state of sedateness (5 min)
We started equipping the patient on the operating table with high resolution audio headphones that allow to listen to both the hypnotist, equipped with a microphone, and music. The relaxation induced by music is the prelude to the verbalized phase during which the patient is invited to welcome the environment and to take a comfortable posture facilitating his body and mental relaxation.
Second phase - progressive muscle relaxation (10 min)
Relaxation reduces stress, anxiety and fear facilitating a sense of empowerment. The use of a regressive numeric count improve internal focus facilitating verbalized suggestions of relaxation. The patient gradually increases his internal focus through attention to his breath and to different districts of his own body. At first, patient concentration is focused on his head and then, in sequence, downwards to his feet. In this way the association of the regressive numeric count from 10 to 1 imply the suggestion of going deeper and deeper into the hypnotic experience.
Third phase - experience of a safety place (15 min)
We induce the patient to imagine of bringing his attention to a “Safe Place”. We performed this process using suggestions without specific content but capable of diverting the subject's attention from surgical environment to a virtual reality. This new “safe place” evoked by patient mental images has the features of a real experience in a general condition of well-being, strangeness and security.
General anesthesia
We induced general anesthesia at 05:30, when the patient reached a deep hypnotic state. A dose of 1.5 mg kg−1 of propofol 10%, a dose of 0.13 μg kg−1 on lean body mass (LBM) of sufentanyl and a dose of 12 mg of cisatracurium were administered intravenously. After intubation, sevoflurane was used for maintenance of general anesthesia in combination with sufentanyl 0.1 μg kg−1 h on LBM and cisatracurium 3 mg h. We also supported arterial pressure levels with noradrenaline tartrate 0.05 μg kg−1 min because OLT is characterized by hemodynamic instability due to vasoactive circulating hepatic metabolites. The surgical operation started at 07:40 and finished at 18:40. At 18:45 we interrupted all pharmacological administrations and we repositioned the headphones for hypnosis.
Fourth phase - exit from hypnosis and reorientation (10 min)
The exit from hypnosis consisted in inviting the patient to a slow but progressive physical and environmental reorientation. Patient ordinary flow of consciousness and awareness was gradually restored by following a numerical count inverse to the induction phase, counting from 1 to 10. The gradual patient perceptions rehabilitation of his own body was performed while maintaining and reinforcing suggestions of well-being already achieved during previous phases of the procedure.
Scientific literature describes efficacy of hypnosis in numerous fields such as interventional procedures, regional anesthesia, transesophageal echocardiography and in obstetrics as support in mitigating anxiety, stress and pain [3,4]. Makovac et al. reported as hypnosis combined with local anesthesia provides an effective alternative in selected patients with very high anesthesiological risk [5]. Montenegro et al. indicate hypnosis as a valuable tool in pain management of patients subjected to surgical procedures in the maxillofacial complex [6]. Werner et al. conducted a RCT with 1222 nulliparous women reporting that a brief course in self-hypnosis clinically improved the women's childbirth experience [7]. Our main aim is to propose hypnosis as a valid aid to anesthesiological management in improving patient compliance and tolerance to medical procedures even in major surgery.
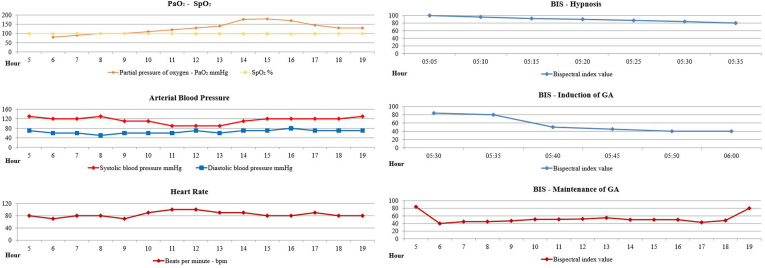
From the point of view of patient vital signs, we reported an overall stability for the entire duration of anesthesiological management (Fig. 2). Blood oxygenation parameters, evaluated through peripheral capillary oxygen saturation (SpO₂), and partial pressure of oxygen (PaO₂), evaluated every hour with an arterial blood gas test, were stable for the entire duration of the surgery. From a cardiovascular point of view, we observed after induction of anesthesia a slight reduction in arterial pressure from 140/70 mmHg to 115/60 mmHg and a reduction heart rate from 80 bpm to 70 bpm. We used BIS (Medtronic-Covidien, Dublin, Ireland) to assess the hypnotic status of the patient and we considered a deep hypnotic state a reduction of BIS value to 85–80 [8]. After induction BIS value was 50 and it remained stable between 40 and 50 values for the rest of the surgical operation. Another aspect to note is that our patient subjected to hypnosis experienced a better comfort during invasive procedures before the induction of general anesthesia. In particular he well tollerated the positioning of peripheral venous catheters (16G) in large caliber veins and the cannulation of the radial artery for invasive blood pressure monitoring.
Fig. 2.
Vital parameters during anesthesiological management.
Our patient experienced an overall state of well-being in dealing with general anesthesia and in the future hypnosis may play a role for the personalization of patient clinical experience by reducing perioperative anxious states and guaranteeing maximum patient collaboration.
Annals of medicine and surgery
The following information is required for submission. Please note that failure to respond to these questions/statements will mean your submission will be returned. If you have nothing to declare in any of these categories then this should be stated.
Funding
None to declare.
Ethical approval
None to declare.
Consent
Written informed consent was obtained from the patient for publication.
Author contribution
Eros Pilia: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Visualization.
Danilo Sirigu: Conceptualization, Methodology, Validation, Writing - Original Draft. Roberto Mereu: Methodology, Formal analysis, Investigation, Resources, Data Curation, Writing - Original Draft.
Fausto Zamboni: Methodology, Resources, Data Curation, Supervision, Project administration.
Elisabetta Pusceddu: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Data Curation, Writing - Original Draft, Supervision, Project administration.
Registration of research studies
-
1.
Name of the registry:
None to declare.
-
2.
Unique Identifying number or registration ID:
None to declare.
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
None to declare.
Guarantor
Pilia Eros.
Danilo Sirigu.
Roberto Mereu.
Fausto Zamboni.
Elisabetta Pusceddu.
Declaration of competing interest
None to declare.
Acknowledgement
This manuscript was published with the written consent of the patient. No external funding or competing interests declared.
References
- 1.Elkins G.R. Springer; New York: 2017. Handbook of Medical and Psychological Hypnosis. [Google Scholar]
- 2.Doyle D.J., Goyal A., Garmon E.H. StatPearls [Internet]. Treasure Island (FL) StatPearls Publishing; 2022 Jan. American society of anesthesiologists classification. 2021 oct 9. PMID: 28722969. [PubMed] [Google Scholar]
- 3.Montis S., Sirigu D., Marini A., Lai A., Setti P., Camboni M., Mura G.C., Congia M., Manca D., Marini E., Merola A., Orrù L., Scano F., Stara R., Urru M., Tumbarello R. L’ipnosi nell’ecocardiografia transesofagea. L’esperienza di un Centro di Cardiologia Pediatrica e delle Cardiopatie Congenite [Hypnosis in transesophageal echocardiography. The experience in a Pediatric Cardiology and Congenital Heart Disease Unit] G. Ital. Cardiol. 2019 Nov;20(11):651–657. doi: 10.1714/3254.32226. Italian. PMID: 31697272. [DOI] [PubMed] [Google Scholar]
- 4.Facco E., Pasquali S., Zanette G., Casiglia E. Hypnosis as sole anaesthesia for skin tumour removal in a patient with multiple chemical sensitivity. Anaesthesia. 2013 Sep;68(9):961–965. doi: 10.1111/anae.12251. Epub 2013 Jul 12. PMID: 23845031. [DOI] [PubMed] [Google Scholar]
- 5.Makovac P., Potié A., Roukain A., Pucci L., Rutz T., Kopp P.A., Matter M. Hypnosis and superficial cervical anesthesia for total thyroidectomy in a high-risk patient - a case report. Int J Surg Case Rep. 2020;72:133–136. doi: 10.1016/j.ijscr.2020.05.078. Epub 2020 Jun 6. PMID: 32535527; PMCID: PMC7298319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montenegro G., Alves L., Zaninotto A.L., Falcão D.P., de Amorim R.F. Hypnosis as a valuable tool for surgical procedures in the oral and maxillofacial area. Am. J. Clin. Hypn. 2017 Apr;59(4):414–421. doi: 10.1080/00029157.2016.1172057. PMID: 28300520. [DOI] [PubMed] [Google Scholar]
- 7.Werner A., Uldbjerg N., Zachariae R., Wu C.S., Nohr E.A. Antenatal hypnosis training and childbirth experience: a randomized controlled trial. Birth. 2013 Dec;40(4):272–280. doi: 10.1111/birt.12071. PMID: 24344708. [DOI] [PubMed] [Google Scholar]
- 8.Dunham C.M., Burger A.J., Hileman B.M., Chance E.A., Hutchinson A.E. Bispectral index alterations and associations with autonomic changes during hypnosis in trauma center researchers: formative evaluation study. JMIR Form. Res. 2021 May 26;5(5) doi: 10.2196/24044. PMID: 34037529; PMCID: PMC8190650. [DOI] [PMC free article] [PubMed] [Google Scholar]